SWARMing Adverse Events to Promote Safe Care and



















- Slides: 37

SWARMing Adverse Events to Promote Safe Care and a Culture of Safety ** add cartoon KSHRM annual meeting November 16, 2018 Paula Holbrook, RN, BHS, JD, CPHRM Associate Director, Risk Management Associate General Counsel pjholbrook@uky. edu

Objectives • Attendees will be able to describe the SWARMing process • Attendees will understand how the SWARMing process is conducted within the PSES umbrella and protected by the Patient Safety and Quality Improvement Act -2 -

HIGH PERFORMANCE, HIGH QUALITY, HIGH RELIABILITY ORGANIZATIONS Steven Spear Identified 4 Key Capabilities of High Performing Organizations KEY CAPABILITY #2 SWARMING This is a characteristic of high velocity (high performing) organizations. They don’t allow workarounds or allow delays between when problem happens and when it is solved. They don’t let problems be solved by people not directly involved with the problem. Delays in solving the problem can mean information and material can be lost. It can also mean the problem can multiply before it is fixed. Swarming means giving people a tool and an expectation to solve problems…to go fix things… to not accept when things don’t work perfectly. 1. STOP WHEN PROBLEMS OCCUR 2. FIX PROBLEMS AS CLOSE TO WHEN THEY OCCUR AS POSSIBLE The closer in time and space the problem is identified the better. -3 -
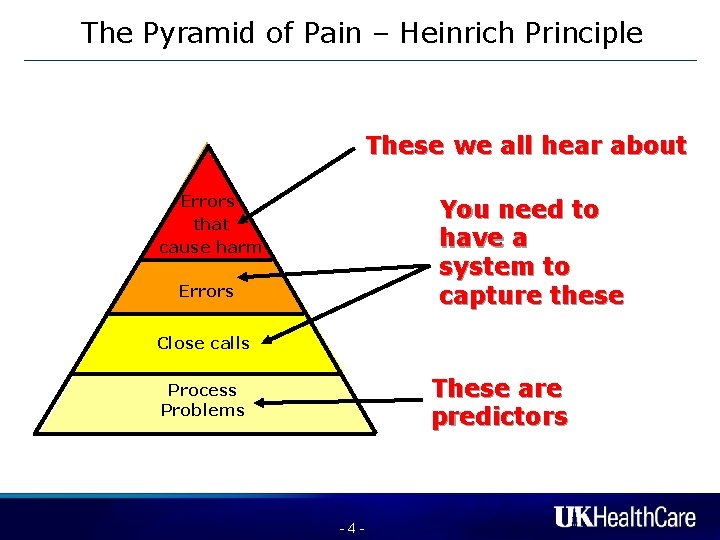
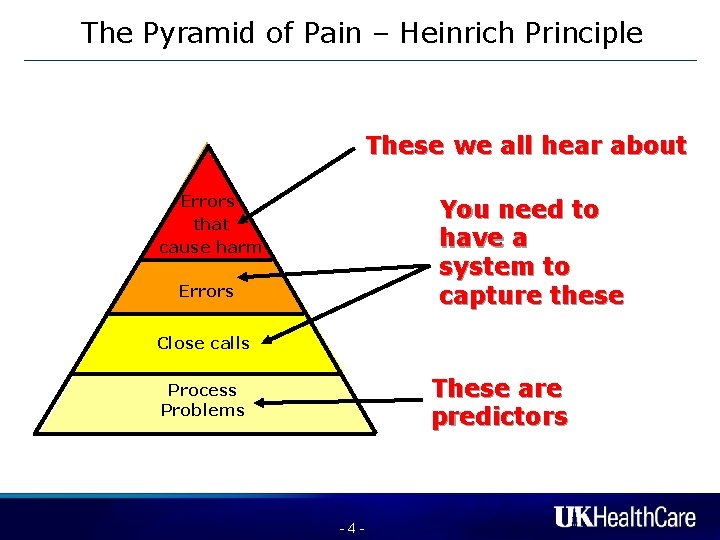
The Pyramid of Pain – Heinrich Principle These we all hear about Errors that cause harm You need to have a system to capture these Errors Close calls These are predictors Process Problems -4 -
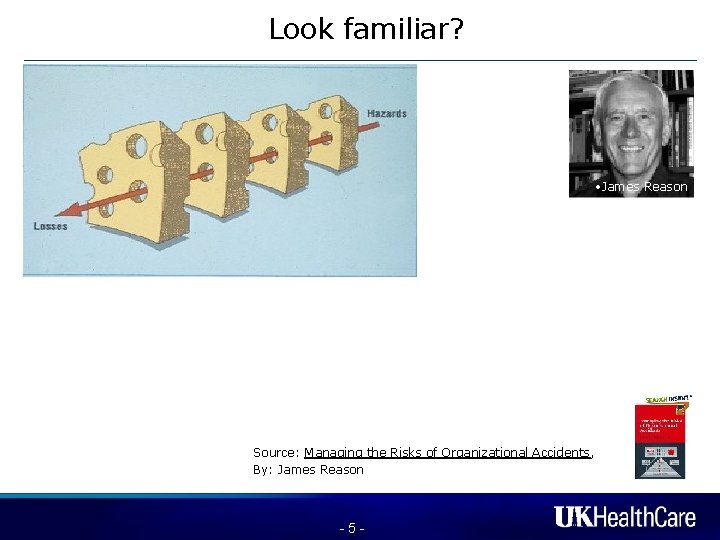
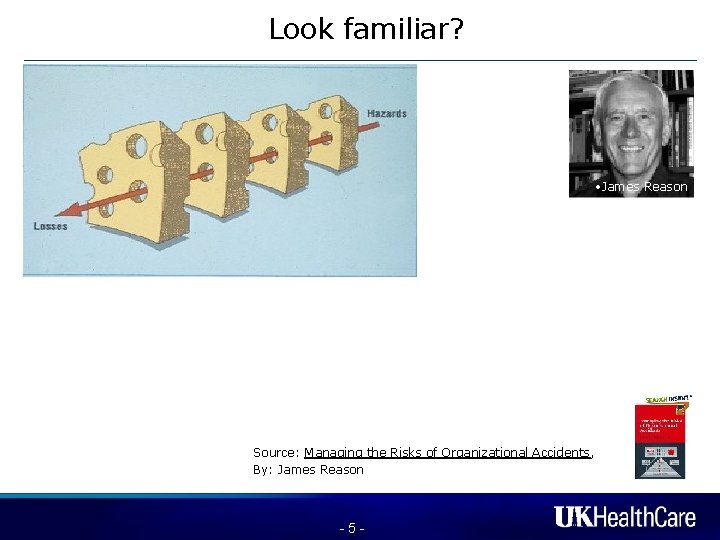
Look familiar? • James Reason Source: Managing the Risks of Organizational Accidents, By: James Reason -5 -
