Shock Emergency Approach First Part Assoc Prof Dr




- Slides: 42
Shock - Emergency Approach First Part Assoc. Prof. Dr. Diana Cimpoesu
Shock - definition, epidemiology �Cardiovascular insufficiency that creates an imbalance between tissue oxygen supply and oxygen demand �USA- over 1 milion cases present to the ED/year �Precocious intervention at the non-traumatic patient – “the golden hour”
Shock – classification: 4 categories by etiology �Hypovolemic- due to inadequate circulating volume �Cardiogenic- due to inadequate cardiac pump function �Distributive- maldistribution of blood flowseptic, anaphylactic, neurogenic �Obstructive- extra-cardiac obstruction to blood flow : pulmonary embolism, cardiac tamponade, tension pneumothorax

Shockphysiopathology �Sa. O 2=100%- normal 25% of the transported O 2 linked to Hb is consumed by the tissues – the venous blood will have a saturation of 75% �O 2 supply is insufficient to meet demands- the first compensatory mechanism is the increase of CO (cardiac output) �If the increase of CO is insufficient – the amount of O 2 extracted from Hb by tissues increses and Sm. VO 2 decreases (O 2 saturation of the venous blood)
Shock-physiopathology q Demand>offer – anaerobic metabolism occurs- lactic acid q Lactic Acidosis : due to -the inadequate O 2 delivery ( like in the cardiogenic shock) -Very high demand (consumption of O 2 increased) -Inadequate use of oxygen at the level of tissues (septic shock or post-resuscitation syndrome ) q Lactic acid - marker of the disturbance demand/offer - used in the patient receiving department, diagnosis, treatment, prognosis q MBP=CO x peripheral vascular resistance, q CO decreases- the peripheral vascular resistance increases MBP is not an exact marker of the tissue hypo-perfusion
Shock- physiopathology Compensatory mechanisms: stimulation of carotid baroreceivers – sympathetic NS: �Arteriolar vessel constriction – circulation redistribution �HR increase and miocardial contractilities – increased DC �Constriction on the vessels of potentia �Release of vaso-active hormones (A, NA, D, C)vasoconstriction �ADH release, activation of the renin-angiotensionretension system of Na and water-maintenance of the intravascular volume.
Hemorrhagic shock physiopathology �Compensatory mechanisms: sympathetic hyperactivity to maintain the effective circular volume �Vasoconstriction, circulation centralization, diuresis decrease �Straling forces modification by precapillar sphincter contraction: interstitial hydrostatic pressure increases, cell dehydration – “transcapillar refilling” �O 2 tissular extraction increases (right deviation of Hb. O dissociation curve)

Hemorrhagic shock: decompensation mechanisms �Loss of precapillar sphincter vasoconstriction– vasodilatation, hypotension, myocardium and NCS ischemia, transudation of interstitial liquid �Increase of capillary permeability �Capillary blockage by leukokeratoses micro aggregates �Erythrocytic deformability decrease �Endothelian edema
Shock- physiopathology- cellular effects of O 2 decrease �ATP depletion- membranous pump malfunction. Na inflow and K release �Cellular edema, cells no longer respond to stress hormones (insulin, cortisol, glucagon, catecholamines) �Intracellular destructions- cellular death �Hyper K, hypo Na, metabolic acidosis, hyperglicemia, lactic acidosis
Shock- symptoms �Symptoms suggesting the volume loss: bleeding, vomiting, diarrhea, polyuria, fever �Symptoms suggesting: acute coronary sdr. , congestive acute heart failure, beta-blockers �Anaphylactic context �Neurological disorders: vertigo, lipothymia, alteration of the mental status-coma �Trauma

Shock- physical examination �CV: distension of the throat veins, tachycardia, arrhythmia, decrease of the coronary perfusion pressure, decrease of the ventricle compliance, increase of the diastolic pressure in LV, pulmonary edema �Respiratory: tachypnea, increase of RR, increase of the dead area, bronchospasm, hypocapnia, respiratory failure, acute respiratory distress sdr.
Shock- physical examination �Visceras: ileus, gastrointestinal bleeding, pancreatitis, alithiasic cholecystitis, mesenteric ischemia �Renal: decrease of the glomerulary filtering rate, redistribution of the renal flux, oliguria �Metabolism: respiratory alkalosis, then metabolic acidosis, hypo/hyperglycemia, hyper. K.

