Transfusion Medicine III Complications and Safety of Transfusion








- Slides: 30
Transfusion Medicine III Complications and Safety of Transfusion Practices Salwa Hindawi Medical Director of Blood Transfusion Services KAUH 4 th year medical students 2 nd Feb, 2008
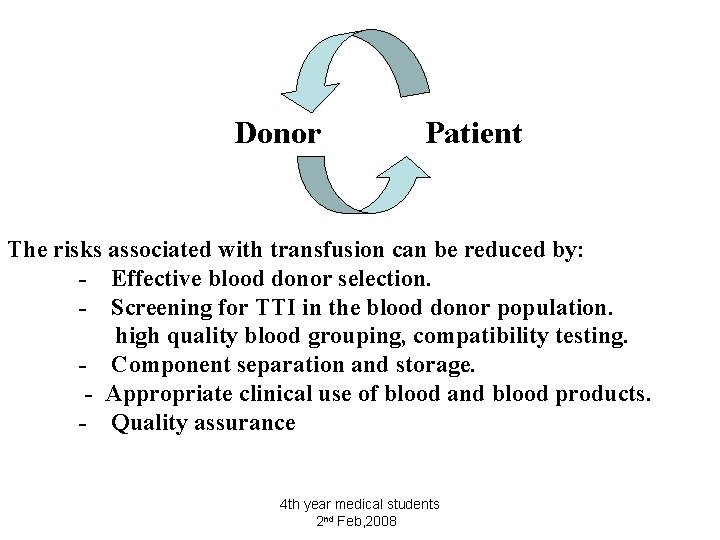
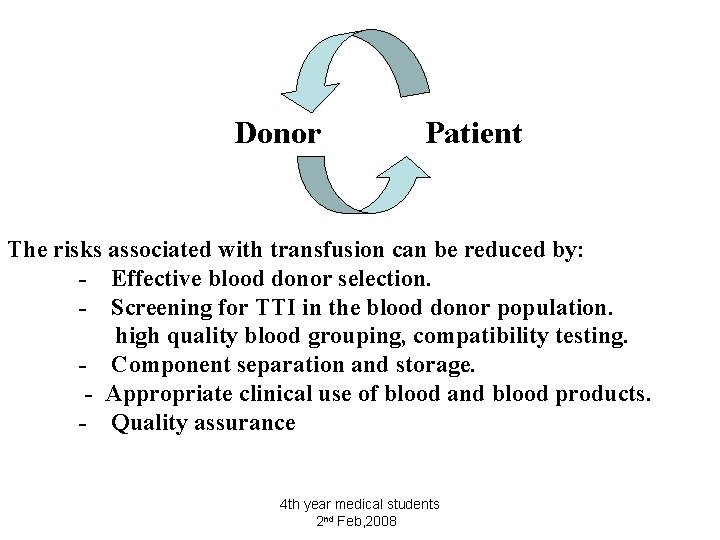
Donor Patient The risks associated with transfusion can be reduced by: - Effective blood donor selection. - Screening for TTI in the blood donor population. high quality blood grouping, compatibility testing. - Component separation and storage. - Appropriate clinical use of blood and blood products. - Quality assurance 4 th year medical students 2 nd Feb, 2008

Principles of Clinical Transfusion Practices v v v Avoid blood transfusion Transfusion is only one part of the patient’s management. Prevention and early diagnosis and treatment of Anemia & underlying condition Use of alternative to transfusion. eg. IV fluids Good anesthetic and surgical management to minimized blood loss. 4 th year medical students 2 nd Feb, 2008
– Prescribing should be based on national guidelines on the clinical use of blood taking individual patient needs into account. – Hb level should not be the sole deciding Factor Clinical evaluation is important 4 th year medical students 2 nd Feb, 2008

– Consent form to be obtained from the patient before transfusion. – The clinician should record the reason for transfusion clearly. – A trained person should monitor the transfused patient and if any adverse effects occur respond immediately. 4 th year medical students 2 nd Feb, 2008
