Introduction to Anesthesiology Clinic zge Kner MD Anesthesiology
- Slides: 57
Introduction to Anesthesiology Clinic Özge Köner, MD Anesthesiology Dept.
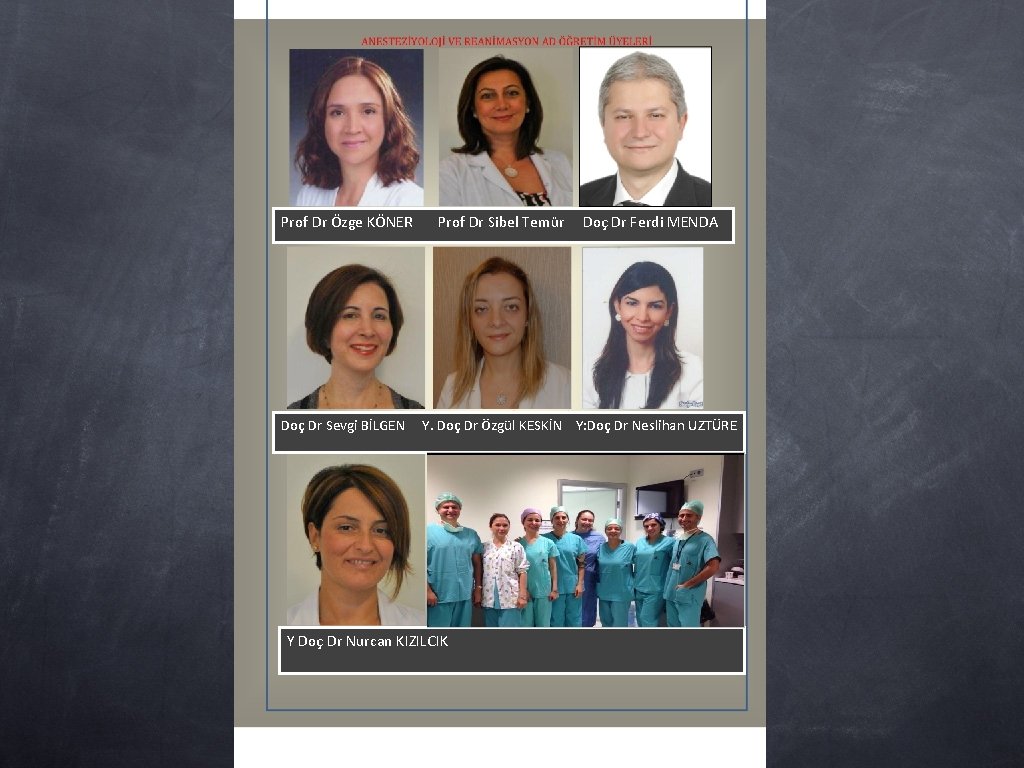
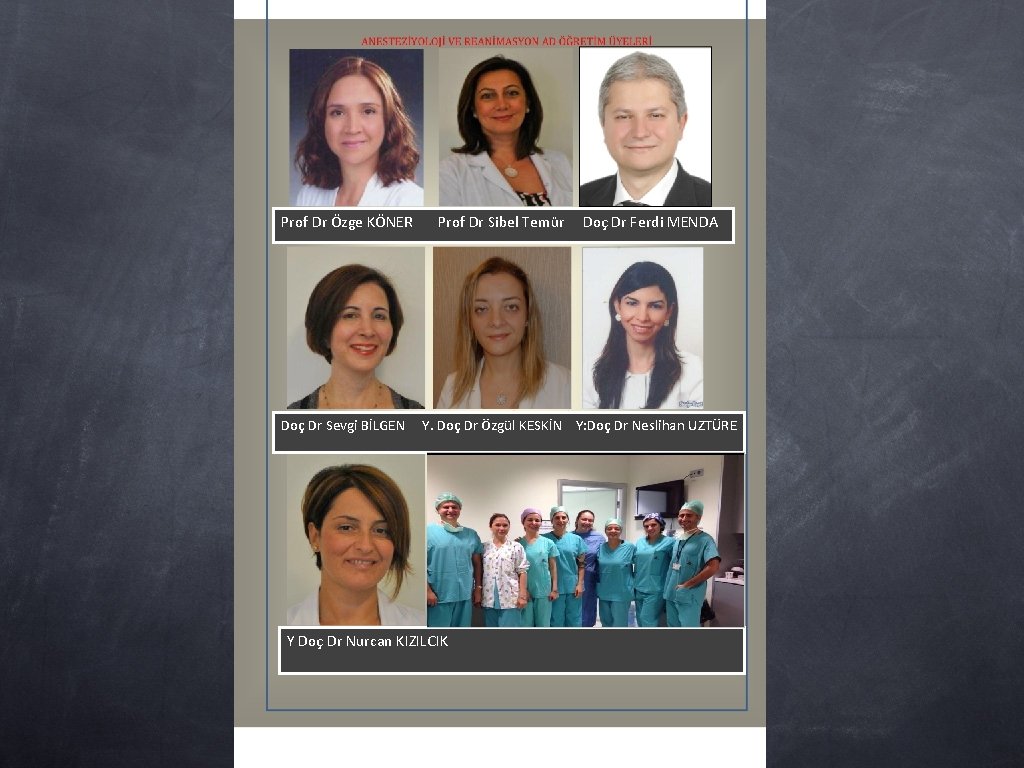
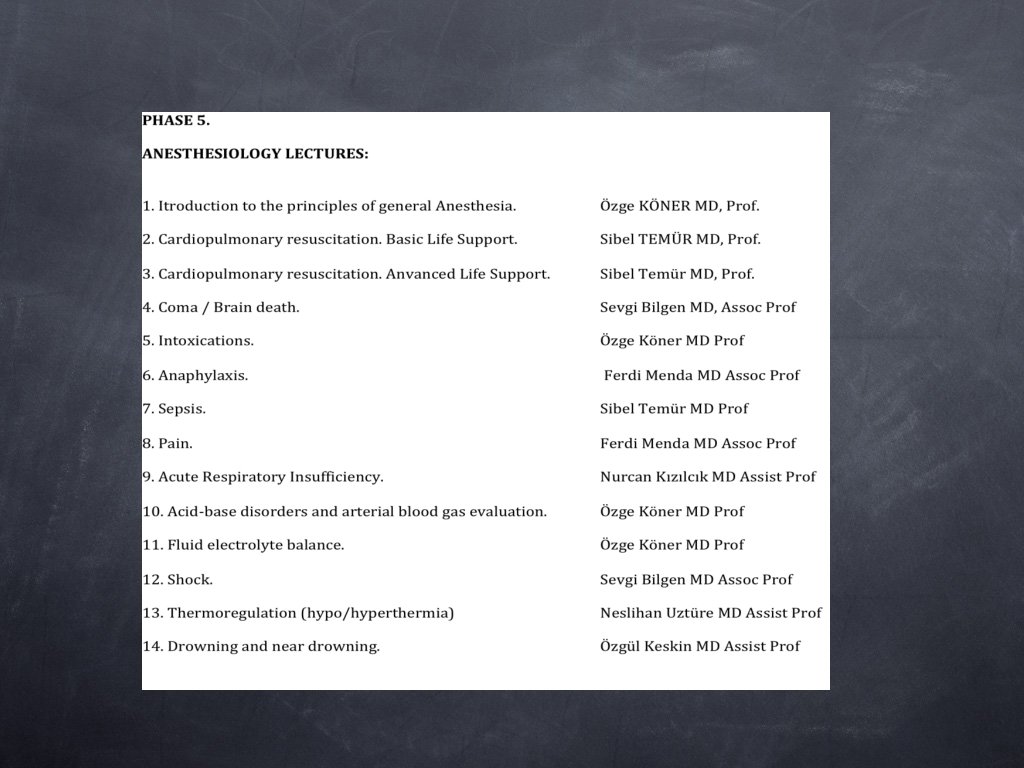
Prof Dr Özge KÖNER Doç Dr Sevgi BİLGEN Prof Dr Sibel Temür Doç Dr Ferdi MENDA Y. Doç Dr Özgül KESKİN Y: Doç Dr Neslihan UZTÜRE Y Doç Dr Nurcan KIZILCIK
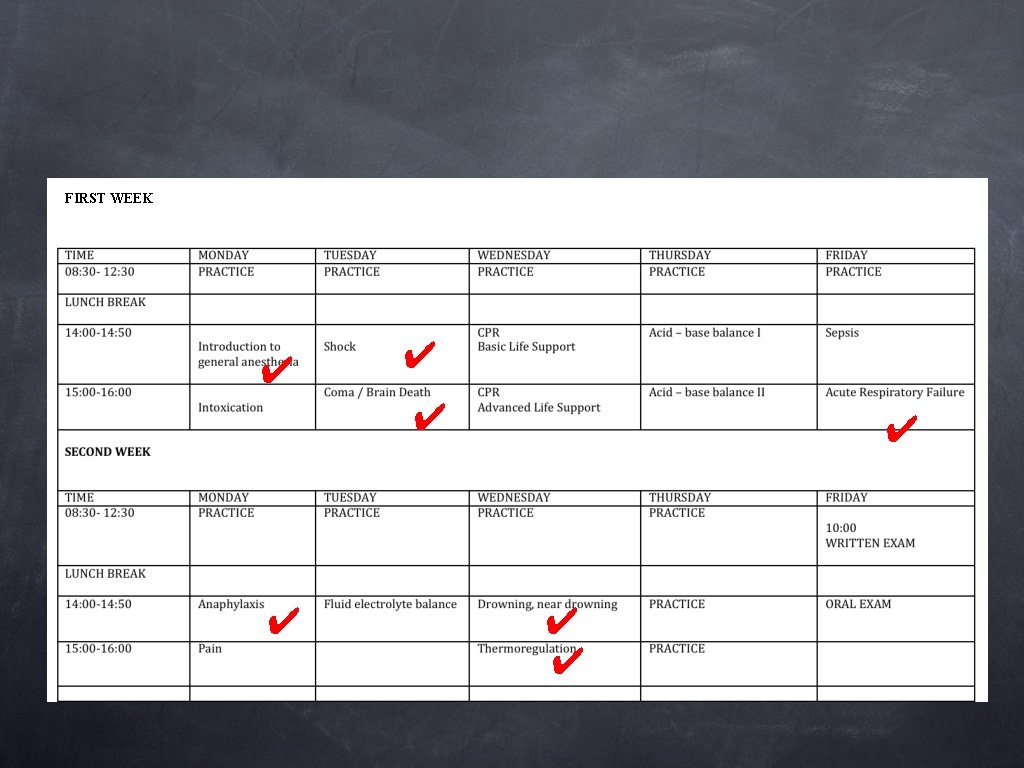
Schedule
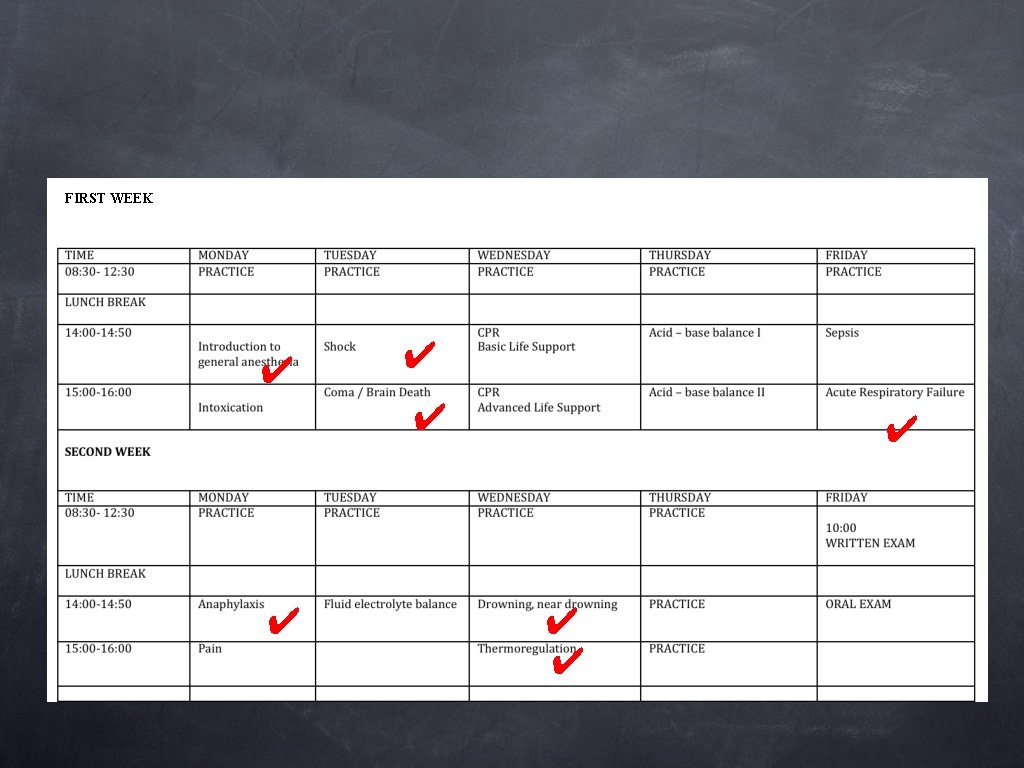
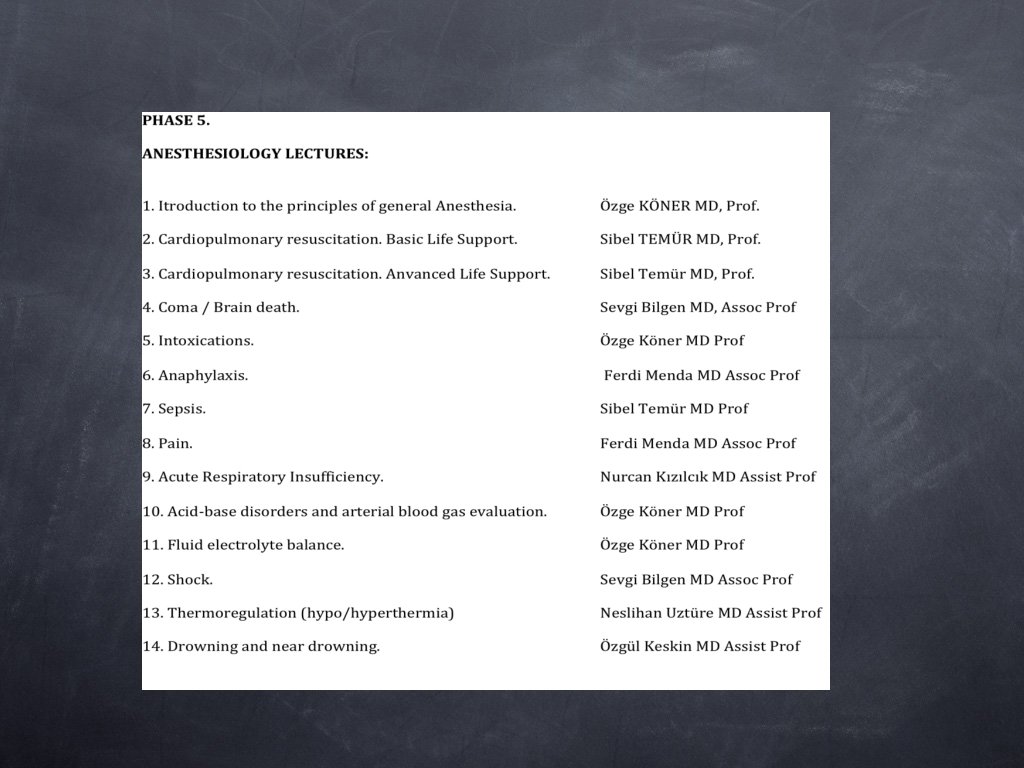
FIRST WEEK ✔ ✔ ✔ ✔
Introduction to General Anesthesia Özge Köner, MD Anesthesiology Dept.