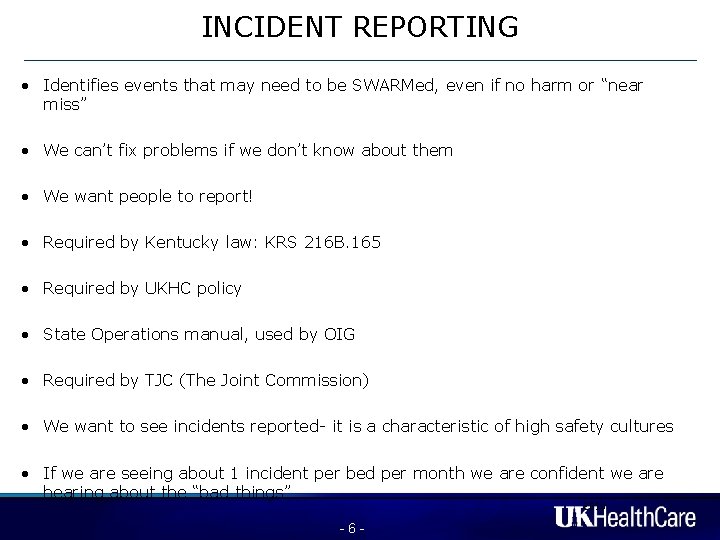
INCIDENT REPORTING • Identifies events that may need to be SWARMed, even if no harm or “near miss” • We can’t fix problems if we don’t know about them • We want people to report! • Required by Kentucky law: KRS 216 B. 165 • Required by UKHC policy • State Operations manual, used by OIG • Required by TJC (The Joint Commission) • We want to see incidents reported- it is a characteristic of high safety cultures • If we are seeing about 1 incident per bed per month we are confident we are hearing about the “bad things” 2010 -6 -
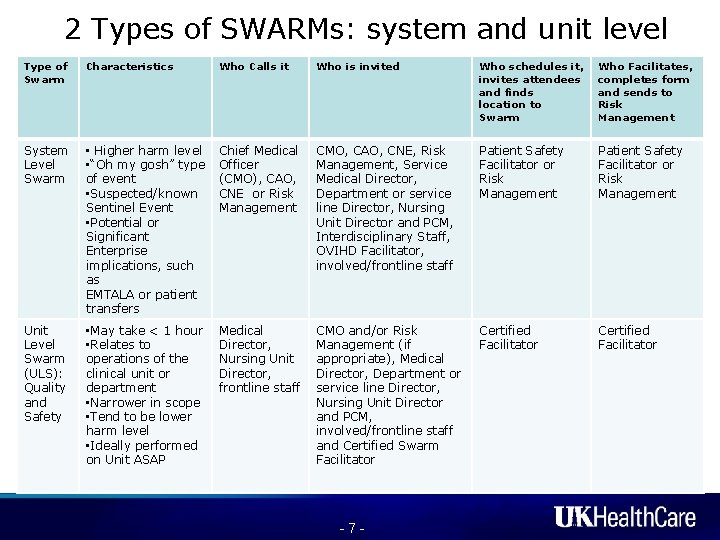
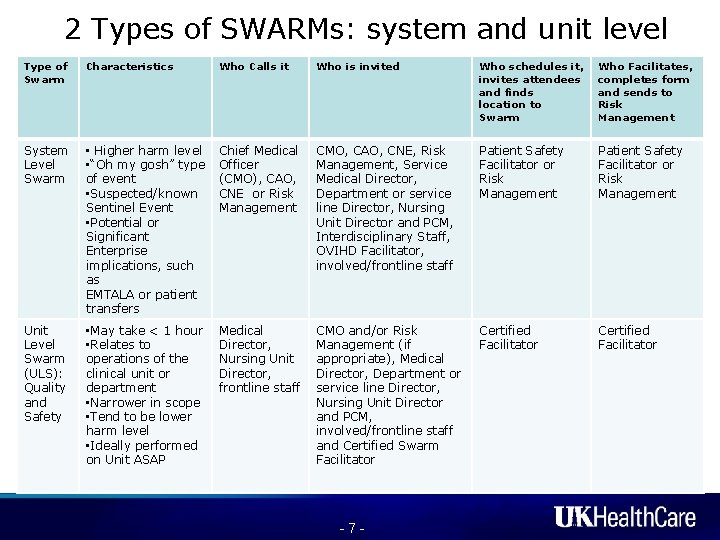
2 Types of SWARMs: system and unit level Type of Swarm Characteristics Who Calls it Who is invited Who schedules it, invites attendees and finds location to Swarm Who Facilitates, completes form and sends to Risk Management System Level Swarm • Higher harm level • “Oh my gosh” type of event • Suspected/known Sentinel Event • Potential or Significant Enterprise implications, such as EMTALA or patient transfers Chief Medical Officer (CMO), CAO, CNE or Risk Management CMO, CAO, CNE, Risk Management, Service Medical Director, Department or service line Director, Nursing Unit Director and PCM, Interdisciplinary Staff, OVIHD Facilitator, involved/frontline staff Patient Safety Facilitator or Risk Management Unit Level Swarm (ULS): Quality and Safety • May take < 1 hour • Relates to operations of the clinical unit or department • Narrower in scope • Tend to be lower harm level • Ideally performed on Unit ASAP Medical Director, Nursing Unit Director, frontline staff CMO and/or Risk Management (if appropriate), Medical Director, Department or service line Director, Nursing Unit Director and PCM, involved/frontline staff and Certified Swarm Facilitator Certified Facilitator -7 -

