Schizophrenia Other Psychotic Disorders Part 1 Clinical Presentation

![COND C] hallucinated voices, commenting permanently the behavior of the patient or they talk COND C] hallucinated voices, commenting permanently the behavior of the patient or they talk](https://slidetodoc.com/presentation_image_h2/3f60cd5c9774afeb16f8ebc2986a80ba/image-37.jpg)

- Slides: 56
Schizophrenia & Other Psychotic Disorders Part 1: Clinical Presentation 28/05/2020 Dr. Anurag Agrawal Associate Professor Department of Psychiatry C. I. M. S. & H. , LUCKNOW
Overview q. Introduction and History q. Epidemiology q. Etiology q. Clinical picture q. Diagnosis q. Subtypes q. Course and prognosis q. Treatment q. Complications
Definition �Fundamental and characteristic distortions of thinking and perception, and affects that are inappropriate or blunted. �Although discussed as a single disease, probably comprises a group of disorders. �Clear consciousness and intellectual capacity are usually maintained. �Certain cognitive deficits may evolve in the course of time.
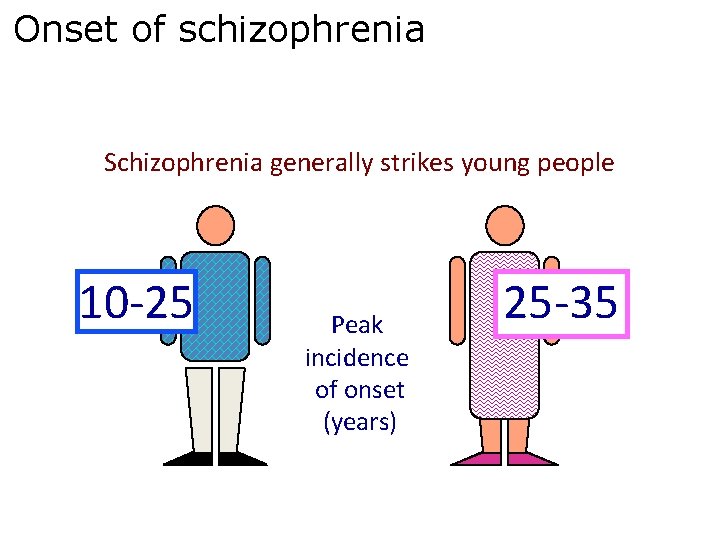
Schizophrenia • Schizophrenia occurs with regular frequency nearly everywhere in the world in 1 % of population and begins mainly in young age (mostly around 16 to 25 years). • Schizophrenia is defined by va group of characteristic positive and negative symptoms vdeterioration in social, occupational, or interpersonal relationships vcontinuous signs of the disturbance for at least 6 months
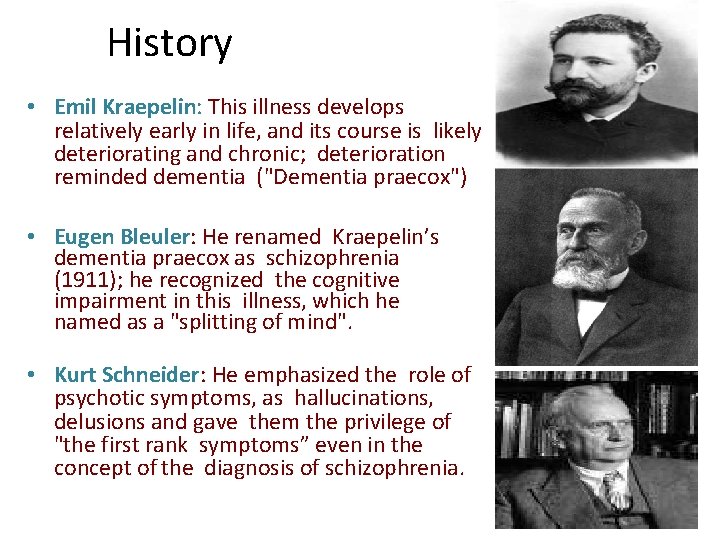
History • Emil Kraepelin: This illness develops relatively early in life, and its course is likely deteriorating and chronic; deterioration reminded dementia ("Dementia praecox") • Eugen Bleuler: He renamed Kraepelin’s dementia praecox as schizophrenia (1911); he recognized the cognitive impairment in this illness, which he named as a "splitting of mind". • Kurt Schneider: He emphasized the role of psychotic symptoms, as hallucinations, delusions and gave them the privilege of "the first rank symptoms” even in the concept of the diagnosis of schizophrenia.
