Perioperative Transfusion Medicine NonTransfusion Methods Hemostasis Surgical Medicine



- Slides: 34

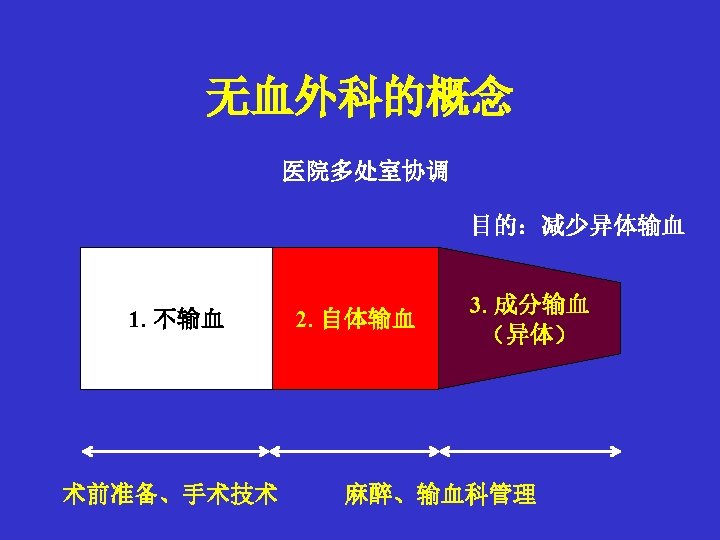
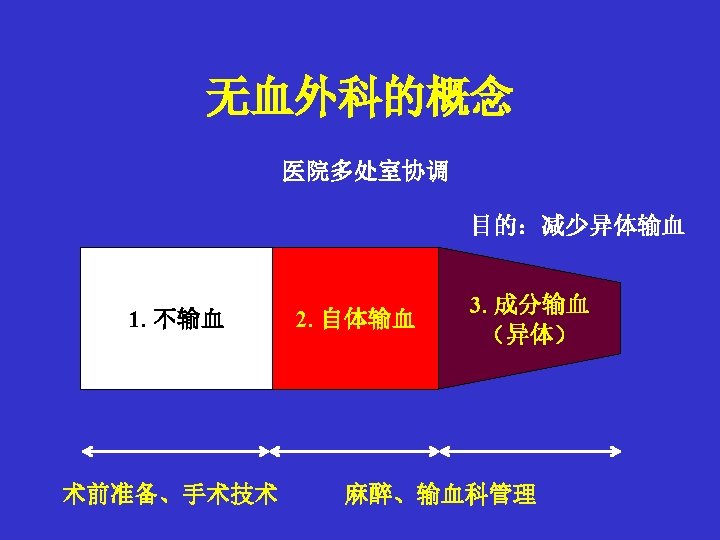
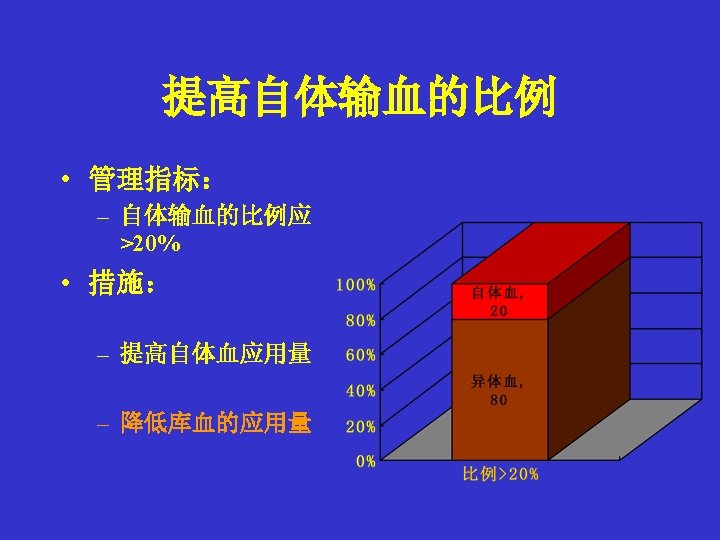
围术期输血 Perioperative Transfusion Medicine • Non-Transfusion Methods – Hemostasis (Surgical / Medicine) – Transfusion Trigger • Indications for Blood Transfusion • Autotransfusion – Preoperative Autologous Donation (PAD) – Acute Normovolemic Hemodilution (ANH) Intraoperative Autologous Donation – Red Cell Salvage (CS) • Minimize Allogeneic Transfusion
过去二十年临床输血的改变 Changes in red blood cell transfusion practice during the past two decades Wass CT, Transfusion. 2007; 47(6): 1022 USA • A retrospective analysis, with the Mayo database, of adult patients undergoing major spine surgery – 1980 to 1985 early practice group; n = 699 – 1995 to 2000 late practice group; n = 610 • Compared to the early practice group: – 所有术前的 Hb 浓度显著降低 – 异体 RBC 输入显著减少,而自体输血明显增加 – no significant difference in major morbidity or mortality was observed between groups
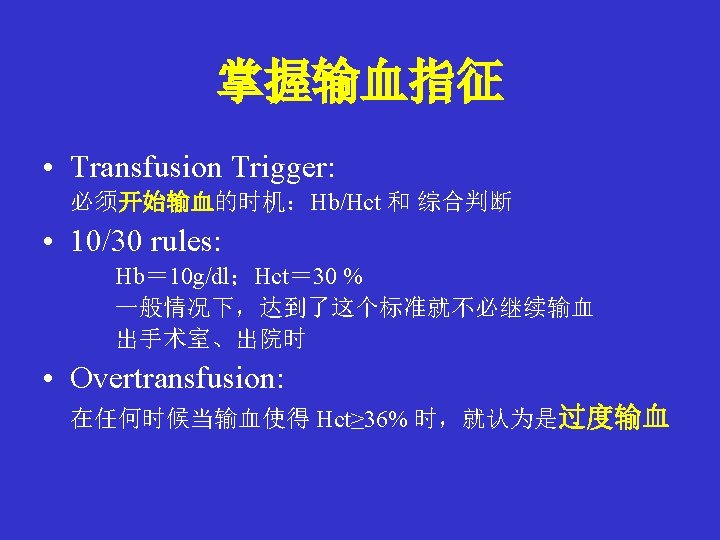

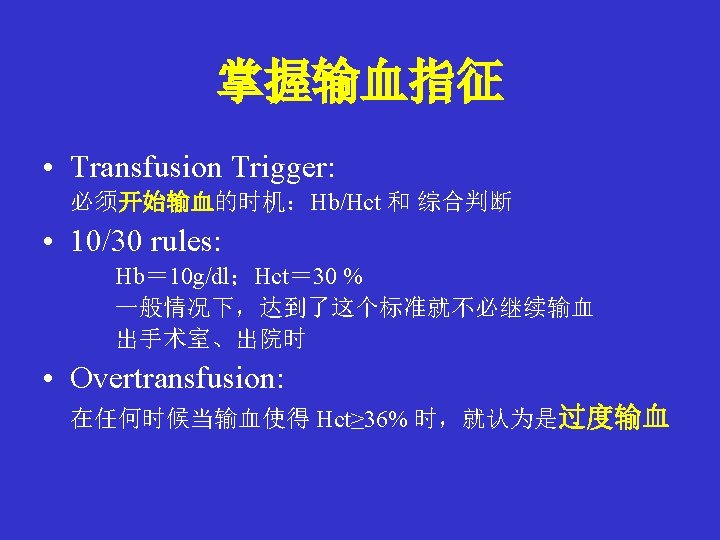
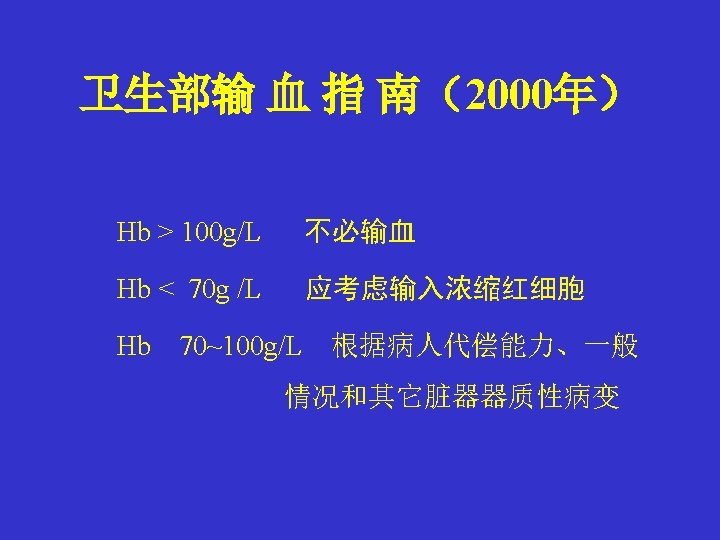
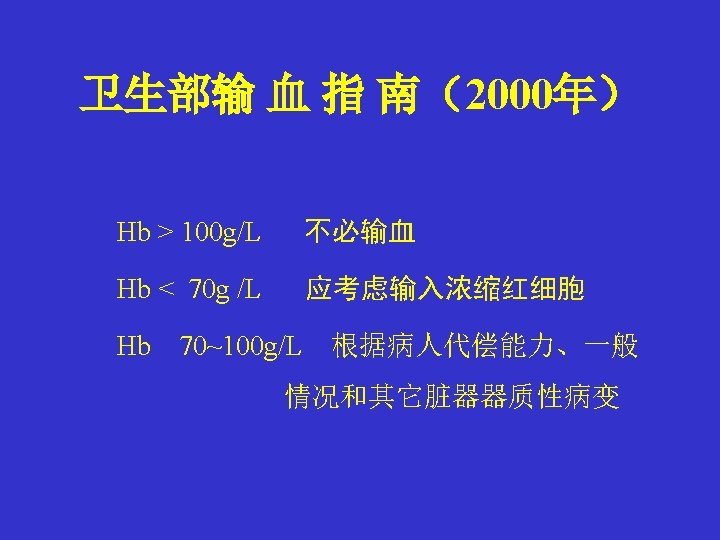
Hb Transfusion Trigger US • 6 g/dl:< 50岁,无心脏病和术后并发症 • 8 g/dl:稳定性的心脏病,失血300 ml • 10 g/dl:老年人,术后有并发症,心肺代偿差 Robertie:Int Anesthesiol Clin 28: 197 -204,1990 • 11 g/dl(Hct 33%):重危病人,强调维持适当 的血容量比输血更重要 Czer and Shoemaker:Optimal hematocrit value in critically ill postoperative patients. Surg Gynecol Obstet 147: 363 -368, 1978
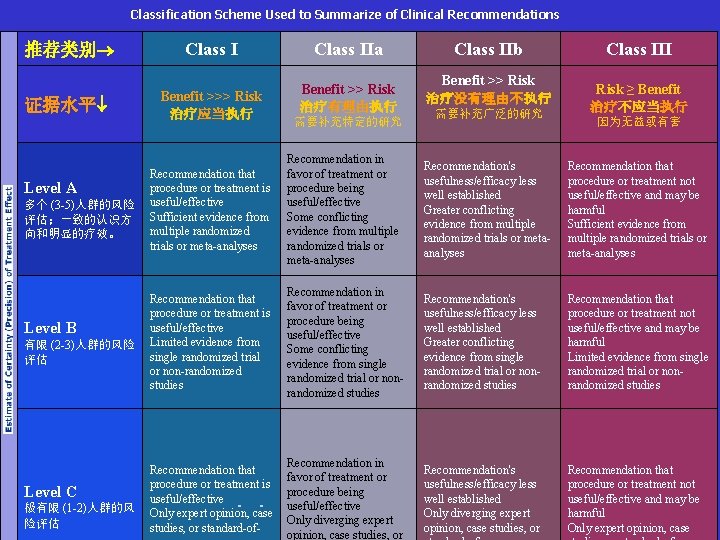
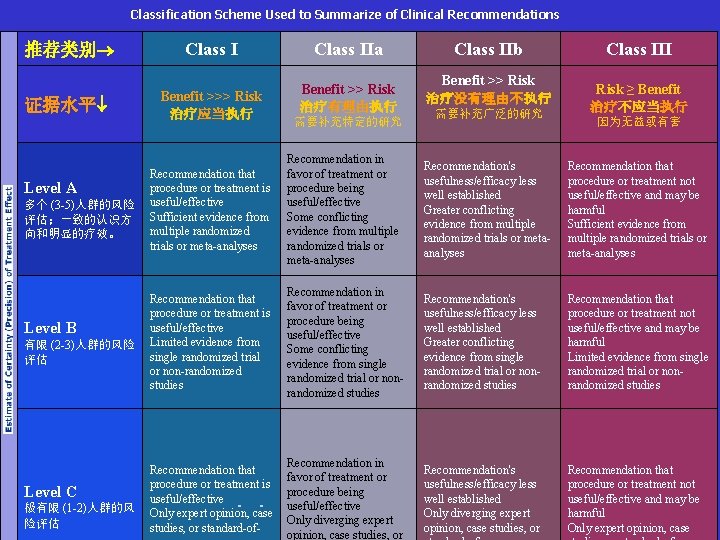