Learning Objectives Historical Perspective Definition of General Anesthesia Theories & Mechanism of Action of General Anesthesia Anesthetic Agents (volatile & intravenous)
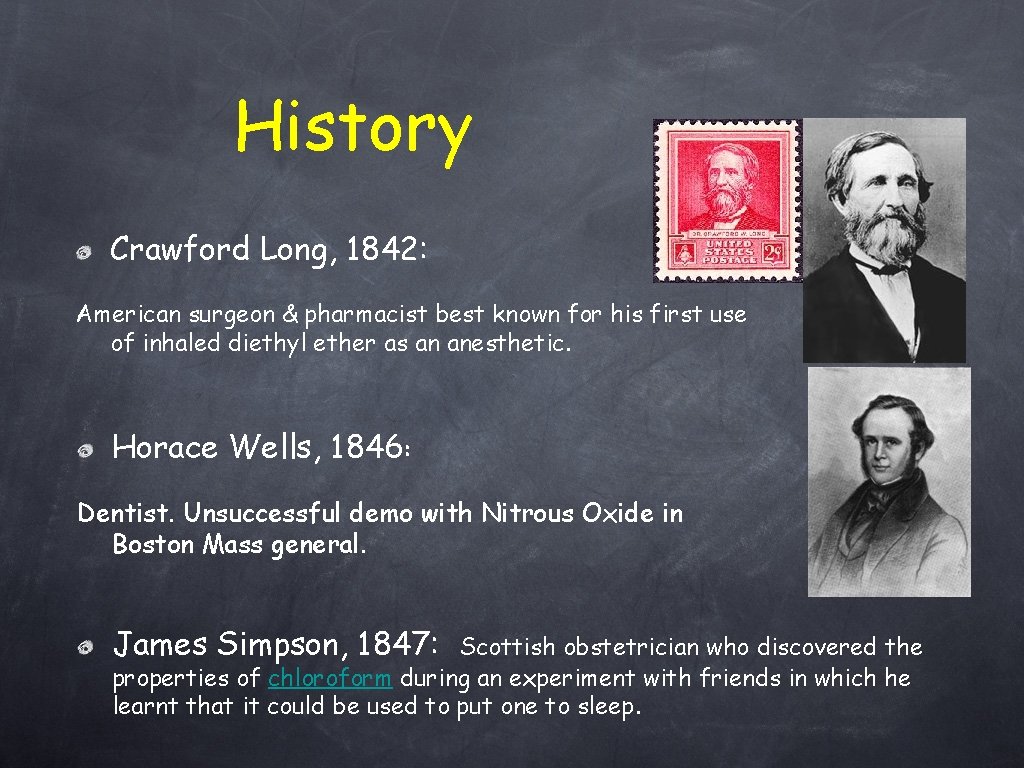
History Crawford Long, 1842: American surgeon & pharmacist best known for his first use of inhaled diethyl ether as an anesthetic. Horace Wells, 1846: Dentist. Unsuccessful demo with Nitrous Oxide in Boston Mass general. James Simpson, 1847: Scottish obstetrician who discovered the properties of chloroform during an experiment with friends in which he learnt that it could be used to put one to sleep.
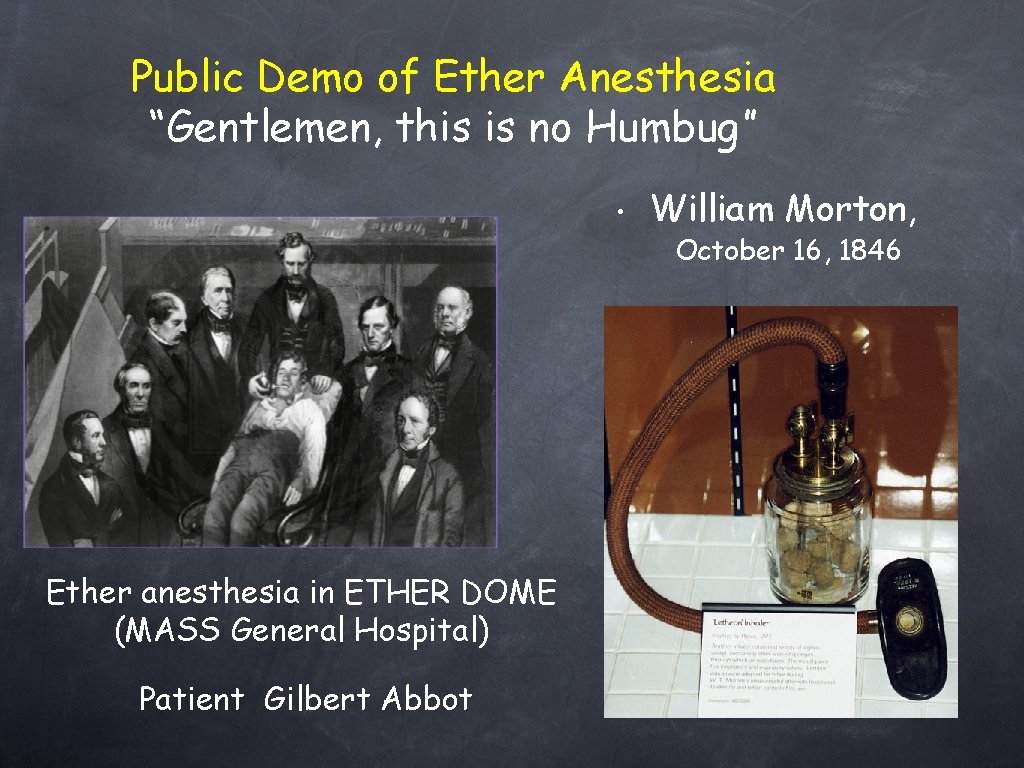
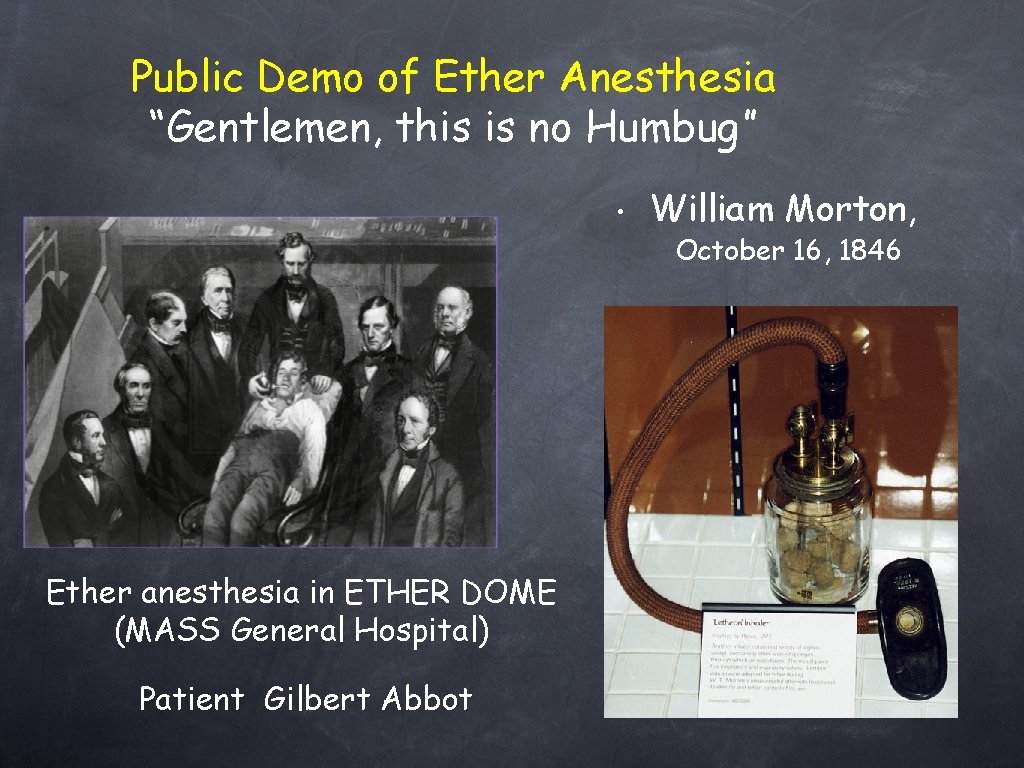
Public Demo of Ether Anesthesia “Gentlemen, this is no Humbug” • William Morton, October 16, 1846 Ether anesthesia in ETHER DOME (MASS General Hospital) Patient Gilbert Abbot
OLIVER WENDELL HOLMES, Sr (1809 -1894) “Everybody wants to have a hand in a great discovery. All I will do is to give you a hint or two as to names—or the name—to be applied to the state produced and the agent. The state should, I think, be called ‘Anaesthesia’ (from the Greek word anaisthesia, ‘lack of sensation’). This signifies insensibility. . The adjective will be ‘Anaesthetic’. Thus we might say the state of Anaesthesia, or the Anaesthetic state. ” Oliver Wendell Holmes 21 November 1846
Cyclopropane, 1929: Most widely used general anesthetic for the following 30 yrs. EXPLOSIVE ! Halothane, 1956: British Research Council & chemists at Imperial Chemical Industries. Although widely replaced with new generation volatiles, it is still in use. Methoxyflurane, 1960: Nephrotoxicity. Sevoflurane & Desflurane, late 1960 s Thiopental, intravenous anesthetic. (Still in use)
Anesthesia • Greek: an- “without” & aisthesis- “sensation”. Blocked or temporarily taken sensation (including the feeling of pain). Reversible, drug-induced loss of consciousness. Amnesia & unconsciousness Analgesia Muscle relaxation Attenuation of autonomic responses to noxious stimulation
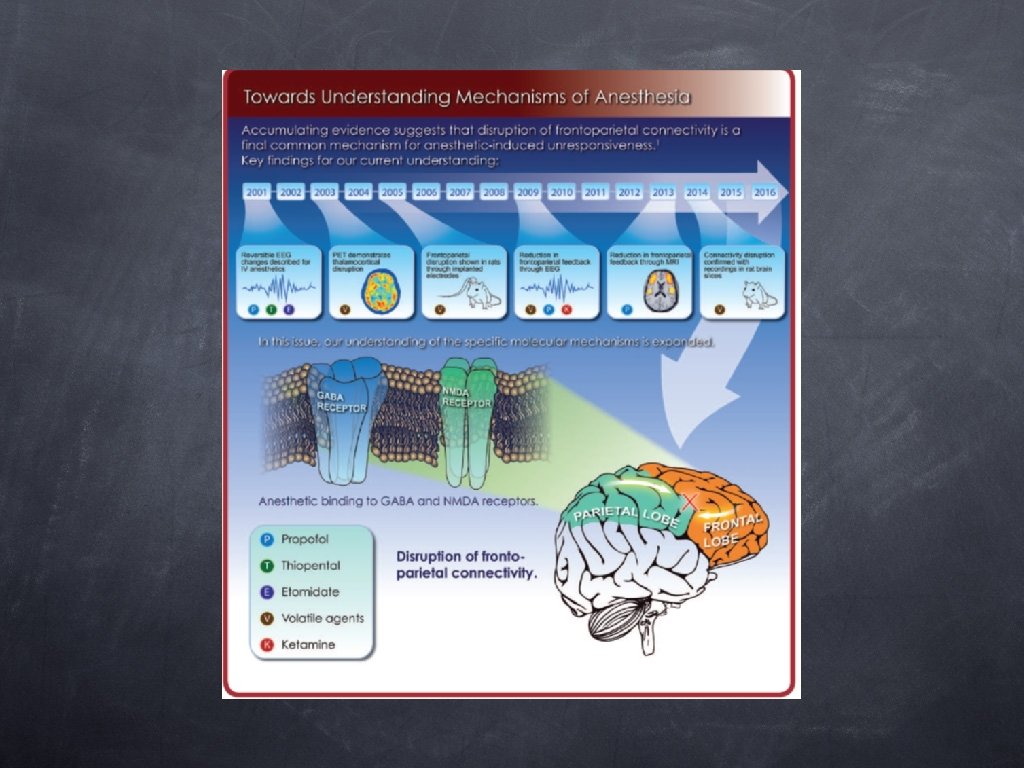
Theories of general anesthetic action 1. Lipid solubility-anesthetic potency correlation • “The Meyer-Overton correlation” Meyer HH; First experimental evidence: anesthetic potency is related to lipid solubility. A similar theory was published independently by Overton in 1901. The greater is the lipid solubility of the compound in olive oil the greater is its anesthetic potency. • • Modern interpretation of theory; general anesthetics dissolve in lipid-bilayer regions of nerve cell membranes and alter the properties of lipids surrounding crucial membrane proteins that protein function is compromised. Meyer HH: "Zur Theorie der Alkoholnarkose". 1899.
Theories of general anesthetic action Alternative idea that proteins are directly affected: 2. Membrane protein hypothesis*: • • Some class of proteins might be sensitive to general anesthetics. Inhalation agents may primarily interact with receptor proteins & produce conformational changes in their molecular structure. These changes affect the function of ion channels or enzymes. GABAA, glycine, glutamate, Ni receptors can be selectively modified by clinical concentrations of volatiles. * Franks NP. Nature, 300: 1982.
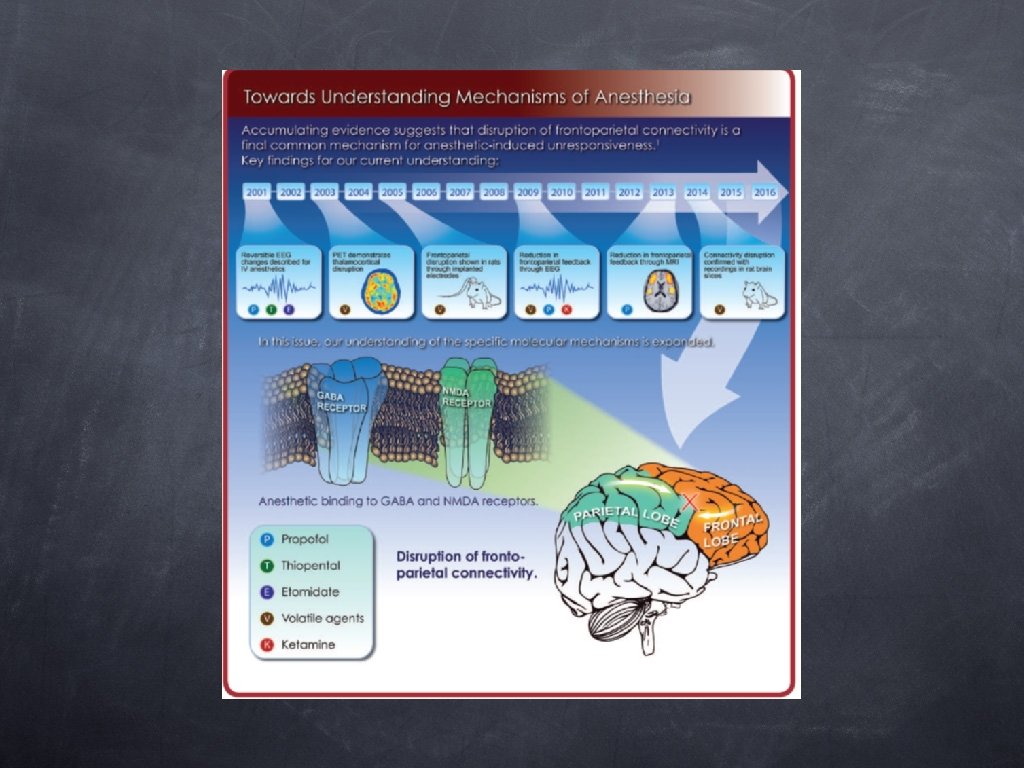
Mechanism of Anesthesia Anesthetic action on spinal cord probably inhibits purposeful responses to noxious stimulation. Inhalational agents can “depress the exitability of thalamic neurons”, “block thalamocortical communication” and the potential result is loss of consciousness. Existing evidence provides no basis for a single anatomic site responsible for anesthesia.
