TISSUE REPAIR REGENERATION HEALING DEFINITIONS REPAIR Restoration of













- Slides: 54

TISSUE REPAIR REGENERATION / HEALING
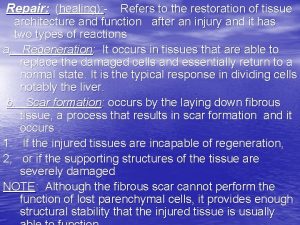
DEFINITIONS: REPAIR: Restoration of normal structure and function of tissues. • For parenchymal and connective tissue. HEALING: For surface epithelium.
REPAIR • Repair of damaged tissue occurs by • 1 - regeneration by proliferation of uninjured cells and maturation of stem cells. • 2 -deposition of connective tissue to form scar.
REGENERATION • Replacement of lost structures • Is dependent on the type of normal turnover the original tissue has, skin, intestine. • Mammals have limited ability to regenerate.
Scar/ CT deposit • If the tissue damage is severe: Connective tissue(fibrous) is laid down to end in scar formation. • Fibrosis, as one of the 3 possible outcomes of inflammation, follows “healing” • Fibrosis + inflammation= organization. Both regeneration and Fibrosis occur simultaneously.

Cell Population Fates • PROLIFERATION – Hormonal, especially steroid hormones – eg. , EPO, CSF • DIFFERENTIATION * – UNIDIRECTIONAL, GAIN (specialization) and LOSS (versatility) • APOPTOSIS *One of the most KEY concepts in neoplasia
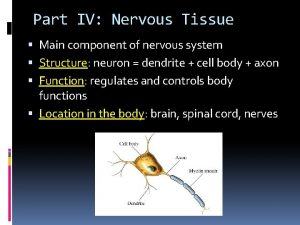
CELL TYPES • Labile/dividing: eg. , marrow, GI • Stable/Quiescent: liver, kidney • NON-mitotic/permanant: neuron, striated muscle
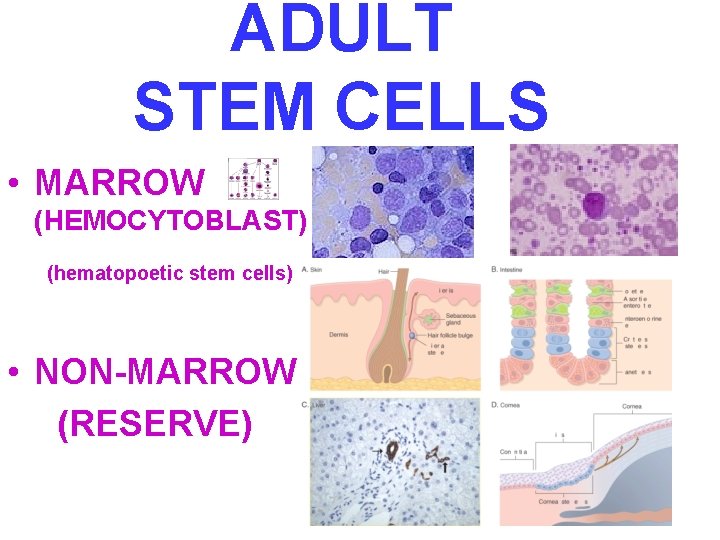
ADULT STEM CELLS • MARROW (HEMOCYTOBLAST) (hematopoetic stem cells) • NON-MARROW (RESERVE)
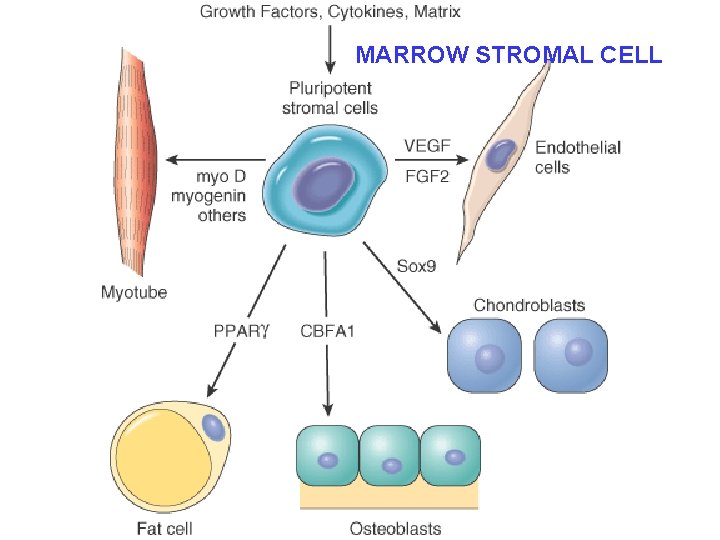
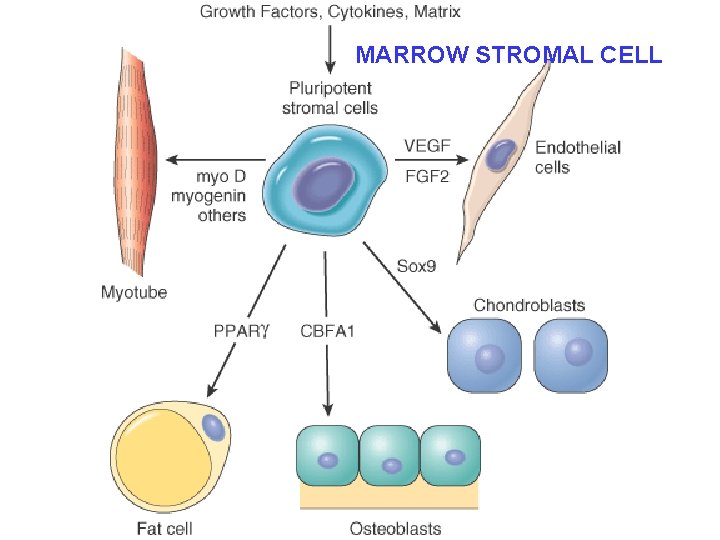
MARROW STROMAL CELL
Growth Factors (GFs) • Polypeptides • Cytokines • LOCOMOTION • CONTRACTILITY • DIFFERENTIATION • ANGIOGENESIS

Growth Factors (GFs) • • Epidermal Transforming (alpha, beta) Hepatocyte Vascular Endothelial Platelet Derived Fibroblast Keratinocyte Cytokines (TNF, IL-1, Interferons)

