1 Approach to Azotemia Dr Shahrzad Shahidi Professor










- Slides: 68

1
Approach to Azotemia Dr. Shahrzad Shahidi Professor of Nephrology Isfahan University of Medical Sciences 2

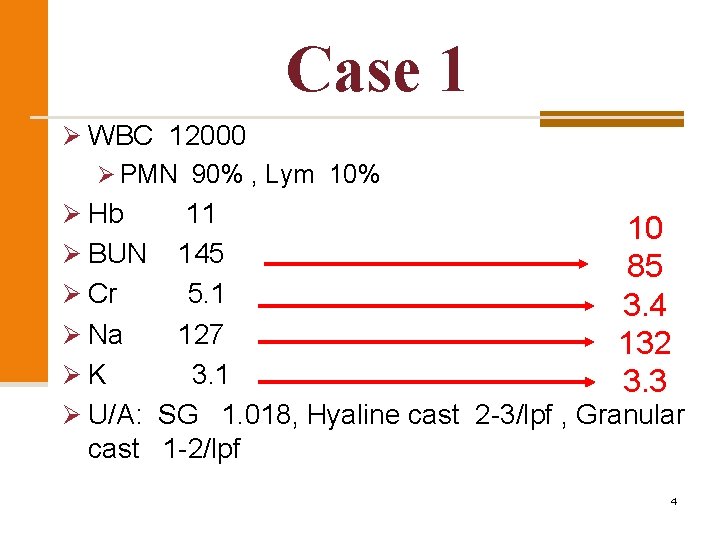
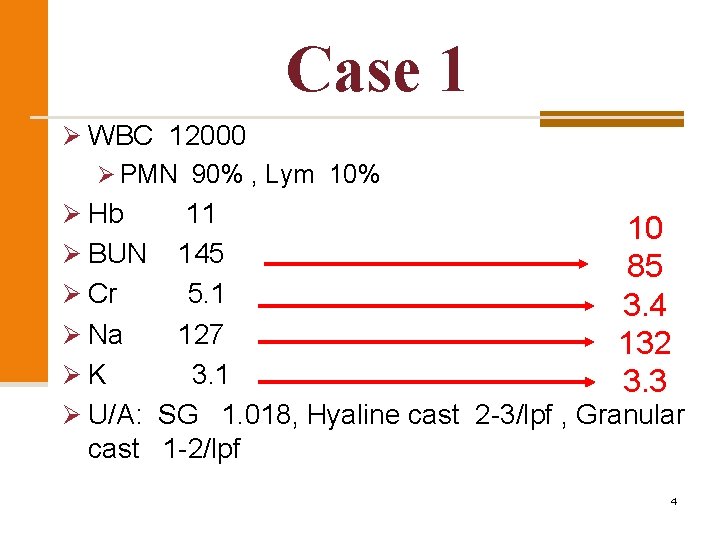
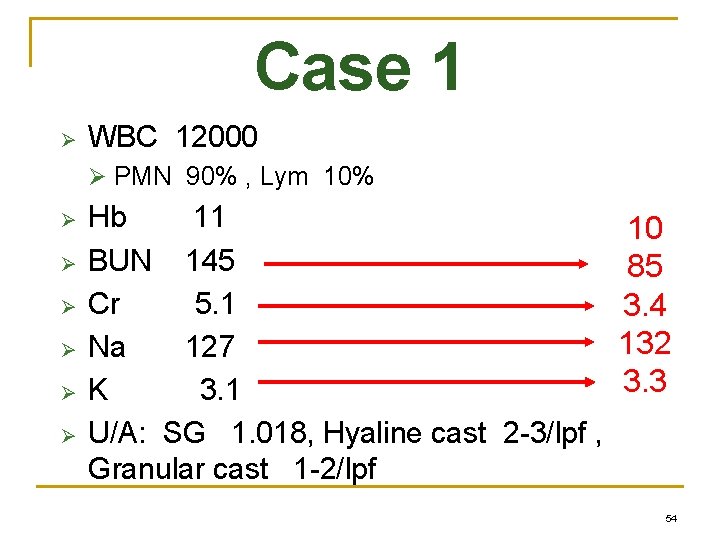
Case 1 Ø WBC 12000 Ø PMN 90% , Lym 10% Ø Hb 11 after 3 days of admission Ø BUN 145 Ø Cr 5. 1 Ø Na 127 Ø K 3. 1 10 85 3. 4 132 3. 3 Ø U/A: SG 1. 018, Hyaline cast 2 -3/lpf , Granular cast 1 -2/lpf 4

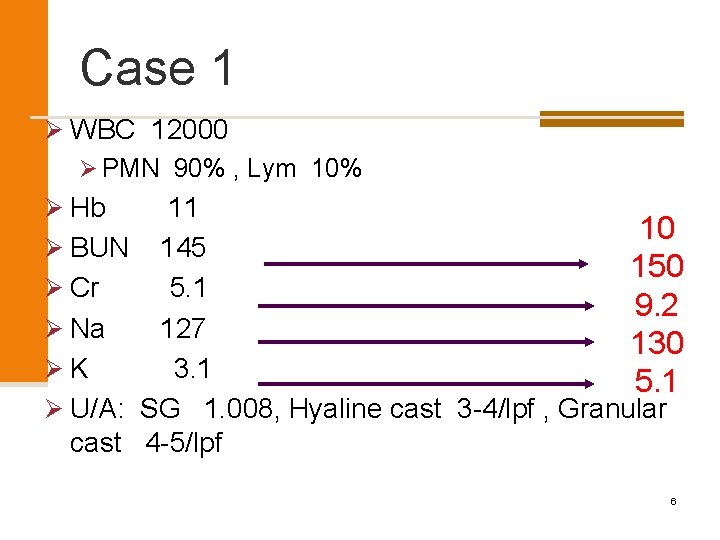
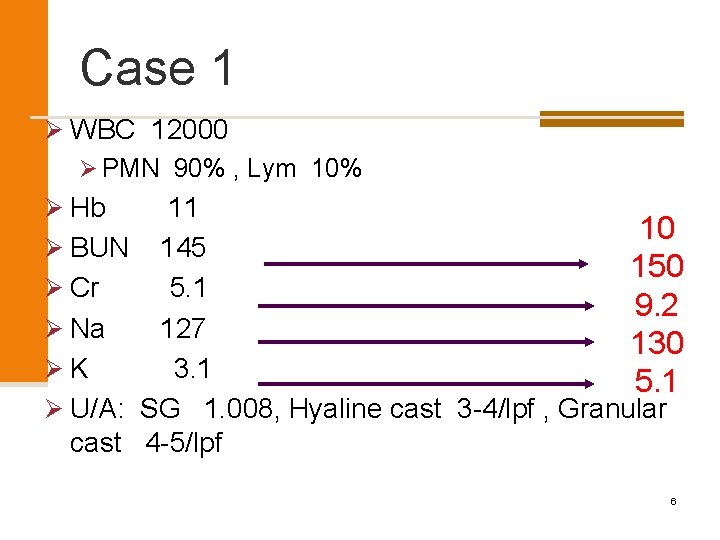
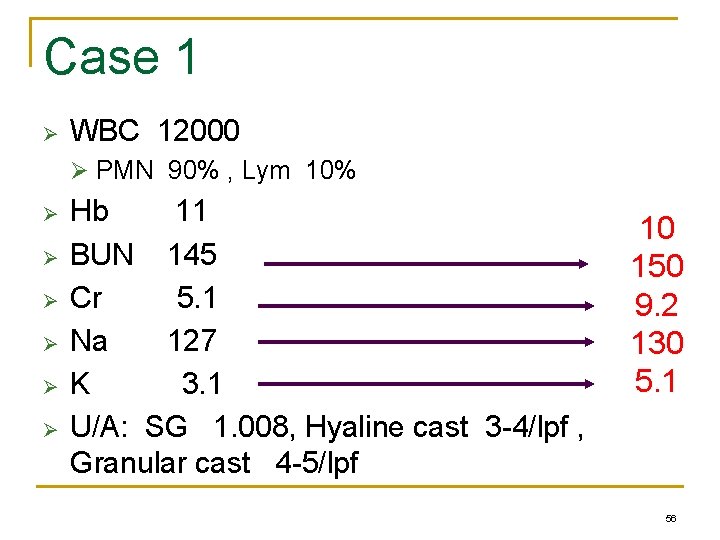
Case 1 Ø WBC 12000 Ø PMN 90% , Lym 10% Ø Hb 11 after 3 days of admission Ø BUN 145 10 150 9. 2 130 5. 1 Ø Cr 5. 1 Ø Na 127 Ø K 3. 1 Ø U/A: SG 1. 008, Hyaline cast 3 -4/lpf , Granular cast 4 -5/lpf 6

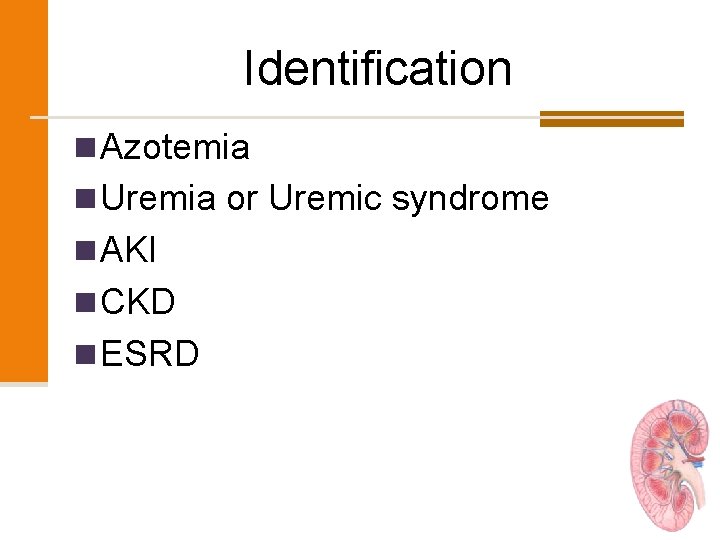
Identification n Azotemia n Uremia or Uremic syndrome n AKI n CKD n ESRD 8
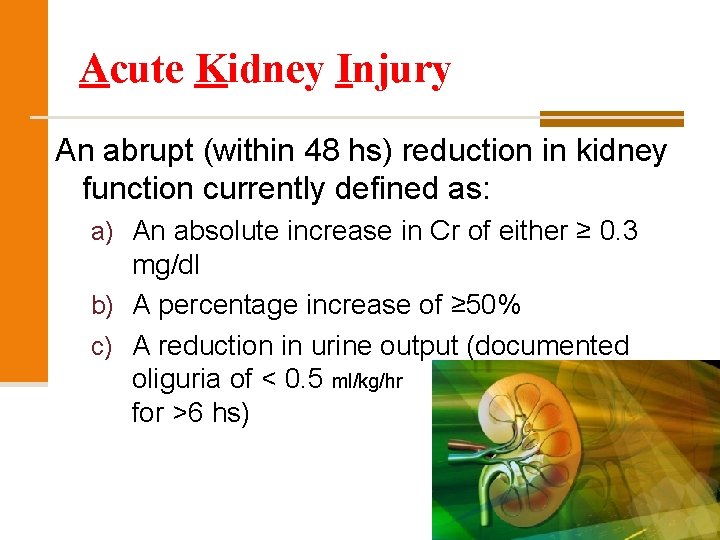
Acute Kidney Injury An abrupt (within 48 hs) reduction in kidney function currently defined as: a) An absolute increase in Cr of either ≥ 0. 3 mg/dl b) A percentage increase of ≥ 50% c) A reduction in urine output (documented oliguria of < 0. 5 ml/kg/hr for >6 hs) 9
D. D of Azotemia 1. Acute Kidney Injury (AKI) 2. Chronic Kidney Disease (CKD) 3. Acute worsening of CRF or Acute on Chronic Renal Failure 10
D. D of Azotemia 1. Acute Kidney Injury (AKI) 2. Chronic Kidney Disease (CKD) 3. Acute worsening of CRF or Acute on Chronic Renal Failure 11
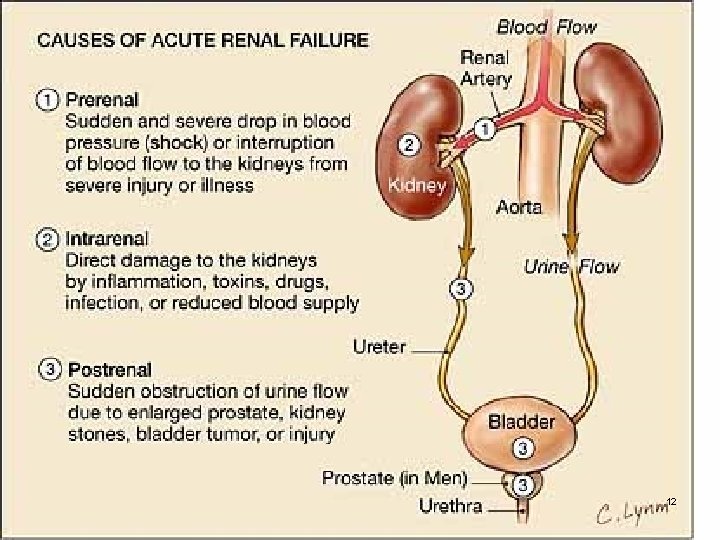
12
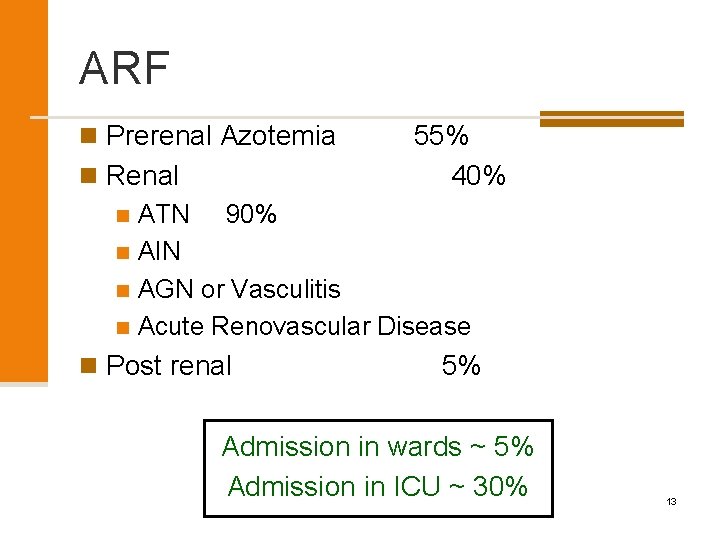
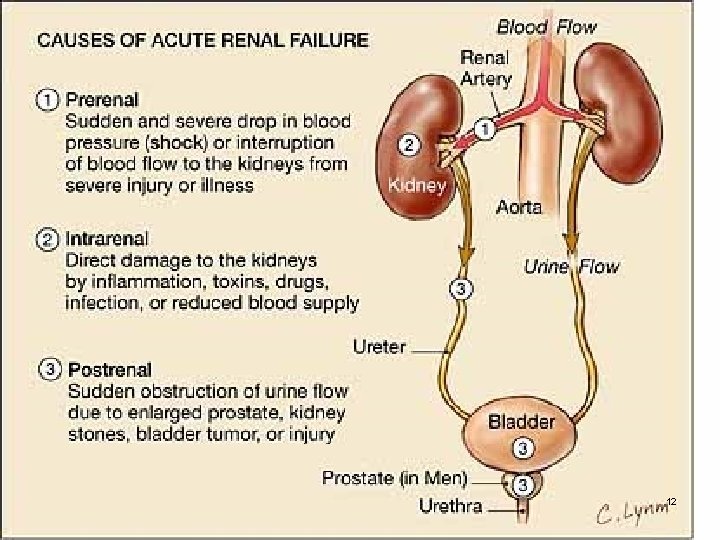
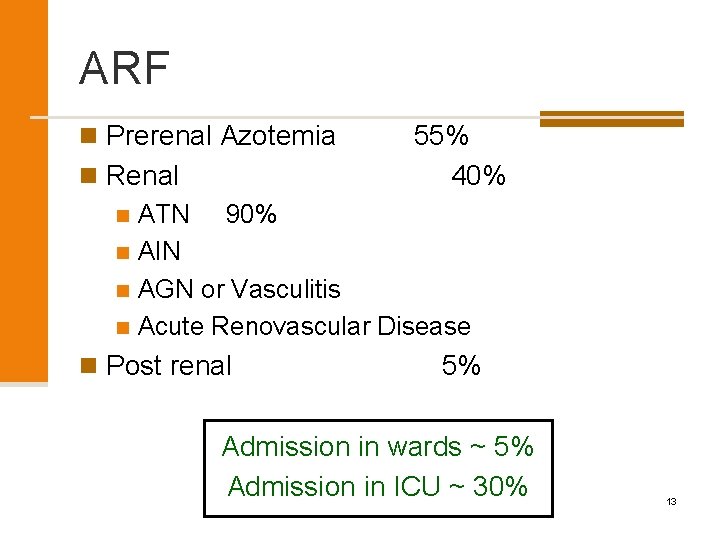
ARF n Prerenal Azotemia 55% n Renal 40% n ATN 90% n AIN n AGN or Vasculitis n Acute Renovascular Disease n Post renal 5% Admission in wards ~ 5% Admission in ICU ~ 30% 13
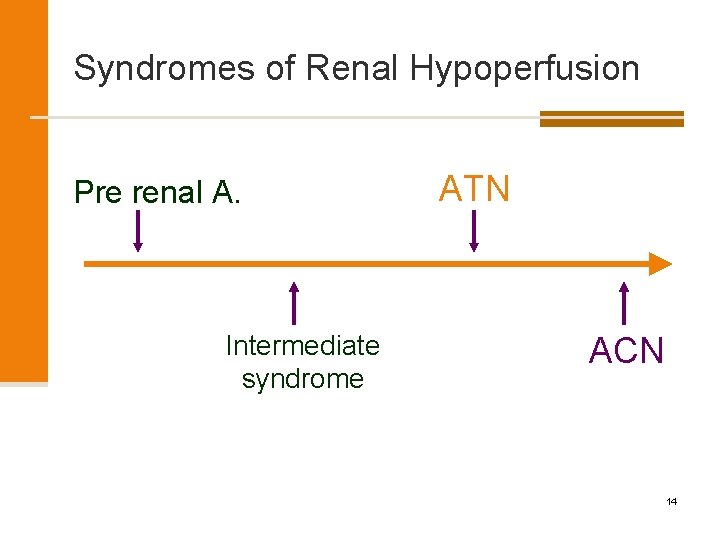
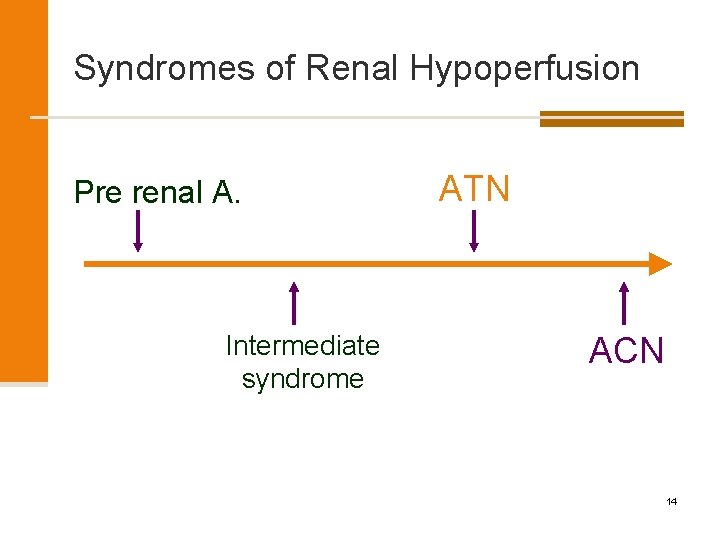
Syndromes of Renal Hypoperfusion Pre renal A. Intermediate syndrome ATN ACN 14