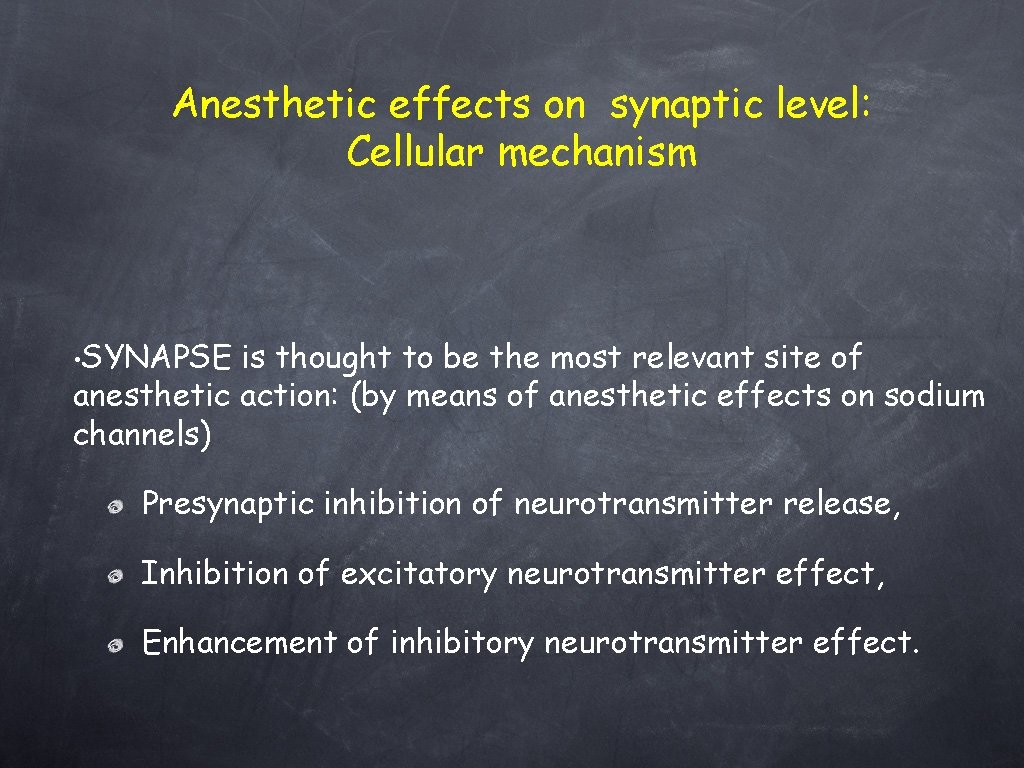
Anesthetic effects on synaptic level: Cellular mechanism • SYNAPSE is thought to be the most relevant site of anesthetic action: (by means of anesthetic effects on sodium channels) Presynaptic inhibition of neurotransmitter release, Inhibition of excitatory neurotransmitter effect, Enhancement of inhibitory neurotransmitter effect.
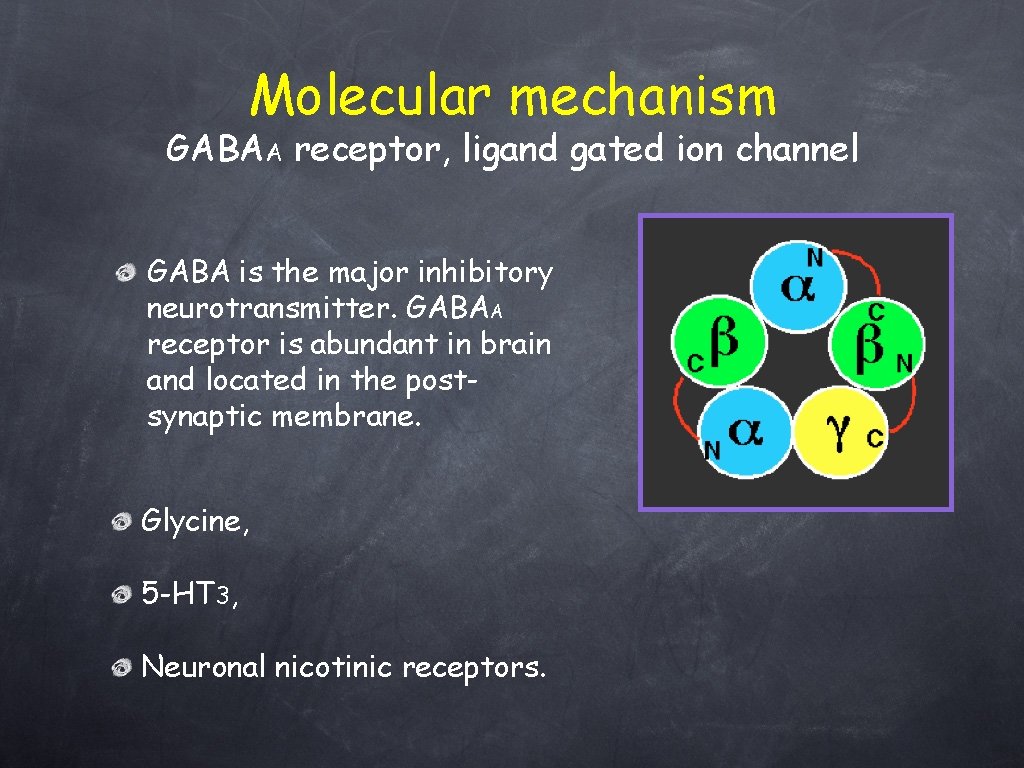
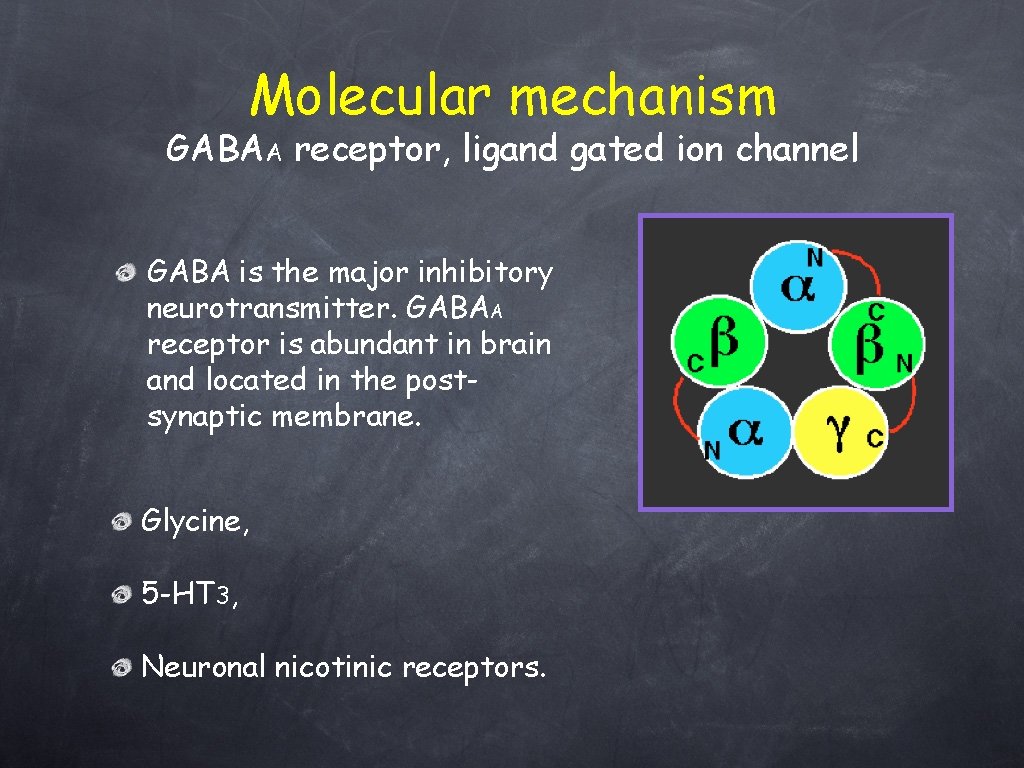
Molecular mechanism GABAA receptor, ligand gated ion channel GABA is the major inhibitory neurotransmitter. GABAA receptor is abundant in brain and located in the postsynaptic membrane. Glycine, 5 -HT 3, Neuronal nicotinic receptors.
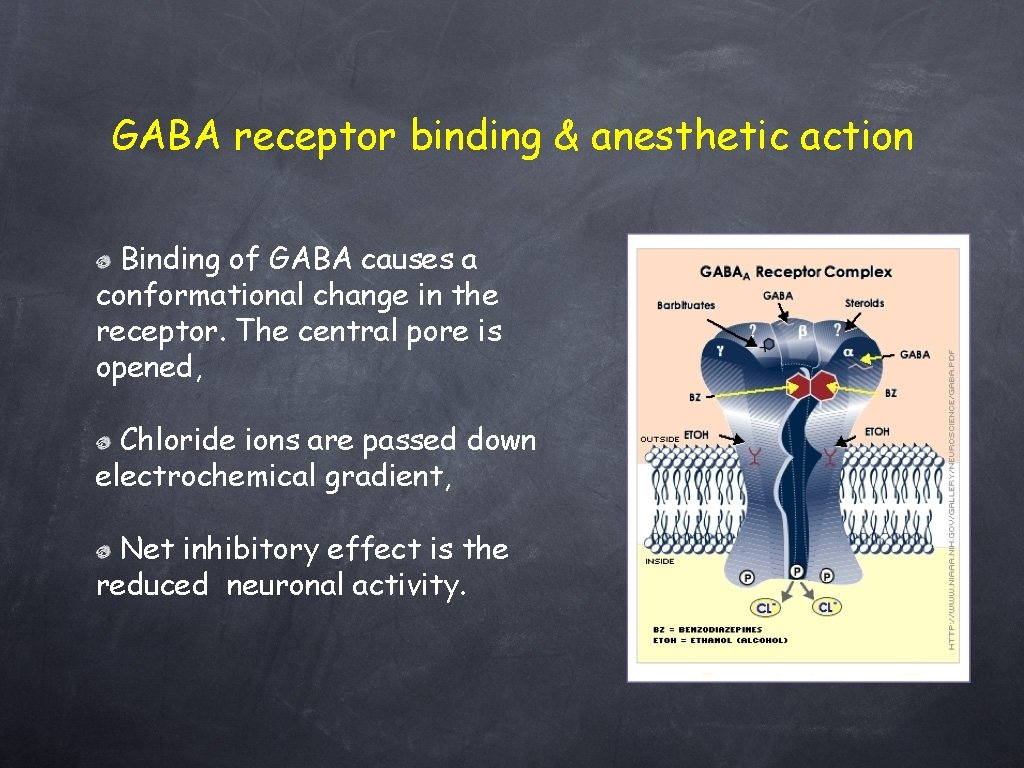
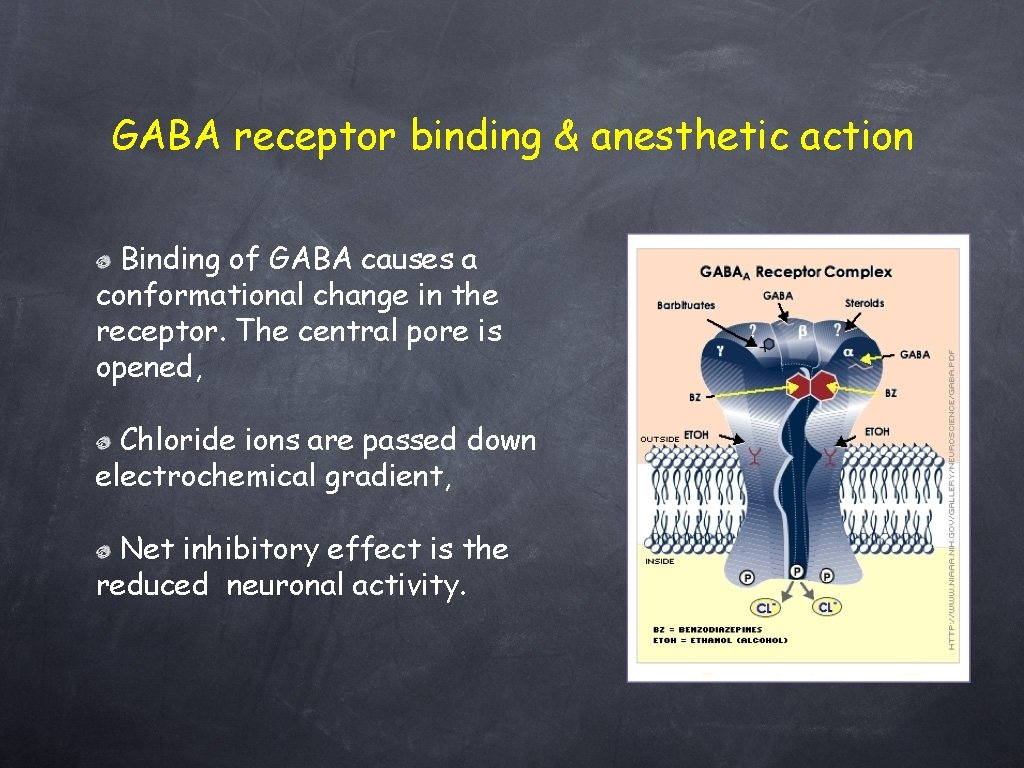
GABA receptor binding & anesthetic action Binding of GABA causes a conformational change in the receptor. The central pore is opened, Chloride ions are passed down electrochemical gradient, Net inhibitory effect is the reduced neuronal activity.
