Epilepsy Surgery American Epilepsy Society Epilepsy Care Seizure

- Slides: 32
Epilepsy Surgery American Epilepsy Society
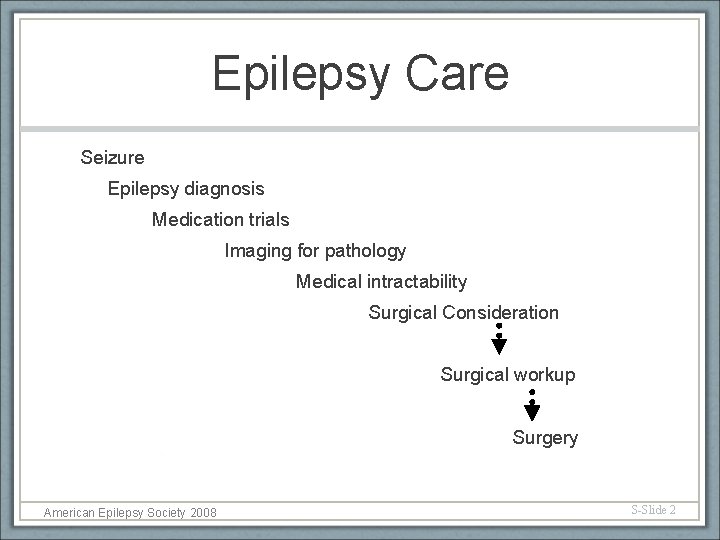
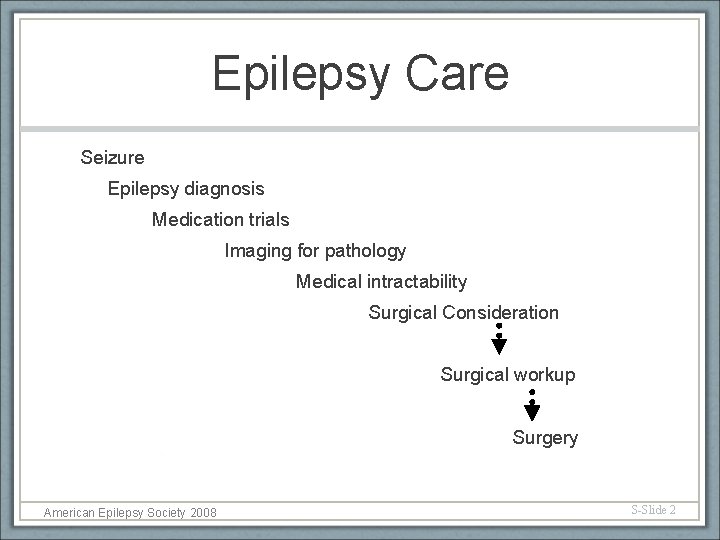
Epilepsy Care Seizure Epilepsy diagnosis Medication trials Imaging for pathology Medical intractability Surgical Consideration Surgical workup Surgery American Epilepsy Society 2008 S-Slide 2
Candidates for Epilepsy Surgery Persistent seizures despite appropriate pharmacological treatment Usually at least two drugs, appropriate to seizure type, at adequate doses, with adequate compliance Impairment of quality of life due to ongoing seizures Loss of driving privileges, employment opportunities, social/cultural stigma, dependence on others, side effects of medications, under achievement in school, memory deficit, attention deficit, injuries, accidents American Epilepsy Society 2008 S-Slide 3
Presurgical Evaluation § History and Physical Exam § Electroencephalography § Imaging § Presurgical Testing § Neuropsychology Evaluation § Comprehensive Patient Care Conference American Epilepsy Society 2008 S-Slide 4
Imaging for Surgical Candidates MRI- with epilepsy protocols • T 1 - inversion prepared, gradient-echo, echoplanar, true inversion recovery image • T-2 - fast spin echo, FLAIR, 3 D volume acquisition American Epilepsy Society 2008 S-Slide 5
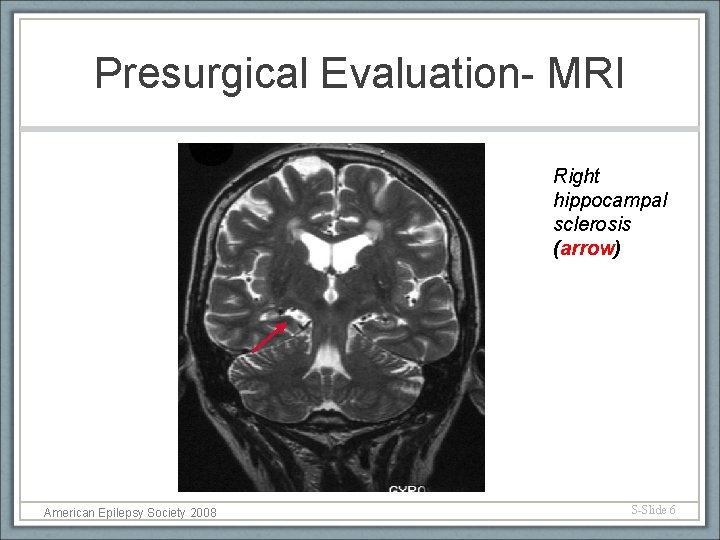
