The Second Victim of Infusion TherapyRelated Adverse Events




- Slides: 37
The Second Victim of Infusion Therapy-Related Adverse Events Linda A. Treiber, Ph. D. , RN Professor of Sociology, Kennesaw State University Jackie H. Jones, Ed. D. , RN Professor of Nursing, Kennesaw State University
About this Session • Infusion therapy-related adverse events can result in distress and professional suffering for the nurse involved with the event. • This session identifies “second victim syndrome” and includes strategies to help the nurse cope with aftermath of an infusion therapy-related adverse event.
Objectives • Identify infusion therapy-related adverse events. • Describe indications of second victim syndrome. • Identify possible ways to care for second victims.
Errors in health care • Institute of Medicine: Between 44, 000 to 98, 000 people die each year from preventable medical errors (IOM 1999). • Department of Health & Human Services (2010): 180, 000 Medicare patients die annually • Leapfrog Group (2013): Up to 440, 000 Americans die annually from preventable hospital errors. • Estimated as the 3 rd leading cause of death in US (Makary and Daniel, BMJ, 2016)
IV Administration Errors High Risk • Observational study: IV errors higher risk and more severe than other medication administration errors – (Westbrook, Robb, Woods, & Parry, 2011). • Reasons for errors include interruptions, knowledge deficits, inexperience, and failure to follow safety routines. • In a UK study of voluntarily reported incidents that led to death, 62% involved IV administrations (National Patient Safety Agency, 2009). • Errors can have long lasting impacts on nurses – (Jones & Treiber, 2010).
The Five Rights: A Destination Without a Map • “If we hold individuals accountable for achieving the five rights, we really should give them the authority to design their own systems for achieving these outcomes. After all, how can we hold individuals accountable for things that are not under their control? ” • (Institute for Safe Medication Practices, 2007)
Second Victims Concept Dr. Albert Wu introduced the concept that after making an error professionally, physicians become the “second victims” of the error. Being confronted with lack of sympathy, blame, resident failed to identify electrocardiographic signs of pericardial tamponade. Deemed incompetent, lack of sympathy, blamed, shamed…. (Wu, 2000)
Healthcare Providers as Second Victims • Involved in an unanticipated adverse patient event, medical error, and/or a patientrelated injury • “Victimized” in that the provider is traumatized by the event • Frequently feel personally responsible for the patient outcome. • Feel as though they have failed the patient; second guess their clinical skills and knowledge base. • (Scott, Hirschinger, Cox, Brandt & Hall, 2009)
Nurses as Second Victims: Case of Julie Thao • Mistook epidural painkiller for PCN and hooked it up to IV line, infusing it directly into the patient’s bloodstream • The young woman, about to give birth, died as a result. The infant survived. • Thao had worked two consecutive eight-hour shifts the day before and then slept in the hospital before coming on duty again the next morning • Lost her job and charged with criminal negligence • Hospitalized with depression • (Laura Landro, The Wall Street Journal, 2010). http: //www. wsj. com/articles/SB 10001424052748704588404 575123500096433436

Julie Thao faces patient’s mother in court Julie Thao looks at mother of Jasmine Gant, during a hearing in 2006 about her medical error that led to Ms. Gant's death. Photo by John Maniaci/Wisconsin State Journal
Nurses as Second Victim: Case of Kimberly Hiatt • Hiatt made a drug miscalculation: gave 10 times the correct amount of calcium chloride to a critically ill infant with heart problems
Kimberley Hiatt, Cont. • Hiatt honest about her error • Infant died five days later • Hiatt lost her job and was unable to be hired elsewhere • Hiatt committed suicide • (Aleccia 2011, NBCNEWS. com)
When the 5 Rights go Wrong: Medication Errors from the Nursing Perspective • Funded by Kennesaw State University, CETL Faculty Incentive Award (2008). Goals/Objectives: • To listen to the voices of nurses • To obtain nurses’ perceptions of why/how medication errors occur • To explore nurses’ feelings about medication errors • Mail Survey with Internet Option – Contributing Factors/Opinions/Current Medication Administration Practices – Series of closed & open ended questions describing the event. – Random sample RN’s in the State of Georgia
Results • 202 Respondents • 78% (158) had made one or more medication errors during their career • Themes that emerged from comments: – Shame and self-blame – Loss of self-esteem professional self-image – An awareness that the system had failed them – Concerns about patient harm
How did you feel after making a medication error? • “Devastated. Did not work for several days. ” • “Awful, I thought I had killed my pt. ” • “I felt sick, ashamed, frightened, and very, very sad. ” • “Like the end of the world…It took a month to get over depression & I still check & recheck everything after 6 months. ” • Horrible, scared, afraid, wanted to leave nursing then I told myself I would not ever let it happen again. ”
5 Rights Study Infusion Error Examples • “increased the rate of lidocaine infusion to 230 cc/hr instead of 23 cc/hr. I was hypoglycemic, no break in 5 hours, no food, and had blurred vision. ” • “Gave Vincristine IV to a leukemia pediatric patient. There is no antidote. . . Child became very ill within 48 to 72 hours. Although it did not impact the length of time child lived, it made him acutely ill. I was devastated. ”
Conclusions from When the 5 Rights Go Wrong Study • Emotional devastation and visceral responses to errors were common. • Nurses judged self harshly regardless of circumstances. • Such gut-level reactions did not depend on the severity of the errors • Remained vivid in memory…did not diminish over time. Nurses described error events that happened decades earlier.
