The SOS Stenting Of Saphenous vein grafts Randomized
- Slides: 32
The SOS (Stenting Of Saphenous vein grafts) Randomized, Controlled Trial of a Paclitaxel-Eluting Stent Vs. a Similar Bare Metal Stent in Saphenous Vein Graft Lesions Emmanouil S. Brilakis, MD, Ph. D Director, Cardiac Catheterization Laboratory VA North Texas Healthcare System On behalf of the SOS investigators
Disclosure Statement of Financial Interest I, Emmanouil Brilakis DO NOT have a financial interest/arrangement or affiliation with one or more organizations that could be perceived as a real or apparent conflict of interest in the context of the subject of this presentation.
Funding • Veteran Affairs, VISN-17 • Clark R. Gregg fund, Harris Methodist Foundation, Fort Worth, Texas
SOS design • DESIGN: Prospective, randomized, multi-center trial comparing the Taxus™ paclitaxel-eluting stent (PES) with a similar Express 2™ bare metal stent (BMS) in saphenous vein graft (SVG) lesions • OBJECTIVE: To compare the 12 -month angiographic and 24 -month clinical outcomes between PES and BMS in SVG lesions • PRINCIPAL INVESTIGATOR: Emmanouil S. Brilakis, MD, Ph. D. VA North Texas Healthcare System, Dallas, Texas
SOS: sample size determination • 31 patients needed per group to have 80% power (2 -sided alpha 0. 05) to detect a 66% reduction in binary angiographic restenosis assuming 50% restenosis in BMS group and 1 lesion treated per pt • Target enrollment: 40 patients per group to account for losses during follow-up