Classification Scheme Used to Summarize of Clinical Recommendations 推荐类别 证据水平 Level A 多个 (3 -5)人群的风险 评估;一致的认识方 向和明显的疗效。 Level B 有限 (2 -3)人群的风险 评估 Level C 极有限 (1 -2)人群的风 险评估 Class I Benefit >>> Risk 治疗应当执行 Class IIa Benefit >> Risk 治疗有理由执行 需要补充特定的研究 Class IIb Benefit >> Risk 治疗没有理由不执行 需要补充广泛的研究 Class III Risk ≥ Benefit 治疗不应当执行 因为无益或有害 Recommendation that procedure or treatment is useful/effective Sufficient evidence from multiple randomized trials or meta-analyses Recommendation in favor of treatment or procedure being useful/effective Some conflicting evidence from multiple randomized trials or meta-analyses Recommendation's usefulness/efficacy less well established Greater conflicting evidence from multiple randomized trials or metaanalyses Recommendation that procedure or treatment not useful/effective and may be harmful Sufficient evidence from multiple randomized trials or meta-analyses Recommendation that procedure or treatment is useful/effective Limited evidence from single randomized trial or non-randomized studies Recommendation in favor of treatment or procedure being useful/effective Some conflicting evidence from single randomized trial or nonrandomized studies Recommendation's usefulness/efficacy less well established Greater conflicting evidence from single randomized trial or nonrandomized studies Recommendation that procedure or treatment not useful/effective and may be harmful Limited evidence from single randomized trial or nonrandomized studies Recommendation that procedure or treatment is useful/effective Only expert opinion, case studies, or standard-of- Recommendation in favor of