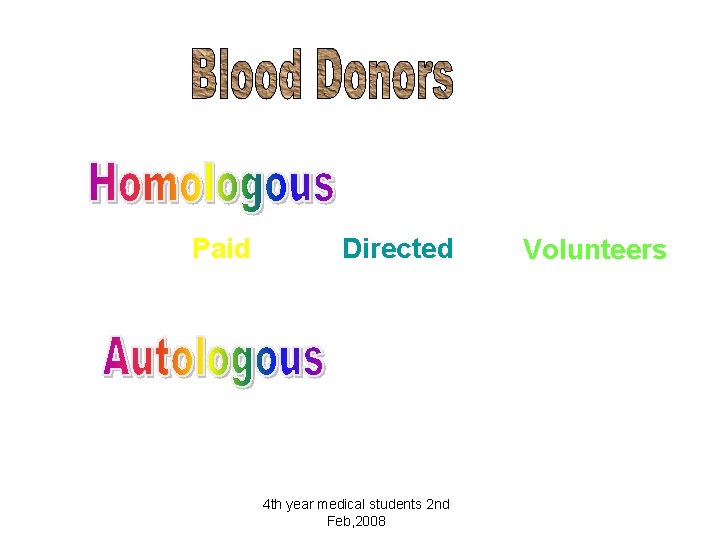
Paid Directed 4 th year medical students 2 nd Feb, 2008 Volunteers
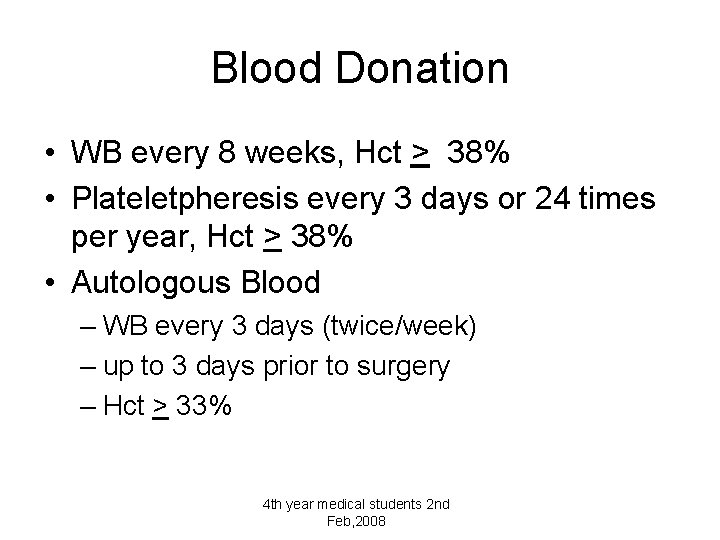
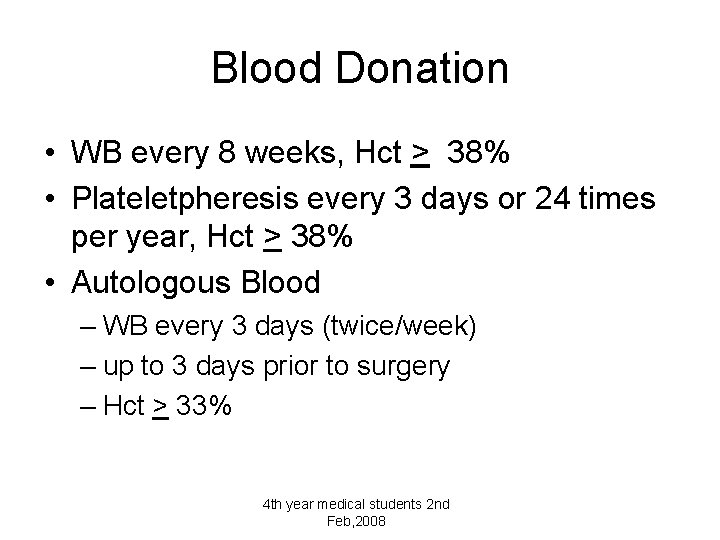
Blood Donation • WB every 8 weeks, Hct > 38% • Plateletpheresis every 3 days or 24 times per year, Hct > 38% • Autologous Blood – WB every 3 days (twice/week) – up to 3 days prior to surgery – Hct > 33% 4 th year medical students 2 nd Feb, 2008

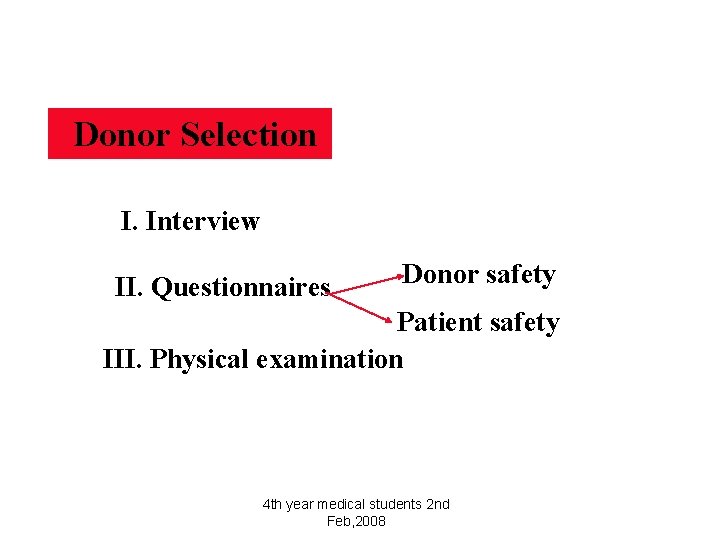
Donor Selection Is Important To Be Sure That The Donor Is Fit To Donate The Required Amount Of Blood Donation Will Not Harm The Donor The Donated Blood Should Be Safe And Free From Transfusion Transmitted Infections TTI 4 th year medical students 2 nd Feb, 2008
Donor Selection I. Interview II. Questionnaires Donor safety Patient safety III. Physical examination 4 th year medical students 2 nd Feb, 2008
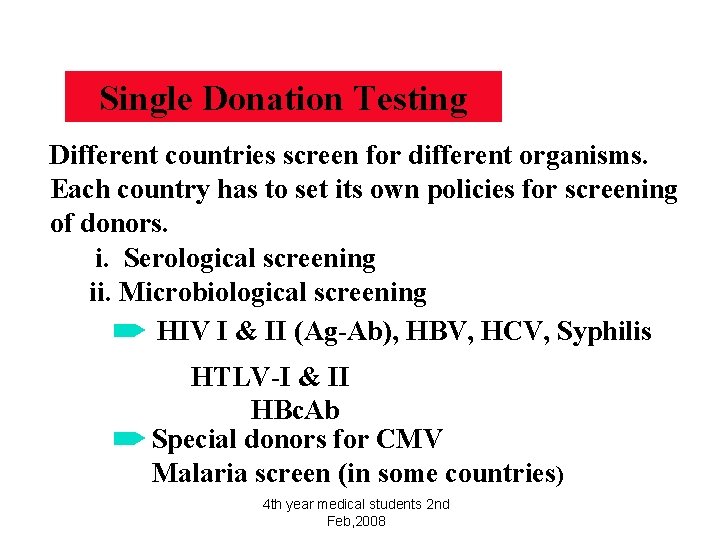
Single Donation Testing Different countries screen for different organisms. Each country has to set its own policies for screening of donors. i. Serological screening ii. Microbiological screening HIV I & II (Ag-Ab), HBV, HCV, Syphilis HTLV-I & II HBc. Ab Special donors for CMV Malaria screen (in some countries) 4 th year medical students 2 nd Feb, 2008
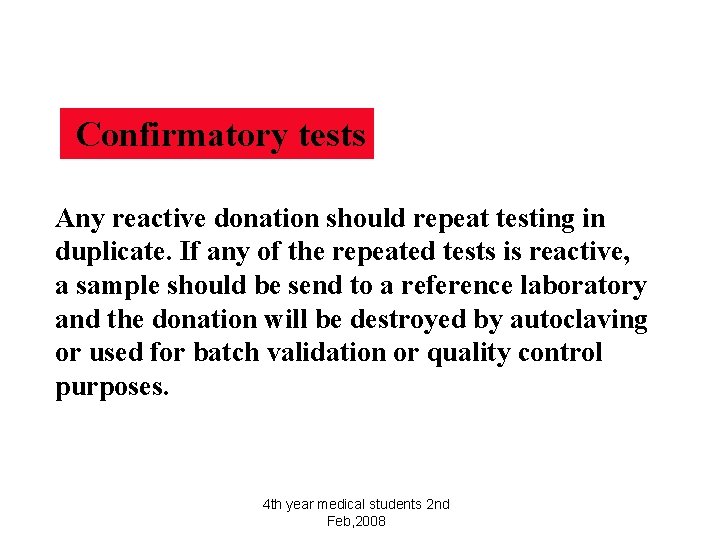
