Using Implementation Science to Address Adolescent HIV Geri






![Preliminary Findings § AGYW’s prefer home-based recruitment [84%] strategy and staff-aided HIV testing Preliminary Findings § AGYW’s prefer home-based recruitment [84%] strategy and staff-aided HIV testing](https://slidetodoc.com/presentation_image_h/d64044f3d0ade94d3bfac0ed2a9637eb/image-31.jpg)





- Slides: 62
Using Implementation Science to Address Adolescent HIV? Geri R. Donenberg, Ph. D Professor of Medicine, Psychology, and Epidemiology and Biostatistics Director, Center for Dissemination and Implementation Science & Healthy Youths Program

In 2016, the US spent nearly $32. 3 billion on medical research https: //www. nih. gov/about-nih/what-we-do/budget
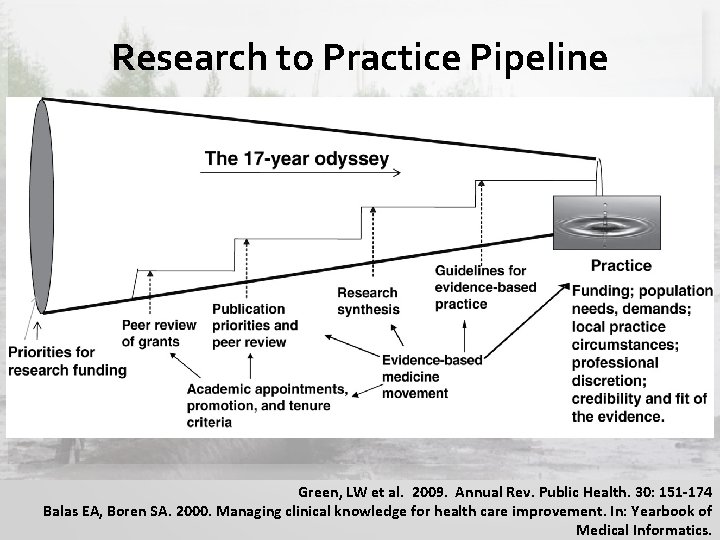
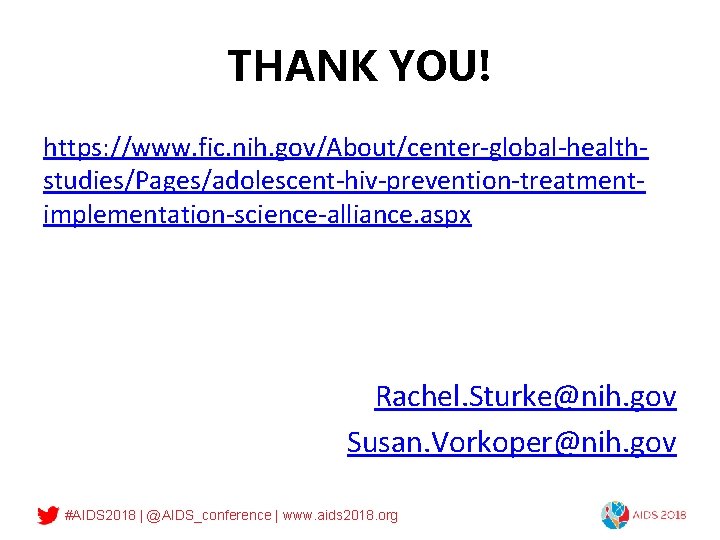
Research to Practice Pipeline Green, LW et al. 2009. Annual Rev. Public Health. 30: 151 -174 Balas EA, Boren SA. 2000. Managing clinical knowledge for health care improvement. In: Yearbook of Medical Informatics.

• Evidence-based interventions exist • Close the 17 year gap between research discovery and practice (Balas, 1998) • Achieve the full public health benefit of the research Ensure research findings are relevant to, inform, and improve health, service delivery, utilization and sustainability.
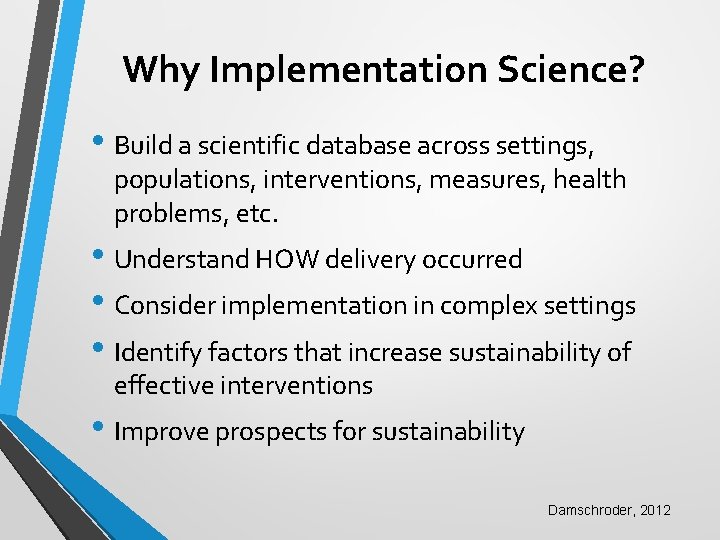
Why Implementation Science? • Build a scientific database across settings, populations, interventions, measures, health problems, etc. • Understand HOW delivery occurred • Consider implementation in complex settings • Identify factors that increase sustainability of effective interventions • Improve prospects for sustainability Damschroder, 2012
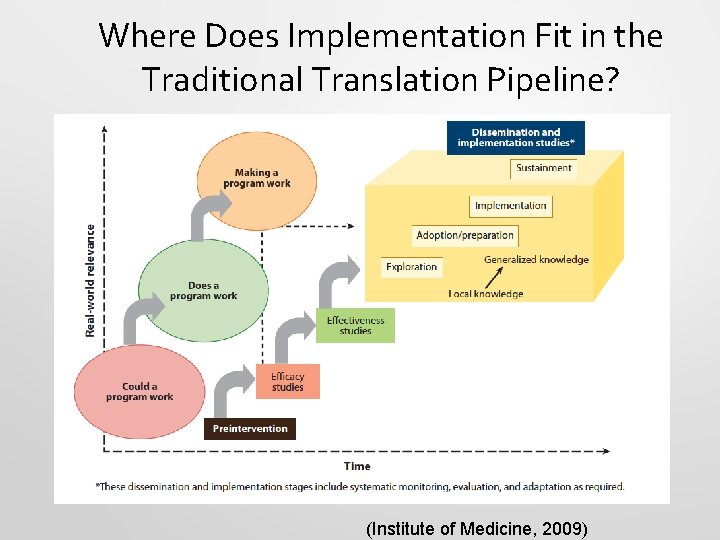
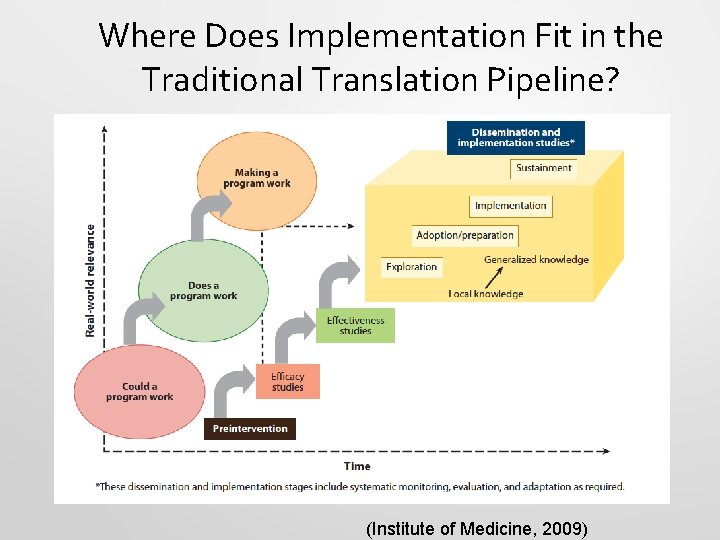
Where Does Implementation Fit in the Traditional Translation Pipeline? (Institute of Medicine, 2009)

IS and Adolescent HIV?