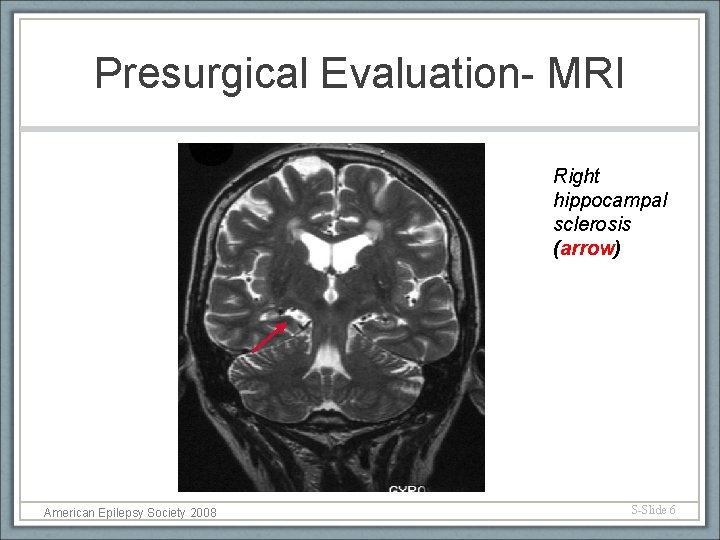
Presurgical Evaluation- MRI Right hippocampal sclerosis (arrow) American Epilepsy Society 2008 S-Slide 6
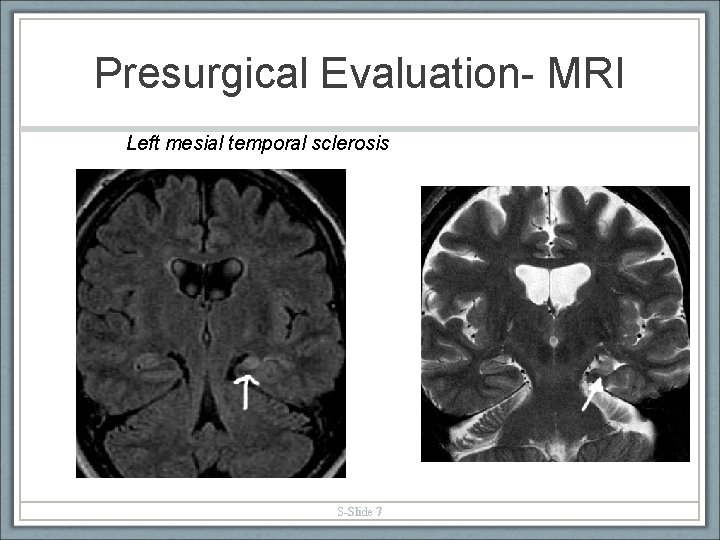
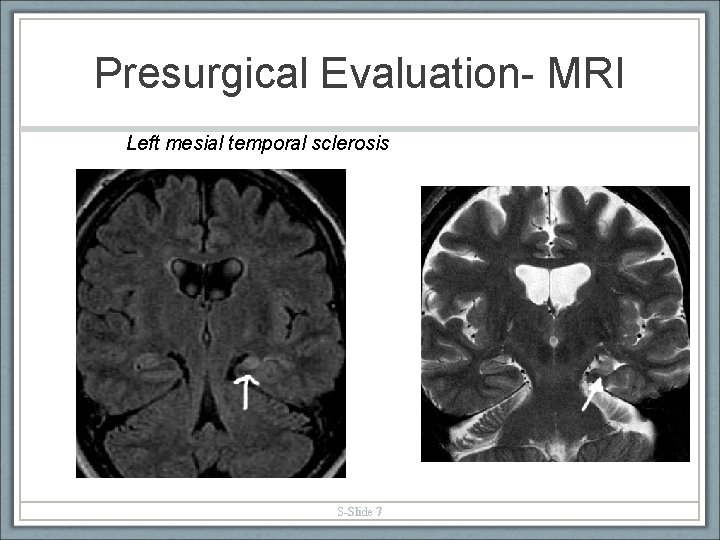
Presurgical Evaluation- MRI Left mesial temporal sclerosis S-Slide 7
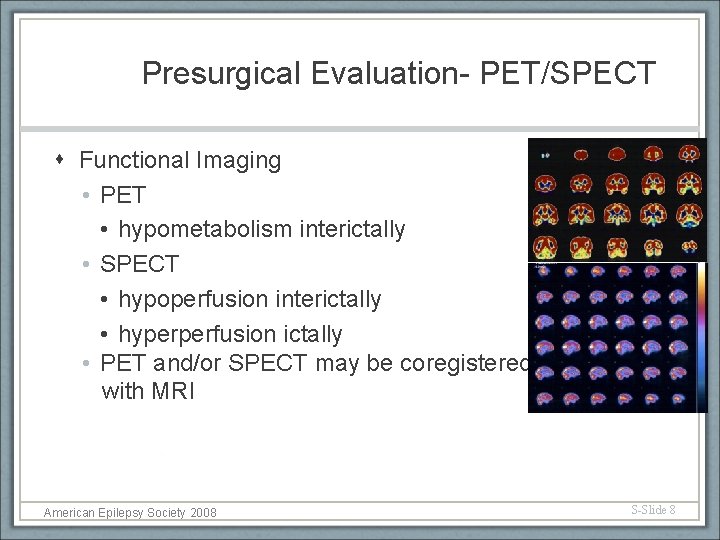
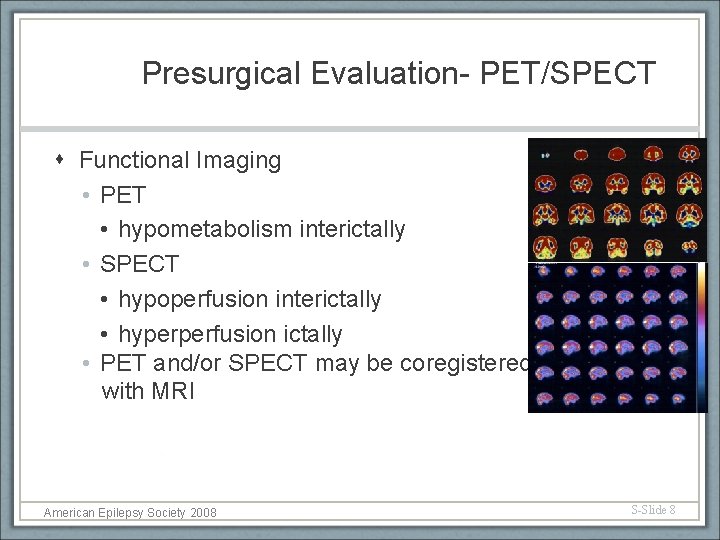
Presurgical Evaluation- PET/SPECT Functional Imaging • PET • hypometabolism interictally • SPECT • hypoperfusion interictally • hyperperfusion ictally • PET and/or SPECT may be coregistered with MRI American Epilepsy Society 2008 S-Slide 8
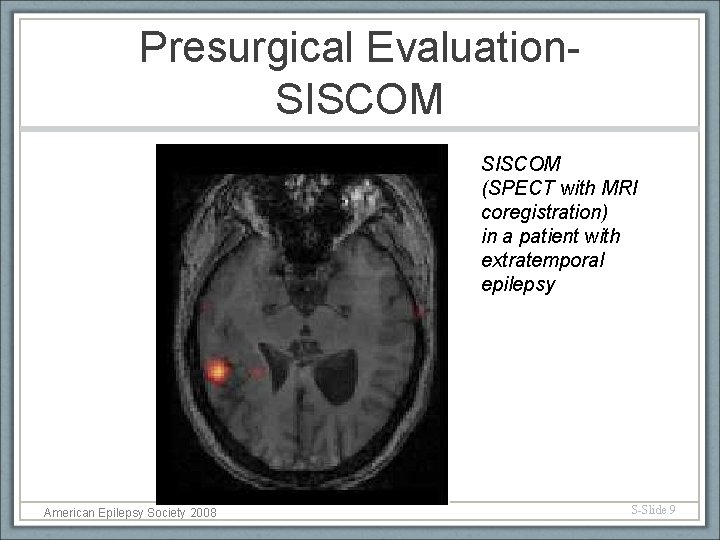
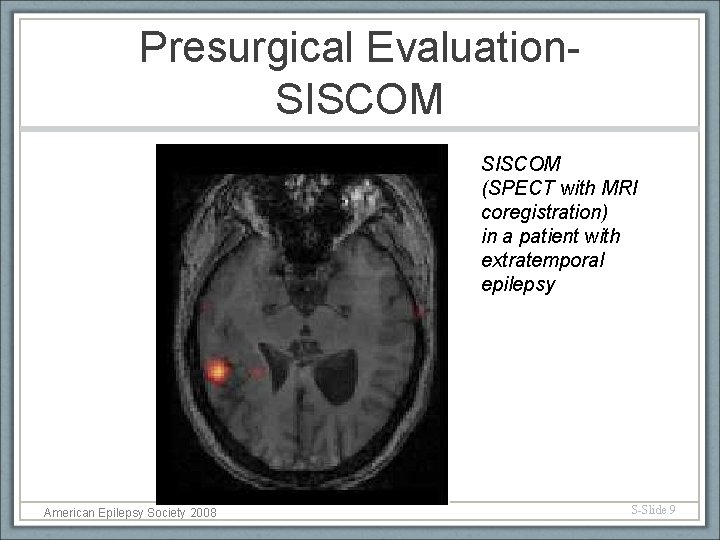
Presurgical Evaluation. SISCOM (SPECT with MRI coregistration) in a patient with extratemporal epilepsy American Epilepsy Society 2008 S-Slide 9
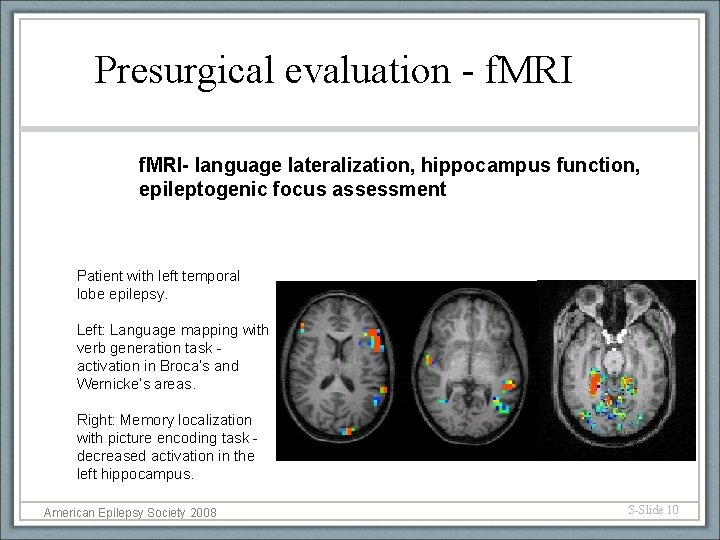
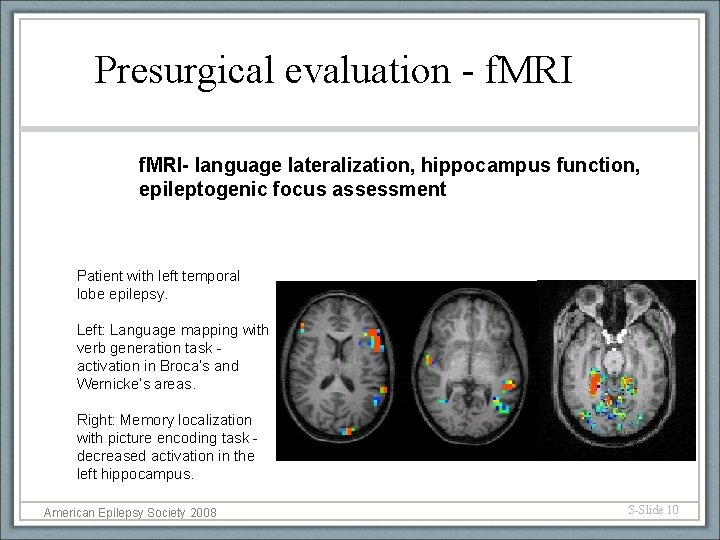
Presurgical evaluation - f. MRI- language lateralization, hippocampus function, epileptogenic focus assessment Patient with left temporal lobe epilepsy. Left: Language mapping with verb generation task activation in Broca’s and Wernicke’s areas. Right: Memory localization with picture encoding task decreased activation in the left hippocampus. American Epilepsy Society 2008 S-Slide 10
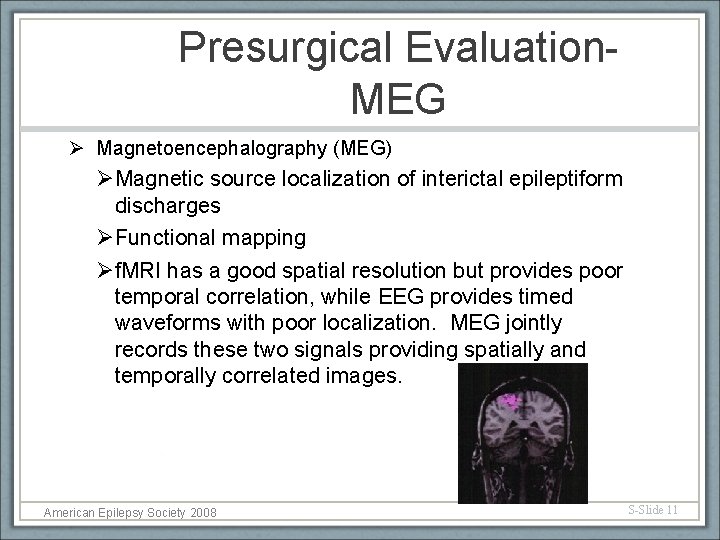
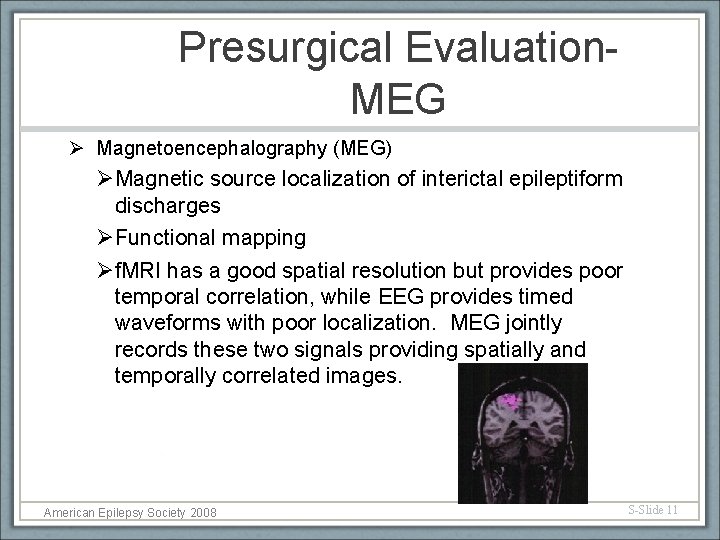