Shock –clinical framework �Temperature �Hyperthermia or hypothermia (endogenous=hypo metabolic shock or exogenous). �Cardiac frequency HR �Usually increased; there can also be paroxistic bradycardia in hypovolemic shock, hypoglycemia, beta -blockers, pre-existent cardiac affections. �SBP �In the precocious phase it can be increased because it is a compensatory mechanism and increases DC and then, it decreases. �DBP �Increases at the debut by arterial vessel constriction and then it decreases.
Shock –clinical outview �Pulse pressure �SBP-DBP, depends on the aorta rigidity and on the diastolic volume: it increases precociously in shock and then decreases before SBP. �Paradoxical pulse �The modification of SBP with breath. The increase and decrease of intratoracic pressure affects the cardiac output. �It is met in asthma, cardiac tamponade and decompensate cardiac insufficiency. �MBP = DBP + (MBP – DBP)/3 �Depends on CO şi RP, assures adequate tissular perfusion, decreases in shock.
Shock – Clinical Framework �Shock index = HR/SBP = 0, 5 -0, 7 (n) �Depends on the effort of the LV in acute circulatory insufficiency �CNS: agitation, delirium, confusion, torpor, coma – decrease of pressure of cerebral perfusion �Skin: cold, wet, sweated, cyanosis �CV, respiratory, visceral organs, renal, metabolism – see above