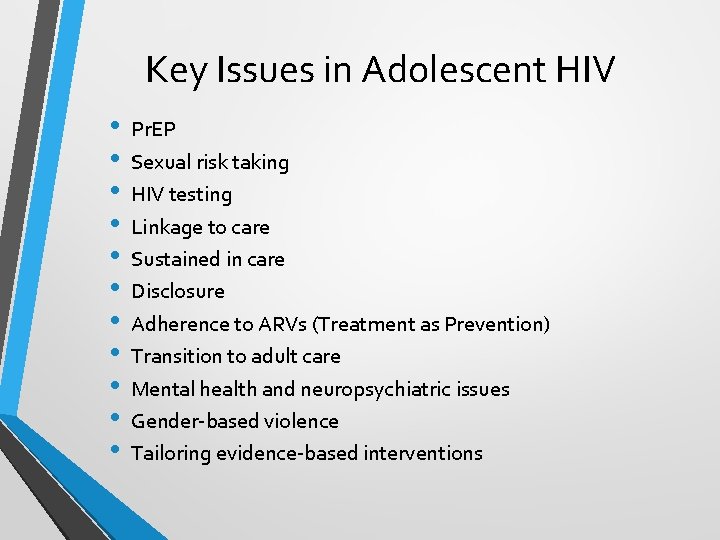
Key Issues in Adolescent HIV • • • Pr. EP Sexual risk taking HIV testing Linkage to care Sustained in care Disclosure Adherence to ARVs (Treatment as Prevention) Transition to adult care Mental health and neuropsychiatric issues Gender-based violence Tailoring evidence-based interventions
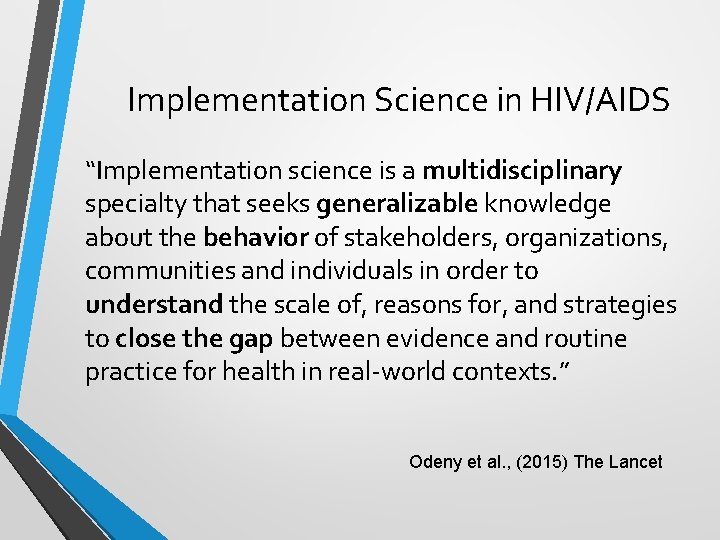
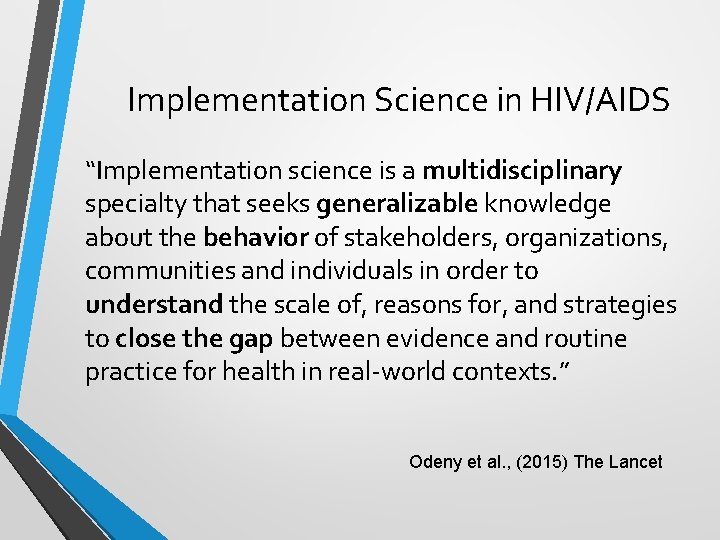
Implementation Science in HIV/AIDS “Implementation science is a multidisciplinary specialty that seeks generalizable knowledge about the behavior of stakeholders, organizations, communities and individuals in order to understand the scale of, reasons for, and strategies to close the gap between evidence and routine practice for health in real-world contexts. ” Odeny et al. , (2015) The Lancet
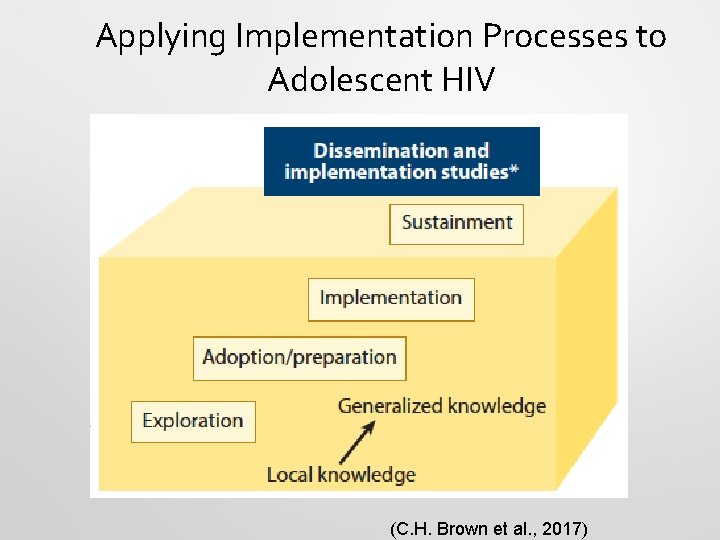
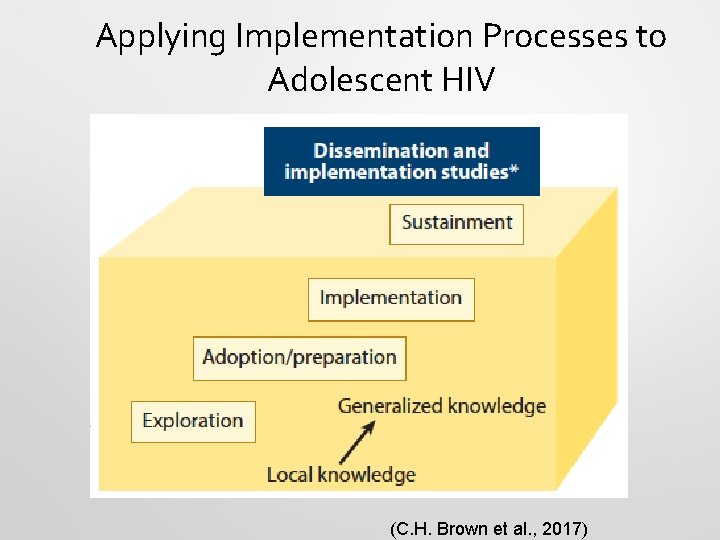
Applying Implementation Processes to Adolescent HIV (C. H. Brown et al. , 2017)
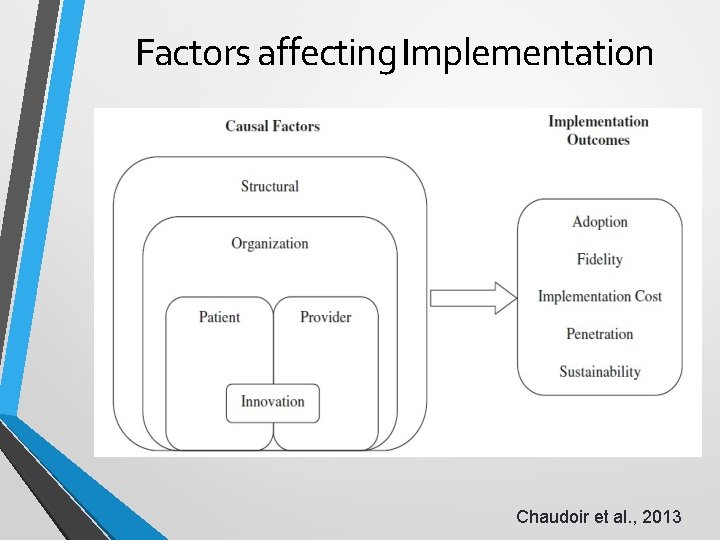
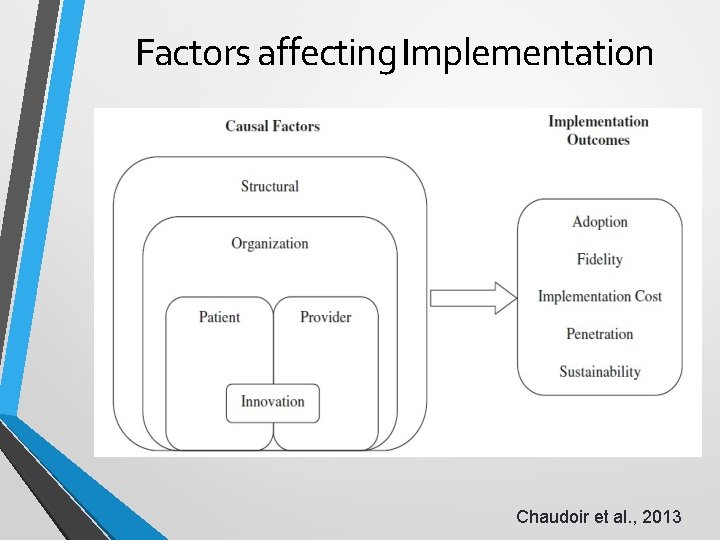
Factors affecting Implementation Chaudoir et al. , 2013
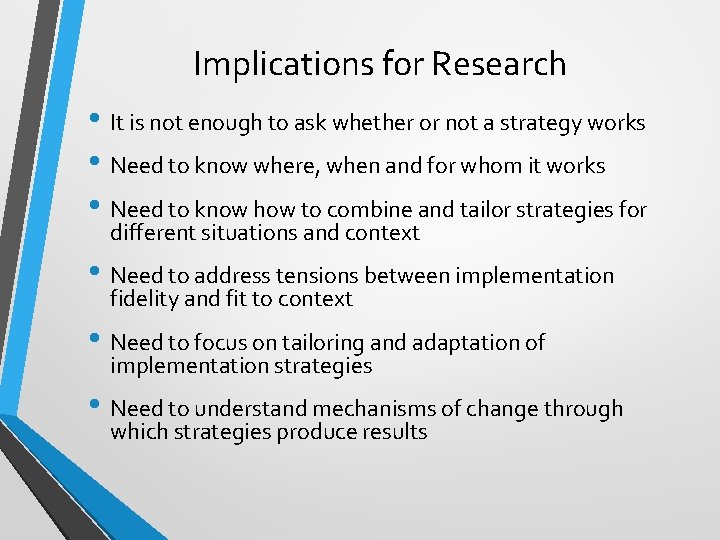
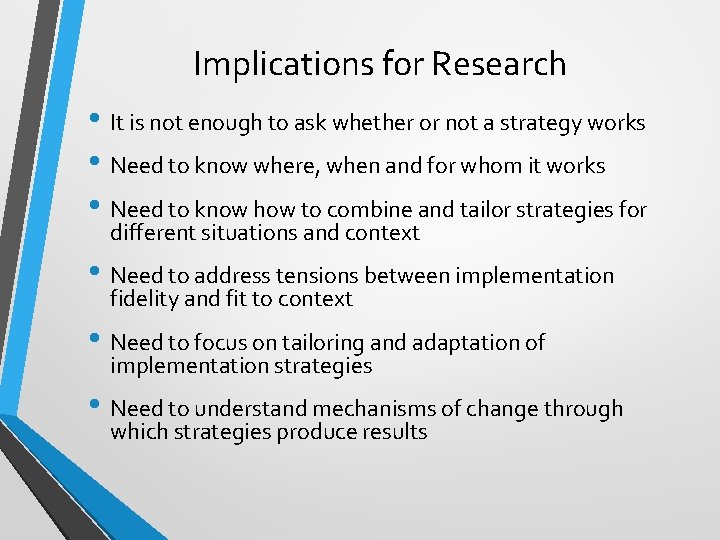
Implications for Research • It is not enough to ask whether or not a strategy works • Need to know where, when and for whom it works • Need to know how to combine and tailor strategies for different situations and context • Need to address tensions between implementation fidelity and fit to context • Need to focus on tailoring and adaptation of implementation strategies • Need to understand mechanisms of change through which strategies produce results
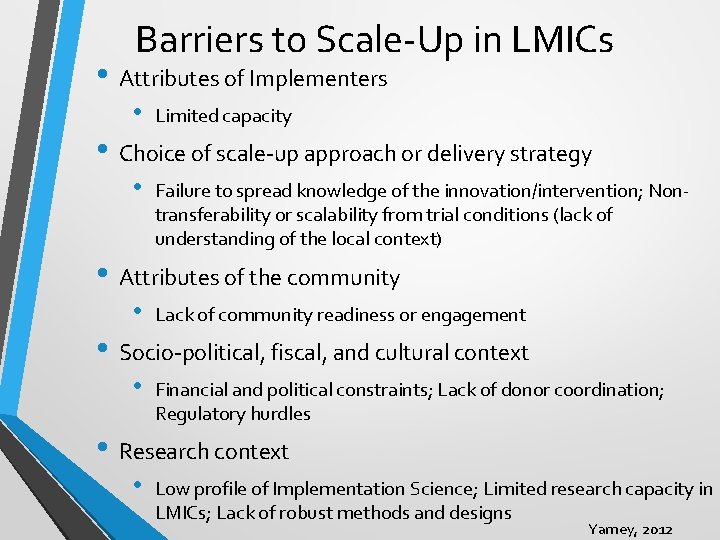
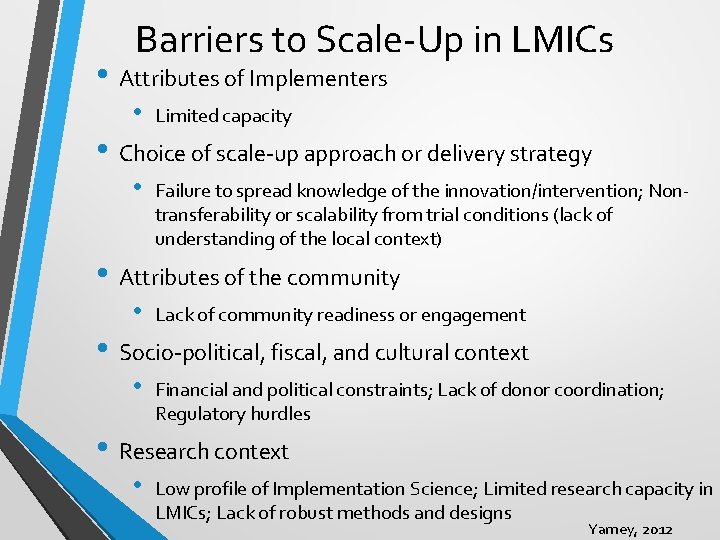
Barriers to Scale-Up in LMICs • Attributes of Implementers • Limited capacity • Choice of scale-up approach or delivery strategy • Failure to spread knowledge of the innovation/intervention; Nontransferability or scalability from trial conditions (lack of understanding of the local context) • Attributes of the community • Lack of community readiness or engagement • Socio-political, fiscal, and cultural context • Financial and political constraints; Lack of donor coordination; Regulatory hurdles • Research context • Low profile of Implementation Science; Limited research capacity in LMICs; Lack of robust methods and designs Yamey, 2012

Where is D&I Research Heading Next? • Pooling D&I research data • Mechanistic D&I research • De-implementation • Innovation vs. Replication • Avoiding silos between D&I research and D&I practice • Harnessing and embracing all evidence • Return on investment of D&I research Brownson, Colditz, & Proctor (2018)

