Drugs for Epilepsy Definition of Epilepsy Group of
- Slides: 20
Drugs for Epilepsy
Definition of Epilepsy Group of disorders characterized by excessive excitability of neurons in the CNS Can produce a variety of symptoms ranging from brief periods of unconsciousness to violent convulsions May also cause problems with learning, memory, and mood
Seizure: Generation Initiated by synchronous, high-frequency discharge from a group of hyperexcitable neurons called a focus Focus may result from Ø Ø Ø Ø Congenital defects Hypoxia at birth Head trauma Brain infection Stroke Cancer Genetic disorders
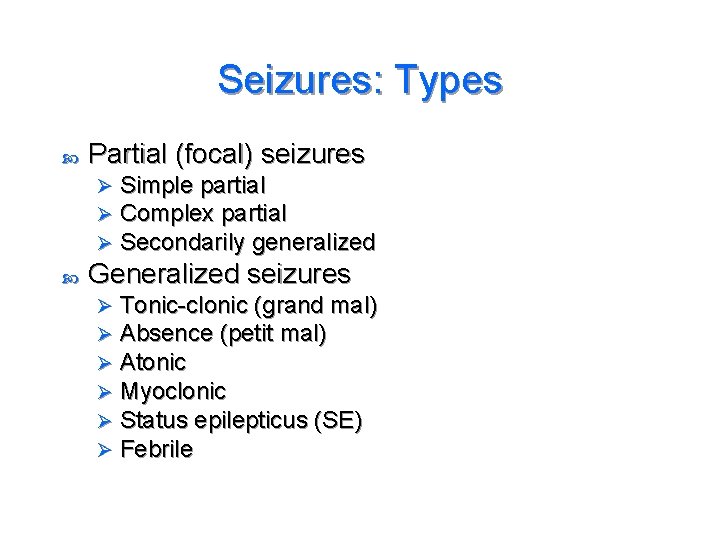
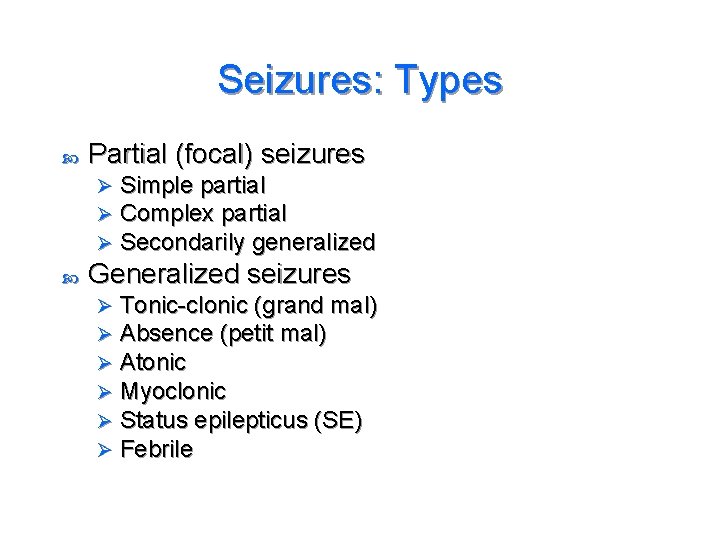
Seizures: Types Partial (focal) seizures Ø Ø Ø Simple partial Complex partial Secondarily generalized Generalized seizures Ø Ø Ø Tonic-clonic (grand mal) Absence (petit mal) Atonic Myoclonic Status epilepticus (SE) Febrile
Antiepileptic Drugs Effects Suppress discharge of neurons within a seizure focus Ø Suppress propagation of seizure activity from the focus to other areas of the brain Ø Mechanisms of action Ø Ø Suppression of sodium influx Suppression of calcium influx Antagonism of glutamate Potentiation of GABA
Mixed Seizures: Lennox-Gastaut Syndrome Severe form of epilepsy that usually develops during the preschool years Developmental delay and a mixture of partial and generalized seizures
Goal of Treatment Reduce seizures to a level that allows the patient to live as normal a life as possible Balance the desire for complete seizure control with the acceptability of side effects
Epilepsy: Therapeutic Considerations Treatment goal and treatment options Ø Ø Ø Neurosurgery (best success rate) Vagal nerve stimulation Ketogenic diet Diagnosis and drug selection Drug evaluation
Epilepsy: Therapeutic Considerations Monitoring plasma drug levels Promoting patient adherence Withdrawing antiepileptic drugs Suicide risk – antiepileptic drugs
Classification of Antiepileptic Drugs Two major categories Traditional antiepileptic drugs (AEDs) • Phenytoin, carbamazepine, valproic acid, and others Ø Newer AEDs • Oxcarbazepine, gabapentin, zonisamide, and others Ø
Phenytoin (Dilantin) Partial and tonic-clonic seizures Mechanism of action: selective inhibition of sodium channels Varied oral absorption Half-life: 8 to 60 hours
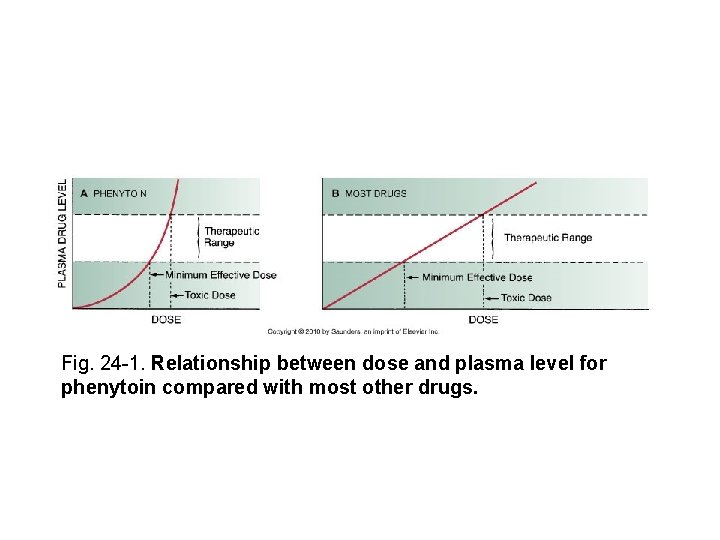
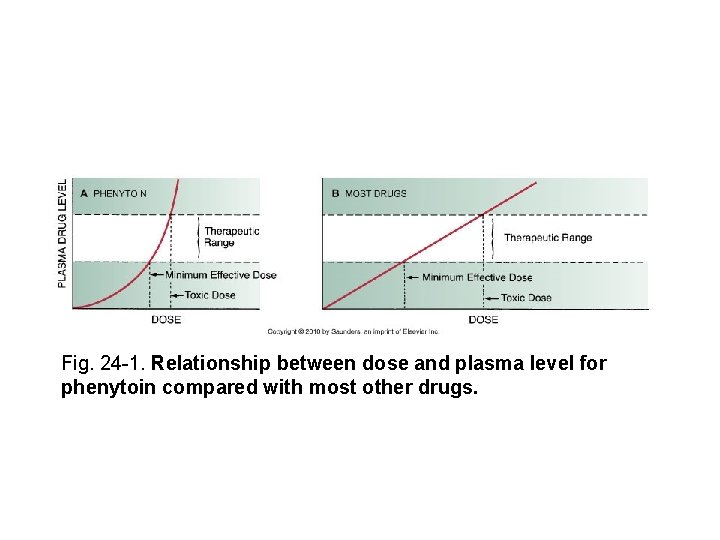