Confirmatory tests Any reactive donation should repeat testing in duplicate. If any of the repeated tests is reactive, a sample should be send to a reference laboratory and the donation will be destroyed by autoclaving or used for batch validation or quality control purposes. 4 th year medical students 2 nd Feb, 2008

Complications of Blood Transfusion Immediate HTR FNTR TRALI Bacterial contamination Allergic, Anaphylaxis Delayed GVHD PTP Iron overload Infectious diseases Alloimmunization 4 th year medical students 2 nd Feb, 2008
Acute Hemolytic Transfusion Reaction • a clerical error (wrong specimen, wrong patient) • 1 in 6, 000 to 25, 000 transfusions • back pain, chest pain, fever, red urine, oliguria, shock, DIC, death in 1 in 4 • stop the transfusion 4 th year medical students 2 nd Feb, 2008
Work up of An AHTR • • • start normal saline treat patient symptomatically send blood bag and tubing to culture send red top and purple top tubes urine specimen for hemoglobinuria DAT is positive 4 th year medical students 2 nd Feb, 2008

Non Hemolytic Febrile Transfusion Reaction • NHFTR (1: 100) • Recipient has WBC antibodies to Donor WBCs contained within RBCs and Plateletpheresis products • DAT is negative • rise in temperature by 2 F or 1 C • other causes for fever are eliminated 4 th year medical students 2 nd Feb, 2008