Shock – paraclinic exams �Base evaluation: HLG, electrolytes, glycemia, urea, creatinine, TQ, IQ, a. PTT, urine summary, ecg, thoracic Rx. �Secondary evaluation: arterial blood gases, lactic acid, PDF, hepatic function �Non invasive monitoring: CO 2 -end tidal, DC calculated, echocardiogram �Invasive monitoring: capillary filling pressure, PVC, DC, Sm. VO 2, vascular resistance, DO 2, VO 2 �For etiology and complications: cultures, cranial CT, pelvis, abdominal, lumbar puncter, cortizol level, pelvian and abdominal echography
Shock - treatment �A – IOT, mechanic ventilation, tracheal aspiration �B – decrease of respiratory labor, sedation, mechanic ventilation, decrease of oxygen demand, Sa. O 2 > 93 %, Pa. CO 2 < 35 -40 mm. Hg, p. H > 7, 3 �C – fluid reanimation (crystalline capsule, colloid), peripheral and central venal access, vasopressin for MBP > 60 mm. Hg and SBP > 90 mm. Hg �Decrease O 2 demand – resolving of hyperandrenergic status (analgesic, relaxation, warmth, tranquilizers), Hb > 10 g%
Shock-vasoactive agents �Dopamina: 0 -25 mcg/kg/min, alfa, beta, D �Noradrenaline: 0, 01 -0, 5 mcg/kgc/min, alfa 1, beta 1 �Phenyleffrine: 0, 15 -0, 75 mcg/kgc/min (alfa) �Adrenaline: 0, 01 -0, 75 mcg/kcg/min �Dobutamine: 2 -20 mcg/kgc/min, beta 1, 2, alfa 1 �Isoproterenol: 0, 01 -0, 02 mcg/kgc/min, beta 1, 2
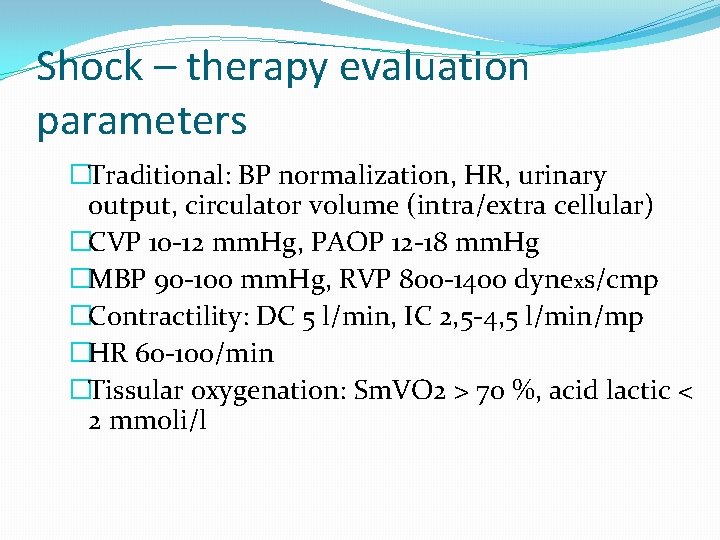
Shock – therapy evaluation parameters �Traditional: BP normalization, HR, urinary output, circulator volume (intra/extra cellular) �CVP 10 -12 mm. Hg, PAOP 12 -18 mm. Hg �MBP 90 -100 mm. Hg, RVP 800 -1400 dynexs/cmp �Contractility: DC 5 l/min, IC 2, 5 -4, 5 l/min/mp �HR 60 -100/min �Tissular oxygenation: Sm. VO 2 > 70 %, acid lactic < 2 mmoli/l