4 A (Bleuler) • Bleuler maintained, that for the diagnosis of schizophrenia are most important the following four fundamental symptoms: • • • affective blunting association disturbance (fragmented thinking) autism ambivalence (fragmented emotional response) The other known symptoms, hallucinations, delusions, which are appearing in schizophrenia very often also, he used to call as a “secondary symptoms”
First rank symptoms (Kurt Schneider). • The most important psychopathological phenomena include – – – Thought echo Thought insertion or withdrawal Thought broadcasting Made impulse Made affect Made volition Audible thoughts 3 rd person hallucinations Running commentary Delusional perception Somatic passivity
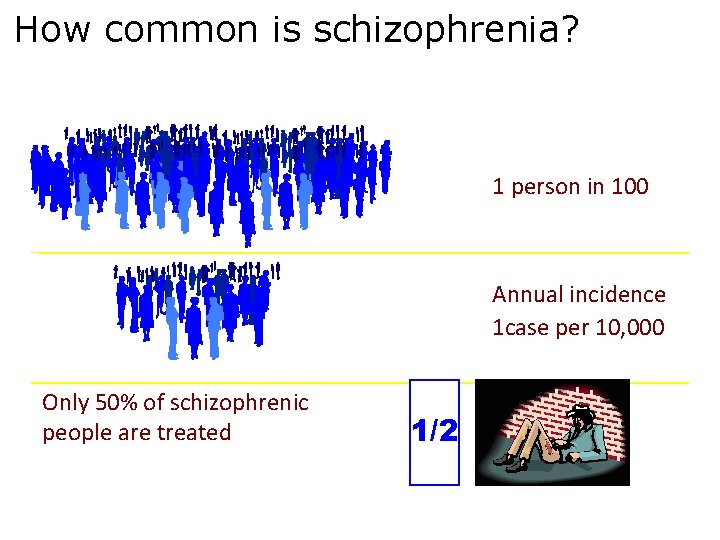
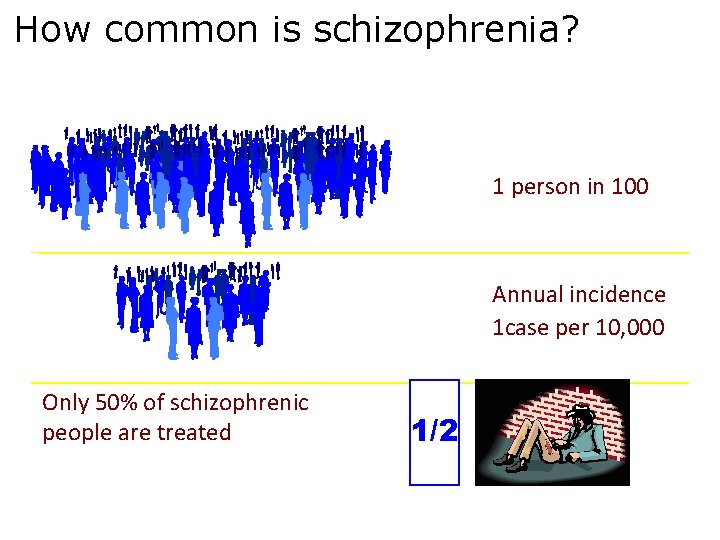
How common is schizophrenia? 1 person in 100 Annual incidence 1 case per 10, 000 Only 50% of schizophrenic people are treated 1/2
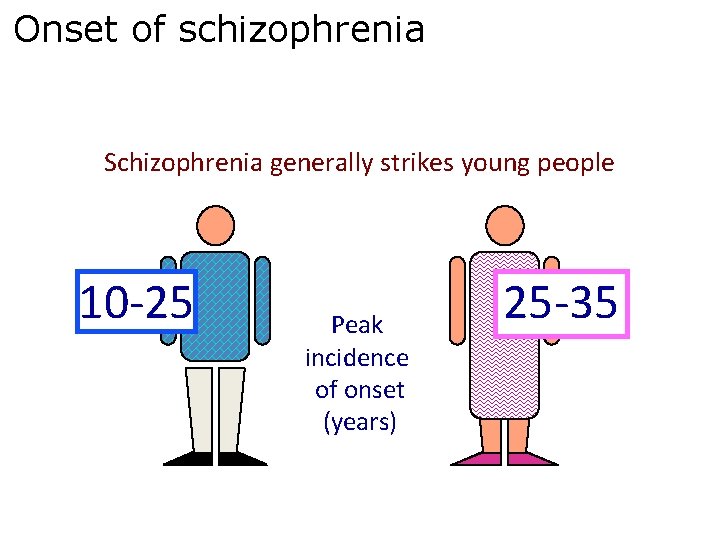
Onset of schizophrenia Schizophrenia generally strikes young people 10 -25 Peak incidence of onset (years) 25 -35
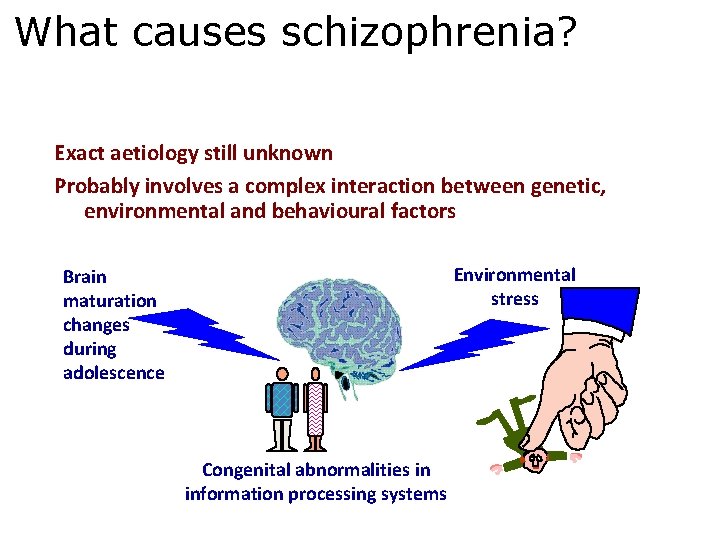
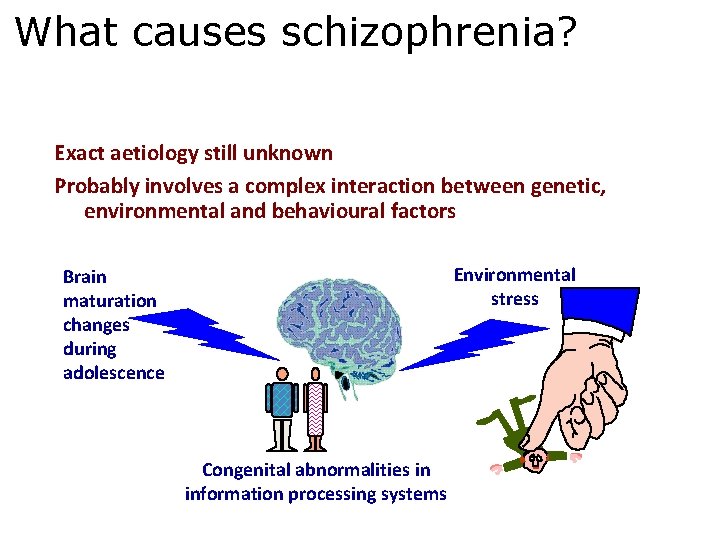
What causes schizophrenia? Exact aetiology still unknown Probably involves a complex interaction between genetic, environmental and behavioural factors Environmental stress Brain maturation changes during adolescence Congenital abnormalities in information processing systems
Etiology v. Genetic factors v. Biochemical factors v. Neuropathology v. Neural circuits v. Brain metabolism v. Psychoneuroendocrinology v. Psychosocial and environmental factors
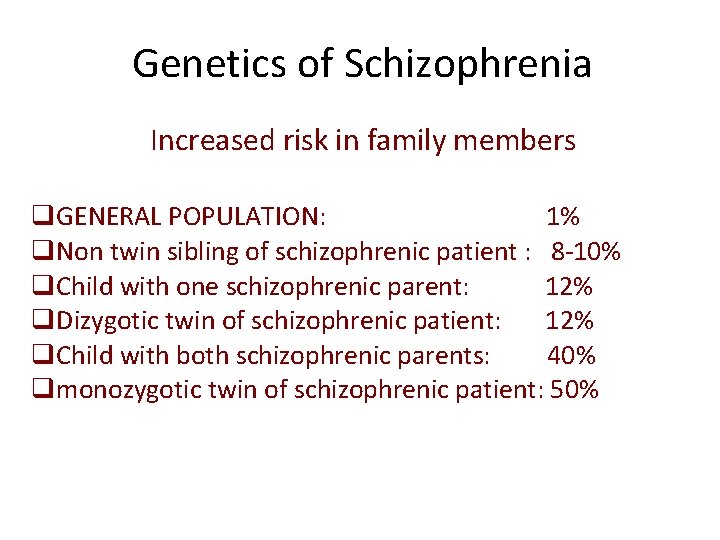
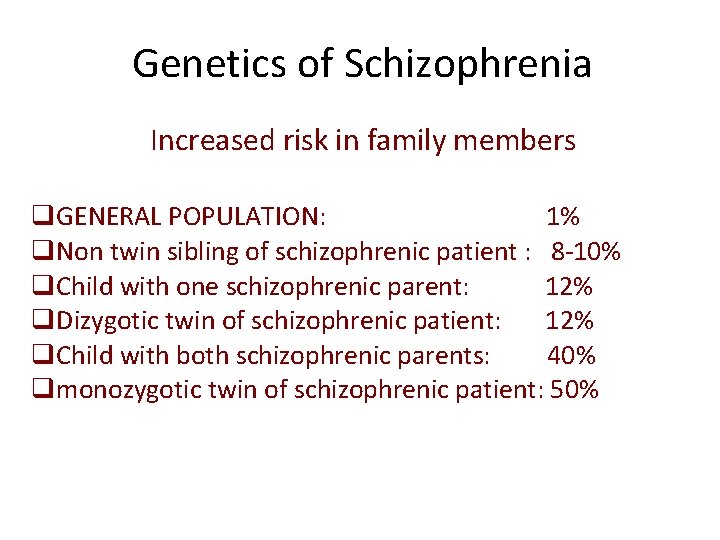
Genetics of Schizophrenia Increased risk in family members q. GENERAL POPULATION: 1% q. Non twin sibling of schizophrenic patient : 8 -10% q. Child with one schizophrenic parent: 12% q. Dizygotic twin of schizophrenic patient: 12% q. Child with both schizophrenic parents: 40% qmonozygotic twin of schizophrenic patient: 50%