SWARM • You may be consulted for participation in or to facilitate a “SWARM. ” • Looks like: shortly after the occurrence of an incident or undesirable event, the people directly involved meet and in a blame-free way quickly analyze what happened, why and how it happened, and decide what needs to be done to prevent it from happening in the future. • Possible tools to use: timeline/flowchart, Go-See, Fishbone, Pareto, 5 -Whys • 2010

SWARM Fishbone Diagram • Epidemiologic Knowledge • Treatment Choices (decision making) • Diagnostic Reasoning • Clinical Assessment • Bias • Outcome • Staff • Power Structure • Staffing • Handoffs/Communi • Personnel/ cation (including People escalation) • Protocol Process • Environment
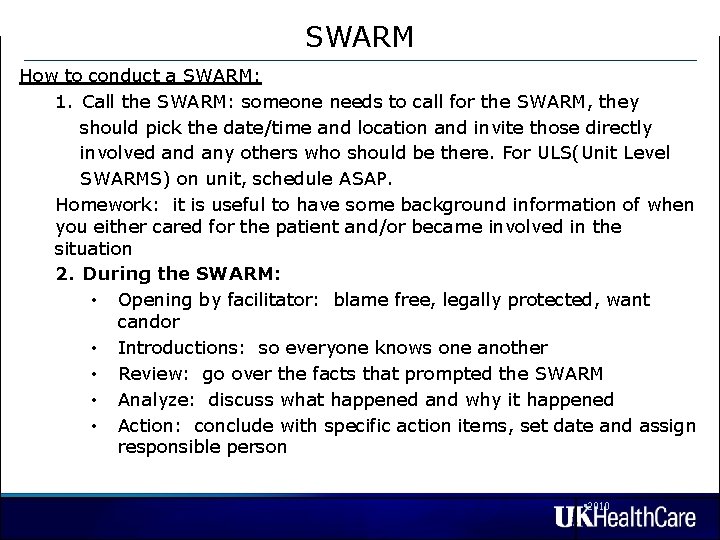
SWARM How to conduct a SWARM: 1. Call the SWARM: someone needs to call for the SWARM, they should pick the date/time and location and invite those directly involved any others who should be there. For ULS(Unit Level SWARMS) on unit, schedule ASAP. Homework: it is useful to have some background information of when you either cared for the patient and/or became involved in the situation 2. During the SWARM: • Opening by facilitator: blame free, legally protected, want candor • Introductions: so everyone knows one another • Review: go over the facts that prompted the SWARM • Analyze: discuss what happened and why it happened • Action: conclude with specific action items, set date and assign responsible person • 2010