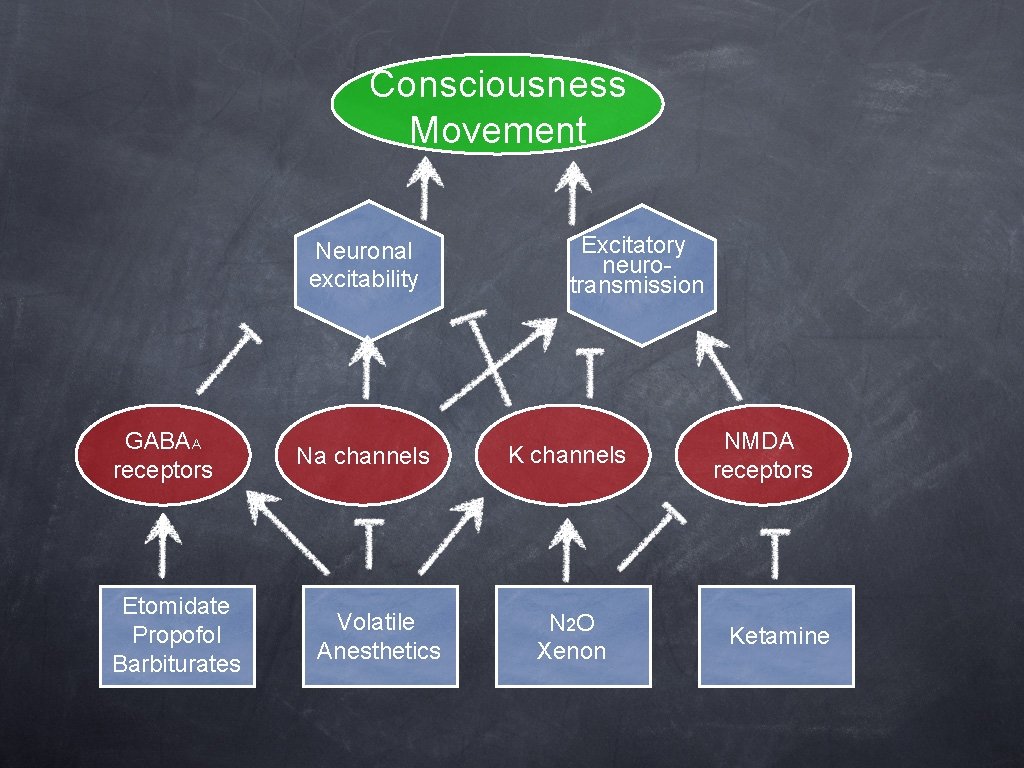
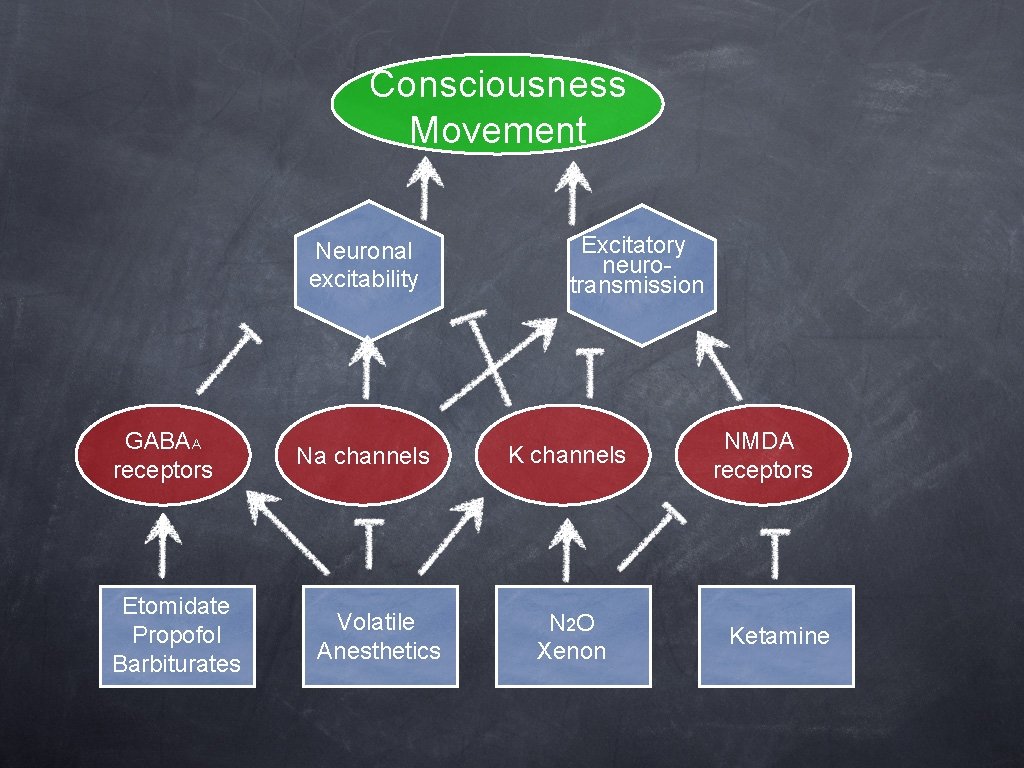
Consciousness Movement Neuronal excitability GABAA receptors Etomidate Propofol Barbiturates Na channels Volatile Anesthetics Excitatory neurotransmission K channels N 2 O Xenon NMDA receptors Ketamine
Anesthetics divide into 2 classes • Inhalation Anesthetics • • Gases or Vapors Usually Halogenated • Intravenous Anesthetics • • Injections Anesthetics or induction agents
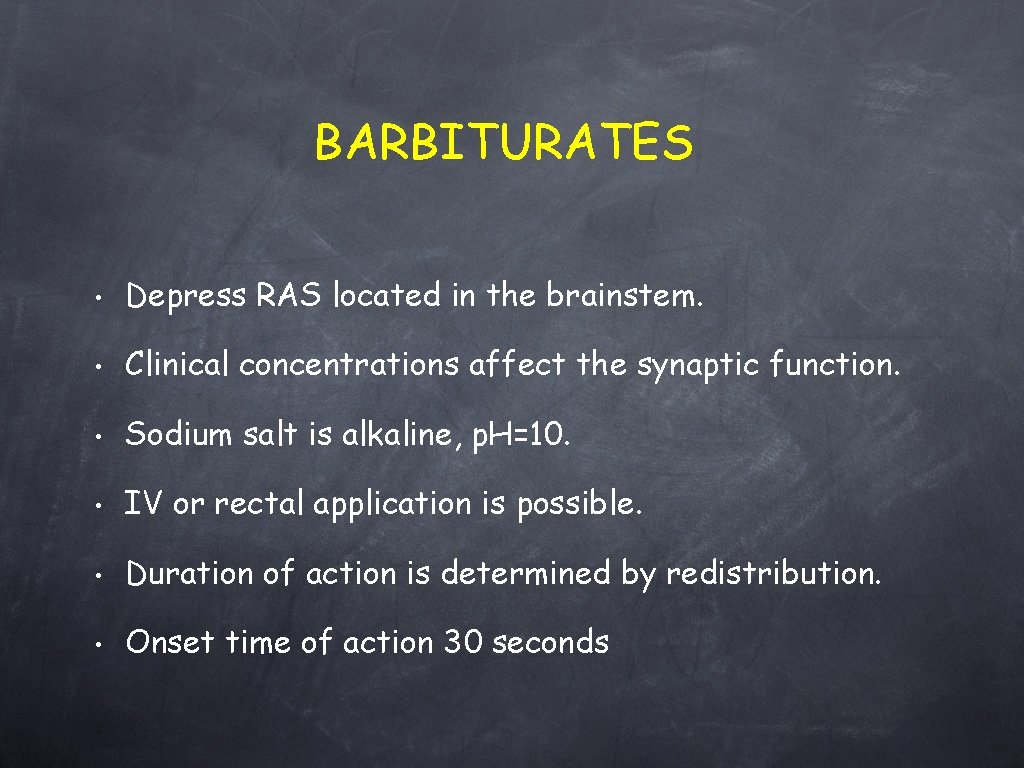
BARBITURATES • Depress RAS located in the brainstem. • Clinical concentrations affect the synaptic function. • Sodium salt is alkaline, p. H=10. • IV or rectal application is possible. • Duration of action is determined by redistribution. • Onset time of action 30 seconds
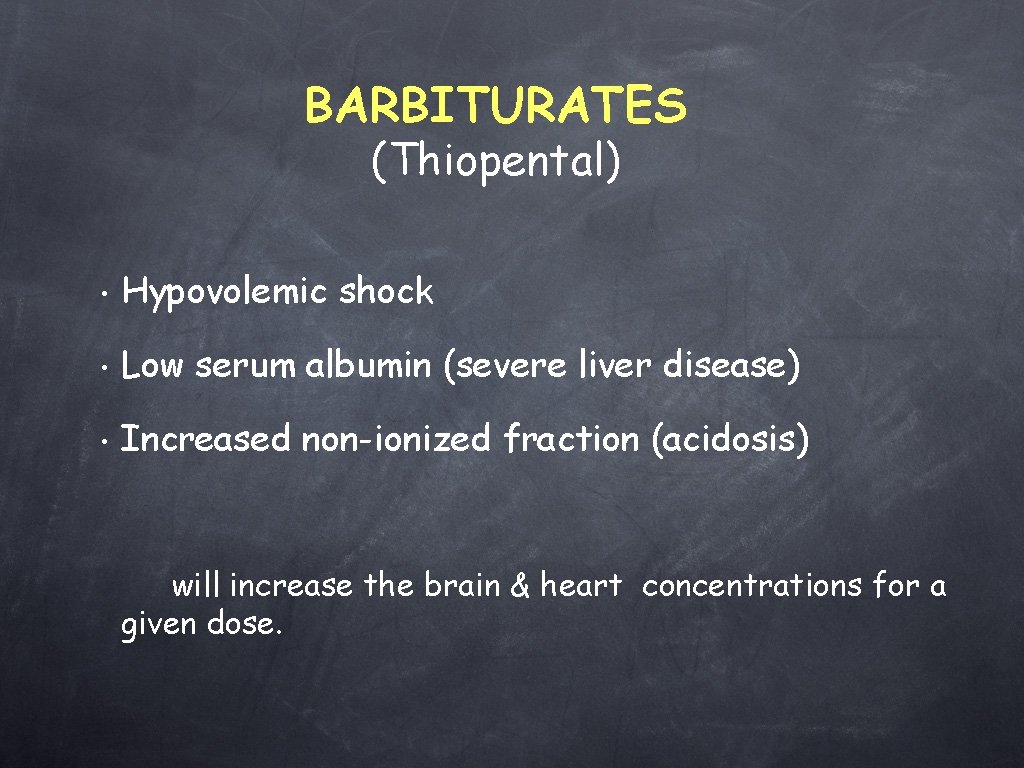
BARBITURATES (Thiopental) • Hypovolemic shock • Low serum albumin (severe liver disease) • Increased non-ionized fraction (acidosis) will increase the brain & heart concentrations for a given dose.
BENZODIAZEPINES Related Neurotransmitters GABA • • Benzodiazepines facilitate GABA binding Agonistic action on GABA may account for the sedative-hypnotic and anesthetic properties
BENZODIAZEPINES (Midazolam) • Absorbtion: Oral, IM, IV, SL, rectal, nasal (p. H<6: water, p. H>6: lipid soluble). • Highly protein bounded, rapid of onset & duration of action relatively long. Metabolized in liver, excreted in the urine. • Midazolam: elimination half life 2 hrs. Renal failure prolongs sedation (α-OH-midazolam) • Controls grand mal seizures. Antegrade amnesia. Mild muscle relaxation, anxiolysis, sedation.
• • Volatile anesthetic agents, ethanol, barbiturates, . . potentiate their sedative effects. Volatile MAC is reduced 30% with concomittant benzodiazepines.
KETAMINE (PHENCYCLIDINE ANALOGUE) • IV, IM, oral. • NMDA-ANTAGONIST (glutamate subtype) • Functionally dissociates the THALAMUS from the LIMBIC cortex. • Dissociative anesthesia. • Analgesic, amnestic, hypnosis.
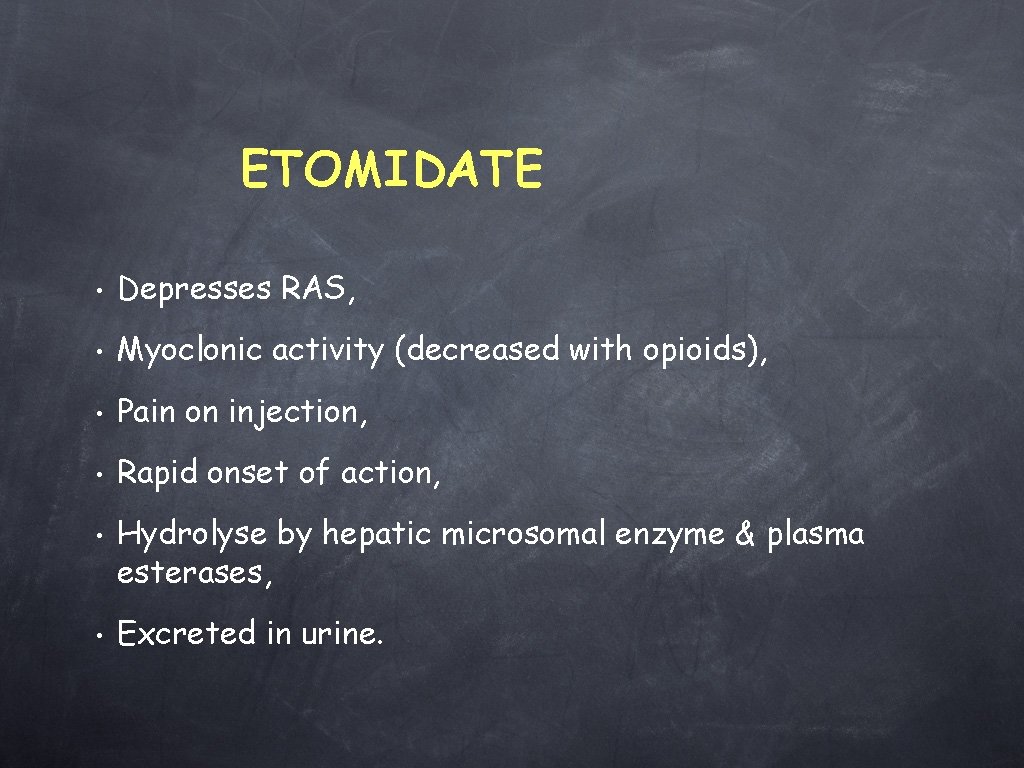
ETOMIDATE • Depresses RAS, • Myoclonic activity (decreased with opioids), • Pain on injection, • Rapid onset of action, • • Hydrolyse by hepatic microsomal enzyme & plasma esterases, Excreted in urine.
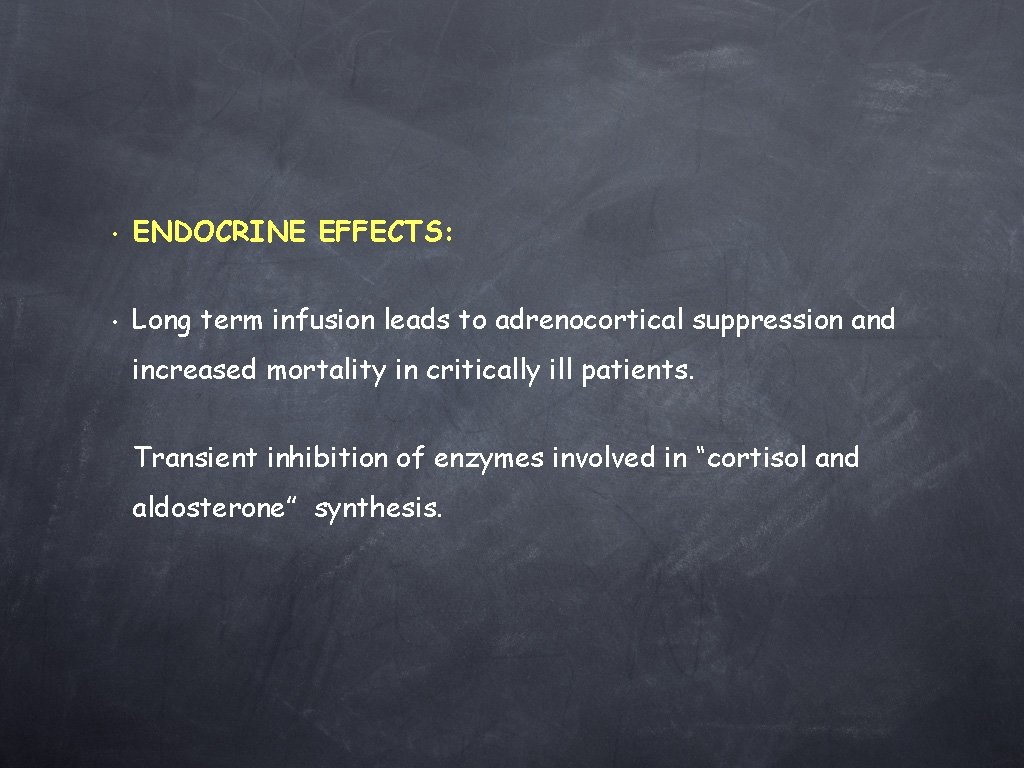
• ENDOCRINE EFFECTS: • Long term infusion leads to adrenocortical suppression and increased mortality in critically ill patients. Transient inhibition of enzymes involved in “cortisol and aldosterone” synthesis.
