SURVEILLANCE AND NOVEL RISK FACTORS FOR HEPATOCELLULAR CARCINOMA


- Slides: 23

SURVEILLANCE AND “NOVEL” RISK FACTORS FOR HEPATOCELLULAR CARCINOMA May 2020 Walid S. Ayoub, MD FAASLD Professor of Medicine Associate Medical Director, Liver Transplant Program Cedars Sinai Medical Center, Los Angeles, USA
DISCLAIMER Please note: The views expressed within this presentation are the personal opinions of the author. They do not necessarily represent the views of the author’s academic institution or the rest of the HCC CONNECT group. This content is supported by an Independent Educational Grant from Bayer. Disclosure: Dr. Walid Ayoub has a financial relationship to disclose with Bayer. 3

HCC INCIDENCE • The incidence of HCC has tripled since the 1980 s 1 • Prognosis remains relatively poor 2 – Median OS 13. 8 months HCC, hepatocellular carcinoma; OS, overall survival 1. El-Serag HB, et al. Hepatology. 2014; 60: 1767 -75. 2. Rich NE, et al. Clin Gastroenterol Hepatol. 2019; 17: 551 -9.
PROSPECTIVE EVALUATION OF BENEFITS AND HARMS OF HCC SURVEILLANCE IN A CIRRHOSIS PATIENT POPULATION Patibandla S, et al. AASLD 2019, Abstract #320
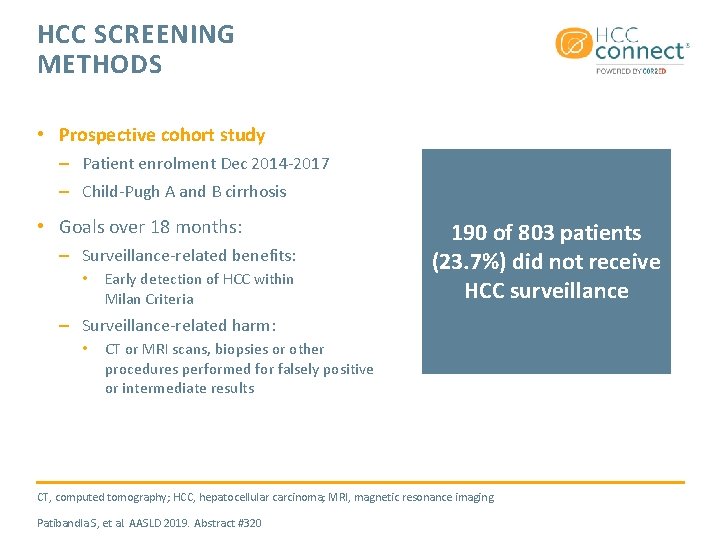
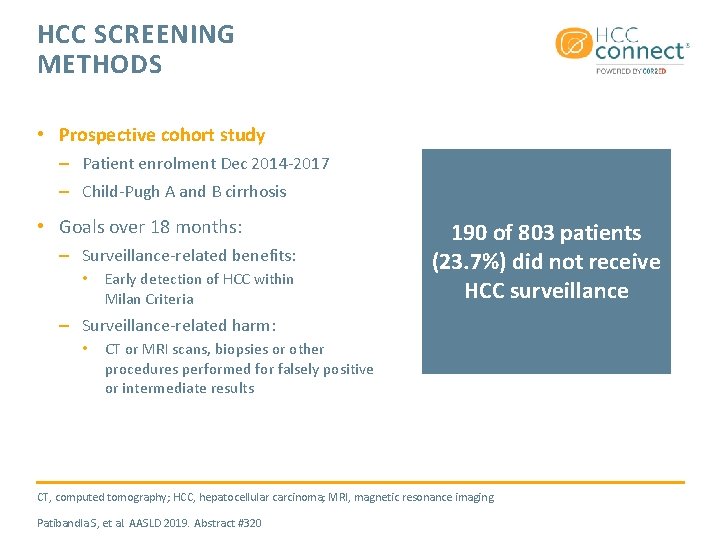
HCC SCREENING METHODS • Prospective cohort study – Patient enrolment Dec 2014 -2017 – Child-Pugh A and B cirrhosis • Goals over 18 months: – Surveillance-related benefits: • Early detection of HCC within Milan Criteria 190 of 803 patients (23. 7%) did not receive HCC surveillance – Surveillance-related harm: • CT or MRI scans, biopsies or other procedures performed for falsely positive or intermediate results CT, computed tomography; HCC, hepatocellular carcinoma; MRI, magnetic resonance imaging Patibandla S, et al. AASLD 2019. Abstract #320
