Workplace violence do nurses have a recourse for
- Slides: 28
Workplace violence: do nurses have a recourse for redress? Peter Kipkorir Ngeny BSc. N/PCCN
OUTLINE 1. Define term work place violence in the context of healthcare service. 2. Understand the gravity of WPV meted on nurses in various set ups. 3. Identify factors or circumstances predisposing health professionals to WPV 4. Discuss the options that an individual nurse has in the event of being assaulted in workplace.
Introduction • Nurses are increasingly facing verbal abuse, physical assault and injuries often from the patients they are trying to help. • Nurses are the first to come in direct contact with sick individuals in any health facility. • They also stay with the patients for a longer period of time compared with other health cadres. • This may justify why nurses are at greater risk of either physical or psychological/emotional violence in their line of duty.
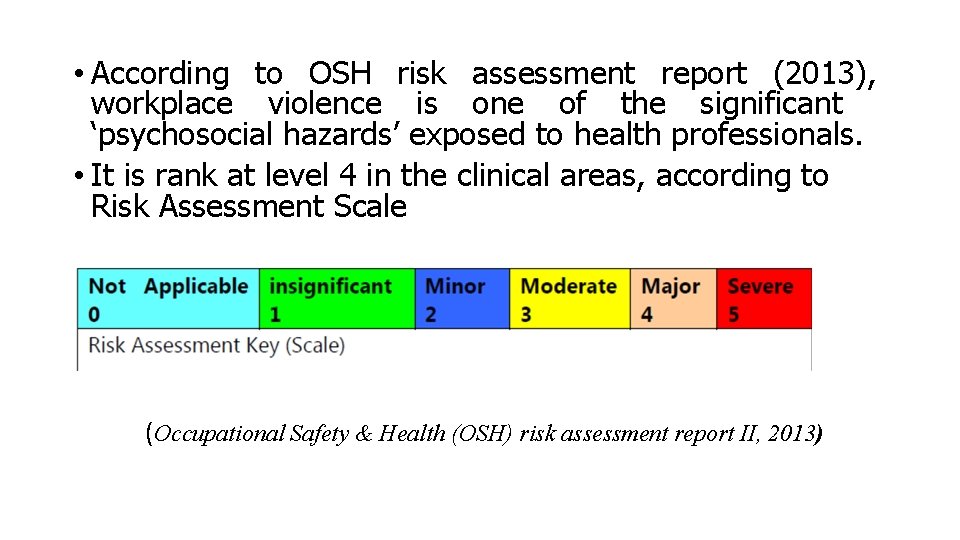
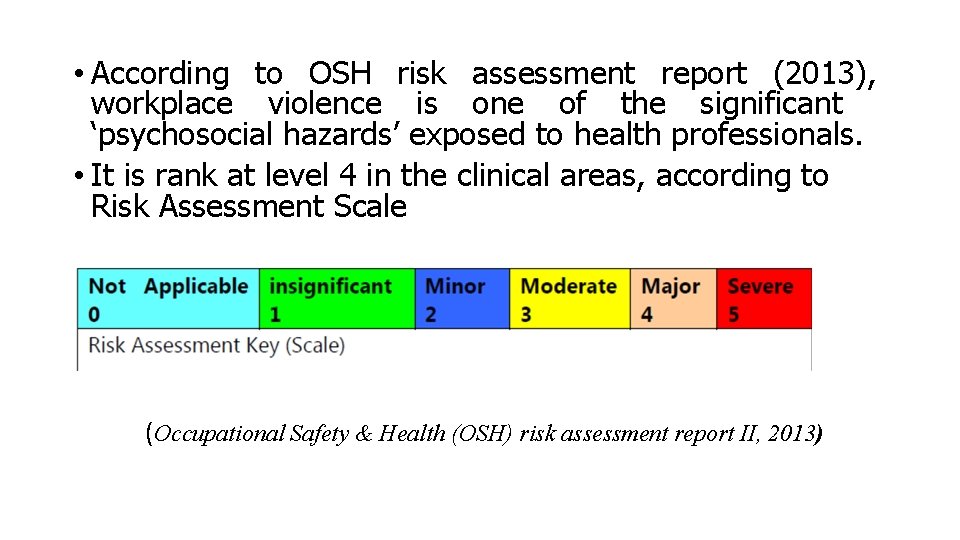
• According to OSH risk assessment report (2013), workplace violence is one of the significant ‘psychosocial hazards’ exposed to health professionals. • It is rank at level 4 in the clinical areas, according to Risk Assessment Scale (Occupational Safety & Health (OSH) risk assessment report II, 2013)
• It is a silent epidemic and is underreported. • There is no database in kenya that can be accessed to determine the gravity of cases of workplace violence in health sector. • The occurrences are underreported because nurses “fear that employers may deem assaults as the result of their negligence or poor job performance…. some nurses consider violence as part of their job” (Mohamed, 2002). • In some major healthcare agencies, underreporting of workplace violence is due to organization's intense focus on customer service which results in the mentality that “the customer is always right”.