Who can facilitate a Unit Level Swarm Anyone including who has been SWARM certified. How to become SWARM certified: • Attend this course • Attend at least 1 unit level SWARM- you will be invited • Facilitate a unit level SWARM on your unit with Paula Holbrook or Jamie Grabowski present • Complete the unit level SWARM form and forward to Paula Holbrook and Jamie Grabowski - 11 -
WHAT TO SWARM • Adverse clinical events • Sentinel events • Clinical surprises “I wonder how that happened? ” • Things that make you go “Hmmm…” • Unusual chain of events • Simple matters • Complex matters - 12 -
WHAT NOT TO SWARM Intentionally unsafe acts Criminal acts David Marx Physician judgment Situations involving alcohol/substance abuse by employees Based On The Works of: David Marx, Just Culture James Reason, Managing the Risk of Organizational Accidents - 13 - James Reason
WHO SHOULD ATTEND? It depends…………… dictated by the circumstances and issues…………. ………frontline staff, hospital leadership/administration, attending physicians, housestaff, nursing leadership, security, housekeeping, pharmacy…

Standard SWARM invitation - patient care/clinical issues Please make every effort to attend or send a representative. Issues to be discussed are patient safety risks. Thank you. PROBLEM: This SWARM relates to patient, ______, MR#_______, regarding ___________________. In your review, you may also refer to SI#: _____. YOU ARE INVITED: On behalf of __________, you are receiving this invitation to a SWARM, because you were either a direct caregiver, consulted, or are responsible for the unit, department or service line. WHAT IS A SWARM? A SWARM is a type of root cause analysis conducted in a blameless environment which provides an opportunity to candidly share concerns for patient quality and safety as well as your insight and ideas for appropriate identification of system opportunities to improve care. This activity is protected from discovery by the Patient Safety Act. WHAT DO YOU NEED TO DO: In advance of the SWARM, please review the medical records of the patient(s) involved, as well as any applicable policy, procedure or protocol, and be prepared to discuss the events and propose workable solutions. TO MAINTAIN OUR LEGAL PROTECTION: • Please do not discuss this matter outside the protected environment of UK Health. Care’s PSES. • Please limit email and casual discussion of this matter. • Please consult with the SWARM scheduler/ and or Risk management if additional individuals are needed. • Do not forward this invitation except to your direct Manager or Director. - 15 -

Standard SWARM invitation - other issues PROBLEM: This SWARM relates to _________, on XX/XX/XXXX. In your review, you may also refer to SI-_____. YOU ARE INVITED: On behalf of __________, you are receiving this invitation to a SWARM, because you were either a direct caregiver, consulted, or are responsible for the unit, department or service line. WHAT IS A SWARM? A SWARM is a type of root cause analysis conducted in a blameless environment which provides an opportunity to candidly share concerns for patient quality and safety as well as your insight and ideas for appropriate identification of system opportunities to improve care. This activity is protected from discovery by the Patient Safety Act. WHAT DO YOU NEED TO DO: In advance of the SWARM, please review the medical records of the patient(s) involved, as well as any applicable policy, procedure or protocol, and be prepared to discuss the events and propose workable solutions. TO MAINTAIN OUR LEGAL PROTECTION: • Please do not discuss this matter outside the protected environment of UK Health. Care’s PSES. • Please limit email and casual discussion of this matter. • Please consult with the SWARM scheduler if additional individuals need to attend • Do not forward this invitation except to your direct Manager or Director. - 16 -

SWARM TOOL KIT • • • Timeline/flowchart Dry Erase board if available SMART Board Color coded table Go-See/demonstration- helpful with equipment and environmental factors Fishbone Pareto Schedule queue/workflow diagram 5 -Whys EMR screen shots *Camera (take photo of notes/board to include in write-up) - 17 -
SWARM – WHAT NOT TO DO • JUST MANAGEMENT • SO FORMAL PEOPLE FOCUS ON PROCESS… AND NOT PROBLEMS - 18 -