Thank You
BUILDING IMPLEMENTATION SCIENCE EXPERTISE IN AFRICA: THE UNC/WITS UNIVERSITY COLLABORATION FOGARTY D 43 Audrey Pettifor Jabulani Ncayiyana Latifat Ibisomi Tobias Chirwa Kathyrn Salisbury Rohit Ramaswamy
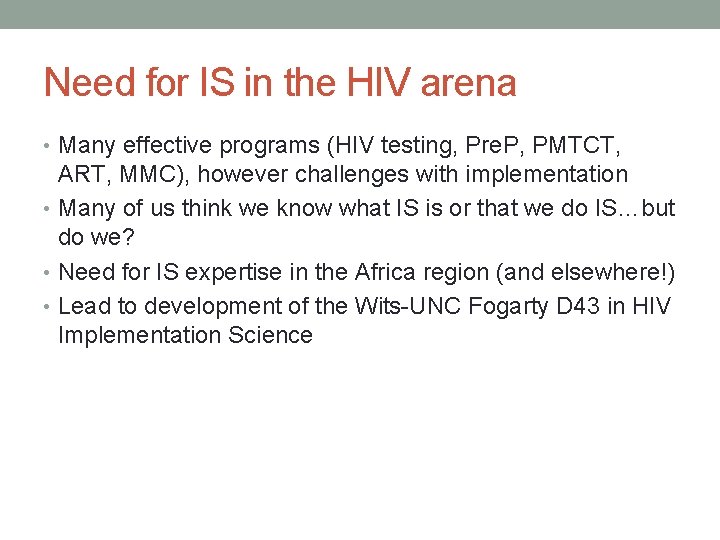
Need for IS in the HIV arena • Many effective programs (HIV testing, Pre. P, PMTCT, ART, MMC), however challenges with implementation • Many of us think we know what IS is or that we do IS…but do we? • Need for IS expertise in the Africa region (and elsewhere!) • Lead to development of the Wits-UNC Fogarty D 43 in HIV Implementation Science
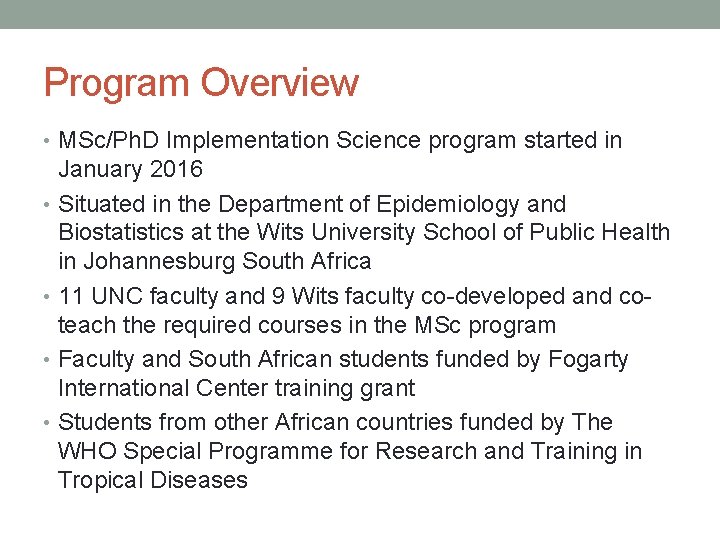
Program Overview • MSc/Ph. D Implementation Science program started in January 2016 • Situated in the Department of Epidemiology and Biostatistics at the Wits University School of Public Health in Johannesburg South Africa • 11 UNC faculty and 9 Wits faculty co-developed and coteach the required courses in the MSc program • Faculty and South African students funded by Fogarty International Center training grant • Students from other African countries funded by The WHO Special Programme for Research and Training in Tropical Diseases
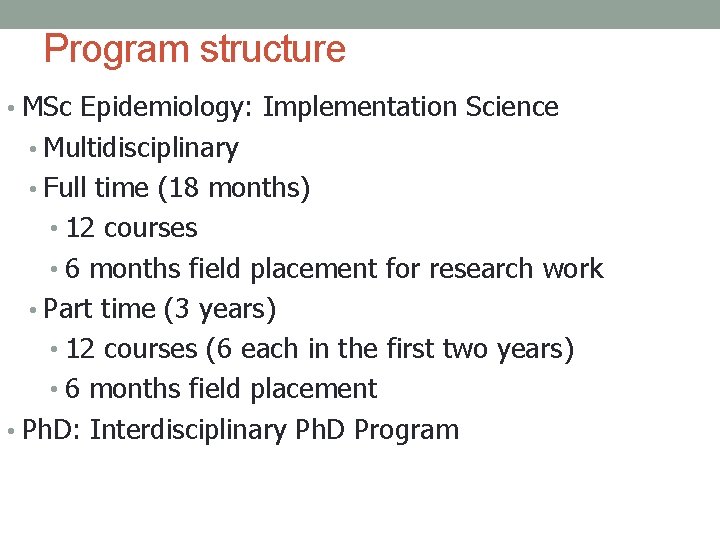
Program structure • MSc Epidemiology: Implementation Science • Multidisciplinary • Full time (18 months) • 12 courses • 6 months field placement for research work • Part time (3 years) • 12 courses (6 each in the first two years) • 6 months field placement • Ph. D: Interdisciplinary Ph. D Program
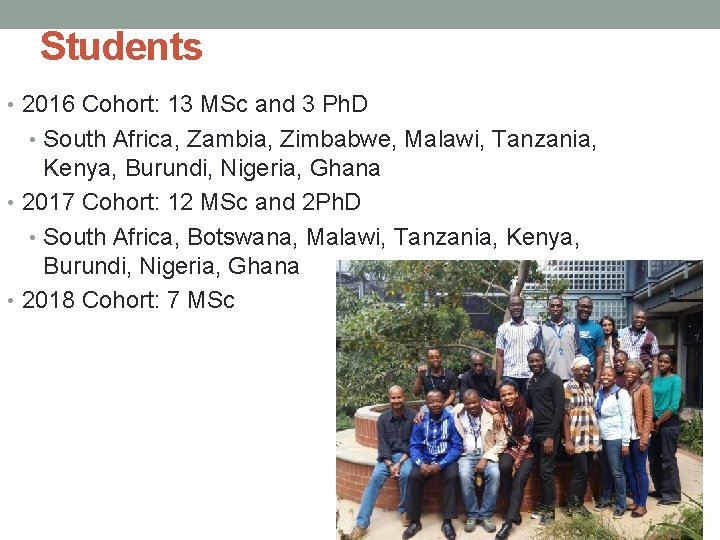
Students • 2016 Cohort: 13 MSc and 3 Ph. D • South Africa, Zambia, Zimbabwe, Malawi, Tanzania, Kenya, Burundi, Nigeria, Ghana • 2017 Cohort: 12 MSc and 2 Ph. D • South Africa, Botswana, Malawi, Tanzania, Kenya, Burundi, Nigeria, Ghana • 2018 Cohort: 7 MSc
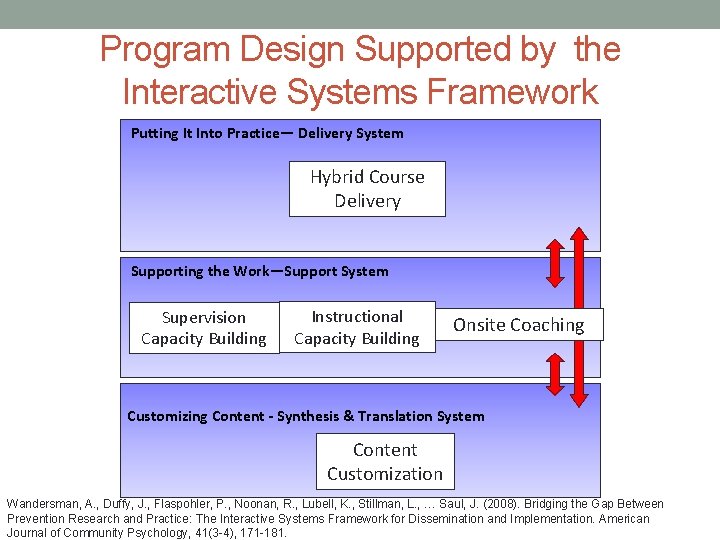
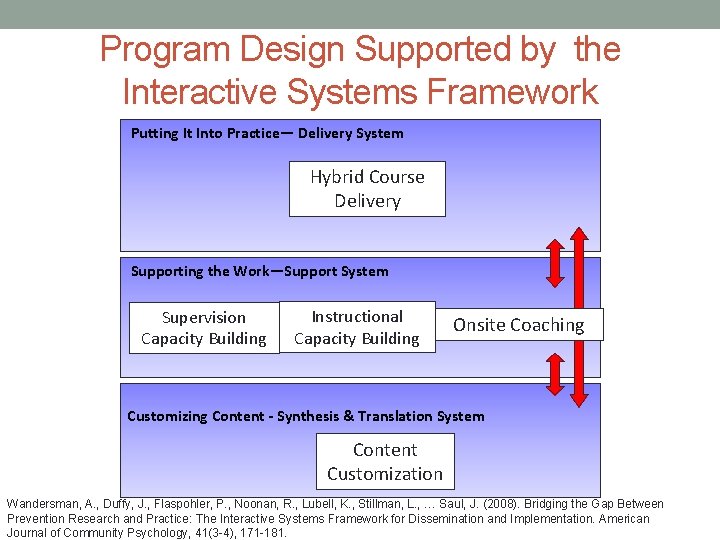
Program Design Supported by the Interactive Systems Framework Putting It Into Practice— Delivery System Hybrid Course Delivery Supporting the Work—Support System Supervision Capacity Building Instructional Capacity Building Onsite Coaching Customizing Content - Synthesis & Translation System Content Customization Wandersman, A. , Duffy, J. , Flaspohler, P. , Noonan, R. , Lubell, K. , Stillman, L. , … Saul, J. (2008). Bridging the Gap Between Prevention Research and Practice: The Interactive Systems Framework for Dissemination and Implementation. American Journal of Community Psychology, 41(3 -4), 171 -181.
