Caring for Our Own Support Following Unanticipated Clinical


- Slides: 36
Caring for Our Own: Support Following Unanticipated Clinical Events Susan D. Scott, Ph. D, RN, CPPS, FAAN Sharp 2018 Do No Harm Patient Safety Conference September 21, 2018
Second Victim Interventions Second victims want to feel. . . Appreciated Respected Valued Understood Last but not least…. Remain a trusted member of the team! 2
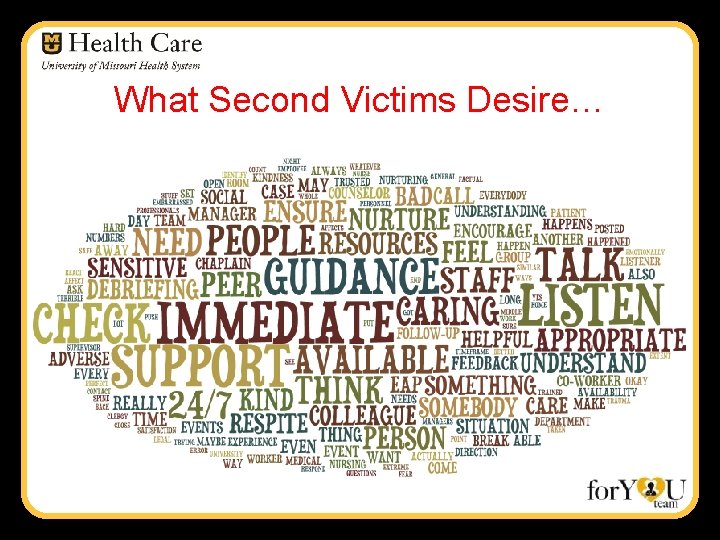
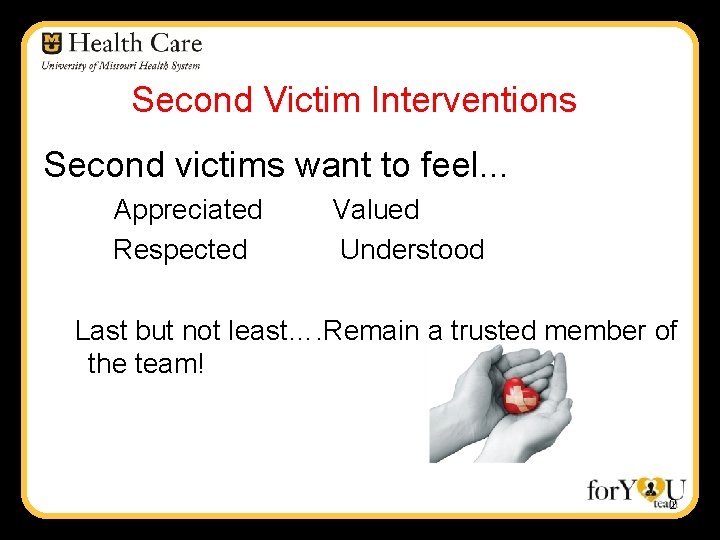
What Second Victims Desire…

Thoughts About Support Clinicians have unique support needs. Health care facilities have unique culture. Both should be considered when designing a network of support for second victims. Two types of support o One on one o Group 4
Challenges to Providing Support • • Stigma to reaching out for help • • Intense fear of the unknown • Fear of future legal woes - HIPAA, Confidentiality Implications High acuity areas have little time to integrate what has happened Fear a compromise of collegial relationships because of event
Benefits of Clinician Support Staff have a way to get their needs meet after going through a traumatic event Helps reduce the harmful effects of stress Provides some normalization and helps the individual gett back to their routine after a traumatic event Promotes the continuation of productive careers while building healthy stress management behaviors
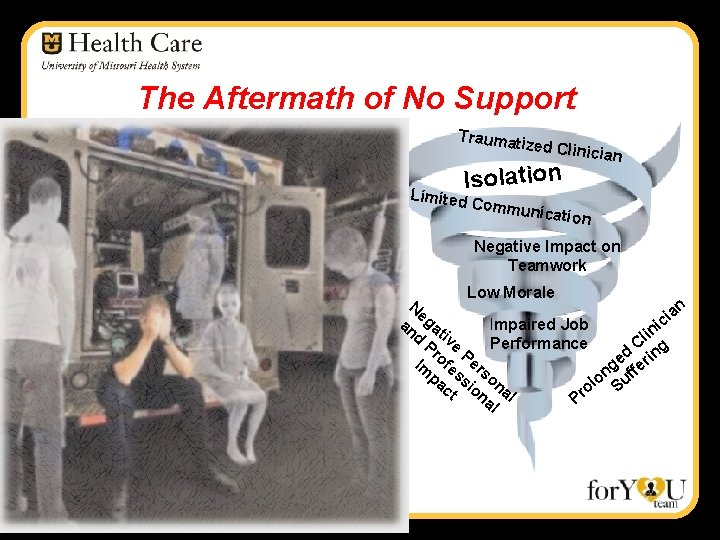
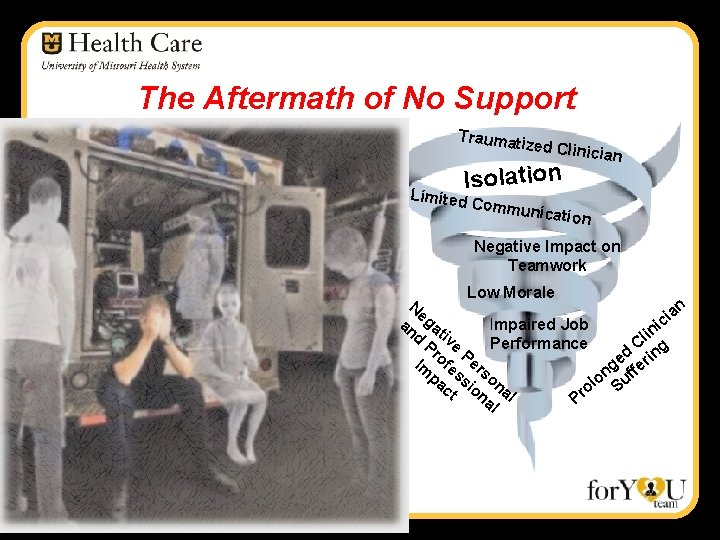