Etiology of Schizophrenia - Dopamine Hypothesis • The most influential and plausible are the hypotheses, based on the supposed disorder of neurotransmission in the brain, derived mainly from 1. the effects of antipsychotic drugs that have in common the ability to inhibit the dopaminergic system by blocking action of dopamine in the brain 2. dopamine-releasing drugs (amphetamine, mescaline, diethyl amide of lysergic acid - LSD) that can induce state closely resembling paranoid schizophrenia • Classical dopamine hypothesis of schizophrenia: Psychotic symptoms are related to dopaminergic hyperactivity in the brain. Hyperactivity of dopaminergic systems during schizophrenia is result of increased sensitivity and density of dopamine D 2 receptors in the different parts of the brain.
Other neuro transmitters Serotonin Nor epinephrine GABA
Neuropathology ØLoss of brain volume ØInvolvement of certain brain areas ØExcessive pruning of synapse during development phase ØReduction in cortical volume ØInvolvement of limbic system, thalamus and prefrontal cortex
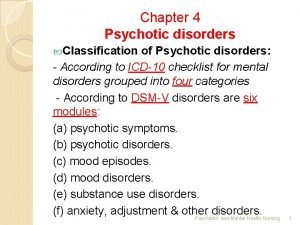
• Clinical Picture Diagnostic manuals: – l. CD-10 (WHO) – DSM-IV (APA) • Clinical picture of schizophrenia is according to l. CD-10, defined from the point of view of the presence and expression of primary and/or secondary symptoms (at present covered by the terms negative and positive symptoms): – the negative symptoms – the positive symptom are characterized by the presence of hallucinations and delusions – the division is not quite strict and lesser or greater mixture of symptoms from these two groups are possible
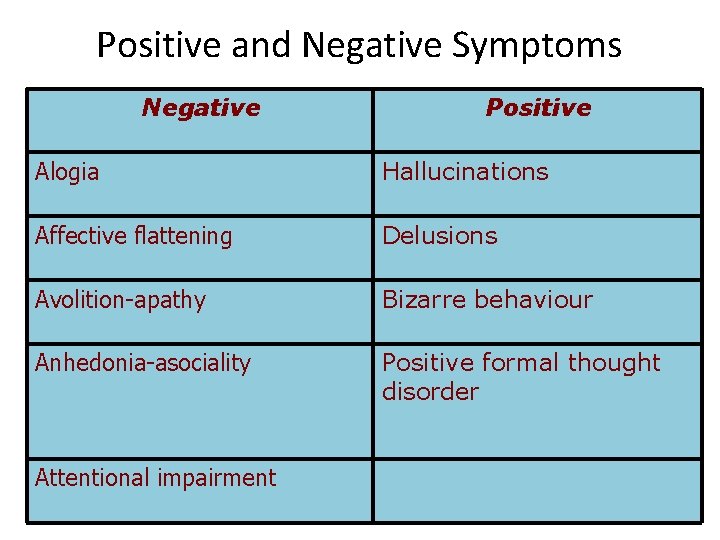
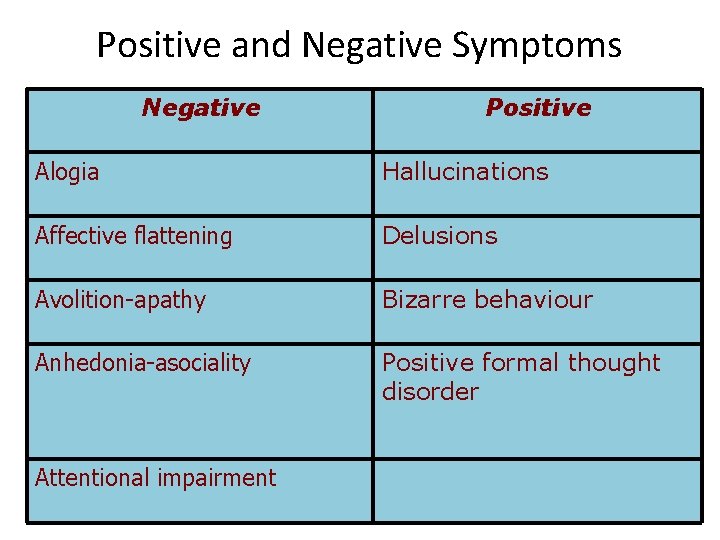
Positive and Negative Symptoms Negative Positive Alogia Hallucinations Affective flattening Delusions Avolition-apathy Bizarre behaviour Anhedonia-asociality Positive formal thought disorder Attentional impairment
Positive symtoms • Those that appear to reflect an excess or distortion of normal functions. Positive symptoms are those that have a positive reaction from some treatment. In other words, positive symptoms respond to treatment.