Allergic (Urticarial) Transfusion Reaction • Recipient has antibodies to the Donor’s plasma proteins (1 in 1000) • offending protein is not identified • urticaria, itching, flushing, wheezing • this is the only transfusion reaction where the blood that is hanging can be restarted after treatment with Benadryl • if symptoms continue then STOP 4 th year medical students 2 nd Feb, 2008

Anaphlyactic Transfusion Reaction • anaphylactic reaction (1 in 150, 000) • 1 in 700 -900 people never made Ig. A • occurs when exposed to normal blood products which contain Ig. A • bronchospasm, vomiting and diarrhea and vascular collapse • treat with Epinepherine, Solu-Medrol, 4 th year medical students 2 nd Feb, 2008
Circulatory Overload • marginal cardiovascular status • given blood components too rapidly • develops acute shortness of breath, heart failure, edema (1: 10, 000) • systolic BP increases 50 mm • infuse slowly, not to exceed 4 hours • split the unit of RBC and give half 4 th year medical students 2 nd Feb, 2008
Transfusion Related Acute Leukocyte Lung Injury • TRALI reaction (1: 10, 000) • Donor plasma contains WBC antibodies that when transfused to the recipient cause agglutination of recipient’s WBC in the pulmonary capillary beds • Chest X ray looks like ARDS • Donor removed from donating blood 4 th year medical students 2 nd Feb, 2008
Transfusion - Related Acute Lung Injury (TRALI) A potentially fatal transfusion reaction Manifested usually within 6 hrs after transfusion Characterised by Hypoxemia Pa. O 2/ Fi. O 2< 300 mmhg O 2 sat <90% on room air Chest X-ray: Bilateral hilar infiltrates Absence of evidence of circulatory overload Toronto TRALI Concensus Conference 1 April 2004 Transfusion, 44; 1774 -91 Dec 2004 4 th year medical students 2 nd Feb, 2008