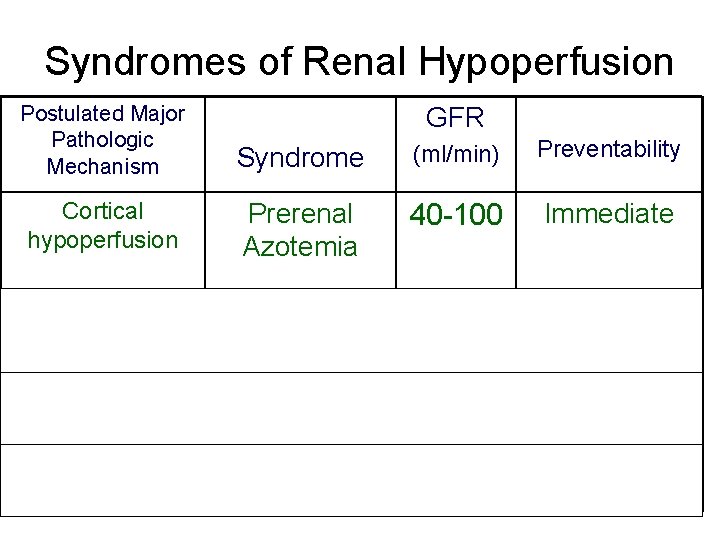
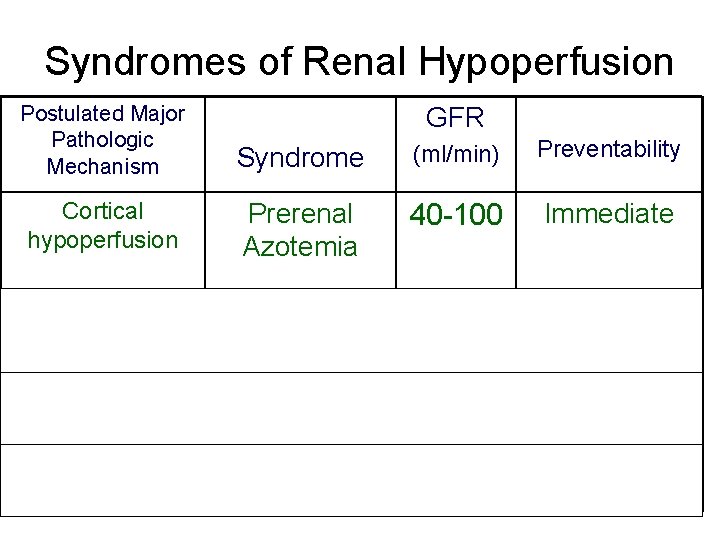
Syndromes of Renal Hypoperfusion Postulated Major Pathologic Mechanism Syndrome (ml/min) Preventability Cortical hypoperfusion Prerenal Azotemia 40 -100 Immediate Medullary hypoperfusion GFR Intermediate 20 - 60 syndrome Medullary ischemia ATN 0 - 25 Cortical ischemia ACN 0 - 5 Within 1– 3 days Within 1– 3 weeks Unpredictable 15
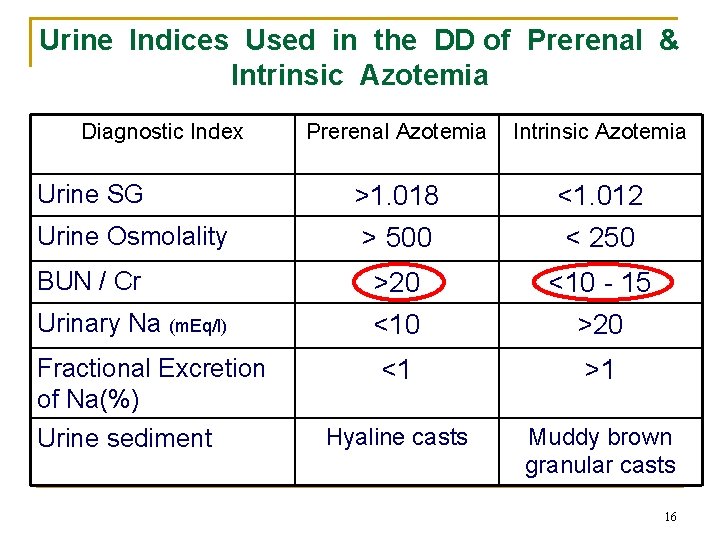
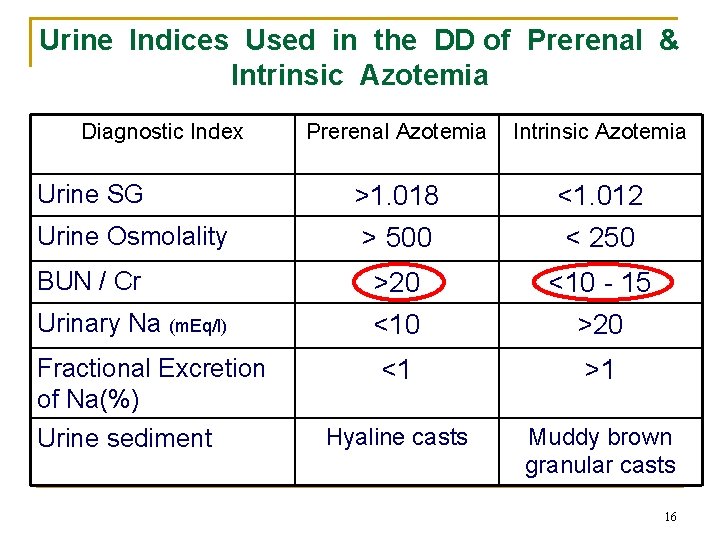
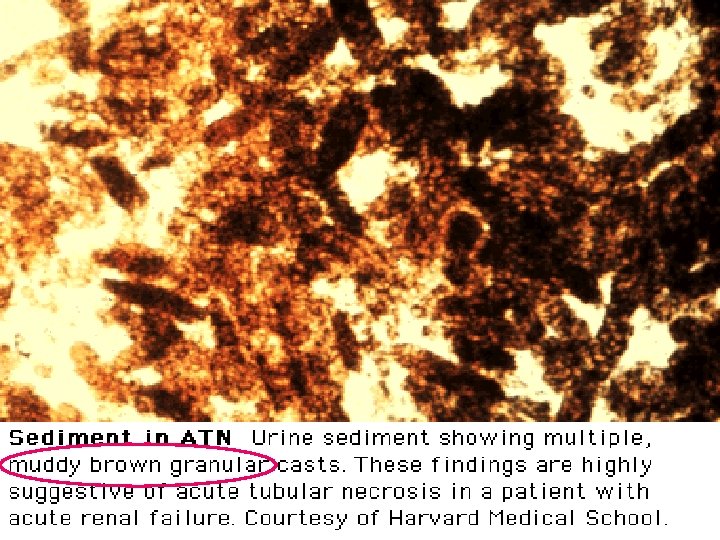
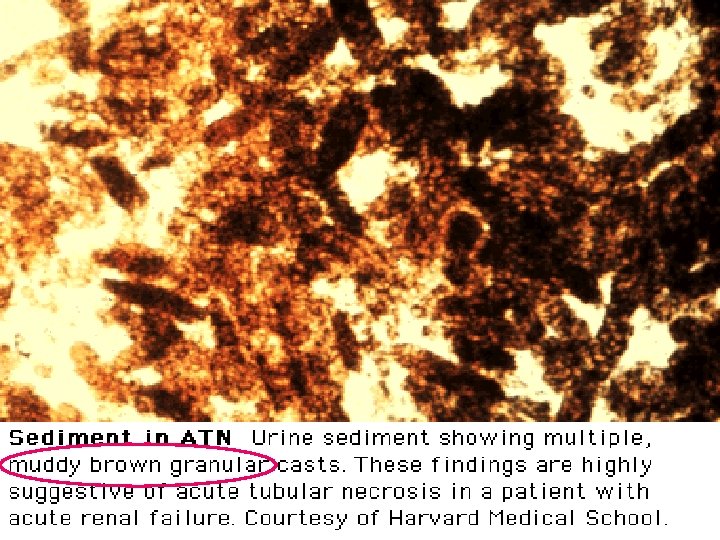
Urine Indices Used in the DD of Prerenal & Intrinsic Azotemia Diagnostic Index Prerenal Azotemia Intrinsic Azotemia >1. 018 > 500 <1. 012 < 250 BUN / Cr >20 <10 - 15 Urinary Na (m. Eq/l) <10 >20 Fractional Excretion of Na(%) Urine sediment <1 >1 Hyaline casts Muddy brown granular casts Urine SG Urine Osmolality 16
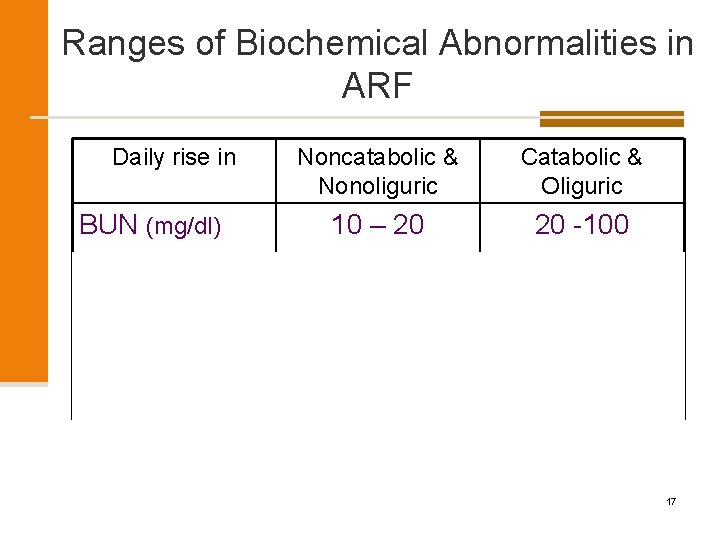
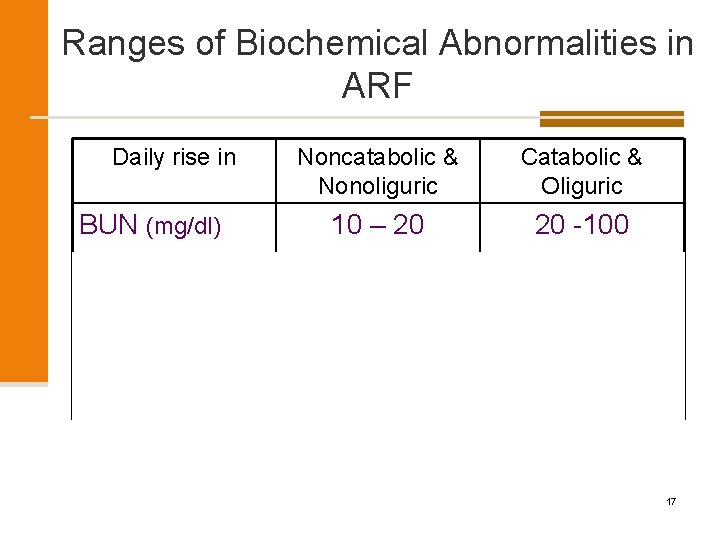
Ranges of Biochemical Abnormalities in ARF Daily rise in Noncatabolic & Nonoliguric Catabolic & Oliguric BUN (mg/dl) 10 – 20 20 -100 Cr (mg/dl) 0. 5 – 1 > 2 K (m. Eq/l) < 0. 5 1 – 2 (more) < 1 > 2 Hco 3 (m. Eq/l) 17
Acute Kidney Injury Spectrum of disorders from reduced function to established failure Multi-factorial causes 18
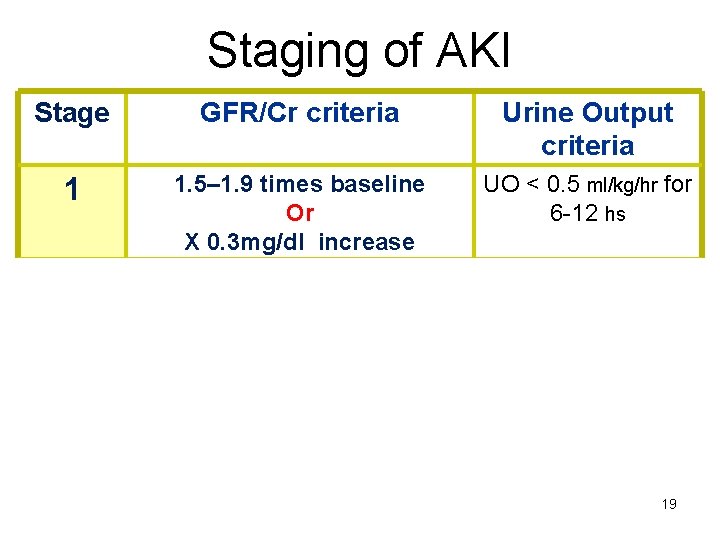
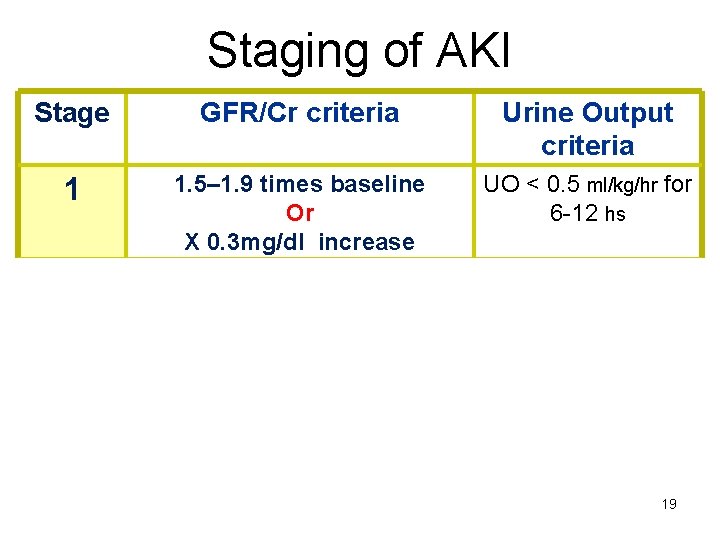
Staging of AKI Stage GFR/Cr criteria Urine Output criteria 1 1. 5– 1. 9 times baseline Or X 0. 3 mg/dl increase UO < 0. 5 ml/kg/hr for 6 -12 hs 2 2. 0– 2. 9 times baseline 3 3. 0 times baseline Or Increase in Cr to X 4. 0 mg/dl Or Initiation of RRT UO < 0. 5 ml/kg/hr for 12 hrs UO < 0. 3 ml/kg/hr for 24 hs Or Anuria for 12 hrs 19
AKI Outcome & Prognosis n The development of AKI is associated with a significantly increased risk of in -hospital & long-term mortality, longer length of stay, & increased costs. n Survivors of an episode of AKI requiring temporary dialysis, are at extremely high risk for progressive CKD, & up to 10% may develop ESRD. 20