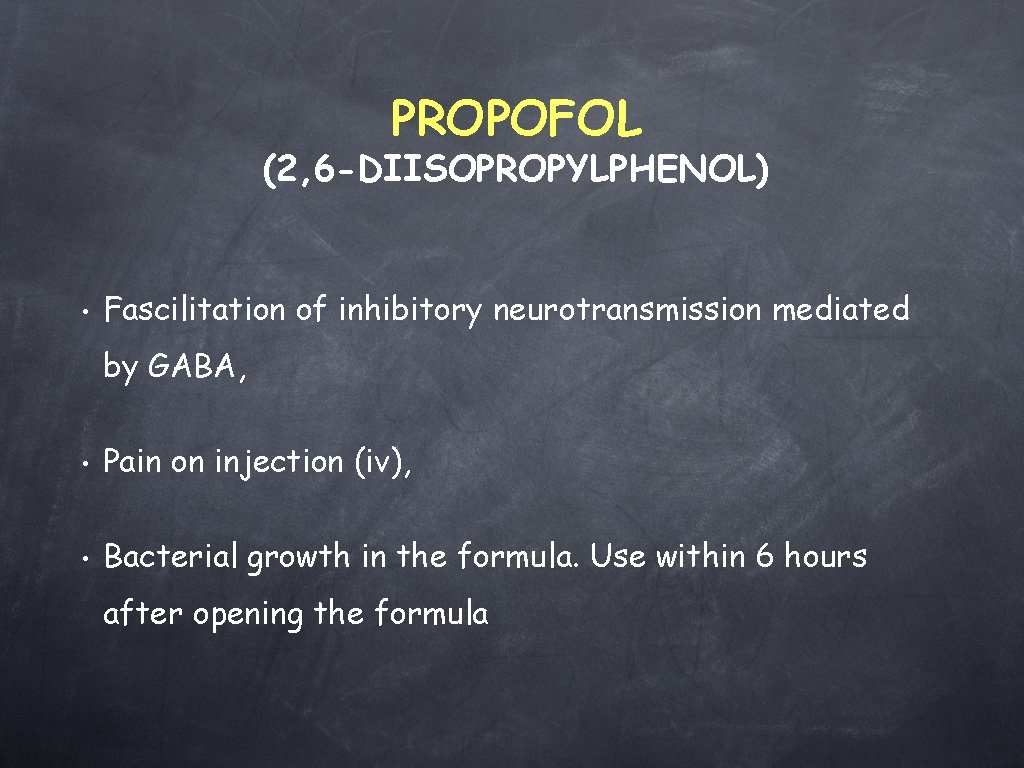
PROPOFOL (2, 6 -DIISOPROPYLPHENOL) • Fascilitation of inhibitory neurotransmission mediated by GABA, • Pain on injection (iv), • Bacterial growth in the formula. Use within 6 hours after opening the formula
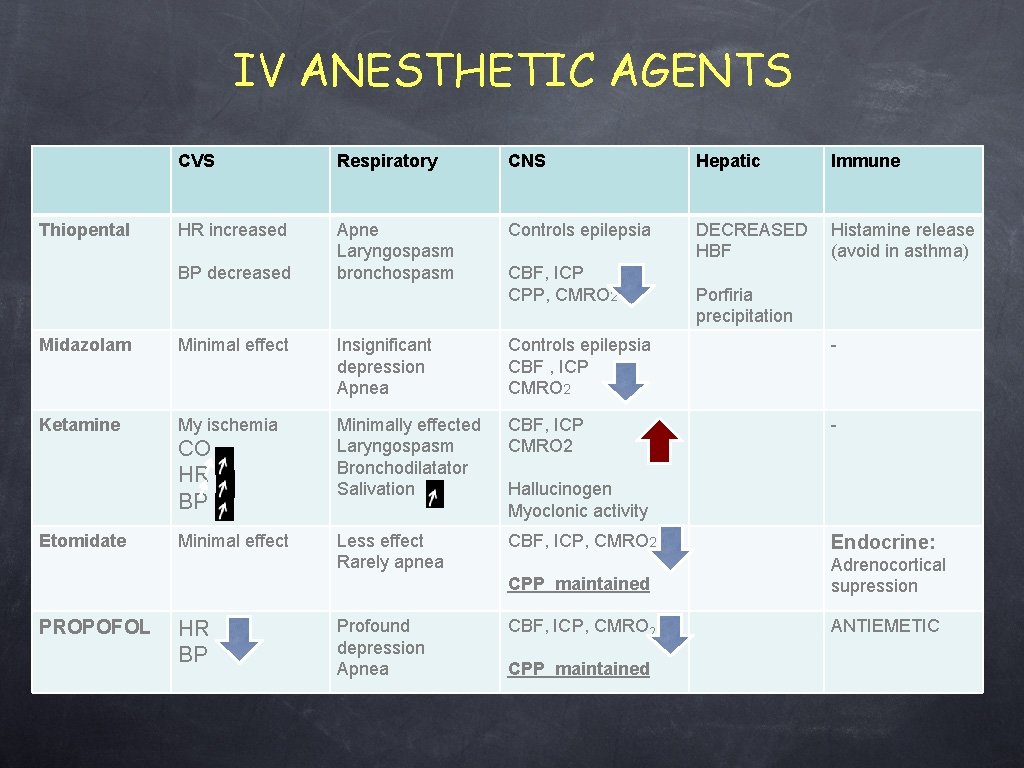
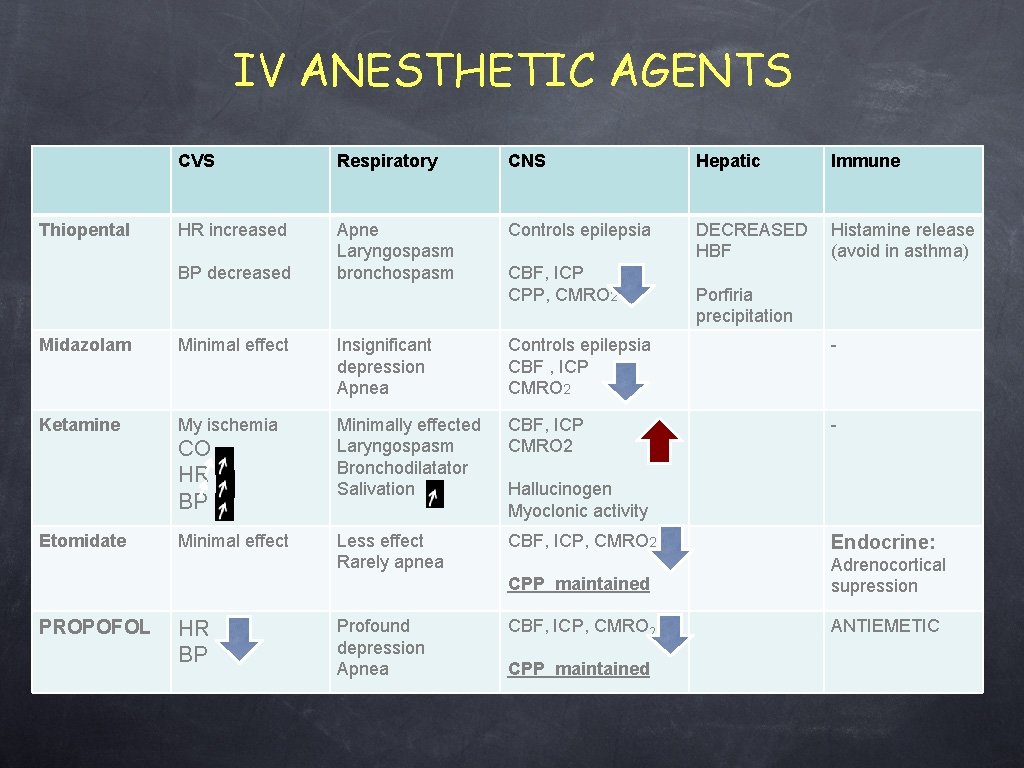
IV ANESTHETIC AGENTS Thiopental CVS Respiratory CNS Hepatic Immune HR increased Apne Laryngospasm bronchospasm Controls epilepsia DECREASED HBF Histamine release (avoid in asthma) BP decreased CBF, ICP CPP, CMRO 2 Porfiria precipitation Midazolam Minimal effect Insignificant depression Apnea Controls epilepsia CBF , ICP CMRO 2 - Ketamine My ischemia Minimally effected Laryngospasm Bronchodilatator Salivation CBF, ICP CMRO 2 - Less effect Rarely apnea CBF, ICP, CMRO 2 Endocrine: CPP maintained Adrenocortical supression CBF, ICP, CMRO 2 ANTIEMETIC CO HR BP Etomidate PROPOFOL Minimal effect HR BP Profound depression Apnea Hallucinogen Myoclonic activity CPP maintained
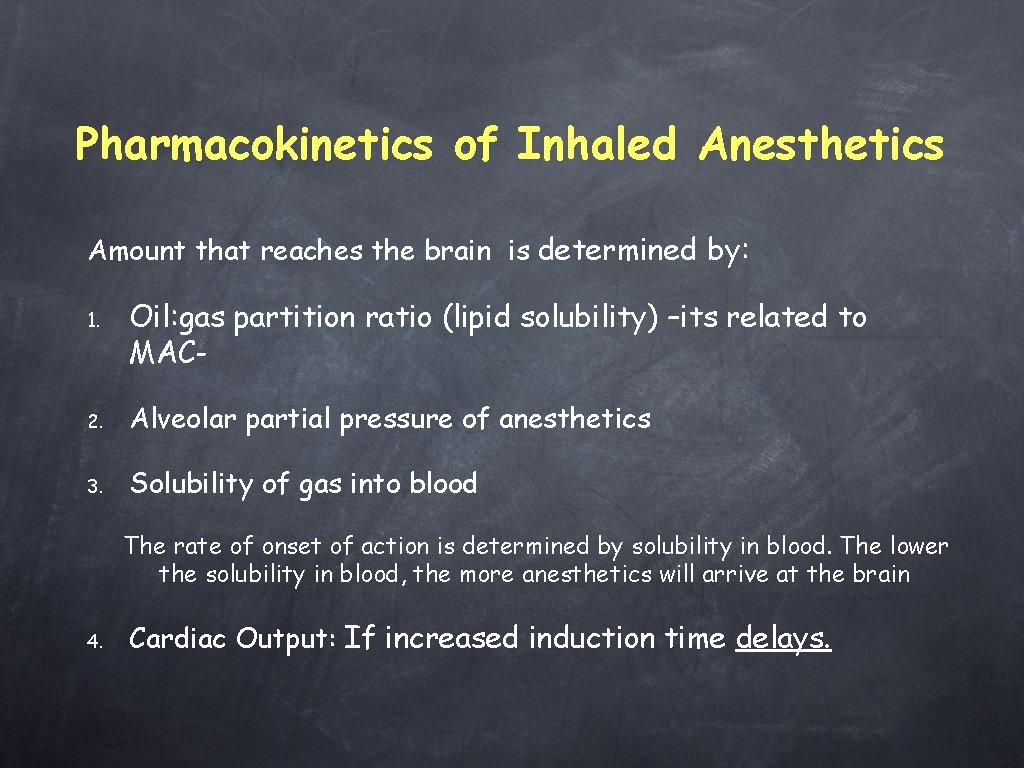
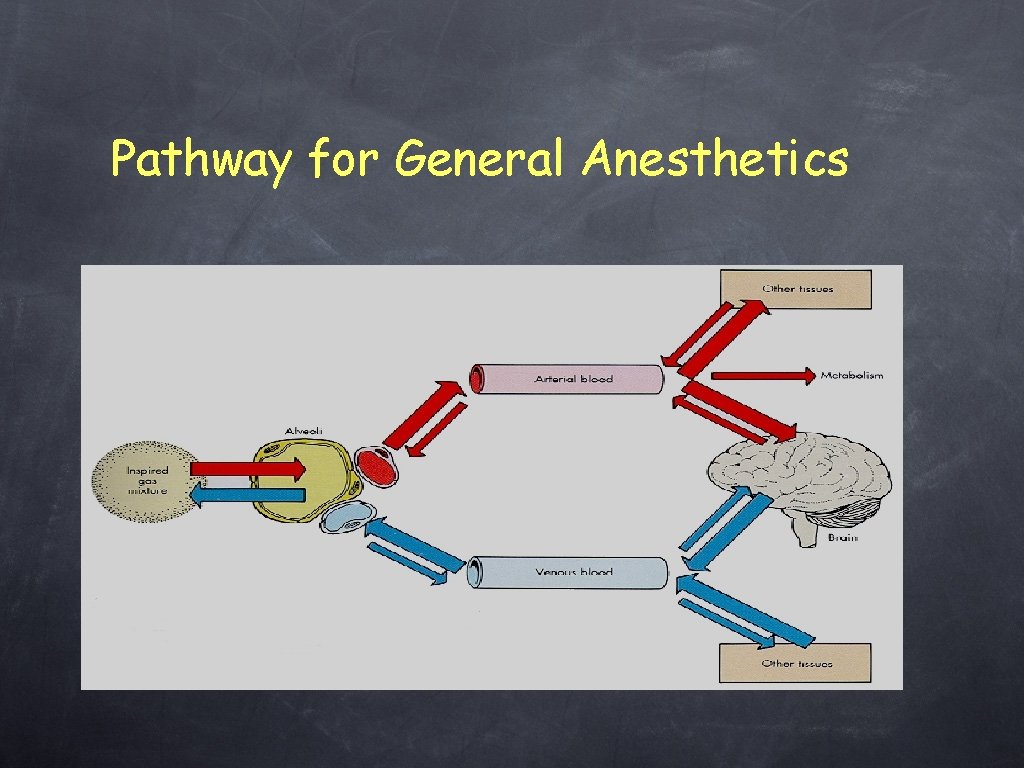
Pharmacokinetics of Inhaled Anesthetics Amount that reaches the brain is determined by: 1. Oil: gas partition ratio (lipid solubility) –its related to MAC- 2. Alveolar partial pressure of anesthetics 3. Solubility of gas into blood The rate of onset of action is determined by solubility in blood. The lower the solubility in blood, the more anesthetics will arrive at the brain 4. Cardiac Output: If increased induction time delays.