Diagnosis High Index of suspicion / Timing of Transfusion Blood Gases Chest X-ray hypoxia and pulmonary oedema ; most consistent findings. Diagnosis of exclusion 4 th year medical students 2 nd Feb, 2008
TRALI Non-cardiogenic pulmonary oedema (result of increased vascular permeability) The first sign of the reaction can be “Production of copious quantities of frothy blood-tinged fluid” from the endotracheal tube during intubation 4 th year medical students 2 nd Feb, 2008
Differential Diagnosis Other courses of pulmonary oedema • • • Volume Overload Congestive heart failure Myocardial infarction Response to diuretics? 4 th year medical students 2 nd Feb, 2008

Other Differential Diagnosis acute reaction • Acute haemolytic transfusion reaction • Bacterial infection(TTI) • Acute anaphylaxis Ig. A def with anti-Ig. A 4 th year medical students 2 nd Feb, 2008
Management • Adequate respiratory support 100% patients need O 2 support 71% required mechanical ventilation Steroids not beneficial Important to distinguish TRALI from volume overload Treatment with diuretics may have a detrimental effect /reduced cardiac out put. May need fluid support. 4 th year medical students 2 nd Feb, 2008
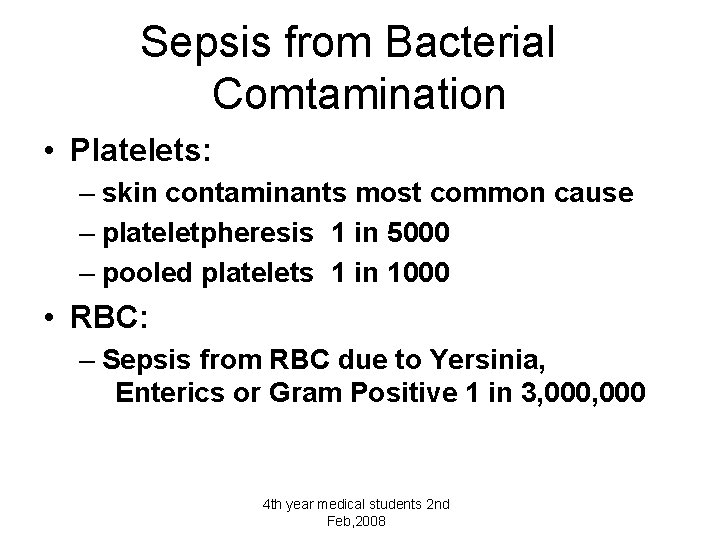
Sepsis from Bacterial Comtamination • Platelets: – skin contaminants most common cause – plateletpheresis 1 in 5000 – pooled platelets 1 in 1000 • RBC: – Sepsis from RBC due to Yersinia, Enterics or Gram Positive 1 in 3, 000 4 th year medical students 2 nd Feb, 2008