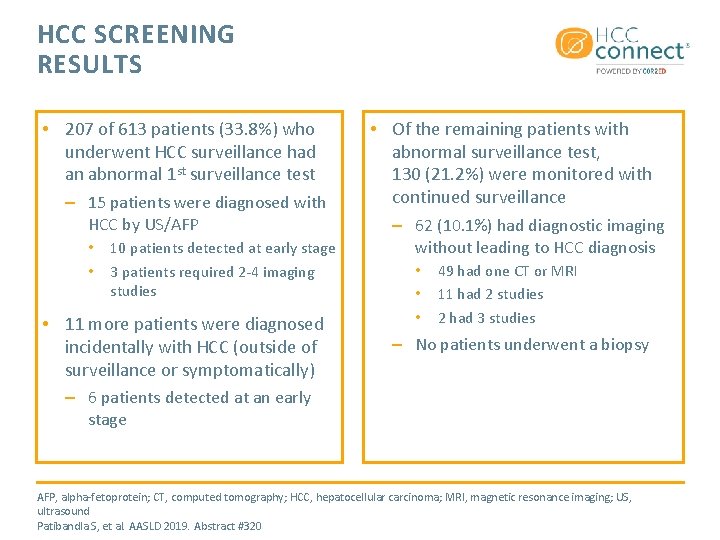
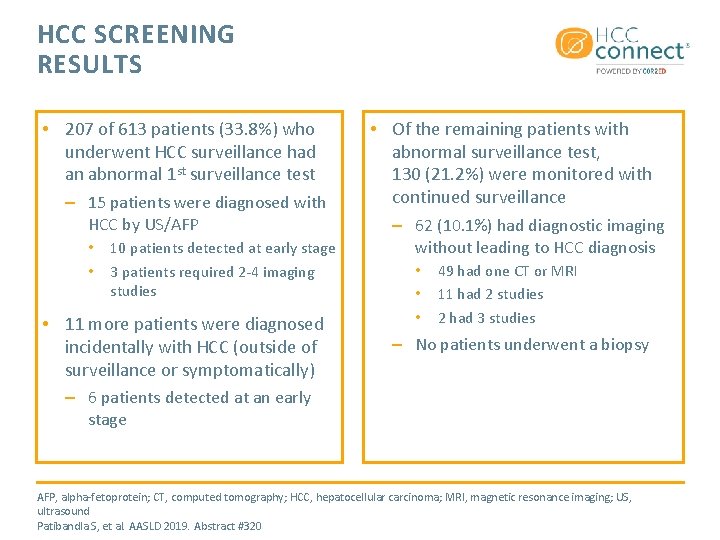
HCC SCREENING RESULTS • 207 of 613 patients (33. 8%) who underwent HCC surveillance had an abnormal 1 st surveillance test – 15 patients were diagnosed with HCC by US/AFP • • 10 patients detected at early stage 3 patients required 2 -4 imaging studies • 11 more patients were diagnosed incidentally with HCC (outside of surveillance or symptomatically) • Of the remaining patients with abnormal surveillance test, 130 (21. 2%) were monitored with continued surveillance – 62 (10. 1%) had diagnostic imaging without leading to HCC diagnosis • • • 49 had one CT or MRI 11 had 2 studies 2 had 3 studies – No patients underwent a biopsy – 6 patients detected at an early stage AFP, alpha-fetoprotein; CT, computed tomography; HCC, hepatocellular carcinoma; MRI, magnetic resonance imaging; US, ultrasound Patibandla S, et al. AASLD 2019. Abstract #320
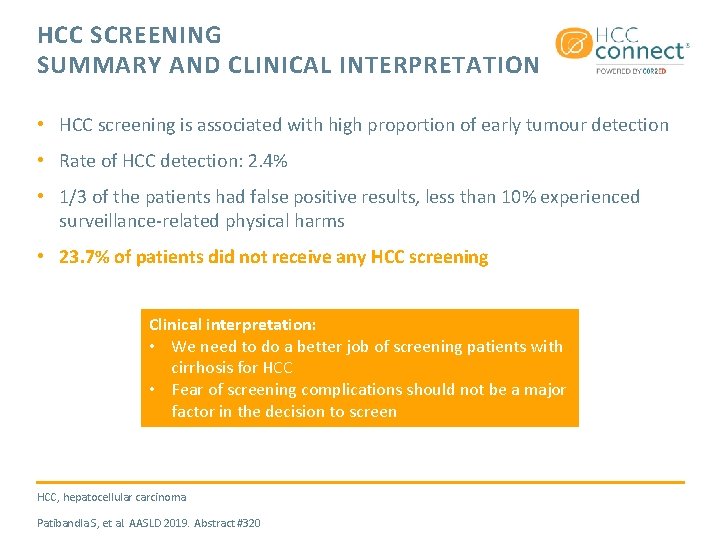
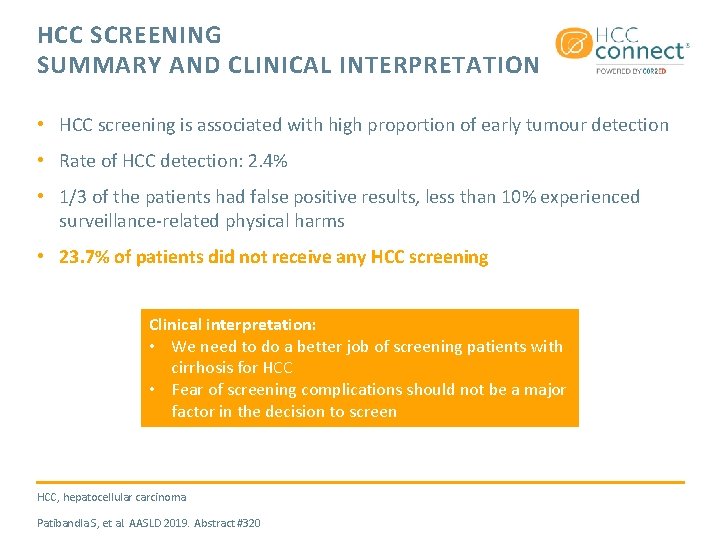
HCC SCREENING SUMMARY AND CLINICAL INTERPRETATION • HCC screening is associated with high proportion of early tumour detection • Rate of HCC detection: 2. 4% • 1/3 of the patients had false positive results, less than 10% experienced surveillance-related physical harms • 23. 7% of patients did not receive any HCC screening Clinical interpretation: • We need to do a better job of screening patients with cirrhosis for HCC • Fear of screening complications should not be a major factor in the decision to screen HCC, hepatocellular carcinoma Patibandla S, et al. AASLD 2019. Abstract #320