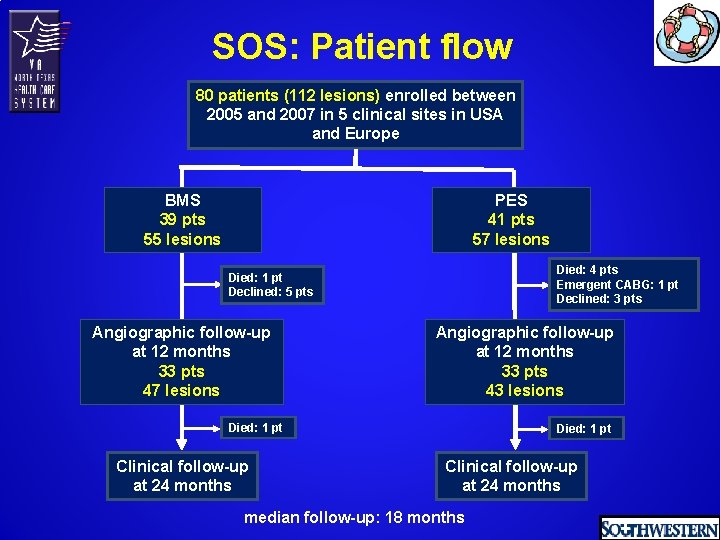
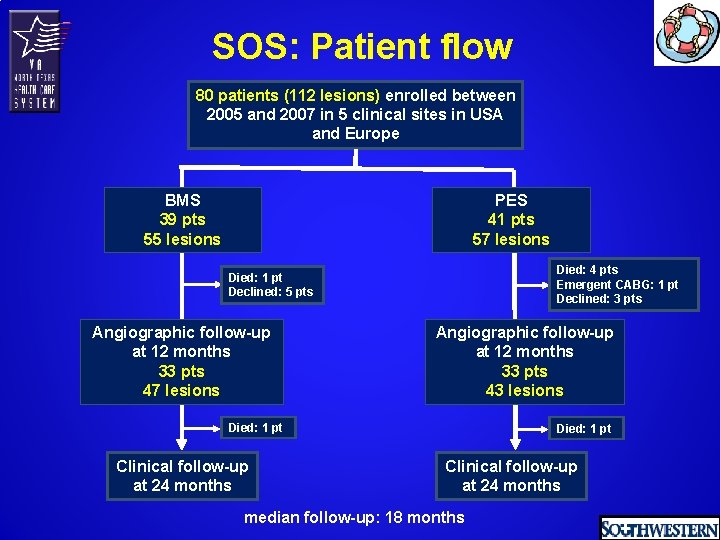
SOS: Patient flow 80 patients (112 lesions) enrolled between 2005 and 2007 in 5 clinical sites in USA and Europe BMS 39 pts 55 lesions PES 41 pts 57 lesions Died: 4 pts Emergent CABG: 1 pt Declined: 3 pts Died: 1 pt Declined: 5 pts Angiographic follow-up at 12 months 33 pts 47 lesions Angiographic follow-up at 12 months 33 pts 43 lesions Died: 1 pt Clinical follow-up at 24 months median follow-up: 18 months
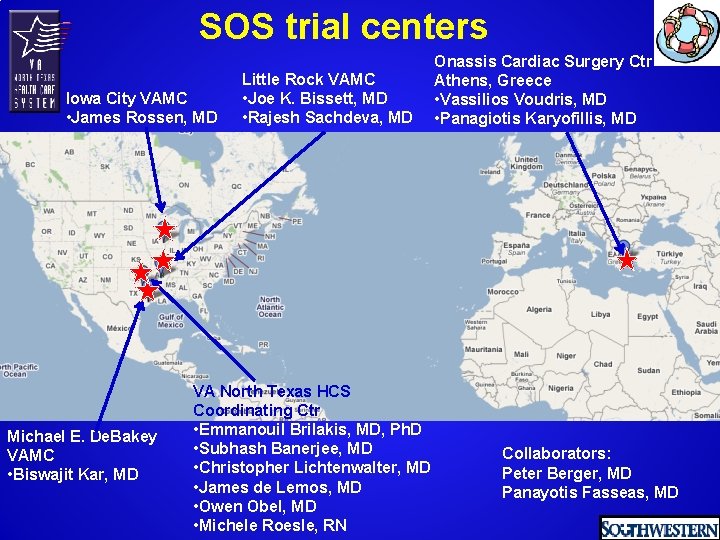
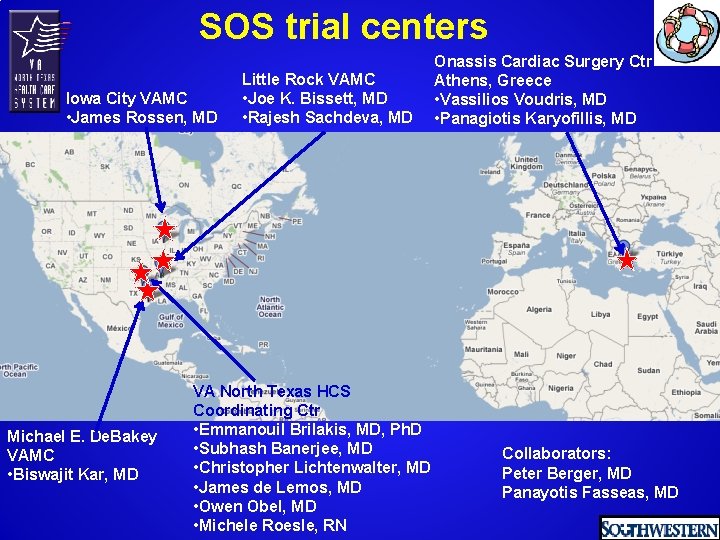
SOS trial centers Iowa City VAMC • James Rossen, MD Michael E. De. Bakey VAMC • Biswajit Kar, MD Little Rock VAMC • Joe K. Bissett, MD • Rajesh Sachdeva, MD VA North Texas HCS Coordinating Ctr • Emmanouil Brilakis, MD, Ph. D • Subhash Banerjee, MD • Christopher Lichtenwalter, MD • James de Lemos, MD • Owen Obel, MD • Michele Roesle, RN Onassis Cardiac Surgery Ctr Athens, Greece • Vassilios Voudris, MD • Panagiotis Karyofillis, MD Collaborators: Peter Berger, MD Panayotis Fasseas, MD
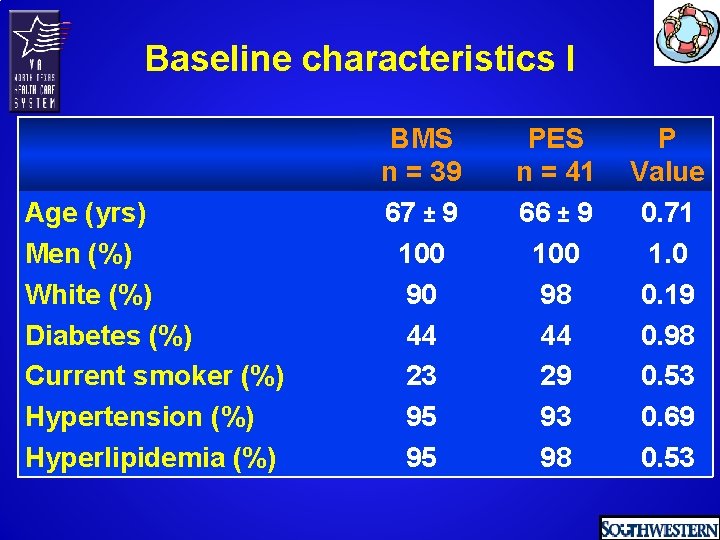
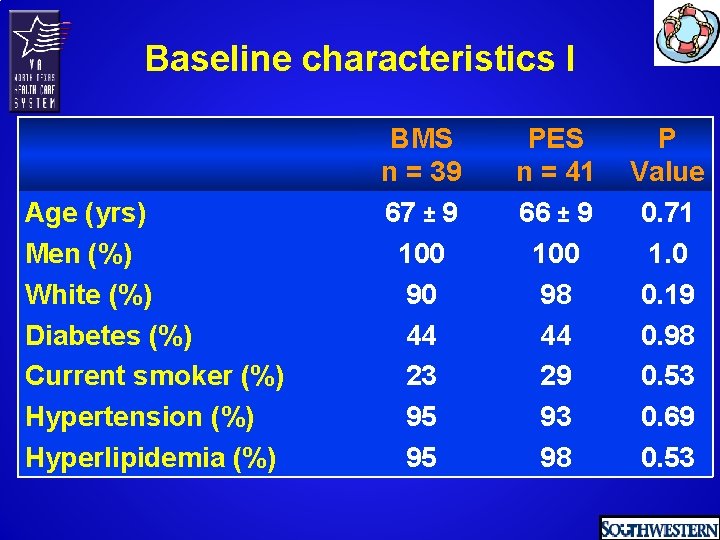
Baseline characteristics I Age (yrs) Men (%) White (%) Diabetes (%) Current smoker (%) Hypertension (%) Hyperlipidemia (%) BMS n = 39 67 ± 9 100 90 44 23 95 95 PES n = 41 66 ± 9 100 98 44 29 93 98 P Value 0. 71 1. 0 0. 19 0. 98 0. 53 0. 69 0. 53