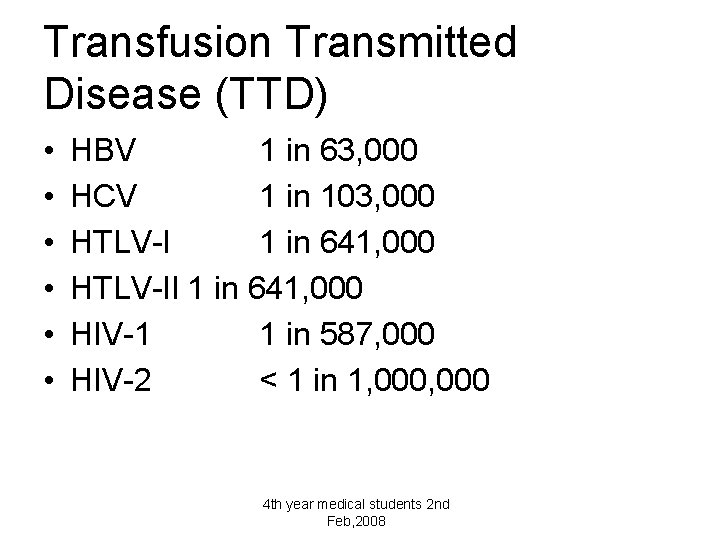
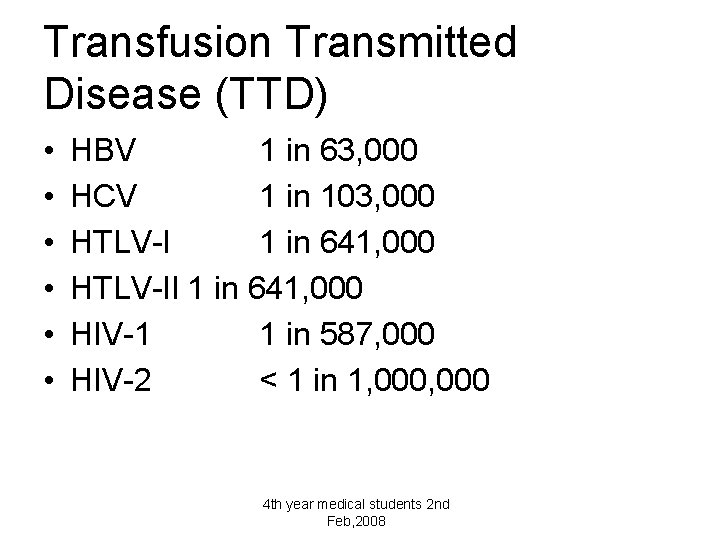
Transfusion Transmitted Disease (TTD) • • • HBV 1 in 63, 000 HCV 1 in 103, 000 HTLV-I 1 in 641, 000 HTLV-II 1 in 641, 000 HIV-1 1 in 587, 000 HIV-2 < 1 in 1, 000 4 th year medical students 2 nd Feb, 2008
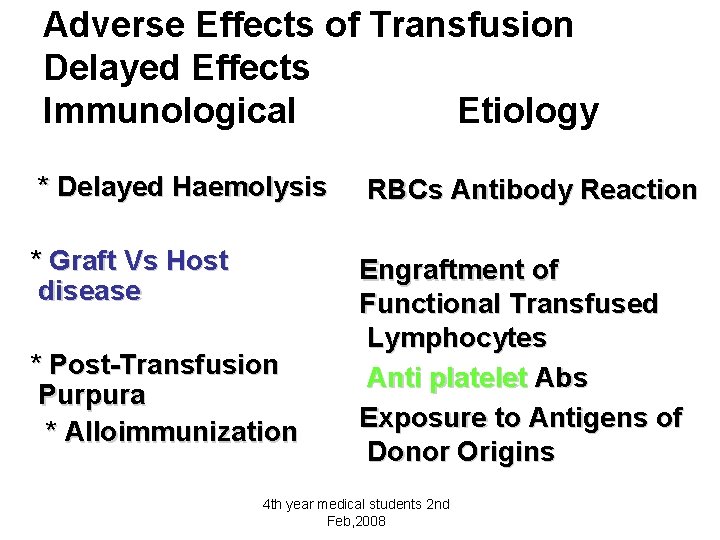
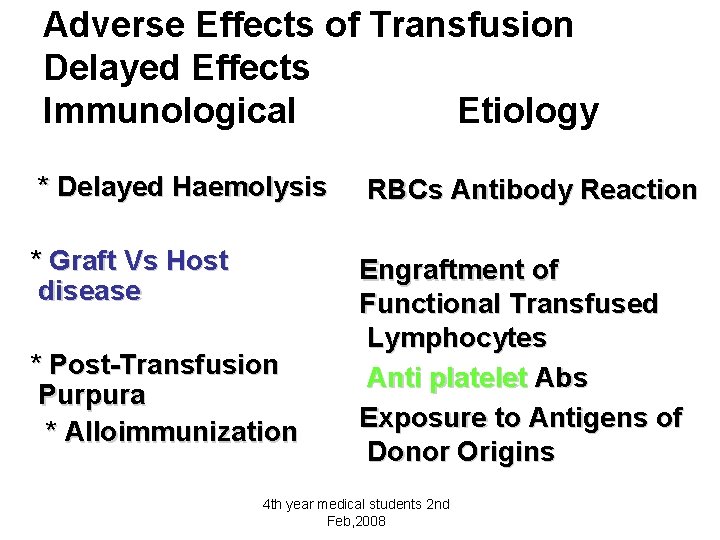
Adverse Effects of Transfusion Delayed Effects Immunological Etiology * Delayed Haemolysis RBCs Antibody Reaction * Graft Vs Host disease Engraftment of Functional Transfused Lymphocytes Anti platelet Abs Exposure to Antigens of Donor Origins * Post-Transfusion Purpura * Alloimmunization 4 th year medical students 2 nd Feb, 2008
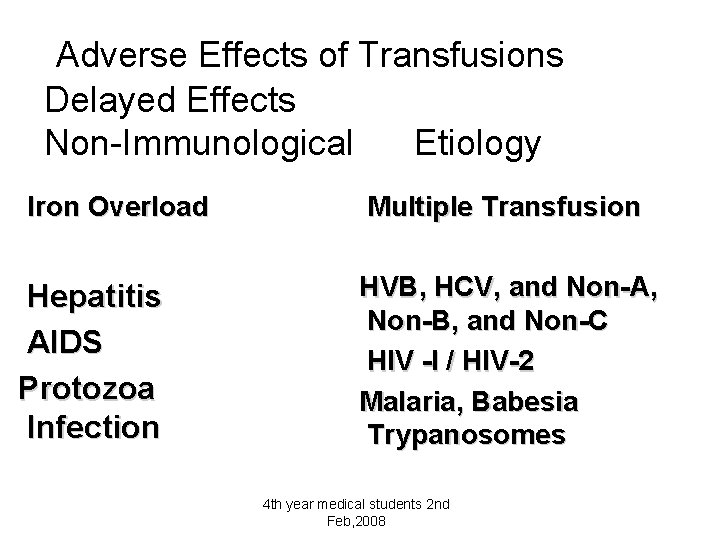
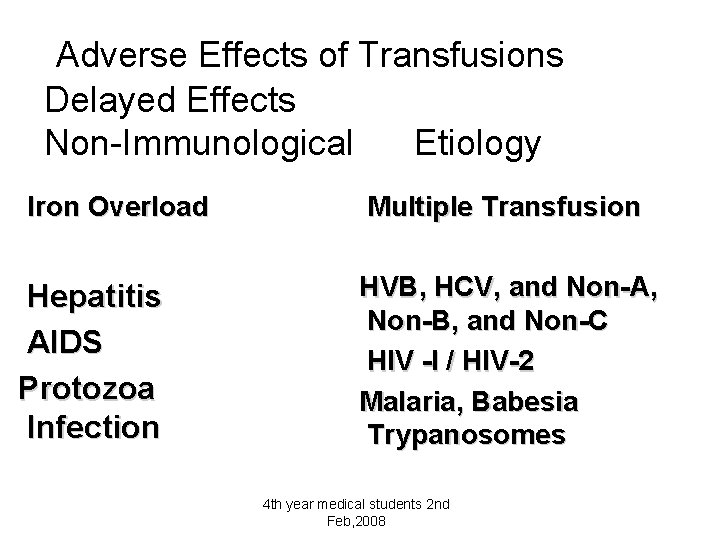
Adverse Effects of Transfusions Delayed Effects Non-Immunological Etiology Iron Overload Hepatitis AIDS Protozoa Infection Multiple Transfusion HVB, HCV, and Non-A, Non-B, and Non-C HIV -I / HIV-2 Malaria, Babesia Trypanosomes 4 th year medical students 2 nd Feb, 2008

4 th year medical students 2 nd Feb, 2008
 Early and late complications of blood transfusion
Early and late complications of blood transfusion Early and late complications of blood transfusion
Early and late complications of blood transfusion Massive transfusion protocol
Massive transfusion protocol Complications of blood transfusion
