UPDATED REVIEW IN NEUROSURGICAL ANESTHESIOLOGY AND NEUROCRITICAL CARE



























































- Slides: 59

UPDATED REVIEW IN NEUROSURGICAL ANESTHESIOLOGY AND NEURO-CRITICAL CARE RAMSIS F. GHALY, MD, FACS DEPARTMENT OF ANESTHESIOLGY AND PAIN MANAGEMENT, ADVOCATE ILLINOIS MASONIC MEDICAL CENTER GHALY NEUROSURGICAL ASSOCIATES

CBF: METHODOLOGY • Methodology: (Kety Schmidt Technique): Consumption of a substance by an organ is the product of blood flow and arteriovenous (arterial and juglar bulb) difference for that substance with knowledge od blood-brain partition coefficient. Indicators: Diffusable substance e. g. N 2 O, Xe, Ar 133, Kr 85, Non-diffusable e. g. microsphere. Arteriovenous sampling over 10 -14 min Or external detection of washout with scintillation detectors post xenon inhalation/injection. Tomographic method: enhancement by stable Xe. PET will require Cyclotron-produced short lived radio isotopes. MRSpectroscopy measures brain substrates like ATP and others.

CEREBRAL METABOLIC RATE • CMR=CBF/ARTERIOVENOUS DIFFERENCE • CMRO 2 relatively stable and no change with Pa. CO 2 2080 mm. Hg • COUPLING: Maintenance of CBF: CMRO 2 ratio (14 -18) i. e. ↑ in acivated areas and ↓ in unstimulated areas) • O 2 3. 3 ML/100 G/MIN (brain 20%O 2 uptake while <2% body weight) 60% for functional & 40% for neuronal integrity • GLUCOSE 4. 5 ml/100 g/min (substrate for mature brain) 95% Aerobic produces efficient energy & 5% Anaerobic produces lactate and inefficient energy • LACTATE 0. 56 ml/100 g/min • ATP 9 umol/g/min

CEREBRAL METABOLIC RATE (CMR) • • CMR (CBF / Arterio-venous difference) O 2 3. 3 m. L/100 g/min • Glucose 4. 5 m. L/100 g/min • • Lactate 0. 56 m. L/100 g/min ATP 9 umol/g/min Oxygen requirements: 60% Functional 40% integrity Glucose, substrate for mature brain 95% Aerobic à efficient energy 5% Anaerobic Lactate à Lactate + inefficient energy • Energy stores are SCANT • • ATP + ½ ADP Energy Charge --------- Normal 0. 87 -0. 96 ATP + ADP + AMP Inadequate O 2 Delivery à â O 2 – Glucose Index á Lactate –glucose Index Phosphocreatine â Global CMRO 2 relatively stable (but varies with age) No CMRO 2 with Pa. CO 2 20 -80 mm. Hg Coupling Maintenance CBF: CMRO 2 Ratio (14 -18 normocapnia) Regional á Activated areas and âunstimulated areas

CNS HYPOTHERMIA • Hypothermia ↓neuronal metabolism and cellular hemeostasis • CO 2 reactivity is maintained during moderate and deep hypothermia • CBF: CMR coupling is maintained during moderate hypothermia • Hypothermia causes relative p. H alkalinity & ↓blood gas solubility • Brain cooling occurs faster during hypercarbia • Prolonged hypothermia is determintal: metabolic acidosis, ↑SVR↓COP, arrythemiacoagulopathy, infection, shivering, irreversible shock in rewarming • Prolonged drug effects by hypothermia

HYPOTHERMIC BRAIN • Q 10= ratio of two metabolic rates separated by 10ºC. A ration of 2 means that a 10ºC decrease in temp. result in a 50% decrease in metabolism (animal=2 -3, human>2). It is non-expotential: Q 10 of 28ºC-18ºC doubled (isolectric EEG) • Tolerance to ischemia: 37ºC→ 5 min 28ºC→ 12 min (2. 4/5) 18ºC→ 60 min(5/12) 12ºC-15ºC→>60 min * Hypothermia 30ºC+hypoxia→↓rate of energy depletion (1/2 normothermic with unchanged energy stores

HYPOTHERMIC BRAIN • OXYGEN CONSUMPTION & HYPOTHERMIA 30ºC-28ºC→↓ 50% O 2 consumption 25ºC→ ↓ 75% 20ºC→ ↓ 85% 18ºC-15ºC→↓ 90% • Hyperthermia 37ºC-42ºC→↑CBF >42ºC→ ↑CBF (toxic) • EEG & HYPOTHERMIA 37ºC-27ºC→↓EEG frequency (5. 7% per 1ºC) ↑amplitude 27ºC-23ºC→ Burst Suppression <21ºC → Isolectric • EVOKED POTENTIAL & HYPOTHERMIA 35ºC-23ºC→ progressive ↑ latency <20ºC-23ºC→potential loss