CELL PLAYERS (source AND targets) • • Lymphocytes, especially T-cells Macrophages Platelets Endothelial cells Fibroblasts Keratinocytes “Mesenchymal” cells Smooth muscle cells
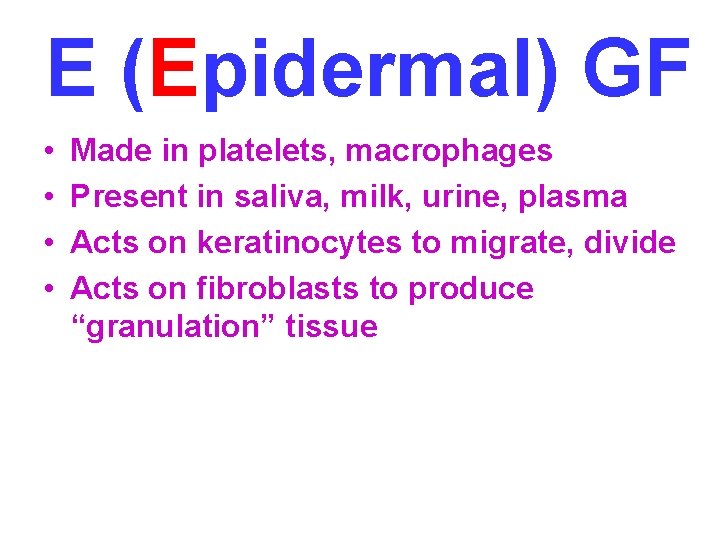
E (Epidermal) GF • • Made in platelets, macrophages Present in saliva, milk, urine, plasma Acts on keratinocytes to migrate, divide Acts on fibroblasts to produce “granulation” tissue
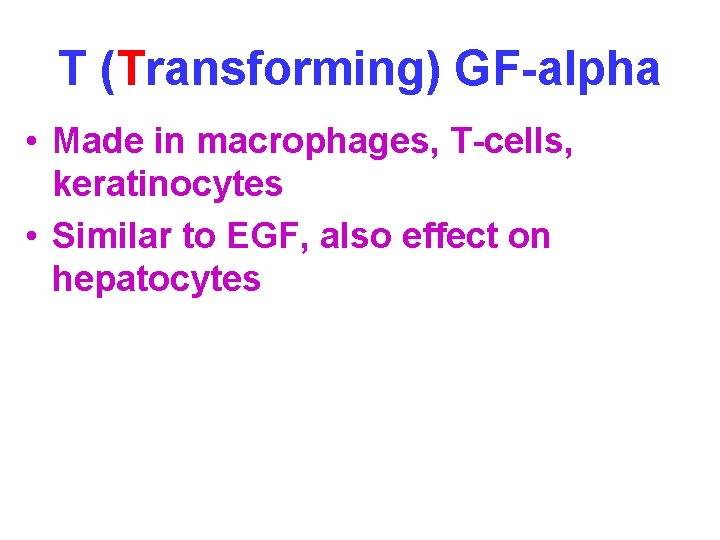
T (Transforming) GF-alpha • Made in macrophages, T-cells, keratinocytes • Similar to EGF, also effect on hepatocytes
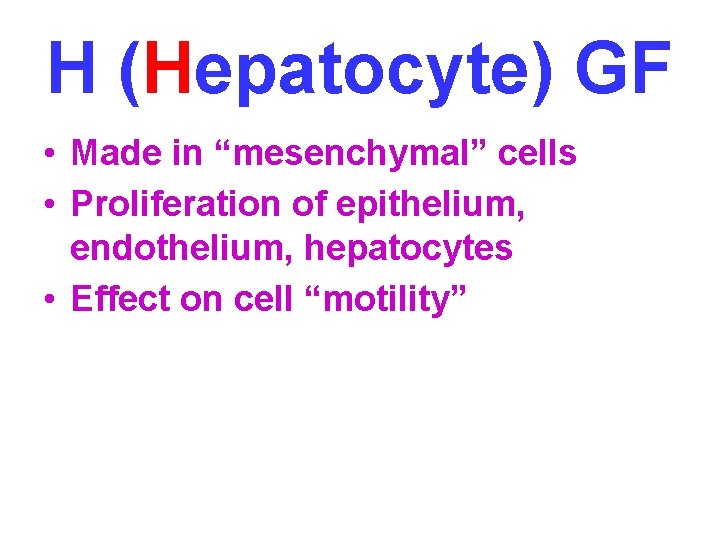
H (Hepatocyte) GF • Made in “mesenchymal” cells • Proliferation of epithelium, endothelium, hepatocytes • Effect on cell “motility”
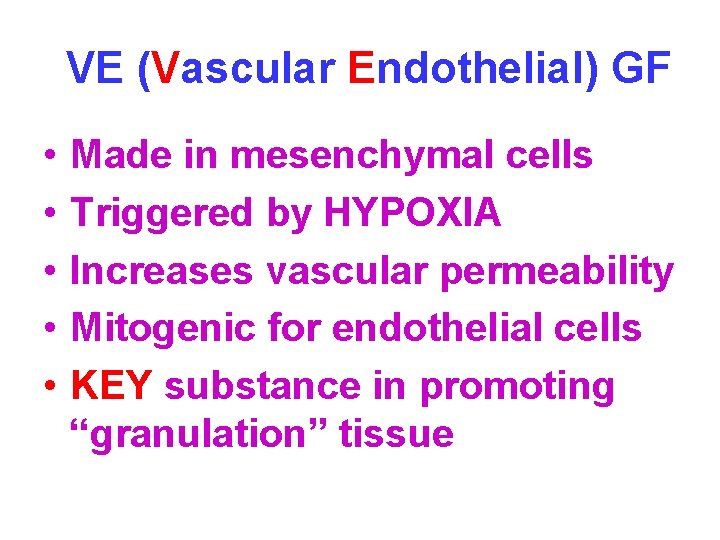
VE (Vascular Endothelial) GF • • • Made in mesenchymal cells Triggered by HYPOXIA Increases vascular permeability Mitogenic for endothelial cells KEY substance in promoting “granulation” tissue
PD (Platelet Derived) GF • Made in platelets, but also MANY other cell types • Chemotactic for MANY cells • Mitogen for fibroblasts • Angiogenesis • Another KEY player in granulation tissue

F (Fibroblast) GF • Made in MANY cells • Chemotactic and mitogenic, for fibroblasts and keratinocytes • Re-epithelialization • Angiogenesis, wound contraction • Hematopoesis • Cardiac/Skeletal (striated) muscle
T (Transforming) GF-beta • Made in MANY CELLS • Chemotactic for PMNs and MANY other types of cells • Inhibits epithelial cells • Fibrogenic • Anti-Inflammatory
K (Keratinocyte) GF • Made in fibroblasts • Stimulates keratinocytes: – Migration – Proliferation – Differentiation
I (Insulin-like) GF-1 • Made in macrophages, fibroblasts • Stimulates: – Sulfated proteoglycans – Collagen – Keratinocyte migration – Fibroblast proliferation • Action similar to GH (Pituitary Growth Hormone)