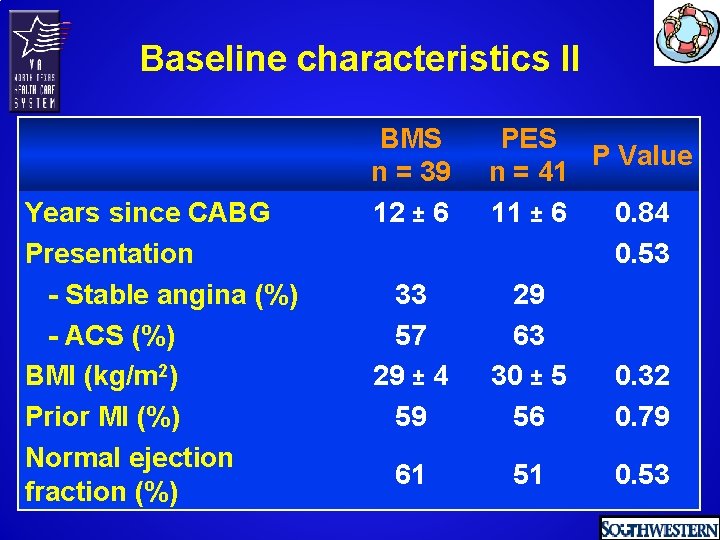
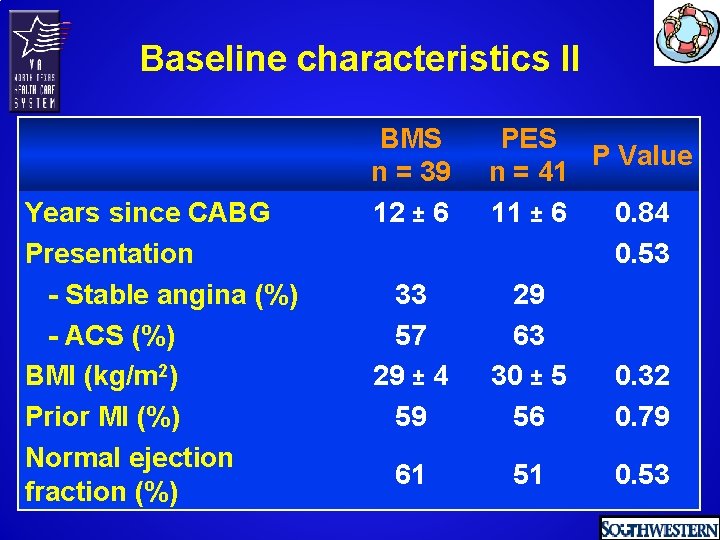
Baseline characteristics II Years since CABG Presentation - Stable angina (%) - ACS (%) BMI (kg/m 2) Prior MI (%) Normal ejection fraction (%) BMS n = 39 12 ± 6 33 57 29 ± 4 59 61 PES P Value n = 41 11 ± 6 0. 84 0. 53 29 63 30 ± 5 0. 32 56 0. 79 51 0. 53
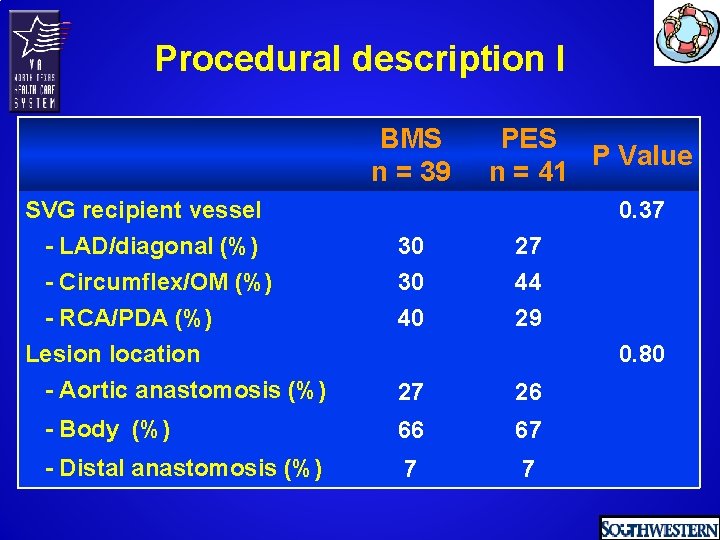
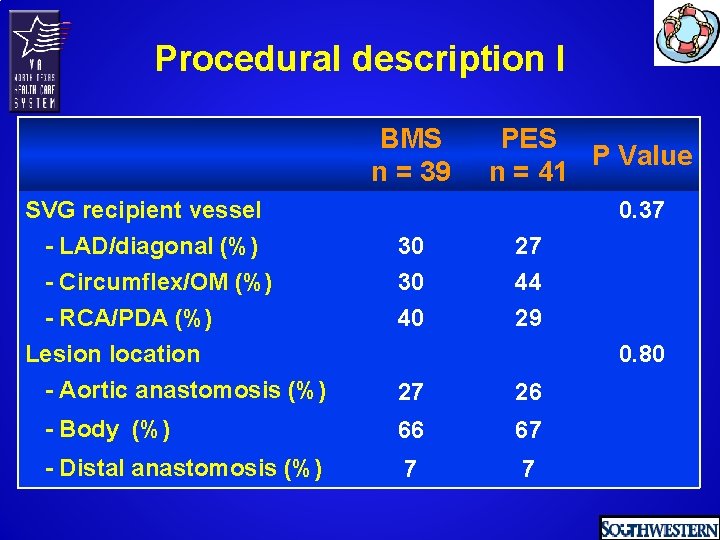
Procedural description I BMS n = 39 SVG recipient vessel - LAD/diagonal (%) - Circumflex/OM (%) - RCA/PDA (%) Lesion location - Aortic anastomosis (%) PES P Value n = 41 0. 37 30 27 30 40 44 29 0. 80 27 26 - Body (%) 66 67 - Distal anastomosis (%) 7 7
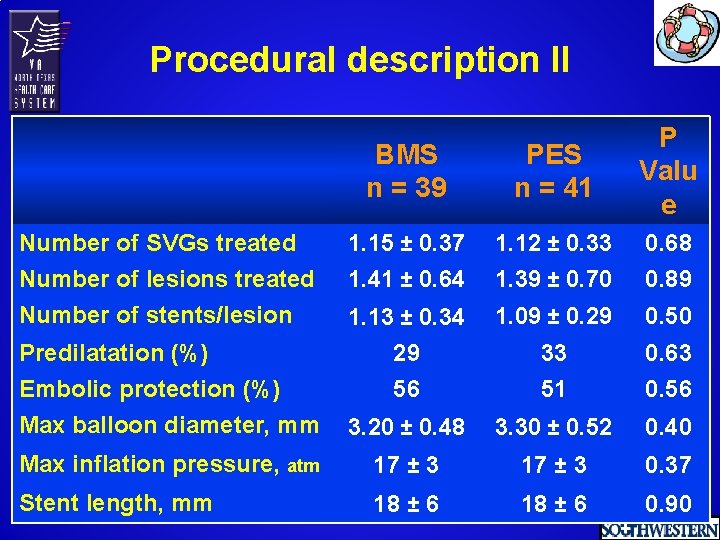
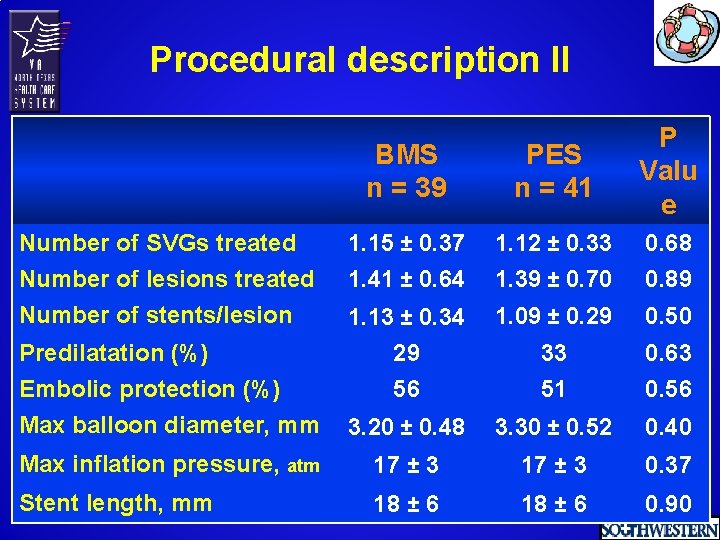
Procedural description II BMS n = 39 PES n = 41 P Valu e Number of SVGs treated 1. 15 ± 0. 37 1. 12 ± 0. 33 0. 68 Number of lesions treated Number of stents/lesion 1. 41 ± 0. 64 1. 39 ± 0. 70 0. 89 1. 13 ± 0. 34 1. 09 ± 0. 29 0. 50 Predilatation (%) Embolic protection (%) Max balloon diameter, mm 29 56 33 51 0. 63 0. 56 3. 20 ± 0. 48 3. 30 ± 0. 52 0. 40 Max inflation pressure, atm 17 ± 3 0. 37 Stent length, mm 18 ± 6 0. 90
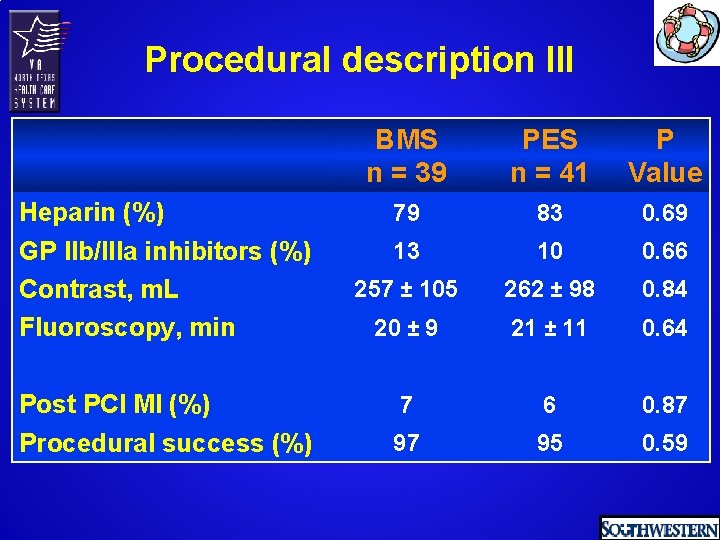
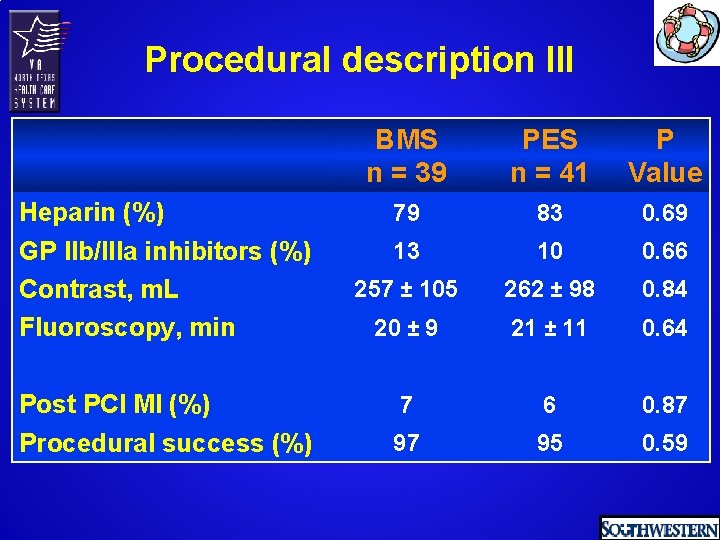