ANALYSIS OF PROGNOSTIC FACTORS OF HEPATOCELLULAR CARCINOMA TREATMENT WITHIN MILAN CRITERIA FOR SUPER-ELDERLY PATIENTS Ochi H, et al. AASLD 2019, Abstract #356
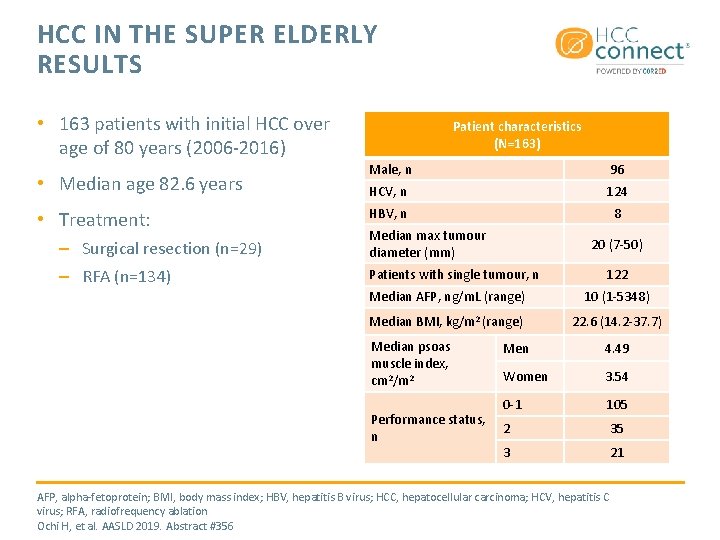
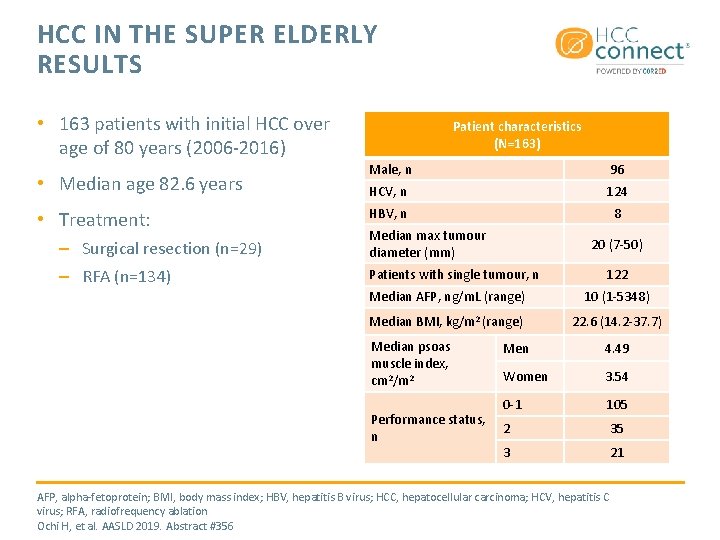
HCC IN THE SUPER ELDERLY RESULTS • 163 patients with initial HCC over age of 80 years (2006 -2016) • Median age 82. 6 years • Treatment: – Surgical resection (n=29) – RFA (n=134) Patient characteristics (N=163) Male, n 96 HCV, n 124 HBV, n 8 Median max tumour diameter (mm) 20 (7 -50) Patients with single tumour, n 122 Median AFP, ng/m. L (range) 10 (1 -5348) Median BMI, kg/m 2 (range) 22. 6 (14. 2 -37. 7) Median psoas muscle index, cm 2/m 2 Performance status, n Men 4. 49 Women 3. 54 0 -1 105 2 35 3 21 AFP, alpha-fetoprotein; BMI, body mass index; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; RFA, radiofrequency ablation Ochi H, et al. AASLD 2019. Abstract #356
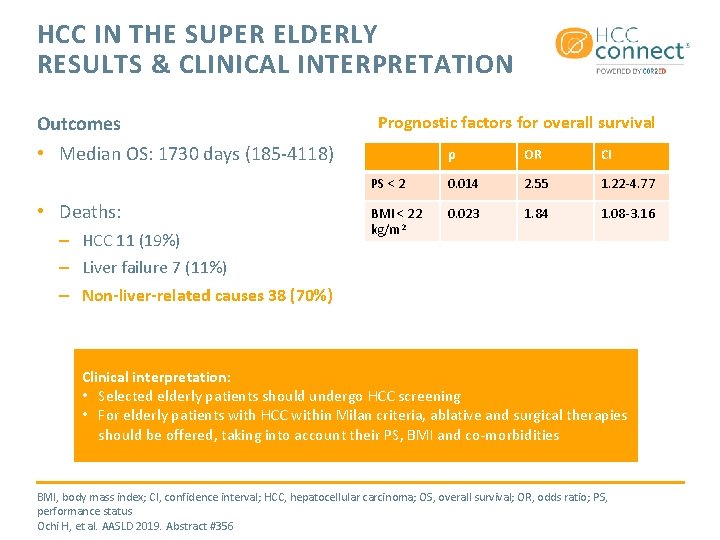
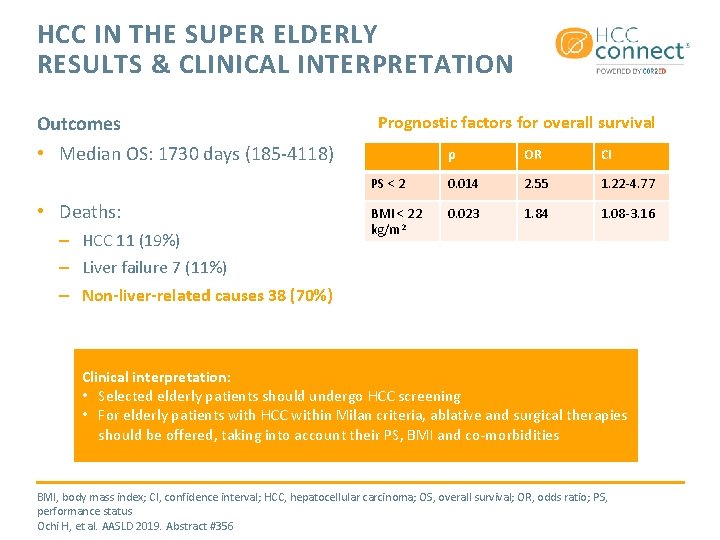
HCC IN THE SUPER ELDERLY RESULTS & CLINICAL INTERPRETATION Outcomes Prognostic factors for overall survival • Median OS: 1730 days (185 -4118) • Deaths: – HCC 11 (19%) – Liver failure 7 (11%) – Non-liver-related causes 38 (70%) p OR CI PS < 2 0. 014 2. 55 1. 22 -4. 77 BMI < 22 kg/m 2 0. 023 1. 84 1. 08 -3. 