Definition • Incidents where staff are abused, threatened or assaulted in circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being or health (WHO, 2002). • ‘‘violent acts (including physical assaults and threats of assaults) directed toward persons at work or on duty’’ (US OSHA & NIOSH) • It includes aggression, horizontal violence, bullying, intimidation, harassment, and workplace incivility
Cases in workplace • A nurse working in an intensive Care Unit is caring for a patient with a traumatic brain injury. During assisted bath, the patient suddenly punches the nurse in the face. The nurse sustains a fractured jaw. • A family member in the PICU shouts loudly at the nurse ‘‘I don’t want to hear your excuses! Can’t you see she’s in pain? Give my daughter more medication immediately or I’ll make you feel the way she does!’’
• For workplace violence to occur, a person must apply, attempt to apply, or threaten to apply physical force against a worker. However, he or she does not need to have the capacity to appreciate that these actions could cause physical harm.
Forms of workplace violence 1. Physical violence: beating, kicking, slapping, stabbing, shooting, pushing, biting, pinching, etc. 2. Psychological violence: threat of physical force against another person or group that can result in harm to physical, mental, spiritual, moral, or social development. • These forms are perpetrated by patients and visitors against the health providers
What could be the cause? • According to Kim & Motsei (2002), causes of WPV against nurses include: 1. Low professional status 2. Frontline exposure with patients and family attendants 3. Long hours spent in the hospital setting 4. Feminization of the nursing profession.
Incidence and prevalence • In kenya, there is no concrete statistics documented on cases of violence meted on nurses in line of duty. • According to the study done by Mohammad, Noghan, Moghimbeygi & Bikmoradi (2012), most committers of verbal misbehavior to ICU nurses were patients (31. 8%) and their companions (31. 8%). Patients' companions (44. 4%) and patients (34. 3%) threatened ICU nurses. It also revealed that the ICU nurses were beaten by companions (60%) and patients (40%).
• In a survey in US, type II workplace violence accounted for 75% of aggravated assaults and 93% of all assaults against employees (Philips, 2016). • Type II WPV occurs when the perpetrator (patient or relative) has a legitimate relationship with the business (health institution) and becomes violent while being served by the business (nurse). • Emergency department (A/E) and psychiatric wards are rated as the most violent hospital environment. Nurses are physicians are the main victims.
• A recent survey done in on one of the US facility indicated that 100% of nurses in A/E reported verbal abuse and 82. 1% reporting physical assault. • Rate of violence correlates with patient contact time, therefore, nurses are victimized at the highest rates. • In a cross-sectional study of 850 nurses in 2013 in Hong Kong revealed an overall prevalence rate of WPV at 44. 6% ( Cheung, Lee, & Yip, 2017).
• A study to determine prevalence rate among physicians and nurses in Macau, China revealed an overall prevalence estimates for workplace violence and harassment at 57. 2% ( Cheung, Lee, & Yip, 2017). • According to Du. Hart (2001), the rate committed against physicians was 16. 2 per 1, 000 workers and against nurses it was 21. 9 per 1, 000 workers.
Risk factors Worker Risk Factors: Characteristics of a health worker that increases the risk 1. Gender: women experienced a higher percentage of verbal and physical violence. However, a cross-sectional study in Palestinian hospitals (Kitaneh &Hamdan, 2012) revealed that male health workers experience more violence. 2. Age: <40 years old are most frequently the victims. According to Gillespie, Gates, Miller & Howard (2010), older nursing staff are ‘more adaptable, patient, and empathetic’ and nonconfrontational. 3. Hours worked: Part-time employees experienced reduced risk compared with full-time employees
Setting and Environmental Risk Factors 1. Inadequate security presence (guard, CCTV) 2. Lack of policies to address assault prevention 3. Certain times of the day. According to Ergun & Karadakovan (2005), 70% of violent events occur between 4 pm and 8 am. Mc. Aneney and Shaw (1994) attributed the incidences during this hours to patients or visitors who are intoxicated.