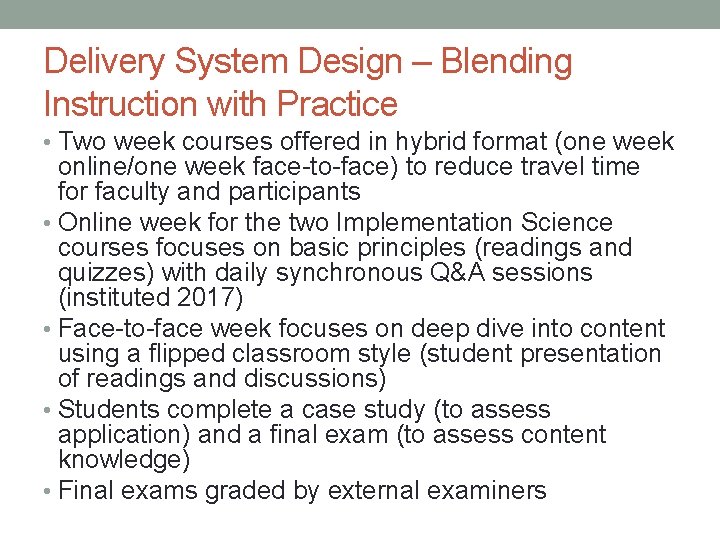
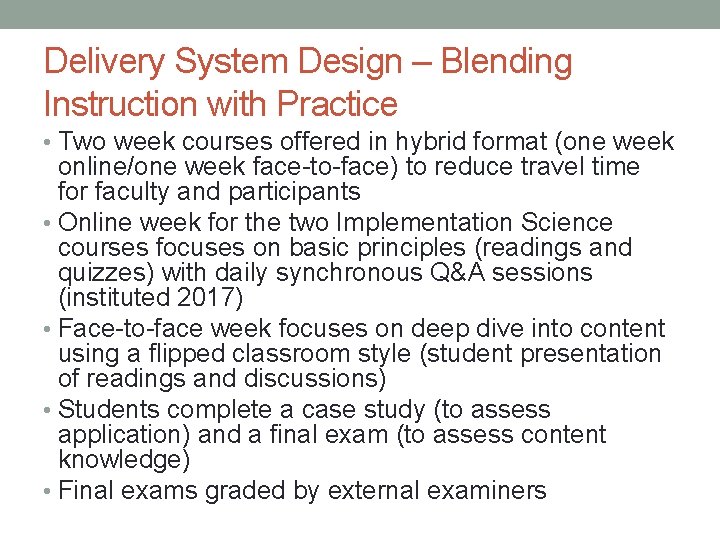
Delivery System Design – Blending Instruction with Practice • Two week courses offered in hybrid format (one week online/one week face-to-face) to reduce travel time for faculty and participants • Online week for the two Implementation Science courses focuses on basic principles (readings and quizzes) with daily synchronous Q&A sessions (instituted 2017) • Face-to-face week focuses on deep dive into content using a flipped classroom style (student presentation of readings and discussions) • Students complete a case study (to assess application) and a final exam (to assess content knowledge) • Final exams graded by external examiners
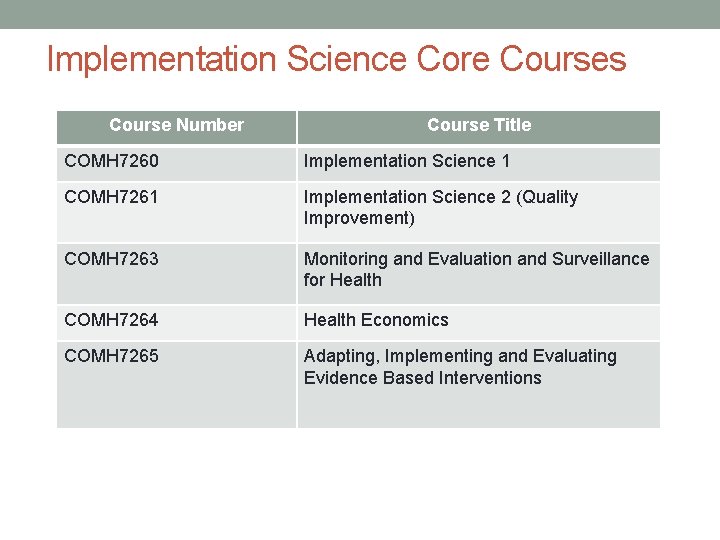
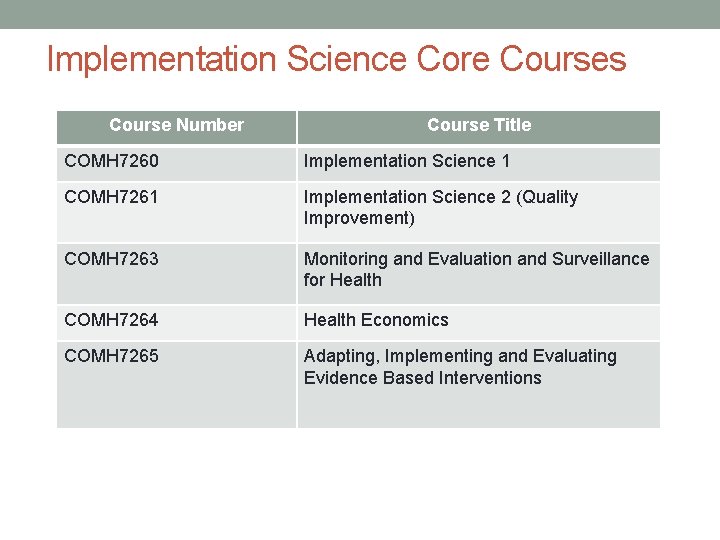
Implementation Science Core Courses Course Number Course Title COMH 7260 Implementation Science 1 COMH 7261 Implementation Science 2 (Quality Improvement) COMH 7263 Monitoring and Evaluation and Surveillance for Health COMH 7264 Health Economics COMH 7265 Adapting, Implementing and Evaluating Evidence Based Interventions
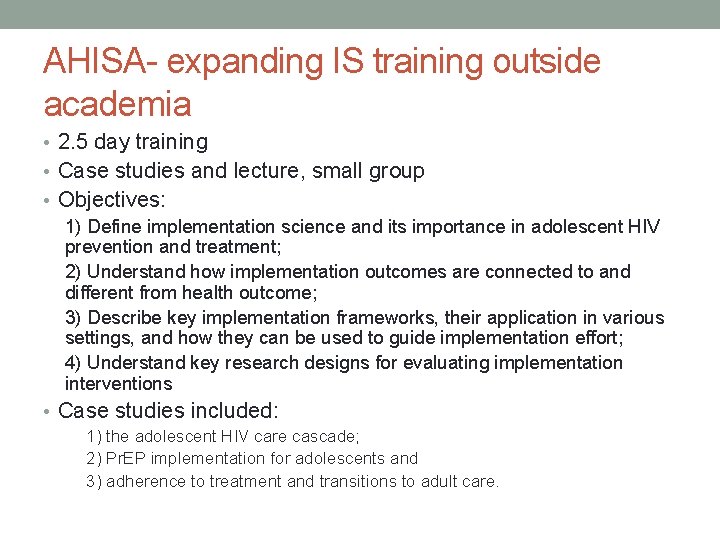
AHISA- expanding IS training outside academia • 2. 5 day training • Case studies and lecture, small group • Objectives: 1) Define implementation science and its importance in adolescent HIV prevention and treatment; 2) Understand how implementation outcomes are connected to and different from health outcome; 3) Describe key implementation frameworks, their application in various settings, and how they can be used to guide implementation effort; 4) Understand key research designs for evaluating implementation interventions • Case studies included: 1) the adolescent HIV care cascade; 2) Pr. EP implementation for adolescents and 3) adherence to treatment and transitions to adult care.