treatment or procedure being useful/effective Only diverging expert opinion, case studies, or Recommendation's usefulness/efficacy less well established Only diverging expert opinion, case studies, or Recommendation that procedure or treatment not useful/effective and may be harmful Only expert opinion, case
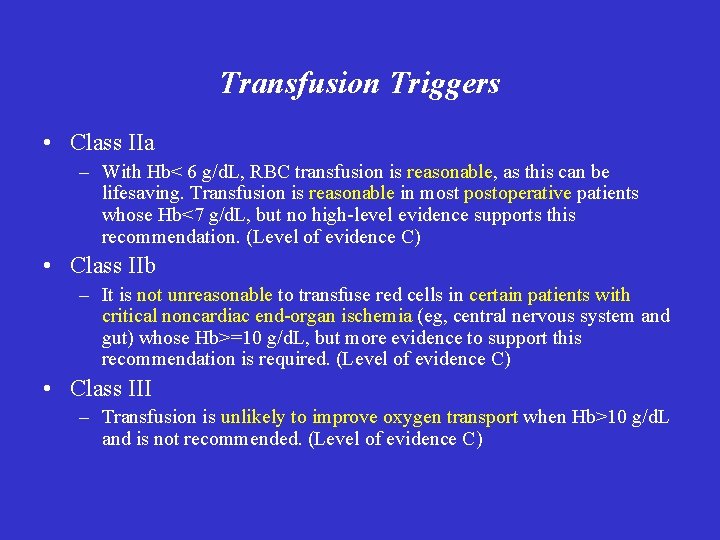
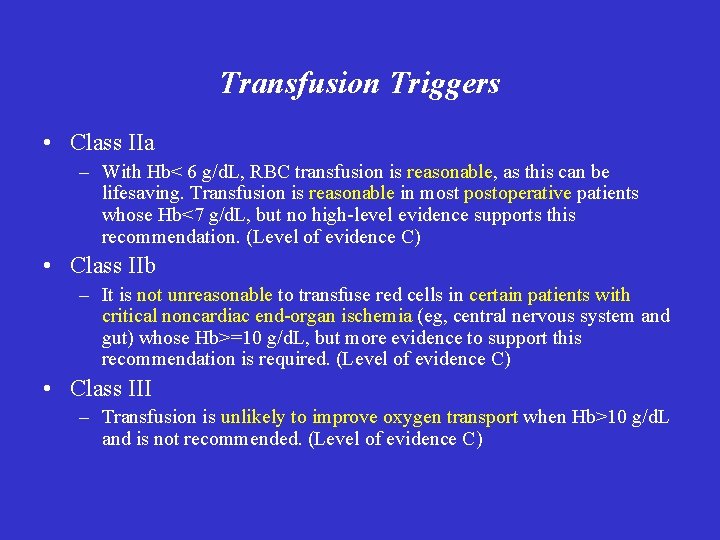
Transfusion Triggers • Class IIa – With Hb< 6 g/d. L, RBC transfusion is reasonable, as this can be lifesaving. Transfusion is reasonable in most postoperative patients whose Hb<7 g/d. L, but no high-level evidence supports this recommendation. (Level of evidence C) • Class IIb – It is not unreasonable to transfuse red cells in certain patients with critical noncardiac end-organ ischemia (eg, central nervous system and gut) whose Hb>=10 g/d. L, but more evidence to support this recommendation is required. (Level of evidence C) • Class III – Transfusion is unlikely to improve oxygen transport when Hb>10 g/d. L and is not recommended. (Level of evidence C)
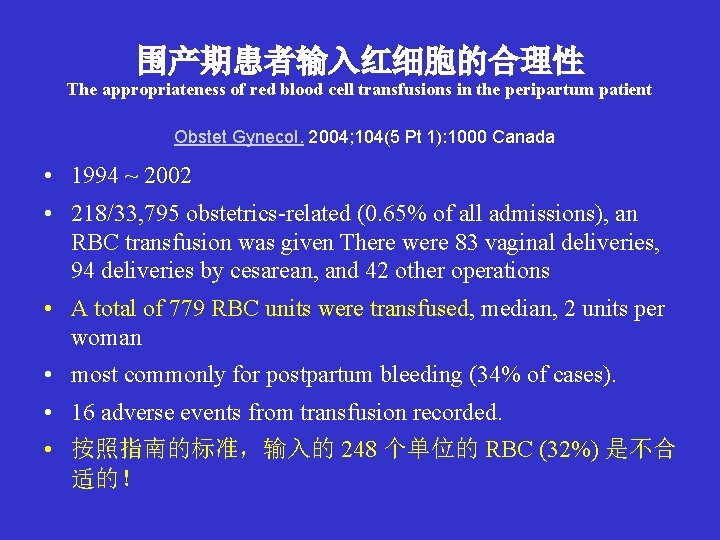
围产期患者输入红细胞的合理性 The appropriateness of red blood cell transfusions in the peripartum patient Obstet Gynecol. 2004; 104(5 Pt 1): 1000 Canada • 1994 ~ 2002 • 218/33, 795 obstetrics-related (0. 65% of all admissions), an RBC transfusion was given There were 83 vaginal deliveries, 94 deliveries by cesarean, and 42 other operations • A total of 779 RBC units were transfused, median, 2 units per woman • most commonly for postpartum bleeding (34% of cases). • 16 adverse events from transfusion recorded. • 按照指南的标准,输入的 248 个单位的 RBC (32%) 是不合 适的!
