Seizure and epilepsy Dr alazar w Outline Definition
![Adults: - Idiopathic[55. 25%] - Vascular[15. 2%]. - Trauma(9. 9%). - CNS tumors[10. 5%] Adults: - Idiopathic[55. 25%] - Vascular[15. 2%]. - Trauma(9. 9%). - CNS tumors[10. 5%]](https://slidetodoc.com/presentation_image_h/1e5b84d97179ef1a958b01565077c377/image-22.jpg)
- Slides: 39
Seizure and epilepsy Dr alazar w.
Outline • Definition • Epidemiology • Classification • Causes • Mechanism of seizure • Evaluation of first seizure • Management • Status epilepticus
DEFINITION • Seizure is paroxysmal event due to abnormal excessive or synchronous neuronal activity in the brain. • Patients manifest with various features ranging from subtle/unrecognizable sxs to dramatic convulsive activity. • Epilepsy is 2 or more unprovoked seizures due to chronic underlying process. • Epilepsy syndrome disorders in which epilepsy is a predominant feature with common underlying mechanism.
epidemology • Overall prevalence =5 -10 person /1000 • Incidence=0. 3 -0. 5% • In USA 120 000 new cases per year • 5 -10% of pop. • once in life • Sex: Male: Female=1. 5: 1 • Age: Bimodal distribution-Childhood and late adulthood. Childhood absence epilepsy remits as Pt gets older
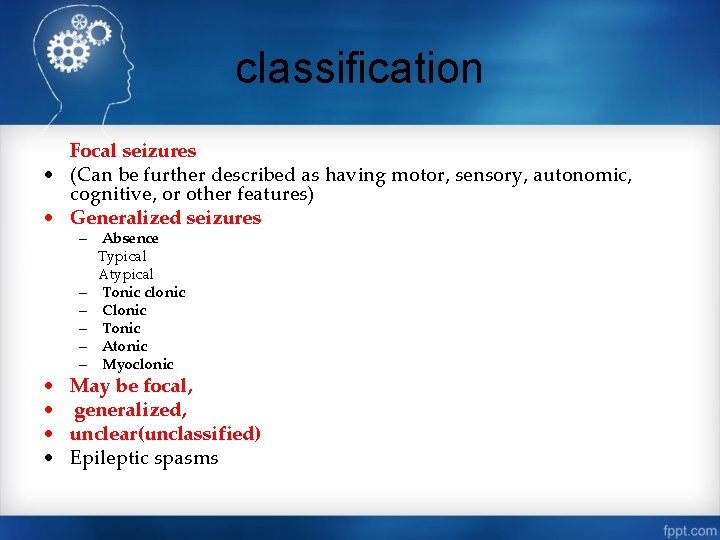
classification Focal seizures • (Can be further described as having motor, sensory, autonomic, cognitive, or other features) • Generalized seizures • • – Absence Typical Atypical – Tonic clonic – Clonic – Tonic – Atonic – Myoclonic May be focal, generalized, unclear(unclassified) Epileptic spasms
A. Focal Seizures • Accounts 70% of seizure in adults(40% in children) • Focal seizures arise from a neuronal network either discretely localized within one cerebral hemisphere • a. Focal Seizures Without Dyscognitive Features • motor, sensory, autonomic, or psychic symptoms without impairment of cognition. • Motor-clonic(repetitive, flexion/extension movements) or tonic posturing
• Jacksonian march represents the spread of seizure activity over a progressively larger region of motor cortex • Todd's paralysis localized paresis for minutes to many hours in the involved region following the seizure. • Epilepsia partialis continua continued seizure activity for hours or days.