Lessons Learned: Medication Errors and Nursing Education • Funded by Wellstar School of Nursing, Kennesaw State University (2015). • Survey of recent BSN graduates – Medication administration preparation – Advocating for patients and self – Nurses’ descriptions medication errors – Nurses’ feelings about medication errors – Support received after making error
Results: Lessons Learned Study • 166 respondents • 56% had made a medication error (41% did not; 5% were unsure). • Reasons for errors include: • Rushing, hurrying, time pressures • Distractions • Inexperience with technologies and protocols • Trying to help others • Pyxis/ did not double check medications.
Infusion Medication Errors • From the self-reported descriptions of error events, 37% were identified as infusion related errors • Medications types included: antibiotics, anticoagulants, antianxiety, and analgesic medications (among others). – – – – Insulin Heparin Levophed Fentanyl Morphine Vancomycin Protonix Lasix
Reactions to making an infusion error • “… so scared. . I thought my pt was not going to tolerate the dose. . . I was reluctant to report the incident bc I was afraid I was going to lose my job. . . My CNL was very supportive and reassured that was the best thing to do. ” • “Guilty! Afraid to report I felt awful, and scared, and was just so grateful the patient was okay. ” • “I felt terrible, but I quickly let my preceptor (I was in orientation then) know. ” • “. . one of the whoas of nursing that makes you stop and reground yourself from becoming so task oriented and in robot mode. However, it makes you feel so incompetent and like you are unable to provide simplicities of care. ”
“…I could have killed my patient” “The patient had a poor reaction; he dropped his blood pressure dangerously low and required an increase in the amount of his dopamine infusion and a fluid bolus. He also verbally expressed how poorly he was feeling. I felt awful. . . I went to the bathroom and vomited. I told my preceptor about that and she found someone to watch our patient for us after he was stable and we took a walk and to talk. …I remember crying all the way home…. All I could think about was how that one brief lapse in judgment and concentration and I could have killed my patient. …I was also really nervous at work for years afterward. ” • (RN hung a bag of precedex on a dopamine line)
“It’s how you learn” “A doctor ordered a Level 1 heparin drip… It was simple human error that I had Level 2 protocol stuck in my brain. All I can say is thank God I under dosed the patient and had to deliver a little more of the bolus to meet the requirement for the correct level. I told the charge nurse and she told me not to report it. I had only been a nurse for a month or so and she said it's how you learn. …I have never made an error with a Heparin drip since then. It scared me to death and the gravity of hurting a patient with medication errors really sunk in. ” • (RN wrong dose of heparin drip)
“I feel guilt over the error …” “…I drew up the Ativan, nearly 1 ml and gave it to her IV. Afterwards I realized the bottle contained 2 mg/ml and so she had been given nearly twice the dose ordered…Oxygen dropped to the mid 60's - 70's and a Rapid Response was called…. I feel guilt over the error and for not directly turning myself in to my manager. I know it wouldn't have changed the outcome for the patient, but I would have been able to let the chips fall where they may. . the possibility of contributing to her transfer [to ICU] plagues me, but I may not know if it was the medication or the inevitable decline associated with her condition. ” • (RN wrong dose of IV Ativan)

Conclusions from the Lessons Learned study • Strong emotional responses • Nurses expressed fear for their patientsand fear for themselves • Some covered up and did not report errors to save face or save their job. • Nurses generally felt supported after making the error, however. • Preceptor, charge nurse, and doctors often helpful
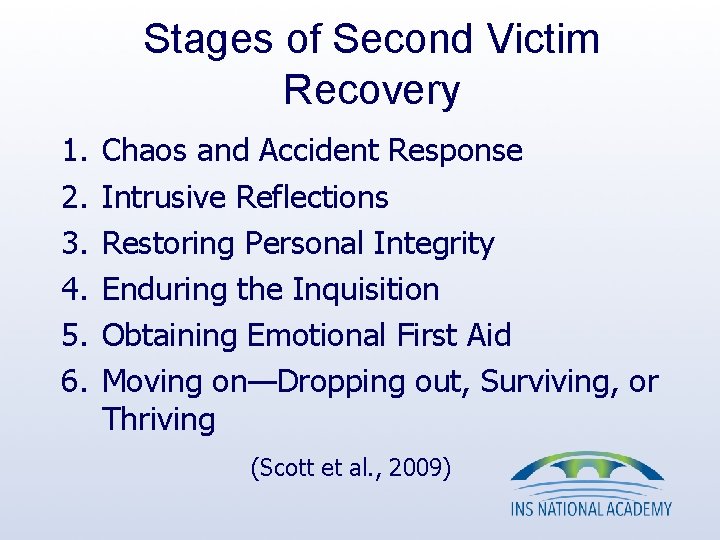
Stages of Second Victim Recovery 1. 2. 3. 4. 5. 6. Chaos and Accident Response Intrusive Reflections Restoring Personal Integrity Enduring the Inquisition Obtaining Emotional First Aid Moving on—Dropping out, Surviving, or Thriving (Scott et al. , 2009)