Procedural description III Heparin (%) GP IIb/IIIa inhibitors (%) Contrast, m. L Fluoroscopy, min Post PCI MI (%) Procedural success (%) BMS n = 39 PES n = 41 P Value 79 83 0. 69 13 10 0. 66 257 ± 105 262 ± 98 0. 84 20 ± 9 21 ± 11 0. 64 7 6 0. 87 97 95 0. 59
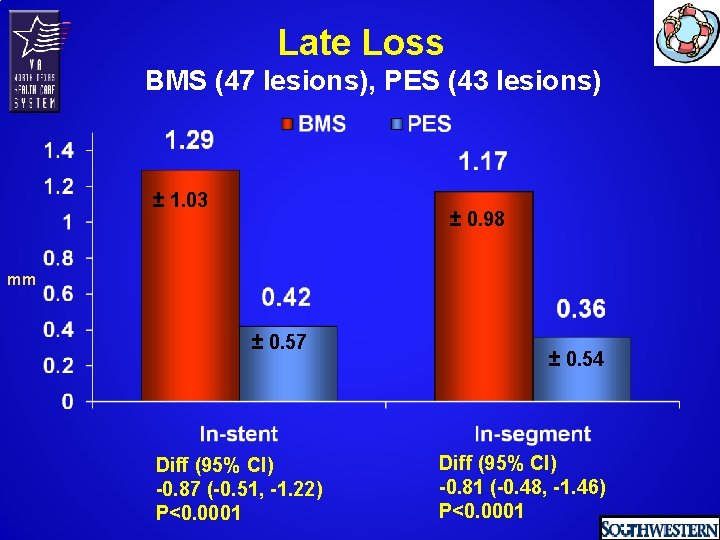
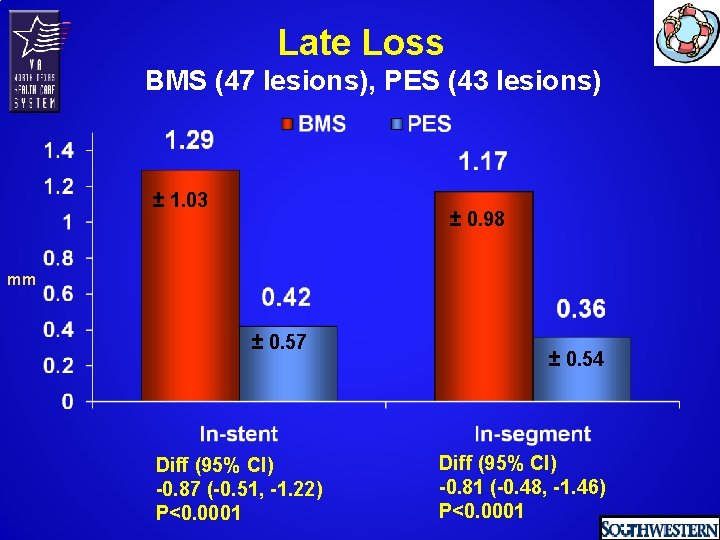
Late Loss BMS (47 lesions), PES (43 lesions) ± 1. 03 ± 0. 98 mm ± 0. 57 Diff (95% CI) -0. 87 (-0. 51, -1. 22) P<0. 0001 ± 0. 54 Diff (95% CI) -0. 81 (-0. 48, -1. 46) P<0. 0001
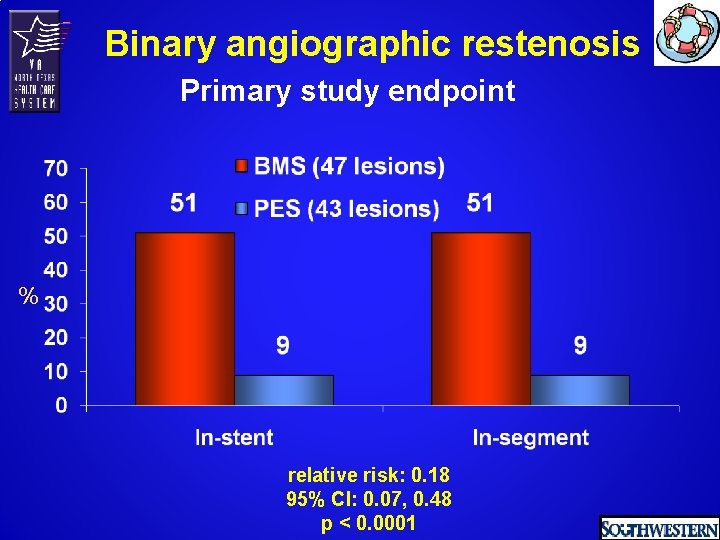
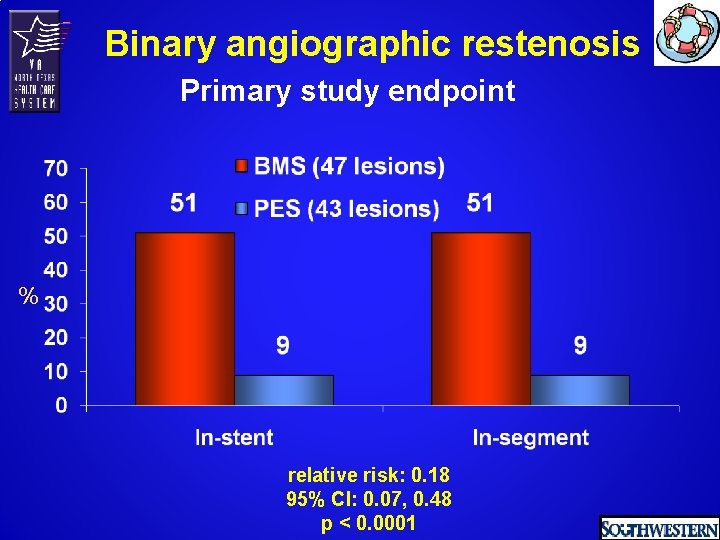
Binary angiographic restenosis Primary study endpoint % relative risk: 0. 18 95% CI: 0. 07, 0. 48 p < 0. 0001
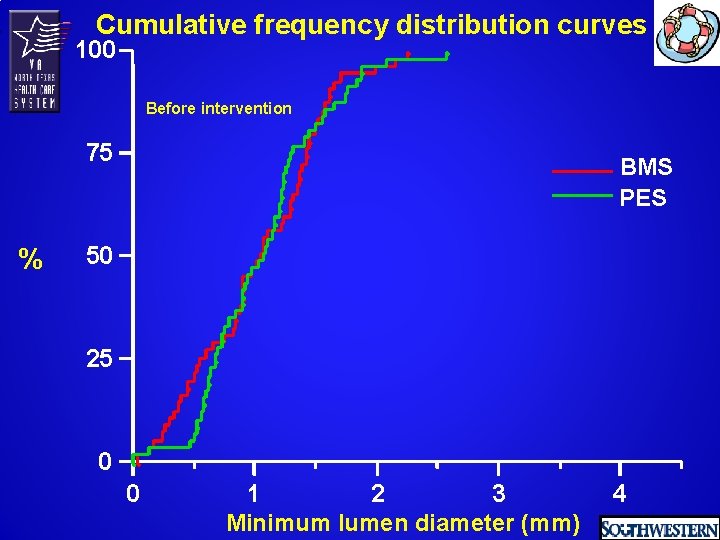
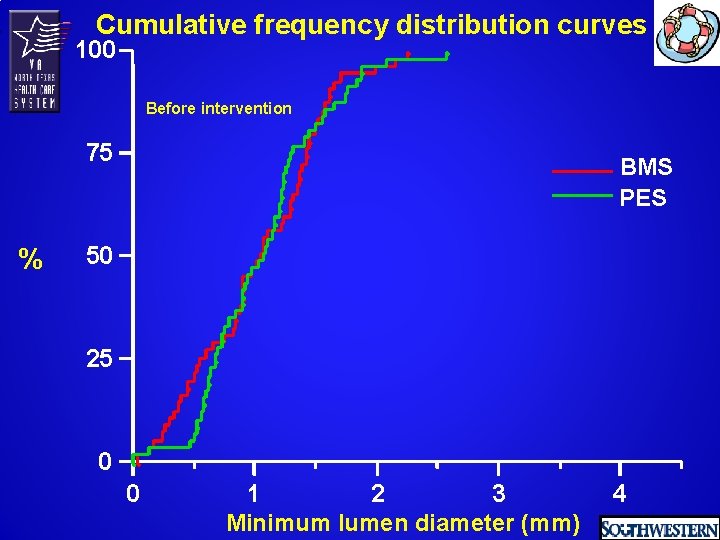
Cumulative frequency distribution curves 100 Before intervention 75 % BMS PES 50 25 0 0 1 2 3 Minimum lumen diameter (mm) 4
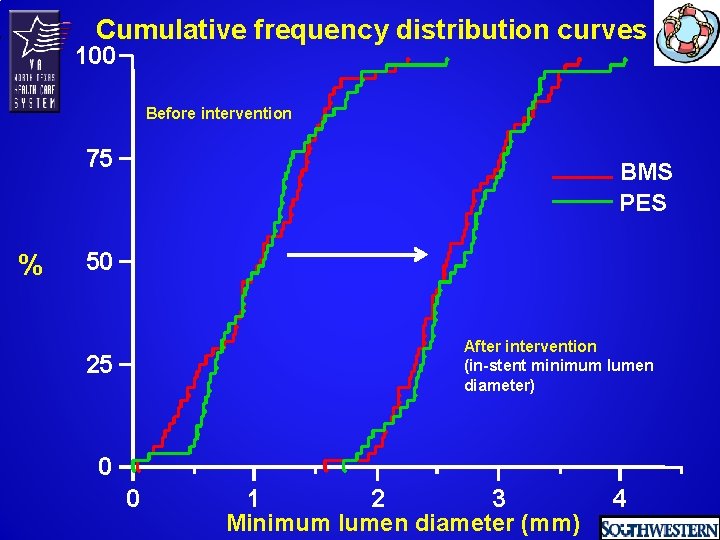
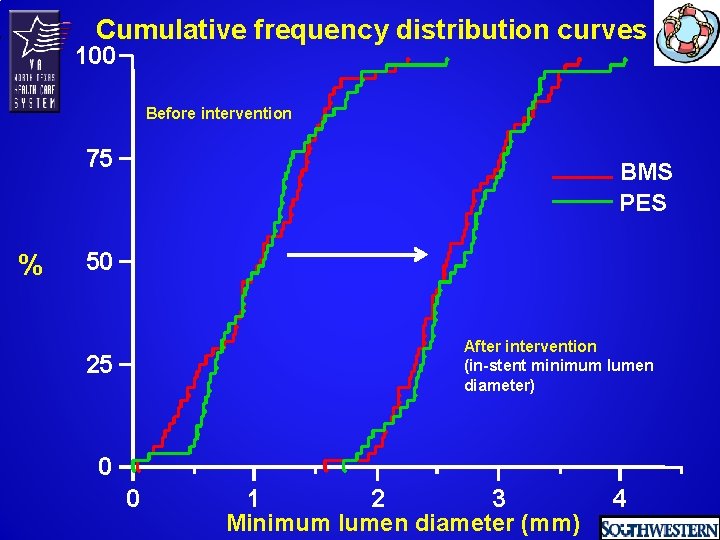
Cumulative frequency distribution curves 100 Before intervention 75 % BMS PES 50 After intervention (in-stent minimum lumen diameter) 25 0 0 1 2 3 Minimum lumen diameter (mm) 4
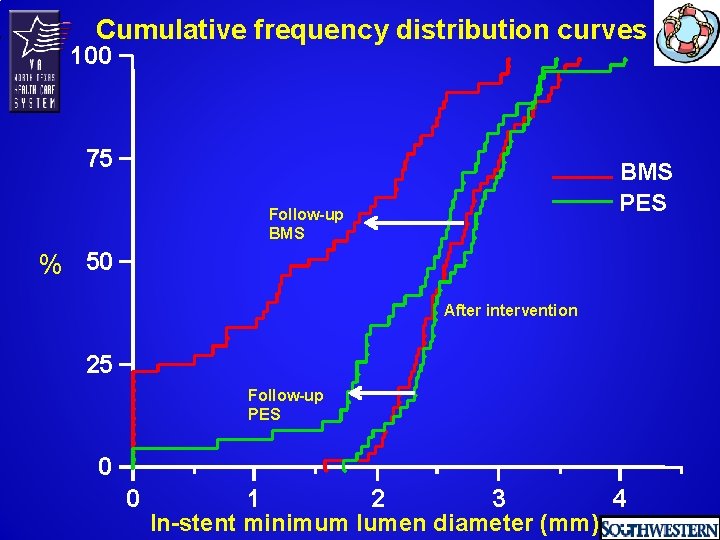
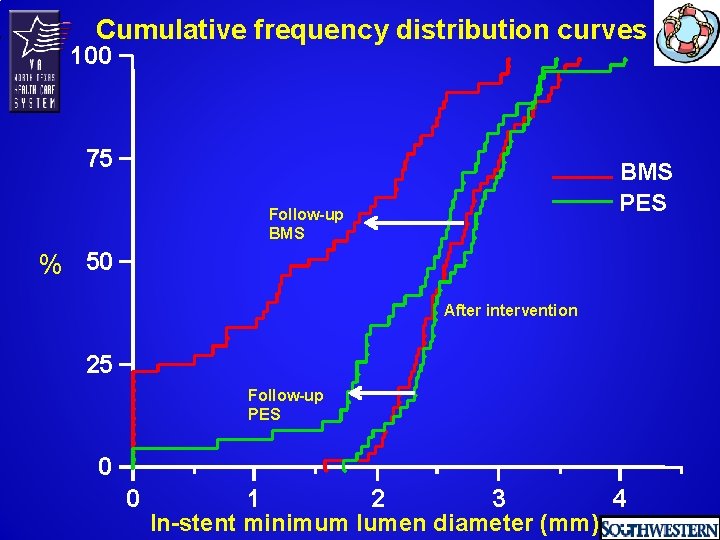
Cumulative frequency distribution curves 100 75 BMS PES Follow-up BMS % 50 After intervention 25 Follow-up PES 0 0 1 2 3 4 In-stent minimum lumen diameter (mm)