Other manifestations • • © © sensory Somatic sensation-eg. parasthesias Visual changes-eg. flashing light, formed hallucinations Equilibrium changes-eg. Vertigo Olfaction-strong smells(burning rubber/kerosene) hearing Autonomic-eg. Flushing, piloerection, sweating Psychic-arise from the temporal or frontal cortex unusual, intense odors (e. g. , burning rubber or kerosene) crude or highly complex sounds Epigastric sensation that rises from the stomach or chest to the head Odd , internal feelings - fear, a sense of impending change, or illusions(objects are growing smaller (micropsia) or larger (macropsia)). These are referred to as auras.
b. Focal Seizures with Dyscognitive Features • There is associated brief impairment of consciousness. • impaired recollection or awareness of the ictal phase. • Preceding aura (i. e. , a focal seizure without cognitive disturbance) is present. • Automatisms which are stereotyped involuntary , repetitive automatic behaviors(chewing, lip smacking, swallowing, or "picking" movements of the hands, or more elaborate behaviors such as a display of emotion or running. ) • typically last less than three minutes • Postictal confusion, aphasia or anterograde amnesia
B. Generalized Seizures • Generalized seizures are thought to arise at some point in the brain but immediately and rapidly involve neuronal networks in both cerebral hemispheres. • Absence Seizures § seizure type in children (4 -8 yr) • Accounts for 15 -20% sz in children • First clue- day dreaming or decreased school performance • frequently occur in clusters and may take place dozens or hundreds of times a day. • Typical : sudden, brief lapses of consciousness without loss of postural control and no postictal confusion • subtle motor manifestation: • Bilateral blinking of eye lids, chewing movements or clonic movement of the hands • typically last between 5 and 10 seconds EEG-generalized, symmetric, 3 -Hz spike-and-wave discharge
• Atypical : longer duration of LOC(>10 sec), slower • • onset, more prominent motor sxs and remission usually associated with diffuse or multifocal structural abnormalities of the brain may be accompany other signs of neurologic dysfunction such as mental retardation. less responsive to anticonvulsants EEG-generalized, slow spike-and-wave pattern with a frequency of ≤ 2. 5 per second
Grand mal (generalized tonic–clonic seizure) § Main seizure type-10% of all epilepsy § Common seizure type seen with metabolic derangements § No aura but vague premonitory symptoms -hours before seizure activity § usually symmetric, but can be asynchronous towards end
§ a- Ictal phase 1. -Tonic phase -tonic contraction of muscles throughout the body • Strained cry “ictal cry”-tonic contraction of muscles of expiration and the larynx at the onset • Impaired respiration with pooling of secretions and Cyanosis • Increase in sympathetic tone: ↑HR, BP, pupillary size • Duration: 10 -20 sec: 2 -Clonic phase: beginning of muscle relaxation which increases progressively • Takes 40 -50 sec
b-postictal phase • unresponsiveness, muscular flaccidity, and excessive salivation • Bowel/bladder incontinence • Postictal confusion or LOC • Muscle pain , headache • EEG: • Tonic-high amplitude poly spike • Clonic-Spike-and-wave pattern • Post ictal-Diffuse slowing gradually
Myoclonic • sudden and brief muscle contraction that may involve one part of the body or the entire body • physiologic form- sudden jerking movement observed while falling asleep. • Pathologic form-associated with metabolic disorders, degenerative CNS diseases, or anoxic brain injury • Focal, multifocal, generalized • EEG may show bilaterally synchronous spike-and-wave discharges
Atonic Seizures • characterized by sudden loss of postural muscle tone lasting 1– 2 seconds. § Brief loss of consciousness § No postictal confusion § Brief vs Longer duration sz § Cause: diffuse encephalopathy § EEG-brief, generalized spike-and-wave discharges then diffuse slow waves that correlate with the loss of muscle tone
C. Unclassifiable seizures • Not having features of focal or generalized seizures • Epileptic spasms: briefly sustained flexion or extension of predominantly muscles. • EEG shows hypsarrhythmias, diffuse, giant slow waves with a chaotic background of irregular, multifocal spikes and sharp waves
mechanism and pathogenesis • Seizures are a result of a shift in the normal balance of excitation and inhibition within the CNS • Why and how do a variety of factors cause seizures or epilepsy? • The normal brain is capable of having a seizure under the appropriate circumstances, and there are differences between individuals in the susceptibility or threshold for seizures
• There a variety of conditions that have an extremely high likelihood of resulting in a chronic seizure disorder • Epileptogenesis transformation of a normal neuronal network into one that is chronically hyperexcitable. • epileptogenic factors -factors that result in a lowered seizure threshold
• Seizures are episodic and many patients are completely normal for months or even years between seizures • Precipitating factors: psychological or physical stress, sleep deprivation, hormonal changes associated with the menstrual cycle, systemic diseases, drug withdrawal, metabolic abnormalities, alcohol or illicit drug.