delusion A fixed, unshakeable belief inappropriate to the person’s socio-economic background and culture
hallucination A perception in the absence of a stimulus may affect any of the senses, but most commonly: Auditory (“voices”) Visual To the patient, these false perceptions are intensely real
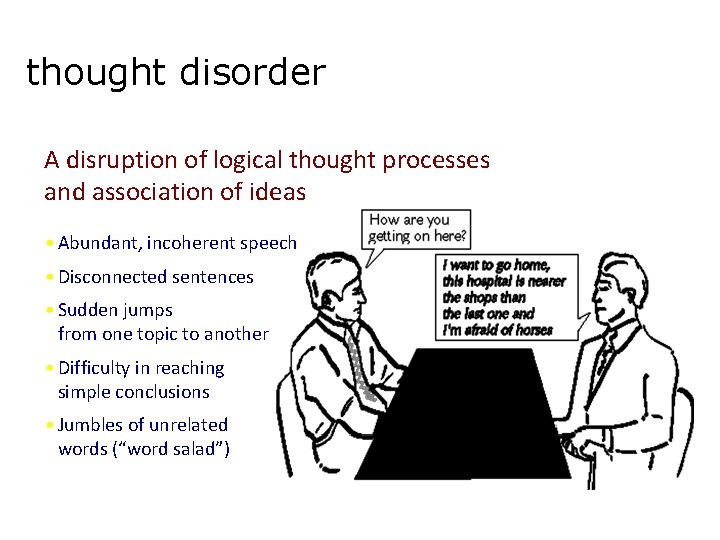
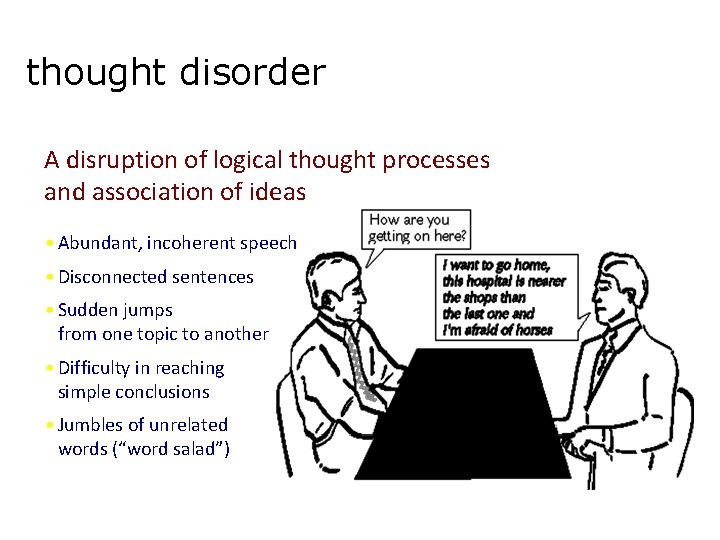
thought disorder A disruption of logical thought processes and association of ideas • Abundant, incoherent speech • Disconnected sentences • Sudden jumps from one topic to another • Difficulty in reaching simple conclusions • Jumbles of unrelated words (“word salad”)
bizarre behaviour Disturbed behavioural organization and control • Highly inappropriate social/sexual behaviour • Repetitive or stereotyped behaviour • Extreme aggressiveness or agitation
• Catatonic behavior. • Marked decrease in reaction to immediate environment, sometimes just unaware of surroundings, rigid or bizarre postures, aimless motor activity.
• • • Inappropriate response to stimuli Unusual motor behavior (pacing, rocking) Depersonalization Derealization Somatic preoccupations
Negative Symptoms • Those that appear to reflect a diminution or loss of normal functions. • May be difficult to evaluate because they are not as grossly abnormal as positive symptoms. • Currently there is no treatment that has a consistent impact on negative symptoms
• Affective flattening • Reduction in the range and intensity of emotional expression, including facial expression, voice tone, eye contact and body language.
• Alogia (poverty of speech) • Lessening of speech fluency and productivity, thought to reflect slowing or blocked thoughts; often manifested as short, empty replies to questions.

• Avolition • The reduction, difficulty or inability to initiate and persist in goal-directed behavior. • Often mistaken for apparent disinterest. No longer interested in going out with friends • No longer interested in activities that the person used to show enthusiasm • No longer interested in anything • Sitting in the house for hours or days doing nothing
anhedonia Loss of capacity to feel joy & pleasure Diminished social/sexual/recreational interests and activities Deterioration of relationships with friends and colleagues Difficulty in achieving intimacy or closeness
attention impairment Inability to focus on tasks or to maintain sustained interest and effort in completing them