16 Clinical interpretation: • Selected elderly patients should undergo HCC screening • For elderly patients with HCC within Milan criteria, ablative and surgical therapies should be offered, taking into account their PS, BMI and co-morbidities BMI, body mass index; CI, confidence interval; HCC, hepatocellular carcinoma; OS, overall survival; OR, odds ratio; PS, performance status Ochi H, et al. AASLD 2019. Abstract #356
THE IMPACT OF HEALTHY LIFESTYLE ON THE INCIDENCE OF HEPATOCELLULAR CARCINOMA AND CIRRHOSIS-RELATED MORTALITY AMONG US ADULTS Simon TG, et al. AASLD 2019, Abst #16
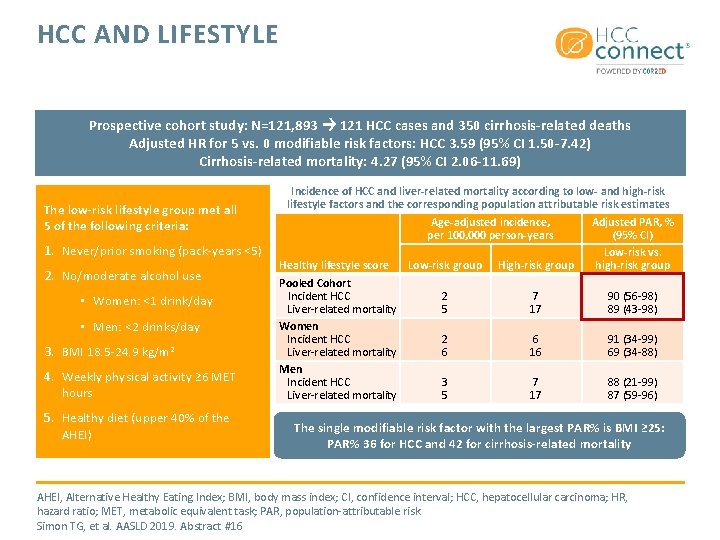
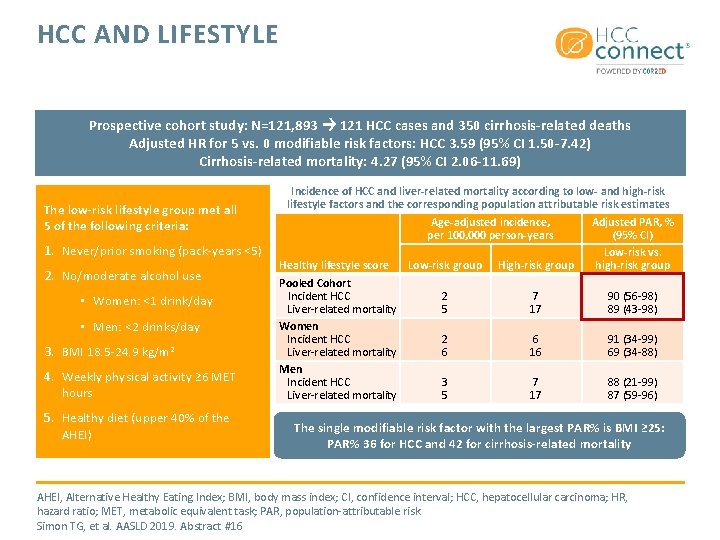
HCC AND LIFESTYLE Prospective cohort study: N=121, 893 121 HCC cases and 350 cirrhosis-related deaths Adjusted HR for 5 vs. 0 modifiable risk factors: HCC 3. 59 (95% CI 1. 50 -7. 42) Cirrhosis-related mortality: 4. 27 (95% CI 2. 06 -11. 69) Incidence of HCC and liver-related mortality according to low- and high-risk lifestyle factors and the corresponding population attributable risk estimates The low-risk lifestyle group met all Age-adjusted incidence, Adjusted PAR, % 5 of the following criteria: per 100, 000 person-years (95% CI) 1. Never/prior smoking (pack-years <5) Low-risk vs. Low-risk group High-risk group high-risk group Healthy lifestyle score 2. No/moderate alcohol use Pooled Cohort Incident HCC 2 7 90 (56 -98) • Women: <1 drink/day Liver-related mortality 5 17 89 (43 -98) Women • Men: <2 drinks/day Incident HCC 2 6 91 (34 -99) 3. BMI 18. 5 -24. 