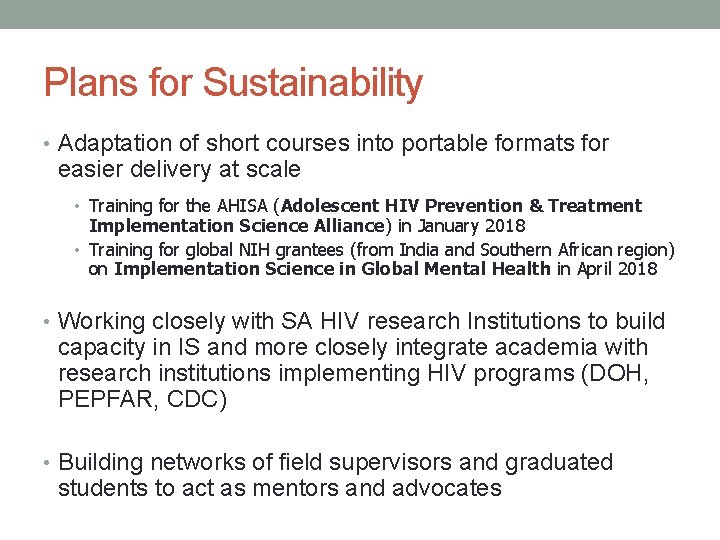
Plans for Sustainability • Adaptation of short courses into portable formats for easier delivery at scale • Training for the AHISA (Adolescent HIV Prevention & Treatment Implementation Science Alliance) in January 2018 • Training for global NIH grantees (from India and Southern African region) on Implementation Science in Global Mental Health in April 2018 • Working closely with SA HIV research Institutions to build capacity in IS and more closely integrate academia with research institutions implementing HIV programs (DOH, PEPFAR, CDC) • Building networks of field supervisors and graduated students to act as mentors and advocates

High-yield HIV testing, facilitated linkage to care and prevention for female youth in Kenya (GIRLS Study) Kawango Agot, Ph. D, MPH AHISA IAS Satellite Session July 26, 2018 Principal Investigators: Ann Kurth, Irene Inwani, Kawango Agot NIAID 1 R 01 AI 122797
Background Compared to women ages 25+ years, AGYW have: § Lower HIV testing rates [KAIS, 2014; UNICEF, 2012; WHO, 2013] § Lower rates of linkage to and retention in care for positives [KASF 2014; Arrive et al, 2012; WHO, 2013] § Lower rates of adherence to treatment and consequently, of viral suppression [Jean et al, AIDS, 2016; Nglazi, et al 2012; Ryscavage, 2011] § Yet, there are fewer effective prevention strategies for HIV negative AGYW [UNAIDS 2014; Dellar et al, 2015; Mavedzenge et al, 2011]
Research Aims Within a framework of implementation science we want to § Aim 1: Determine preferred recruitment venue and testing modality that targets and finds the highest number of previously undiagnosed HIV infected and high risk uninfected AGYW aged 15 -24 years in Homa Bay County § § 2 ‘seek’ strategies: community or home-based 3 ‘test’ strategies: self-testing, HTS in home or mobile setting by study staff, or referral for facility-based HTS § Aim 3: Conduct cost effectiveness analyses to determine the relative utility of the different seek, testing, and linkage interventions
Research Aims § Aim 2 a: Pilot and evaluate an adaptive intervention to link HIVpositive female youth to treatment and care services § Aim 2 b: Identify barriers and facilitators to seeking HIV care services after receiving a positive diagnosis § Aim 2 c: Identify barriers and facilitators to seeking HIV prevention services for high risk female youth after receiving a negative HIV test result § Aim 2 d: Provide an HIV prevention intervention to a randomly selected subset of high risk negatives (n≈185) (motivational text message, with referral for combination prevention interventions), and retest them at 12 months
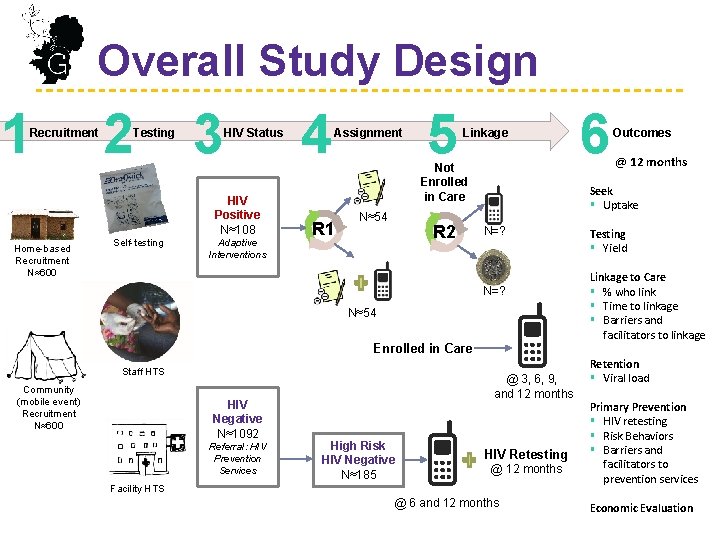
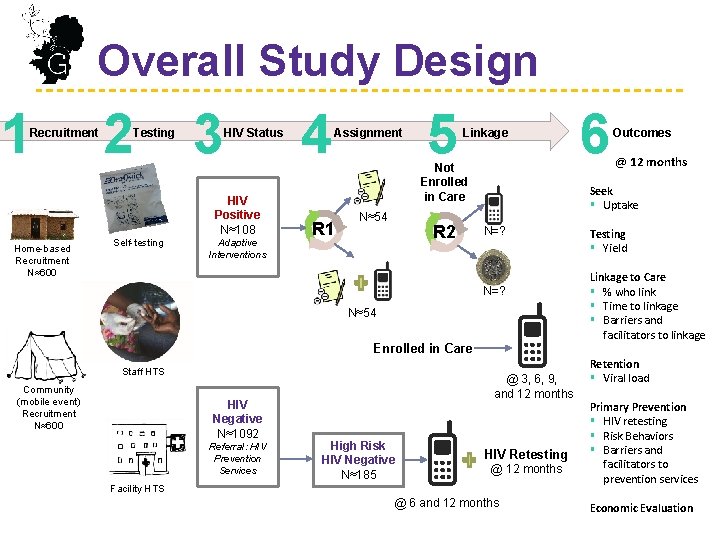
Overall Study Design 1 Recruitment 2 Testing 3 HIV Status HIV Positive N≈108 Home-based Recruitment N≈600 Self-testing Adaptive Interventions 4 Assignment R 1 5 Linkage Not Enrolled in Care N≈54 R 2 N=? N≈54 Enrolled in Care Community (mobile event) Recruitment N≈600 HIV Negative N≈1092 Referral: HIV Prevention Services @ 3, 6, 9, and 12 months High Risk HIV Negative N≈185 @ 12 months Seek § Uptake N=? Staff HTS 6 Outcomes HIV Retesting @ 12 months Facility HTS @ 6 and 12 months Testing § Yield Linkage to Care § % who link § Time to linkage § Barriers and facilitators to linkage Retention § Viral load Primary Prevention § HIV retesting § Risk Behaviors § Barriers and facilitators to prevention services Economic Evaluation
![Preliminary Findings AGYWs prefer homebased recruitment 84 strategy and staffaided HIV testing Preliminary Findings § AGYW’s prefer home-based recruitment [84%] strategy and staff-aided HIV testing](https://slidetodoc.com/presentation_image_h/d64044f3d0ade94d3bfac0ed2a9637eb/image-31.jpg)
Preliminary Findings § AGYW’s prefer home-based recruitment [84%] strategy and staff-aided HIV testing [81%] § For those who selected the self-testing option: • No invalid results • No serious adverse events • 99% strongly agreed or agreed that HIVST was acceptable • 99% thought doing HIVST was easy or very easy § Newly diagnosed HIV prevalence 2. 7% § 18% negative AGYW identified as high risk (with a HIV prevalence of 6. 5%)
Next Steps § High prevalence of high risk HIV-negative AGYW demonstrate the importance of HIV testing to inform prevention interventions to avert new infections § What public health campaign will be needed to increase uptake of HIV self-testing among AGYW? § How can implementation science guide HTS delivery to AGYW and identification of previously undiagnosed individuals?