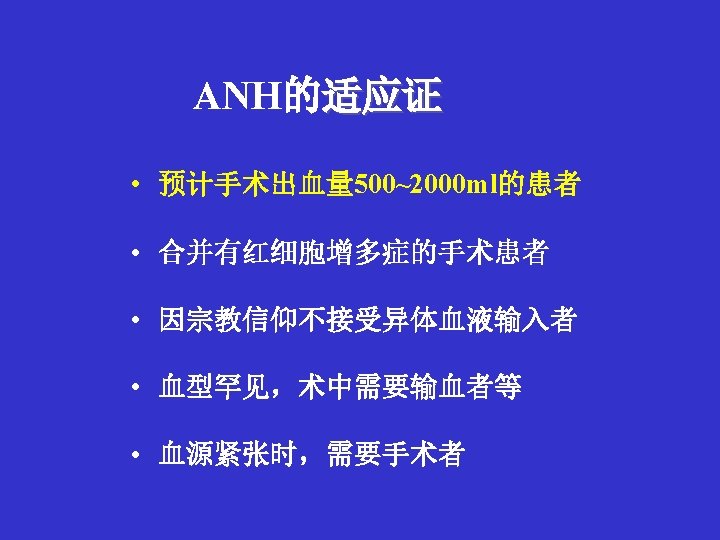
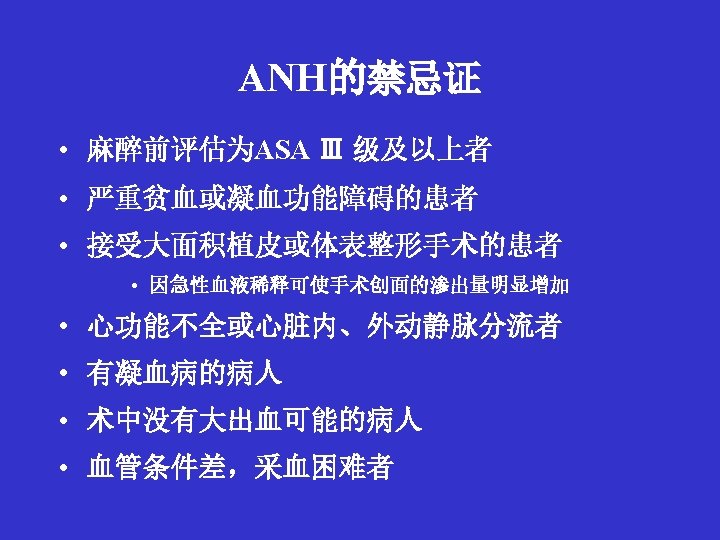
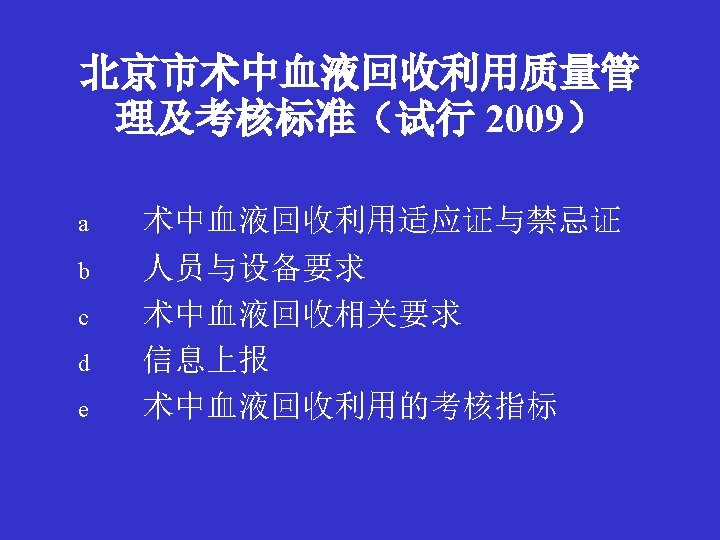
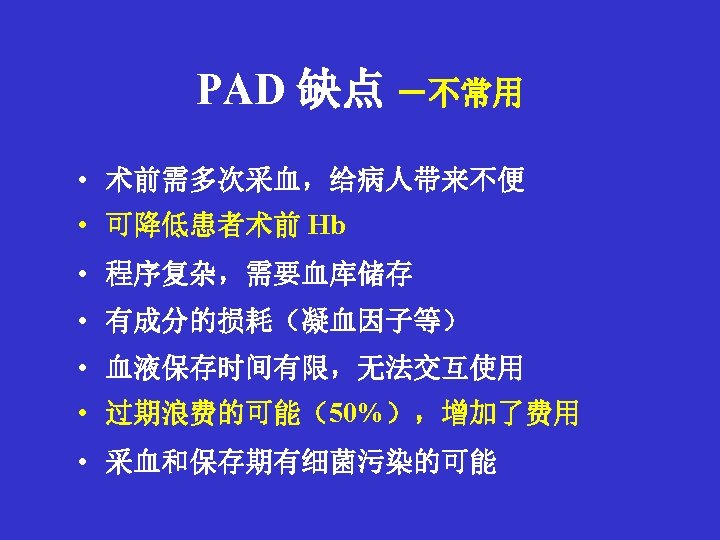
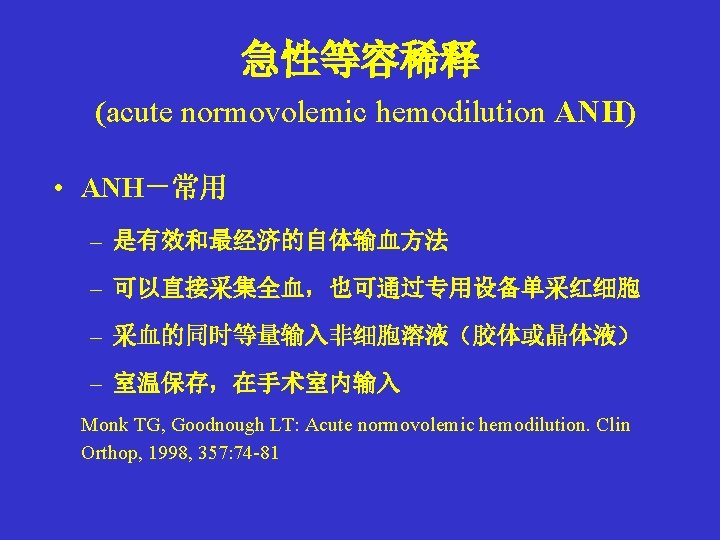
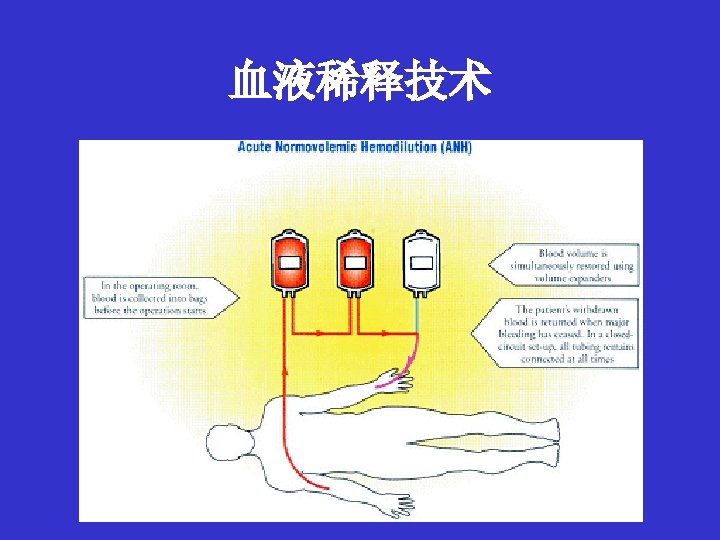
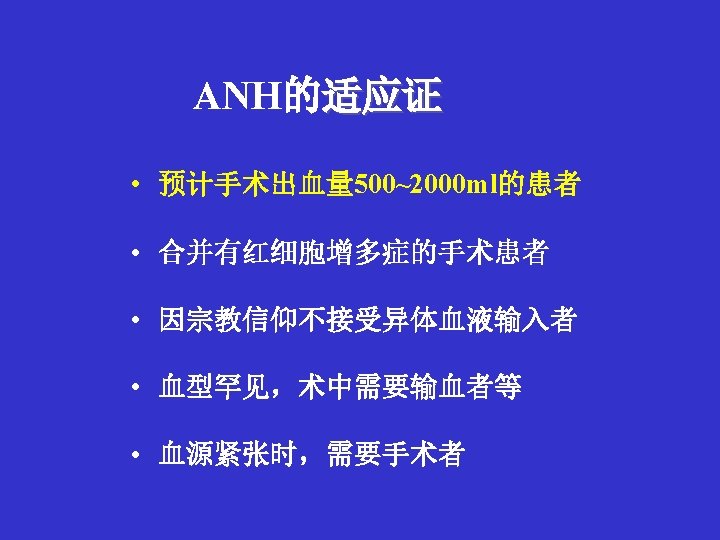
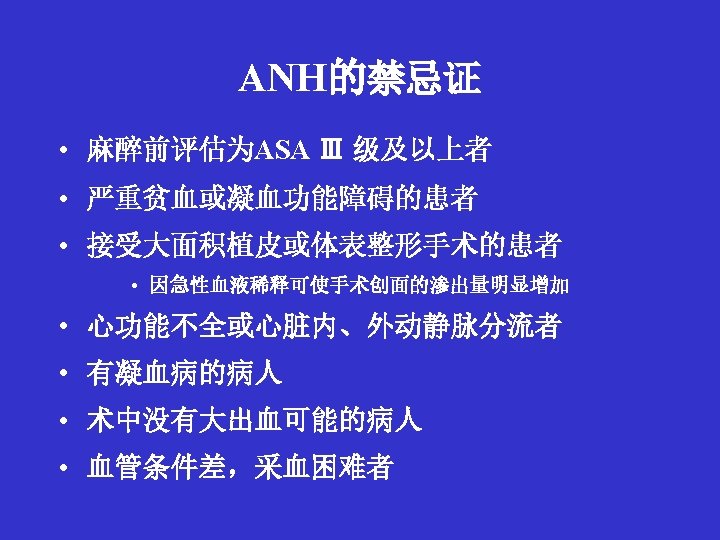
围术期自体输血的种类 • 储存式 • 术前自体献血( Preoperative Autologous Donation PAD) • 急性等容稀释 (Acute Normovolemic Hemodilution