Presurgical Evaluation. MEG Ø Magnetoencephalography (MEG) ØMagnetic source localization of interictal epileptiform discharges ØFunctional mapping Øf. MRI has a good spatial resolution but provides poor temporal correlation, while EEG provides timed waveforms with poor localization. MEG jointly records these two signals providing spatially and temporally correlated images. American Epilepsy Society 2008 S-Slide 11
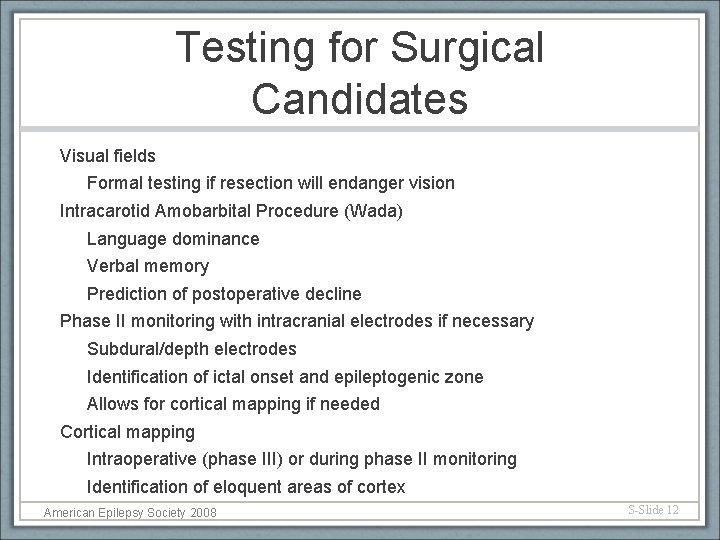
Testing for Surgical Candidates Visual fields Formal testing if resection will endanger vision Intracarotid Amobarbital Procedure (Wada) Language dominance Verbal memory Prediction of postoperative decline Phase II monitoring with intracranial electrodes if necessary Subdural/depth electrodes Identification of ictal onset and epileptogenic zone Allows for cortical mapping if needed Cortical mapping Intraoperative (phase III) or during phase II monitoring Identification of eloquent areas of cortex American Epilepsy Society 2008 S-Slide 12
Neuropsychological Evaluation for Surgical Candidates Provides preoperative baseline Predicts risk of cognitive decline with surgery Testing includes: IQ battery of tests Language localization Memory- verbal and visual localization Visuospatial function Attention/Executive Motor- coordination and speed Psych- expectations of surgery, coping skills, social support, stability American Epilepsy Society 2008 S-Slide 13