CAUSES ACCORDING TO AGE. • Age determines the incidence & likely etiology of seizures. childhood: - Idiopathic[67. 6%] Congenital[20. 0%] trauma[4. 7%] infection[4. 0%] metabolic, vascular, neoplastic, etc.
![Adults Idiopathic55 25 Vascular15 2 Trauma9 9 CNS tumors10 5 Adults: - Idiopathic[55. 25%] - Vascular[15. 2%]. - Trauma(9. 9%). - CNS tumors[10. 5%]](https://slidetodoc.com/presentation_image_h/1e5b84d97179ef1a958b01565077c377/image-22.jpg)
Adults: - Idiopathic[55. 25%] - Vascular[15. 2%]. - Trauma(9. 9%). - CNS tumors[10. 5%] - Degenerative diseases. - Alcohol withdrawal. - Infections, degenerative, etc
Broad age range: - -Electrolyte imbalance. - -Hypo- / hyperglycemia. - -Hepatic / renal failure. - -Endocrine disorders. - -Hematological disorders. - -Vasculitidis.
Approach to a patient with seizure -Always start with ABC -Determine the presence of epilepsy -Classify seizure and type of epilepsy -Identify the cause - General management • First seizure: - Seizure or another paroxysmal event? • Known Hx of seizure/epilepsy: - identify underlying & precipitating causes. - determine adequacy of current Rx • Characterize Seizure: - Ask pt & witnesses on Sx before, during, & after the episode. -Auras -Neurological status between attacks -Circumstance, evolution, rate of occurrence -Change in characteristics of seizure