ANH) (Intraoperative Autologous Donation) • 急性高容稀释 (Acute Hypervolemic Hemodilution AHH) • 回收式(Blood Salvage BS) • 术中对自体血回收及回输 • 术后对自体血回收及回输
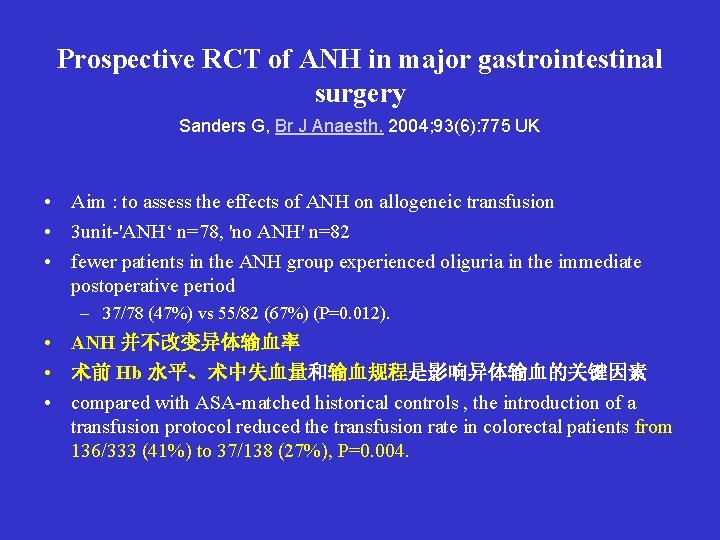
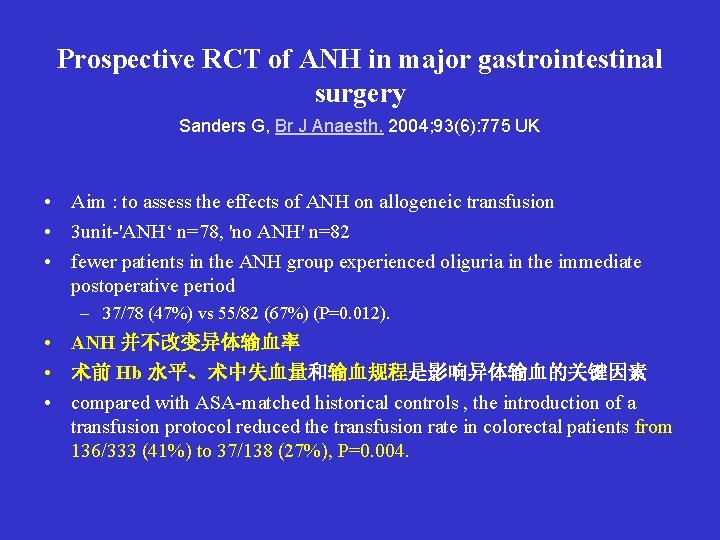
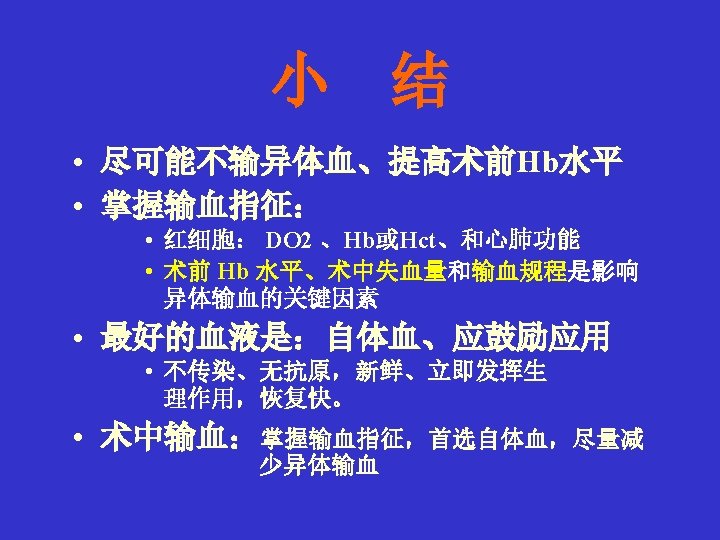
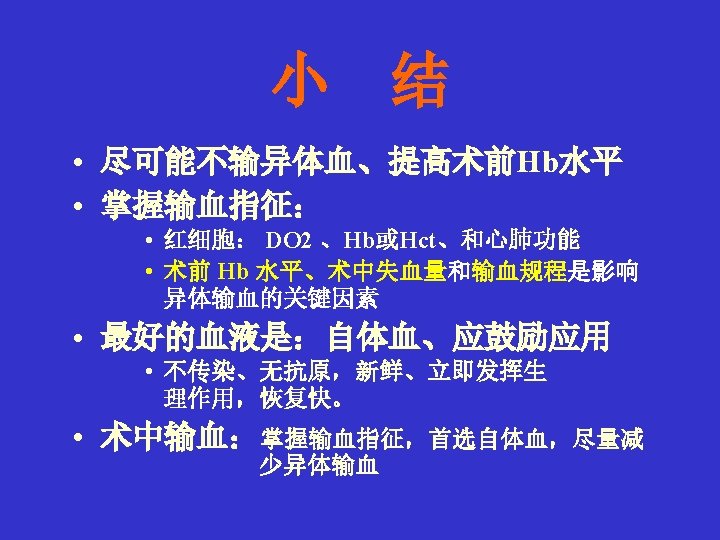
Prospective RCT of ANH in major gastrointestinal surgery Sanders G, Br J Anaesth. 2004; 93(6): 775 UK • Aim : to assess the effects of ANH on allogeneic transfusion • 3 unit-'ANH‘ n=78, 'no ANH' n=82 • fewer patients in the ANH group experienced oliguria in the immediate postoperative period – 37/78 (47%) vs 55/82 (67%) (P=0. 012). • ANH 并不改变异体输血率 • 术前 Hb 水平、术中失血量和输血规程是影响异体输血的关键因素 • compared with ASA-matched historical controls , the introduction of a transfusion protocol reduced the transfusion rate in colorectal patients from 136/333 (41%) to 37/138 (27%), P=0. 004.