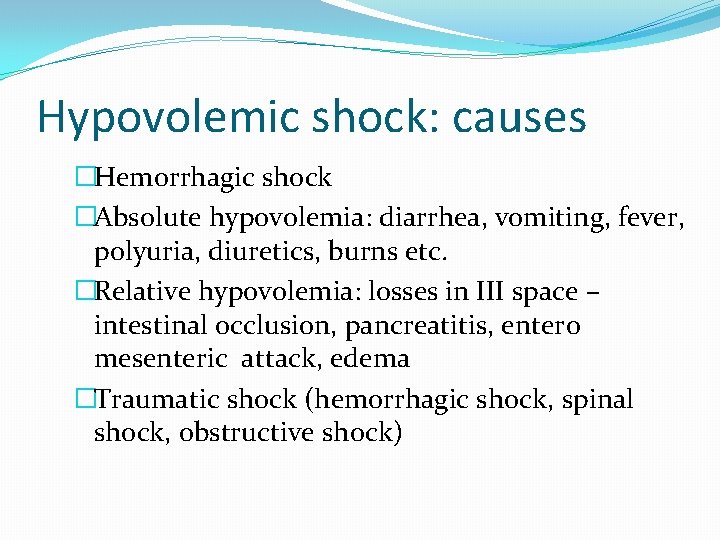
Hypovolemic shock: causes �Hemorrhagic shock �Absolute hypovolemia: diarrhea, vomiting, fever, polyuria, diuretics, burns etc. �Relative hypovolemia: losses in III space – intestinal occlusion, pancreatitis, entero mesenteric attack, edema �Traumatic shock (hemorrhagic shock, spinal shock, obstructive shock)
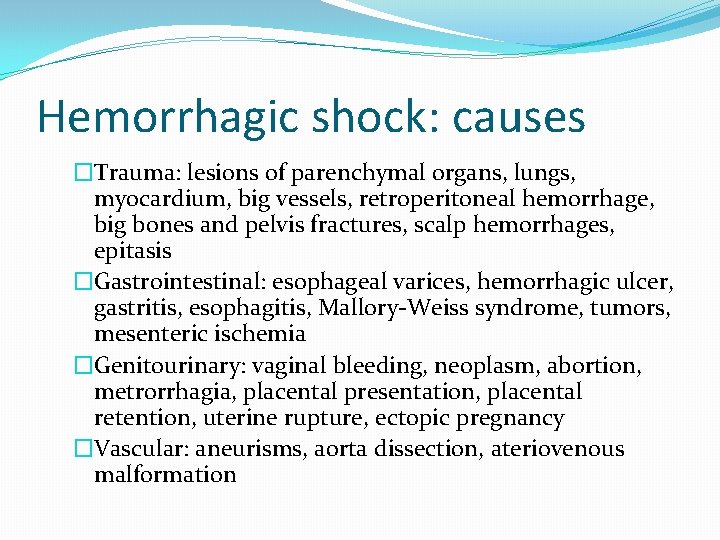
Hemorrhagic shock: causes �Trauma: lesions of parenchymal organs, lungs, myocardium, big vessels, retroperitoneal hemorrhage, big bones and pelvis fractures, scalp hemorrhages, epitasis �Gastrointestinal: esophageal varices, hemorrhagic ulcer, gastritis, esophagitis, Mallory-Weiss syndrome, tumors, mesenteric ischemia �Genitourinary: vaginal bleeding, neoplasm, abortion, metrorrhagia, placental presentation, placental retention, uterine rupture, ectopic pregnancy �Vascular: aneurisms, aorta dissection, ateriovenous malformation
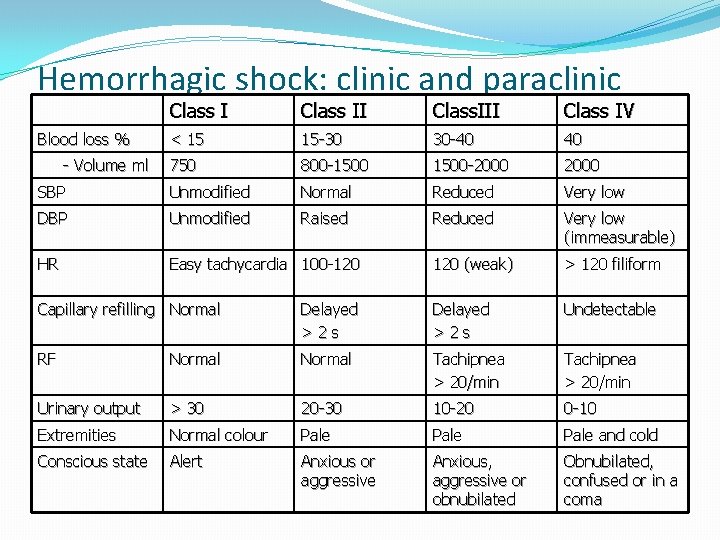
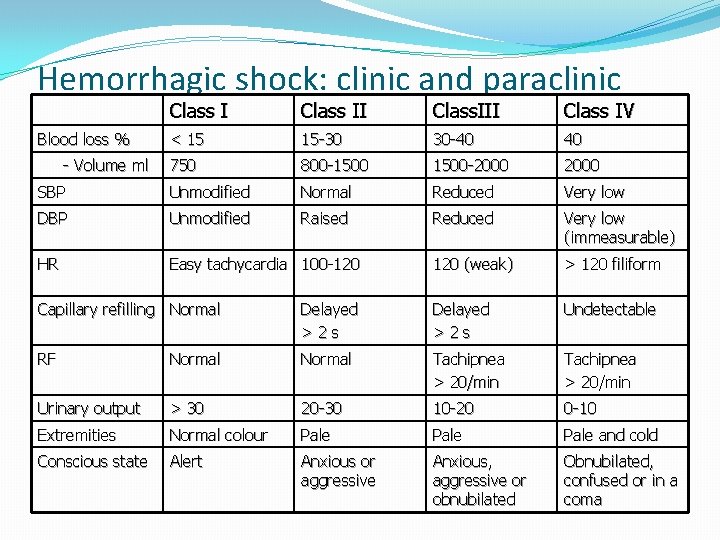
Hemorrhagic shock: clinic and paraclinic Class II Class. III Class IV < 15 15 -30 30 -40 40 750 800 -1500 -2000 SBP Unmodified Normal Reduced Very low DBP Unmodified Raised Reduced Very low (immeasurable) HR Easy tachycardia 100 -120 (weak) > 120 filiform Blood loss % - Volume