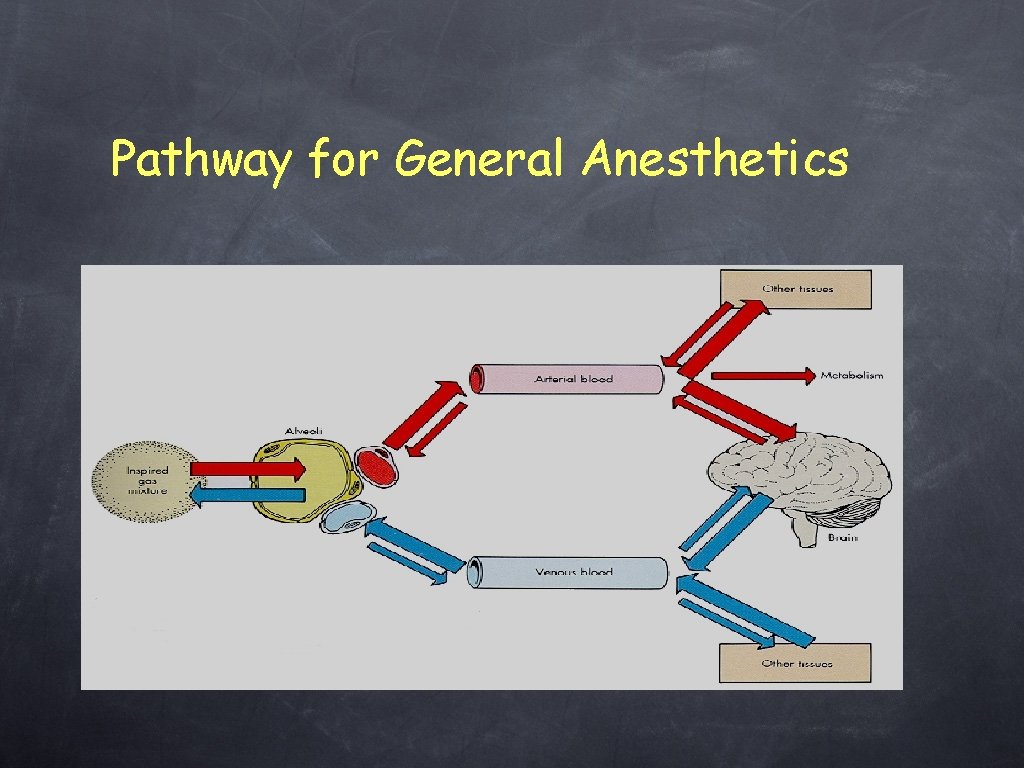
Pathway for General Anesthetics
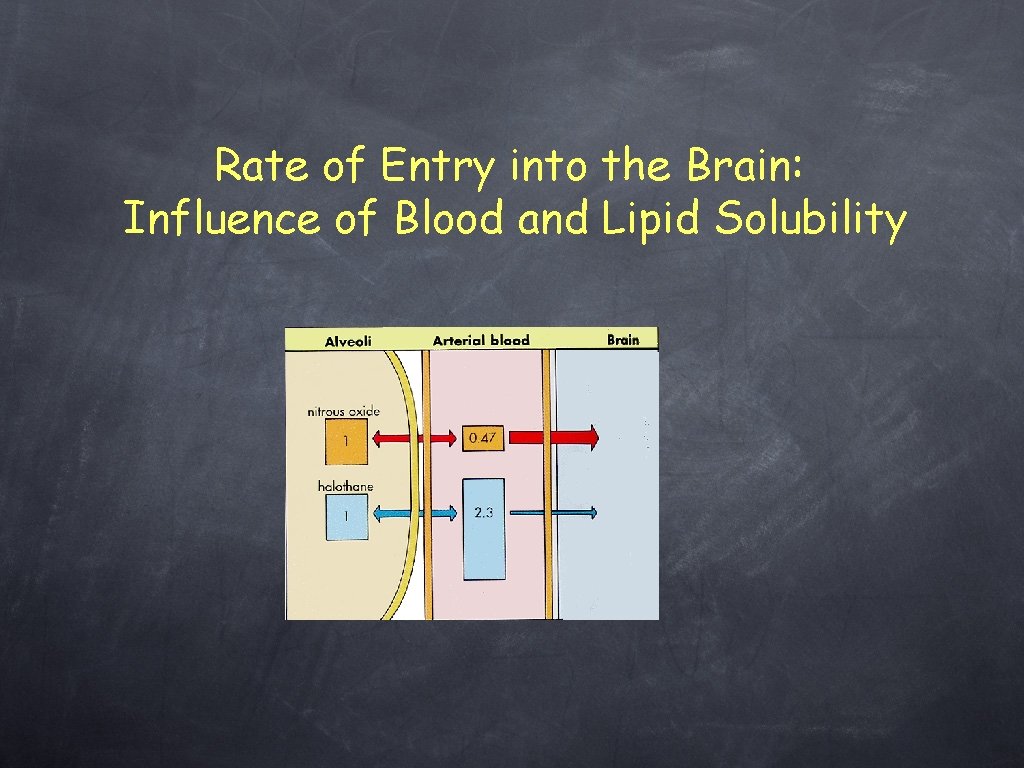
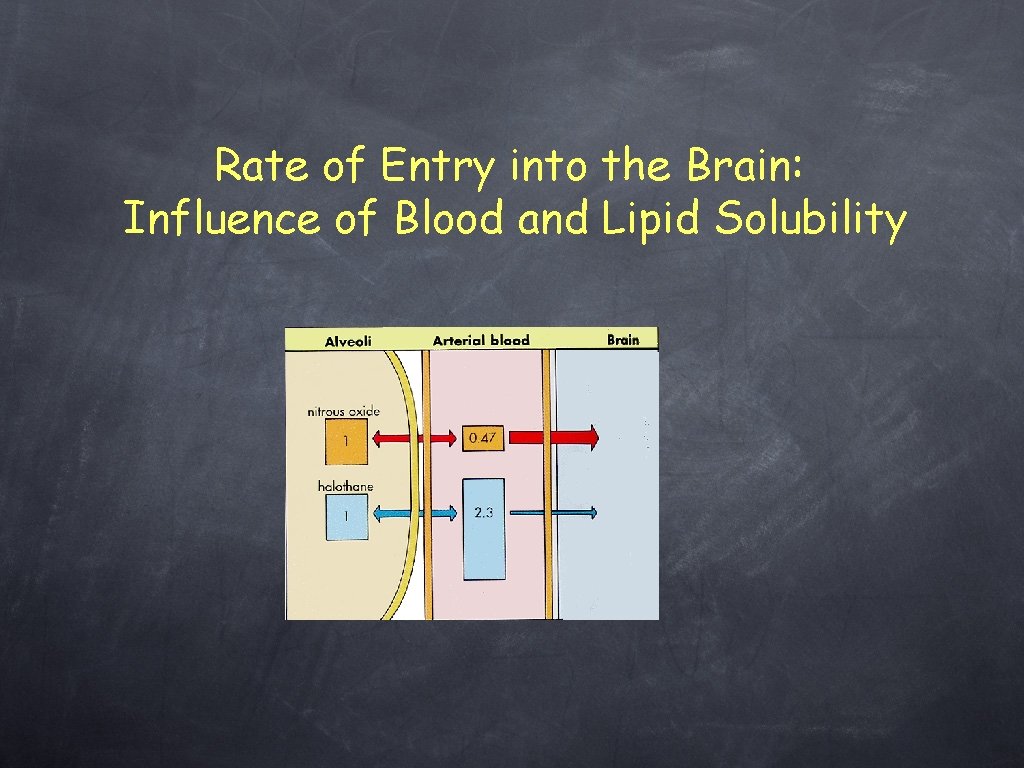
Rate of Entry into the Brain: Influence of Blood and Lipid Solubility
Control of volatile Partial Pressure in Brain • • Direct Physician's Control • Solubility of agent • Concentration of agent in inspired gas • Magnitude of alveolar ventilation Indirect Physician’s Control • Pulmonary blood flow (function of CO) • Arterio-venous concentration gradient
MAC (minimal alveolar concentration) • • • A measure of potency 1 MAC is the concentration necessary to prevent movement in response to painful stimulus in 50% of population. Values of MAC are additive: • Avoid cardiovascular depressive concentration of potent agents.
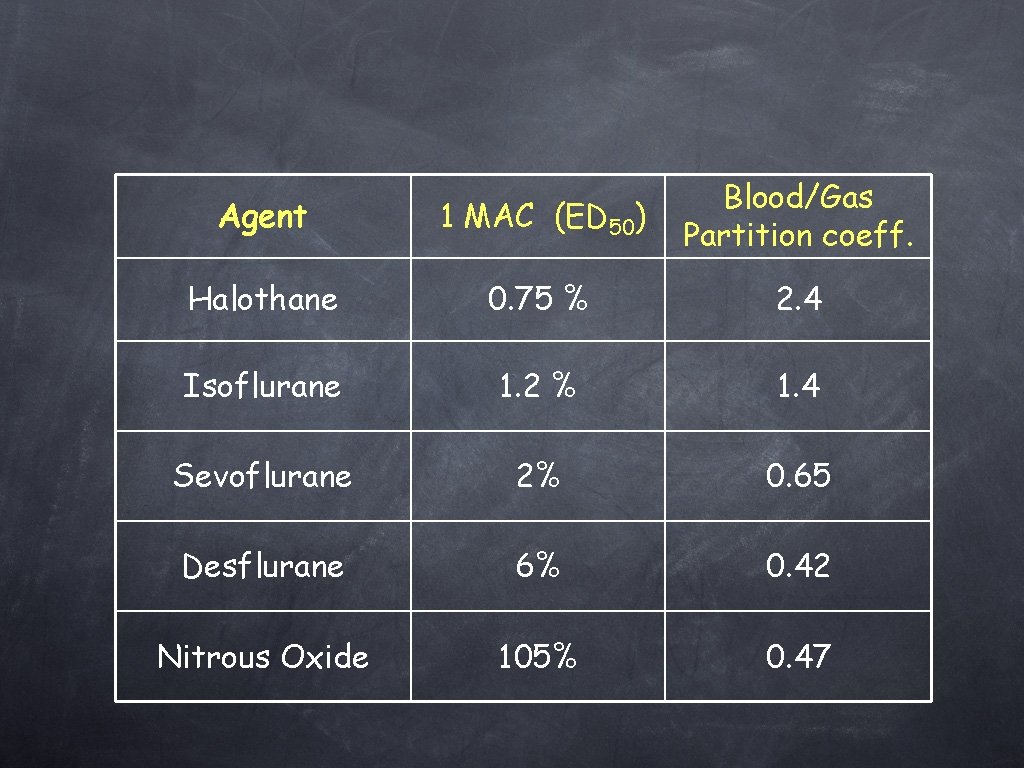
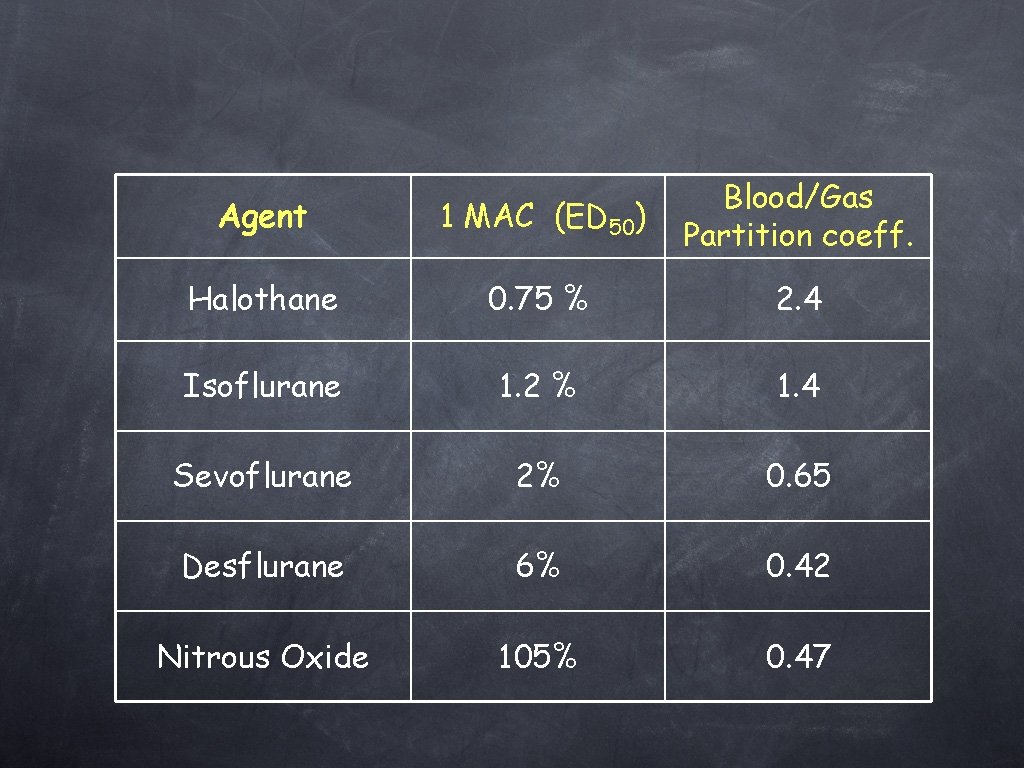
Agent 1 MAC (ED 50) Blood/Gas Partition coeff. Halothane 0. 75 % 2. 4 Isoflurane 1. 2 % 1. 4 Sevoflurane 2% 0. 65 Desflurane 6% 0. 42 Nitrous Oxide 105% 0. 47
General Actions of Inhaled Anesthetics • Respiration: Depress respiration and response to CO 2 • Kidney: • Muscle: High concentrations will relax skeletal muscle • Depress renal blood flow and urine output CNS: Increased cerebral blood flow, decreased cerebral metabolism
• Cardiovascular System • Generalized reduction in arterial pressure and peripheral vascular resistance. Isoflurane maintains cardiac output and coronary function better than other agents
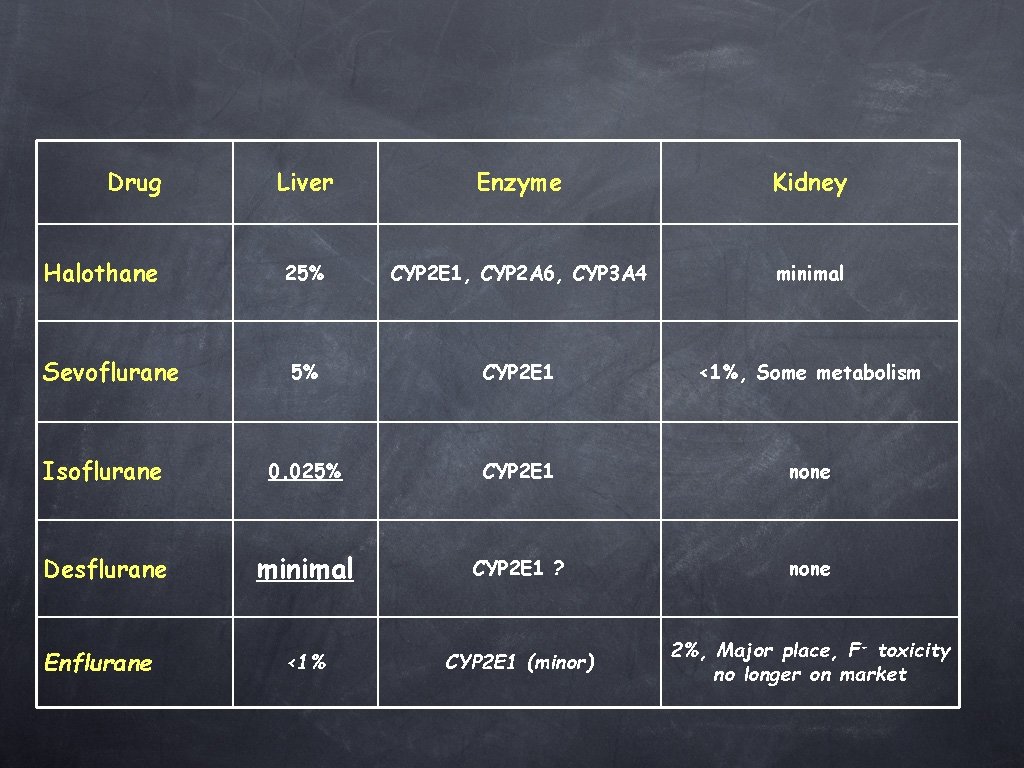
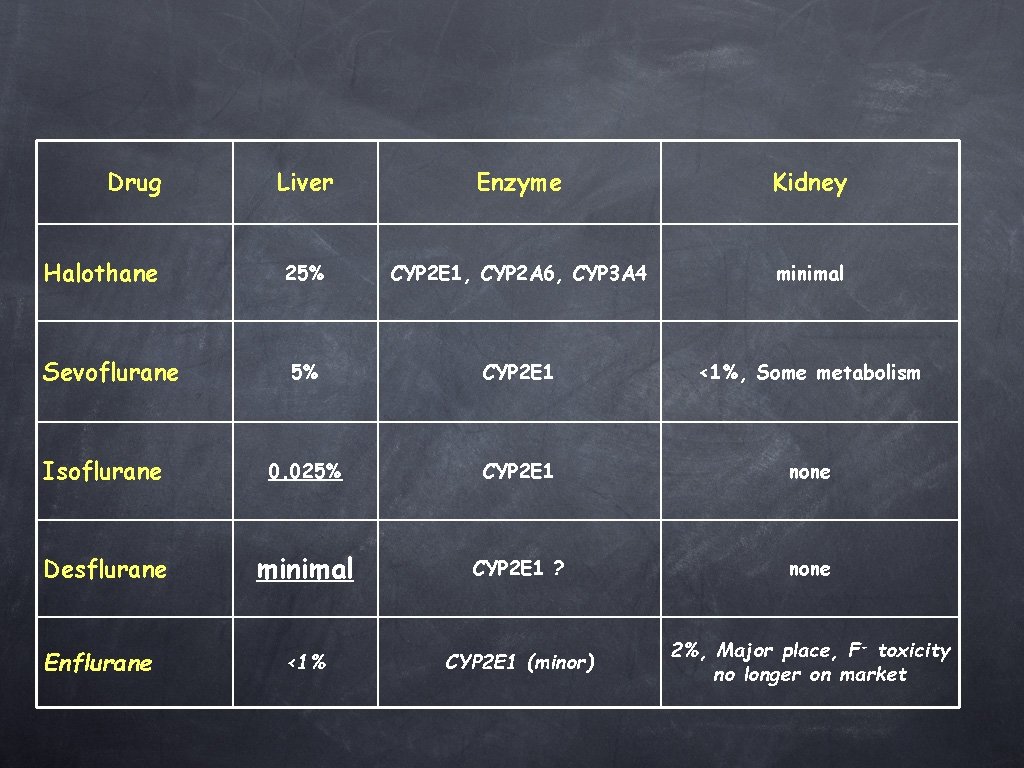
Drug Liver Enzyme Kidney 25% CYP 2 E 1, CYP 2 A 6, CYP 3 A 4 minimal 5% CYP 2 E 1 <1%, Some metabolism Isoflurane 0. 025% CYP 2 E 1 none Desflurane minimal CYP 2 E 1 ? none CYP 2 E 1 (minor) 2%, Major place, F- toxicity no longer on market Halothane Sevoflurane Enflurane <1%