CEREBRAL TEMPERATURE • SITE BRAIN- TYMPANIC- NASOPHARYNGEAL (32ºC-34ºC) • METHODS OF COOLING ROOM BLANKETS INTRAVENOUS FLUID IRRIGATION OF CENTRAL CAVITY

CEREBRAL DYNAMICS • CVR=CPP/CBF • CPP=MAP-ICP • A-VO 2=ARTERIO-VENOUS (JUGLAR BULB OR SAGITTAL SINUS OXYGEN CONTENT DIFFERENCE • CMRO 2=CBF/A-VO 2

(MAP-ICP) CBF= CVR

FACTORS AFFECTING CBF: AUTOREGULATION • • AUTOREGULATION: MYOGENIC INTRINSIC CAPACITY TO MIANTAIN CBF CONSTANT OVER A WIDE RANGE OF CPP (PRODUCT OF CVR AND BP=50 -150 mm. Hg in normotensive patients under normal physiologic condition IMPAIRED IN PATHOLOGICAL CONDITIONS e. g. brain tumors, trauma, hemorrhage, metabolic, infection, encephalopathy, ischemia, hypoxia, pharmacological HYPERTENSION: normal autoregulation if BP controlled, Subacute increase cause slight shift to the right, chronically untreated causes complete shift to the right. Vascular changes occur 1 -2 months and tolerance to high BP and higher ischemic threshold. Malignant hypertension may lead to acute hypertensive encephalopathy. Drug-induced hypotension lower the ischemic threshold & hypovolemic hypotension elevates the ischemic threshold

FACTORS AFFECTING CBF • METABOLIC (CMR) Coupling with CMR status e. g. sleep decrease CMR and CBF & seizure, motor activity and intellectual exercises elevate CMR and CBF • NEUROGENIC: Sympathetic elevate CBF 10 -15% & parasympathetic depresses CBF. • CO 2(MOST POTENT): Mediated through hydrogen ion in the extracellular fluid of the vascular smooth muscle. Hyperventilation decreases CO 2 via vasoconstriction(Pa. CO 2 20 mm. Hg halve CBF) & CO 2 retention increases CBF (double CO 2 doubles CBF) via vasodilation


FACTORS AFFECTING CBF • O 2: hyperoxia >300 mm. Hg decreases CBF & hypoxia <5060 mm. Hg increases CBF (doubles at Pa. O 2 30 mm. Hg via arteriolar dilation) 1 Atmospheric O 2 decrease 10 -15% CBF, hyperbaric O 2 decreases CBF • TEMPERATURE: Hypothermia reduces CBF For each 1◦C decrease CMRO 2 decrease 7% • CEREBRAL DYNAMICS (CPP, CVR, CBV): Cardiac output improves CBF • RHEOLOGIC FACTORS: VISCOSITY IS DETERMINED PRIMARILY BY HCT 33 -45% normal CBF, Anemia increases CBF and decrease CVR, Polycythemia increases CVR and decreases CBF. Optimal O 2 delivery at HCT 30 -34% • PHARMACOLOGY: Dose-related anesthetic or drug effects can alter vasoactive response just as BP & CO 2

VOLATILE INHALED ANESTHETIC EFFECTS ON BRAIN METABOLISM • HALOTHANE, ISOFLURANE, SEVOFLURANE AND DESFLURANE ↓CMRO 2 , ↓CSF PRODUCTION, AND DO NOT ABOLISH CEREBROVASCULAR RESPONISEVENESS TO CO 2. HALOTHANE LACK BURST SUPPRESSION • NEUROPROTECTION FOCAL AND INCOMPLETE GLOBAL ISCHEMIA • ↑CBF HALOTHANE>ISO-SEVO OR DESFLURANE • In normocapnic, 0. 6 MAC cerebral vasodilatation • Biphasic dose dependent effect on CBF: At 0. 5 MAC ↓CMRO 2 counteracts the vasodilatation with no changes on CBF. At >1 MAC→vasodilatation→↑CBF

VOLATILE ANESTHETICS & BRAIN • VOLATILE ANESTHETICS ↑ICP AT DOSES >1 MAC AND AUTOREGULATION IS IMPAIRED • ISOFLURANE, DESFLURANE & SEVOFLURANE PRODUCE BURST SUPPRESSION ON EEG AT 1. 5 -2 MAC. ENFLURANE AND SEVOFLURANE PRODUCE EPILEPTOFORM ACTIVITY. • VOLATILE AGENTS PRODUCE LATENCY DELAY AND AMPLITUDE DEPRESSION ON SSEP ARE DOSE-DEPENDENT (0. 2 -0. 5 MAC