Comprehensive Patient Care Conference for Surgical Candidates § Epileptologist presents the patient § Video-EEG studies are reviewed § Semiology § Interictal EEG morphology § Ictal EEG morphology § Neuroradiologist discusses imaging studies § Neuropsychology results are examined § Neurosurgeon delineates surgical options § Discussion of risks/benefits/outcomes § Group consensus American Epilepsy Society 2008 S-Slide 14
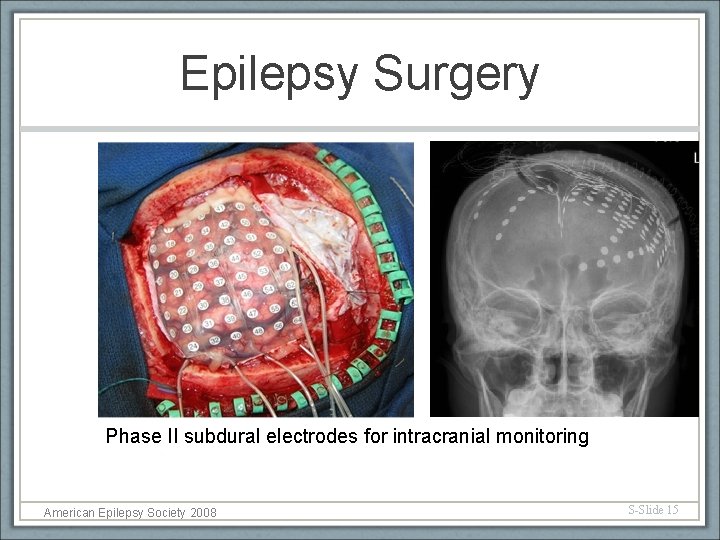
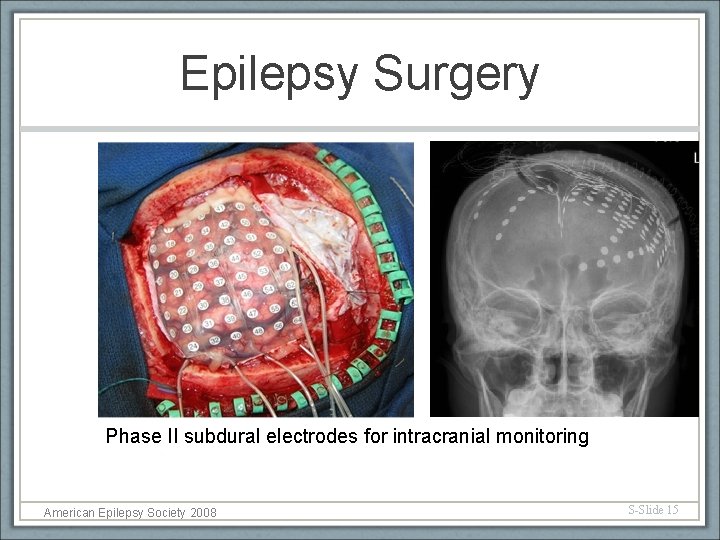
Epilepsy Surgery Phase II subdural electrodes for intracranial monitoring American Epilepsy Society 2008 S-Slide 15
Types of Surgical Procedures Resective Surgery: Lesionectomy Selective amygdalohippocampectomy Corticectomy Lobectomy (e. g. temporal lobectomy) Multilobar resection American Epilepsy Society 2008 S-Slide 16
Types of Surgical Procedures Disconnective/Palliative Surgery: Hemispherectomy Anatomic Functional Corpus Callosotomy Multiple Subpial Transections Vagus Nerve Stimulator American Epilepsy Society 2008 S-Slide 17

Surgical Treatment of Epilepsy MRI frameless stereotactic localization of focal cortical dysplasia at the base of the central sulcus (center of cross hairs) American Epilepsy Society 2008 S-Slide 18
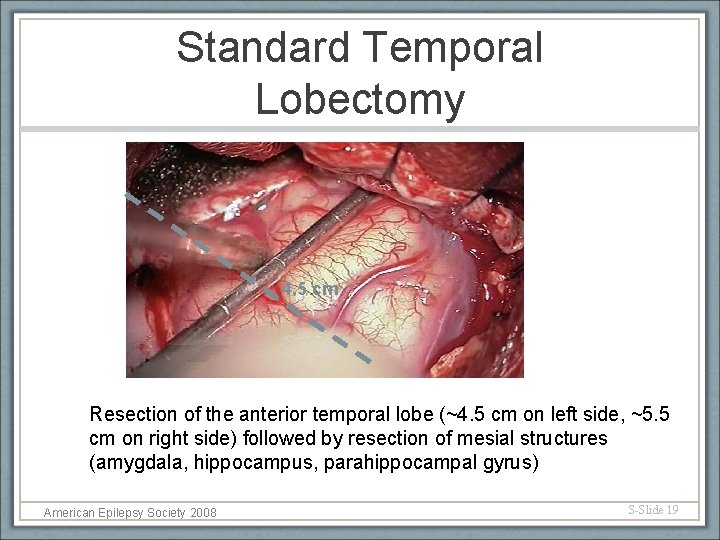
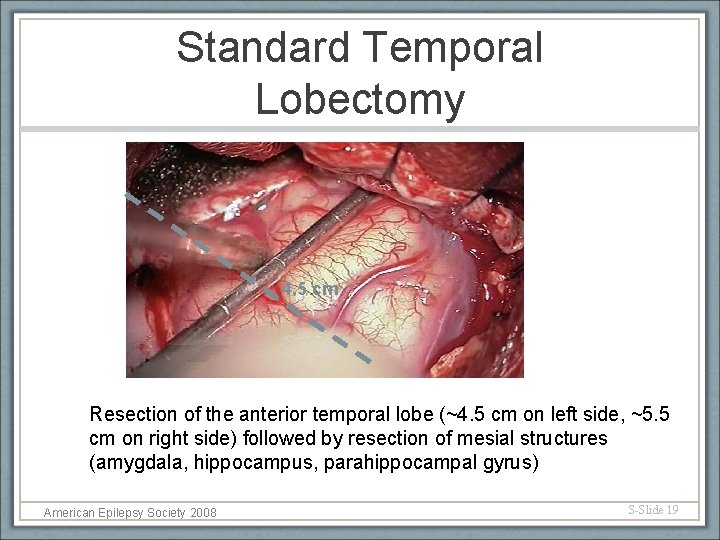