Cognitive Symptoms • Difficulties in concentration and memory: – Disorganized thinking – Slow thinking – Difficulty understanding – Poor concentration – Poor memory – Difficulty expressing thoughts – Difficulty integrating thoughts, feelings, behaviors
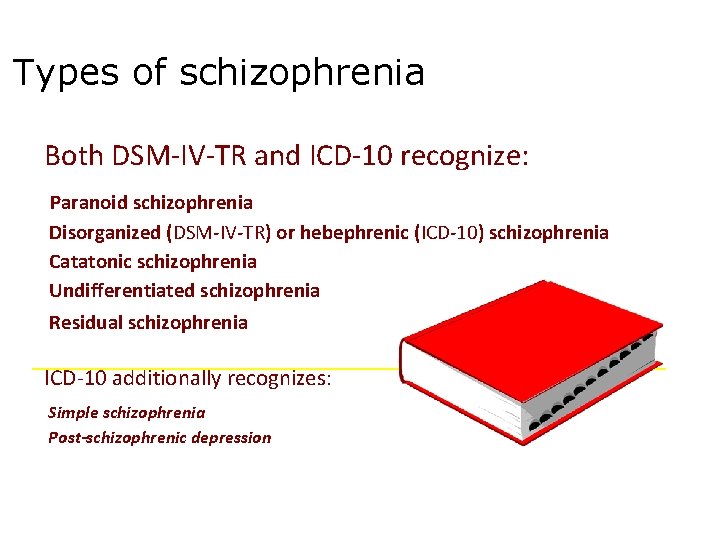
Types of schizophrenia Both DSM-IV-TR and ICD-10 recognize: Paranoid schizophrenia Disorganized (DSM-IV-TR) or hebephrenic (ICD-10) schizophrenia Catatonic schizophrenia Undifferentiated schizophrenia Residual schizophrenia ICD-10 additionally recognizes: Simple schizophrenia Post-schizophrenic depression
The ICD-10 Criteria of Diagnosis
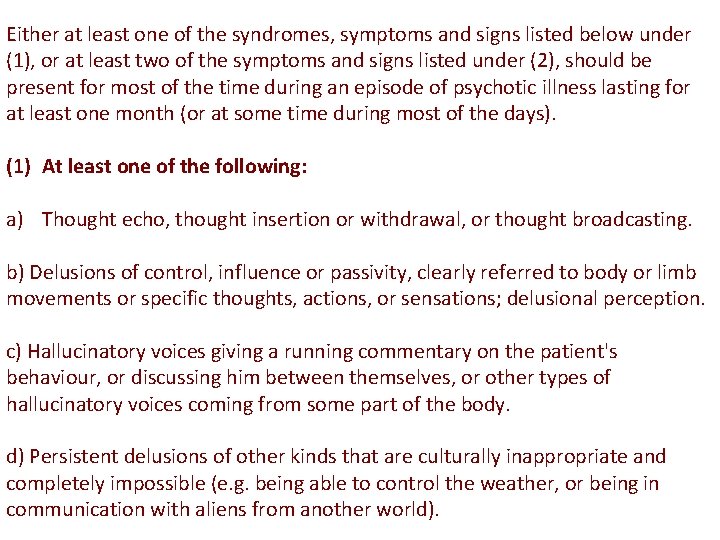
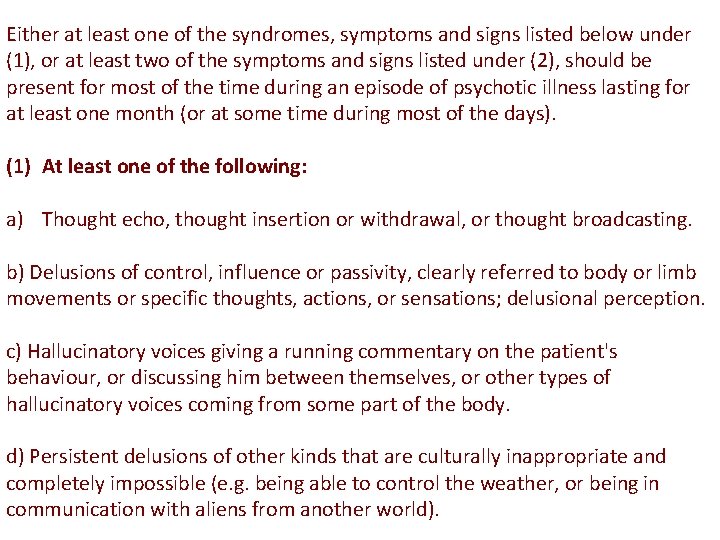
Either at least one of the syndromes, symptoms and signs listed below under (1), or at least two of the symptoms and signs listed under (2), should be present for most of the time during an episode of psychotic illness lasting for at least one month (or at some time during most of the days). (1) At least one of the following: a) Thought echo, thought insertion or withdrawal, or thought broadcasting. b) Delusions of control, influence or passivity, clearly referred to body or limb movements or specific thoughts, actions, or sensations; delusional perception. c) Hallucinatory voices giving a running commentary on the patient's behaviour, or discussing him between themselves, or other types of hallucinatory voices coming from some part of the body. d) Persistent delusions of other kinds that are culturally inappropriate and completely impossible (e. g. being able to control the weather, or being in communication with aliens from another world).
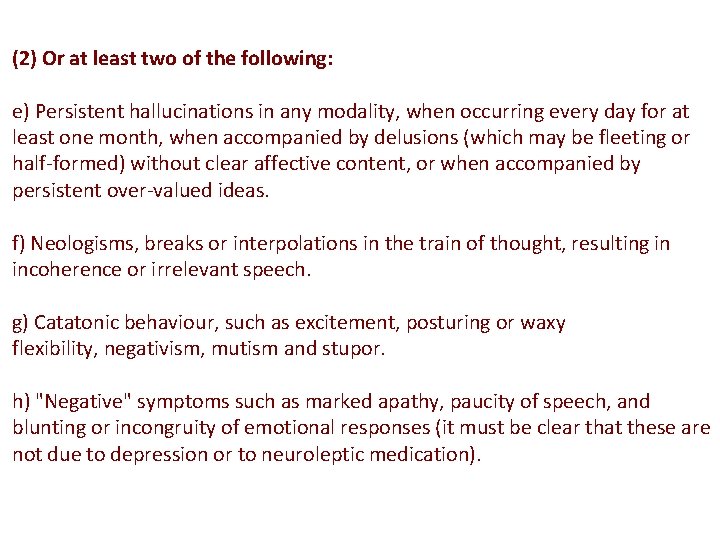
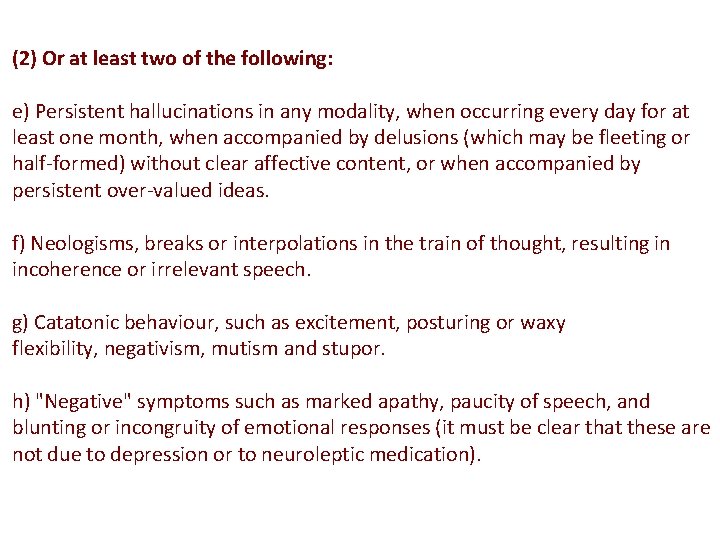
(2) Or at least two of the following: e) Persistent hallucinations in any modality, when occurring every day for at least one month, when accompanied by delusions (which may be fleeting or half-formed) without clear affective content, or when accompanied by persistent over-valued ideas. f) Neologisms, breaks or interpolations in the train of thought, resulting in incoherence or irrelevant speech. g) Catatonic behaviour, such as excitement, posturing or waxy flexibility, negativism, mutism and stupor. h) "Negative" symptoms such as marked apathy, paucity of speech, and blunting or incongruity of emotional responses (it must be clear that these are not due to depression or to neuroleptic medication).