The Aftermath of No Support Traumati z ed Clinic Isolation Limited ian Commu nication Negative Impact on Teamwork Low Morale Ne an i g an a ic Impaired Job il n d tiv Pr e Performance C g Pe d o e erin Im fe rs g n uff pa ss on o l ct ion al o S al Pr
Second Victims Need Support A systematic literature victimization findings: review of second 1) Significant emotional toll on care providers 2) Need for institutional support programs 3) Varied approaches for support “Unethical not to have a clinician support program as the evidence supported the emotional toll that being a second victim takes on a clinician and then in turn, their paitents as well. ” Butler, S. (2015). The Just Culture, Second Victimization, and Clinician Support: An Educational/Awareness Campaign. University of Massachusetts-Amherst. Doctor of Nursing Practice Capstone.
What Clinicians Desire…… 8 Basic Components of Support • A brief respite from the clinical area to allow clinician to ‘regroup’ • Ensure a just, no-blame approach • Educate clinicians about safety investigations, the second victim experience & institutionally sanctioned support networks prior to event. • Ensure a systemic review of the event with opportunity for feedback and reflection on care rendered.
What Clinicians Desire (continued) 8 Basic Components of Support • • Ensure internal support team is available 24/7. Ensure a predictable f/u with second victim. Provide confidential services. Provide services that are individualized based on the unique needs of the clinician.