NITROUS OXIDE AND BRAIN METABOLISM • N 2 O →↑CMRO 2 - ↑CBF (Cerebral vasodilation)- ↑ICP. Coadministration of opoids, barbiturate, or propofol • NEUROLOGIC DEFICITS IN B 12 DEFICIENT PATIENTS • HYPERHOMOCYSTEINEMIA ASSOCIATED WITH DEMENTIA AND CEREBROVASCULAR DISEASE • NEURODEGENERATION IN NEONATES • SURGICAL WOUND INFECTION • NAUSEA AND VOMITING • INCREASE PRESSURE IN AIR CONTAINING CLOSED SPACES • REGARDLESS, IT IS USED DAILY WITH NO OBVIOUS ILL EFFECT. NO WELL DOCUMENTED DETRIMENTAL OR BENEFICIAL IMPACT ON NEUROLOGIC OR NEUROPSYCHOLOGICAL OUTCOMES.

INTRAVENOUS BARBITURATES & BRAIN METABOLISM • • • BARBITURATES, IDEAL NEUROANESTHETIC FOR YEARS Dose-dependent CNS depression, potent vasoconstrictor and ↓CBF, ↓CMRO 2, ↓ CBV & ↓ICP MAXIMUM ↓ICP & ↓CMRO 2 ACHIEVED WITH BURST SUPPRESSION EEG. Suppression of seizures Membrane stabilizer and free radical scavenger Cerebral edema, CSF secretion NEUROPROTECTION FOR FOCAL (stroke, surgical retraction, temporary clipping) but not for global (cardiac arrest) ischemia. Long acting and strong hemodynamic suppressant METHOHEXITONE activates epileptic foci and used for electroconvulsive therapy. MAJOR CARDIOVASCULAR AND RESPIRATORY DEPRESSANT ESPECIALLY IN HIGH ANESTHETIC DOSES.

INTRAVENOUS ETOMIDATE & BRAIN METABOLISM • NON-BARBITURATE CARBOXYLATED IMIDAZOLE • POTENT CEREBRAL VASOCONSTRICTOR, ↓CBF, ↓CBV, ↓CMRO 2 &↓ICP • PRESERVE CO 2 REACTIVITY • FAVORABLE CBF REDISTRIBUTION • MEMBRANE STABLIZER • SHORT DURATION OF ACTION • HEMODYNAMIC STABILITY • NEUROPROTECTIVE (BURST SUPPRESSION EEG), BUT DATA IS LACKING • EXCITATORY SPIKES ON EEG • MYOCLONIC MOVEMENT AND TWITCHING 50% OF PATIENTS WITH SEIZURE LIKE ACTIVITY ON EEG • ADRENOCORTICAL SUPPRESSION

INTRAVENOUS BENZODIAZEPINES & BRAIN METABOLISM • BENZODIAZEPINES ↓CMRO 2, ↓CBF (25%-34%) • CEILING EFFECT IN CMRO 2 BY NO BURST SUPPRESSION EEG • NO DEMONSTRABLE EFFECT IN ICP • PRESERVE VASOREACTIVITY • NO DEMONSTRABLE NEUROPROTECTIVE EFFECT • POTENT ANTICONVULSANT EFFECT

INTRAVENOUS OPIODS AND LIDOCAINE AND BRAIN METABOLISM • INTRAVENOUS OPIODS: PRODUCE MINIMAL CHANGES IN CMRO 2 & CBF • INTRAVENOUS LIDOCAINE ↓CBF & ↓CMRO 2 • BRAIN AUTOREGULATION IS PRESERVED

INTRAVENOUS DEXMEDETOMIDINE & BRAIN METABOLISM • SELECTIVE ALPHA 2 ADRENERGIC AGONIST, ↓CBF WITH SIGNIFICANT CHANGES ON CMRO 2 OR ICP • TOLERANCE AND DEPENDANCE

INTRAVENOUS KETAMINE & BRAIN METABOLISM • KETAMINE, DISSOCIATIVE ANESTHETIC • CEREBRAL VASODILATOR, ↑CMRO 2, CBF, CBV, ICP • NORMOCAPNIA BLUNTS CBF EFFECTS • PRODUCES MYCLONIC MOVEMENT BUT IT IS ANTICONVULSANT

MUSCLE RELAXANTS AND BRAIN METABOLISM • SUCCINYLCHOLINE PRODUCES TRANSIENT ICP AND CAN BE ATTENUATED BY BARBITURATES OR DEFASCICULATING DOSE OF A NONDEPOLARIZING MUSCLE RELAXANT • OTHER MUSCLE RELAXANTS HAVE NO EFFECT