investigation 1. Blood studies: § CBC, ESR § Electrolytes § Chemistry: Glucose, LFT, RFT § Serum or urine drug level/ Toxicology screen § blood culture 2. CSF: suspicion of meningitis/encephalitis, In HIV infected 3. ECG/ECHO 4. Brain imaging- To determine underlying structural abnormality • Brain CT, MRI(superior to CT) • PET, SPECT: evaluation of medically refractory epilepsy
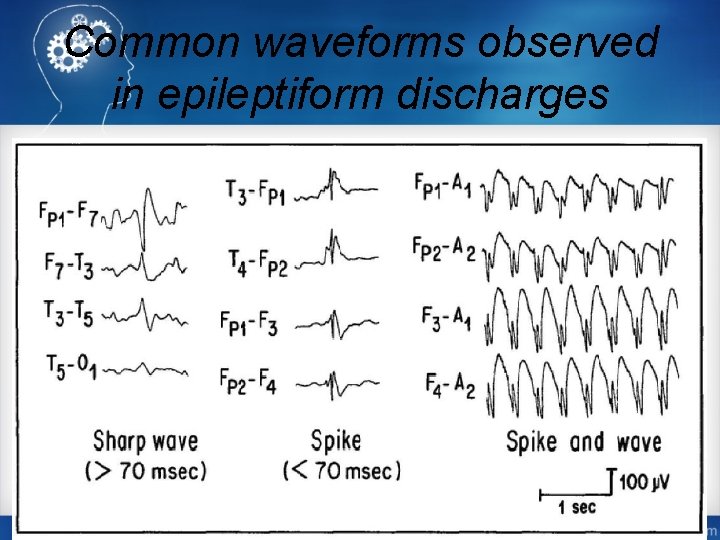
§ 5. ELECTROENCEPHALOGRM(EEG) § Essential for diagnosis, classification, Treatment decision, prognosis § measures electrical activity of the brain by recording from electrodes placed on the scalp § It should be performed after a first fit. § during a seizure the EEG is almost invariable abnormal, because spikes reach the brain surface § Electrographic Sz activity + clinically evident event ═ Dx established
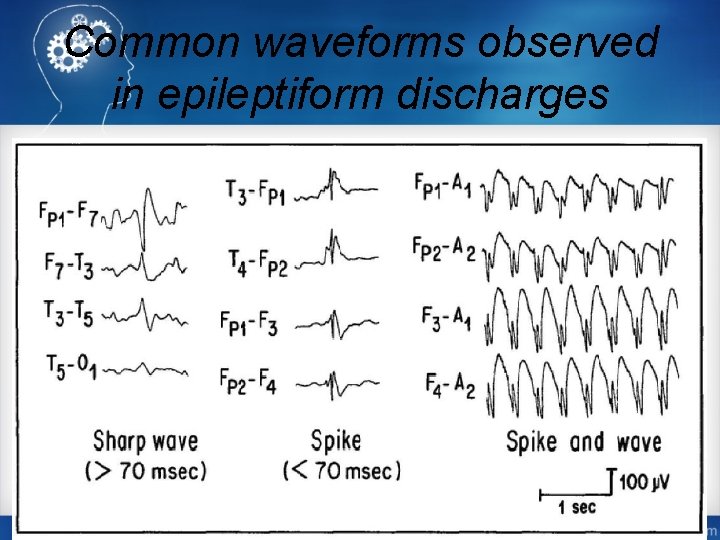
Common waveforms observed in epileptiform discharges
Differential diagnosis • Syncope • Psychological disorders • Metabolic disturbance • Psychoactive drugs (e. g. , hallucinogens) • Migraine • Transient ischemic attack (TIA) • Sleep disorders • Movement disorders
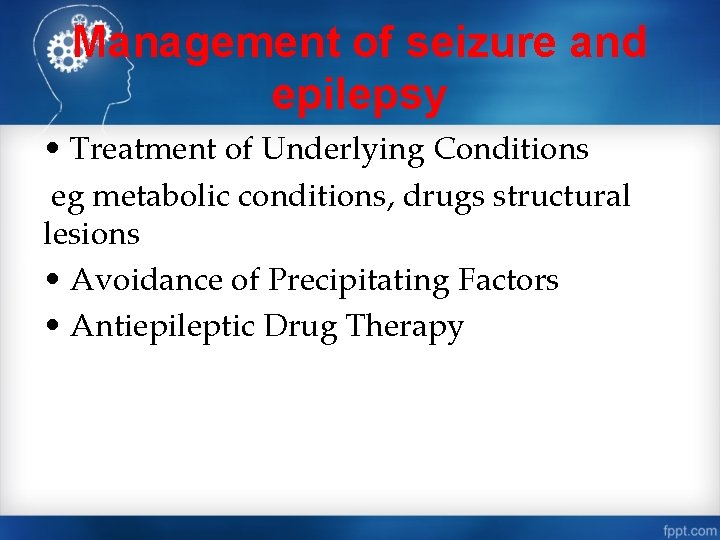
Management of seizure and epilepsy • Treatment of Underlying Conditions eg metabolic conditions, drugs structural lesions • Avoidance of Precipitating Factors • Antiepileptic Drug Therapy
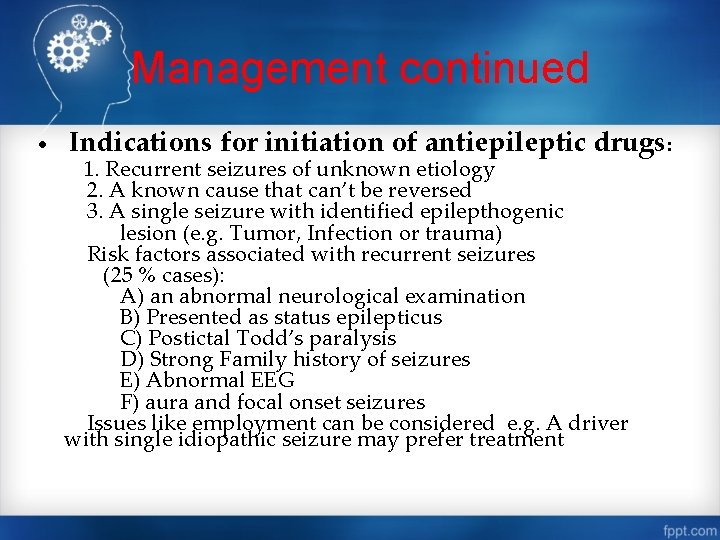