KRISTIN BEIMA-SOFIE, PHD, MPH IRENE NJUGUNA, MBCHB, MSC, MPH Global WACh at the University of Washington
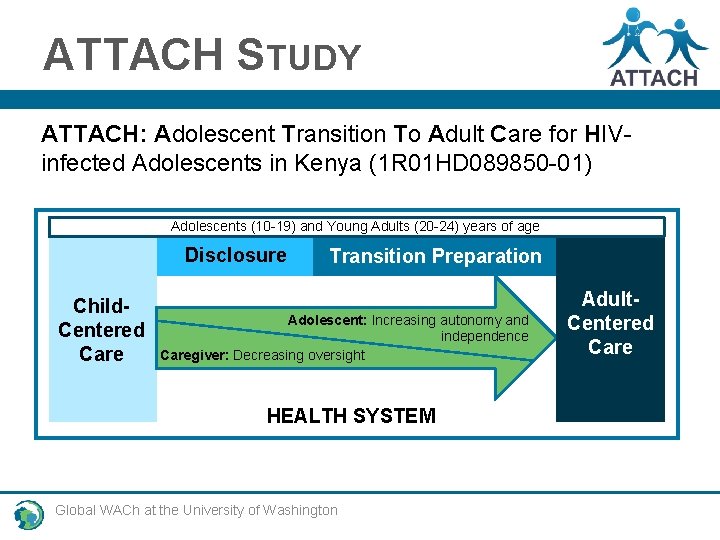
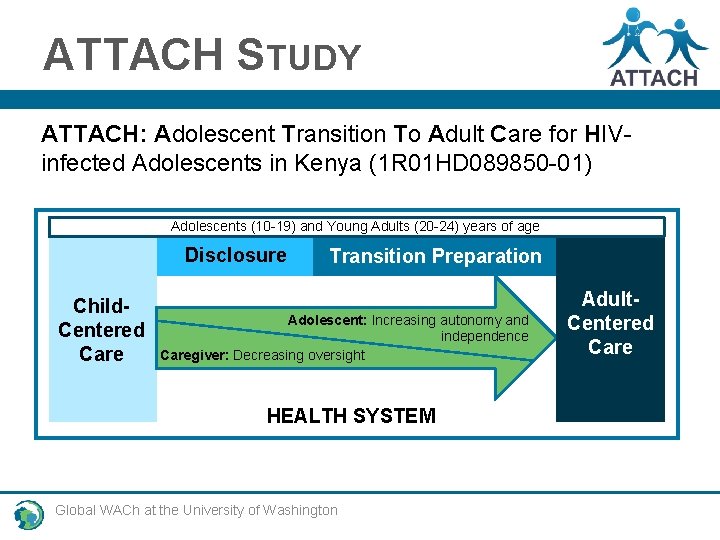
ATTACH STUDY ATTACH: Adolescent Transition To Adult Care for HIVinfected Adolescents in Kenya (1 R 01 HD 089850 -01) Adolescents (10 -19) and Young Adults (20 -24) years of age Disclosure Child. Centered Care Transition Preparation Adolescent: Increasing autonomy and independence Caregiver: Decreasing oversight HEALTH SYSTEM Global WACh at the University of Washington Adult. Centered Care
ATTACH STUDY ATTACH: Adolescent Transition To Adult Care for HIVinfected Adolescents in Kenya (1 R 01 HD 089850 -01) Primary Study Objectives: 1 – Improve knowledge of transition practices and outcomes *International Workshop on HIV Pediatrics Abstract #123: Transitioning adolescents to adult HIV care: Health facility models of care and transition practices in Kenya 2 – Develop and evaluate an Adolescent Transition Package Global WACh at the University of Washington
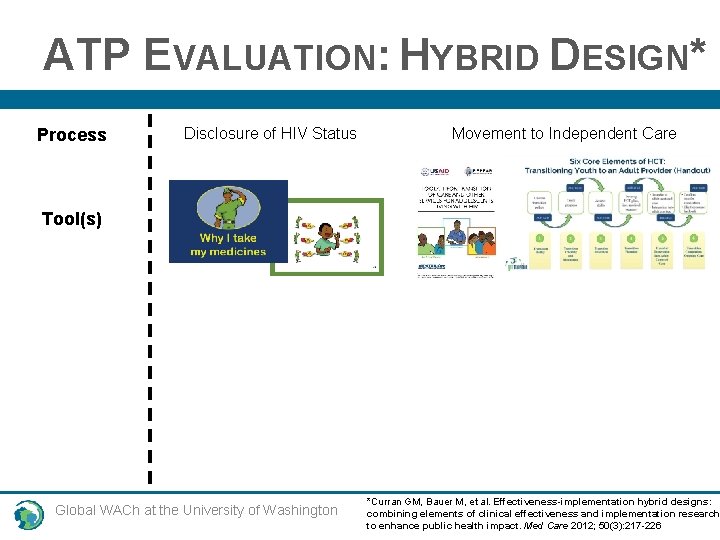
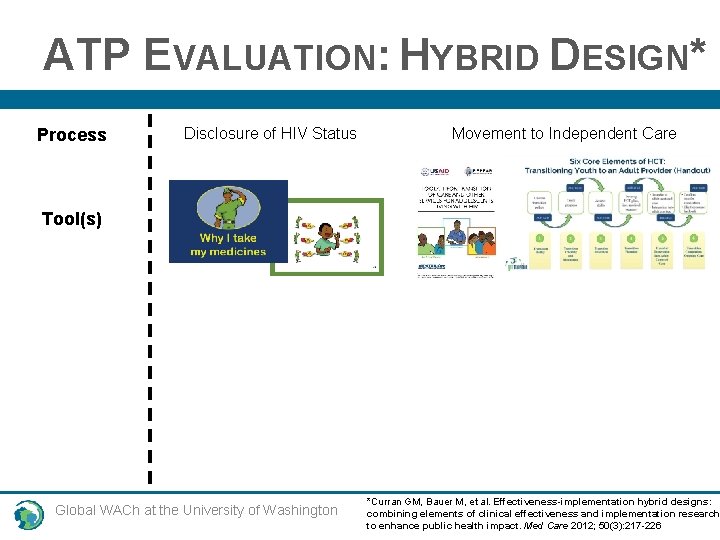
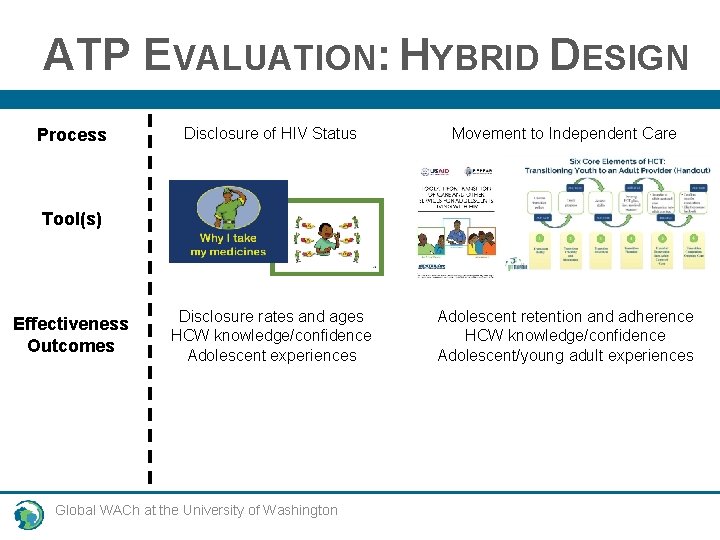
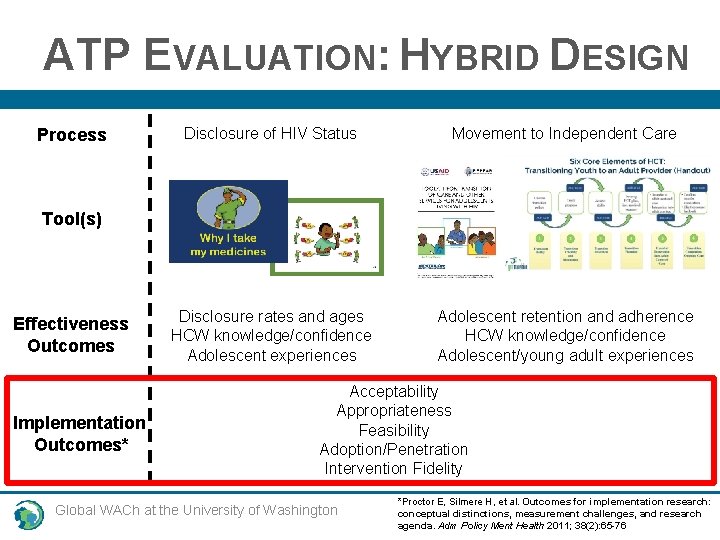
ATP EVALUATION: HYBRID DESIGN* Process Disclosure of HIV Status Movement to Independent Care Tool(s) Global WACh at the University of Washington *Curran GM, Bauer M, et al. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012; 50(3): 217 -226
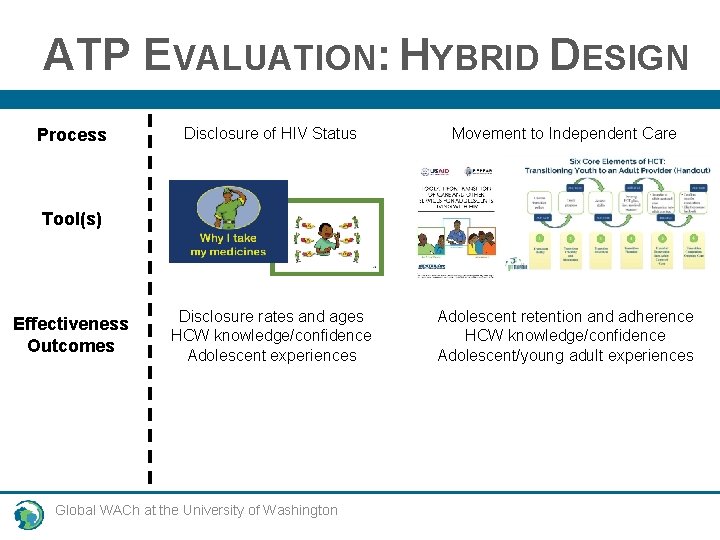
ATP EVALUATION: HYBRID DESIGN Process Disclosure of HIV Status Movement to Independent Care Disclosure rates and ages HCW knowledge/confidence Adolescent experiences Adolescent retention and adherence HCW knowledge/confidence Adolescent/young adult experiences Tool(s) Effectiveness Outcomes Global WACh at the University of Washington
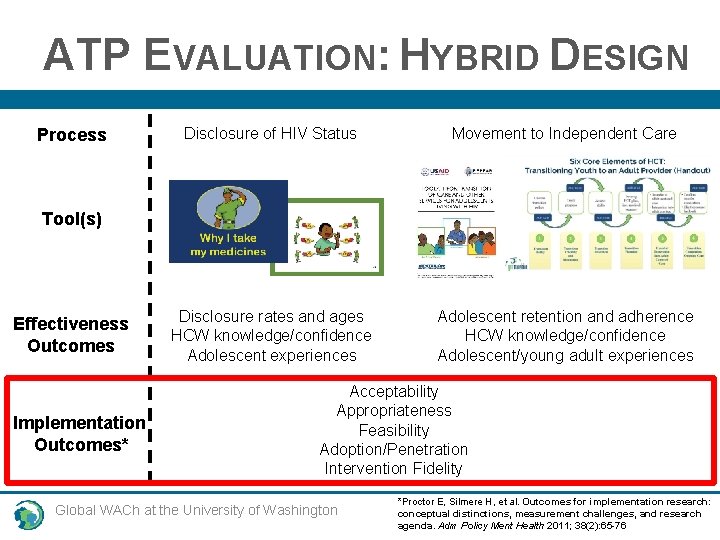
ATP EVALUATION: HYBRID DESIGN Process Disclosure of HIV Status Movement to Independent Care Disclosure rates and ages HCW knowledge/confidence Adolescent experiences Adolescent retention and adherence HCW knowledge/confidence Adolescent/young adult experiences Tool(s) Effectiveness Outcomes Implementation Outcomes* Acceptability Appropriateness Feasibility Adoption/Penetration Intervention Fidelity Global WACh at the University of Washington *Proctor E, Silmere H, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011; 38(2): 65 -76
NEXT STEPS: 1 Health System 2 Adolescent Autonomy 3 Influence of Technology Global WACh at the University of Washington
THANK YOU! Global WACh at the University of Washington

Social Media Messaging for HIV Testing in Zimbabwe Marguerita Lightfoot, Ph. D University of California, San Francisco 2018 Internationa AIDS Conference Adolescent HIV prevention and treatment implementation science alliance
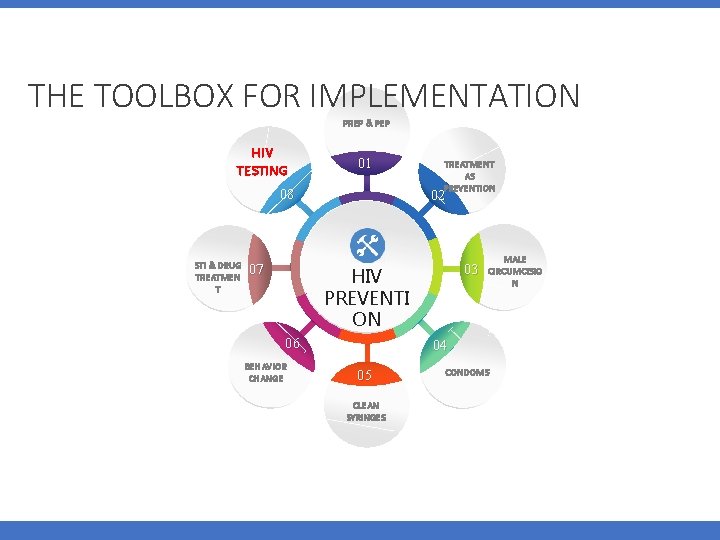
THE TOOLBOX FOR IMPLEMENTATION PREP & PEP HIV TESTING 01 08 STI & DRUG TREATMEN T 07 TREATMENT AS PREVENTION 02 03 HIV POWERP PREVENTI OINT TEMPLATE ON 06 BEHAVIOR CHANGE MALE CIRCUMCISIO N 04 05 CLEAN SYRINGES CONDOMS