TNF (Tumor Necrosis Factor) • Made in macrophages, mast cells, T-cells • Activates macrophages (cachexin) • KEY influence on other cytokines • The MAJOR TNF is TNF-alpha
Interleukins • Made in macrophages, mast cells, T-cells, but also MANY other cells • MANY functions: – Chemotaxis – Angiogenesis – REGULATION of other cytokines
INTERFERONS • Made by lymphocytes, fibroblasts • Activates MACROPHAGES • Inhibits FIBROBLASTS • REGULATES other cytokines
SIGNALING • Autocrine (same cell) • Paracrine (next door neighbor) (many GFs) • Endocrine (far away, delivered by blood, steroid hormones)

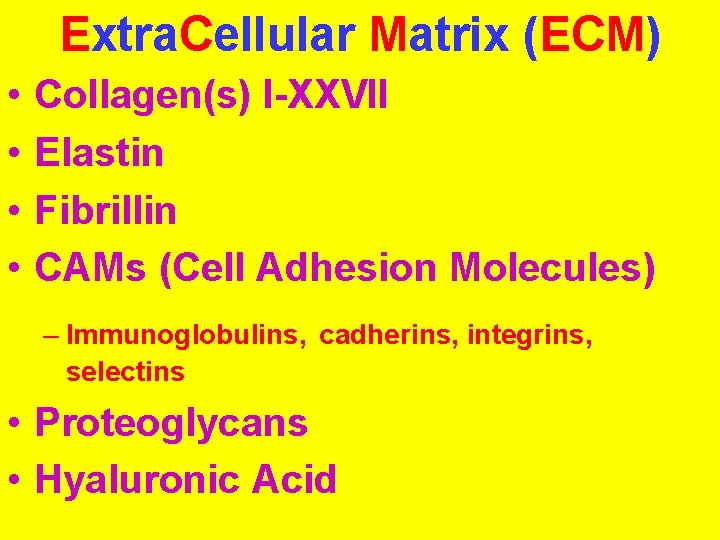
Extra. Cellular Matrix (ECM) • • Collagen(s) I-XXVII Elastin Fibrillin CAMs (Cell Adhesion Molecules) – Immunoglobulins, cadherins, integrins, selectins • Proteoglycans • Hyaluronic Acid
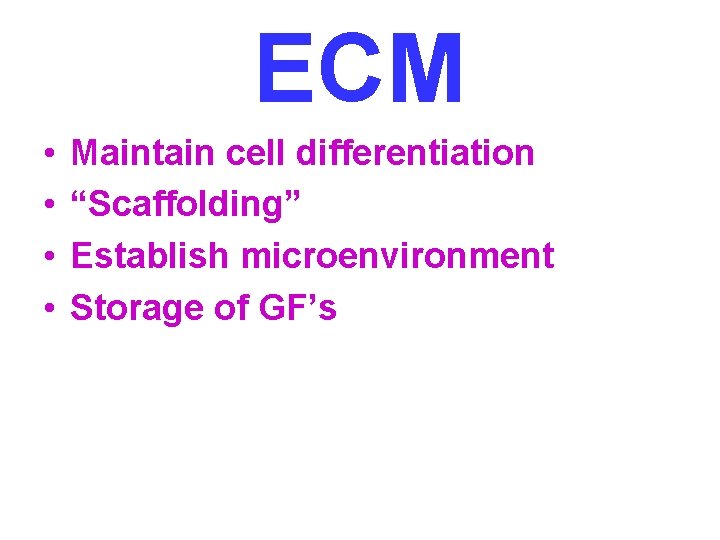
ECM • • Maintain cell differentiation “Scaffolding” Establish microenvironment Storage of GF’s
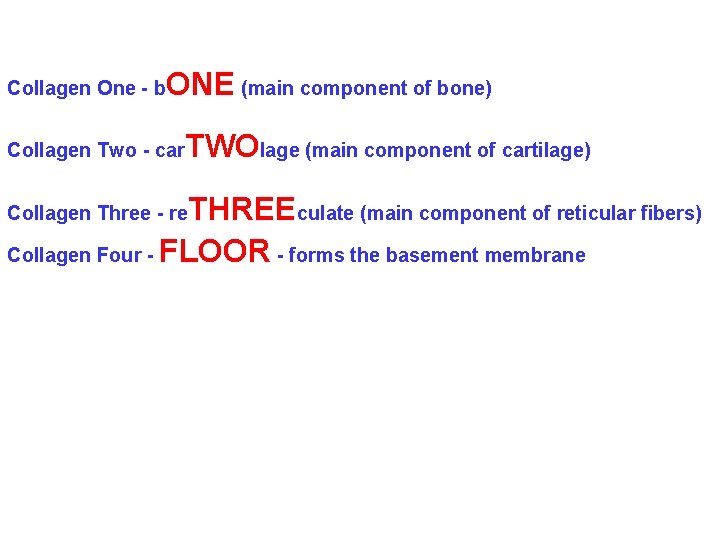
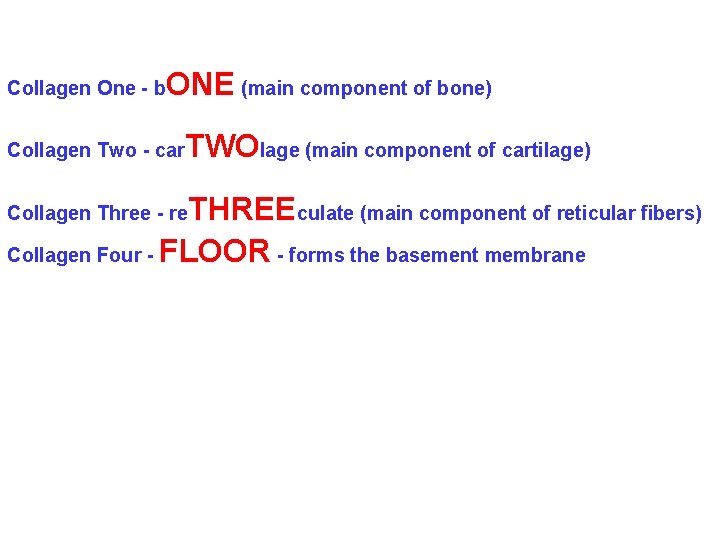
Collagen One - b ONE (main component of bone) Collagen Two - car TWOlage (main component of cartilage) THREEculate (main component of reticular fibers) Collagen Four - FLOOR - forms the basement membrane Collagen Three - re
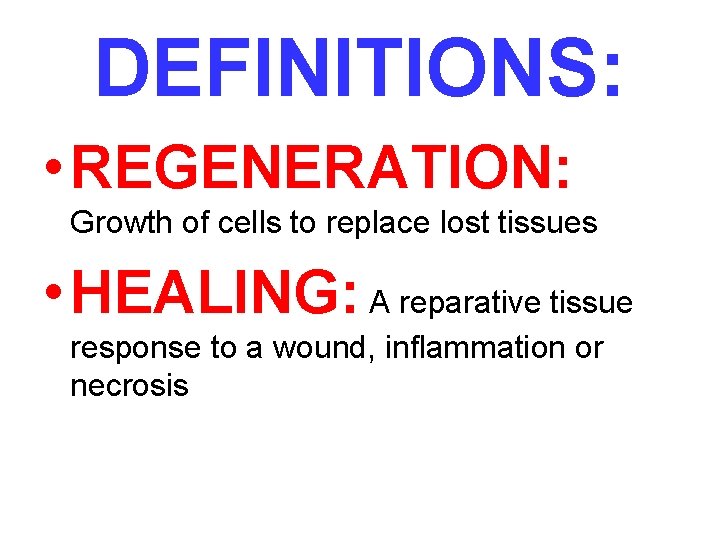
DEFINITIONS: • REGENERATION: Growth of cells to replace lost tissues • HEALING: A reparative tissue response to a wound, inflammation or necrosis
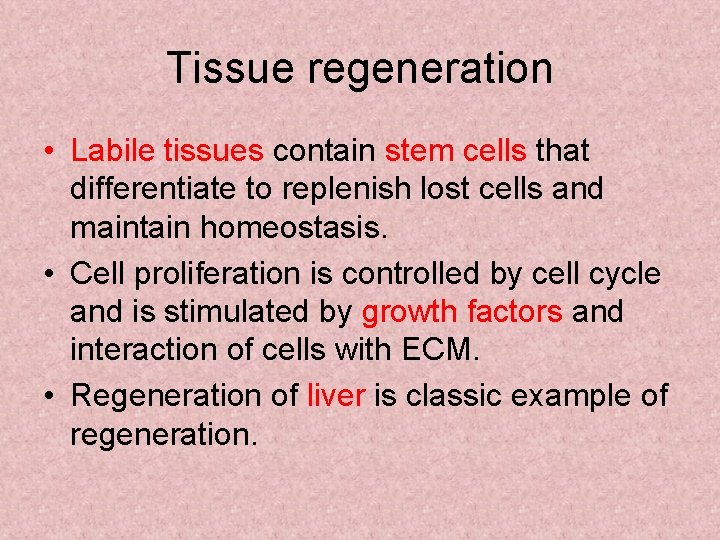
Tissue regeneration • Labile tissues contain stem cells that differentiate to replenish lost cells and maintain homeostasis. • Cell proliferation is controlled by cell cycle and is stimulated by growth factors and interaction of cells with ECM. • Regeneration of liver is classic example of regeneration.