What Should Support Look Like? Confidential 24/7 availability Voluntary clinician participation ‘Fast track’ referral to support/guidance Types of support offered – peer, 1: 1, team Who can fulfill role of support
The for. YOU Team is Formed • Incorporates evidence-based findings • Peer to peer support model • Referral systems coordinated to facilitate prompt referrals when necessary • Two Types of Supportive Intervention One-On-One Group Debriefings
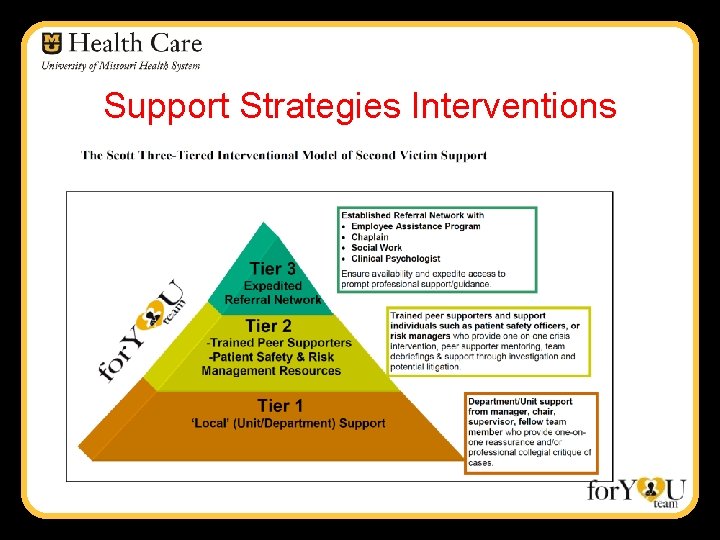
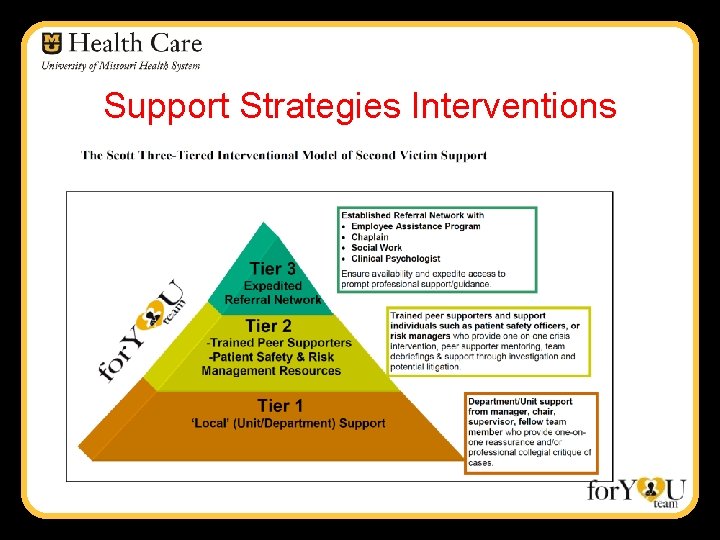
Support Strategies Interventions
Tier One – ‘Local’ support Five Key Actions – Department Leaders • • • Connect with clinical staff involved Reaffirm confidence in staff Consider brief respite/calling in flex staff Notify staff of next steps – keep them informed Check on them regularly
Basic Support Strategies �Be a good listener! �Do not try to fix it… �Provide �Let emotional first aid them know you care… �Avoid second-guessing performance
Tier Two – Peers! • One on one peer support • Team De-Briefings
Peer Supporters • Personal Characteristics – High Emotional Intelligence – Respect and Trust of Peers – Ability to Keep Confidences – Effective Communication Skills – Empathic – Non-judgmental