SWARM – WHAT NOT TO DO • • • WARNINGS: (Things that keep the swarm from working well) Delaying before holding the swarm- the sooner the better Getting caught up in tools and forms and not focusing on what really caused the problem to happen and what to do about it Not having the right people present; to be effective, Swarms need to include front line staff who are directly involved in the incident Overuse of the tool- causes fatigue and stresses the system Blame and shame…………. Use of SWARM to displace leadership action and responsibility for management issues - 19 -
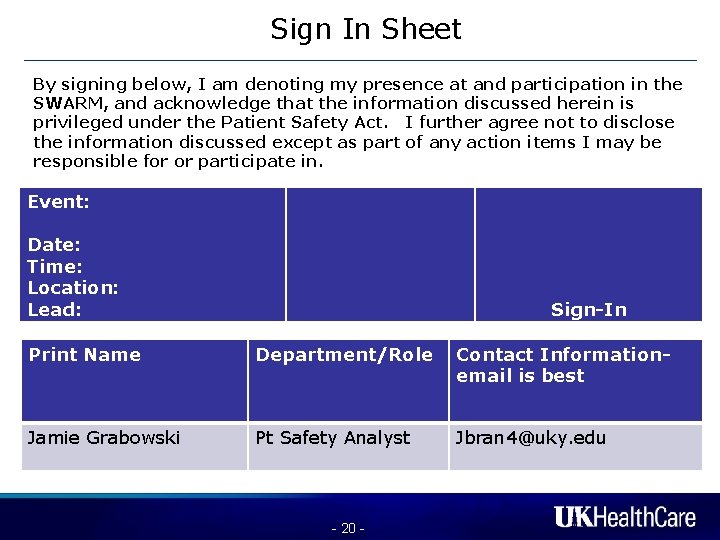
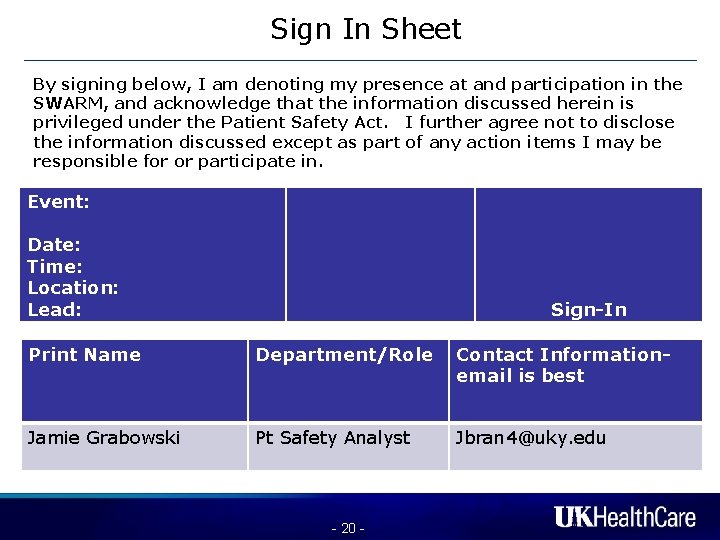
Sign In Sheet By signing below, I am denoting my presence at and participation in the SWARM, and acknowledge that the information discussed herein is privileged under the Patient Safety Act. I further agree not to disclose the information discussed except as part of any action items I may be responsible for or participate in. Event: Date: Time: Location: Lead: Sign-In Print Name Department/Role Contact Informationemail is best Jamie Grabowski Pt Safety Analyst Jbran 4@uky. edu - 20 -