AKI Outcome & Prognosis n Postdischarge care under the supervision of a nephrologist for aggressive secondary prevention of kidney disease is prudent. n Patients with AKI are more likely to die prematurely after they leave the hospital even if their kidney function has recovered. 21
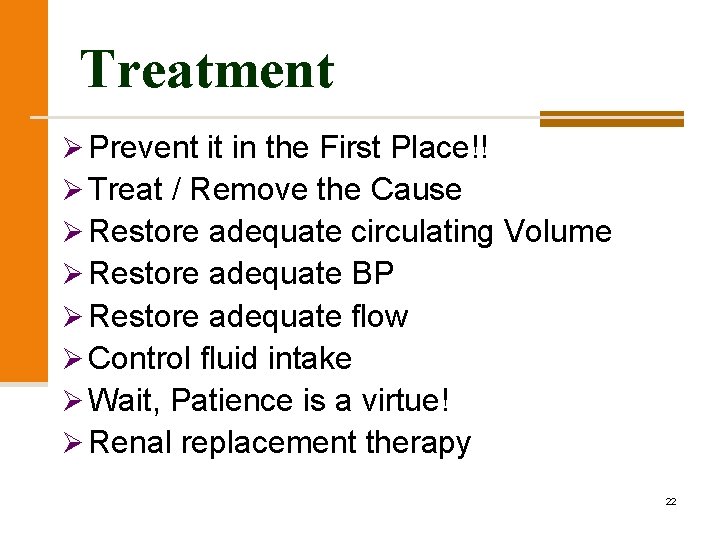
Treatment Ø Prevent it in the First Place!! Ø Treat / Remove the Cause Ø Restore adequate circulating Volume Ø Restore adequate BP Ø Restore adequate flow Ø Control fluid intake Ø Wait, Patience is a virtue! Ø Renal replacement therapy 22
D. D of Azotemia 1. Acute Renal Failure (ARF) 2. Chronic Kidney Disease (CKD) 3. Acute worsening of CRF or Acute on Chronic Renal Failure 23
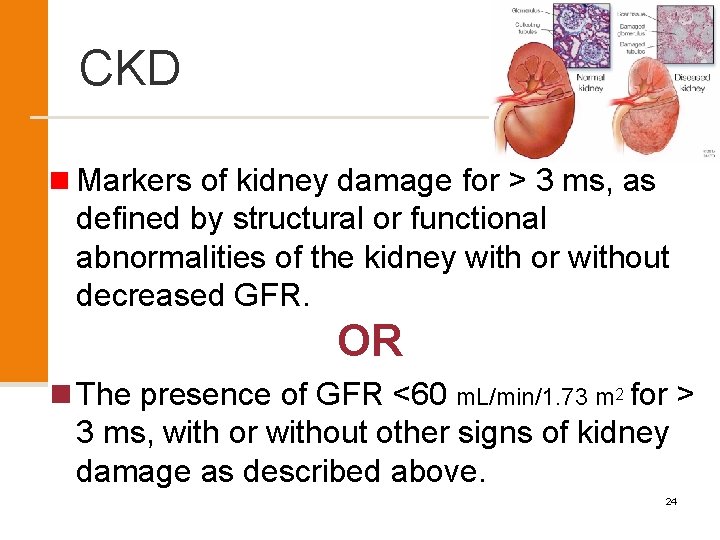
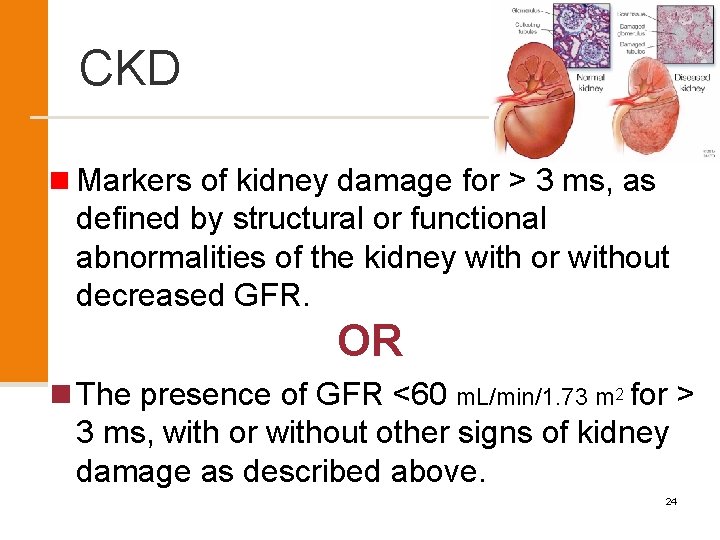
CKD n Markers of kidney damage for > 3 ms, as defined by structural or functional abnormalities of the kidney with or without decreased GFR. OR n The presence of GFR <60 m. L/min/1. 73 m 2 for > 3 ms, with or without other signs of kidney damage as described above. 24
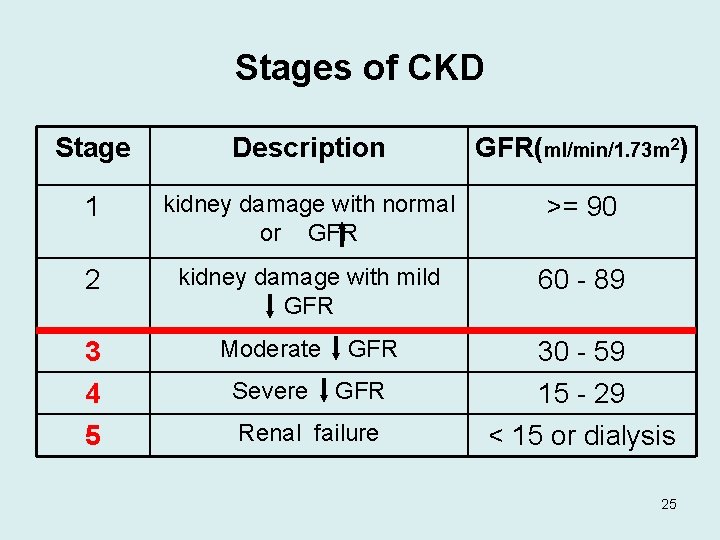
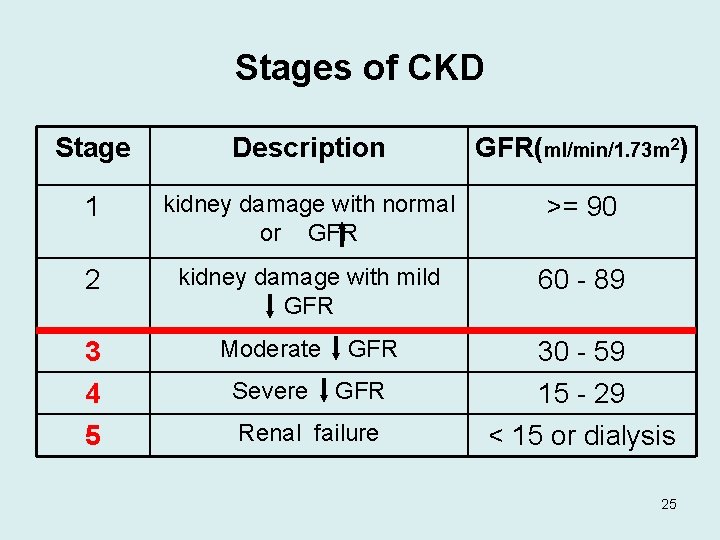
Stages of CKD Stage Description GFR(ml/min/1. 73 m 2) 1 kidney damage with normal or GFR >= 90 2 3 4 5 kidney damage with mild GFR Moderate GFR Severe GFR Renal failure 60 - 89 30 - 59 15 - 29 < 15 or dialysis 25
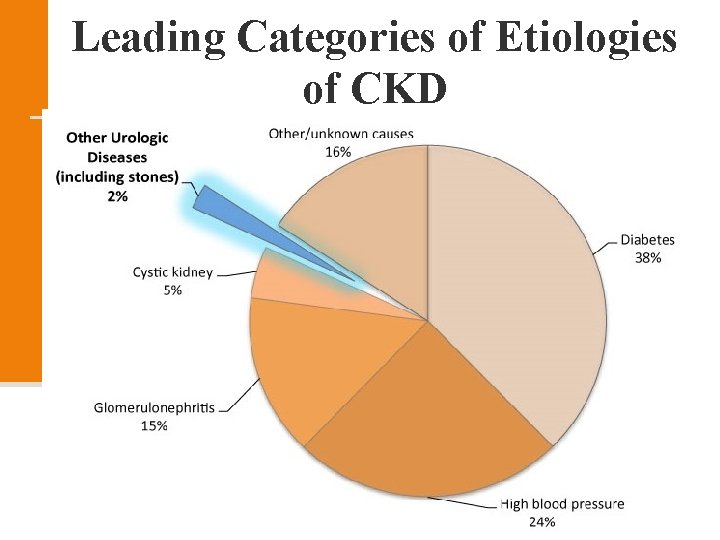
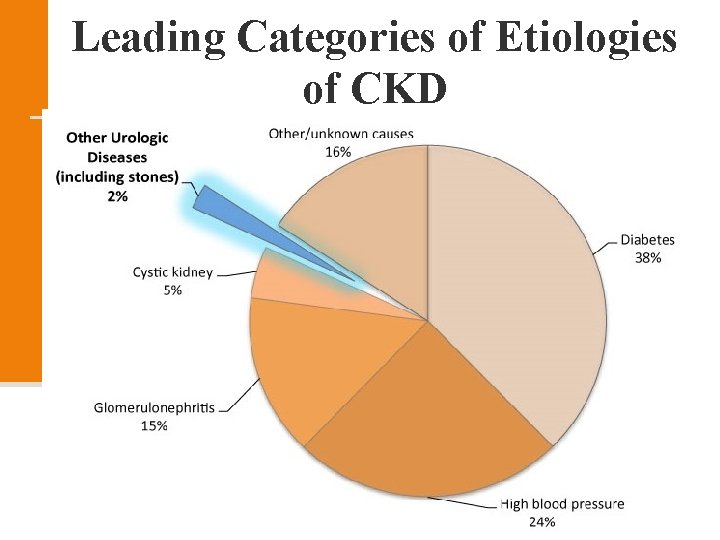
Leading Categories of Etiologies of CKD n Diabetic glomerular disease n Hypertensive nephropathy n Glomerulonephritis n Autosomal dominant polycystic kidney disease n Other cystic & tubulointerstitial nephropathy 26
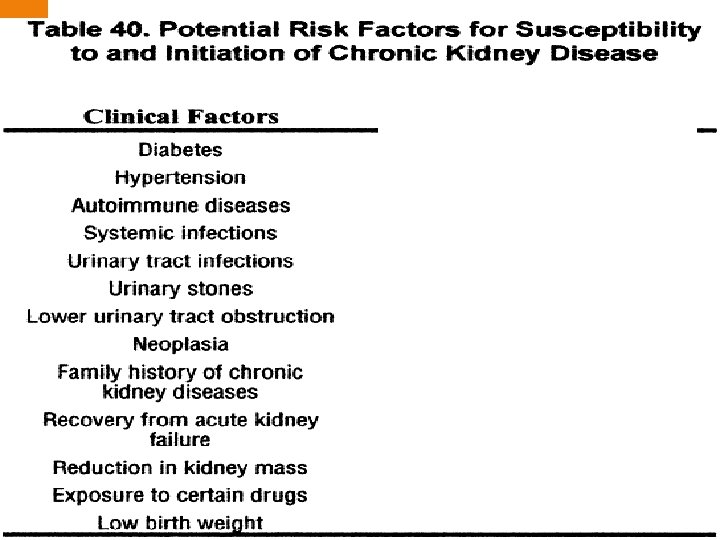
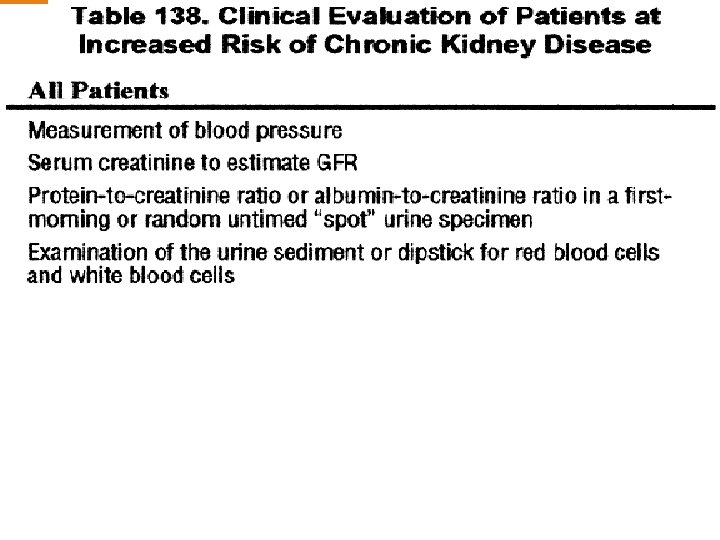
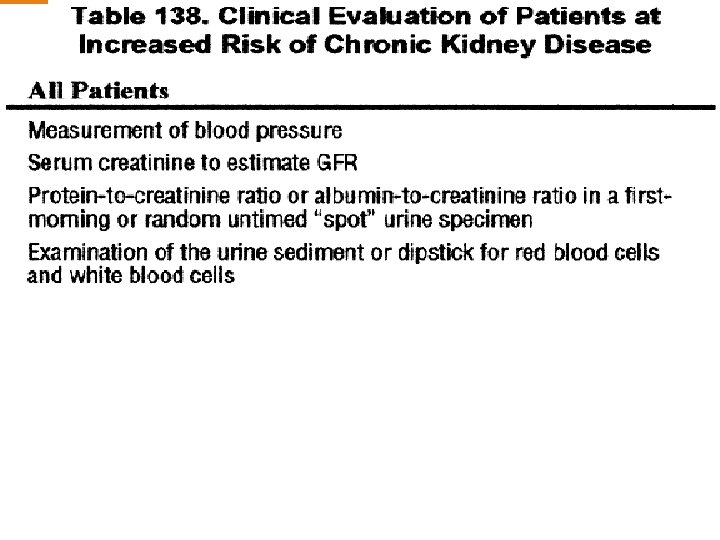
Screening of CKD Individuals at high risk for kidney disease. 27
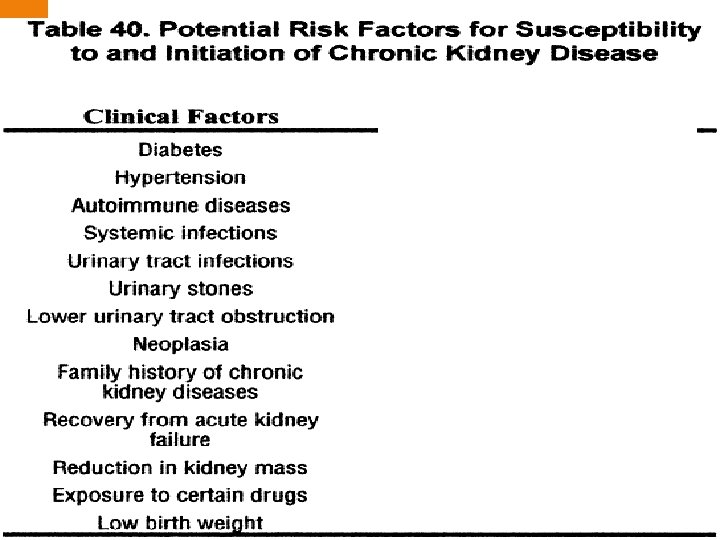
28
29
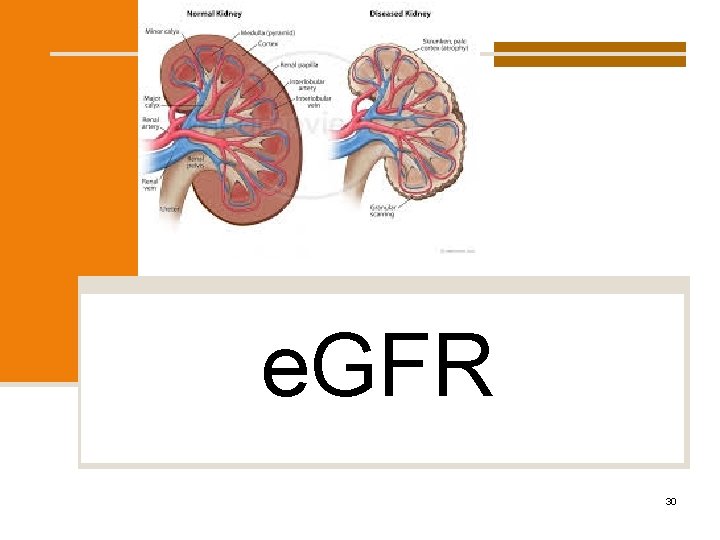
e. GFR 30
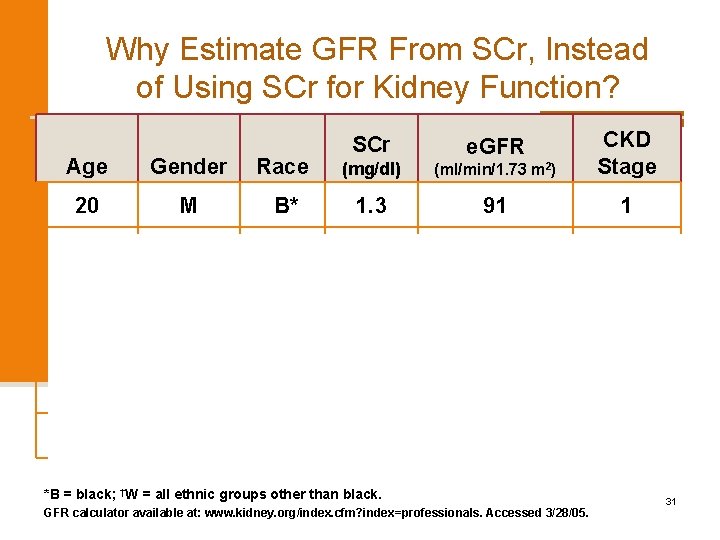
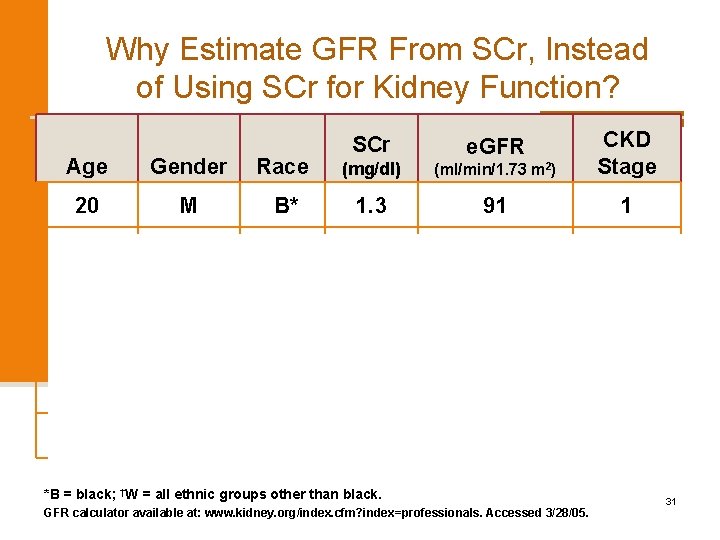