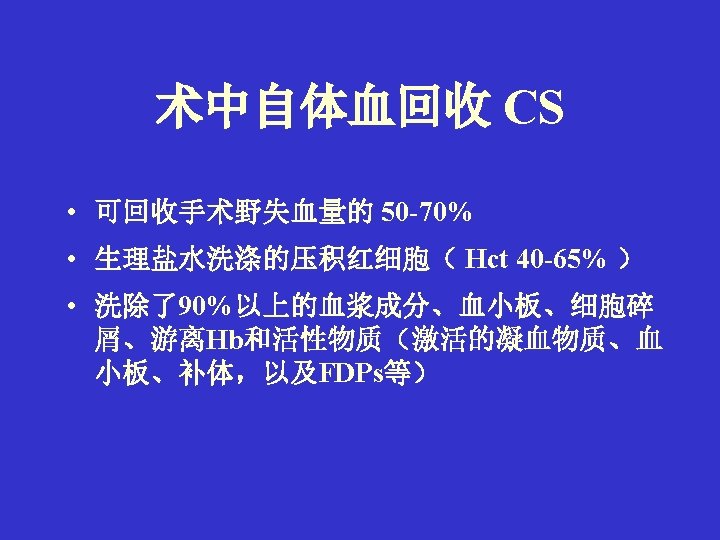
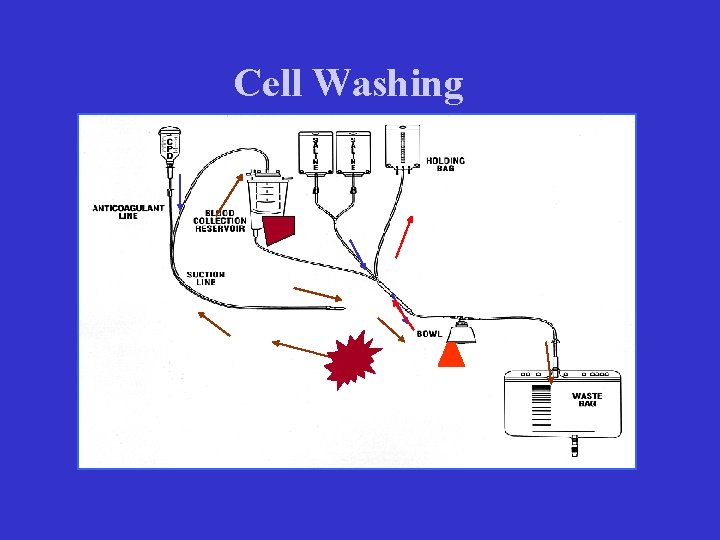
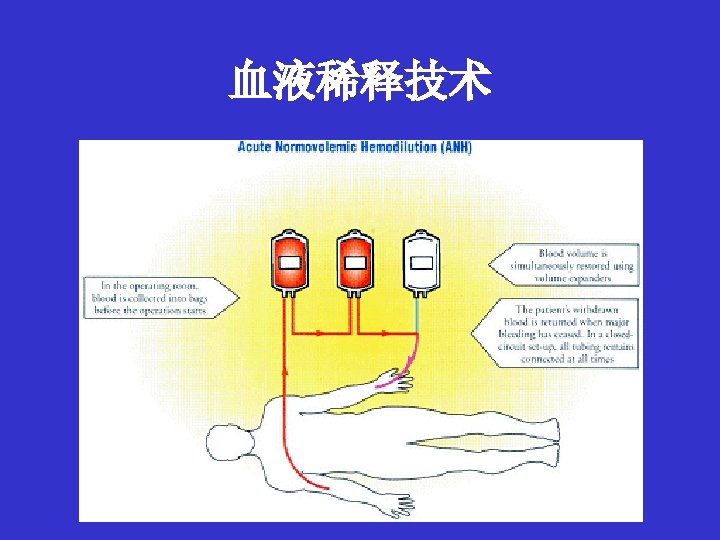
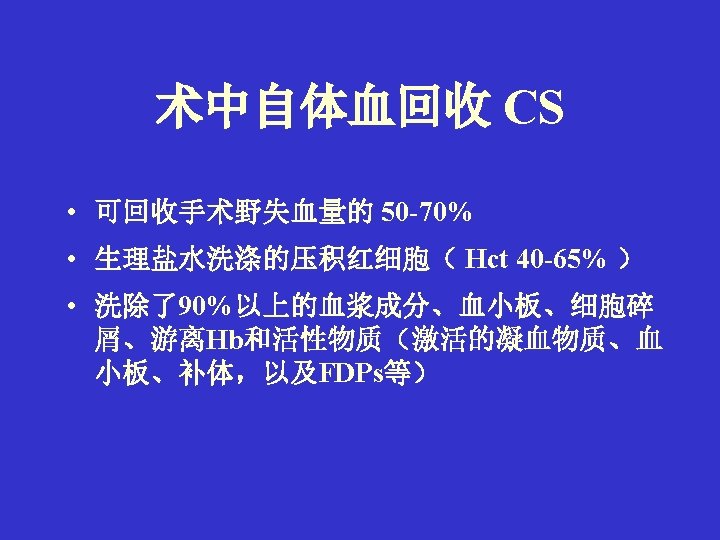
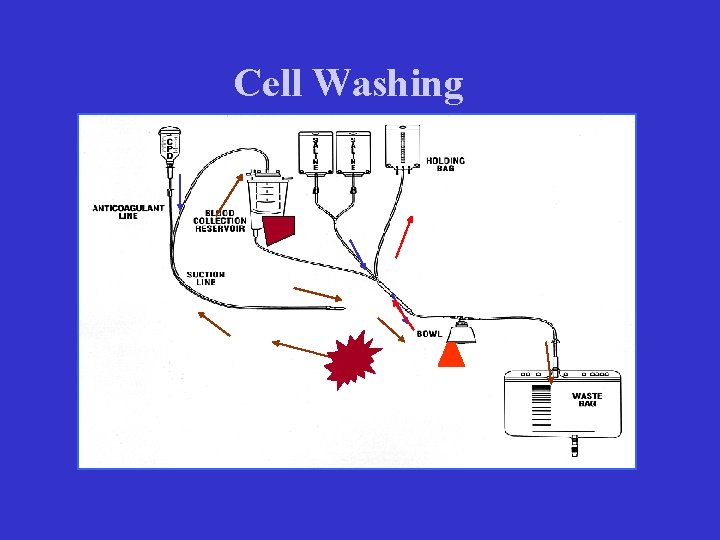
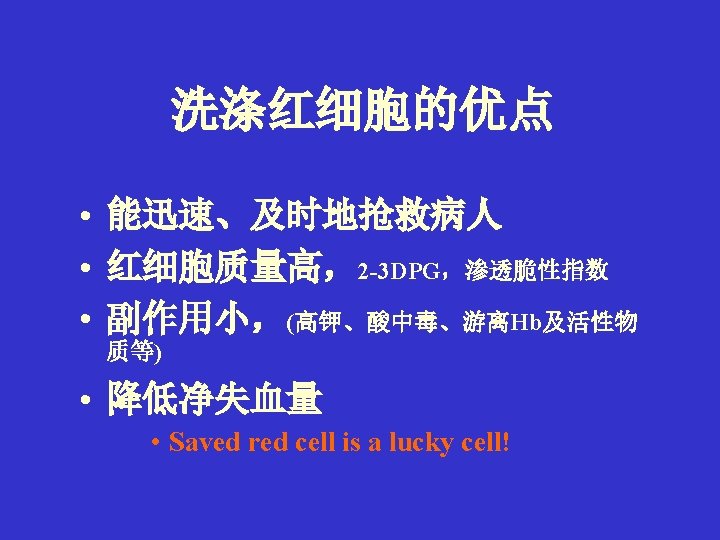
Cell Washing
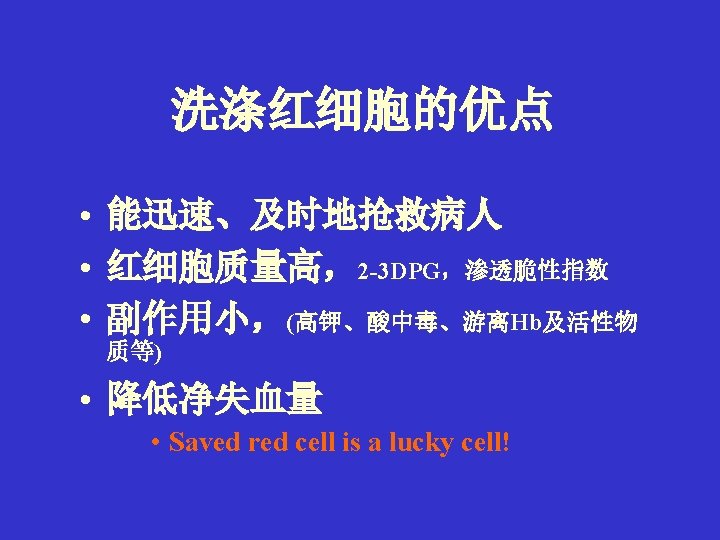
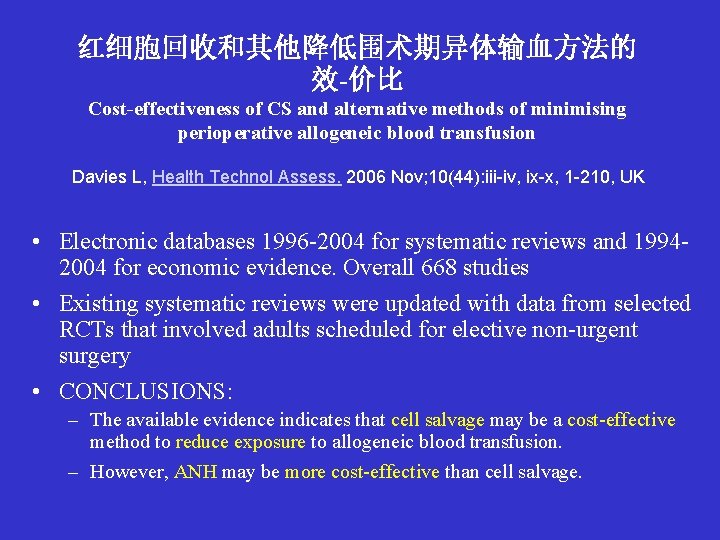
红细胞回收和其他降低围术期异体输血方法的 效-价比 Cost-effectiveness of CS and alternative methods of minimising perioperative allogeneic blood transfusion Davies L, Health Technol Assess. 2006 Nov; 10(44): iii-iv, ix-x, 1 -210, UK • Electronic databases 1996 -2004 for systematic reviews and 19942004 for economic evidence. Overall 668 studies • Existing systematic reviews were updated with data from selected RCTs that