TRUST: The “Five Rights” of Second Victims 1. 2. 3. 4. 5. Treatment that is just Respect Understanding and compassion Supporting care Transparency and opportunity to contribute (Denham, 2007)
Helping Second Victims • Second-victim rapid response teams • Respectful management of serious clinical adverse events • Do not abandon 2 nd victims – (Gissinger, 2014) • Barriers exist even when organizations do provide support – Reluctance of individuals to use available services – Fear – Stigma attached to mental health care – (Edrees, Paine, Feroli, & Wu, 2011).
American Nurses Association Focus on “Culture of Safety” • The Johns Hopkins Hospital: – Rapid Response Teams (after death of Josie King) – Caring for the Caregiver Program – R. I. S. E (Resilience in Stressful Events) – Support program trains caregivers to help give emotional support to providers • (Trossman 2016)
Support for Advanced Practice Nurses – CRNA’s at risk for becoming second victims: – They often reassure anxious pt. before surgery – Feelings of guilt if something goes wrong – Reliving the event • (van Pelt dissertation)
What Any Caregiver Can Do to Support a ‘Second Victim’ • Do: – – Find a quiet place Ask open-ended questions Listen and paraphrase Direct to resources • Don’t: – Try to investigate to determine whether or not the caregiver was at fault – Try to fix things – Shut down the person’s emotions or tell them how to feel – Minimize the error • (Cheryl Connors, Johns Hopkins, Armstrong Institute (2015)
Summary and Conclusions – Errors often result in suffering and guilt for the provider involved with the event. – The “second victim syndrome” can happen regardless of severity. – Infusion therapy-related adverse events can be minor or deadly, and can lead to distress after the event. – Helping strategies can be initiated at the individual and organizational level.
Opportunities for Future Research and Applications • Additional work on support for 2 nd victims. • Increasing awareness of systemic issues that must be resolved. • Role of nursing education • Explore the “Third Victim” concept: Organizations also suffer after errors

Thank you! Any Questions?
References • Aleccia, Jo. Nel. (June 27, 2011). Nurse's Suicide Highlights Twin Tragedies of Medical Error, NBCNEWS. com. http: //www. nbcnews. com/id/43529641/ns/health-health_care/t/nurses-suicide-highlights-twin-tragedies-medicalerrors/#. V 83 JK 2 c. UXIU Accessed September 4, 2016. • Connors, Cheryl. What Any Caregiver Can Do to Support a ‘Second Victim’ https: //armstronginstitute. blogs. hopkinsmedicine. org/2015/07/30/what-any-caregiver-can-do-to-support-a-secondvictim/ Accessed September 4, 2016. • Denham, Charles R. (2007). TRUST: The 5 Rights of the Second Victim. Journal of Patient Safety, 3(2), 107 -119. • Edrees, Hanan H. , Paine, Lori A. , Feroli, E. Robert, & Wu, Albert W. (2011). Health care workers as second victims of medical errors. Polskie Archiwum Medycyny Wewnetrenej, 121(4), 101 -107. • Grissinger, Matthew (2014). Too Many Abandon the “Second Victims” Of Medical Errors. P&T, 39(9), 591 -592. • Institute for Safe Medication Practices. (2007). The five rights: A destination without a map. http: //www. ismp. org/Newsletters/acutecare/articles/20070125. asp Accessed September 21, 2016. • Jones, Jackie H. , & Treiber, Linda A. (2010). When the 5 Rights Go Wrong: Medication Errors from the Nursing Perspective. Journal of Nursing Care Quality (JNCQ) 25(3), 240 -247. doi: 10. 1097/NCQ. 0 b 013 e 3181 d 5 b 948 • Kohn, Linda T. , Corrigan, Janet M. , & Donaldson, Molla S. (2000). To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press. • Landro, Laura. (2010, March 16, 2010). New Focus on Averting Errors: Hospital Culture, The Wall Street Journal. http: //www. wsj. com/articles/SB 10001424052748704588404575123500096433436 Accessed August 7, 2016. • Leapfrog. Group, The. (2013). Hospital Errors are the Third Leading Cause of Death in U. S. , and New Hospital Safety Scores Show Improvements Are Too Slow. from http: //www. hospitalsafetyscore. org/newsroom/display/hospitalerrors -thirdleading-causeofdeathinus-improvementstooslow Accessed September 21, 2016.