Prometheus, Zeus.
Liver regeneration. • After resection, IL-6 primes hepatocytes to receive new cells. • Growth factors and cytokines push hepatocytes into cell cycle and later divide kupffer cells, endothelial and stellate cells. • In last termination phase, hepatocytes return to quiescent phase.
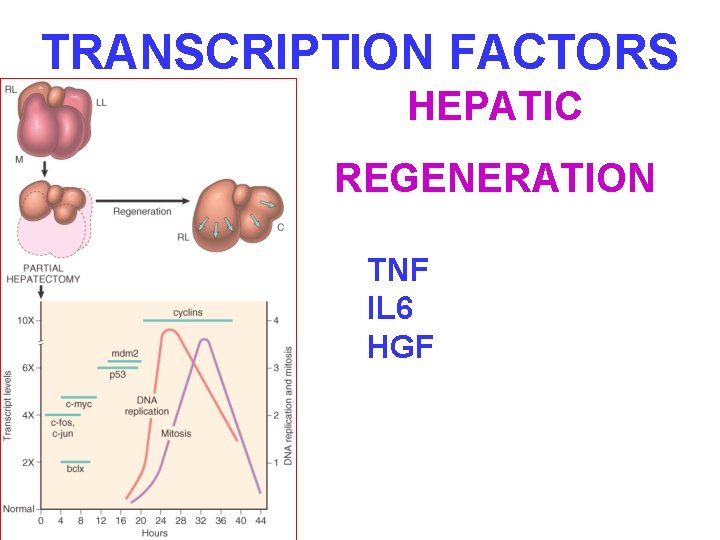
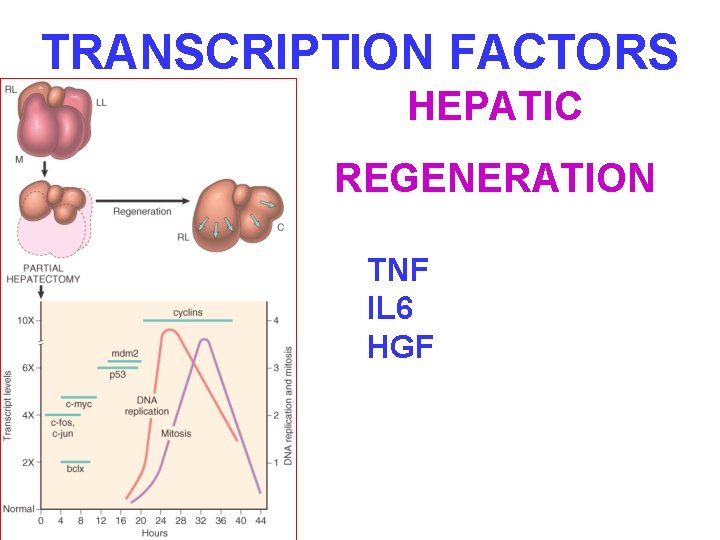
TRANSCRIPTION FACTORS HEPATIC REGENERATION TNF IL 6 HGF

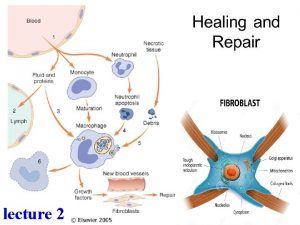
HEALING/REPAIR • FOLLOWS INFLAMMATION • PROLIFERATION and MIGRATION of connective tissue cells • ANGIOGENESIS (Neovascularization) • Collagen, other ECM protein synthesis • Tissue Remodeling • Wound contraction • Increase in wound strength (scar = fibrosis)