9 kg/m 2 Liver-related mortality 6 16 69 (34 -88) Men 4. Weekly physical activity ≥ 6 MET Incident HCC 3 7 88 (21 -99) hours Liver-related mortality 5 17 87 (59 -96) 5. Healthy diet (upper 40% of the AHEI) The single modifiable risk factor with the largest PAR% is BMI ≥ 25: PAR% 36 for HCC and 42 for cirrhosis-related mortality AHEI, Alternative Healthy Eating Index; BMI, body mass index; CI, confidence interval; HCC, hepatocellular carcinoma; HR, hazard ratio; MET, metabolic equivalent task; PAR, population-attributable risk Simon TG, et al. AASLD 2019. Abstract #16
DIETARY FAT INTAKE AND RISK OF HEPATOCELLULAR CARCINOMA IN TWO LARGE PROSPECTIVE COHORT STUDIES Yang W, et al. AASLD 2019, Abstract #854
DIETARY FAT AND HCC METHODS • Prospective analysis of intake of total and specific fats and major sources of dietary fats in relation to HCC risk within the Nurses’ Health Study and the Health Professionals Follow-up Study • Dietary fats were measured at baseline and approximately every 4 years • Average follow-up of 28 years HCC, hepatocellular carcinoma Yang W, et al. AASLD 2019. Abstract #854
DIETARY FAT AND HCC RESULTS AND CLINICAL INTERPRETATION • Vegetable fat intake had a significant inverse association with HCC risk – HR 0. 61, 95% CI: 0. 39 -0. 96; P=0. 02 • Replacing animal or dairy fats with an equivalent amount of vegetable fat was associated with a lower HCC risk – HR 0. 79, 95% CI: 0. 65 -0. 97 • Both monounsaturated and polyunsaturated fatty acids (PUFAs), including omega-3, were inversely associated with HCC risk – HR=0. 63, 95% CI: 0. 41 -0. 96; P=0. 14 • Polyunsaturated and/or monounsaturated fat to saturated fat ratios were all statistically inversely associated with HCC risk (all Ptrend≤ 0. 