Management continued • Indications for initiation of antiepileptic drugs: 1. Recurrent seizures of unknown etiology 2. A known cause that can’t be reversed 3. A single seizure with identified epilepthogenic lesion (e. g. Tumor, Infection or trauma) Risk factors associated with recurrent seizures (25 % cases): A) an abnormal neurological examination B) Presented as status epilepticus C) Postictal Todd’s paralysis D) Strong Family history of seizures E) Abnormal EEG F) aura and focal onset seizures Issues like employment can be considered e. g. A driver with single idiopathic seizure may prefer treatment
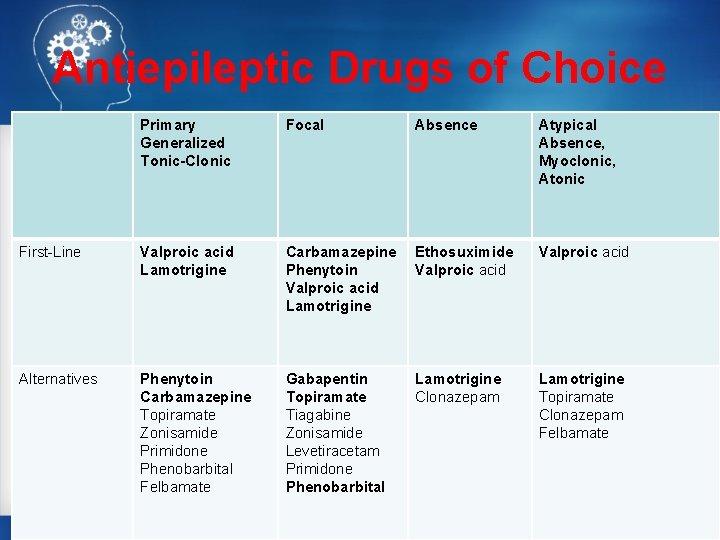
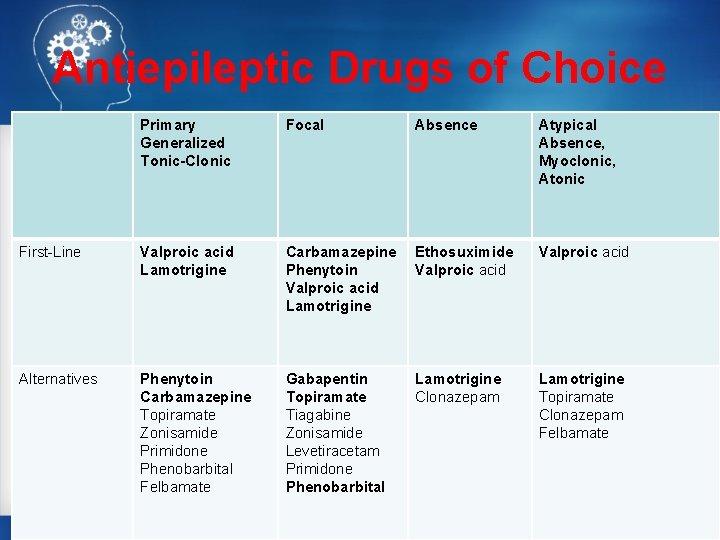
Antiepileptic Drugs of Choice Primary Generalized Tonic-Clonic Focal Absence Atypical Absence, Myoclonic, Atonic First-Line Valproic acid Lamotrigine Carbamazepine Phenytoin Valproic acid Lamotrigine Ethosuximide Valproic acid Alternatives Phenytoin Carbamazepine Topiramate Zonisamide Primidone Phenobarbital Felbamate Gabapentin Topiramate Tiagabine Zonisamide Levetiracetam Primidone Phenobarbital Lamotrigine Clonazepam Lamotrigine Topiramate Clonazepam Felbamate
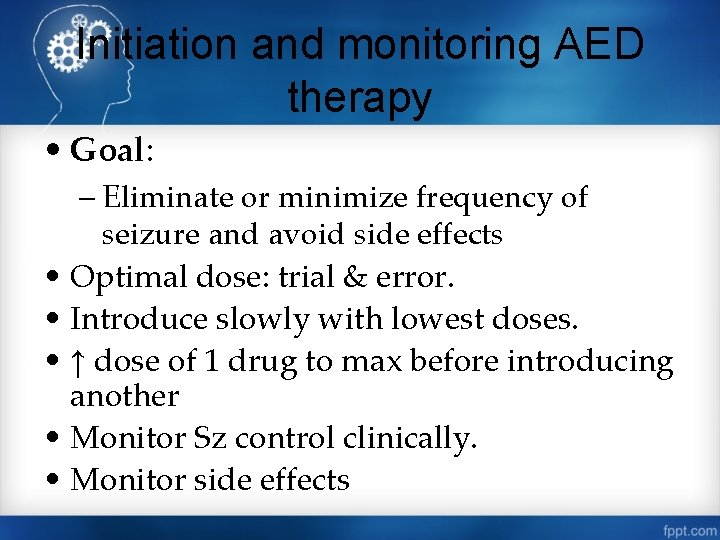
Initiation and monitoring AED therapy • Goal: – Eliminate or minimize frequency of seizure and avoid side effects • Optimal dose: trial & error. • Introduce slowly with lowest doses. • ↑ dose of 1 drug to max before introducing another • Monitor Sz control clinically. • Monitor side effects
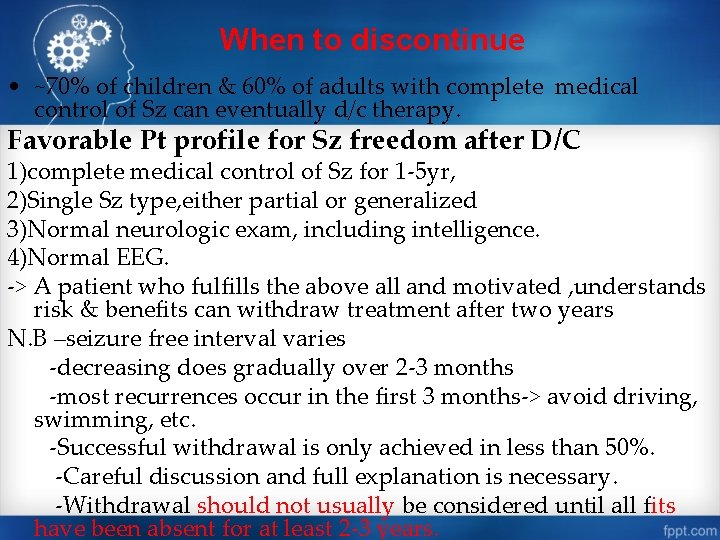