Providing peer support �Talk through the experience �Listen to the story �Help put incident in perspective �Used as a “band-aide”
The Supportive Interaction 1. 2. 3. 4. Introduction Exploration Information Follow-up
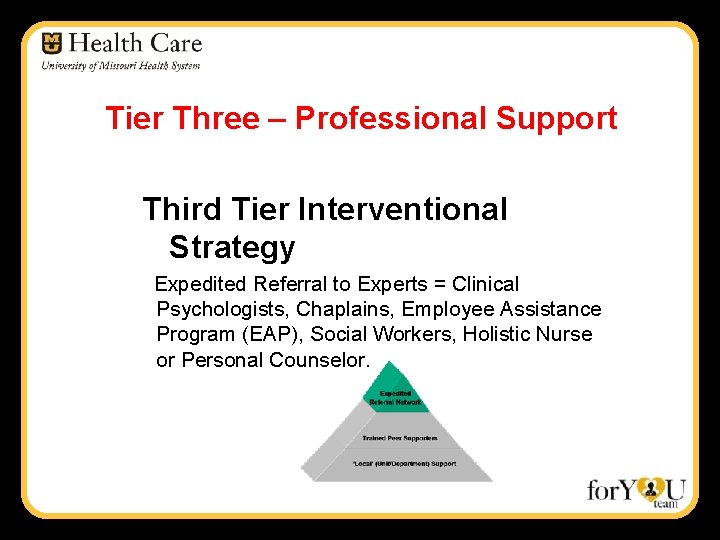
Tier Three – Professional Support Third Tier Interventional Strategy Expedited Referral to Experts = Clinical Psychologists, Chaplains, Employee Assistance Program (EAP), Social Workers, Holistic Nurse or Personal Counselor.
for. YOU Team Objectives…. • Minimize the human toll when unanticipated adverse events occur. • Provide a ‘safe zone’ for faculty and staff to receive support to mitigate the impact of an adverse event. • an internal rapid response infrastructure of ‘emotional first aid’ for clinicians and personnel following an adverse event.
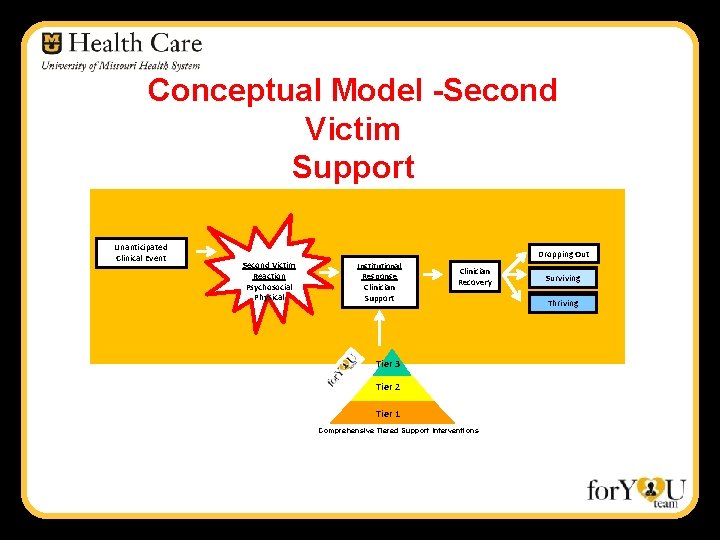
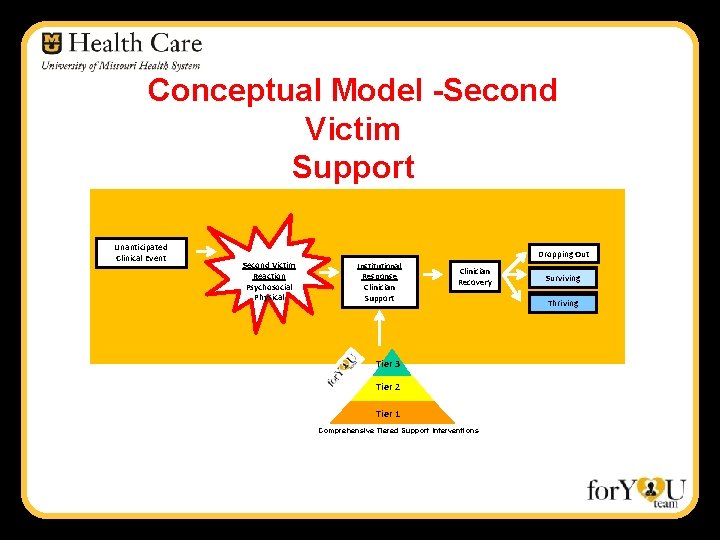
Conceptual Model -Second Victim Support Unanticipated Clinical Event Dropping Out Second Victim Reaction Psychosocial Physical Institutional Response Clinician Support Clinician Recovery Tier 3 Tier 2 Tier 1 Comprehensive Tiered Support Interventions Surviving Thriving