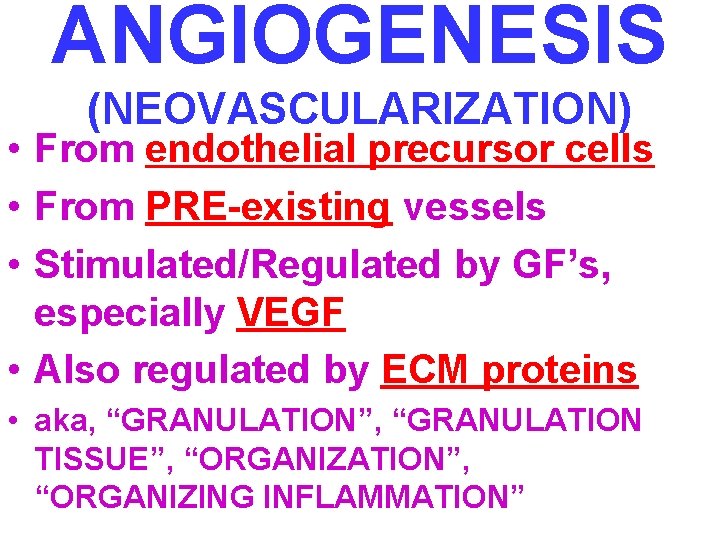
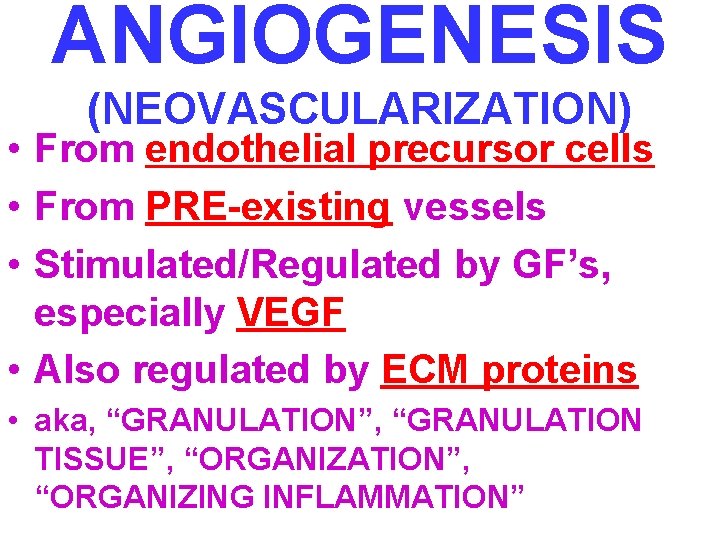
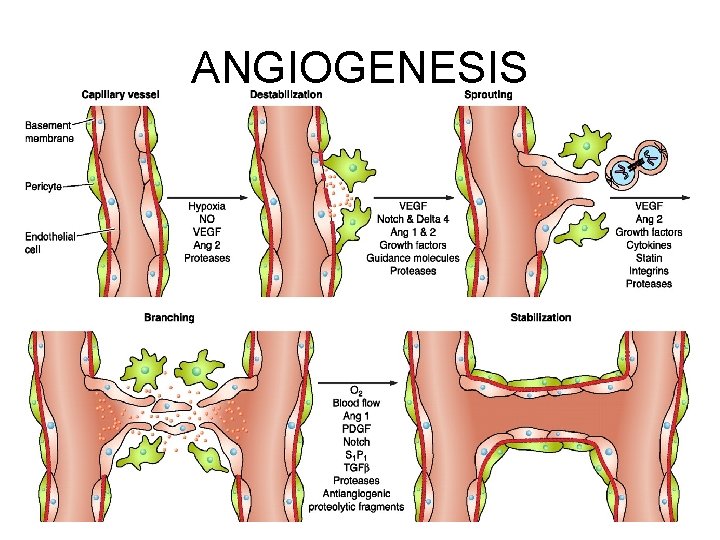
ANGIOGENESIS (NEOVASCULARIZATION) • From endothelial precursor cells • From PRE-existing vessels • Stimulated/Regulated by GF’s, especially VEGF • Also regulated by ECM proteins • aka, “GRANULATION”, “GRANULATION TISSUE”, “ORGANIZATION”, “ORGANIZING INFLAMMATION”
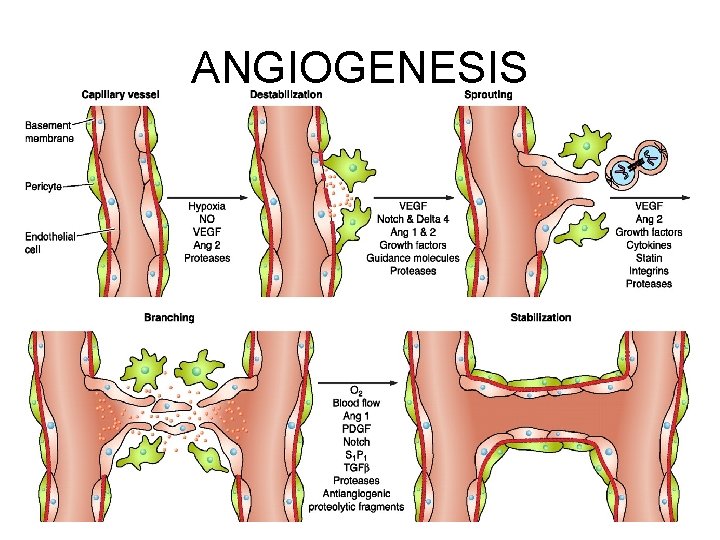
ANGIOGENESIS
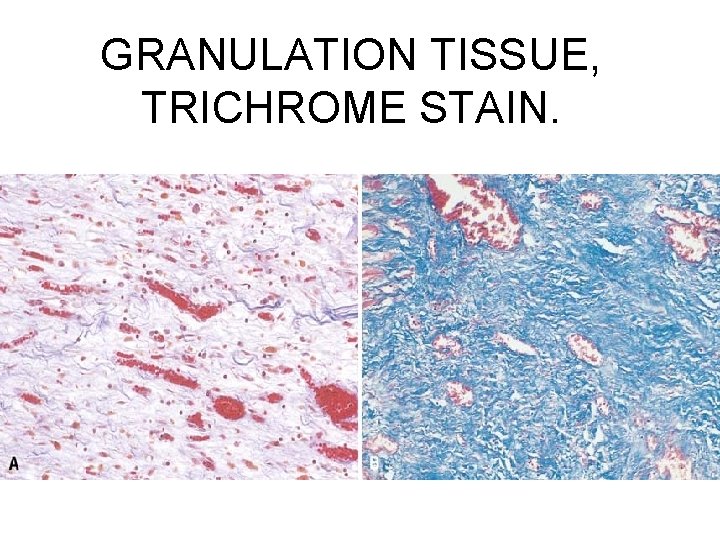
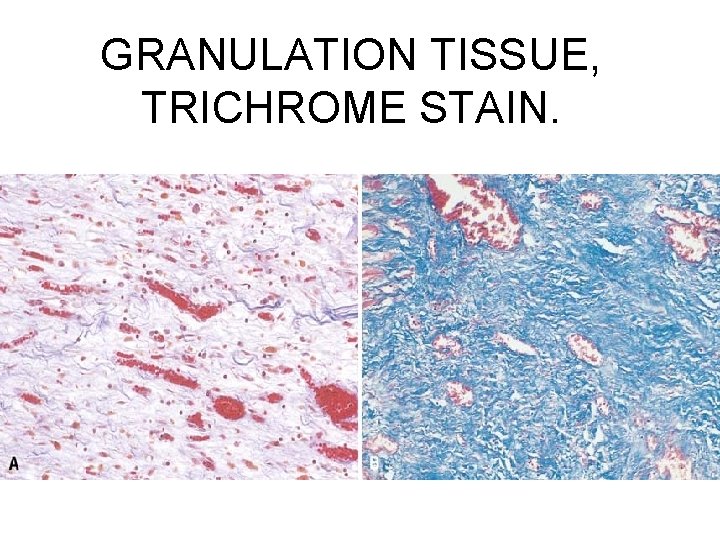
GRANULATION TISSUE, TRICHROME STAIN.