Why Estimate GFR From SCr, Instead of Using SCr for Kidney Function? Age Gender Race (mg/dl) (ml/min/1. 73 m 2) CKD Stage 20 M B* 1. 3 91 1 20 M W† 1. 3 75 2 55 M W 1. 3 61 2 20 F W 1. 3 56 3 55 F B 1. 3 55 3 50 F W 1. 3 46 3 SCr e. GFR *B = black; †W = all ethnic groups other than black. GFR calculator available at: www. kidney. org/index. cfm? index=professionals. Accessed 3/28/05. 31
e. GFRcreat Report e. GFRcreat in adults using the 2009 CKDEpidemiology Collaboration (CKD-EPI) cr equation 32
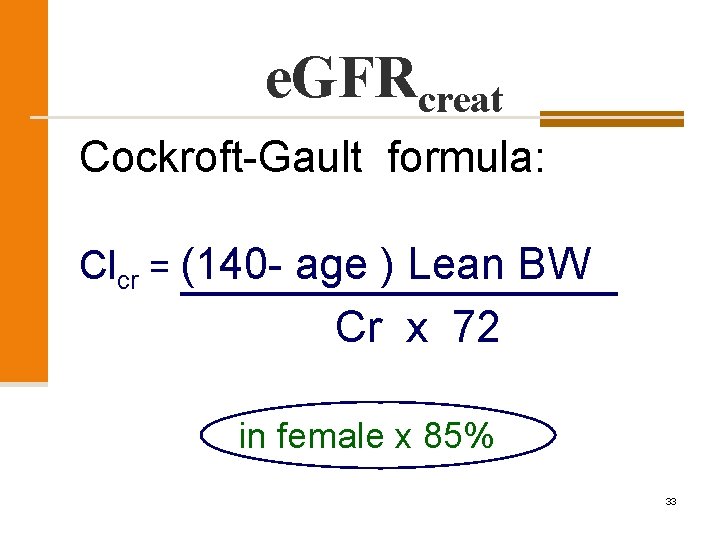
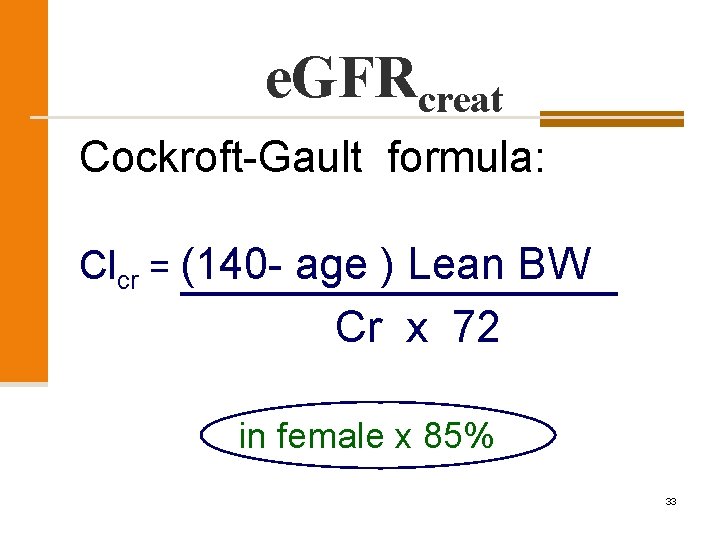
e. GFRcreat Cockroft-Gault formula: Clcr = (140 - age ) Lean BW Cr x 72 in female x 85% 33
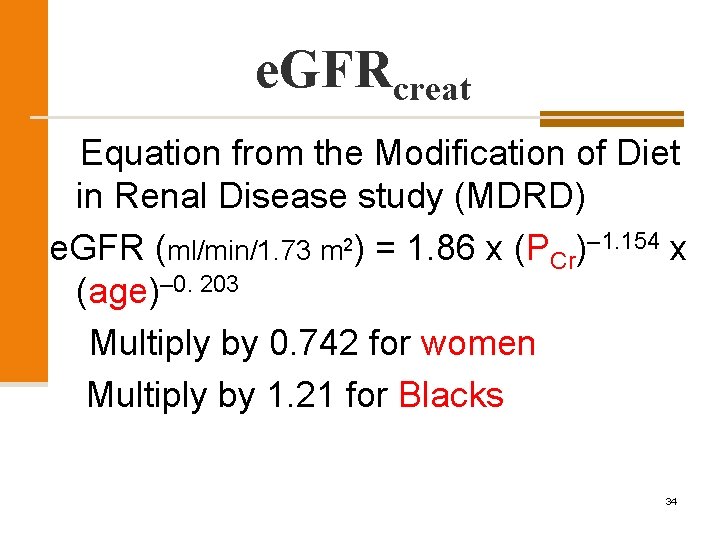
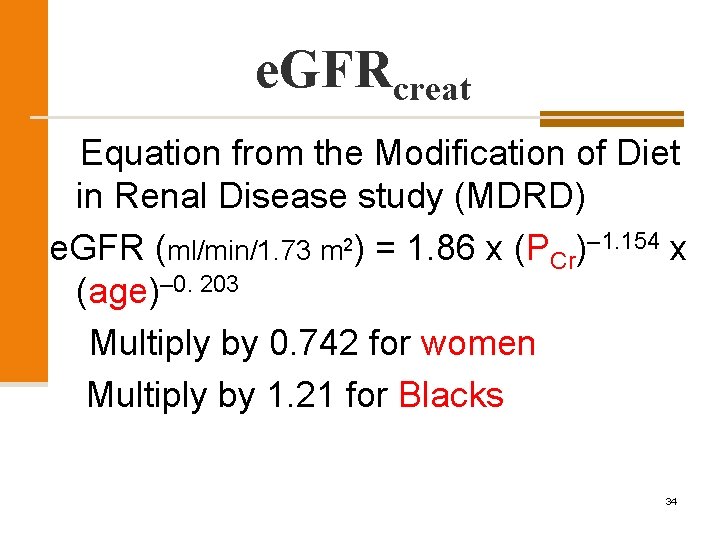
e. GFRcreat Equation from the Modification of Diet in Renal Disease study (MDRD) e. GFR (ml/min/1. 73 m 2) = 1. 86 x (PCr)– 1. 154 x (age)– 0. 203 Multiply by 0. 742 for women Multiply by 1. 21 for Blacks 34
D. D of Azotemia 1. Acute Renal Failure (ARF) 2. Chronic Renal Failure (CRF) 3. Acute worsening of CRF or Acute on Chronic Renal Failure 35
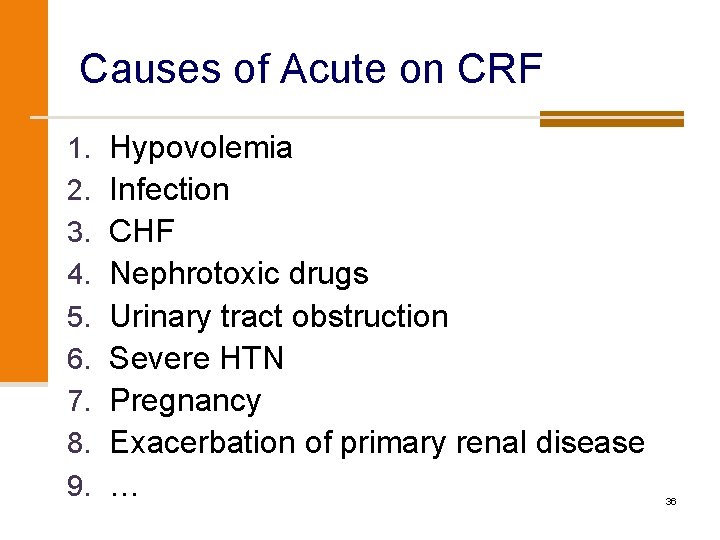
Causes of Acute on CRF 1. 2. 3. 4. 5. 6. 7. 8. 9. Hypovolemia Infection CHF Nephrotoxic drugs Urinary tract obstruction Severe HTN Pregnancy Exacerbation of primary renal disease … 36
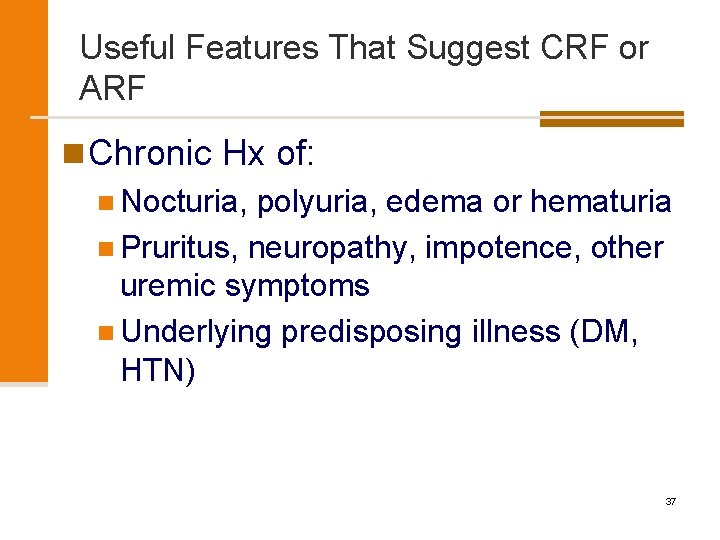
Useful Features That Suggest CRF or ARF n Chronic Hx of: n Nocturia, polyuria, edema or hematuria n Pruritus, neuropathy, impotence, other uremic symptoms n Underlying predisposing illness (DM, HTN) 37
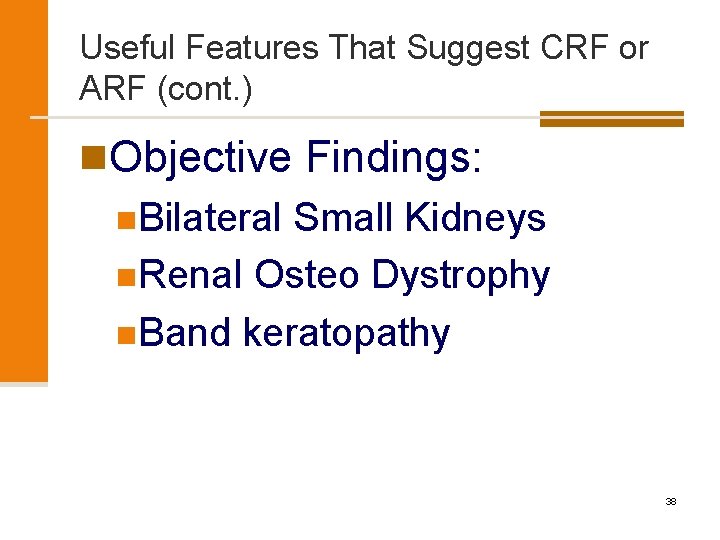
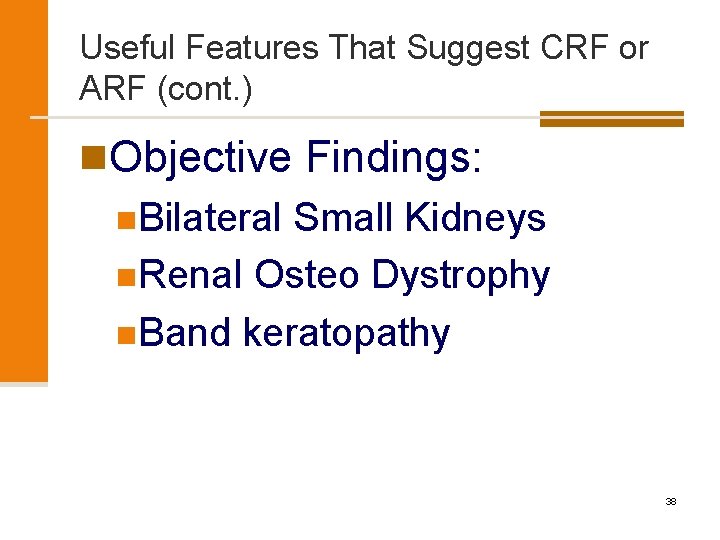
Useful Features That Suggest CRF or ARF (cont. ) n. Objective Findings: n. Bilateral Small Kidneys n. Renal Osteo Dystrophy n. Band keratopathy 38
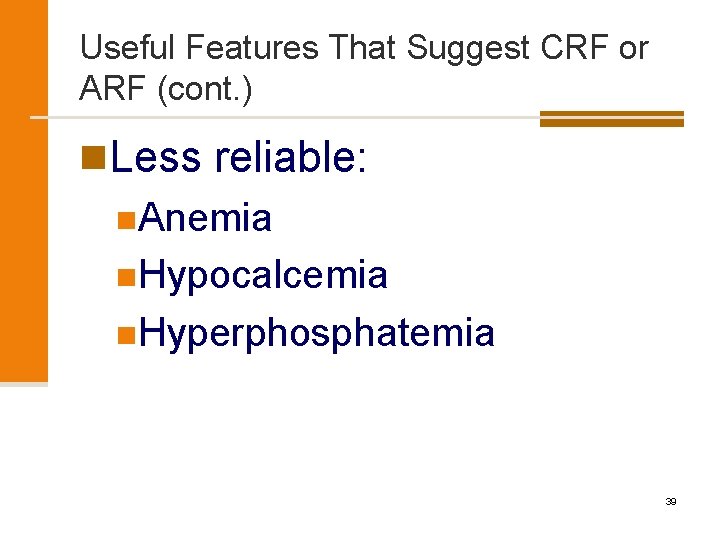
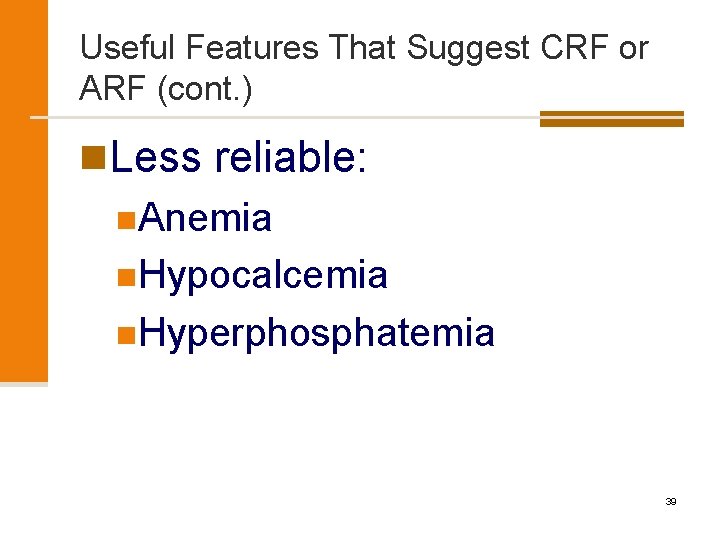
Useful Features That Suggest CRF or ARF (cont. ) n. Less reliable: n. Anemia n. Hypocalcemia n. Hyperphosphatemia 39
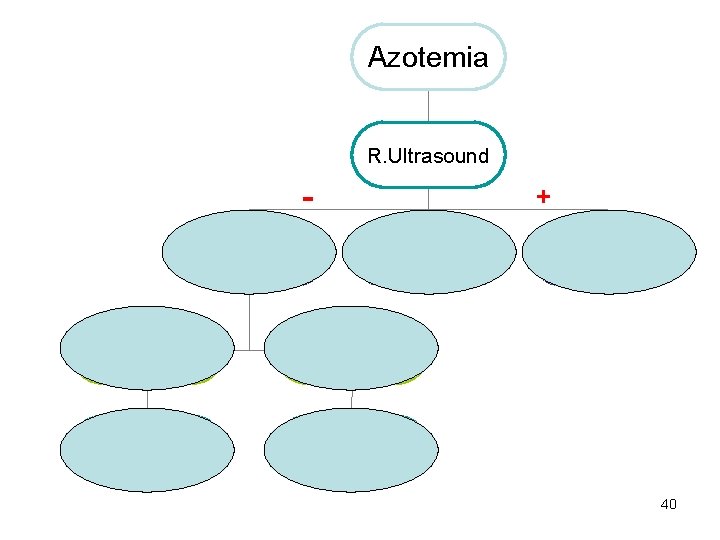
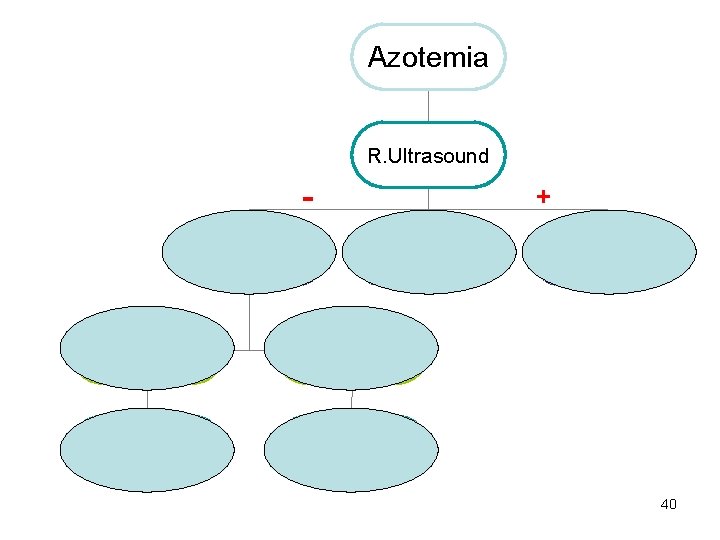