Nitrous Oxide • Simple linear compound • Not metabolized • • Only anesthetic agent that is inorganic Colorless, odorless, tasteless
Nitrous Oxide • Major difference is low potency • Weak anesthetic, powerful analgesic • Needs other agents for surgical anesthesia • Low blood solubility (quick recovery)
Nitrous Oxide • Minimal effects on heart rate and blood pressure • May cause myocardial depression • Little effect on respiration • Beginning of case: second gas effect • End of case: diffusion hypoxia
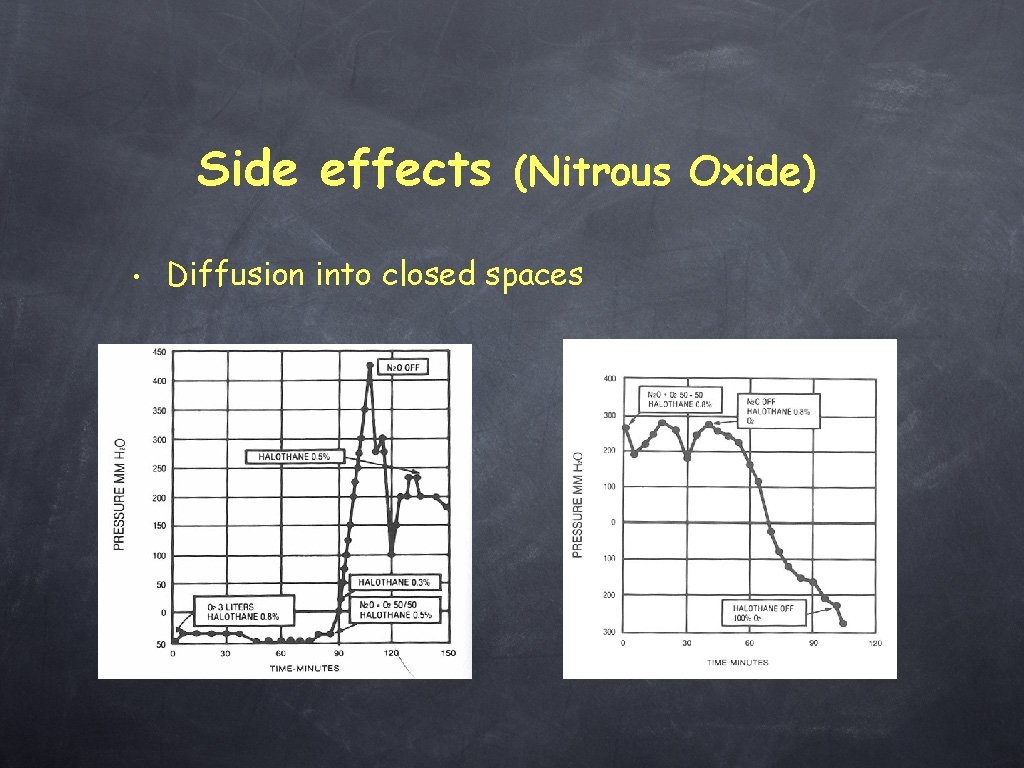
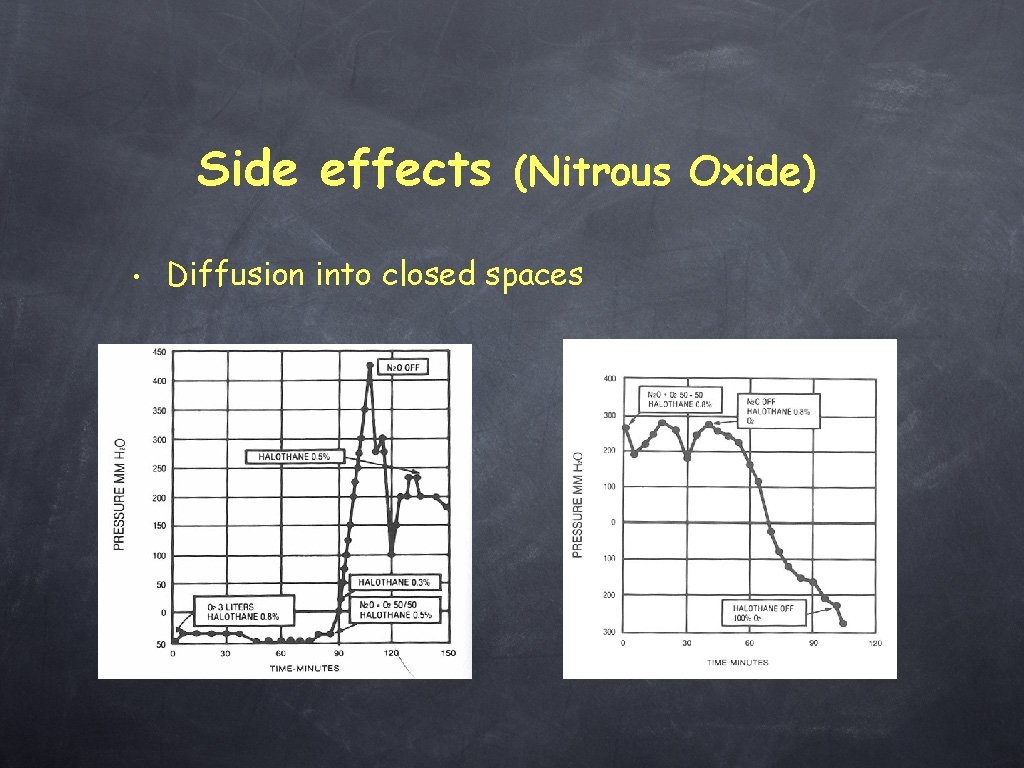
Side effects (Nitrous Oxide) • Diffusion into closed spaces
Side effects (Nitrous Oxide) • • Inhibits methionine synthetase (precursor to DNA synthesis) & vitamin B 12 metabolism, Dentists, operating room personnel, abusers are at risk.
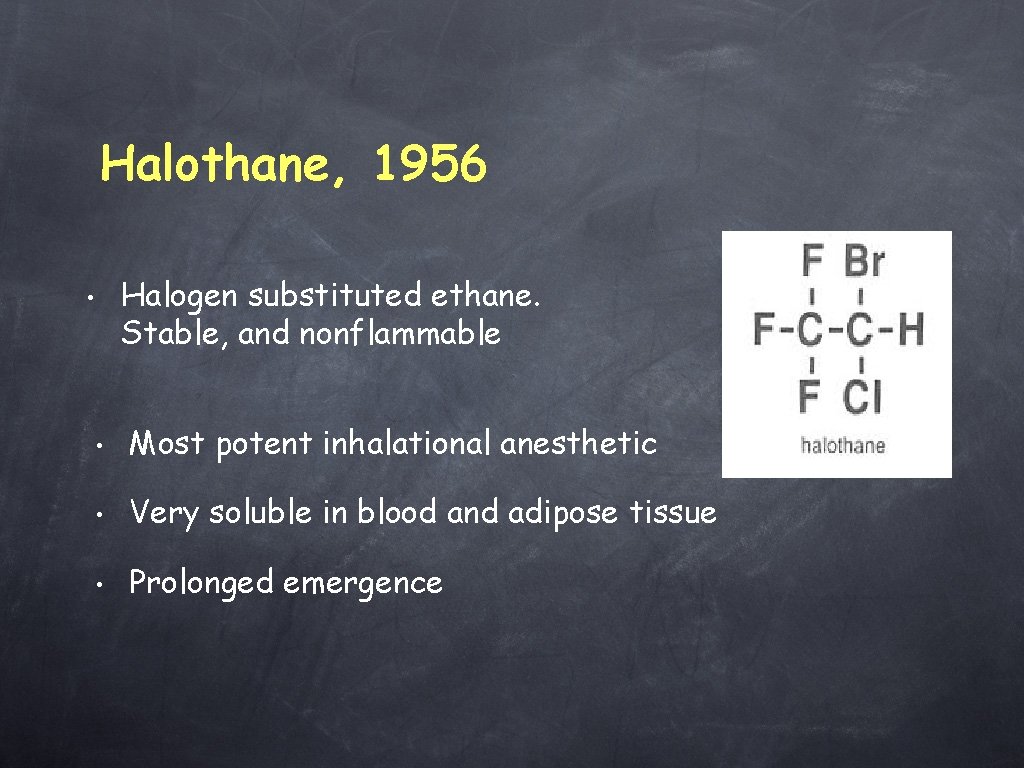
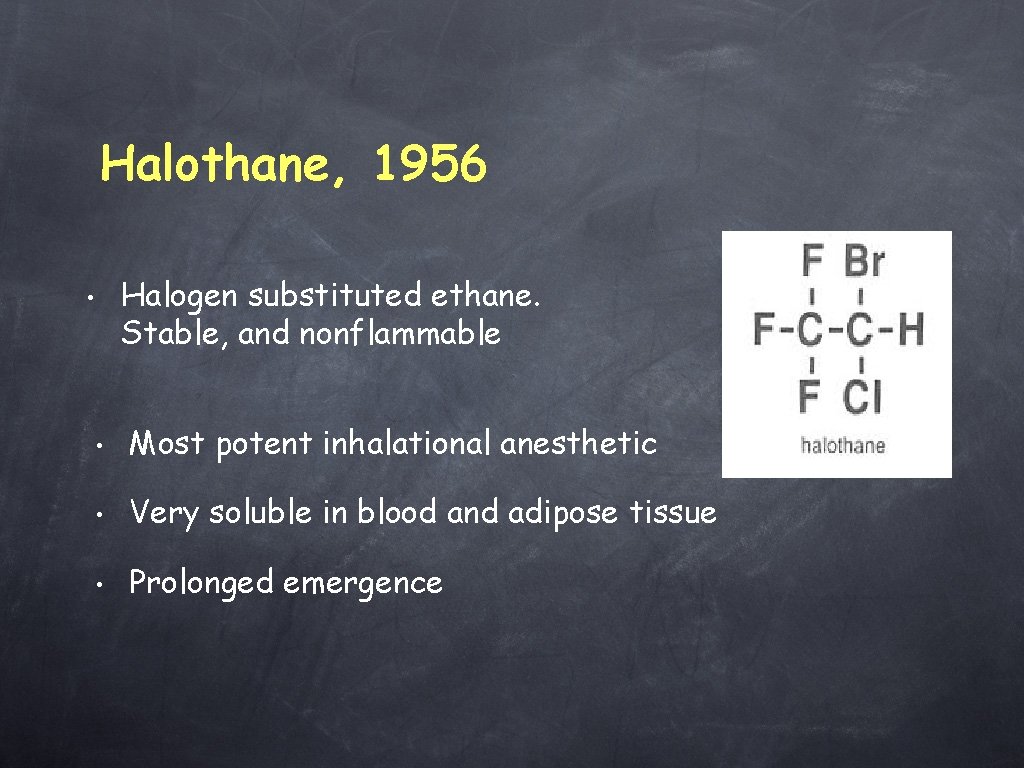
Halothane, 1956 Halogen substituted ethane. Stable, and nonflammable • • Most potent inhalational anesthetic • Very soluble in blood and adipose tissue • Prolonged emergence
• • Sensitizes myocardium to effects of exogenous catecholamines-- ventricular arrhythmias Depresses myocardium-- lowers blood pressure and slows conduction- • Decreases respiratory drive -central response to CO 2 - • Shallow respiration -- atelectasis • Depresses protective airway reflexes
Halothane (Side Effects) • “Halothane Hepatitis” -- 1/10, 000 cases (immunologically mediated) • fever, jaundice, hepatic necrosis, death • exposure dependent • • metabolic breakdown products are hapten-protein conjugates Malignant Hyperthermia-- 1/60, 000 (with succinylcholine to 1/260, 000).