CEREBRAL PERFUSIONRESERVE-STEAL • HYPERPERFUSION AND CIRCULATORY REAKTHROUGH: if CPP exceeds upper limit of autoregulation may lead to arteriolar dilatation and fall in resistance and may result in brain swelling and hemorrhage e. g. postoperative brain swelling and ICH after AVM resection (normal pressure perfusion breakthrough) • HYPOPERFUSION: may lead to ischemia. CBV increases as arterioles dilates until is exhausted and CBF decline passively as CPP decreases. Oxygen extraction increase to maximum as CMRO 2 declines. Synaptic transmission and neuronal function shuts down and energy is barely enough for neuronal survival. Then membrane failure (Na, Ca, H 2 O enter cell and K exit and cytotoxic edema takes place. At such low CBF, irreversible injury and infarction takes place and can not be corrected. Penumbra (almost shadow) area around the infarcted portion that is salvageable if flow restored soon

HYPERPERFUSION • HYPERTENSION AND ↑COP →↑CBF • INDICATIONS: Dysautoregulated ischemic region CBF pressure dependent SAH-induced vasospasm, focal ischemia • METHODS IONOTROPES INCREASE CARDIAC OUTPUT VOLUME EXPANDERS (HYPERVOLEMIA) • Deleterious if used post-injury (HTN-hemorrhage

NEUROPROTECTION RAMSIS F. GHALY, MD, FACS

NEUROPROTECTION • INCREASE TOLERANCE OF NEURAL TISSUE TO ISCHEMIA • IMPROVED OUTCOME AS EVIDENCED BY ELECTROPHYSIOLOGIC, METABOLIC, OR HISTOLOGIC INDICES OF RECOVERY OR ULTIMATELY BY IMPROVED CLINICAL NEUROLOGIC RECOVERY • PROTECTION CAN BE ACHIEVED BY PRETREATMENT (in anticipation of ischemia), DURING or AFTER ISCHEMIA • MAXIMUM COUPLED SUPPRESSION OF CMRO 2 & CBF WITH CEILING EFFECT ONCE BURST SUPPRESSION EEG • FOCAL ISCHEMIA PROTECTION ACHIEVED BY OPTIMIZING SUBSTRATE/DEMAND RATIO • GLOBAL ISCHEMIA, NO PROTECTIVE MEASURES IS LIMITED AND AIMED AT SECONDARY PROCESSES (EDEMA, HYPOPERFUSION, MEMBRANE DAMAGE.

NEUROPROTECTION • NEUROPROTECTION IS SEEN WITH AGENTS INDUCE CMR DEPRESSION, GABA AGONISM, ADENOSINE A 1 RECEPTOR AGONISM, NMDA RECEPTOR ANTAGONISM. For example protective effect of isoflurane (GABA receptor Agonist was reversed by trimethaphan (GABA receptor antagonist) • Isolflurane protective effect dose-dependent <1. 5 MAC and above 0. 5 MAC • Neuroprotective effects being stipulated for Desflurane via CMR depression and enhanced cerebral perfusion, Propofol via mitochondrial swelling and morphine via protien kinase C and NMDA receptors. • Ischemic models examined were for focal cerebral ischemia

TEMPORARY FOCAL ISCHEMIA ANTICIPATED TEMPORAY CLIPPING: MAINTAIN BURST SUPPRESSION DURING ISCHEMIC PERIOD THIOPENTAL 3 -5 mg/kg (5 min) 10 -15 mg/kg (10 min) then 35 mg/kg/hr

CSF REGULATION • • CSF (Vf)is formed at a rate 0. 4 ml/min (500 -600 cc/day) Total CSF volume is replaced 4 times/day. 60 -70% formed actively at the choroid plexus and 30% at extrachoroidal sites across ependyma and pia. CSF reabsorption (Va) via arachnoid villi and granulations. EQUILIBRIUM: Vf balance with Va /ICP. Vf relatively constant. ICP<7 cm. H 2 O minimal Va, ICP>7 cm. H 2 O linear ↑Va. Vf↓ when CPP<70 mm. Hg NEURAL: Choroid plexus richly supplied by adrenergic, cholinergic and peptidergic affecting CSF rate formation. TEMPERATURE: hypothermia ↓ CSF formation (1 C→ 11%) CO 2: Hypocarbia ↓CSF transiently METABOLIC ALKALOSIS: ↓CSF formation OSMOLARITY: ↓CSF formation →↓CPP

PHARMACOLOGICAL ALTERATIONS OF CSF DYNAMICS • N 2 O has no effect • ISOFLURANE: ↓Ra and no change to Vf • ENFLURANE transiently ↑Vf 80% and Ra(resistance to reabsorption) • HALOTHANE ↓Vf and ↑Ra • KETAMINE: ↑Ra no change Vf • ETOMIDATE and BARBITURATE (HIGH DOSE) ↓Vf and Ra • OPOID↓Ra • BENZODIAZEPINE↓Vf, ↑Ra • DIURETICS ↓Vf. Acetazolamide reduces by 50% (carbonic anhydrase inhibitor)

INTRACRANIAL PRESSURE • ICP is determined by the raltionship of the volume of intracranial contents(brain+blood+CSF=12001500 cm 3) and the volume of the cranial vault (fixed by rigid dura and skull bone). • ELASTANCE is the relationship of pressure and volume (d. P/d. V). In normal condition a small increase in intracranial volume will not result in ↑ICP. • COMPLIANCE is the relationship of volume and pressure (d. V/d. P) i. e. inverse of Elastance. • Initially, as intracranial volume increases, no change in ICP occurs (point A, well compensated) until point B where any further increase will cause dramatic increase in ICP (point C).