involved adults scheduled for elective non-urgent surgery • CONCLUSIONS: – The available evidence indicates that cell salvage may be a cost-effective method to reduce exposure to allogeneic blood transfusion. – However, ANH may be more cost-effective than cell salvage.
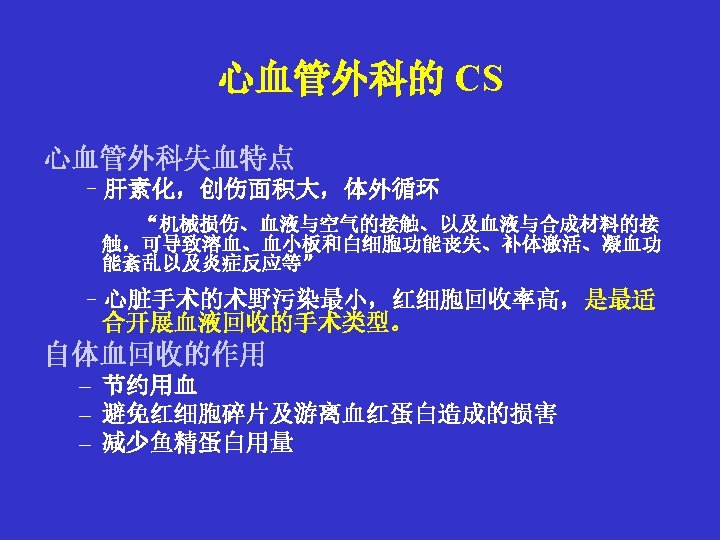
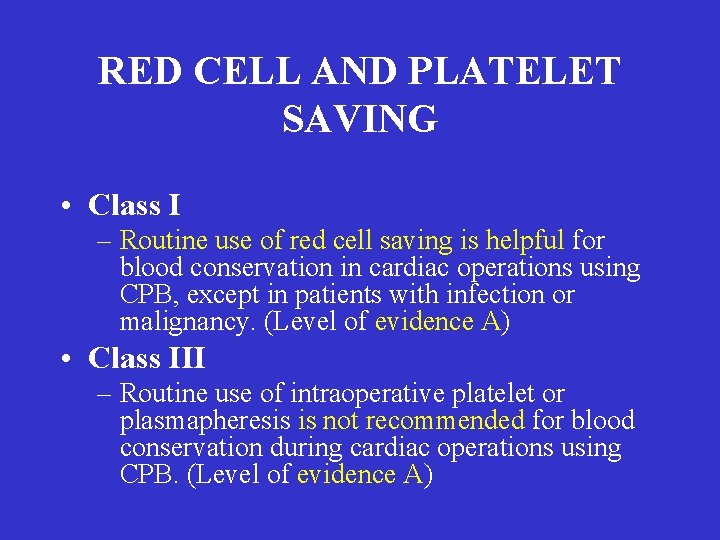
RED CELL AND PLATELET SAVING • Class I – Routine use of red cell saving is helpful for blood conservation in cardiac operations using CPB, except in patients with infection or malignancy. (Level of evidence A) • Class III – Routine use of intraoperative platelet or plasmapheresis is not recommended for blood conservation during cardiac operations using CPB. (Level of evidence A)

The End