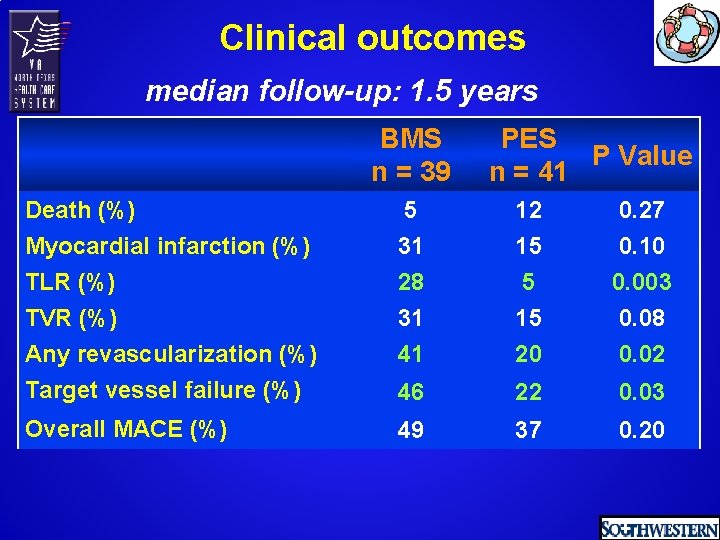
Clinical outcomes median follow-up: 1. 5 years
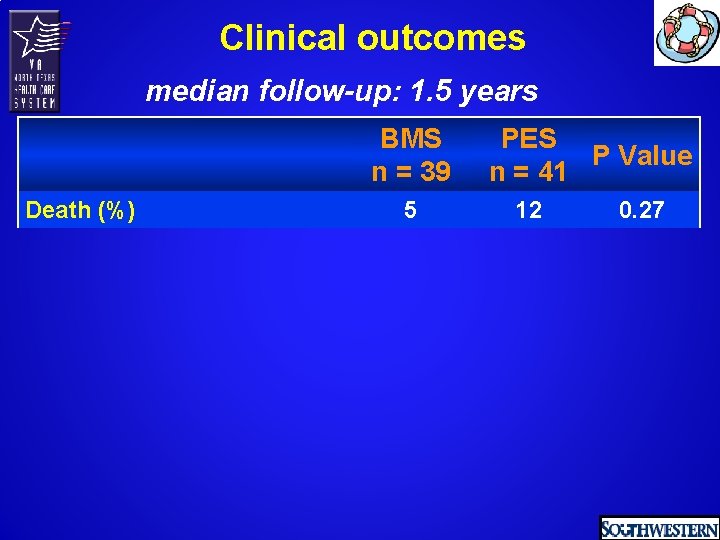
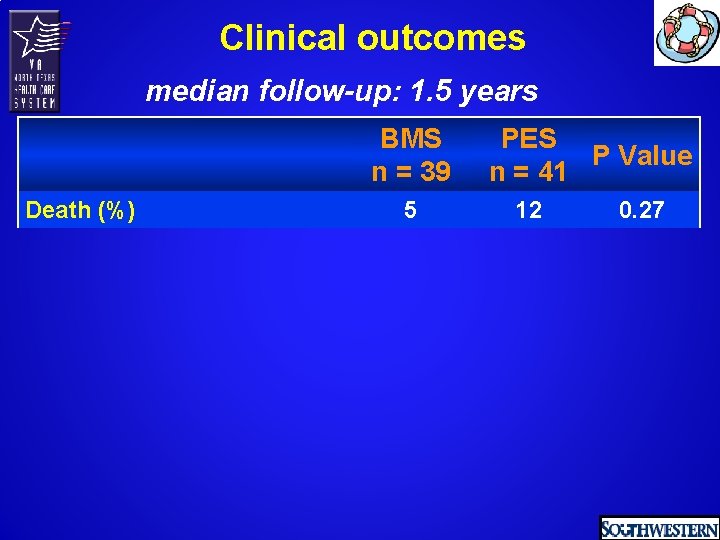
Clinical outcomes median follow-up: 1. 5 years BMS n = 39 Death (%) 5 PES P Value n = 41 12 0. 27
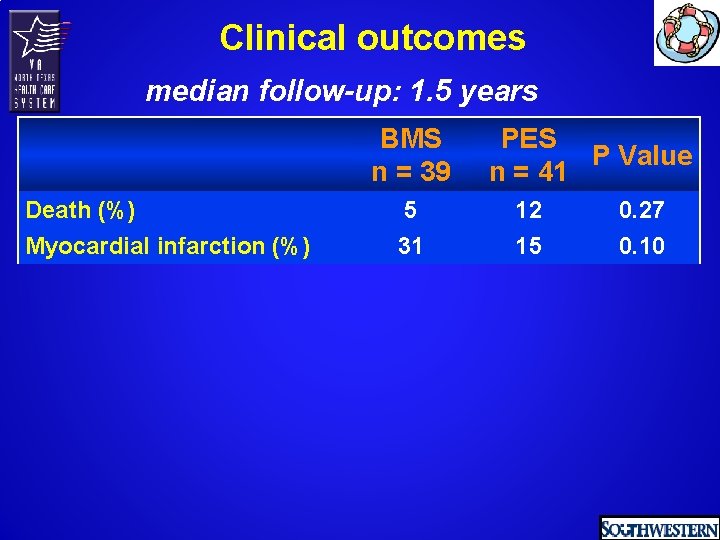
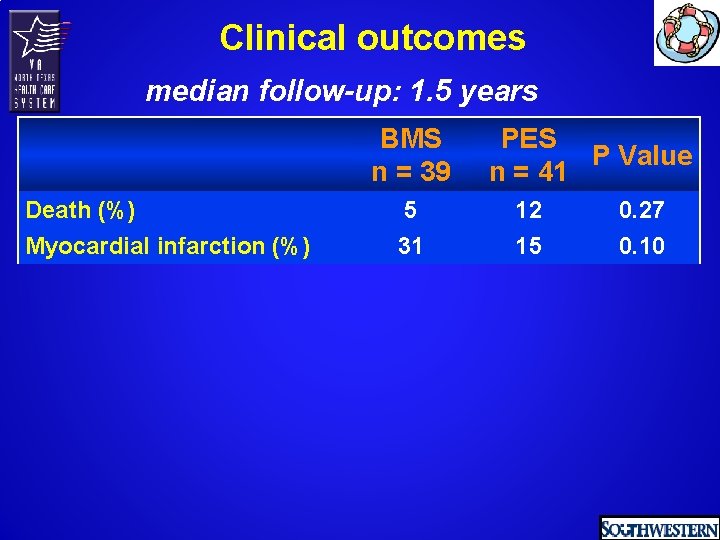
Clinical outcomes median follow-up: 1. 5 years BMS n = 39 Death (%) Myocardial infarction (%) 5 31 PES P Value n = 41 12 15 0. 27 0. 10
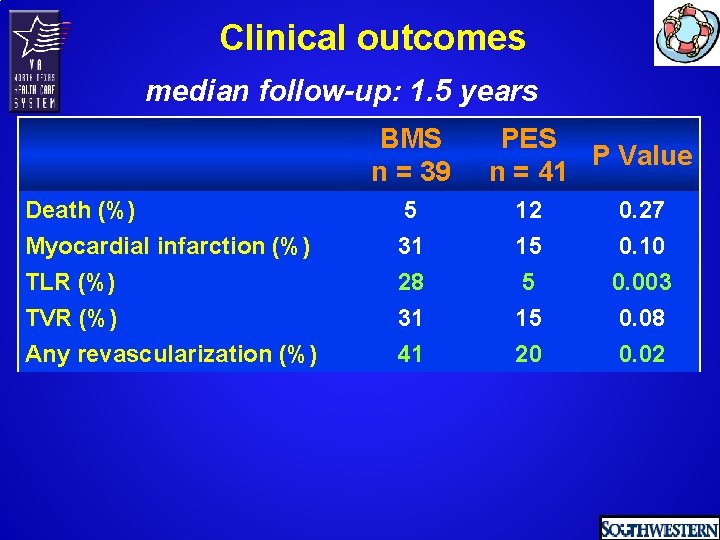
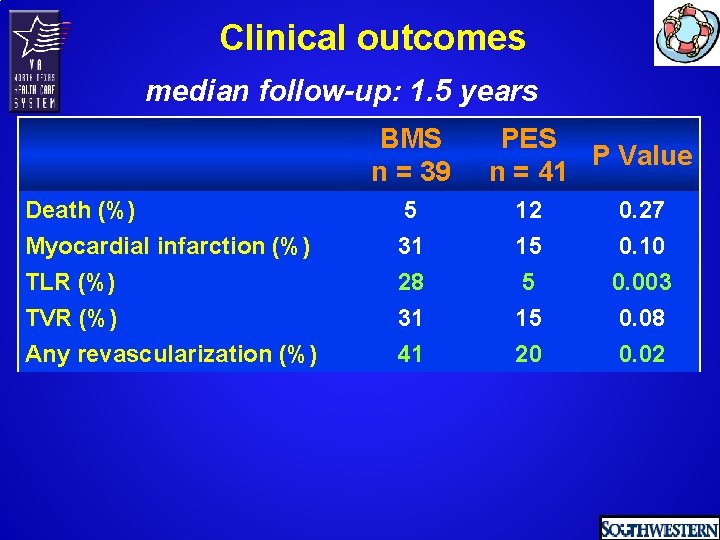
Clinical outcomes median follow-up: 1. 5 years BMS n = 39 PES P Value n = 41 Death (%) Myocardial infarction (%) 5 31 12 15 0. 27 0. 10 TLR (%) TVR (%) Any revascularization (%) 28 31 41 5 15 20 0. 003 0. 08 0. 02
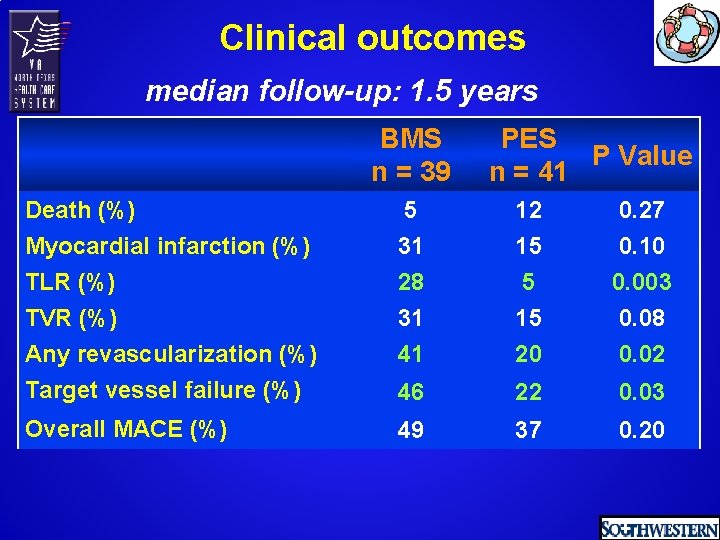
Clinical outcomes median follow-up: 1. 5 years BMS n = 39 PES P Value n = 41 Death (%) Myocardial infarction (%) 5 31 12 15 0. 27 0. 10 TLR (%) TVR (%) Any revascularization (%) Target vessel failure (%) 28 31 41 5 15 20 0. 003 0. 08 0. 02 46 22 0. 03 Overall MACE (%) 49 37 0. 20
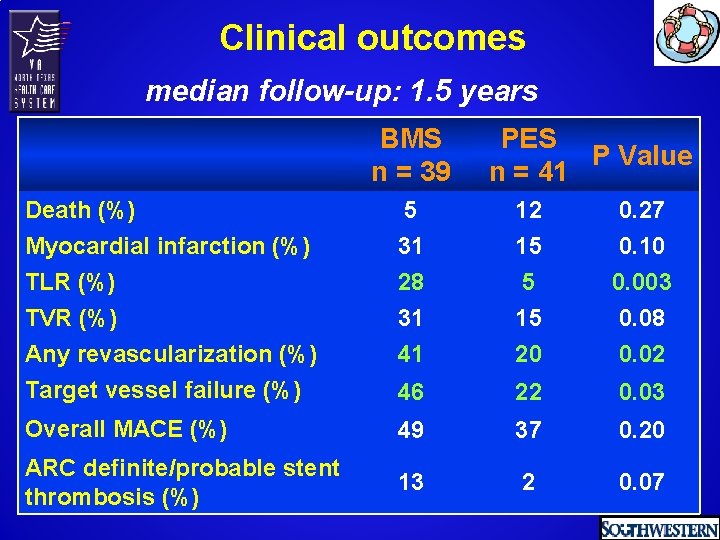
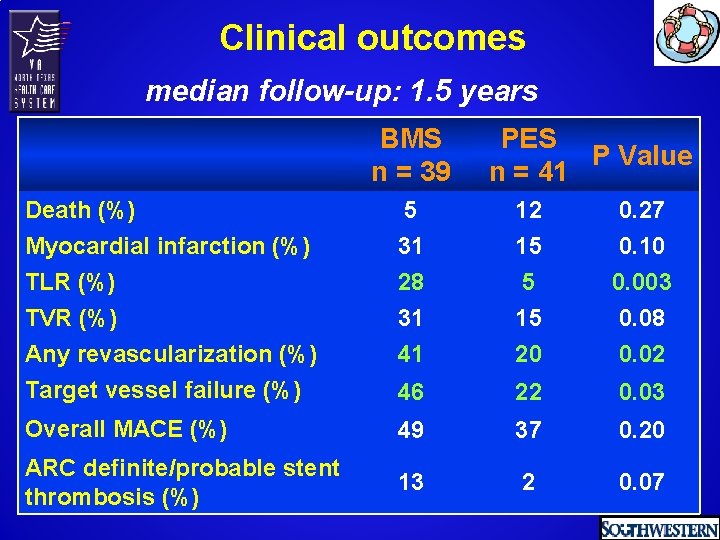
Clinical outcomes median follow-up: 1. 5 years BMS n = 39 PES P Value n = 41 Death (%) Myocardial infarction (%) TLR (%) TVR (%) Any revascularization (%) Target vessel failure (%) 5 31 28 31 41 12 15 5 15 20 0. 27 0. 10 0. 003 0. 08 0. 02 46 22 0. 03 Overall MACE (%) 49 37 0. 20 ARC definite/probable stent thrombosis (%) 13 2 0. 07