INTRACRANIAL PRESSURE • CPP=MAP-ICP (zero point at foramen of Monro) • Normal ICP <10 -14 mm. Hg during no stimulation • INTRACRANIAL CONTENTS AND CRANIAL VAULT VOLUME: brain matter and intracellular water (13501450 g) 80 -85%. Cerebral blood volume (CBV) 3 -7 ml/100 g 3 -6%. Cerebrospinal fluid (450 cc/day) 5 -15%. CBV: CBF homogenous changes but not always and inhomogenous in pathological condition. • VPR Pressure change per 1 ml fluid injection (0. 7% total CSF) Normal <2 mm. Hg (plateau). Pathological >4 -5 mm. Hg (↑ steepness small segment) • VPI (index)=P/V-(log. Pp/P 0). Volume addition required to change ICP by 10 folds (normal 25 ml poor<15 ml). Surgical intervention before steep portion of VP curve.

ANESTHETIC INDUCTION IN NEUROANESTHESIA: GOALS • Deep anesthetic level with adequate muscle relaxation and blunting response to intubation, pins and craniotomy • No increase ICP, CBV, BP and No decrease in CPP, CBF, BP • No hypoxia • No coughing

ANESTHETIC INDUCTION IN NEUROANESTHESIA • Thiopental (3 -7 mg/kg, Propofol 22. 5 mg/kg, Midazolam 0. 2 -0. 4 mg/kg, Etomidate 0. 2 -0. 4 mg/kg, Fentanyl 510 ug/kg, Lidocaine 1. 5 mg/kg prior to intubation (Lidocaine oral and laryngeal spray) • Adquate airway ventilation • Non-depolarizing muscle relaxant intubating dose or succinylecholine 1. 5 mg/kg after defasciculating dose of non-depolarizer

ANESTHETIC INDUCTION IN NEUROANESTHESIA • • • Thoroughly securing the Airway Eye protection watertight Adequate positioning and padding Avoid head down position Avoid pressure over the neck or tight tape around • Keep access to the patient and lines • Recheck tubes and lines after positioning • Lidocaine at the Pin sites before head pins placement

ASA TASK FORCE IN POSITIONING 2000 • ASA TASK FORCE ON PREVENTION OF PERIOPERATIVE PERIPHERAL NEUROPATHIES; PRACTICE ADVISORY IN POSITIONING 2000. • LIMIT ARM ABDUCTION TO 90 AND CAREFUL PADDING OF VULNERABLE PRESSURE POINTS • CAREFFULL PAD AND ASSESS AREAS SENSITIVE TO PRESSURE NECROSIS e. g. EYES, EARS, NOSE, GENITALIA AND BREASTS. FEMALE BREASTS DISPLACED MEDIAL AND INFERIOR IN RELATION TO CHEST SUPPORTS • PATIENTS WHO HAVE POSITION-DEPENDENT NEUROLOGIC SYMPTOMS OR EXTREMELY OBESE BENEFIT FROM AWAKE INTUBATION FOLLOWED BY AWAKE POSITIONING

PROBLEMS RELATED TO PRONE POSITION • • BRACHIAL PLEXUS INJURY AIR EMBOLI AND CV COLLAPSE BLINDNESS OBSTRUCTION OF FEMORAL VEINS AND IVC→↓VR→↓CVP AND ↓COP • ENGORGEMENT OF PERIVERTEBRAL VENOUS PLEXUSES→DIFFICULT SURGICAL EXPOSURE AND ↑BLOOD LOSS • ABDOMEN HANG FREE→NEGATIVE PRESSURE WITHIN IVC→ PERIVERTEBRAL VENOUS PLEXUSES-→ AIR EMBOLIZATION • FROM SUPINE TO PRONE→↓SV AND↓ CI AND↑ PVR AND ↑SVR. LEAST CHANGES WITH JACKSON SPINE AND LONGITUDINAL BOLSTERS. CARDIAC PATIENTS MAY NOT TOLERATE AND SWAN-GANZ CATHETER MAY BE NEEDED

ROBLEMS RELATED TO PRONE POSITION • CABG PATIENTS MAY OCCLUDE BYPASS GRAFTS • ABDOMINAL PRESSURE → DISPLACE DIAPHRAGM→ REDUCE LUNG COMPLIANCE→ POSITIVE PRESSURE VENTILATION→BAROTRAUMA. • POSITIVE INSPIRATORY EFFECT ON DIAPHRAGM-→ INCREASE FRC AND DESRIABLE EFFECT ON GAS EXCHANGE • VISUAL LOSS 1: 100 SPINE SURGERIES DUE TO ISCHEMIC OPTIC NEUROPATHY (↑FLUID, ↑BLOOD LOSS, ↑IOP , ↓PERFUSION PRESSURE) • FACIAL EDEMA