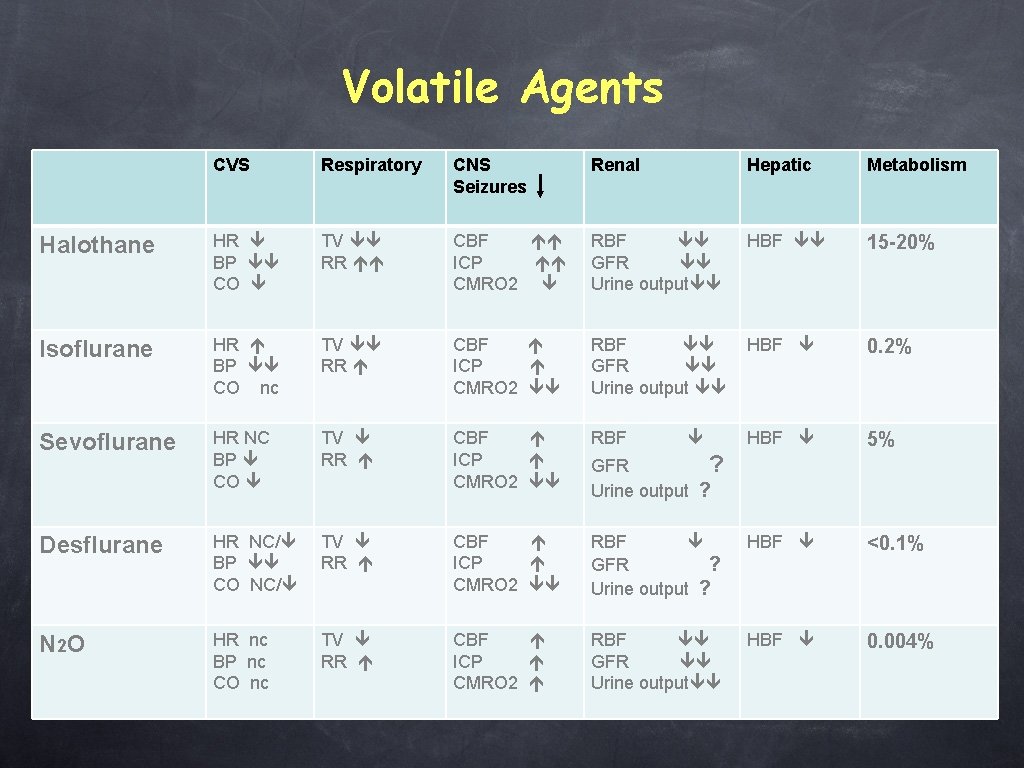
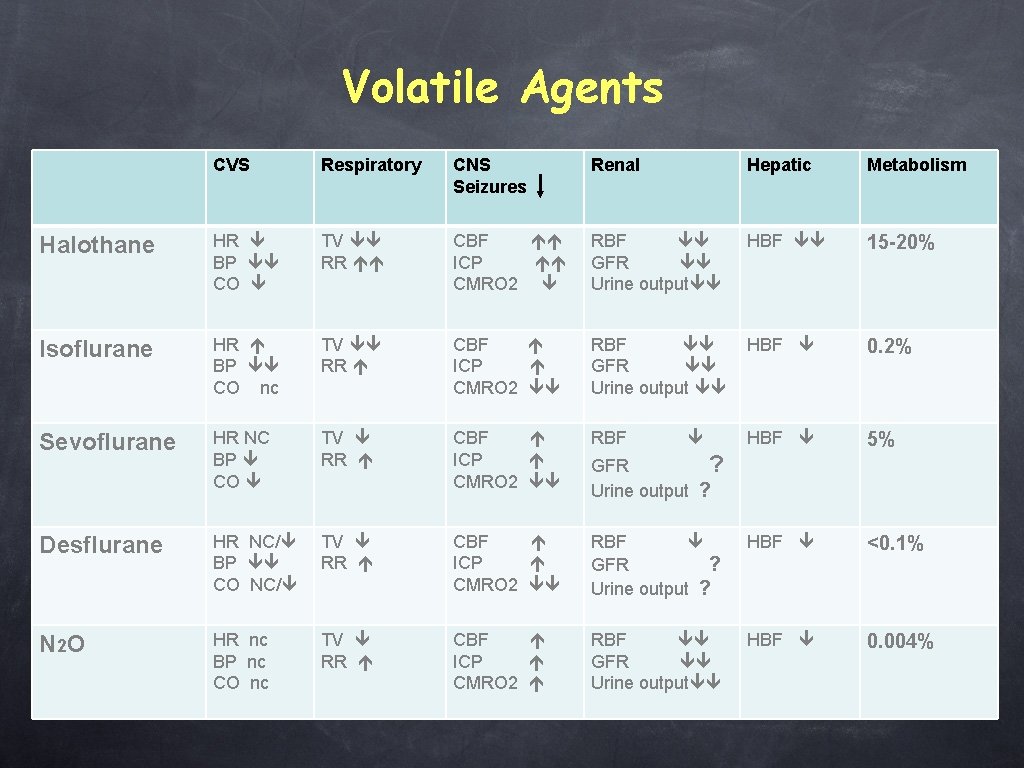
Volatile Agents CVS Respiratory CNS Seizures Renal Hepatic Metabolism Halothane HR BP CO TV RR CBF ICP CMRO 2 RBF GFR Urine output HBF 15 -20% Isoflurane HR BP CO nc TV RR CBF ICP CMRO 2 RBF GFR Urine output HBF 0. 2% Sevoflurane HR NC BP CO TV RR CBF ICP CMRO 2 RBF HBF 5% Desflurane HR NC/ BP CO NC/ TV RR CBF ICP CMRO 2 RBF GFR ? Urine output ? HBF <0. 1% N 2 O HR nc BP nc CO nc TV RR CBF ICP CMRO 2 RBF GFR Urine output HBF 0. 004% GFR ? Urine output ?
Isoflurane • Metabolized into trifluoroacetic acid • Nephrotoxicity is extremely unlikely • NMBA are potentiated by isoflurane
Sevoflurane • A potent inhalational anesthetic • Very soluble in blood and adipose tissue • Smooth and rapid induction • Fast emergence
Sevoflurane • • Advantages • It can be used for anesthesia induction • Less CNS activation • Cardio-protective Disadvantages • High cost • Compound A (possible nephrotoxicity)
Sevoflurane & Compound A • Sevoflurane reacts with sodalime (used in anesthetic circuit to absorb CO 2) to form a renal toxin “compound. A” (Trifluoromethyl- vinyl ether) • Some reports of fire and explosion • Little evidence of harm unless • • Low gas flow (≥ 2 L/min gas flow rate is recommended) • Prolonged exposure Some evidence for changes in renal damage markers but not clinically significant
Desflurane • Advantages • Disadvantages High cost • Insoluble • • Fast on/off • CNS stimulation (minor) Low residual at the end of case • Not suitable for induction • CO production (not relevant) •
Anesthetics & Carbon Monoxide • All anesthetic agents react with sodalime to produce CO • CO is toxic and binds to Hb in preference to oxygen Desflur > enflur >>> isoflur > sevoflur > halothane • Risk Factors • Dryness & high temperature of soda lime • In general, not clinically significant • No deaths reported
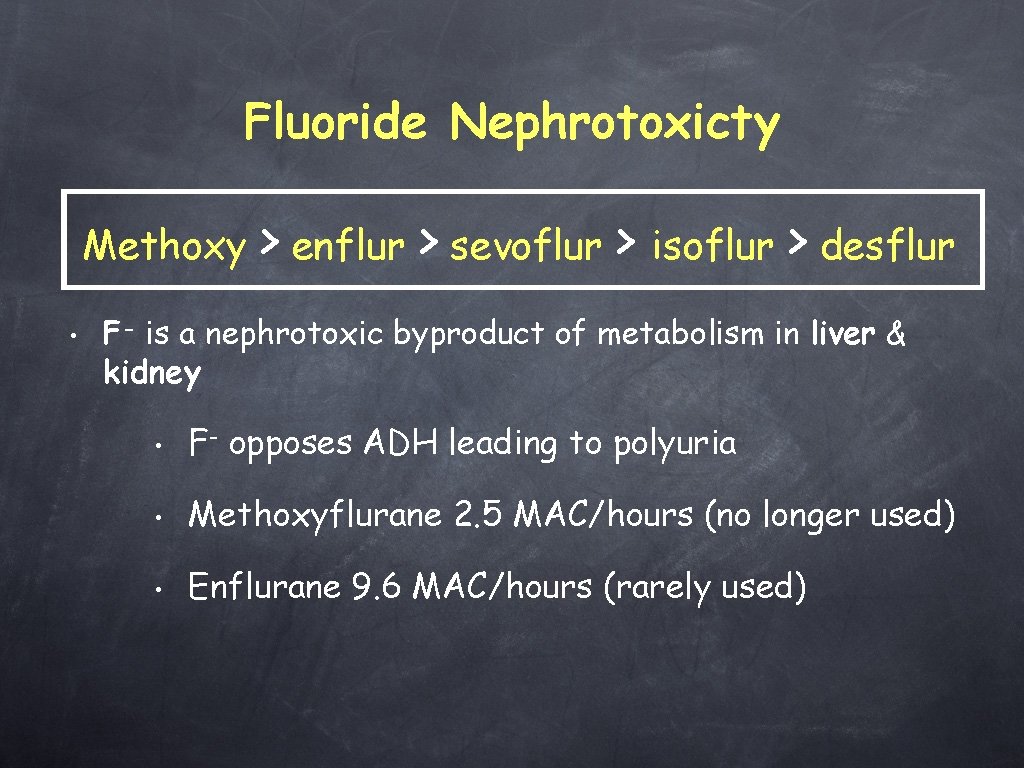
Fluoride Nephrotoxicty Methoxy • > enflur > sevoflur > isoflur > desflur F- is a nephrotoxic byproduct of metabolism in liver & kidney • F- opposes ADH leading to polyuria • Methoxyflurane 2. 5 MAC/hours (no longer used) • Enflurane 9. 6 MAC/hours (rarely used)
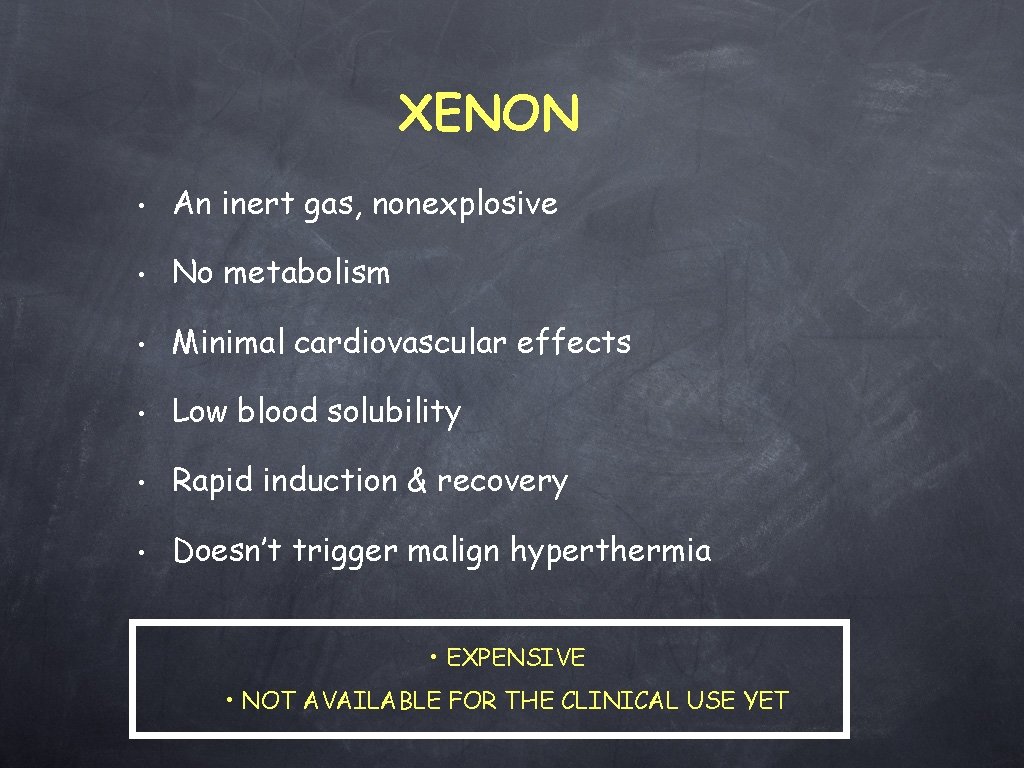
XENON • An inert gas, nonexplosive • No metabolism • Minimal cardiovascular effects • Low blood solubility • Rapid induction & recovery • Doesn’t trigger malign hyperthermia • EXPENSIVE • NOT AVAILABLE FOR THE CLINICAL USE YET
 Lahey clinic anesthesiology residency
Lahey clinic anesthesiology residency �zge�mi? haz?rlama
�zge�mi? haz?rlama Umass neurology residency
Umass neurology residency York hospital eye clinic appointments
York hospital eye clinic appointments Unc heme onc fellowship
Unc heme onc fellowship Mayo clinic dress code
Mayo clinic dress code Andrea beyer cleveland clinic
Andrea beyer cleveland clinic Stroke and turn clinic
Stroke and turn clinic Tgw
Tgw Integrative medical clinic santa rosa
Integrative medical clinic santa rosa Uccs health circle
Uccs health circle Ideal clinic components
Ideal clinic components +weekend +clinic
+weekend +clinic Mt washington feeding clinic
Mt washington feeding clinic Chemster medical clinic
Chemster medical clinic Dr. ibrahim askar clinic
Dr. ibrahim askar clinic Mary bridge neurology clinic
Mary bridge neurology clinic Dr veronica white
Dr veronica white Lower elwha health clinic
Lower elwha health clinic Argument clinic gif
Argument clinic gif Lahey coumadin clinic
Lahey coumadin clinic Caswell clinic
Caswell clinic Gum clinics surrey
Gum clinics surrey Ideal clinic
Ideal clinic Cleveland clinic revenue
Cleveland clinic revenue Htp secundara usoara
Htp secundara usoara Chemical hazards in a veterinary clinic
Chemical hazards in a veterinary clinic Metta clinic calgary
Metta clinic calgary Tablou clinic ulcer gastric
Tablou clinic ulcer gastric Falls team glasgow
Falls team glasgow Dr maeve durkan cork clinic
Dr maeve durkan cork clinic Copper queen physical therapy
Copper queen physical therapy Cleveland clinic second opinion
Cleveland clinic second opinion Christus mobile clinic
Christus mobile clinic Wilcox clinic
Wilcox clinic Biocleanse plus
Biocleanse plus Augusta health care walk in clinic
Augusta health care walk in clinic Asp medical clinic
Asp medical clinic Oban dental clinic
Oban dental clinic Ama clinic
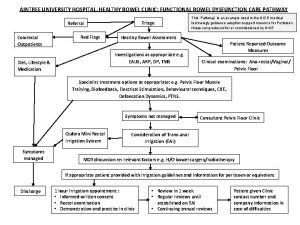
Ama clinic Healthy bowel clinic aintree
Healthy bowel clinic aintree Thirlby clinic traverse city michigan
Thirlby clinic traverse city michigan 21 audubon pediatric clinic
21 audubon pediatric clinic Uta math department
Uta math department Christy shifa clinic
Christy shifa clinic Umn faculty dental clinic
Umn faculty dental clinic Vance afb clinic
Vance afb clinic Npaihb
Npaihb Keller army pharmacy
Keller army pharmacy Lummi tribal health clinic
Lummi tribal health clinic Coumadin clinic emory
Coumadin clinic emory Trial clinic randomizat
Trial clinic randomizat Hackney adhd clinic
Hackney adhd clinic Osa labaka
Osa labaka Kaiser sleep clinic
Kaiser sleep clinic Is sentara a nonprofit organization
Is sentara a nonprofit organization San francisco community clinic consortium
San francisco community clinic consortium Psychrometric chart trane
Psychrometric chart trane