G 2. Most commonly used exclusion criteria: If the patient also meets criteria for manic episode (F 30) or depressive episode (F 32), the criteria listed under G 1. 1 and G 1. 2 above must have been met before the disturbance of mood developed. G 3. The disorder is not attributable to organic brain disease (in the sense of F 0), or to alcohol- or drug-related intoxication, dependence or withdrawal
![COND C hallucinated voices commenting permanently the behavior of the patient or they talk COND C] hallucinated voices, commenting permanently the behavior of the patient or they talk](https://slidetodoc.com/presentation_image_h2/3f60cd5c9774afeb16f8ebc2986a80ba/image-37.jpg)
COND C] hallucinated voices, commenting permanently the behavior of the patient or they talk about him between themselves, or the other types of hallucinatory voices, coming from different parts of body. D] permanent delusions of different kind, which are inappropriate and unacceptable in given culture
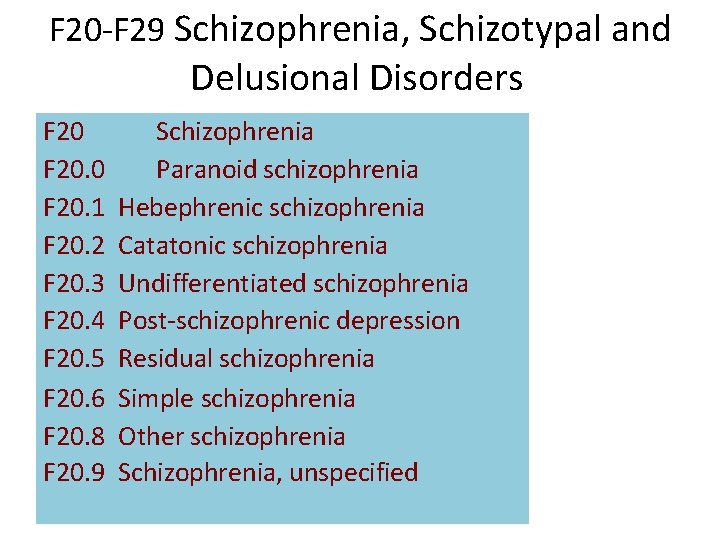
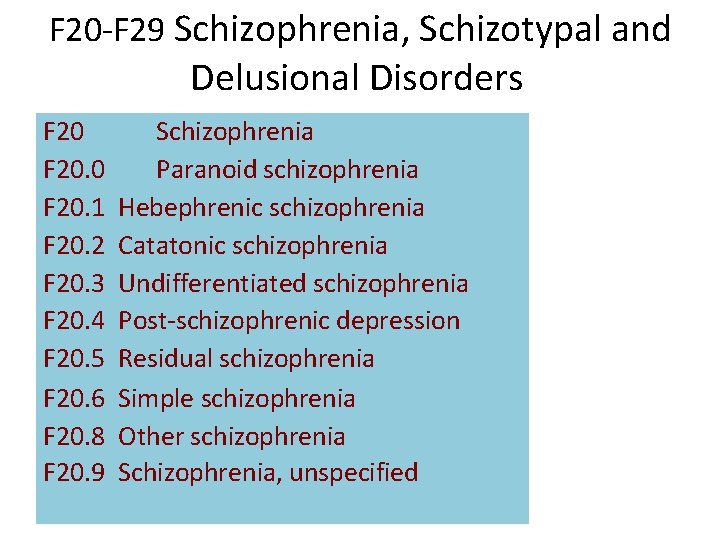
F 20 -F 29 Schizophrenia, Schizotypal and Delusional Disorders F 20. 0 F 20. 1 F 20. 2 F 20. 3 F 20. 4 F 20. 5 F 20. 6 F 20. 8 F 20. 9 Schizophrenia Paranoid schizophrenia Hebephrenic schizophrenia Catatonic schizophrenia Undifferentiated schizophrenia Post-schizophrenic depression Residual schizophrenia Simple schizophrenia Other schizophrenia Schizophrenia, unspecified
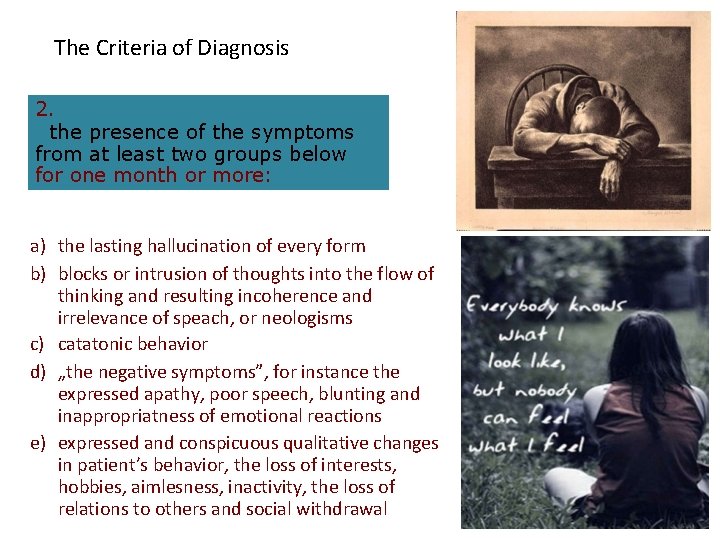
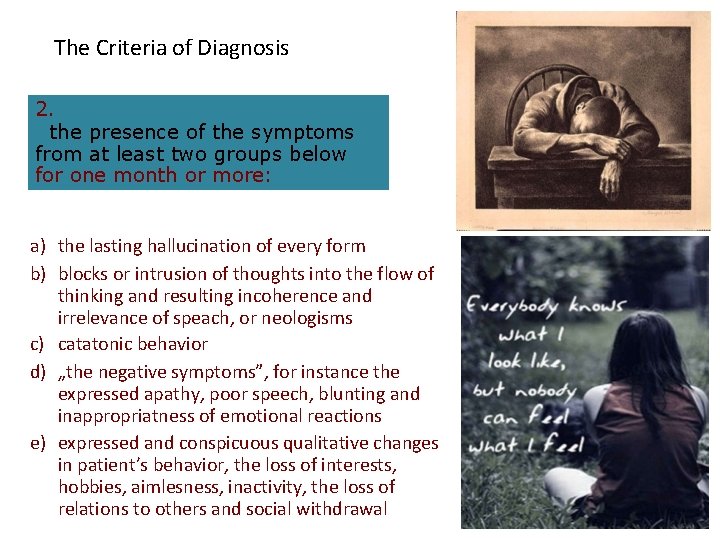
The Criteria of Diagnosis 2. the presence of the symptoms from at least two groups below for one month or more: a) the lasting hallucination of every form b) blocks or intrusion of thoughts into the flow of thinking and resulting incoherence and irrelevance of speach, or neologisms c) catatonic behavior d) „the negative symptoms”, for instance the expressed apathy, poor speech, blunting and inappropriatness of emotional reactions e) expressed and conspicuous qualitative changes in patient’s behavior, the loss of interests, hobbies, aimlesness, inactivity, the loss of relations to others and social withdrawal