Before the Swarm • Decide who should attend and when to meet - the closer to the event, the more effective • Gather supplies: Sign-in sheet, dry erase markers, camera, a quiet setting; • Remember not to Swarm employment matters, criminal acts, physician judgment - 21 -
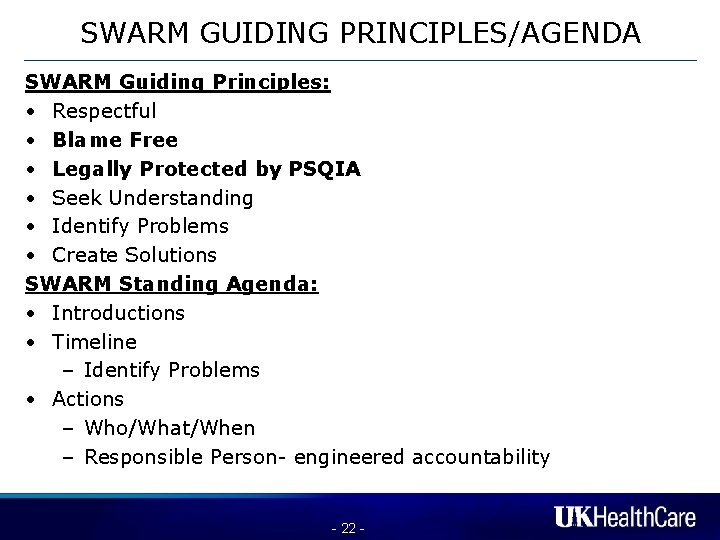
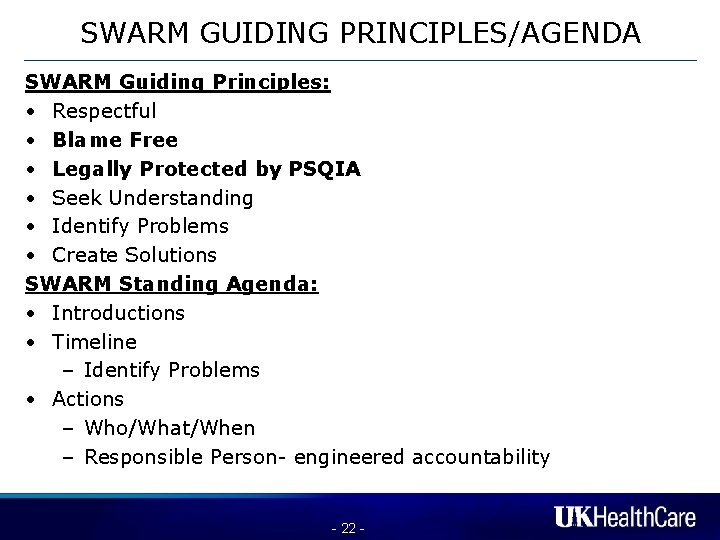
SWARM GUIDING PRINCIPLES/AGENDA SWARM Guiding Principles: • Respectful • Blame Free • Legally Protected by PSQIA • Seek Understanding • Identify Problems • Create Solutions SWARM Standing Agenda: • Introductions • Timeline – Identify Problems • Actions – Who/What/When – Responsible Person- engineered accountability - 22 -
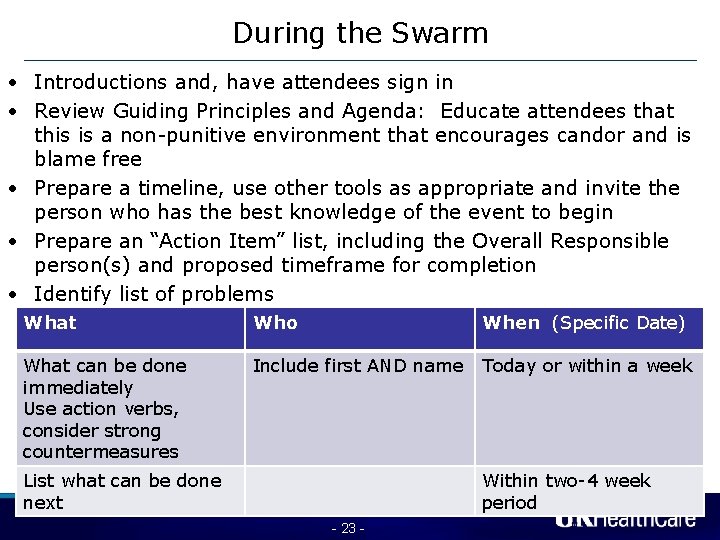
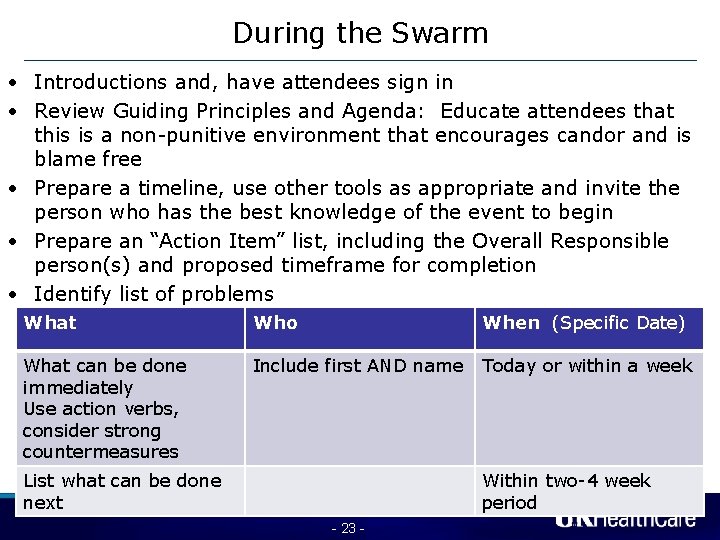
During the Swarm • Introductions and, have attendees sign in • Review Guiding Principles and Agenda: Educate attendees that this is a non-punitive environment that encourages candor and is blame free • Prepare a timeline, use other tools as appropriate and invite the person who has the best knowledge of the event to begin • Prepare an “Action Item” list, including the Overall Responsible person(s) and proposed timeframe for completion • Identify list of problems What Who When (Specific Date) Overall “Responsibility”: _____ What can be done immediately Use action verbs, consider strong countermeasures Include first AND name List what can be done next Today or within a week Within two-4 week period - 23 -
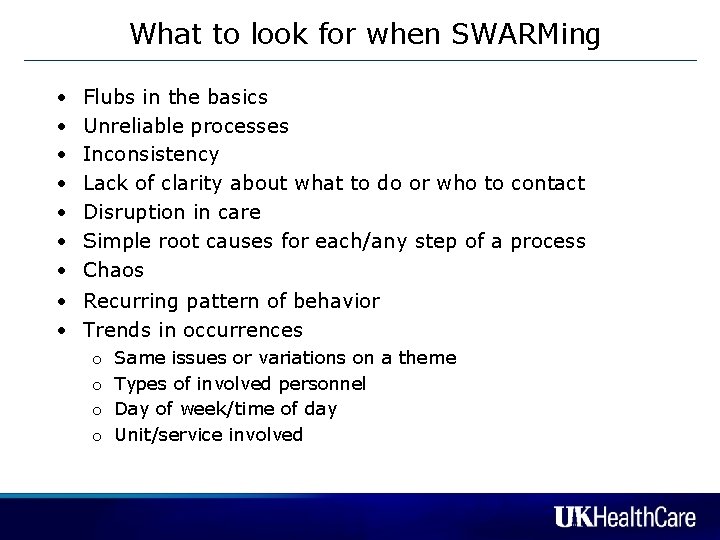
What to look for when SWARMing • • Flubs in the basics Unreliable processes Inconsistency Lack of clarity about what to do or who to contact Disruption in care Simple root causes for each/any step of a process Chaos • Recurring pattern of behavior • Trends in occurrences o o Same issues or variations on a theme Types of involved personnel Day of week/time of day Unit/service involved