Azotemia R. Ultrasound R. Size & parechyma + Hydronephrosis Small kidneys Thin cortex Nr. size kidneys Intact parechyma CRF Urinalysis Urologic eval. 40
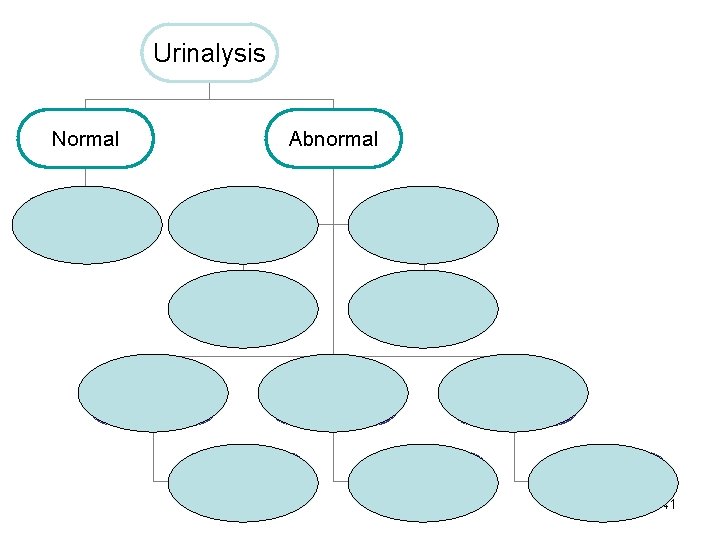
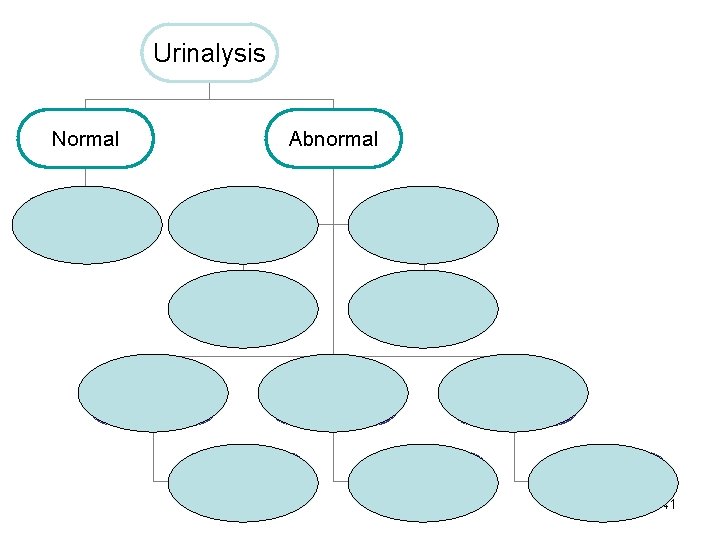
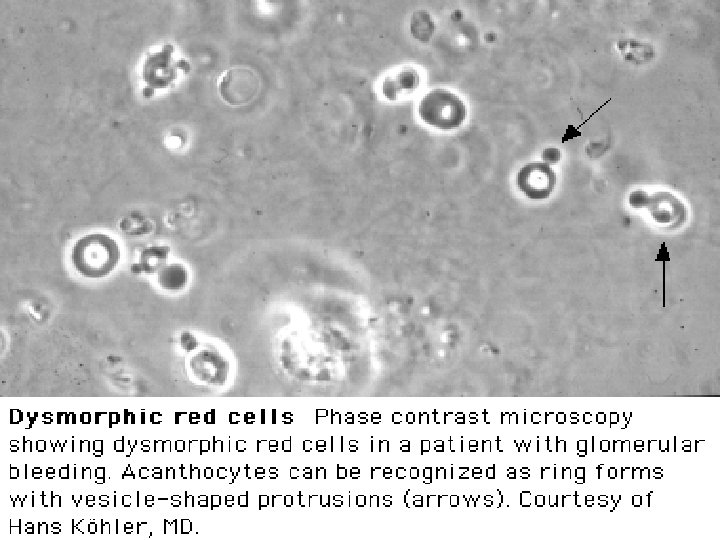
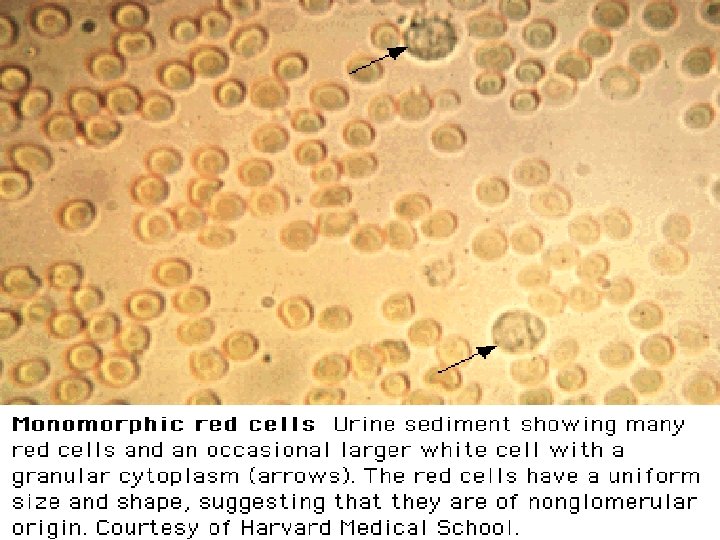
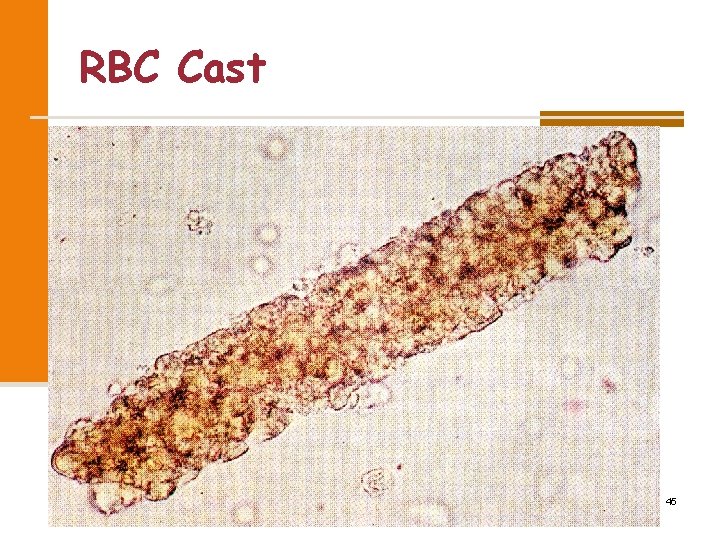
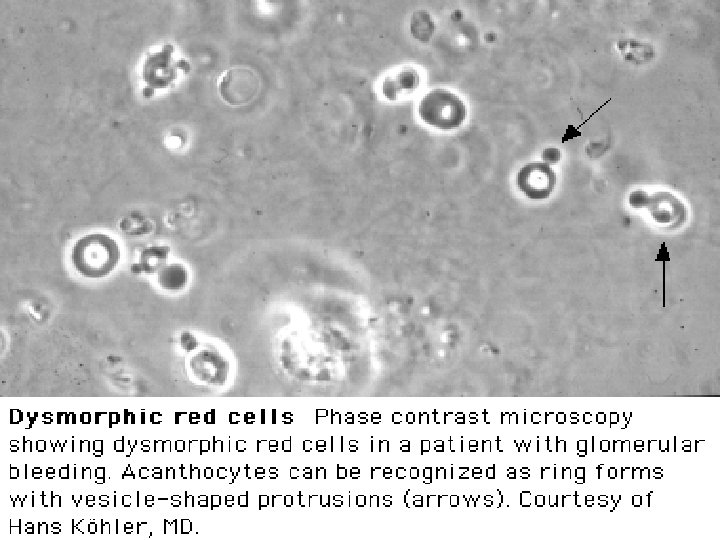
Urinalysis Normal Urine Electrolytes Abnormal WBC, WBC cast, Eosinophils Bacteria AIN Pyelonephritis RBC cast, proteinuria AGN or vasculitis RBC Muddy brown casts Large vessel occlusion ATN 41
42
43
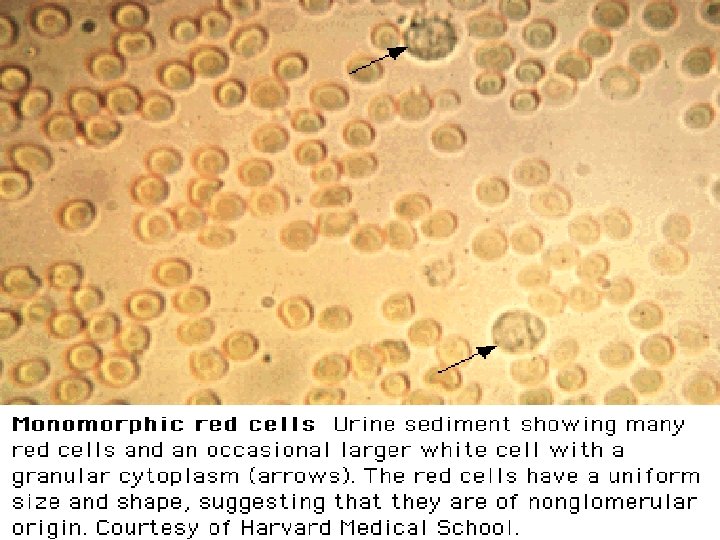
44
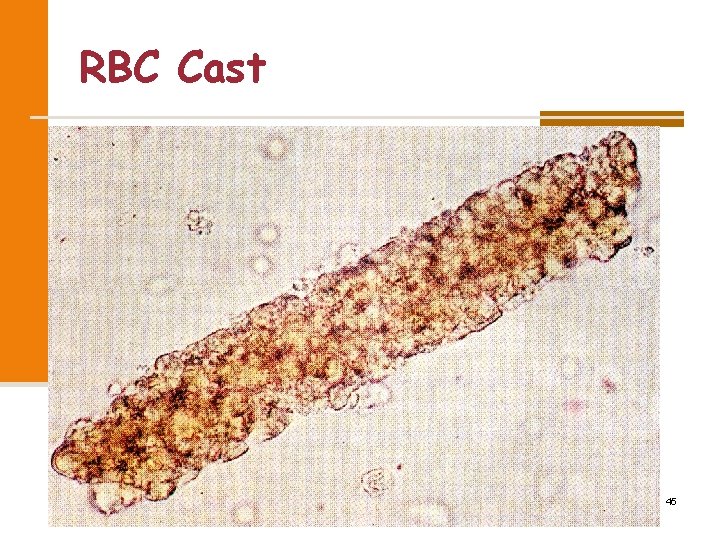
RBC Cast 45
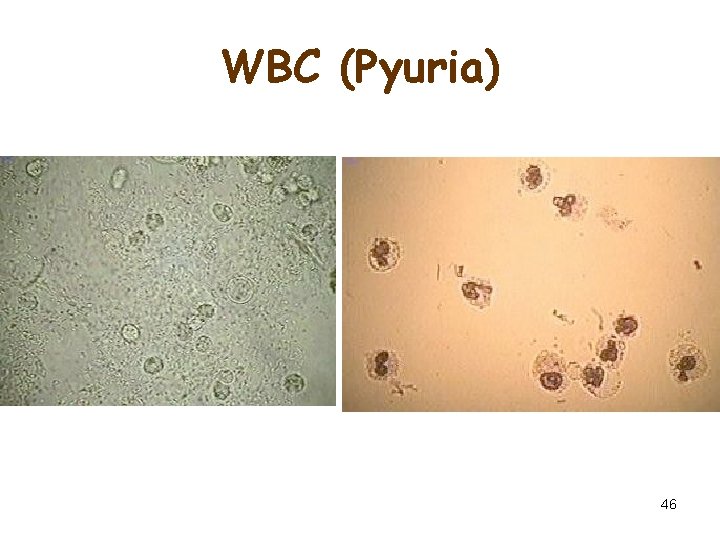
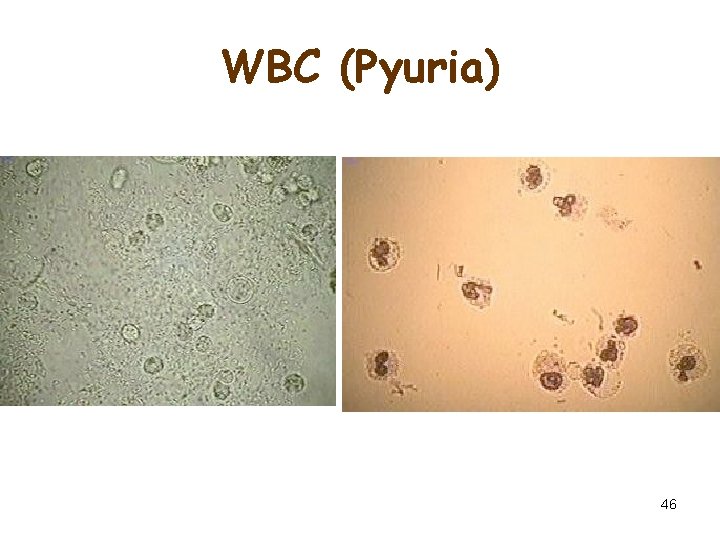
WBC (Pyuria) 46
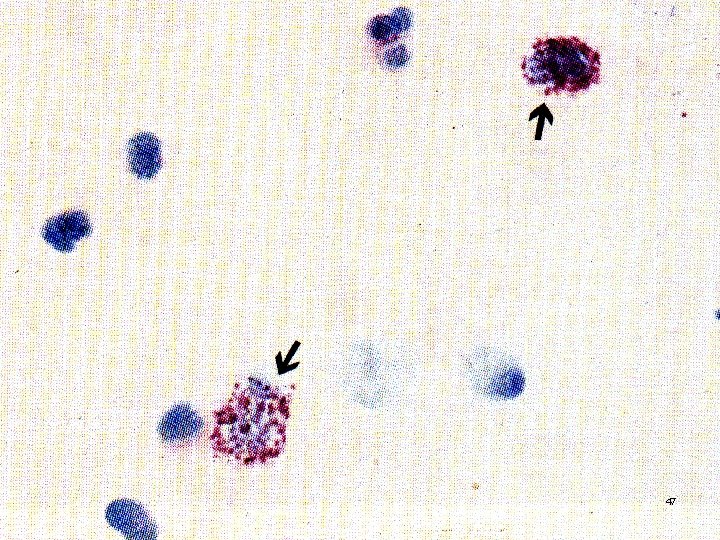
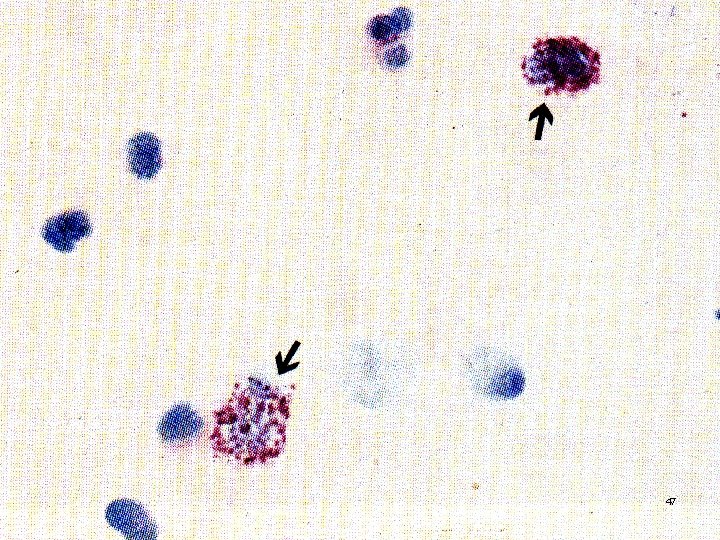
47
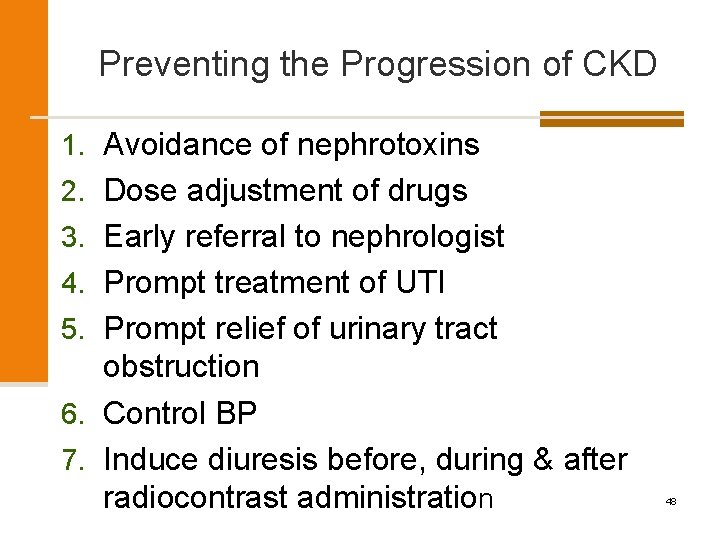
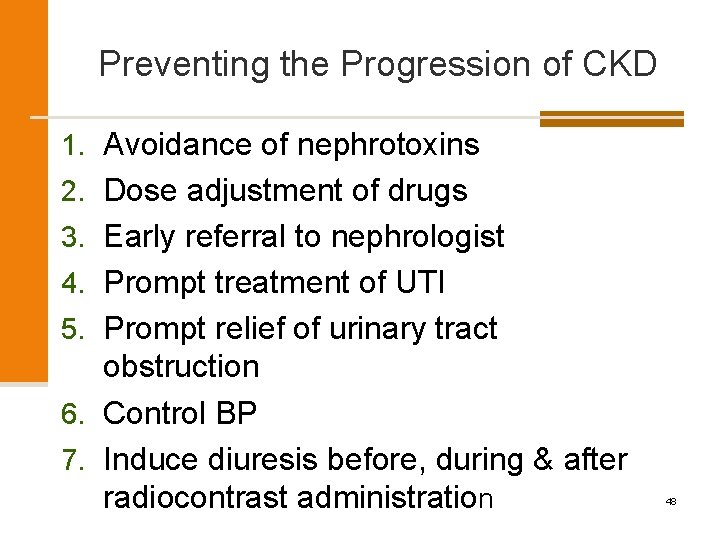
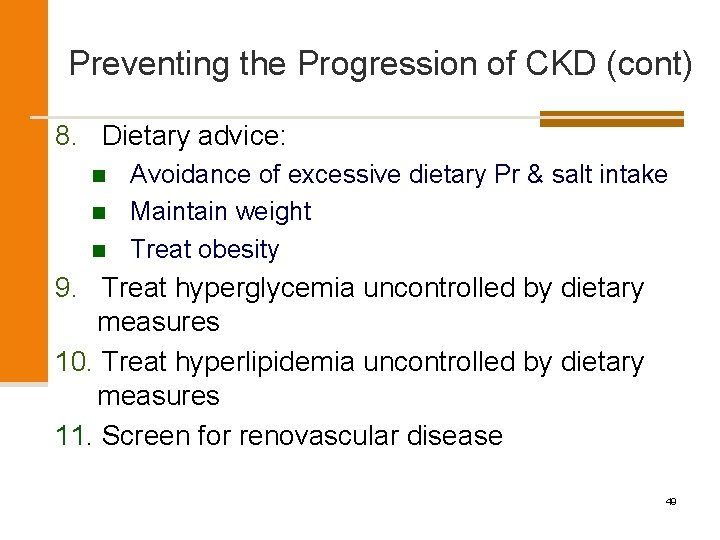
Preventing the Progression of CKD 1. Avoidance of nephrotoxins 2. Dose adjustment of drugs 3. Early referral to nephrologist 4. Prompt treatment of UTI 5. Prompt relief of urinary tract obstruction 6. Control BP 7. Induce diuresis before, during & after radiocontrast administration 48
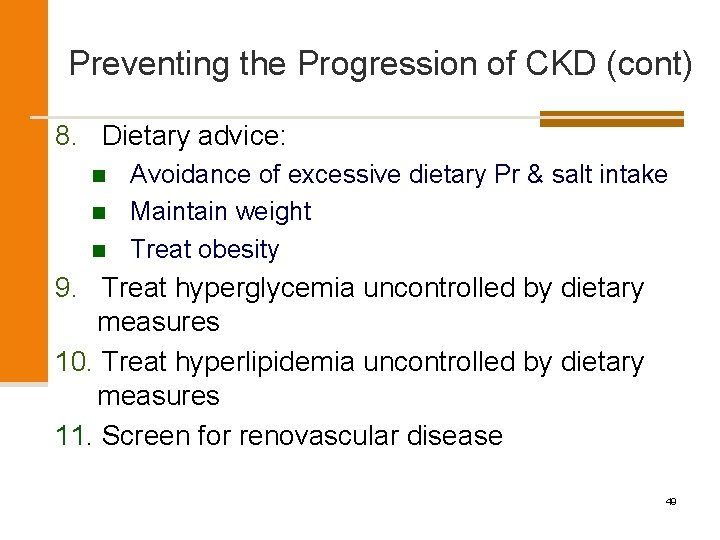
Preventing the Progression of CKD (cont) 8. Dietary advice: n n n Avoidance of excessive dietary Pr & salt intake Maintain weight Treat obesity 9. Treat hyperglycemia uncontrolled by dietary measures 10. Treat hyperlipidemia uncontrolled by dietary measures 11. Screen for renovascular disease 49
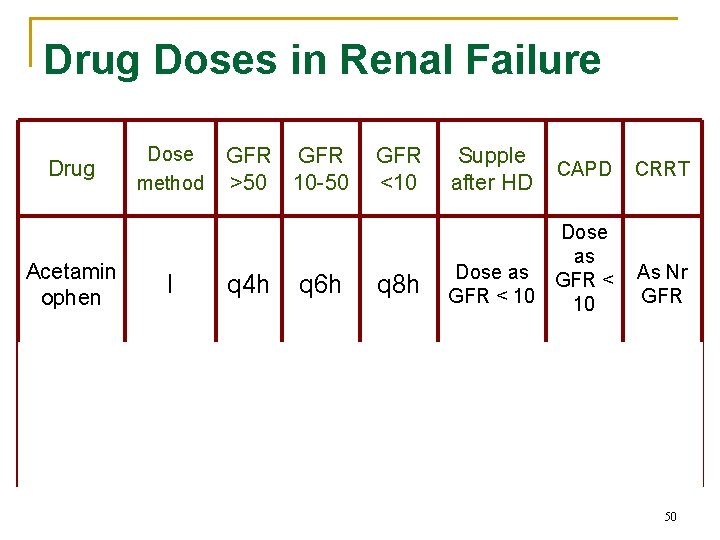
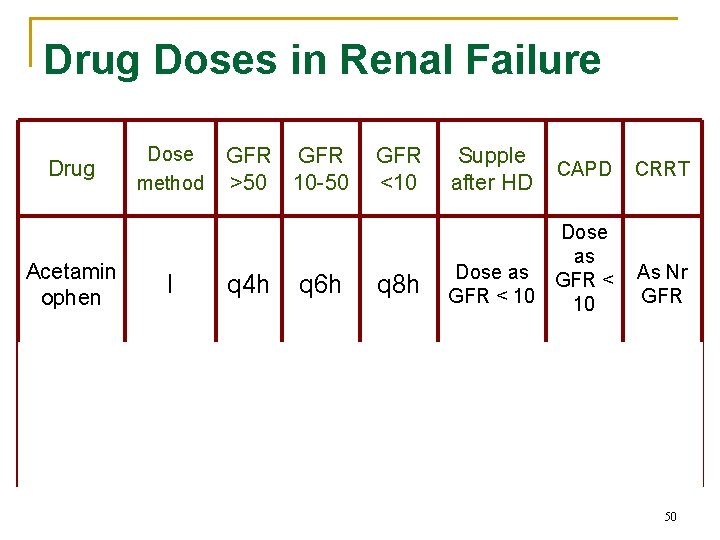
Drug Doses in Renal Failure Drug Acetamin ophen Amikacin Dose method I D, I GFR >50 10 -50 q 4 h 60 90% q 12 h q 6 h 30 70% q 1218 h GFR <10 q 8 h 20 30% q 2448 h Supple after HD CAPD CRRT Dose as GFR < As Nr GFR < 10 GFR 10 normal dose 15 -20 mg/l/d Dose for GFR 10 -50 50
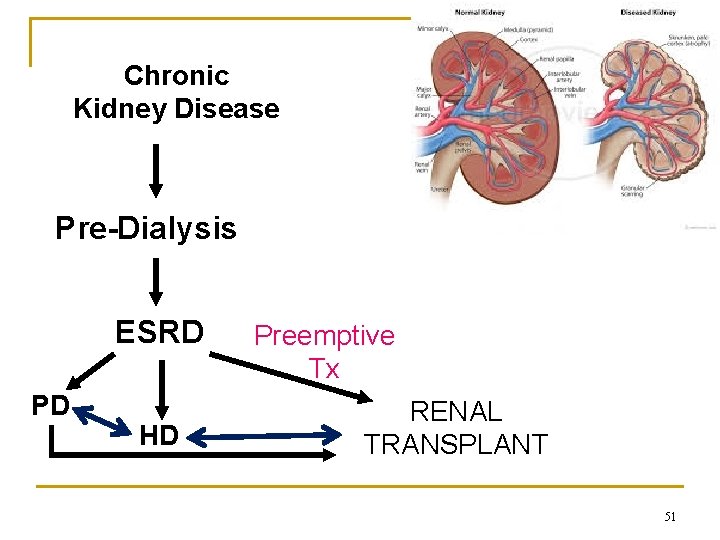
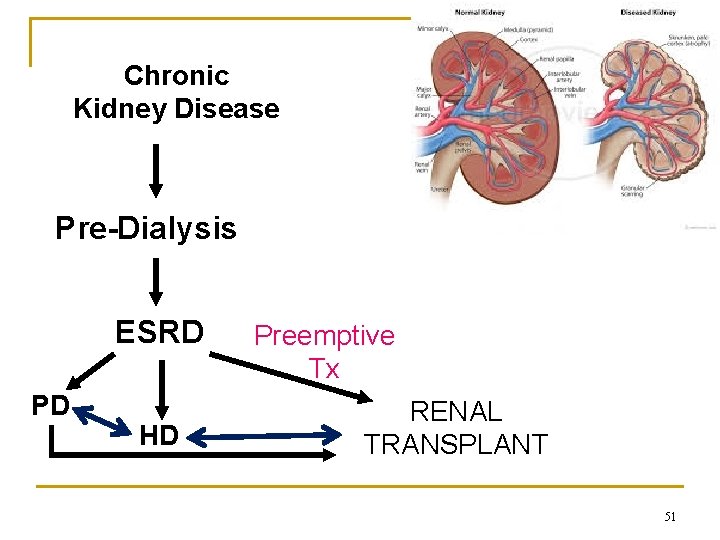