• Diagnosis of acute schizophorm disorder (F 23. 2) – if the conditions for diagnosis of schizophrenia are fulfilled, but lasting less than one month • Diagnosis of schizoaffective disorder (F 25) - if the schizophrenic and affective symptoms are developing together at the same time
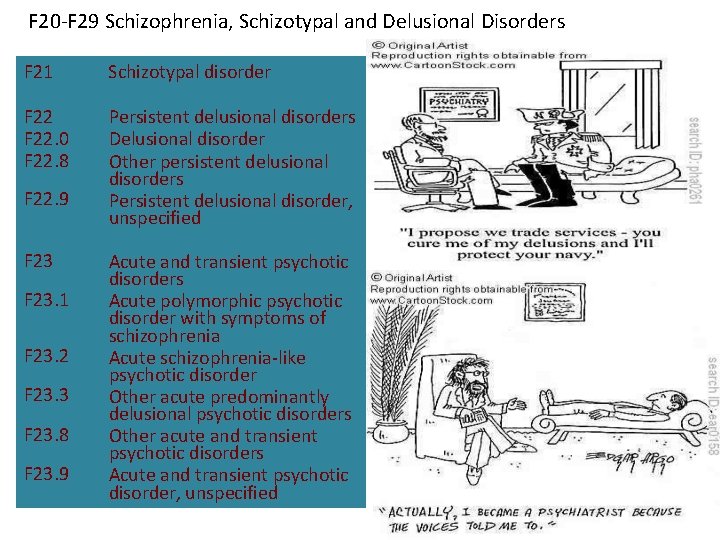
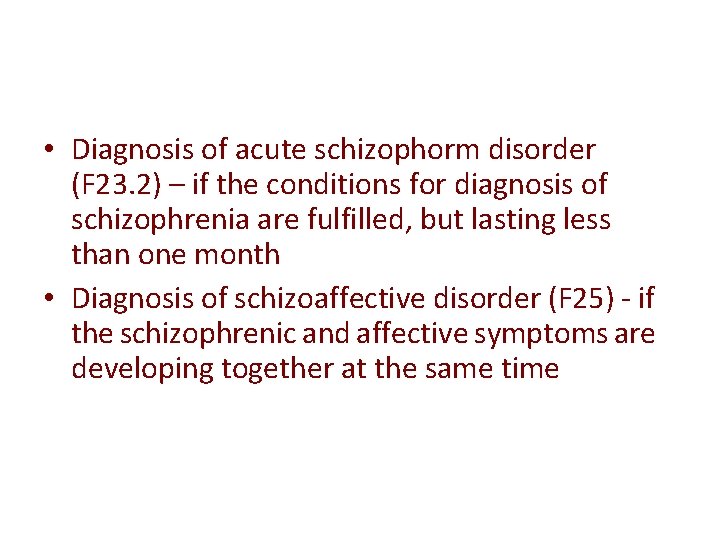
F 20 -F 29 Schizophrenia, Schizotypal and Delusional Disorders F 21 Schizotypal disorder F 22. 0 F 22. 8 Persistent delusional disorders Delusional disorder Other persistent delusional disorders Persistent delusional disorder, unspecified F 22. 9 F 23. 1 F 23. 2 F 23. 3 F 23. 8 F 23. 9 Acute and transient psychotic disorders Acute polymorphic psychotic disorder with symptoms of schizophrenia Acute schizophrenia-like psychotic disorder Other acute predominantly delusional psychotic disorders Other acute and transient psychotic disorders Acute and transient psychotic disorder, unspecified
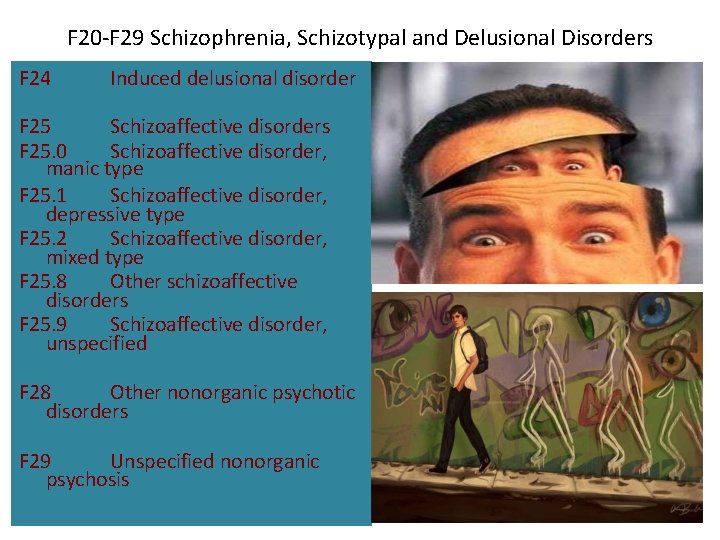
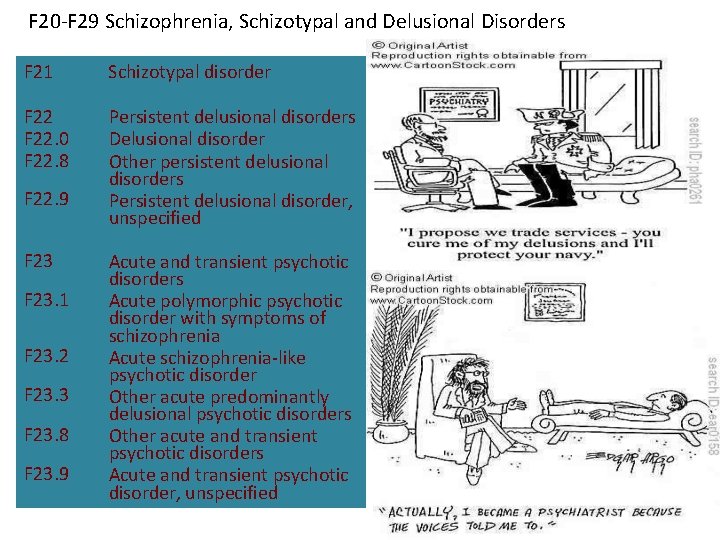
F 20 -F 29 Schizophrenia, Schizotypal and Delusional Disorders F 24 Induced delusional disorder F 25 Schizoaffective disorders F 25. 0 Schizoaffective disorder, manic type F 25. 1 Schizoaffective disorder, depressive type F 25. 2 Schizoaffective disorder, mixed type F 25. 8 Other schizoaffective disorders F 25. 9 Schizoaffective disorder, unspecified F 28 Other nonorganic psychotic disorders F 29 Unspecified nonorganic psychosis
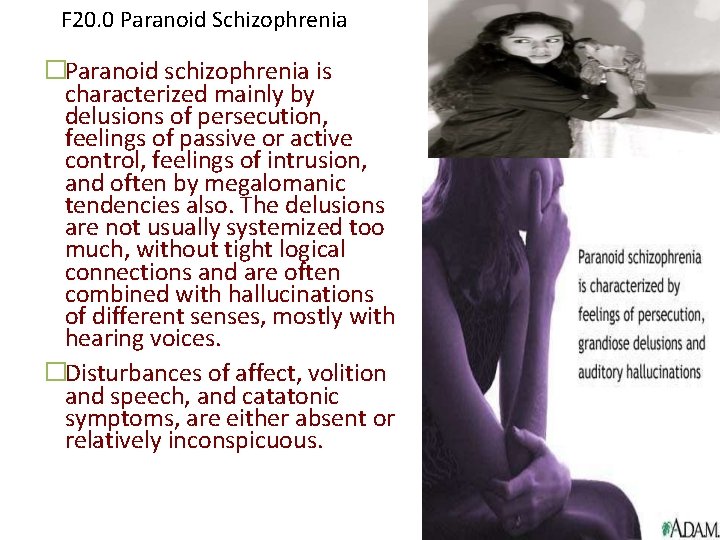
F 20. 0 Paranoid Schizophrenia �Paranoid schizophrenia is characterized mainly by delusions of persecution, feelings of passive or active control, feelings of intrusion, and often by megalomanic tendencies also. The delusions are not usually systemized too much, without tight logical connections and are often combined with hallucinations of different senses, mostly with hearing voices. �Disturbances of affect, volition and speech, and catatonic symptoms, are either absent or relatively inconspicuous.