Concluding the Swarm • Review white board & action item list to see if everyone is in agreement • Set a date when to meet again, if applicable or • Set a time when the findings will be completed -usually is the latest date on the Action Plan, but no greater than 60 days • Thank everyone for attending • Complete Swarm Form and forward institutional designee: Ex: pjholbrook@uky. edu (Paula Holbrook) and jbran 4@uky. edu (Jamie Grabowski) - 25 -

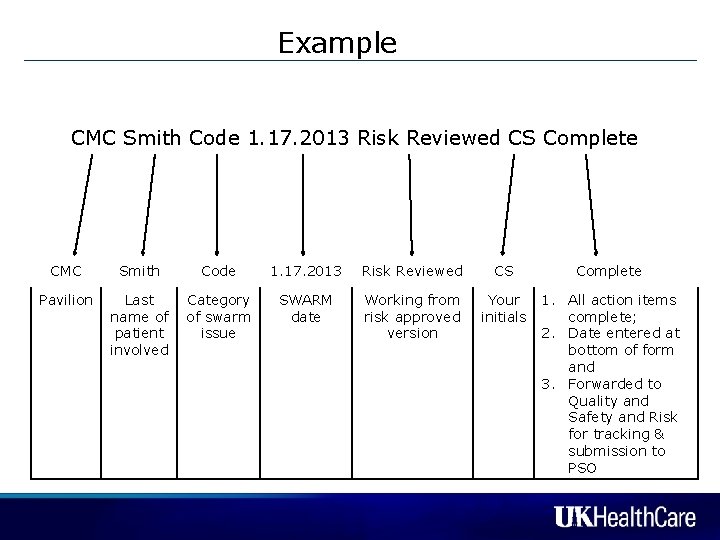
As the person having the “R” you are responsible for: ◦ Ensuring that the action items are completed, and determining whether the items are achievable ◦ Escalating to your “ 1 up” if there are barriers or the item becomes unachievable/unmanageable ◦ Documenting closure of the SWARM When all items are completed, denote “Complete” in the status column, rename the document too include your initials and completion date and send form to Mary Moore and Paula Holbrook Example: “CMC Holbrook Code 1. 17. 2013 Risk reviewed CS Complete”
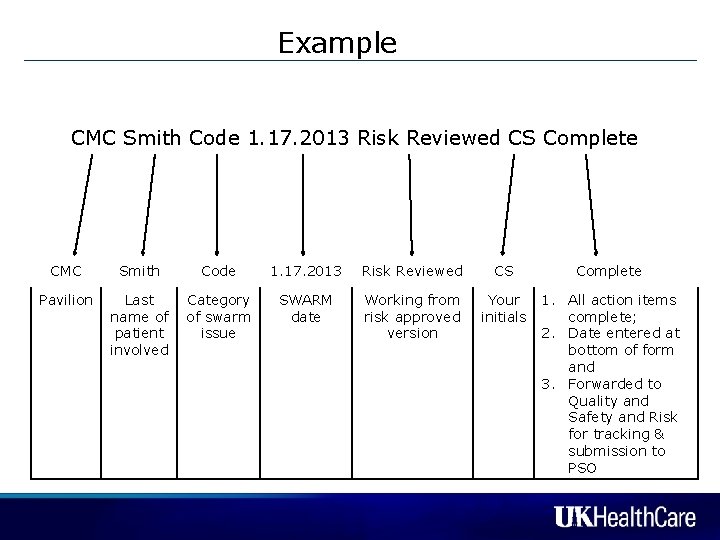
Example CMC Smith Code 1. 17. 2013 Risk Reviewed CS Complete CMC Pavilion Smith Code Last Category name of of swarm patient issue involved 1. 17. 2013 Risk Reviewed CS SWARM date Working from risk approved version Your initials Complete 1. All action items complete; 2. Date entered at bottom of form and 3. Forwarded to Quality and Safety and Risk for tracking & submission to PSO