Fig. 24 -1. Relationship between dose and plasma level for phenytoin compared with most other drugs.
Phenytoin (Dilantin) Adverse effects Ø Ø Ø Ø Ø Nystagmus Sedation Ataxia Diplopia Cognitive impairment Gingival hyperplasia Skin rash Effects in pregnancy Cardiovascular effects
Phenytoin (Dilantin) Drug interactions Decreases the effects of oral contraceptives, warfarin, and glucocorticoids Ø Increases levels of diazepam, isoniazid, cimetidine, alcohol, and valproic acid Ø
Carbamazepine (Tegretol) Uses Ø Ø Ø Epilepsy Bipolar disorder Trigeminal and glossopharyngeal neuralgias Adverse effects Neurologic effects: nystagmus, ataxia Hematologic effects: leukopenia, anemia, thrombocytopenia Ø Birth defects Ø Hypo-osmolarity Ø Dermatologic effects: rash, photosensitivity reactions Ø Ø
Valproic Acid (Depakene, Depakote, Depacon) Uses Ø Ø Ø Seizure disorders Bipolar disorder Migraine Adverse effects Ø Ø GI effects Hepatotoxicity: liver failure Pancreatitis Teratogenic effects
Ethosuximide Drug of choice for absence seizures Generally devoid of significant adverse effects and interactions Initially may cause drowsiness, dizziness, and lethargy
Phenobarbital Uses Epilepsy (partial and generalized tonic-clonic seizures) Ø Promotes sleep and sedation Ø
Newer Antiepileptic Drugs Gabapentin Lamotrigine Levetiracetam Oxcarbazepine Tiagabine Topiramate Zonisamide
Management of Generalized Convulsive Status Epilepticus Continuous series of tonic-clonic seizures lasting 20 to 30 minutes Goals of treatment Maintain ventilation Correct hypoglycemia Terminate seizures • IV benzodiazepines (lorazepam or diazepam) Ø Initiate or continue long-term suppression drugs Ø Ø Ø
 Northeast regional epilepsy group
Northeast regional epilepsy group Northeast regional epilepsy
Northeast regional epilepsy Xl spikes on eeg
Xl spikes on eeg Scientific working group for the analysis of seized drugs
Scientific working group for the analysis of seized drugs Fspos
Fspos Typiska drag för en novell
Typiska drag för en novell Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Personalliggare bygg undantag
Personalliggare bygg undantag Tidböcker
Tidböcker A gastrica
A gastrica Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare Stig kerman
Stig kerman Hur skriver man en tes
Hur skriver man en tes Delegerande ledarskap
Delegerande ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Vätsketryck formel
Vätsketryck formel