When to discontinue • ~70% of children & 60% of adults with complete medical control of Sz can eventually d/c therapy. Favorable Pt profile for Sz freedom after D/C 1)complete medical control of Sz for 1 -5 yr, 2)Single Sz type, either partial or generalized 3)Normal neurologic exam, including intelligence. 4)Normal EEG. -> A patient who fulfills the above all and motivated , understands risk & benefits can withdraw treatment after two years N. B –seizure free interval varies -decreasing does gradually over 2 -3 months -most recurrences occur in the first 3 months-> avoid driving, swimming, etc. -Successful withdrawal is only achieved in less than 50%. -Careful discussion and full explanation is necessary. -Withdrawal should not usually be considered until all fits have been absent for at least 2 -3 years.
Status epilepticus • occurrence of a single unremitting seizure with a duration longer than 5 to 10 minutes or frequent clinical seizures without regaining consciousness in between. • 50, 000 -60, 000 cases in the U. S. each year. • 18 -28 per 100, 000 persons in the U. S. and U. K. • SE is most common at the extremes of age.
PATHOPHYSIOLOGY • Cardio respiratory dysfunction, hyperthermia, & metabolic derangements → irreversible neuronal damage. • Significant physiologic changes accompany SE: -Catecholamine surge -Hypertension, tachycardia, cardiac arrhythmias, hyperglycemia occur (early) -Body temperature may increase and lactic acidosis is common. -Cerebral metabolic demand increases, however, cerebral blood flow and oxygenation are persevered or slightly elevated.