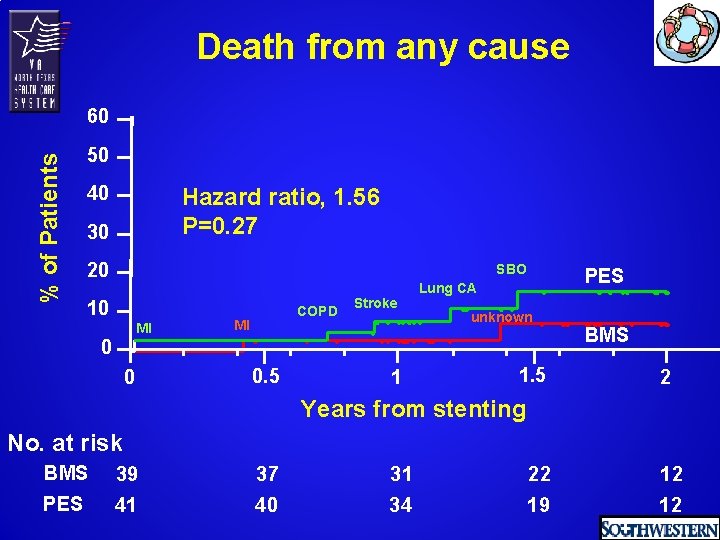
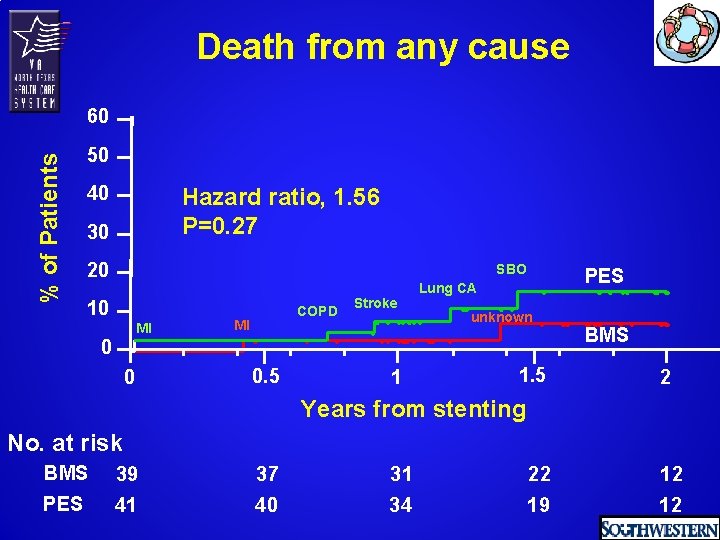
Death from any cause % of Patients 60 50 40 Hazard ratio, 1. 56 P=0. 27 30 20 SBO 10 MI COPD MI Stroke PES Lung CA unknown 0 0 0. 5 1 1. 5 BMS 2 Years from stenting No. at risk BMS 39 37 31 22 12 PES 41 40 34 19 12
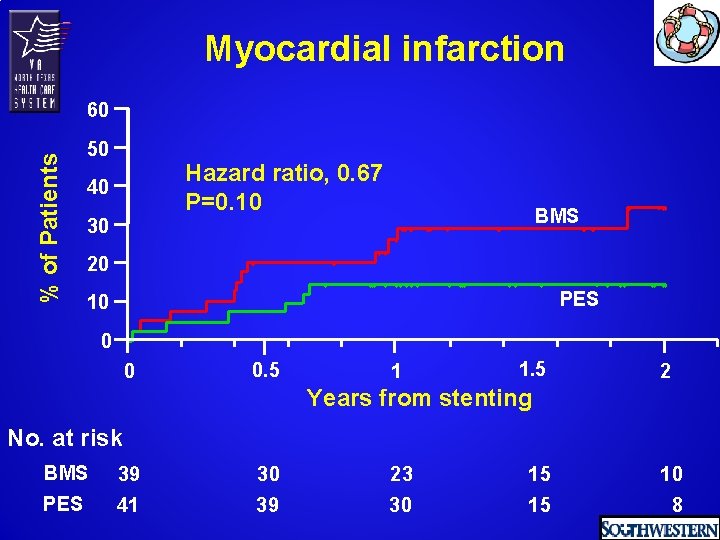
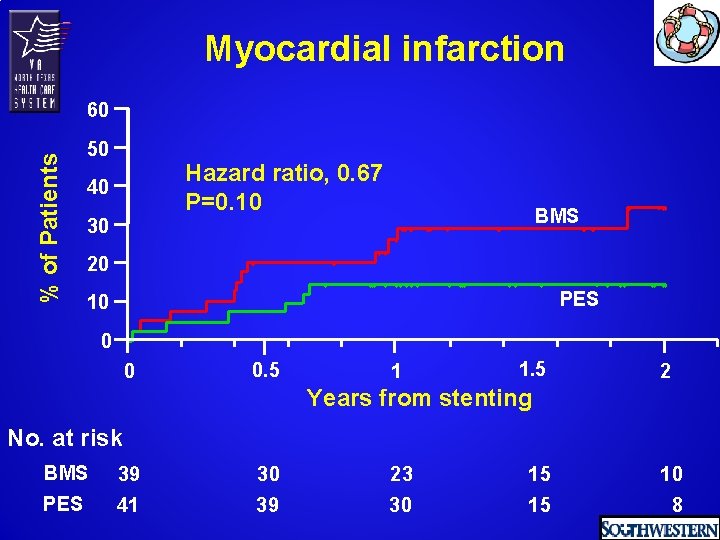
Myocardial infarction % of Patients 60 50 Hazard ratio, 0. 67 P=0. 10 40 30 BMS 20 PES 10 0 0 0. 5 1 1. 5 2 Years from stenting No. at risk BMS 39 30 23 15 10 PES 41 39 30 15 8
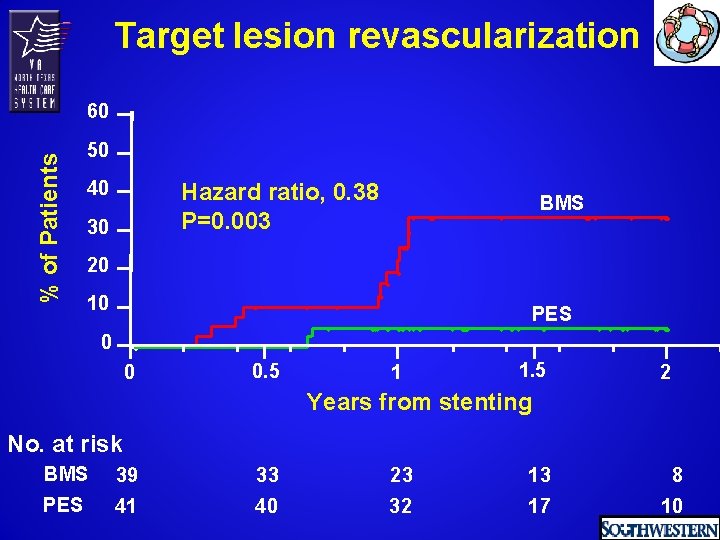
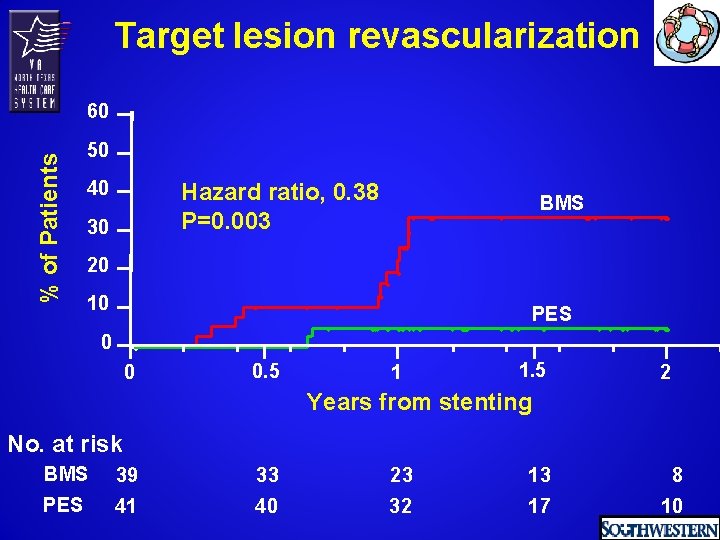
Target lesion revascularization % of Patients 60 50 40 Hazard ratio, 0. 38 P=0. 003 30 BMS 20 10 PES 0 0 0. 5 1 1. 5 2 Years from stenting No. at risk BMS 39 33 23 13 8 PES 41 40 32 17 10
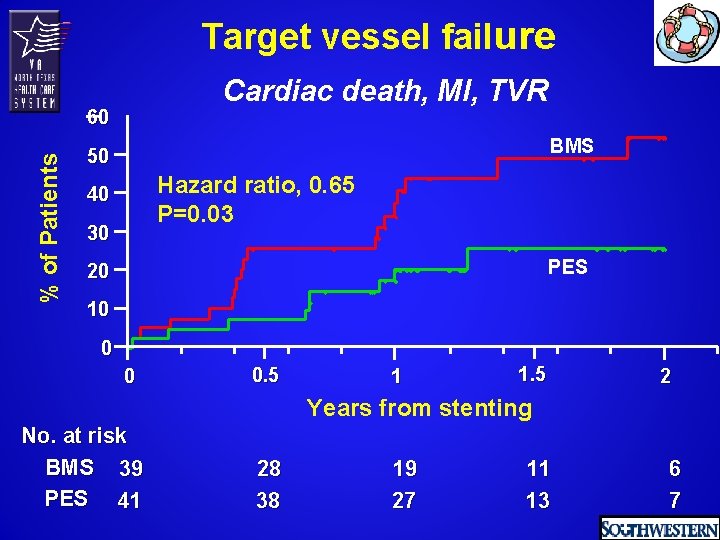
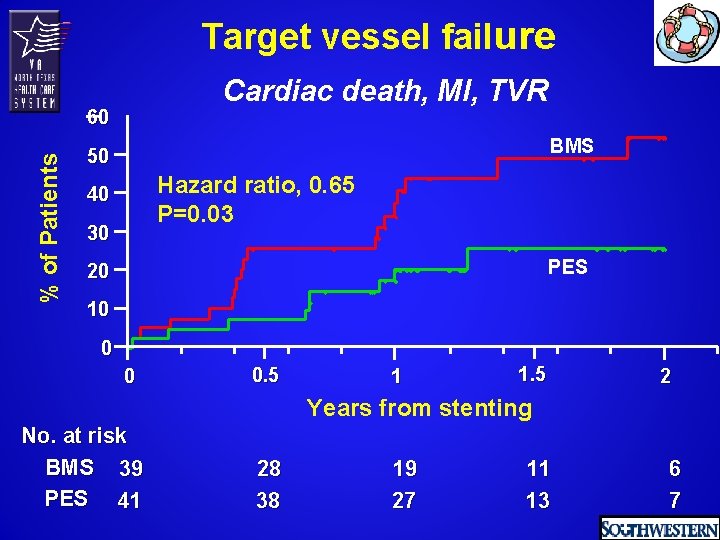
Target vessel failure Cardiac death, MI, TVR % of Patients 60 BMS 50 Hazard ratio, 0. 65 P=0. 03 40 30 PES 20 10 0 0 0. 5 1 1. 5 2 Years from stenting No. at risk BMS 39 PES 41 28 38 19 27 11 13 6 7
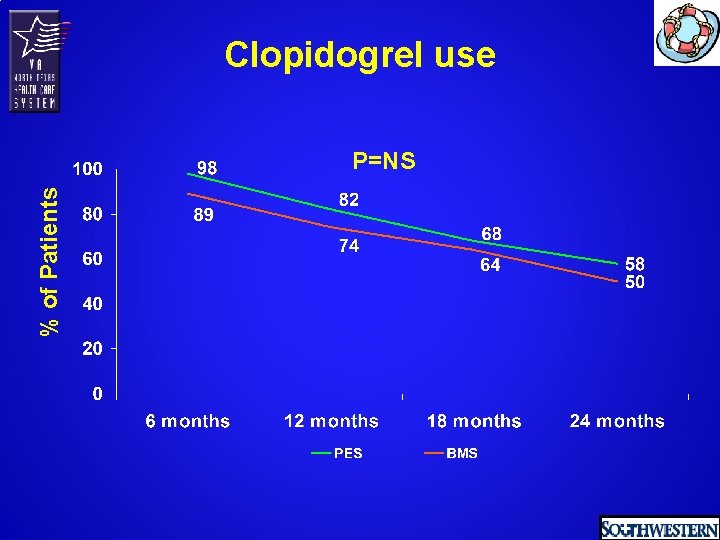
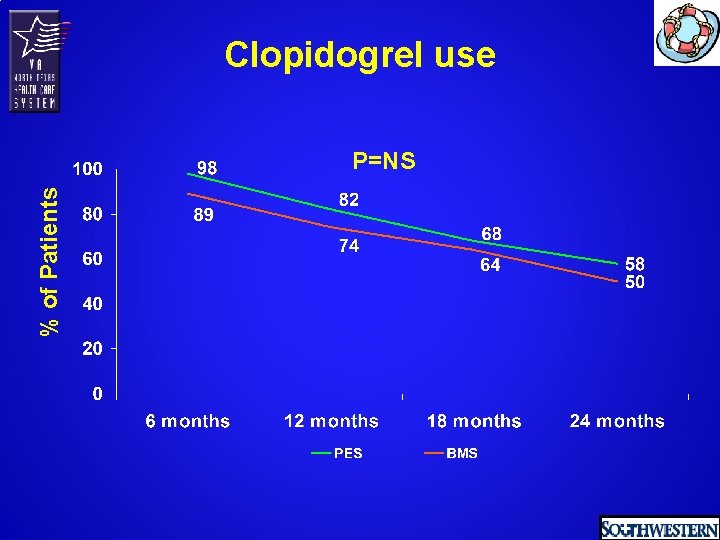
Clopidogrel use % of Patients P=NS