02) Clinical interpretation: • Higher intake of vegetable fats and PUFAs could be associated with lower HCC risk • Replacing animal or dairy fats with vegetable fats, or replacing saturated fats with poly- or monounsaturated fats was associated with reduced risk of HCC among US adults CI, confidence interval; HCC, hepatocellular carcinoma; HR, hazard ratio; PUFA, polyunsaturated fatty acid Yang W, et al. AASLD 2019. Abstract #854
INCREASED RISK OF HEPATOCELLULAR CARCINOMA IN DIABETICS WITH NASH: UNOS DATABASE ANALYSIS Doycheva IB, et al. AASLD 2019, Abstract #348
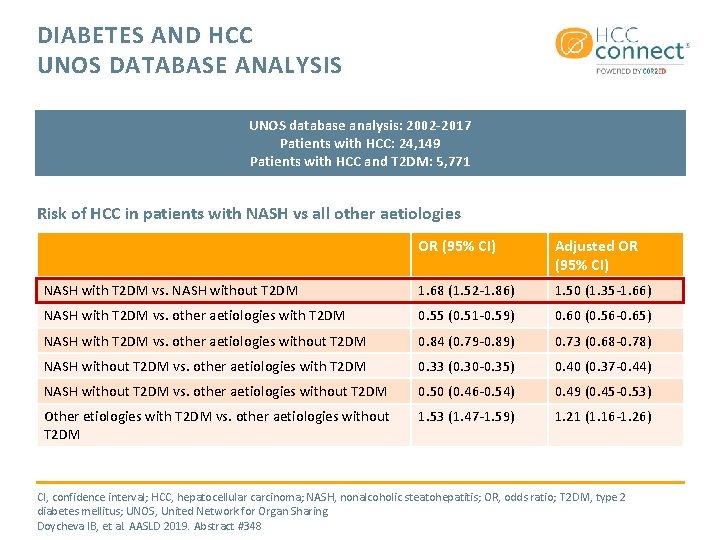
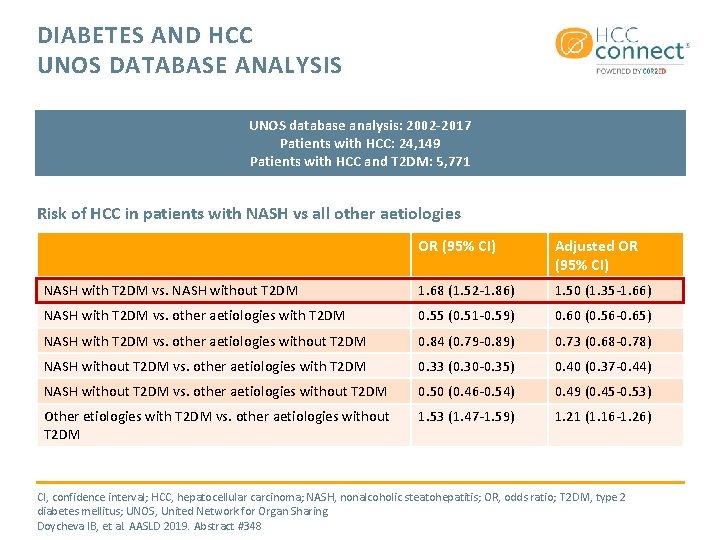
DIABETES AND HCC UNOS DATABASE ANALYSIS UNOS database analysis: 2002 -2017 Patients with HCC: 24, 149 Patients with HCC and T 2 DM: 5, 771 Risk of HCC in patients with NASH vs all other aetiologies OR (95% CI) Adjusted OR (95% CI) NASH with T 2 DM vs. NASH without T 2 DM 1. 68 (1. 52 -1. 86) 1. 50 (1. 35 -1. 66) NASH with T 2 DM vs. other aetiologies with T 2 DM 0. 55 (0. 51 -0. 59) 0. 60 (0. 56 -0. 65) NASH with T 2 DM vs. other aetiologies without T 2 DM 0. 84 (0. 79 -0. 89) 0. 73 (0. 68 -0. 78) NASH without T 2 DM vs. other aetiologies with T 2 DM 0. 33 (0. 30 -0. 35) 0. 40 (0. 37 -0. 44) NASH without T 2 DM vs. other aetiologies without T 2 DM 0. 50 (0. 46 -0. 54) 0. 49 (0. 45 -0. 53) Other etiologies with T 2 DM vs. other aetiologies without T 2 DM 1. 53 (1. 47 -1. 59) 1. 21 (1. 16 -1. 26) CI, confidence interval; HCC, hepatocellular carcinoma; NASH, nonalcoholic steatohepatitis; OR, odds ratio; T 2 DM, type 2 diabetes mellitus; UNOS, United Network for Organ Sharing Doycheva IB, et al. AASLD 2019. Abstract #348