Lessons Learned Nine Years of Support……. 04/01/2009 to 3/31/2018
Clinician Support No two clinicians have the same support needs! Awareness is the first intervention – Proactively plan & educate regarding institutional response plan Fear of the unknown (next steps) is profound
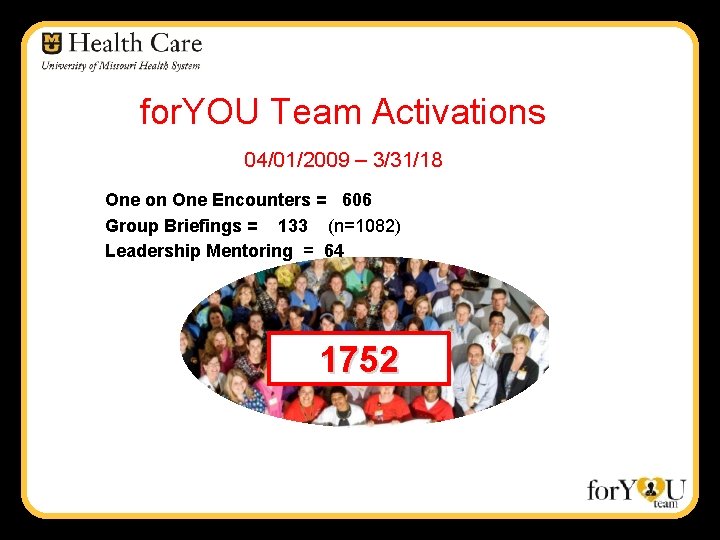
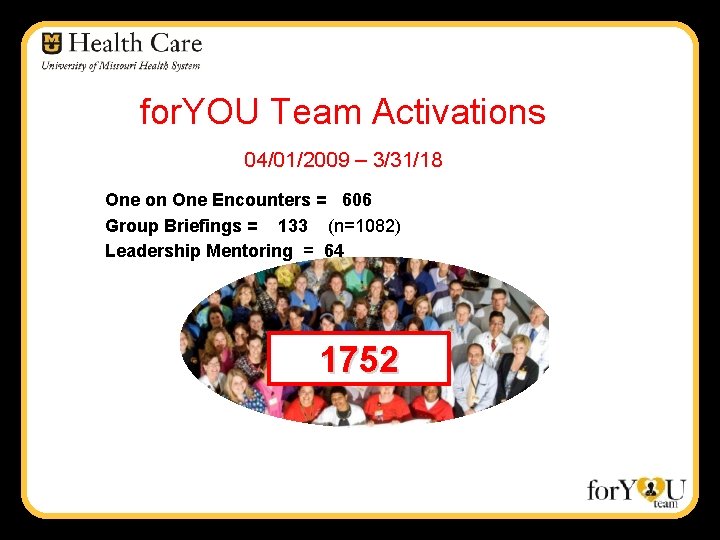
for. YOU Team Activations 04/01/2009 – 3/31/18 One on One Encounters = 606 Group Briefings = 133 (n=1082) Leadership Mentoring = 64 1752
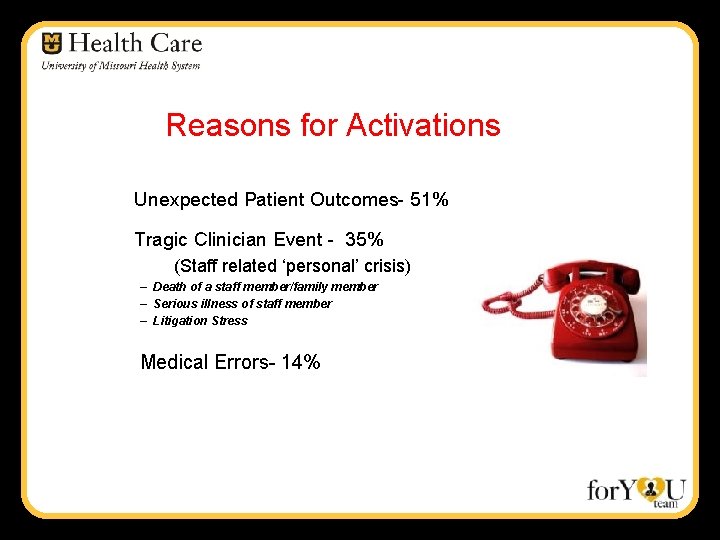
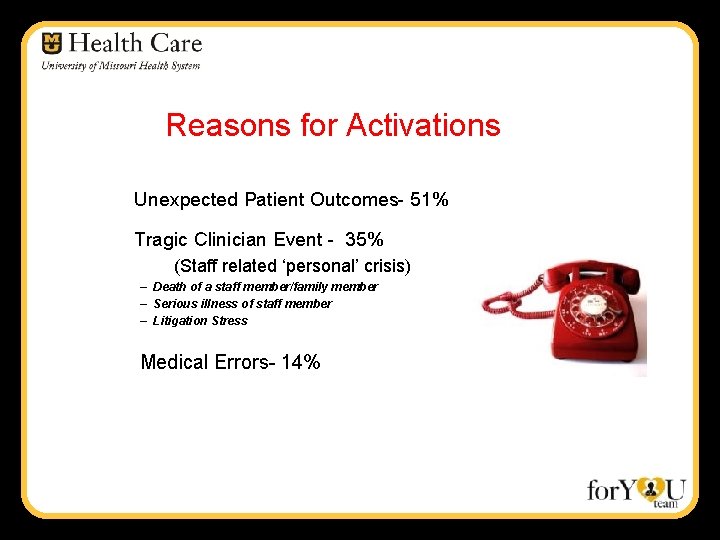
Reasons for Activations Unexpected Patient Outcomes- 51% Tragic Clinician Event - 35% (Staff related ‘personal’ crisis) – Death of a staff member/family member – Serious illness of staff member – Litigation Stress Medical Errors- 14%
for. YOU Team Impact “There is always a window of opportunity…. . I had questioned myself, staying as a trauma nurse. The for. YOU Team was able to intervene at appropriate timing and within my window of opportunity to stay as a trauma nurse. And today – a year later – I feel better than ever!” Second Victim RN
Research Informed - Guidelines for Clinician Care Institute for Health Care Improvement http: //www. ihi. org/knowledge/Pages/IHIWhite. Papers/Respectful. Management. Serious. Clinical. AEs. White. Paper. aspx
Research Informed Regulatory Guidelines LD. 04. 05 – EP 9 The leaders make support systems available for staff who have been involved in an adverse of sentinel event. http: //www. jointcommission. org/improving_Patient_Worker_Safety/
Research Informed Resources: AHRQ – CANDOR Tool http: //www. ahrq/gov/professionals/qulaity-patient-safety/patient-safety-resources/candor

Research Informed Resources: Medically Induced Trauma Support Services www. mitss. org
Final Thoughts…. • The most desired form of support is from a respected colleague. • Higher physical distress and lower institutional support are associated with turnover intent • Higher physical distress and lower colleague support are associated with absenteeism • Perhaps programs that provide peer support will also contribute to less burnout and the impact it has on health care providers Quillivan, R. , Burlison, J. , Browne, E. , Scott, SD. , and Hoffman, JM. (2016). Patient safety culture and the second victim phenomenon: Connecting culture to staff distress in nurses.