Chronic Kidney Disease Pre-Dialysis ESRD PD HD Preemptive Tx RENAL TRANSPLANT 51
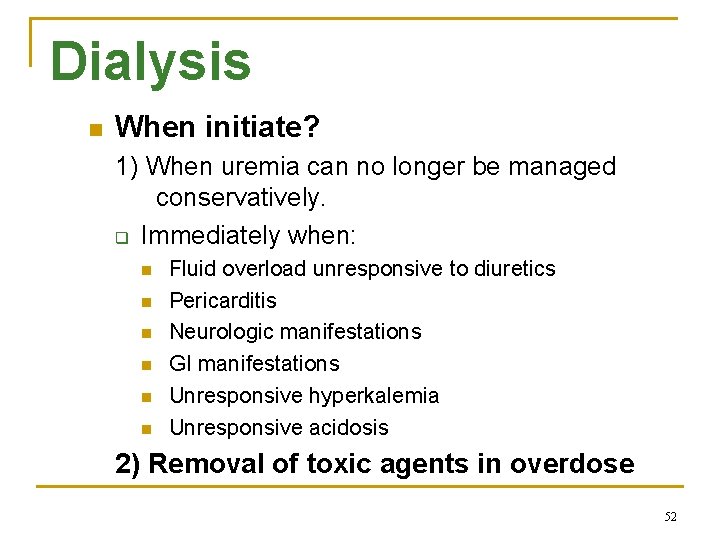
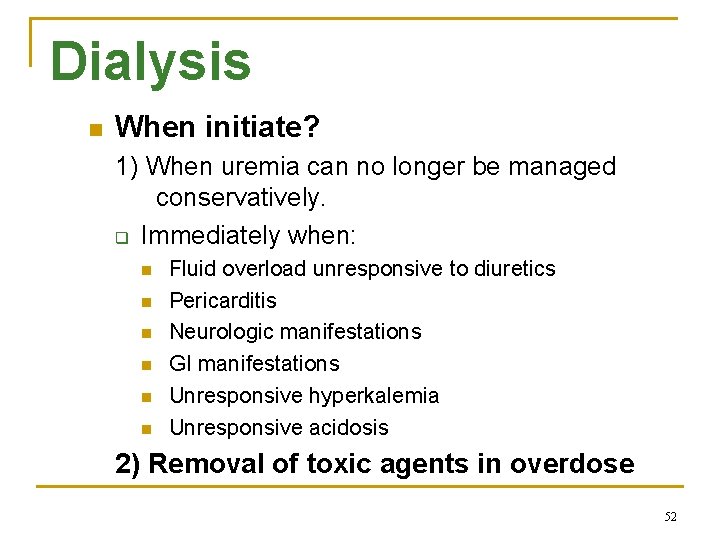
Dialysis n When initiate? 1) When uremia can no longer be managed conservatively. q Immediately when: n n n Fluid overload unresponsive to diuretics Pericarditis Neurologic manifestations GI manifestations Unresponsive hyperkalemia Unresponsive acidosis 2) Removal of toxic agents in overdose 52

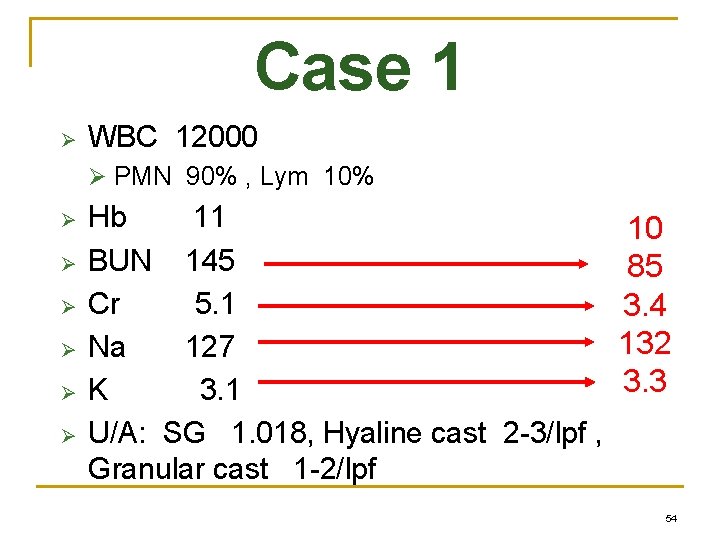
Case 1 Ø WBC 12000 Ø PMN 90% , Lym 10% Ø Ø Ø Hb 11 after 3 days of admission 10 BUN 145 85 Cr 5. 1 3. 4 Na 127 132 K 3. 1 3. 3 U/A: SG 1. 018, Hyaline cast 2 -3/lpf , Granular cast 1 -2/lpf 54

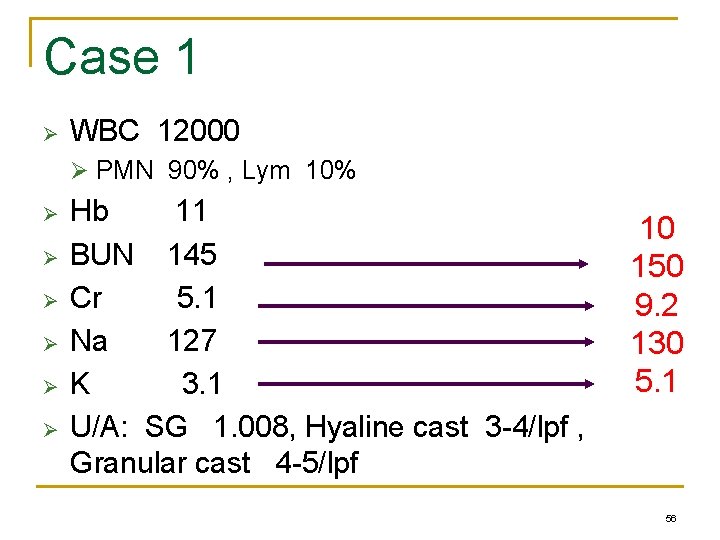
Case 1 Ø WBC 12000 Ø PMN 90% , Lym 10% Ø Ø Ø Hb 11 after 3 days of admission BUN 145 Cr 5. 1 Na 127 K 3. 1 U/A: SG 1. 008, Hyaline cast 3 -4/lpf , Granular cast 4 -5/lpf 10 150 9. 2 130 5. 1 56


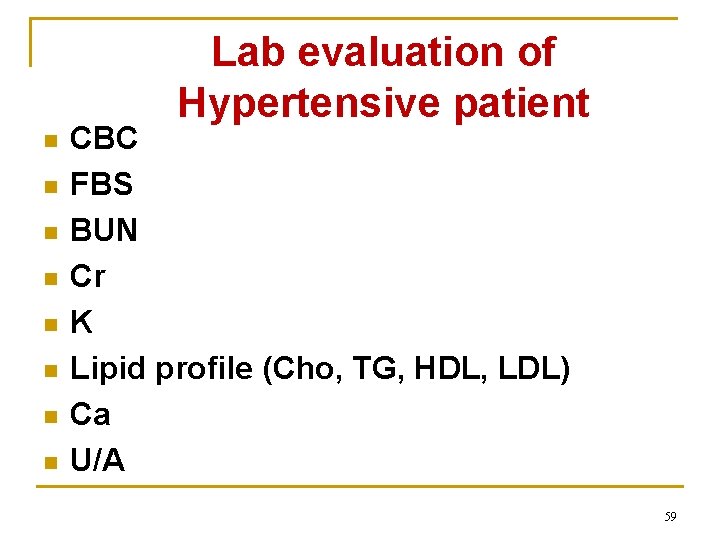
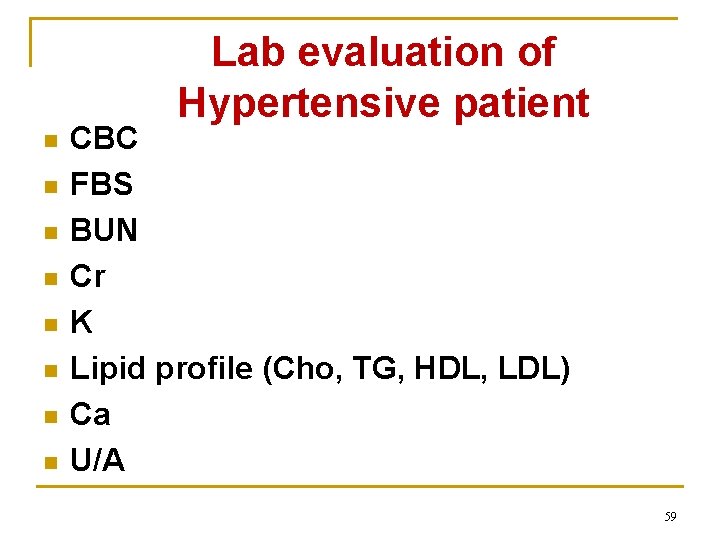
Lab evaluation of Hypertensive patient n n n n CBC FBS BUN Cr K Lipid profile (Cho, TG, HDL, LDL) Ca U/A 59
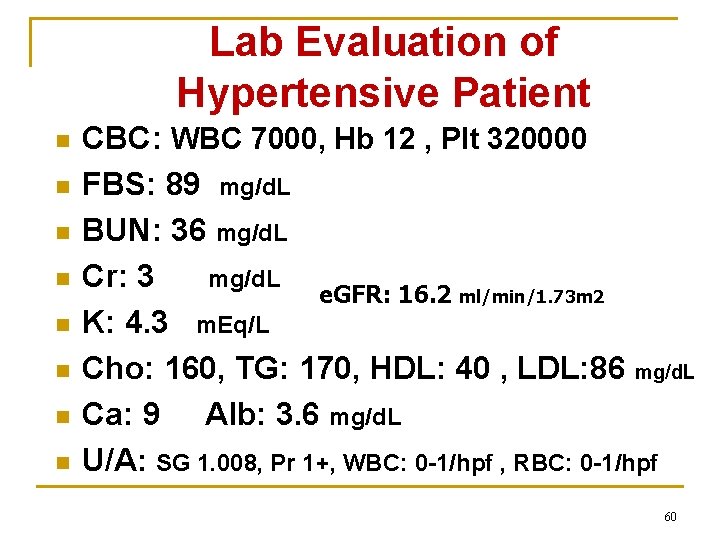
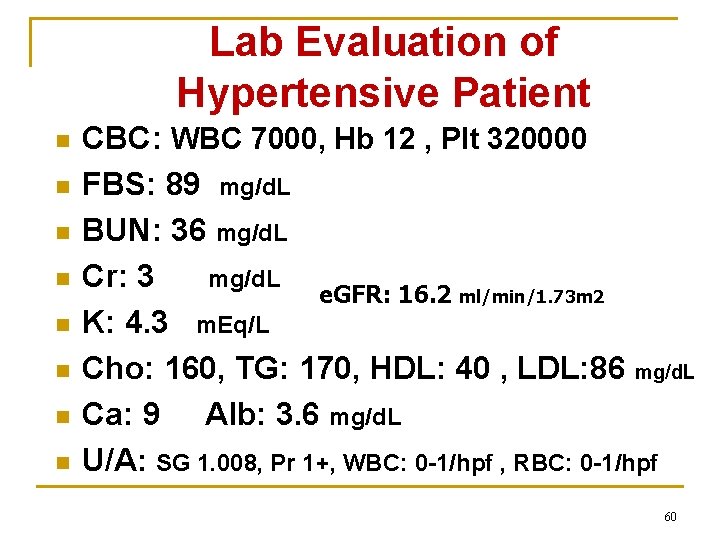
Lab Evaluation of Hypertensive Patient n n n n CBC: WBC 7000, Hb 12 , Plt 320000 FBS: 89 mg/d. L BUN: 36 mg/d. L Cr: 3 mg/d. L e. GFR: 16. 2 ml/min/1. 73 m 2 K: 4. 3 m. Eq/L Cho: 160, TG: 170, HDL: 40 , LDL: 86 mg/d. L Ca: 9 Alb: 3. 6 mg/d. L Corrected Ca: 9. 32 U/A: SG 1. 008, Pr 1+, WBC: 0 -1/hpf , RBC: 0 -1/hpf 60


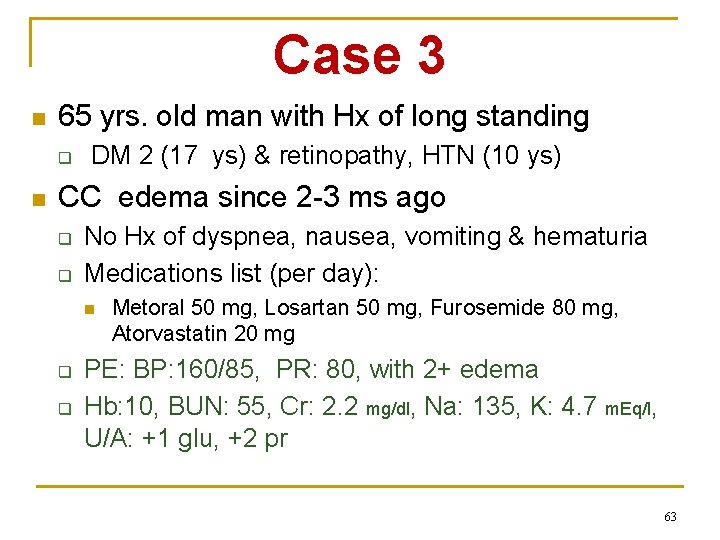
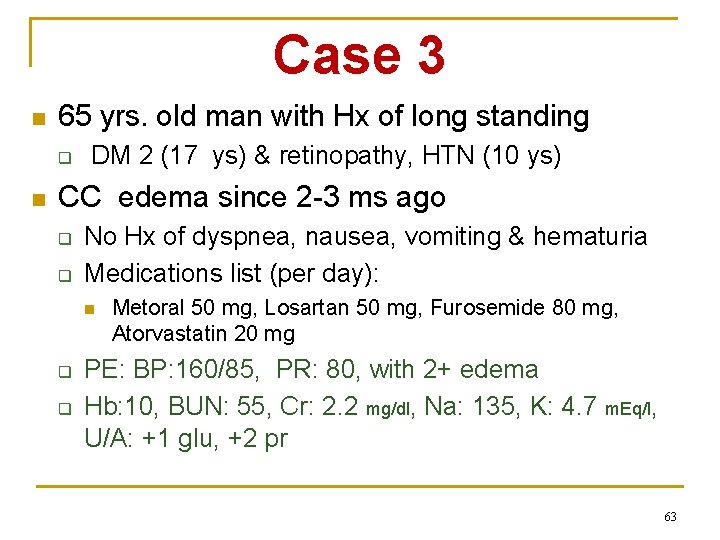
Case 3 n 65 yrs. old man with Hx of long standing q n DM 2 (17 ys) & retinopathy, HTN (10 ys) CC edema since 2 -3 ms ago q q No Hx of dyspnea, nausea, vomiting & hematuria Medications list (per day): n q q Metoral 50 mg, Losartan 50 mg, Furosemide 80 mg, Atorvastatin 20 mg PE: BP: 160/85, PR: 80, with 2+ edema Hb: 10, BUN: 55, Cr: 2. 2 mg/dl, Na: 135, K: 4. 7 m. Eq/l, U/A: +1 glu, +2 pr 63
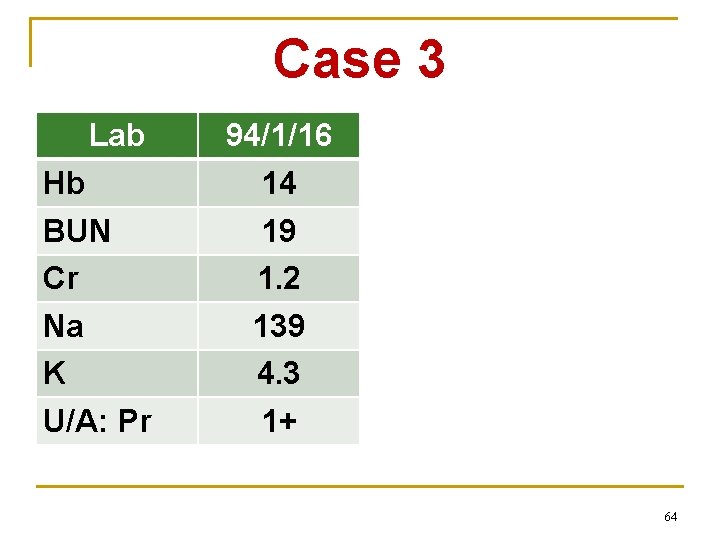