F 20. 1 Hebephrenic Schizophrenia • disorganized thinking with blunted and inappropriate emotions. • adolescent age, the behavior is often bizarre. • There could appear mannerisms, grimacing, inappropriate laugh and joking, pseudophilosophical brooding and sudden impulsive reactions without external stimulation. There is a tendency to social isolation. • Usually the prognosis is poor because of the rapid development of "negative" symptoms, particularly flattening of affect and loss of volition. Hebephrenia should normally be diagnosed only in adolescents or young adults. • Denoted also as disorganized schizophrenia
F 20. 2 Catatonic Schizophrenia • Catatonic schizophrenia is characterized mainly by motoric activity, which might be strongly increased (hypekinesis) or decreased (stupor), or automatic obedience and negativism. • We recognize two forms:
COND – productive form — which shows catatonic excitement, extreme and often aggressive activity. Treatment by neuroleptics or by electroconvulsive therapy. – stuporose form — characterized by general inhibition of patient’s behavior or at least by retardation and slowness, followed often by mutism, negativism, fexibilitas cerea or by stupor. The consciousness is not absent.
F 20. 3 Undifferentiated Schizophrenia • Psychotic conditions meeting the general diagnostic criteria for schizophrenia but not conforming to any of the subtypes in F 20. 0 -F 20. 2, or exhibiting the features of more than one of them without a clear predominance of a particular set of diagnostic characteristics. • This subgroup represents also the former diagnosis of atypical schizophrenia.
F 20. 4 Postschizophrenic Depression • A depressive episode, which may be prolonged, arising in the aftermath of a schizophrenic illness. Some schizophrenic symptoms, either „positive“ or „negative“, must still be present but they no longer dominate the clinical picture. • These depressive states are associated with an increased risk of suicide.
F 20. 5 Residual Schizophrenia • A chronic stage in the development of schizophrenia with clear succession from the initial stage with one or more episodes characterized by general criteria of schizophrenia to the late stage with long-lasting negative symptoms and deterioration (not necessarily irreversible).
F 20. 6 Simple Schizophrenia • Simple schizophrenia is characterized by early and slowly developing initial stage with growing social isolation, withdrawal, small activity, passivity, avolition and dependence on the others. • The patients are indifferent, without any initiative and volition. There is not expressed the presence of hallucinations and delusions.
F 21 Schizotypal disorder • According to l. CD-10 this disorder is characterized by eccentric behavior and by deviations of thinking and affectivity, which are similar to that occurring in schizophrenia, but without psychotic features and expressed symptoms of schizophrenia of any type.
F 22 Persistent Delusional Disorders • Includes a variety of disorders in which longstanding delusions constitute the only, or the most conspicuous, clinical characteristic and which cannot be classified as organic, schizophrenic or affective. • Their origin is probably heterogeneous, but it seems, that there is some relation to schizophrenia.
F 22. 0 Delusional Disorder • A disorder characterized by the development of one delusion or of the group of similar related delusions, which are persisting unusually long, very often for the whole life. • Other psychopathological symptoms — hallucinations, intrusion of thoughts etc. are not present and are excluding this diagnosis. • It begins usually in the middle age.
F 23 Acute and Transient Psychotic Disorders • The criteria should be the following features: – acute beginning (to two weeks) – presence of typical symptoms (quickly changing “polymorphic symptoms”) – presence of typical schizophrenic symptoms. • Complete recovery usually occurs within a few months, often within a few weeks or even days. • The disorder may or may not be associated with acute stress, defined as usually stressful events preceding the onset by one to two weeks.
F 24 Induced Delusional Disorder �A delusional disorder shared by two or more people with close emotional links. Only one of the people suffers from a genuine psychotic disorder; the delusions are induced in the other(s) and usually disappear when the people are separated. �The psychotic disorder of the dominant member of this dyad is mainly, but not necessarily, of schizophrenic type. The original delusions of dominant member and his partner are usually chronic, either persecutory or megalomanic.

THANK YOU
 Looseness of association
Looseness of association Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Is schizophrenia on a spectrum
Is schizophrenia on a spectrum Psycopath traits
Psycopath traits Schizophreniform disorder icd-10
Schizophreniform disorder icd-10 Schizophrenia
Schizophrenia Difference between neurotic and psychotic
Difference between neurotic and psychotic Chapter 31 schizophrenia and other psychoses
Chapter 31 schizophrenia and other psychoses Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Hodgkin's lymphoma clinical presentation
Hodgkin's lymphoma clinical presentation Types of embolism
Types of embolism Cll clinical presentation
Cll clinical presentation Itk sisekliinik
Itk sisekliinik Self-initiated other-repair
Self-initiated other-repair Example of mse report
Example of mse report Schizophrenia warning signs
Schizophrenia warning signs Humanistic approach to schizophrenia
Humanistic approach to schizophrenia Schizoaffective disorder
Schizoaffective disorder Akathisea
Akathisea Bleuler 4a
Bleuler 4a Schizophrenia literal meaning
Schizophrenia literal meaning Types of delusions
Types of delusions Thesis statement about schizophrenia
Thesis statement about schizophrenia Types of schizophrenia
Types of schizophrenia Hebephrenic schizophrenia
Hebephrenic schizophrenia Sel tmu
Sel tmu Catatonic behavior example
Catatonic behavior example Loose associations psychology
Loose associations psychology Hebephrenic schizophrenia
Hebephrenic schizophrenia Phases of schizophrenia
Phases of schizophrenia Double bind
Double bind Negative explanatory style
Negative explanatory style Strengths of the psychodynamic approach
Strengths of the psychodynamic approach Schizophrenia meaning
Schizophrenia meaning Loose associations
Loose associations Motivational interviewing schizophrenia
Motivational interviewing schizophrenia Axis 1-5 mental health
Axis 1-5 mental health Module 68 schizophrenia
Module 68 schizophrenia Prevalence of schizophrenia
Prevalence of schizophrenia Dr tachere
Dr tachere Dsm 5 vs dsm 4
Dsm 5 vs dsm 4 Cognitive explanations of schizophrenia
Cognitive explanations of schizophrenia Example of loose associations in schizophrenia
Example of loose associations in schizophrenia Schizophrenia def
Schizophrenia def First-line treatment for schizophrenia
First-line treatment for schizophrenia Timmy turner on drugs
Timmy turner on drugs Undifferentiated schizophrenia
Undifferentiated schizophrenia Schizophrenia def
Schizophrenia def Schizophrenia literally means
Schizophrenia literally means Loose associations
Loose associations Dopamine hypothesis psychosis
Dopamine hypothesis psychosis What is schizophrenia
What is schizophrenia What causes schizophrenia
What causes schizophrenia Avolition definition schizophrenia
Avolition definition schizophrenia We are done quotes
We are done quotes Biological explanations of schizophrenia
Biological explanations of schizophrenia