CLINICAL PATTERNS OF HEPATOCELLULAR CARCINOMA IN NON-ALCOHOLIC FATTY LIVER DISEASE AND HEPATITIS B Tay BWR, et al. AASLD 2019, Abstract #859
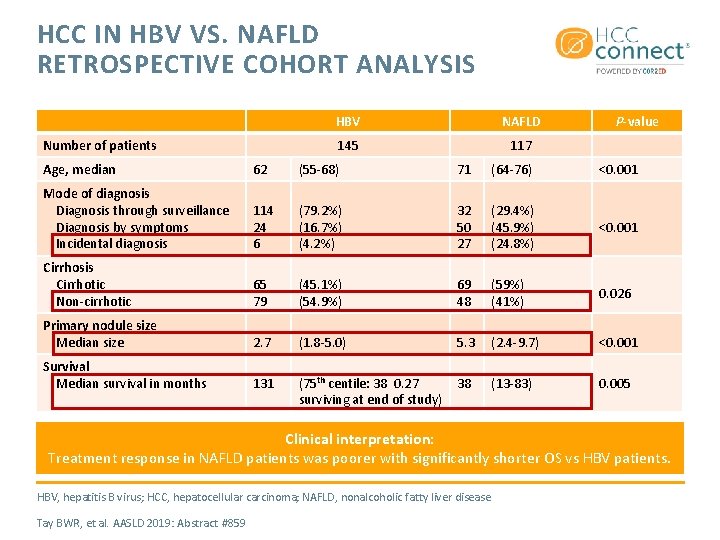
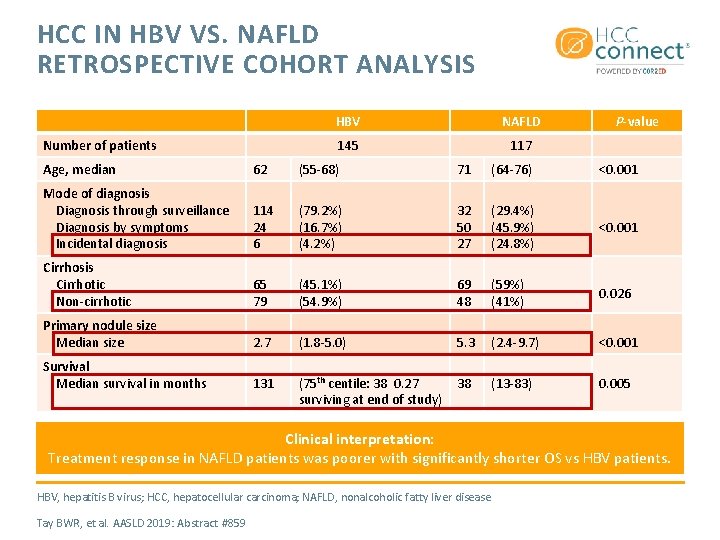
HCC IN HBV VS. NAFLD RETROSPECTIVE COHORT ANALYSIS Number of patients HBV NAFLD 145 117 P-value Age, median 62 (55 -68) 71 (64 -76) <0. 001 Mode of diagnosis Diagnosis through surveillance Diagnosis by symptoms Incidental diagnosis 114 24 6 (79. 2%) (16. 7%) (4. 2%) 32 50 27 (29. 4%) (45. 9%) (24. 8%) <0. 001 Cirrhosis Cirrhotic Non-cirrhotic 65 79 (45. 1%) (54. 9%) 69 48 (59%) (41%) 0. 026 Primary nodule size Median size 2. 7 (1. 8 -5. 0) 5. 3 (2. 4 -9. 7) <0. 001 Survival Median survival in months 131 (75 th centile: 38 0. 27 surviving at end of study) 38 (13 -83) 0. 005 Clinical interpretation: Treatment response in NAFLD patients was poorer with significantly shorter OS vs HBV patients. HBV, hepatitis B virus; HCC, hepatocellular carcinoma; NAFLD, nonalcoholic fatty liver disease Tay BWR, et al. AASLD 2019: Abstract #859
CONCLUSIONS • Many patients with cirrhosis are not getting screened for HCC • Screening for HCC in selected elderly patients should be considered • Liver cancer is influenced by many factors, including diabetes and NASH • There is a signal that lifestyle and dietary changes could impact the development of liver cancer 21