Conclusions In saphenous vein graft lesions, compared to a similar bare metal stent, the Taxus™ PES resulted in:
Conclusions In saphenous vein graft lesions, compared to a similar bare metal stent, the Taxus™ PES resulted in: • Significant reduction in 12 -month binary angiographic restenosis, target lesion revascularization and target vessel failure
Conclusions In saphenous vein graft lesions, compared to a similar bare metal stent, the Taxus™ PES resulted in: • Significant reduction in 12 -month binary angiographic restenosis, target lesion revascularization and target vessel failure • Trends for lower target vessel revascularization, myocardial infarction
Conclusions In saphenous vein graft lesions, compared to a similar bare metal stent, the Taxus™ PES resulted in: • Significant reduction in 12 -month binary angiographic restenosis, target lesion revascularization and target vessel failure • Trends for lower target vessel revascularization, myocardial infarction • No difference in mortality and stent thrombosis
 Lymphatic and venous drainage
Lymphatic and venous drainage Median cubital vein
Median cubital vein Saphenous vein dog
Saphenous vein dog Medial saphenous vein cat
Medial saphenous vein cat ชนิดของหลอดเลือด
ชนิดของหลอดเลือด Trendelenburg procedure
Trendelenburg procedure Great and small saphenous vein
Great and small saphenous vein Great and small saphenous vein