ml Capillary refilling Normal Delayed >2 s Undetectable RF Normal Tachipnea > 20/min Urinary output > 30 20 -30 10 -20 0 -10 Extremities Normal colour Pale and cold Conscious state Alert Anxious or aggressive Anxious, aggressive or obnubilated Obnubilated, confused or in a coma
Hemorrhagic shock: Therapeutic objectives �Adequate lung oxygenation �Hemorrhage control �Loss replacements �Monitoring therapy effects �Myocardic contractibility support �Acido-basic and electrolytic reequilibration �Sustaining renal function
Hemorrhagic shock: treatment �ABC �External hemorrhages control: raising the extremities, compressive bandage, surgery �Loss replacement: peripheral and central venous acces, intravascular volume replacement, oxygen transport replacement, coagulation anomalies correction
Crystalline solutions �Isotones: NS, Ringer lactate - replace the interstitial deficit also rapid intra and extra vascular equilibration; it is administrated 3: 1 compared to lost volume of blood �Hypertonic fluids: Na. Cl hypertonic solutionperfusion reduced volume for a satisfactory volemic recovery, positive intropic effect, peripheral vasodilatator; hypernatremia danger, extreme cerebral dehydration (Na >170 m. Eq/l) �Economic reason - accessibility
Colloidal solutions �Important intravascular remanence time, small volumes use for adequate volemic resuscitation, maintenance of intravascular colloidal osmotic, useful in cardiac and renal insufficiency �Albumen, dextran 40 -70, HAES, Haemacel, plasma �High price, anaphylactic reactions, antiplachetary effect and of faking direct compatibility result, histocitary system blockage, infection transmission
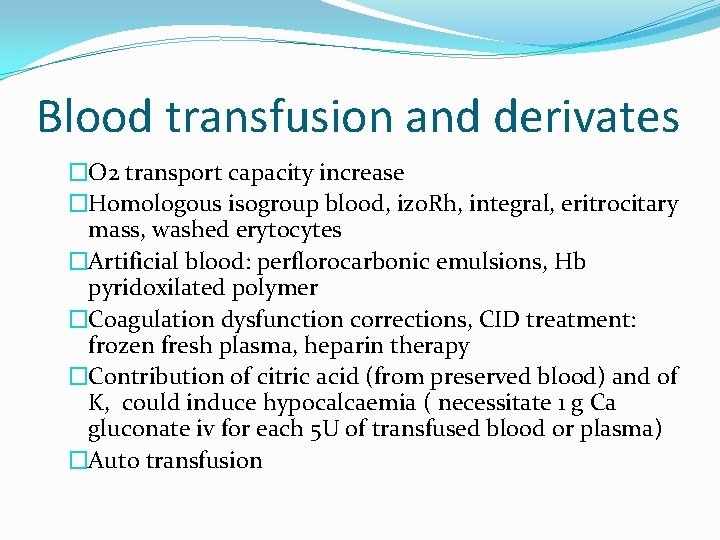
Blood transfusion and derivates �O 2 transport capacity increase �Homologous isogroup blood, izo. Rh, integral, eritrocitary mass, washed erytocytes �Artificial blood: perflorocarbonic emulsions, Hb pyridoxilated polymer �Coagulation dysfunction corrections, CID treatment: frozen fresh plasma, heparin therapy �Contribution of citric acid (from preserved blood) and of K, could induce hypocalcaemia ( necessitate 1 g Ca gluconate iv for each 5 U of transfused blood or plasma) �Auto transfusion
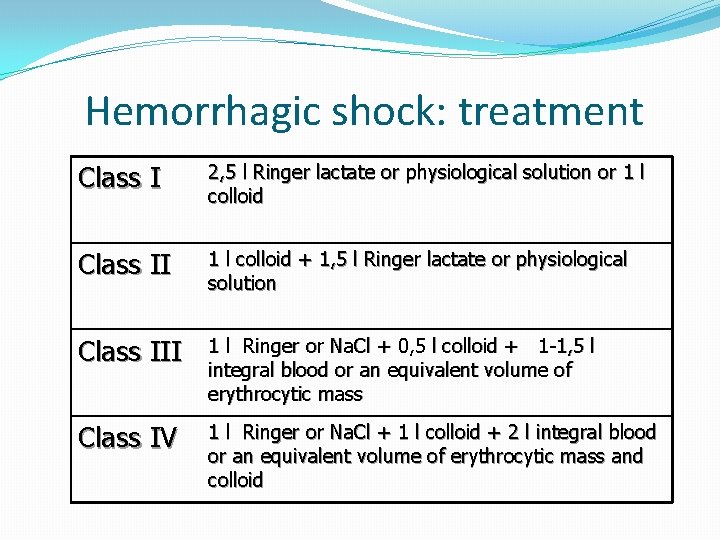
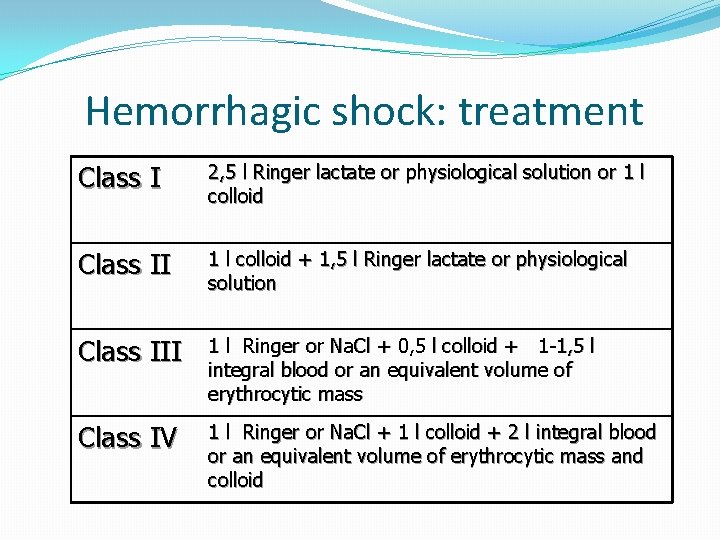
Hemorrhagic shock: treatment Class I 2, 5 l Ringer lactate or physiological solution or 1 l colloid Class II 1 l colloid + 1, 5 l Ringer lactate or physiological solution Class III 1 l Ringer or Na. Cl + 0, 5 l colloid + 1 -1, 5 l integral blood or an equivalent volume of erythrocytic mass Class IV 1 l Ringer or Na. Cl + 1 l colloid + 2 l integral blood or an equivalent volume of erythrocytic mass and colloid
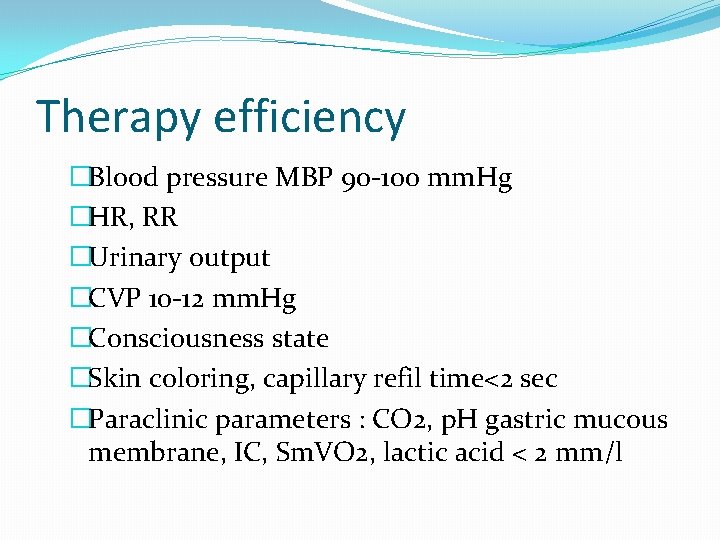
Therapy efficiency �Blood pressure MBP 90 -100 mm. Hg �HR, RR �Urinary output �CVP 10 -12 mm. Hg �Consciousness state �Skin coloring, capillary refil time<2 sec �Paraclinic parameters : CO 2, p. H gastric mucous membrane, IC, Sm. VO 2, lactic acid < 2 mm/l