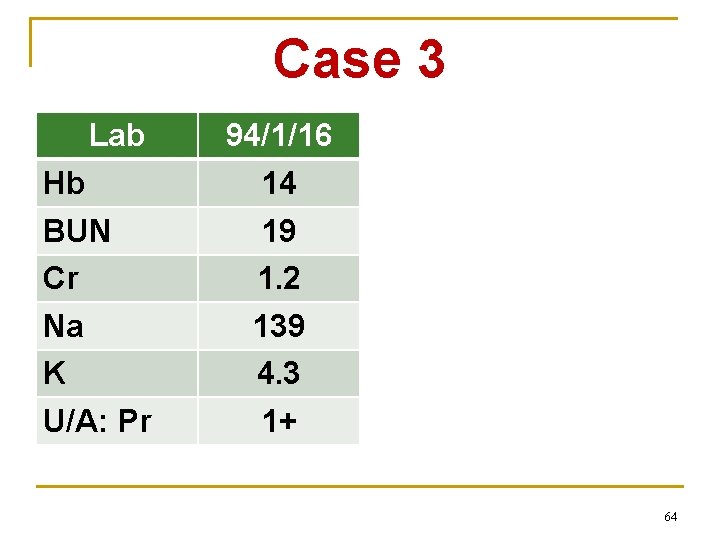
Case 3 Lab Hb BUN Cr Na K U/A: Pr 94/1/16 14 19 1. 2 139 4. 3 1+ 94/4/29 12 30 1. 7 135 4. 9 1+ 94/12/8 10 55 2. 2 135 4. 7 2+ 64
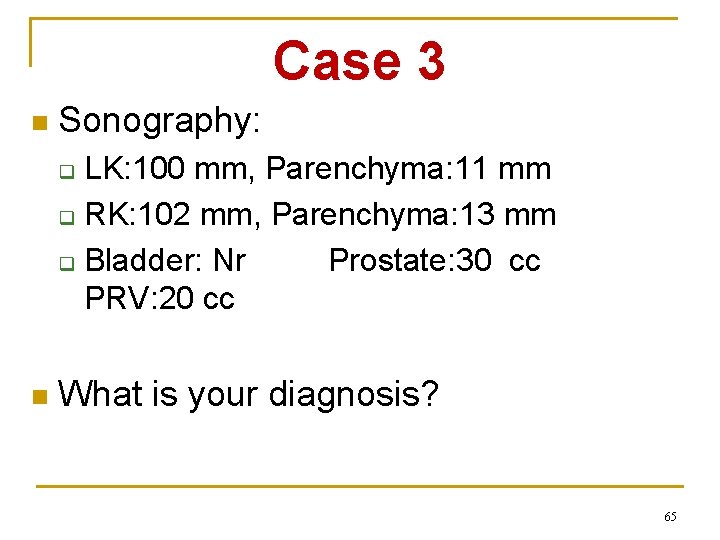
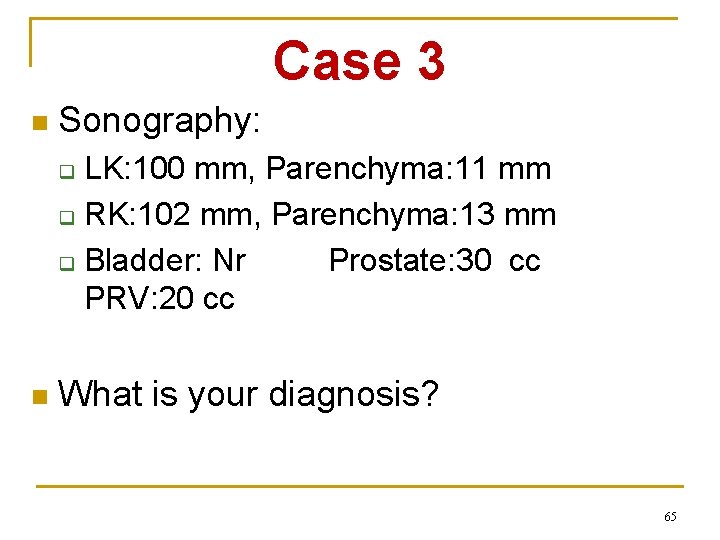
Case 3 n Sonography: LK: 100 mm, Parenchyma: 11 mm q RK: 102 mm, Parenchyma: 13 mm q Bladder: Nr Prostate: 30 cc PRV: 20 cc q n What is your diagnosis? 65
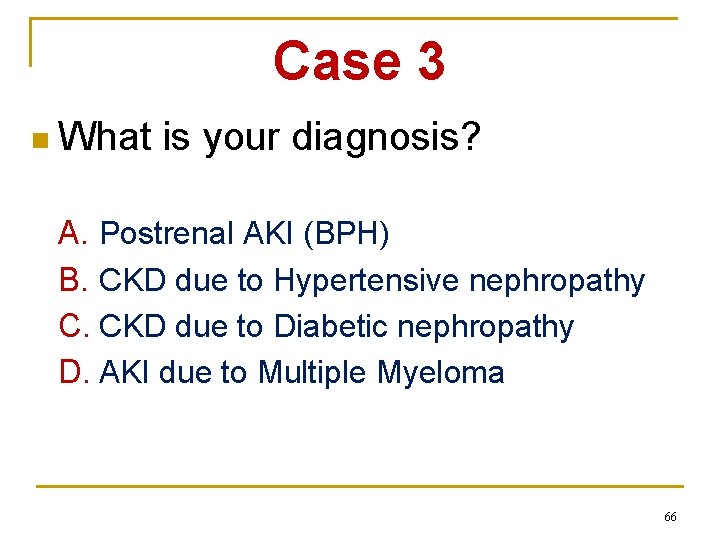
Case 3 n What is your diagnosis? A. Postrenal AKI (BPH) B. CKD due to Hypertensive nephropathy C. CKD due to Diabetic nephropathy D. AKI due to Multiple Myeloma 66
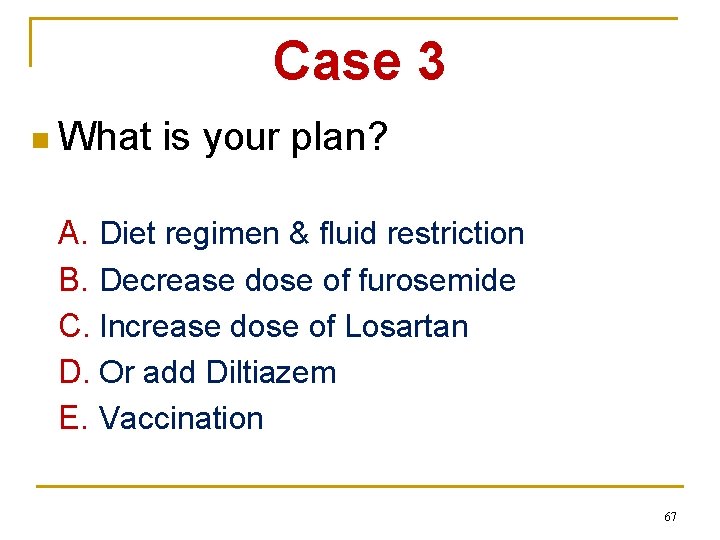
Case 3 n What is your plan? A. Diet regimen & fluid restriction B. Decrease dose of furosemide C. Increase dose of Losartan D. Or add Diltiazem E. Vaccination 67
68
 Ali shahidi
Ali shahidi Azotemia
Azotemia Uremia
Uremia Azotemia
Azotemia Pckd icd 10
Pckd icd 10 Myoglobinuria
Myoglobinuria Promotion from assistant to associate professor
Promotion from assistant to associate professor Bandura's reciprocal determinism
Bandura's reciprocal determinism Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Definition of research approach
Definition of research approach Shower approach in international marketing
Shower approach in international marketing Traditional approach of development
Traditional approach of development Avoidance
Avoidance Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Datagram switching
Datagram switching Professor miller meme
Professor miller meme Evan korth rate my professor
Evan korth rate my professor Professor david best
Professor david best Professor angela wallace
Professor angela wallace Certo dia os professores
Certo dia os professores Ochsner’s clasping test
Ochsner’s clasping test Mattie is a new sociology professor
Mattie is a new sociology professor Professor emeritus keith l. moore
Professor emeritus keith l. moore Dr syed hasan
Dr syed hasan Hill’s strategy development framework
Hill’s strategy development framework Professor john wood