Standard Temporal Lobectomy 4. 5 cm Resection of the anterior temporal lobe (~4. 5 cm on left side, ~5. 5 cm on right side) followed by resection of mesial structures (amygdala, hippocampus, parahippocampal gyrus) American Epilepsy Society 2008 S-Slide 19
Selective Amygdalohippocampectomy Idea is to remove mesial structures (hippocampus, amygdala, parahippocampal gyrus) leaving lateral temporal cortex intact Distinct surgical approaches include: Transsylvian Transcortical Subtemporal American Epilepsy Society 2008 S-Slide 20
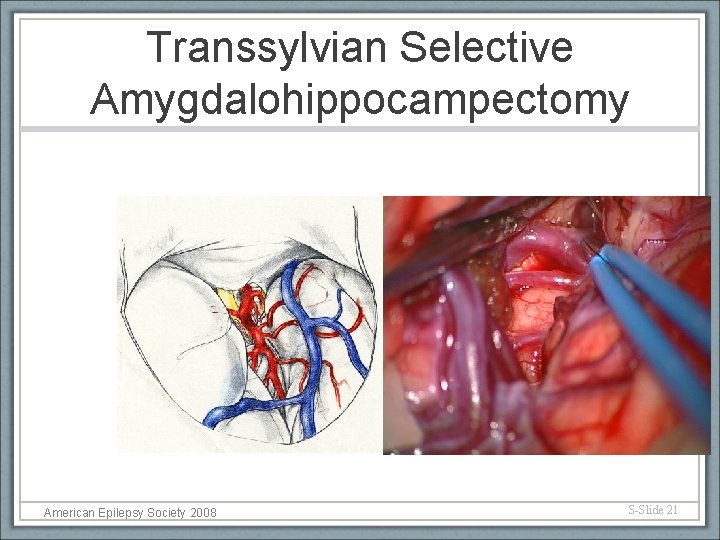
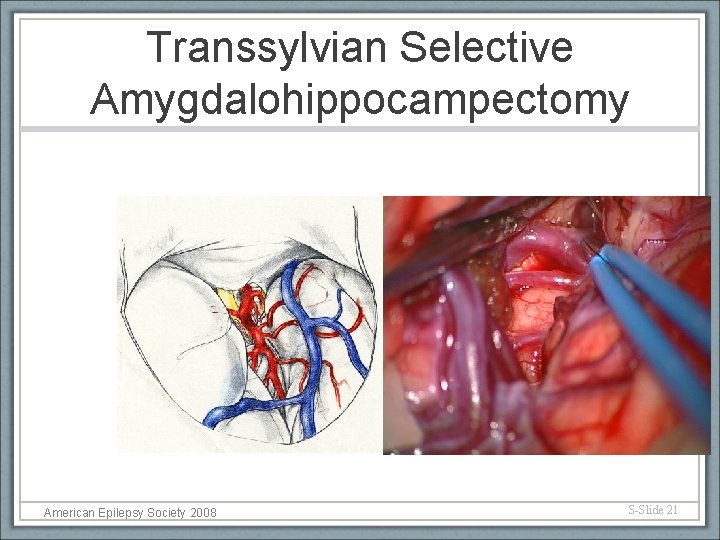
Transsylvian Selective Amygdalohippocampectomy American Epilepsy Society 2008 S-Slide 21
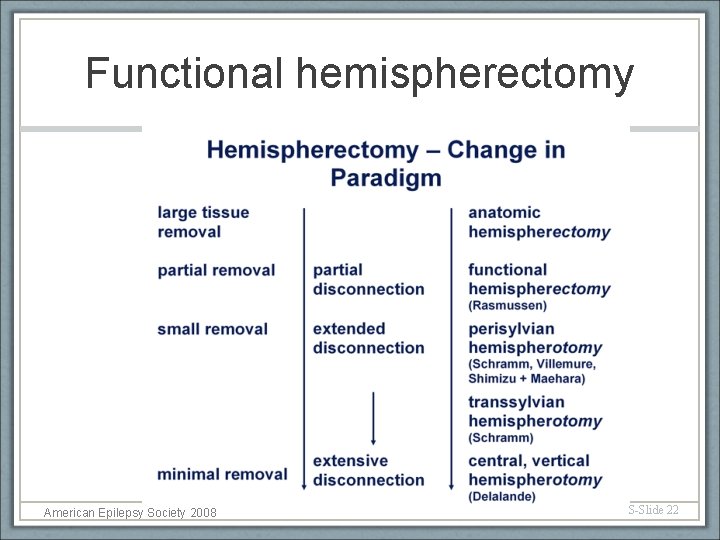
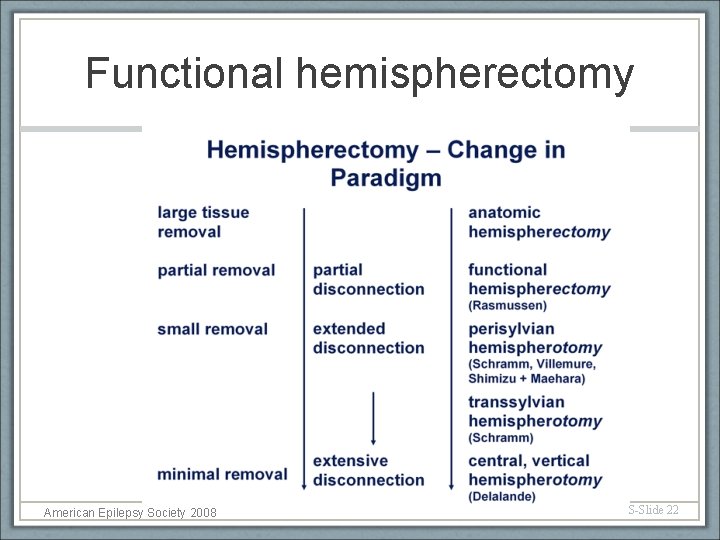
Functional hemispherectomy American Epilepsy Society 2008 S-Slide 22
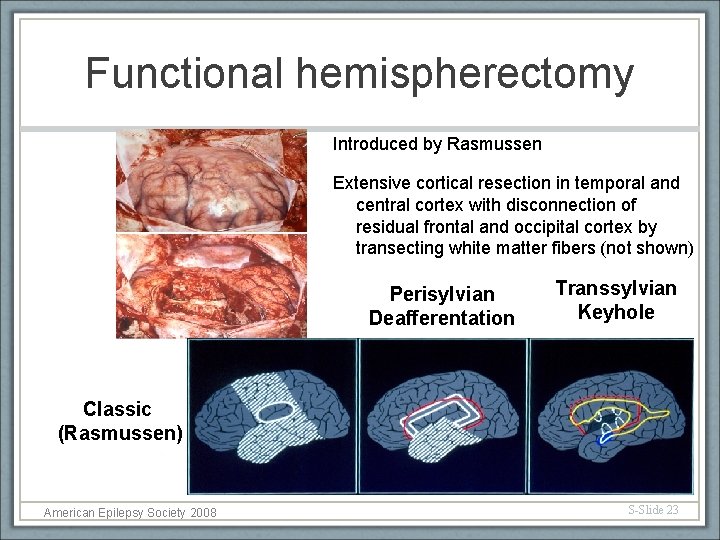
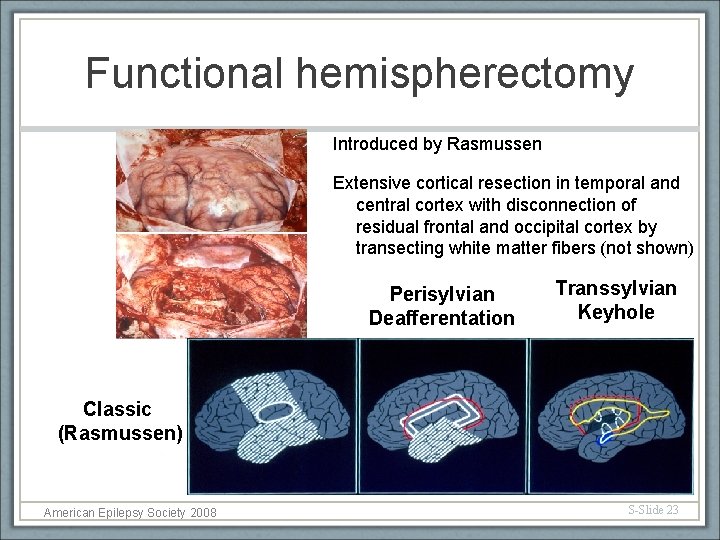
Functional hemispherectomy Introduced by Rasmussen Extensive cortical resection in temporal and central cortex with disconnection of residual frontal and occipital cortex by transecting white matter fibers (not shown) Perisylvian Deafferentation Transsylvian Keyhole Classic (Rasmussen) American Epilepsy Society 2008 S-Slide 23
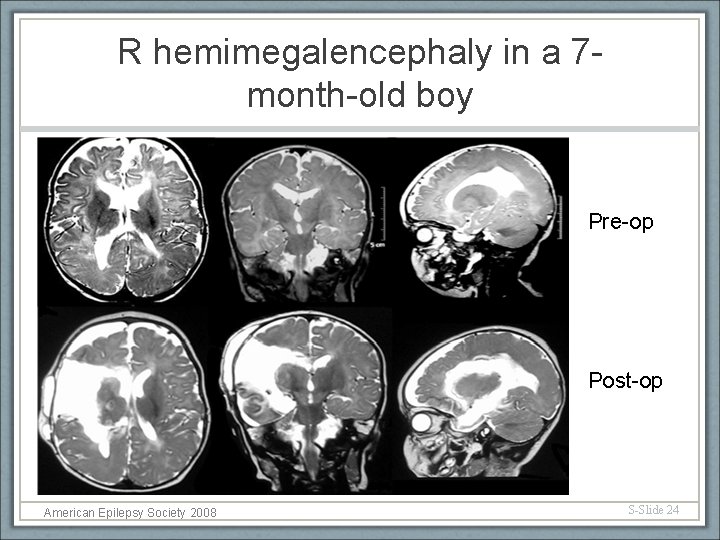
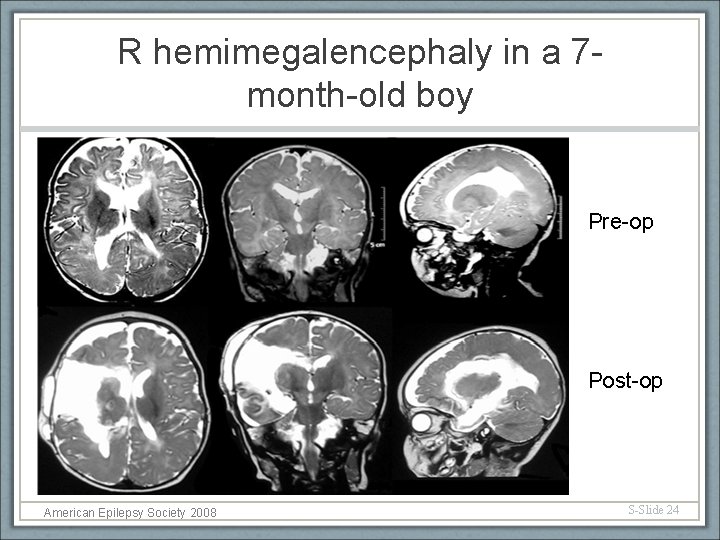
R hemimegalencephaly in a 7 month-old boy Pre-op Post-op American Epilepsy Society 2008 S-Slide 24