REACH HCC CONNECT VIA TWITTER, LINKEDIN, VIMEO & EMAIL OR VISIT THE GROUP’S WEBSITE http: //www. hccconnect. info Follow us on Twitter @hccconnectinfo Follow the HCC CONNECT group on Linked. In Watch us on the Vimeo Channel HCC CONNECT Email froukje. sosef@cor 2 ed. com 22 22
HCC CONNECT Bodenackerstrasse 17 4103 Bottmingen SWITZERLAND Dr. Froukje Sosef MD +31 6 2324 3636 froukje. sosef@cor 2 ed. com Dr. Antoine Lacombe Pharm D, MBA +41 79 529 42 79 antoine. lacombe@cor 2 ed. com Heading to the heart of Independent Medical Education Since 2012
 Hepatocellular jaundice
Hepatocellular jaundice Wikipedia commons
Wikipedia commons Credit risk market risk operational risk
Credit risk market risk operational risk Brfss texas
Brfss texas Cervix carcinoma
Cervix carcinoma Papillary renal cell carcinoma
Papillary renal cell carcinoma Carcinoma in situ
Carcinoma in situ Carcinoma in situ
Carcinoma in situ Invasive ductal carcinoma with medullary features
Invasive ductal carcinoma with medullary features Breast ca tnm staging
Breast ca tnm staging Carcinoma de mama
Carcinoma de mama Carcinoma in situ
Carcinoma in situ Breast cancer biopsy
Breast cancer biopsy Kode icd 10 oat
Kode icd 10 oat Squamous cell carcinoma louisiana
Squamous cell carcinoma louisiana Brown tumor
Brown tumor Breast papillary carcinoma
Breast papillary carcinoma Hormones
Hormones Carcinoma micropapilar invasivo de mama
Carcinoma micropapilar invasivo de mama Carcinoma
Carcinoma Carcinoma of stomach
Carcinoma of stomach Hospital max peralta extensiones
Hospital max peralta extensiones Haggit evrelemesi
Haggit evrelemesi Basal cell carcinoma
Basal cell carcinoma