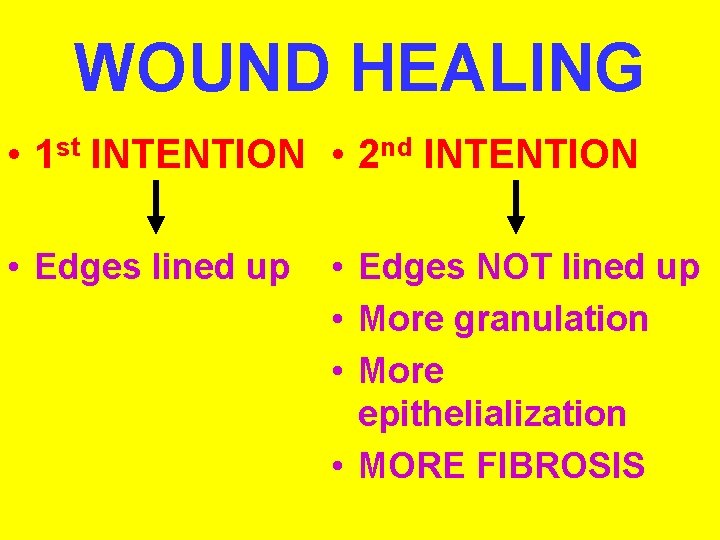
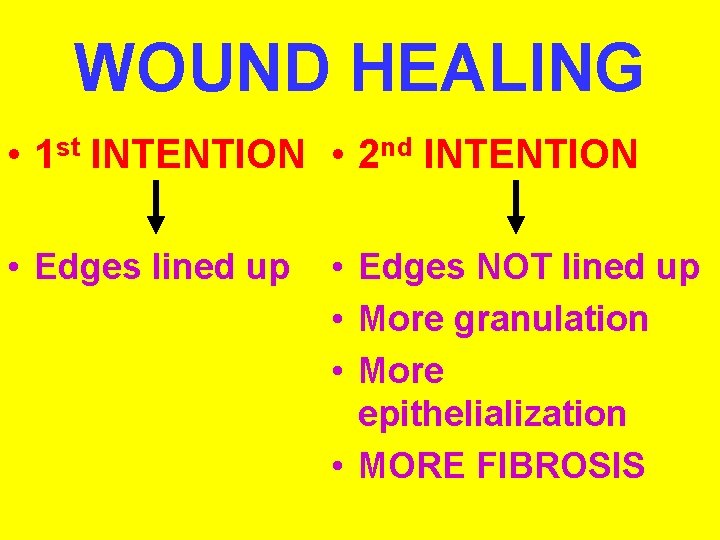
WOUND HEALING • 1 st INTENTION • 2 nd INTENTION • Edges lined up • Edges NOT lined up • More granulation • More epithelialization • MORE FIBROSIS
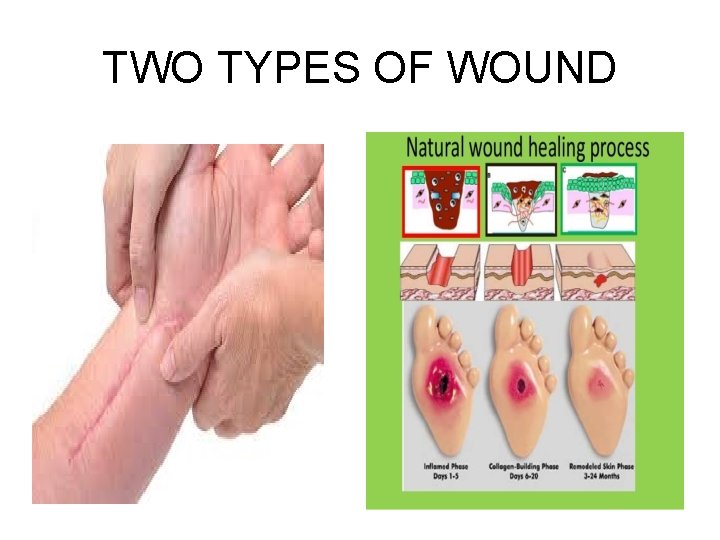
TWO TYPES OF WOUND
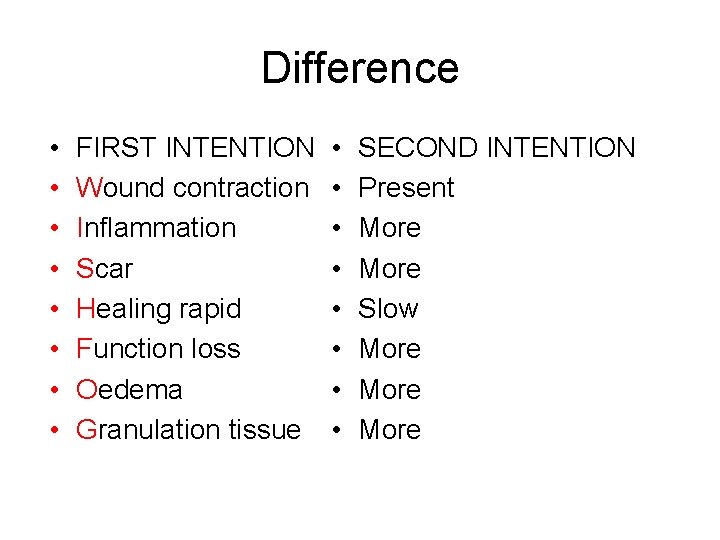
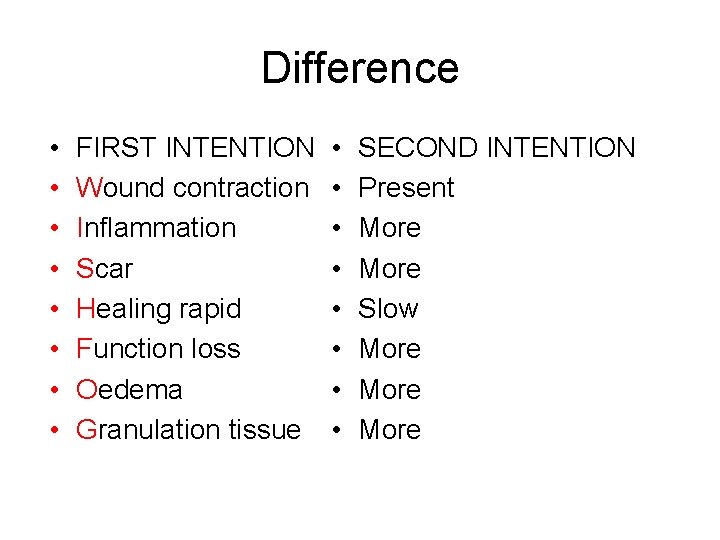
Difference • • FIRST INTENTION Wound contraction Inflammation Scar Healing rapid Function loss Oedema Granulation tissue • • SECOND INTENTION Present More Slow More


“HEALTHY” Granulation Tissue
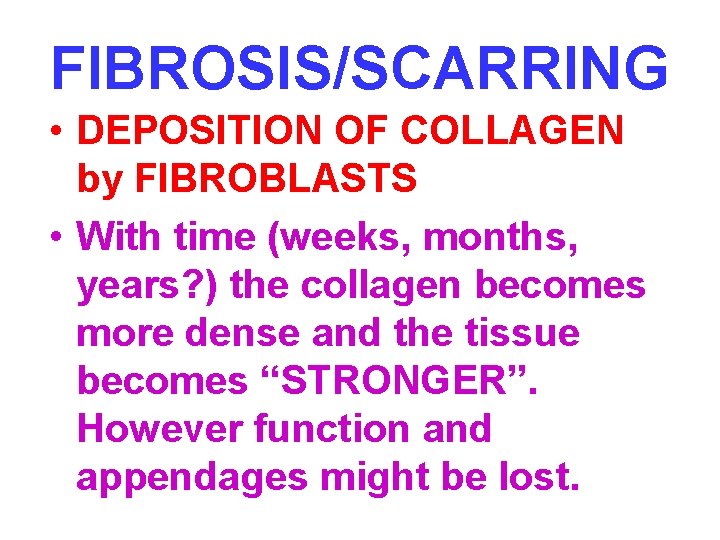