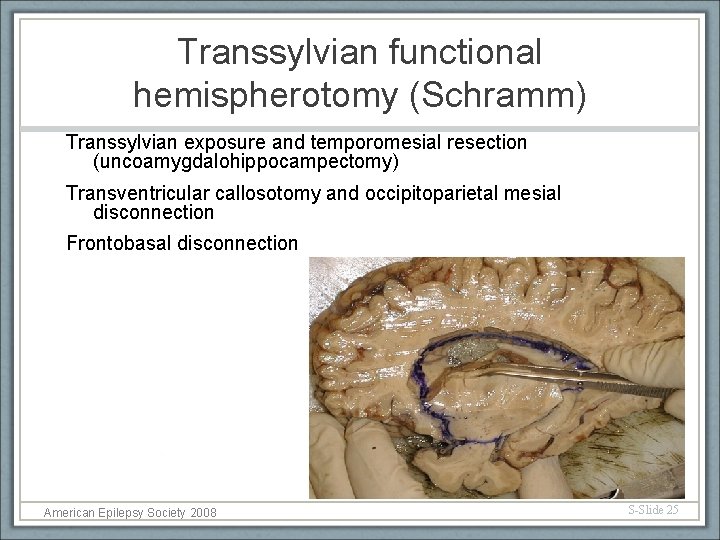
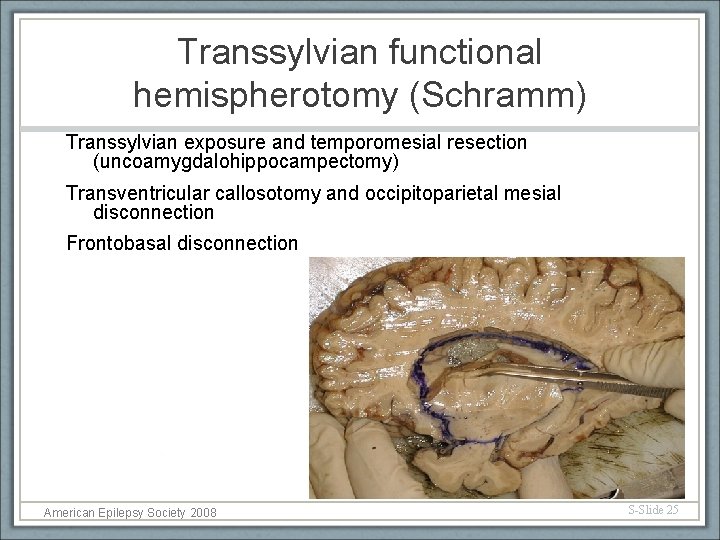
Transsylvian functional hemispherotomy (Schramm) Transsylvian exposure and temporomesial resection (uncoamygdalohippocampectomy) Transventricular callosotomy and occipitoparietal mesial disconnection Frontobasal disconnection American Epilepsy Society 2008 S-Slide 25
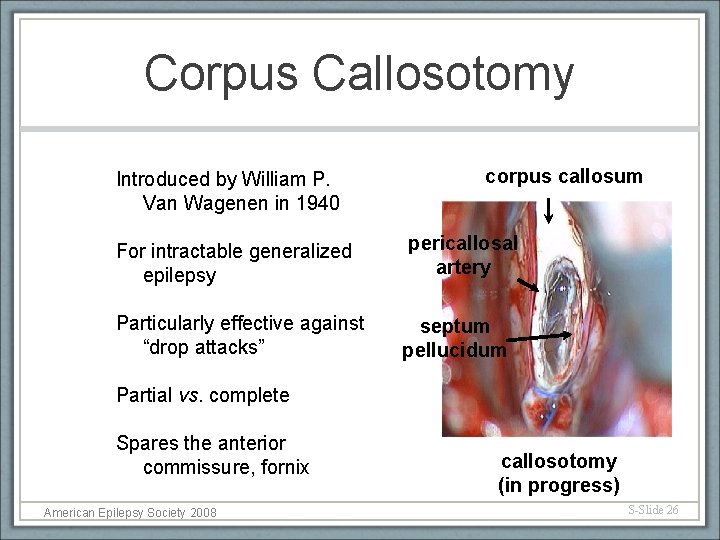
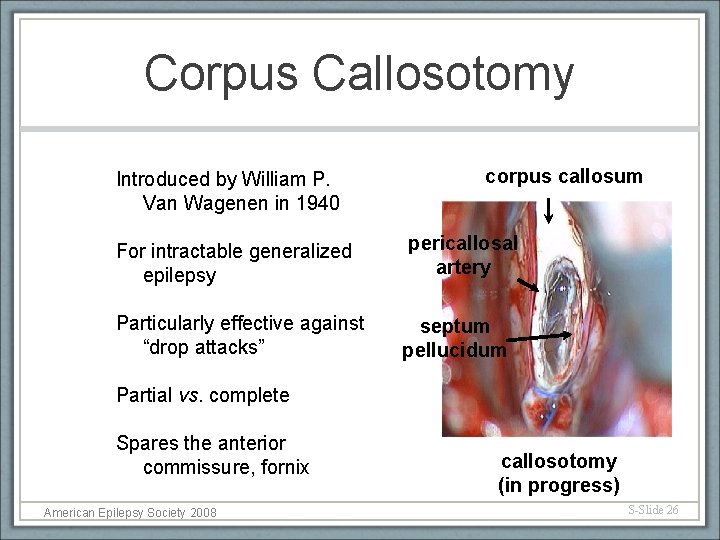
Corpus Callosotomy Introduced by William P. Van Wagenen in 1940 For intractable generalized epilepsy Particularly effective against “drop attacks” corpus callosum pericallosal artery septum pellucidum Partial vs. complete Spares the anterior commissure, fornix American Epilepsy Society 2008 callosotomy (in progress) S-Slide 26
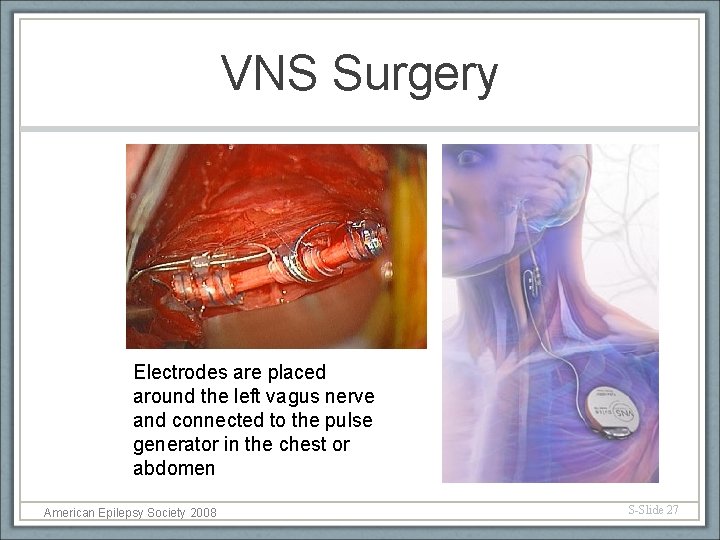
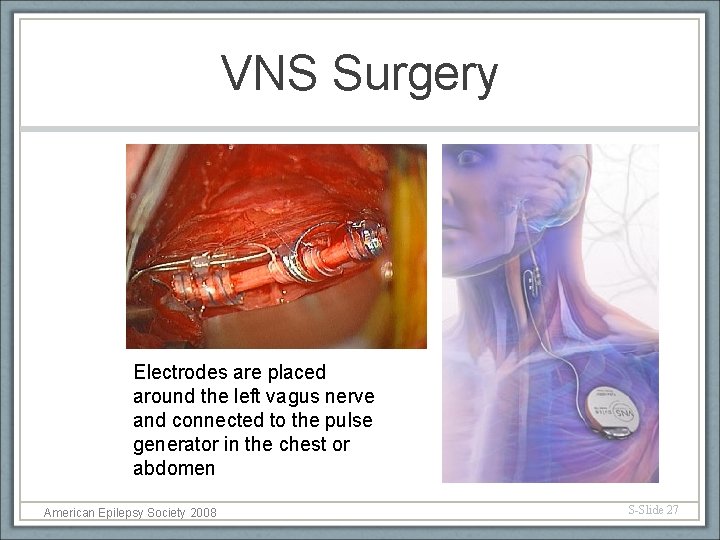
VNS Surgery Electrodes are placed around the left vagus nerve and connected to the pulse generator in the chest or abdomen American Epilepsy Society 2008 S-Slide 27
Clinical Trials Experimental Surgical Treatments Under Clinical Trials • Deep brain stimulation • Responsive neurostimulation • Gamma knife radiosurgery American Epilepsy Society 2008 S-Slide 28
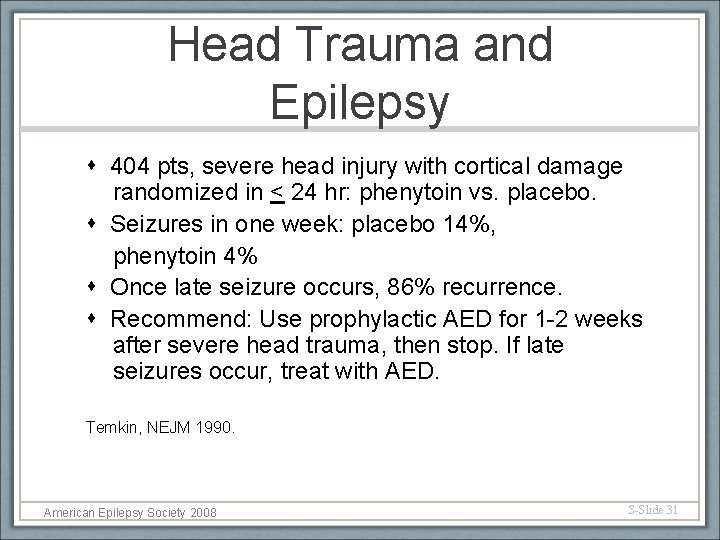
Head Trauma and Epilepsy • Acute symptomatic seizures • Usually within few days after head trauma • Incidence is proportional to the severity of trauma • Remote symptomatic seizures • Seizure prevention in patients with traumatic brain injury American Epilepsy Society 2008 S-Slide 29