Great and small saphenous vein Small saphenous vein
Small saphenous vein Great and small saphenous vein
Great and small saphenous vein Lymphatic drainage of legs
Lymphatic drainage of legs Reverse tap technique
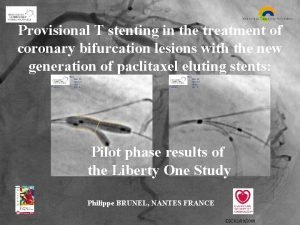
Reverse tap technique Mini culotte stenting
Mini culotte stenting Inverted provisional stenting
Inverted provisional stenting Deep fascia of leg
Deep fascia of leg Gait support
Gait support Saphenous nerve plexus
Saphenous nerve plexus Saphenous opening
Saphenous opening Hunterian perforator
Hunterian perforator Randomized skip list
Randomized skip list Randomized block design example
Randomized block design example Completely randomized design (crd)
Completely randomized design (crd) Layout of rbd
Layout of rbd Advantage of randomized controlled trial
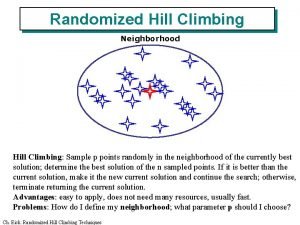
Advantage of randomized controlled trial Randomized hill climbing
Randomized hill climbing Randomized design
Randomized design Randomized group design
Randomized group design Factorial randomized block design
Factorial randomized block design Types of randomized algorithms
Types of randomized algorithms Randomized polynomial time
Randomized polynomial time How to pronounce nivolumab
How to pronounce nivolumab Randomized hill climbing
Randomized hill climbing Difference between rcbd and latin square design
Difference between rcbd and latin square design