Complications of blood transfusion Blood grouping and crossmatching
Blood grouping and crossmatching Blood transfusion allergic reaction
Blood transfusion allergic reaction What are the complications of blood transfusion
What are the complications of blood transfusion Platelet concentrate transfusion
Platelet concentrate transfusion Corcider
Corcider Hamlet act iii scene ii
Hamlet act iii scene ii The events and complications begin to resolve themselves
The events and complications begin to resolve themselves Aspects of the setting
Aspects of the setting Medicine safety
Medicine safety Medicine safety
Medicine safety Levothyroxine side effects
Levothyroxine side effects Eswl complications
Eswl complications Complications c section
Complications c section Duodenal switch complications
Duodenal switch complications Complications of shigellosis
Complications of shigellosis Trachestomy tube
Trachestomy tube Complications of asthma
Complications of asthma Who stroke definition
Who stroke definition Thoracentesis indications
Thoracentesis indications Complications of eclampsia
Complications of eclampsia Bishop scoring
Bishop scoring Post dated pregnancy complications
Post dated pregnancy complications Naciecie krocza
Naciecie krocza Bronchoscopy complications
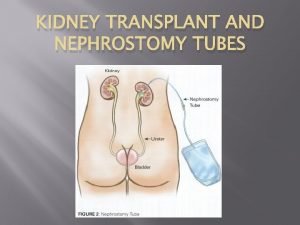
Bronchoscopy complications Neph tubes
Neph tubes How to mix shingrix vaccine
How to mix shingrix vaccine Bronchoscopy complications
Bronchoscopy complications