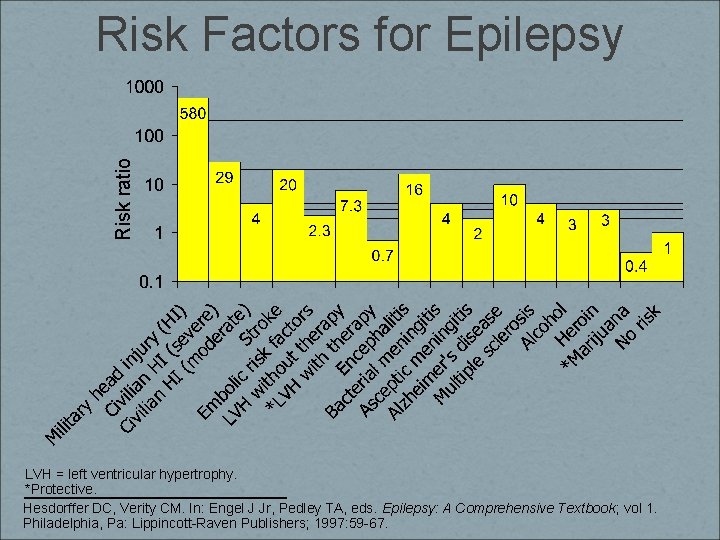
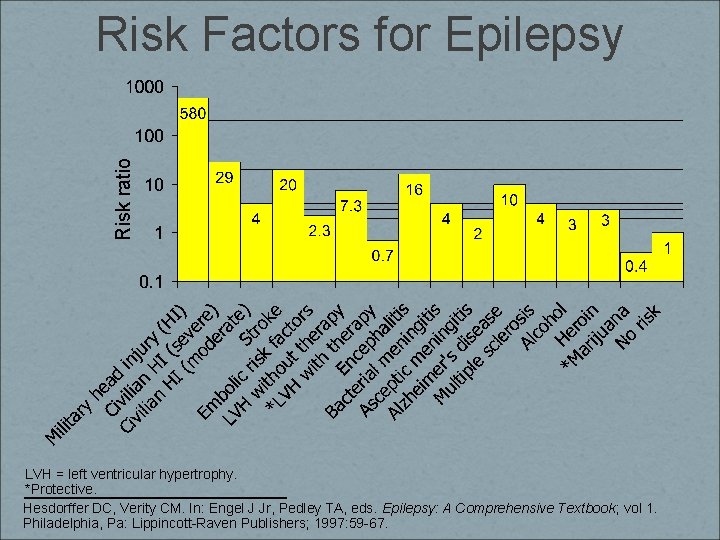
Risk ratio Risk Factors for Epilepsy LVH = left ventricular hypertrophy. *Protective. Hesdorffer DC, Verity CM. In: Engel J Jr, Pedley TA, eds. Epilepsy: A Comprehensive Textbook ; vol 1. Philadelphia, Pa: Lippincott-Raven Publishers; 1997: 59 -67.
Head Trauma and Epilepsy 404 pts, severe head injury with cortical damage randomized in < 24 hr: phenytoin vs. placebo. Seizures in one week: placebo 14%, phenytoin 4% Once late seizure occurs, 86% recurrence. Recommend: Use prophylactic AED for 1 -2 weeks after severe head trauma, then stop. If late seizures occur, treat with AED. Temkin, NEJM 1990. American Epilepsy Society 2008 S-Slide 31
Conclusion Ø Many patients with medically-intractable epilepsy are surgical candidates Ø All patients with epilepsy should undergo epilepsy protocol imaging Ø Many modern epilepsy surgery options exist, including resection, disconnection and palliation American Epilepsy Society 2008 S-Slide 32
 Difference between seizure and epilepsy
Difference between seizure and epilepsy Epilepsy and seizure services near walnut creek
Epilepsy and seizure services near walnut creek Difference between seizure and epilepsy
Difference between seizure and epilepsy American epilepsy society annual meeting 2017