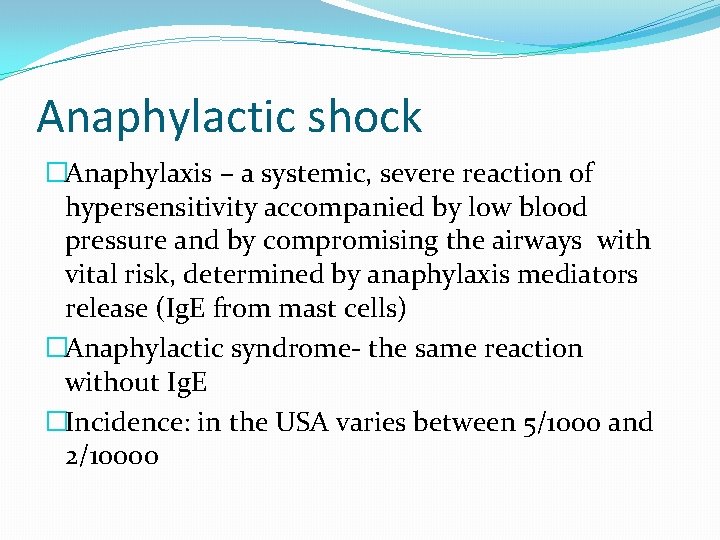
Anaphylactic shock �Anaphylaxis – a systemic, severe reaction of hypersensitivity accompanied by low blood pressure and by compromising the airways with vital risk, determined by anaphylaxis mediators release (Ig. E from mast cells) �Anaphylactic syndrome- the same reaction without Ig. E �Incidence: in the USA varies between 5/1000 and 2/10000
Anaphylactic shock-physiopathology �Hypersensitivity reaction type I-Ig. E �Mast cells digranulation �Mediators issue �Complement activation �Metabolism modulation arachidonic acid �But also hypersensitivity reaction of type II and III
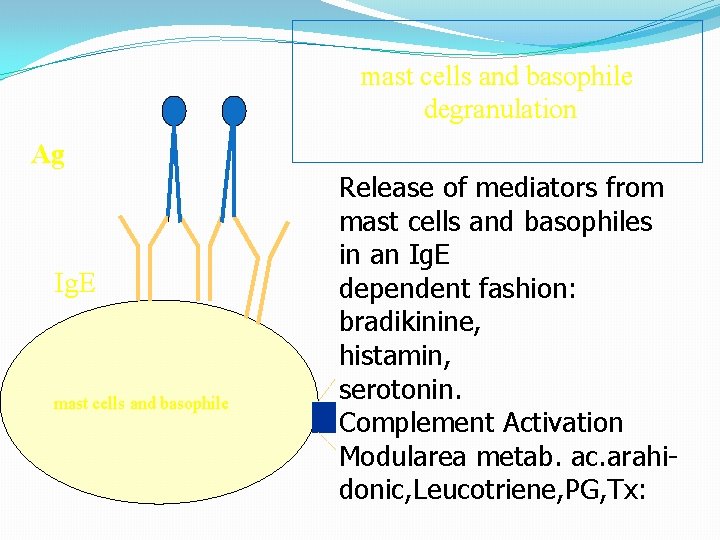
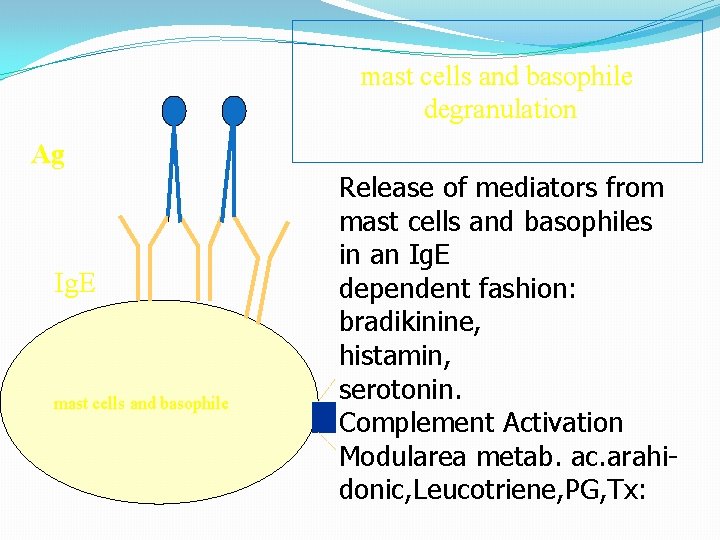
mast cells and basophile degranulation Ag Ig. E mast cells and basophile Release of mediators from mast cells and basophiles in an Ig. E dependent fashion: bradikinine, histamin, serotonin. Complement Activation Modularea metab. ac. arahidonic, Leucotriene, PG, Tx:
Anaphylactic shock: causes � Medicines � Penicillin and other � aspirin � trimetroprim � AINS � Foods and additives � Sea fruits, fish � Soy, nuts � Flour, milk, eggs � Monosodium glutamate, tartrasine � Nitrates and nitrites � Others � Hymenoptera stings � Insects � Contrast substances from radiology