References, Continued • • Makary, Martin, & Daniel, Michael. (2016). Medical Error-The Third Leading Cause of Death in the US. BMJ, 353(2139), 1 -5. doi: http: //dx. doi. org/10. 1136/bmj. i 2139 Philips, J. , Beam, S. , Brinker, A. , Holquist, C. , Honig, P. , Lee, L. Y. , & Pamer, C. (2001). Retrospective analysis of mortalities associated with medication errors. American Journal of Health-System Pharmacy, 58(19), 1835 -1841. Scott, S. D. , Hirschinger, L. E. , Cox, K. R. , Mc. Coig, M. , Brandt, J. , & Hall, L. W. (2009). The Natural History of Recovery for the Healthcare Provider "Second Victim" after Adverse Patient Events. Quality and Safety in Healthcare, 18, 325 -330. Treiber, Linda A. , & Jones, Jackie H. (2010). Devastatingly Human: An Analysis of Registered Nurses’ Medication Error Accounts. Qualitative Health Research, 20(10), 13271342. doi: 10. 1177/1049732310372228 Trossman, Susan. (2016). Second Victims: Offering peer support after adverse or stressproducing events. The American Nurse, 48(1), 1, 8 -9. Westbrook, Johanna, Rob, Marilyn, Woods, Amanda, & Parry, Dave. (2011). Errors in the Administration of Intravenous Medications in Hospital and the Role of Correct Procedures and Nurse Experience. BMJ Quality & Safety, 20(12), 1027 -1034. doi: 10. 1136/bmjqs 2011 -000089 Wu, Albert W. (2000). Medical error: the second victim. The doctor who makes the mistake needs help, too. BMJ, 320, 726 -727
 Adverse events in hospital
Adverse events in hospital Aefi examples
Aefi examples Adverse events in hospital
Adverse events in hospital Adverse events in hospital
Adverse events in hospital Three tiers of support for second victims
Three tiers of support for second victims Mutually exclusive vs non mutually exclusive
Mutually exclusive vs non mutually exclusive Who fought in the punic wars?
Who fought in the punic wars? 186 282 miles per second into meters per second
186 282 miles per second into meters per second Ivf calculation formula
Ivf calculation formula Infusion hierarchy
Infusion hierarchy Disposable pca pump
Disposable pca pump Calculating rate of infusion
Calculating rate of infusion Etymology euphemism
Etymology euphemism Dopamine dose
Dopamine dose Dopamina dosis infusion
Dopamina dosis infusion Resin infusion disadvantages
Resin infusion disadvantages Infiltration iv
Infiltration iv Iv flow rate
Iv flow rate Tabla de goteo de soluciones por minuto
Tabla de goteo de soluciones por minuto Insulin infusion protocol
Insulin infusion protocol Gingettage
Gingettage Insulin
Insulin Indicacion de bicarbonato en acidosis metabolica
Indicacion de bicarbonato en acidosis metabolica Primary vs secondary iv lines
Primary vs secondary iv lines Midazolam infusion dose
Midazolam infusion dose Durchflussregler infusion
Durchflussregler infusion Corcider
Corcider Language
Language Target controlled infusion
Target controlled infusion Iv medication calculation formula
Iv medication calculation formula Dobutamine dose
Dobutamine dose Anesthesia definition
Anesthesia definition Heparin drip protocol
Heparin drip protocol Examples of galenicals
Examples of galenicals Nitroprusiato sodico
Nitroprusiato sodico Loading dose formula
Loading dose formula Iaware infusion
Iaware infusion Drops per minutes calculation
Drops per minutes calculation