American epilepsy society annual meeting 2017 Susanne finn
Susanne finn Types of care primary secondary tertiary
Types of care primary secondary tertiary Postoperative nursing diagnosis of cataract
Postoperative nursing diagnosis of cataract Gertler econ
Gertler econ Guidelines for measuring vital signs
Guidelines for measuring vital signs Postictal
Postictal Seizure vs syncope
Seizure vs syncope Seizure precautions bed rails
Seizure precautions bed rails Myoclonic seizure symptoms
Myoclonic seizure symptoms Ativan status epilepticus
Ativan status epilepticus Jitteriness and seizure
Jitteriness and seizure Warning signs of a seizure
Warning signs of a seizure Seizure precautions bed rails
Seizure precautions bed rails Dr gregory barkley
Dr gregory barkley Migraine vs epilepsy
Migraine vs epilepsy Grand mosque seizure
Grand mosque seizure Meniere's disease
Meniere's disease Febrile seizure criteria
Febrile seizure criteria Aed medical abbreviation seizure
Aed medical abbreviation seizure Seizure triggers
Seizure triggers Seizure
Seizure Seizure threshold definition
Seizure threshold definition Non epileptic seizure
Non epileptic seizure Epilepsy ilae 2017
Epilepsy ilae 2017 Post-ictal
Post-ictal Stages of seizure
Stages of seizure Seizures
Seizures Lateral rectus spikes eeg
Lateral rectus spikes eeg Warning signs of a seizure
Warning signs of a seizure