PERIPHERAL NERVE INJURY • • • IMPROPER INTRAOPERATIVE POSITIONINGT REGIONAL ANESTHETIC TECHNIQUES INJECTION SITES DIRECT SURGICAL RETRACTION OR DAMAGE RISK FACTORS: BODY HABITUS, PREVIOUS H/O NEUROPATHY, SMOKING, DIABETES • ULNAR NERVE INJURY 1/3 OF ASA CLOSED CLAIM ANALYSIS • BRACHIAL PLEXUS AND PERONEAL NERVE FOLLOWED

PERIPHERAL NERVE INJURY • OTHER SITES: MEDIAN AND ULNAR NERVE AT WRIST, RADIAL NERVE AT INNER ARM, VII NERVE AT EXIT SITE COMPRESSED BY MASK AIRWAY • PROLONGED OR IMPROPER LITHOTOMY SCIATIC, FEMORAL, COMMON PERONEAL, SAPHENOUS NERVES • COMPRESSION OR STRETCHING OF NERVE WITH DEMYELINATION • REMYELINATION OCCURS 6 -8 WEEKS • IMMEDIATE DIAGNOSIS, EARLY NEUROLOGY CONSULTATION AND REHABILITATION ARE CRUCIAL FOR FULL RECOVERY

NEUROANESTHETIC MAINTENANCE ADEQUATE BRAIN RELAXATION • Adequate oxygenation and ventilation (Pa. CO 2 3335 mm. Hg), , venous return, muscle relaxation, anesthetic depth • Furosmide 10 -20 mg iv, Mannitol 0. 5 -1. 5 g/kg iv, iv thiopental, CSF drainage

NEUROANESTHETIC MAINTENANCE STABLE ANESTHETIC STATE AND RAPID SMOOTH EMERGENCE • Low after the craniotomy (brain is devoid of sensation) • Isoflurane, Sevoflurane or Desflurane 0. 5 MAC & Propofol 50 -150 ug/kg/min and Remifentanil 0. 1 -0. 5 ug/kg/min • Muscle relaxant maintaining 2 twitches (phenytoin may increase requirment of muscle relaxants)

NEUROANESTHETIC EMERGENCE • AVOID COUGHING STRAINING OR BP INCREASE • Normalize gradually Pa. CO 2 • Full reversal of muscle relaxant • IV Lidocaine • IV labetolol, Nicardpine, NTP, NTG • Brief neurological Assessment before leaving OR

Pre emergence • 1 -2 hr before end • Gradual decrease anesth aiming for bis 80 at end • Treat post op htn before hand, I aim for SBP 110 • Maintain solid reversible NMB!!

IMMEDIATE POSTOPERATIVE CARE IN NEUROANESTHESIA • • • ADEQUATE VENTILATION AND OXYGENATION HEAD OF BED (10 -25 C 0 NEUROLOGIC FUNCTION CEREBRAL DYNAMICS MONITORING AND CONTROL SERUM ELECTROLYTE: SIADH (↓Na, ↓serum osm, ↑urine osmo) Treatment restrict water intake ‡meds DI (polyuria, ↑Na, ↑serum osmo, ↓urine osmo) Treatment Aqueous vasopressin 5 -10 USP units sq or 3 units iv OR desmporessin 1 -2 ug iv sq q 6 -12 hr. Plus adequate fluid replacement • SEIZURE (adequate oxygenation, ventilation and airway protection: midazolam (2 -4 mg), thiopental (100 -150 mg), fosphenytoin 15 -20 mg/kg, 100 mg/min) • POSTOPERATIVE IMAGING (CTScan, MRI, Angiography)

TRANSPORT FROM OPERATING ROOM TO NEURO-ICU OR PACU: • PRIOR COMPLETE REPORT TO ACCEPTING UNIT WITH SET-UP NEEDED • TRANSPORT ONLY WHEN PATIENT IS STABLE OR AS STABLE AS CAN BE • DIRECT SUPERVISION OF ANESTHETIST • HEMODYNAMIC AND RESPIRATORY SYSTEMS MONITORED AND CONTROLLED • O 2 SUPPLEMENT • WORKING IV AND RUNNING INFUSION PUMPS • BLANKETS AND HEAT LOSS PREVENTION • EMERGENCY MEDS AND INTUBATION KIT • ENDORSEMENT IS NOT COMPLETE UNTIL PATIENT IS STABLE AND COMPREHENSIVE REPORT HAS BEEN DELIVERED