Other Risk factors 1. Prevalence of guns and other weapons among patients, their families, or friends. 2. The availability of drugs or money at hospitals, clinics, and pharmacies, making them likely robbery targets. 3. The increasing use of hospitals by police and the criminal justice system for criminal holds and the care of acutely disturbed, violent individuals.
5. Working directly with volatile people, especially if they are under the influence of drugs or alcohol or have a history of violence or certain psychotic diagnoses. 6. Long waits for service. 7. Working alone.
Professionals at risk • According to WHO (2002), exposure to WPV was classified at different levels of risks as 1. at extremely high risk: nursing and ambulance staff 2. at high risk: doctors, support and technical staff 3. at risk: all other allied professionals:
Aftermath of the violence • Some nurses will internalize (depression, avoidance, withdrawal) while others externalize (anger, outbursts, fluctuating mood) emotional and behavioral responses. • Can have repercussions on the physical and/or emotional health of the victims, and thus on their wellbeing and the quality of their work. • Nurses’ reduction in efficiency, displacement and change in working position, absence, low morale and reduction in quality of life.
• Emotional symptoms similar to post-traumatic stress disorder. • Early feelings of burnout. • Hospitals suffer the financial burden of decreased productivity and excessive lawsuits.
What are the options of the nurse who survives WPV? • Do something or do nothing? 1. Sue the perpetrator (patient or relative) : is it possible in our context? • Determining factors include patient’s medical condition and the health organization’s support. • It is universal that a professional caregiver cannot file a lawsuit over the conduct of a patient when the conduct is, in whole or in part, the very reason for the caregiver’s role with the patient.
• But what does the Constitution of kenya 2010 entails on the bill of rights? Constitution of Kenya 2010 • Chapter 4 on Bill of rights article • Article 22. (1) Every person has the right to institute court proceedings claiming that a right or fundamental freedom in the Bill of Rights has been denied, violated or infringed, or is threatened
• Can the health organization take action on behalf of the nurse? • According to Mc. Neil (2007), hospitals are reluctant to file a complaint and in particularly the private hospitals may be unwilling to launch a legal complaint feeling that their reputation will be besmirched. 2. The only viable option is the worker’s compensation claim. • Contained in The Work Injury Benefit’s Act, 2007. • An ACT of Parliament to provide for compensation to employees for work related injuries and diseases contracted in the course of their employment and for connected purposes.
• Nurses posses referent power because of trust the public has in us. • We have ability to wedge political power because of our numbers. However, we have allowed ourselves to be divided and thus weakened hence have been losing our share of power. • Let us empower ourselves by sharing knowledge, maintaining cohesiveness, valuing our profession and supporting each other. • STOP ACTING LIKE A VICTIM.
Thank you
• Ergün, F. S. , & Karadakovan, A. (2005). Violence towards nursing staff in emergency departments in one Turkish city. International Nursing Review, 52, 154– 160. ) • Mc. Aneney, C. M. , & Shaw, K. N. (1994). Violence in the pediatric emergency department. Annals of Emergency Medicine, 23(6), 1248– 1251. ) • Du. Hart, D. T. (2001). Violence in the workplace, 1993– 99 (NCJ Publication No. 190076). Washington, DC: Bureau of Justice Statistics • Kim, J. , & Motsei, M. (2002). “Women enjoy punishment”: Attitudes and experiences of gender-based violence among PHC nurses in rural South Africa. Social Science & Medicine, 54(8), 1243 e 1254.
• Salimi J, Ezazi Ardi L, Karbakhsh Davari M. Workplace violence against nursing personnel of nonpsychiatric emergency wards. Sci Journal of forensic medicine. 2006; 12(4): 202 -9. • Gillespie GL, Gates DM, Miller M, Howard PK. Workplace violence in healthcare settings: risk factors and protective strategies. Rehabilitation Nursing. 2010; 35(5): 177– 184. [Pub. Med: 20836482]