Professor john wood Professor edley
Professor edley Dr atinga
Dr atinga How to write a formal email to teacher
How to write a formal email to teacher Dioptro plano
Dioptro plano Professor pete's classroom
Professor pete's classroom Professor john forsythe
Professor john forsythe Sige palmas professor
Sige palmas professor Raymond flood
Raymond flood Feedback hattie effect size
Feedback hattie effect size Dear mr professor
Dear mr professor Lora koretz rate my professor
Lora koretz rate my professor Titular professor
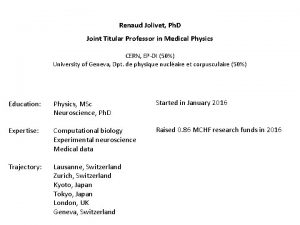
Titular professor Professor thurstan shaw
Professor thurstan shaw Rapd relative afferent pupillary defect
Rapd relative afferent pupillary defect Fcps uk
Fcps uk Professor maro
Professor maro Professor bill lucas
Professor bill lucas Good morning everyone vs everybody
Good morning everyone vs everybody Professor belinda tynan
Professor belinda tynan Jonathan benger
Jonathan benger Professor joelson lima
Professor joelson lima Professor brian peskin
Professor brian peskin Professor john hughes
Professor john hughes Baudelaire heautontimorumenos
Baudelaire heautontimorumenos Daniel currie rate my professor
Daniel currie rate my professor Deutropia
Deutropia How to read literature like a professor violence
How to read literature like a professor violence Professor helen sullivan
Professor helen sullivan Captain beatty character traits
Captain beatty character traits Anuj chopra rate my professor
Anuj chopra rate my professor Ruth guthrie rate my professor
Ruth guthrie rate my professor Professor david denning
Professor david denning Tspci
Tspci Rose gordon flowers for algernon
Rose gordon flowers for algernon Edmund crampin
Edmund crampin Lindab professor
Lindab professor Back formation
Back formation Research problem formulation
Research problem formulation Professor grant schofield
Professor grant schofield Professor frank kee
Professor frank kee Sia professor
Sia professor Professor michael bagshaw
Professor michael bagshaw Professor raymond flood
Professor raymond flood