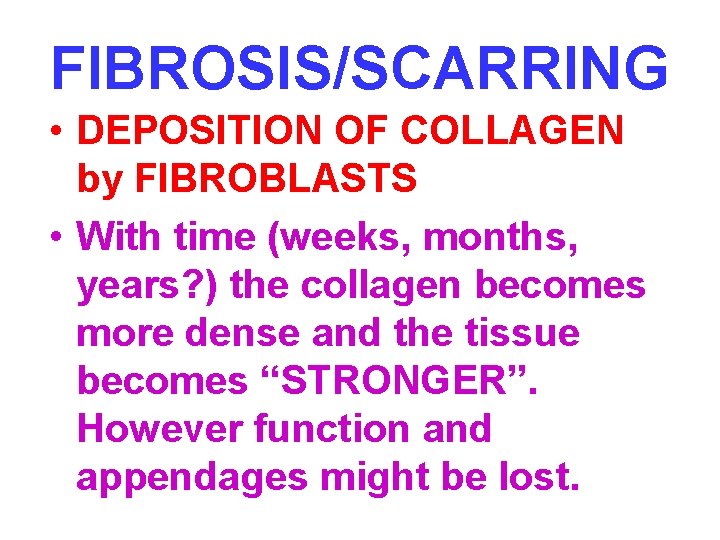
FIBROSIS/SCARRING • DEPOSITION OF COLLAGEN by FIBROBLASTS • With time (weeks, months, years? ) the collagen becomes more dense and the tissue becomes “STRONGER”. However function and appendages might be lost.
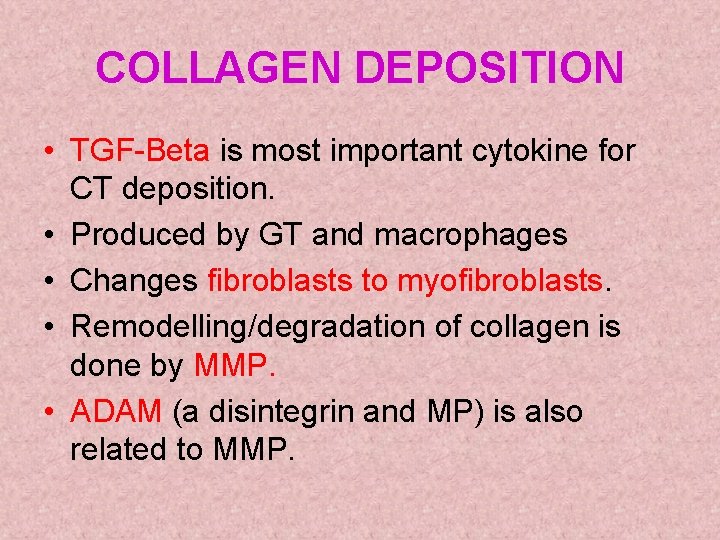
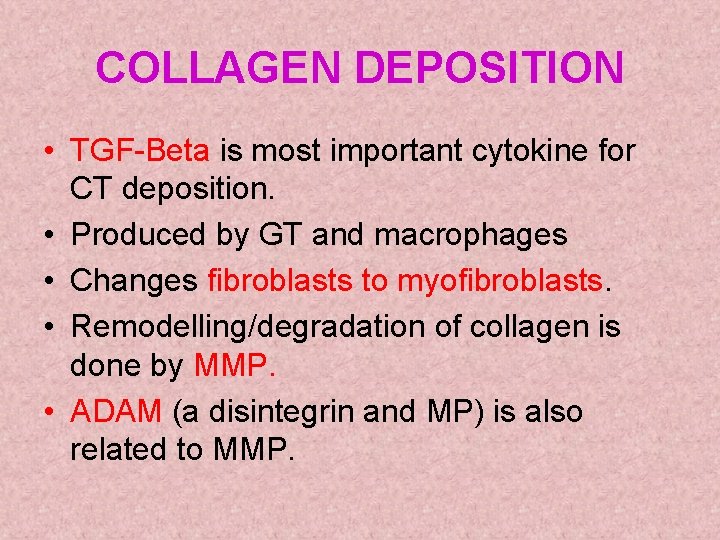
COLLAGEN DEPOSITION • TGF-Beta is most important cytokine for CT deposition. • Produced by GT and macrophages • Changes fibroblasts to myofibroblasts. • Remodelling/degradation of collagen is done by MMP. • ADAM (a disintegrin and MP) is also related to MMP.