Protecting PSWP Revised method For e-mails related to SI reports, SWARMs, adverse events, action items, SWARM follow up : – Include “PSWP” in the cc or “To” line of the email for general patient safety (as if PSWP were an individual) – Emails will go to “pswp@uky. edu” address for review by Risk and placement in our secure PSWP repository – Use the confidentiality statement recommended by Corporate Compliance For documents/powerpoints: all documents that contain patient safety work product should still include the PSWP language and need to be sent to pswp@uky. edu address - 28 -
SIMPLE RULE! If you want to protect a communication or document or data as Patient Safety Work Product so that it can’t be produced in a lawsuit or to someone outside of UK: Send it to: pswp@uky. edu address Risk Management will be responsible for sorting all information that comes into the mailbox to submit it to our PSO. - 29 -

Helpful Hints • OVERUSE of the PSES/PSWP heading or e-mail descriptor threatens to dilute the validity of our claim of privilege • DO NOT send routine e-mails regarding meetings, personnel issues, scheduling, or discussions of patient complaints not involving patient safety to pswp@uky. edu address. Use only when the issue discussed pertains to a valid patient safety event or concern or the quality of patient care • Do not provide copies of individual or aggregated SI reports or SWARM documents outside the normal chain of distribution; vet all such request through Risk • In reporting an incident via Safety Intelligence, do not use the narrative section of this report to criticize or place blame. Report the facts. • Refer all questions about applicability of PSWP to Risk Management

What to do with your findings Build solutions/Build collaboration Act on the findings: follow up is key Evaluate current policies Brainstorm using institutional experts Solicit help from outside experts Conduct literature searches Conduct trials of small cycles of change or limited initial implementation • Spend time on the clinical units • Focus on action and learning • • •
What to do next • Make SWARMs part of your daily work • Start slow, start small • Continue to refine the process to foster collaboration between services and departments and hardwire completion dates of action items • Share results to foster learning and improve care • Educate more staff to expand the SWARM process to unit level activity and reinforce culture of safety

Take AWAY Points • • • Valuable tool to mine rich target Blameless Productive Collaborative Focus on facts and process improvement and action items • Learn together • Adaptable process • Patients are safer and care is better - 33 -

Examples of key initiatives from SWARMS • • • Code team reconfiguration Code cart standardization VIR reconfiguration/enhancement/scheduling MRI scheduling Service coordination between cath lab & PICU Insulin drip protocol Elopement risk assessment & response Risk assessment for violent/aggressive behavior Tourniquet color and use protocol Communication plan, including handoffs and disclosure • IV Pumps • 72 Hour hold process
Incident & SWARM Analysis Other observations �IT/EMR events - primarily related to order entry �Pharmacy (involving high risk drugs) (IV electrolyte therapy, heparin, Vancomycin) �SWARM issues are complex, interrelated, and recurring �The SWARM process is a “game changer”; we now have the capacity to do 15 swarms per week at each facility. �The biggest challenge is in following up and implementing action items and key initiatives - 35 -

Potentially SWARMable?
Questions? ? ? ? ? - 37 -
 Swarming incident management
Swarming incident management Swarming proteus
Swarming proteus Adverse events in hospital
Adverse events in hospital Adverse events in hospital
Adverse events in hospital Puerperal sepsis definition
Puerperal sepsis definition Adverse events following immunization (aefi) course answers
Adverse events following immunization (aefi) course answers Safe feed safe food
Safe feed safe food Safe people safe places
Safe people safe places Health care levels primary secondary tertiary
Health care levels primary secondary tertiary Mutually exclusive vs non mutually exclusive
Mutually exclusive vs non mutually exclusive Implement tasks that promote reasoning and problem solving
Implement tasks that promote reasoning and problem solving What is community meal
What is community meal What is fcclas tagline
What is fcclas tagline Promote personal growth
Promote personal growth Protect, promote, and improve the health of all people
Protect, promote, and improve the health of all people What is a significant life event
What is a significant life event Scottish patient safety programme
Scottish patient safety programme Communist manifesto
Communist manifesto Promote service arrange decide
Promote service arrange decide Active learning strategies to promote critical thinking
Active learning strategies to promote critical thinking How to promote bookkeeping services
How to promote bookkeeping services E4 evaluation examples
E4 evaluation examples Ead 520
Ead 520 The monroe doctrine what ideas did the measure contain?
The monroe doctrine what ideas did the measure contain? R051 contemporary issues in sport
R051 contemporary issues in sport How does polymorphism promote extensibility
How does polymorphism promote extensibility Which of the following is a strategy to promote leveling?
Which of the following is a strategy to promote leveling? Promote webtoon
Promote webtoon Active learning strategies to promote critical thinking
Active learning strategies to promote critical thinking Promote active participation
Promote active participation When should you promote hipaa awareness
When should you promote hipaa awareness Kelly gallagher deeper reading
Kelly gallagher deeper reading Advertising is a message designed to promote
Advertising is a message designed to promote Promote together
Promote together How did the mauryan empire’s army help to promote trade?
How did the mauryan empire’s army help to promote trade? Adverse reaction definition
Adverse reaction definition Difference between near miss and unsafe condition
Difference between near miss and unsafe condition Adverse selection
Adverse selection