CAUSES OF POSTANESTHETIC HYPOTENSION • • HYPOVOLEMIA ↑HR, RR, SKIN TURGOR, DRY MUCOUS MEMBRANE, OLIGURIA AND THIRST. INADEQUATE FLUID REPLACEMENT, ONGOING LOSS, OSMOTIC POLURIA, FLUID SEQUESTRATION (ASCITIS, INTESTINAL OBSTRUCTION A MEANINGFUL VOLUME CHALLENGE AND FURTHER ASSESSMENT (CAUTIOUS IN IMPAIRED BBB) IMPAIRED VENOUR RETURN JUGLAR VEIN DISTENTION, ↑CVP, ↓BREATH SOUNDS AND ↓HEART TONES. POSITIVE PRESSURE VENTILATION, PEEP, PNEUMOTHORAX, PERICARDIAL TAMPONADE. TREATED BY VOLUME AND THE CAUSE

CAUSES OF POSTANESTHETIC HYPOTENSION • VASODILATION REWARMING, RESIDUAL INHALATION AGENTS, NEUROAXIAL ANESTHESIA, TRANSFUSION REACTION, ANAPHYLAXIS, INFLAMMATION, SEPSIS, ADRENAL INSUFFICIENCY, LIVER FAILURE • DECREASED CARDIAC OUTPUT MYOCARDIAL ISCHEMIA, INFARCTION, CHF, NEGATIVE INOTROPIC DRUGS, SEPSIS, HYPOTHYRODISM, MALIGNANT HYPERTHERMIA DYSPNEA, DIAPHORESIS, CYANOSIS, JUGLAR VEIN DISTENTION, OLIGURIA, RHYTHM DISTURBANCES, WHEEZING, DEPENDENT CRACKLES, AND S 3 GALLOP INOTROPIC AGENTS (e. g. DOPAMINE) AFTERLOAD REDUCTION (e. g. Nitrate) DIURESIS for fluid overload ANTIDYSRHYTHMICS OR ELECTRICAL CARDIOVERSION

CAUSES OF POST-ANESTHETIC DYSRHYTHMIAS • • • INCREASED SYMPATHETIC OUTFLOW (PAIN) HYPOXEMIA, PE HYPERCARBIA HYPO-HYPERTHERMIA HYPOVOLEMIA ELECTROLYTE AND ACID-BASE IMBALANCE DRUG TOXICITY THYROTOXICOSIS MALIGNANT HYPERTHERMIA MYOCARDIAL ISCHEMIA, CHF ELEVATED ICP

COMMON TYPES OF POSTANESTHETIC DYSRHYTHMIAS SUPRAVENTRICULAR DYSRHYTHMIAS • SINUS TACHYCARDIA • SINUS BRADYCARDIA • PAROXYSMAL SUPRAVENTRICULAR TACHYDYSRHYTHMIAS VENTRICULAR DYSRHYTHMIAS; STABLE • PVCS • VENTRICULAR TACHYCARDIA (NON-SUSTAINED) UNSTABLE VENTRICULAR TACHYCARDIA AND VENTRICULAR FIBRILLATION

GENERAL TREATMENT OF POSTANESTHETIC DYSRHYTHMIAS • • • O 2 SUPPLEMENT INCREASE PERFUSION TREAT THE CAUSE (S) Pain: Opiods Bradycardia: Atropine 0. 2 -0. 4 mg or glycopyrrolate 0. 2 mg Synchronized cardioversion if unstable arrthymia Adenosine 6 mg then 12 mg rapid to convert PACS B-adrenergic blockers (labetalol 5 -20 mg -2 mg/min, esmolol 10100 mg or 25 -300 ug/kg/min, propranolol 0. 5 -1 mg iv) Calcium-channel blockers (Verapamil 2. 5 -5 mg increment, diltiazem 5 -20 mg iv or 0. 25 -0. 35 mg/kg iv then 5 -15 mg/hr Amiodarone 150 mg over 10 min then 1 mg/min for 6 hrs then 0. 5 mg/min Digoxin 0. 25 mg increment 1. 5 mg Ibutilide, Procainamide 20 -30 mg/min iv up 17 mg/kg 1 -2 mg/min, Lidocaine 1. 5 mg/kg then 1 -4 mg/min

PERIOPERATIVE FLUID MANAGEMENT IN NEUROANESTHESIA • Avoid infusion of water or dextrose in water (Water freely passes through BBB) • BBB is impermeable to most ions. Total osmolarity rather than oncotic pressure determine osmotic gradient. • Maintenance of high serum osmolality decrease brain water content • Large, polar substances cross poorly BBB e. g albumin • If BBB is disrupted, permeability to mannitol, albumin, and saline increases and edema formation