Challenges to adhering to HIV Testing recommendations • Low use of primary care • Lack of adolescent-friendly service • Cost • Transportation • Lack of adolescent knowledge of HIV/STI • Stigma • Providers (Untrained for working with adolescents, Judgmental) • Consent laws for sexual and reproductive health
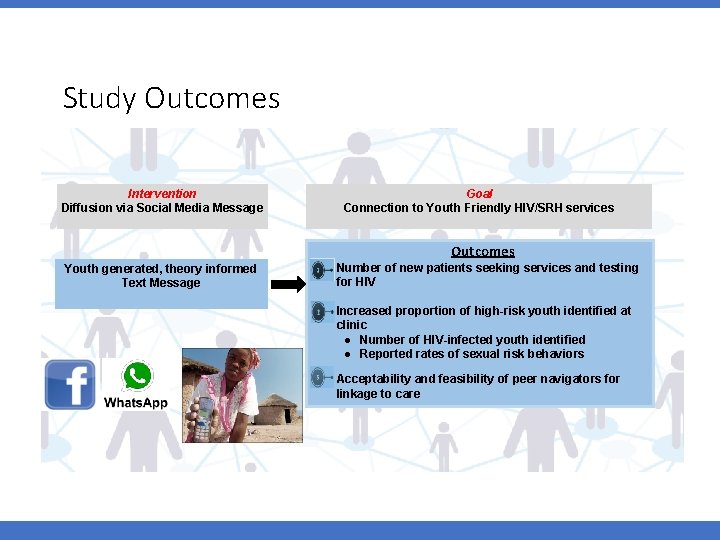
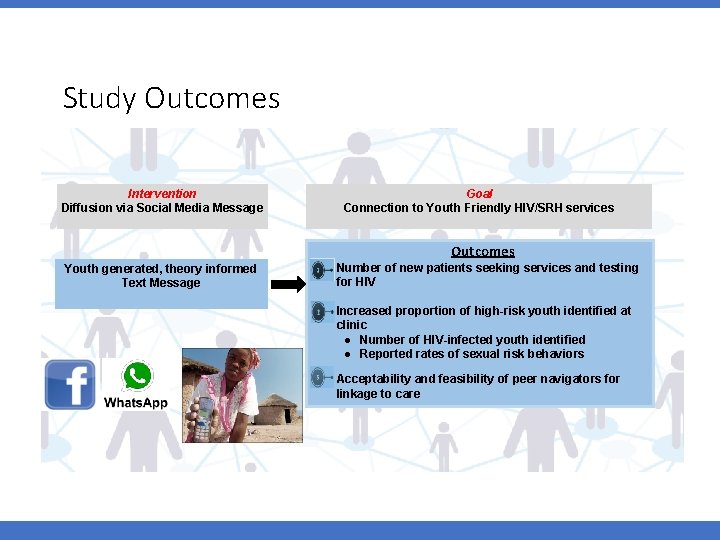
Study Outcomes Intervention Diffusion via Social Media Message Youth generated, theory informed Text Message Goal Connection to Youth Friendly HIV/SRH services Outcomes Number of new patients seeking services and testing for HIV Increased proportion of high-risk youth identified at clinic ● Number of HIV-infected youth identified ● Reported rates of sexual risk behaviors Acceptability and feasibility of peer navigators for linkage to care
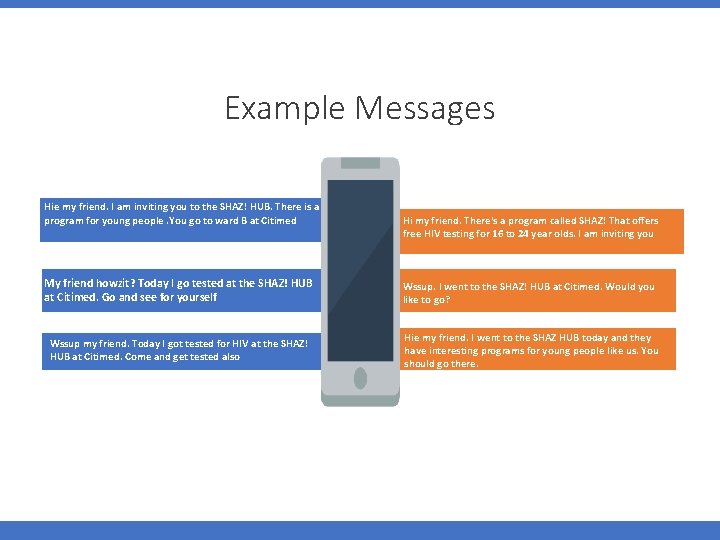
Example Messages Hie my friend. I am inviting you to the SHAZ! HUB. There is a program for young people. You go to ward B at Citimed Hi my friend. There's a program called SHAZ! That offers free HIV testing for 16 to 24 year olds. I am inviting you My friend howzit? Today I go tested at the SHAZ! HUB at Citimed. Go and see for yourself Wssup. I went to the SHAZ! HUB at Citimed. Would you like to go? Wssup my friend. Today I got tested for HIV at the SHAZ! HUB at Citimed. Come and get tested also Hie my friend. I went to the SHAZ HUB today and they have interesting programs for young people like us. You should go there.
Example Responses From recipients of messages • I will pay them a visit. Thanks my friend • You should have come so that we could go together • I would like to go. You can come and take me then we can go together • Thanks. I also want to and get circumcised • Thanks. Are there any jobs because we are tired of staying at home? • I will first have to gather courage because I have indulged in scary things • Do they open on weekends so that we can go? • Do they give you bus fare? • The pricking is painful. It's better not to go
The Way Forward Formal integration of implementation models Further examination of peer based models Messaging to create demand Understand strengthen provider-initiated testing and counseling o Extend clinic hours o Adolescent consent o Provider training on adolescent development • School-based testing? • •
Thank you Team Megan Dunbar (Pangaea Zimbabwe) Alfred Chingono (UZ UCSF) Nicola Willis (Africaid) Staff and Collaborators Ministry of Health Youth and families NICHD
The Girl Power Case Study: Enhancing Service Uptake in the Public Sector among Adolescent Girls and Young Women Nora E. Rosenberg, Ph. D July 26, 2018 AHISA Co-investigators: Audrey Pettifor, Linda-Gail. Bekker, Laura Myers Malawi team: Dhru Vansia, Twambilile Phanga, Nivedita Bhushan, Bertha Maseko, Annie Kachigamba The Girl Power study was funded by Evidence for HIV Prevention in Southern Africa (EHPSA), a DFID program managed by Mott Mac. Donald.