• The hippocampus, seems especially vulnerable to damage by this mechanism. • Neuronal damage during SE results primarily from continuing seizure discharges rather any systemic effects of convulsions. • The longer SE continues the clinical manifestations will be subtle
• causes • Antiepileptic drug noncompliance or discontinuation • Withdrawal syndromes (eg. discontinuation of alcohol) • Acute structural injury (eg, brain tumor , stroke, head trauma) or infection (encephalitis, meningitis, abscess). • Remote or longstanding structural injury (eg, prior head injury) • Metabolic abnormalities • Use of, or overdose with drugs that lower the seizure threshold (eg, theophylline)
classification • Generalized Convulsive Status Epilepticus • Simple Partial Status Epilepticus • Complex Partial Status Epilepticus • Absence Status Epilepticus • Generalized Myoclonic Status Epilepticus
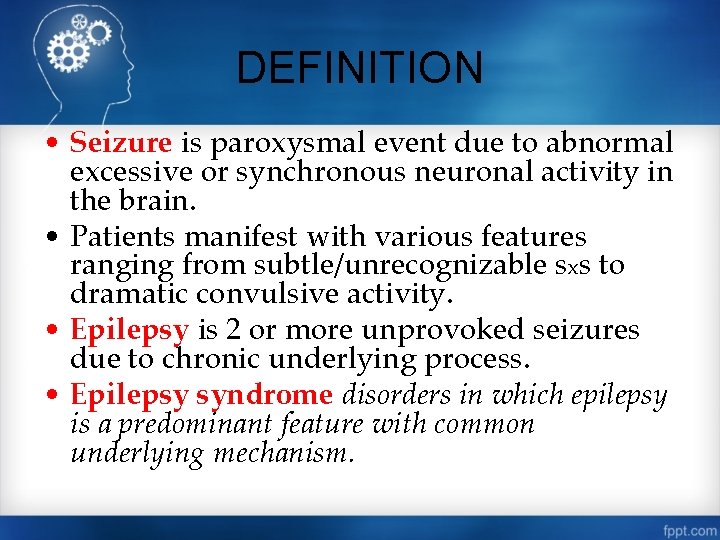
management • A medical emergency. • ABC Determine serum glucose IV thiamine 100 mg; 50 ml of 50% glucose. Supportive: O 2, positioning, iv fluids ü Rapid general evaluation & neurologic exam- to establish the diagnosis Draw blood for OFT, Serum electrolytes, toxicology screening AED: IV diazepam/lorazepam→iv phenytoin Add IV phenobarbital Last option propofol or barbiturate coma
 Shaking vs seizure
Shaking vs seizure Epilepsy
Epilepsy Difference between seizure and epilepsy
Difference between seizure and epilepsy Dr alazar
Dr alazar Dr alazar
Dr alazar Seizure threshold meaning
Seizure threshold meaning What is a quote sandwich examples
What is a quote sandwich examples Difference between jitteriness and seizure
Difference between jitteriness and seizure Seizure types and symptoms
Seizure types and symptoms Plessy v ferguson
Plessy v ferguson A mob's illegal seizure and execution of a person.
A mob's illegal seizure and execution of a person. A mob's illegal seizure and execution of a person
A mob's illegal seizure and execution of a person Baseline vital signs
Baseline vital signs Postictal
Postictal Keppra loading dose
Keppra loading dose Seizure precautions bed rails
Seizure precautions bed rails Hypsarrhythmia eeg
Hypsarrhythmia eeg Ativan status epilepticus
Ativan status epilepticus Warning signs of a seizure
Warning signs of a seizure Seizure precautions nursing
Seizure precautions nursing Gregory barkley md
Gregory barkley md Seizure vs syncope
Seizure vs syncope Juhayman
Juhayman Vestibular neuritis vs labyrinthitis
Vestibular neuritis vs labyrinthitis Febrile seizure criteria
Febrile seizure criteria Cps epilepsy
Cps epilepsy Epilepsy trigger
Epilepsy trigger Seizure
Seizure Non epileptic seizures
Non epileptic seizures Postical
Postical Stages of seizure
Stages of seizure Epilepsy symptoms
Epilepsy symptoms Seizure
Seizure Food red flags
Food red flags Febrile convulsion
Febrile convulsion Suped seizure
Suped seizure Simple partial seizures vs complex
Simple partial seizures vs complex Seizure
Seizure Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Catamenial epilepsy and birth control pills
Catamenial epilepsy and birth control pills