What Can You Do Differently Tomorrow? • Understand the concept of Second Victims • Talk about the Second Victim concept and spread the word – Awareness is the first intervention! • Determine a way that you can make an individual difference. • If you are worried about a colleague >>> Reach Out! • ‘Be there’!
A Closing Thought…. “Any is Too Many…”
Questions… “Helping one person might not change the whole world, but it could change the world for one Akanksha Raj person. ”
References • • • Chantler, C. (1999). Lancet. 353: 1178 -91. James, J. T. (2013). A new, evidence-based estimate of patient harms associated with hospital care. Journal of Patient Safety, 9(3), 122 -128. Kohn, LT, Corrigan, JM, & Donaldson, MS. (2000). To err is human: building a safer health system. Washington, D. C. : National Academy of Sciences Press. Rodriquez, J. & Scott, S. D. (2017). Dropping out and starting over: The impact of adverse events on clinicians. Joint Commission Journal on Quality and Patient Safety. 44: 137 -145. DOI: 10. 1016/j. jcjq. 2017. 08. 008. Scott, S. D. & Mc. Coig, M. (2016). Care at the point of impact – Insights into the second victim experience. Journal of Healthcare Risk Management. 35(4), 6 -13. Scott, SD. Second victim support: Implications for patient safety attitudes and perceptions. Patient Safety & Quality Healthcare. 2015. 12(5), 26 -31. Scott SD, Hirschinger LE, Cox KR, Mc. Coig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider "second victim" after adverse patient events. Qual Saf Health Care. 2009 Oct; 18(5): 325 -30. Scott SD, Hirschinger LE, Cox KR, Mc. Coig M, Hahn-Cover K, Epperly KM, et al. Caring for our own: deploying a system-wide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010 May; 36(5): 233 -40. Wu, AW. Medical error: The second victim. The doctor who makes the mistake needs help too. BMJ. 2000 Mar 18; 320(7237): 726 -7.
 Jean watson theory
Jean watson theory Norco high school mascot
Norco high school mascot Mobile team challenge
Mobile team challenge Unanticipated problem vs adverse event
Unanticipated problem vs adverse event Who is hurt and who is helped by unanticipated inflation
Who is hurt and who is helped by unanticipated inflation Cost of unanticipated inflation
Cost of unanticipated inflation Analytical sae examples
Analytical sae examples Iliad clinical decision support system
Iliad clinical decision support system Clinical research support services
Clinical research support services Isabel clinical decision support
Isabel clinical decision support Sharjah our own school boy school
Sharjah our own school boy school Come let us create man in our own image
Come let us create man in our own image A future not our own poem
A future not our own poem Thinking affects our language which then affects our
Thinking affects our language which then affects our Our census our future
Our census our future Christ, be our light
Christ, be our light Our life is what our thoughts make it
Our life is what our thoughts make it We bow our hearts
We bow our hearts Our census our future
Our census our future Our life is what our thoughts make it
Our life is what our thoughts make it Summary of poem money madness
Summary of poem money madness Awareness of ourselves and our environment is:
Awareness of ourselves and our environment is: Awareness of ourselves and our environment is:
Awareness of ourselves and our environment is: God our father christ our brother
God our father christ our brother Our future is in our hands quotes
Our future is in our hands quotes Awareness of ourselves and our environment
Awareness of ourselves and our environment Awareness of ourselves and our environment
Awareness of ourselves and our environment Signal words example
Signal words example In your notebook define the following terms in your own
In your notebook define the following terms in your own Fspos vägledning för kontinuitetshantering
Fspos vägledning för kontinuitetshantering Novell typiska drag
Novell typiska drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Tidböcker
Tidböcker