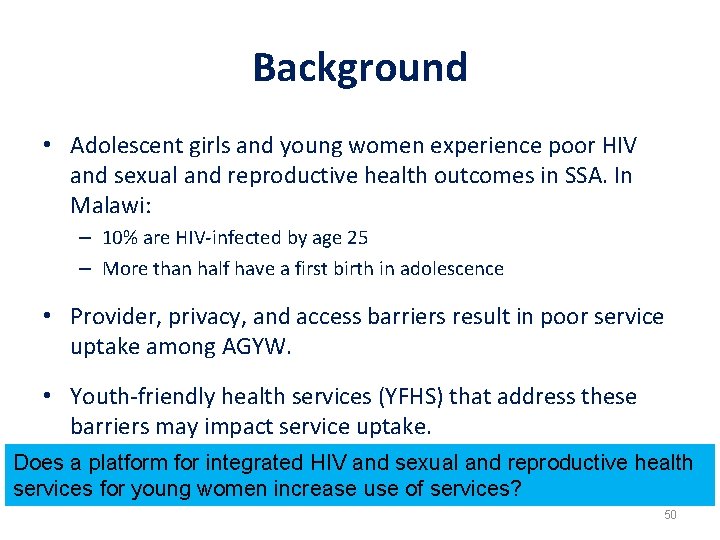
Background • Adolescent girls and young women experience poor HIV and sexual and reproductive health outcomes in SSA. In Malawi: – 10% are HIV-infected by age 25 – More than half have a first birth in adolescence • Provider, privacy, and access barriers result in poor service uptake among AGYW. • Youth-friendly health services (YFHS) that address these barriers may impact service uptake. Does a platform for integrated HIV and sexual and reproductive health services for young women increase use of services? 50
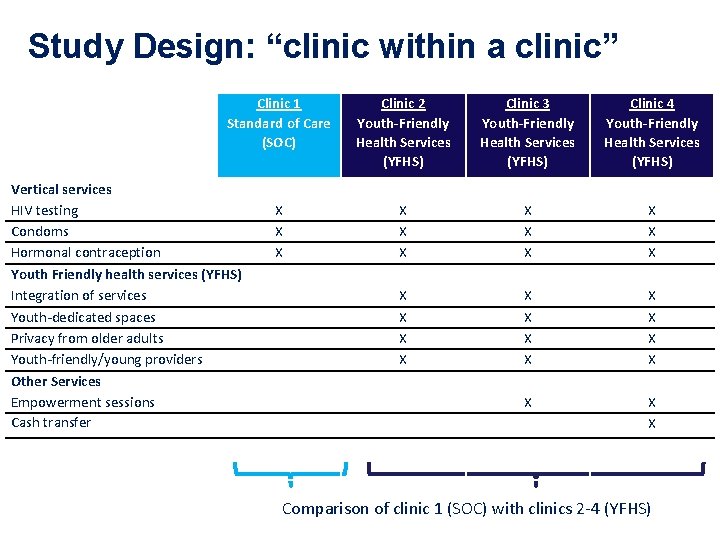
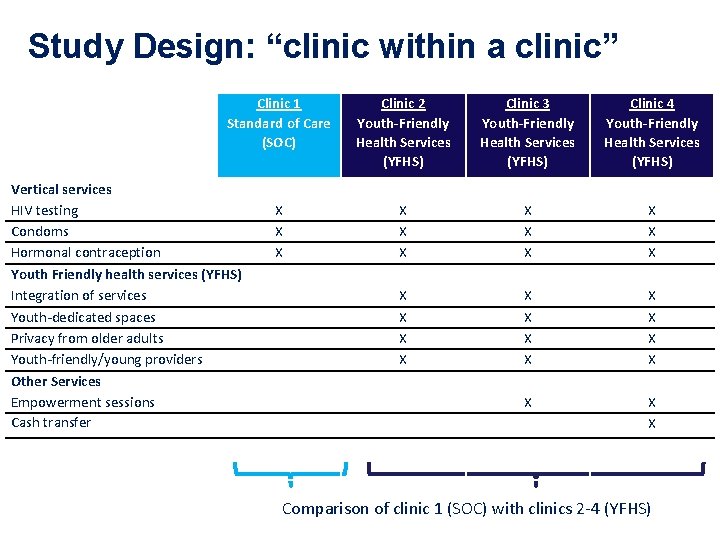
Study Design: “clinic within a clinic” Clinic 1 Standard of Care (SOC) Vertical services HIV testing Condoms Hormonal contraception Youth Friendly health services (YFHS) Integration of services Youth-dedicated spaces Privacy from older adults Youth-friendly/young providers Other Services Empowerment sessions Cash transfer Clinic 2 Youth-Friendly Health Services (YFHS) Clinic 3 Youth-Friendly Health Services (YFHS) Clinic 4 Youth-Friendly Health Services (YFHS) X X X X X X X X Comparison of clinic 1 (SOC) with clinics 2 -4 (YFHS)
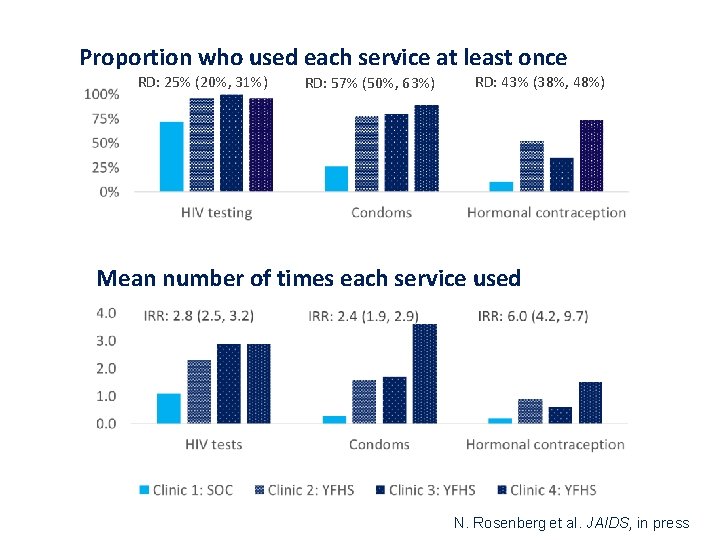
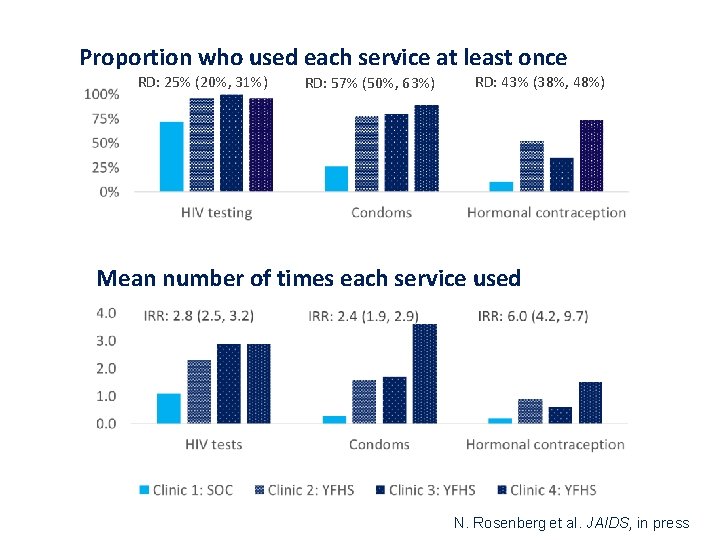
Proportion who used each service at least once RD: 25% (20%, 31%) RD: 57% (50%, 63%) RD: 43% (38%, 48%) Mean number of times each service used N. Rosenberg et al. JAIDS, in press
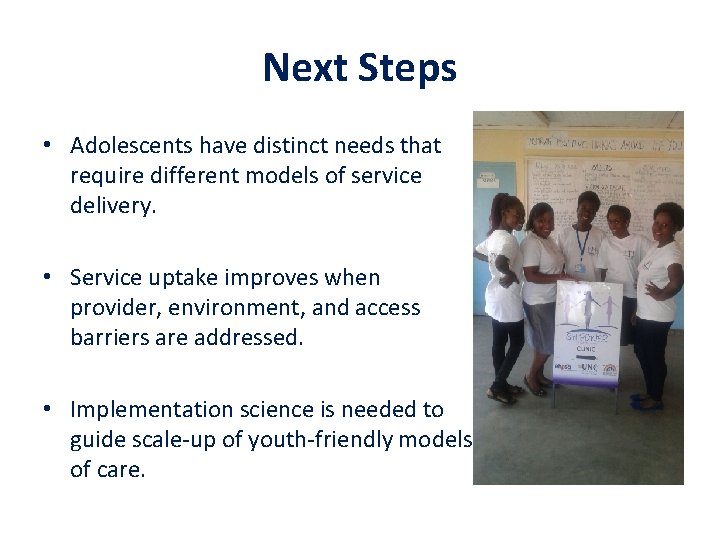
Next Steps • Adolescents have distinct needs that require different models of service delivery. • Service uptake improves when provider, environment, and access barriers are addressed. • Implementation science is needed to guide scale-up of youth-friendly models of care.

The Nigeria Implementation Science Alliance (NISA) Dr. Nadia A. Sam-Agudu Senior Technical Advisor, Pediatric and Adolescent HIV Institute of Human Virology Nigeria Abuja, Nigeria. Institute of Human Virology, University of Maryland School of Medicine, Baltimore, USA July 26, 2018 #AIDS 2018 | @AIDS_conference | www. aids 2018. org
Brief NISA Background • NIH PMTCT Implementation Science Alliance • NIH Adolescent HIV Prevention and Treatment Implementation Science Alliance (AHISA) • NISA, born 2015: a collaborative consortium of – Public health NGOs (local Implementing Partners) – Researchers and academia – Policy-makers • NISA also collaborates with bilateral and #AIDS 2018 | @AIDS_conference | www. aids 2018. org multi-lateral organizations.

NISA Vision and its 20 Member Organizations • Implementation Science + Alliance • Overall aim: to generate, evaluate and disseminate implementation science evidence in Nigeria. • Focus on public health problems of greatest importance. #AIDS 2018 | @AIDS_conference | www. aids 2018. org
NISA: A Different Way of Thinking and Doing • Approach: Active and equitable participation of committed and competent partners – Interests are national and collective; not individual • Annual conference since 2015 – Collectively & exclusively funded by consortium • Grant-writing: – Idea Lead PI/NGO; multi-PI mechanism • Study protocols: IS, multi-site, multi-partner – Potentially national scope and impact #AIDS 2018 | @AIDS_conference | www. aids 2018. org
NISA: A Different Way of Thinking and Doing • Dissemination: to policy-makers with whom we have continuous, collaborative contact • Scholarship: annual conference papers and collaborative articles • Capacity-building: mentorship, menteeship – NISA wants to develop local, independent IS PIs #AIDS 2018 | @AIDS_conference | www. aids 2018. org
Do You Want a NISA in Your Country? Here are some lessons learned: • Examine and re-examine state of public health, public health research and IS in your country • Engage the right stakeholders: Competent, Committed, and Influential • Be ready to relinquish power/distribute it as equitably as possible • Focus on “collective >> individual” theme – Means sometimes sacrifices have to be made • Practice true Global Health and IS principles – Serve needs and interests of your target population • Be fiercely protective of your collective vision! #AIDS 2018 | @AIDS_conference | www. aids 2018. org

Shameless plug… https: //www. nisaresearch. org/ #AIDS 2018 | @AIDS_conference | www. aids 2018. org

Acknowledgements • NISA members and partners – esp. Dr. Echezona Ezeanolue & Ms. Dina Patel, PNP • US National Institutes of Health – esp. Fogarty International Center, AHISA • Government of Nigeria – esp. Federal Ministry of Health • Nigerians – Esp. people living with HIV #AIDS 2018 | @AIDS_conference | www. aids 2018. org
THANK YOU! https: //www. fic. nih. gov/About/center-global-healthstudies/Pages/adolescent-hiv-prevention-treatmentimplementation-science-alliance. aspx Rachel. Sturke@nih. gov Susan. Vorkoper@nih. gov #AIDS 2018 | @AIDS_conference | www. aids 2018. org