PERIOPERATIVE FLUID MANAGEMENT IN NEUROANESTHESIA • Physiologic mainenance fluid given hourly without replacement of overnight deficit • Third spacing is minimal during craniotomy surgery • 2/3 of total intraoperative urine output is replaced with crystalloid • Iso-osmolar crystalloid sol (0. 9 NS, 309 m. Osm. Large quantity may cause metabolic acidosis) • Hypokalemia secondary to steriod, porassiumwasting diuretics, hyperventilation. • Hyponatremia caused by SIADH and diuretic used

Brain Death • Apnea test Determination • Disconnect the ventilator • Deliver 100% FIO 2 via t-piece/trach collar • Monitor for ventilatory effort until ABG confirms a Pa. CO 2 greater than 60 mm Hg • Reconnect ventilator • If patient becomes unstable, terminate apnea test • Patient is considered apneic if Pa. CO 2 is > 60 and there is no respiratory effort

THE END THANK YOU ? QUESTIONS
 Subclinical seizures eeg
Subclinical seizures eeg Enls neurocritical care
Enls neurocritical care Lahey clinic anesthesiology residency
Lahey clinic anesthesiology residency Umass memorial pharmacy residency
Umass memorial pharmacy residency The symbol tsfa in alu operations include
The symbol tsfa in alu operations include Performance monitoring and coaching form 2021 sample
Performance monitoring and coaching form 2021 sample Levels of care primary secondary tertiary quaternary
Levels of care primary secondary tertiary quaternary Health and social care values unit 2
Health and social care values unit 2 Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Ap gov review final exam review
Ap gov review final exam review Nader amin-salehi
Nader amin-salehi Narrative review vs systematic review
Narrative review vs systematic review Narrative review vs systematic review
Narrative review vs systematic review Care first counselling
Care first counselling Chapter 3 careers in health care review questions
Chapter 3 careers in health care review questions Care certificate standard 3
Care certificate standard 3 Magnetii sunt corpurile care
Magnetii sunt corpurile care Palliative care vs hospice care
Palliative care vs hospice care Animale care fac oua
Animale care fac oua Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate Care certificate 13
Care certificate 13 Hip fracture care clinical care standard
Hip fracture care clinical care standard West yorkshire and harrogate health and care partnership
West yorkshire and harrogate health and care partnership Humber coast and vale ics map
Humber coast and vale ics map Supervision and appraisal
Supervision and appraisal Health and social component 3
Health and social component 3 Sam and verna case study
Sam and verna case study Adoption and foster care analysis and reporting system
Adoption and foster care analysis and reporting system Review adalah
Review adalah Electric forces and fields concept review
Electric forces and fields concept review Unit 11 volume and surface area homework 4
Unit 11 volume and surface area homework 4 System maintenance and review
System maintenance and review Define area in math
Define area in math Section 33-1 review porifera answer key
Section 33-1 review porifera answer key Spanish 1 semester 1 final exam answer key
Spanish 1 semester 1 final exam answer key Stringer bead in flat position
Stringer bead in flat position Language english proficiency
Language english proficiency Comic relief in romeo and juliet
Comic relief in romeo and juliet Romeo and juliet jeopardy
Romeo and juliet jeopardy Mpe and cre review
Mpe and cre review Reteaching 9-1 review percents and probability
Reteaching 9-1 review percents and probability Chapter 14 review acids and bases section 1
Chapter 14 review acids and bases section 1 Literature review introduction example
Literature review introduction example Chapter 9, section 1: labor and wages worksheet answers
Chapter 9, section 1: labor and wages worksheet answers Circuit court maps
Circuit court maps Geometry chapter 12
Geometry chapter 12 Listing domain and range
Listing domain and range Section 39-2 review jawless and cartilaginous fishes
Section 39-2 review jawless and cartilaginous fishes Chapter 4 ecosystems and communities vocabulary review
Chapter 4 ecosystems and communities vocabulary review Chapter 8 review chemical equations and reactions section 2
Chapter 8 review chemical equations and reactions section 2 Chapter 8 skin disorders and diseases review questions
Chapter 8 skin disorders and diseases review questions Chapter 8 review chemical equations and reactions
Chapter 8 review chemical equations and reactions Chapter 7 review chemical formulas and chemical compounds
Chapter 7 review chemical formulas and chemical compounds Chapter 5 pollen and spore examination review answers
Chapter 5 pollen and spore examination review answers Chapter 11 review cash control and banking activities
Chapter 11 review cash control and banking activities Chapter 1 review matter and change
Chapter 1 review matter and change Review and discuss
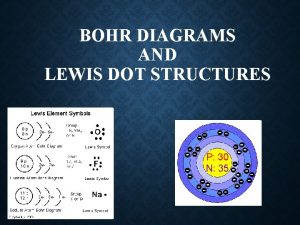
Review and discuss Review bohr and lewis dot diagrams
Review bohr and lewis dot diagrams Review exercise terms and events answer key
Review exercise terms and events answer key Amphibians images with names
Amphibians images with names