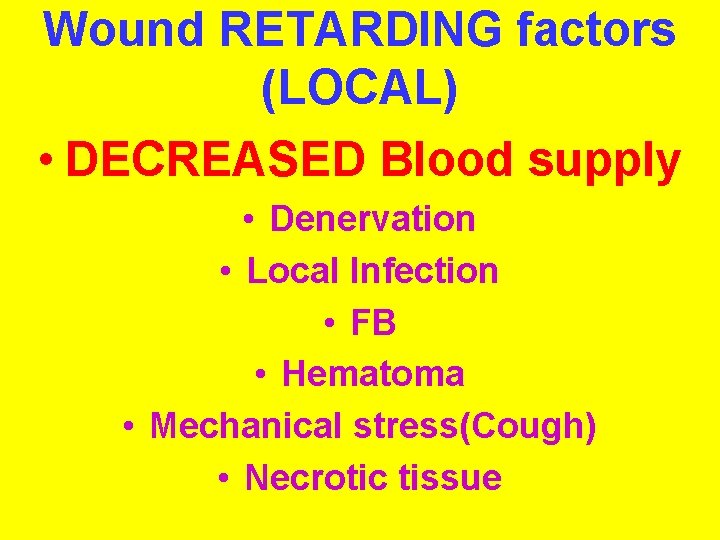
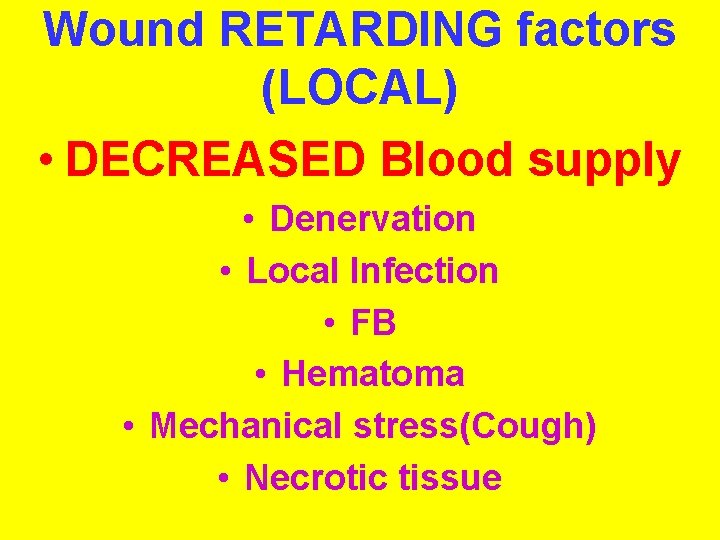
Wound RETARDING factors (LOCAL) • DECREASED Blood supply • Denervation • Local Infection • FB • Hematoma • Mechanical stress(Cough) • Necrotic tissue
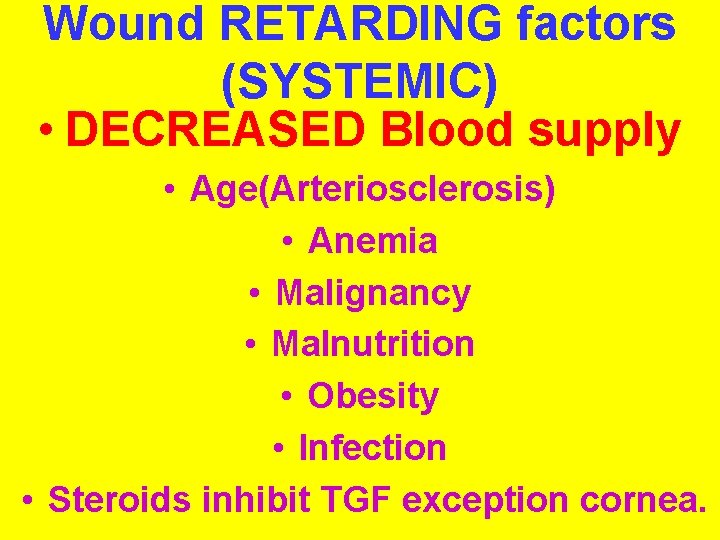
Wound RETARDING factors (SYSTEMIC) • DECREASED Blood supply • Age(Arteriosclerosis) • Anemia • Malignancy • Malnutrition • Obesity • Infection • Steroids inhibit TGF exception cornea.
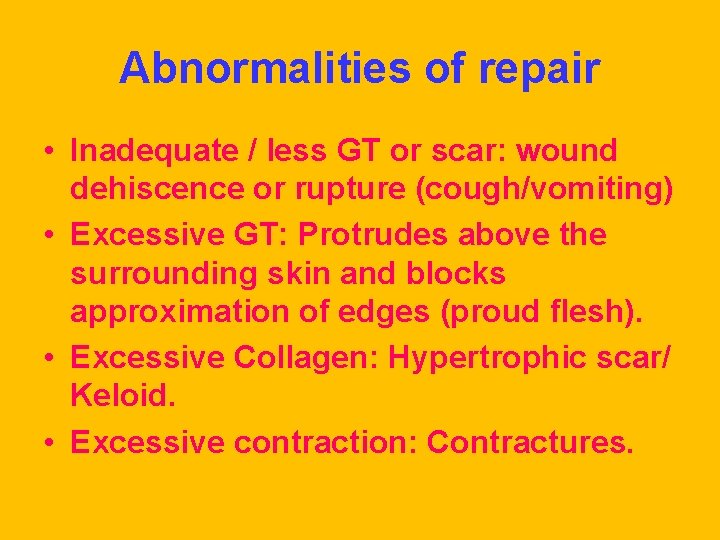
Abnormalities of repair • Inadequate / less GT or scar: wound dehiscence or rupture (cough/vomiting) • Excessive GT: Protrudes above the surrounding skin and blocks approximation of edges (proud flesh). • Excessive Collagen: Hypertrophic scar/ Keloid. • Excessive contraction: Contractures.


THANK YOU
 Tissue regeneration
Tissue regeneration Repair and restoration theory of sleep
Repair and restoration theory of sleep Repair renovation and restoration of water bodies
Repair renovation and restoration of water bodies Repair and restoration theory of sleep
Repair and restoration theory of sleep Base excision repair
Base excision repair Mismatch repair
Mismatch repair Planarian regeneration
Planarian regeneration Objectives of artificial regeneration
Objectives of artificial regeneration Organisms that reproduce asexually
Organisms that reproduce asexually Brayton cycle with regeneration pv diagram
Brayton cycle with regeneration pv diagram Classification of gas turbine power plant
Classification of gas turbine power plant Gas turbine with regeneration
Gas turbine with regeneration Fiat doblo dpf regeneration procedure
Fiat doblo dpf regeneration procedure Nottingham regeneration
Nottingham regeneration Cellules ciliées régénération
Cellules ciliées régénération Was the london docklands regeneration a success
Was the london docklands regeneration a success Healing by first intention
Healing by first intention Nervous tissue repair
Nervous tissue repair Perforation plates
Perforation plates Jesus healing the lepers
Jesus healing the lepers 4rs of fracture management
4rs of fracture management Nbcda
Nbcda Marumali program
Marumali program When the healer needs healing
When the healer needs healing Healing of the blind man at bethsaida
Healing of the blind man at bethsaida Dallas willard healing the heart
Dallas willard healing the heart Bhaktamar stotra for health
Bhaktamar stotra for health Healing is a process not an event
Healing is a process not an event Enaahtig
Enaahtig Whakatauki about healing
Whakatauki about healing Concealed puncture wound
Concealed puncture wound Institute of health and healing
Institute of health and healing Trabacule
Trabacule New formula
New formula Zoroastrian prayers for healing
Zoroastrian prayers for healing Primary union wound healing
Primary union wound healing Plastibell healing chart
Plastibell healing chart Healing by listening to quran
Healing by listening to quran Quantum edge healing institute
Quantum edge healing institute Healing beyond borders
Healing beyond borders Healing and rebuilding our communities
Healing and rebuilding our communities Words of institution
Words of institution Went about doing good
Went about doing good Perkins formula fracture
Perkins formula fracture Diagram microscopic structure of bone
Diagram microscopic structure of bone Wound type
Wound type Medical sheepskin healing
Medical sheepskin healing Jesus heals the leper clipart
Jesus heals the leper clipart Wound healing nutrition handout
Wound healing nutrition handout Native american healing prayers for the sick
Native american healing prayers for the sick Perkins timetable of fracture healing
Perkins timetable of fracture healing Greenstone karakia
Greenstone karakia Lessons from naaman
Lessons from naaman Inflammation fever
Inflammation fever Systemic factors influencing wound healing
Systemic factors influencing wound healing