Anaphylactic shock-clinic �Urticaria �Angioedema �Non systematic abdominal pains �Nausea, vomiting, diarrhea �Bronchospasm �Rhinorrhea �Conjunctivitis �Lipothymia or palpitations �Anaphylaxis= any combinations of these signs and low blood pressure or compromising of air way
Clinic signs evolution �Pruritus �Erythema �Urticaria �Dyspnea, anxiety, lipothymia, syncope �Apparition within 60 minutes from the exposuregravity sign – death risk �Symptoms recurrence - biphasic phenomenon - 20% of patients
Positive and differential diagnosis Positive = historic and physical exam Differential: �Vague vessel reactions �Myocardium ischemia �Status astmaticus �Convulsions �Epiglottises �Congenital angioedema �Obstruction of air ways by foreign bodies �Laboratory: histamine, high tryptase
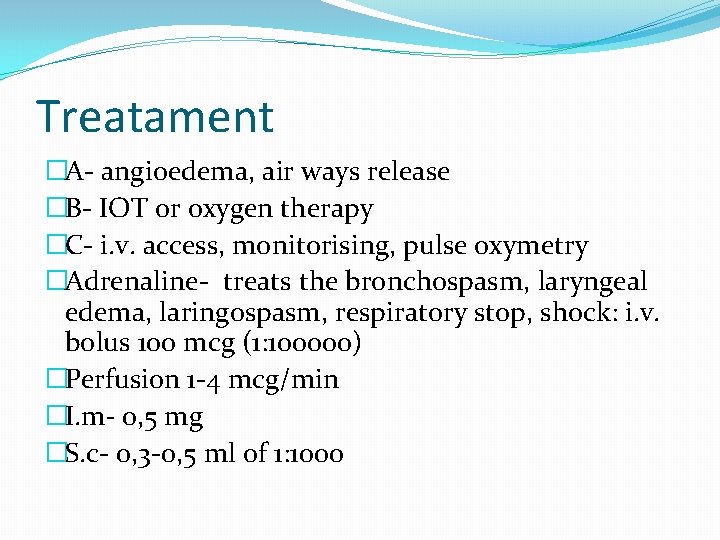
Treatament �A- angioedema, air ways release �B- IOT or oxygen therapy �C- i. v. access, monitorising, pulse oxymetry �Adrenaline- treats the bronchospasm, laryngeal edema, laringospasm, respiratory stop, shock: i. v. bolus 100 mcg (1: 100000) �Perfusion 1 -4 mcg/min �I. m- 0, 5 mg �S. c- 0, 3 -0, 5 ml of 1: 1000
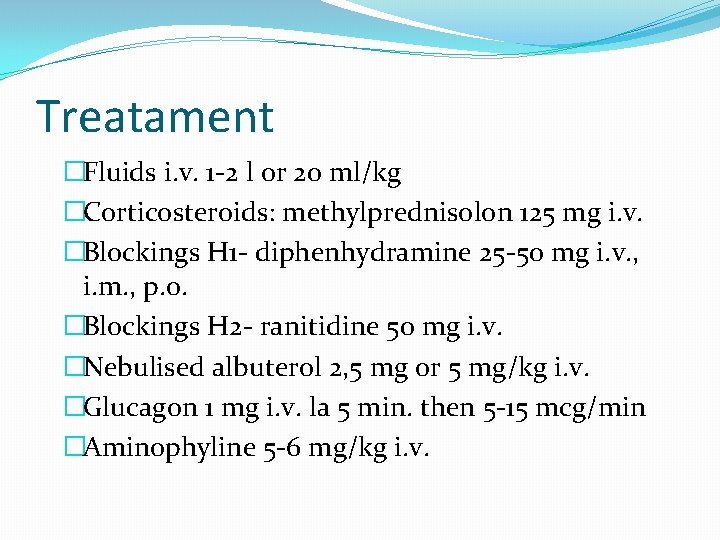
Treatament �Fluids i. v. 1 -2 l or 20 ml/kg �Corticosteroids: methylprednisolon 125 mg i. v. �Blockings H 1 - diphenhydramine 25 -50 mg i. v. , i. m. , p. o. �Blockings H 2 - ranitidine 50 mg i. v. �Nebulised albuterol 2, 5 mg or 5 mg/kg i. v. �Glucagon 1 mg i. v. la 5 min. then 5 -15 mcg/min �Aminophyline 5 -6 mg/kg i. v.