Schizophrenia and Other Psychotic Disorders Chapter 14 Schizophrenia






- Slides: 27
Schizophrenia and Other Psychotic Disorders Chapter 14
• • • Schizophrenia http: //www. youtube. com/watch? v=H_j. Yq. SA_f. Jk Schizophrenia Part 1 - ABC 20/20 coverage http: //www. youtube. com/watch? v=mo. P_e-gx 5 hk Schizophrenia Part 2 - ABC 20/20 coverage http: //www. youtube. com/watch? v=QPXkw. YM 9 G-s What is Schizophrenia? (Schizophrenia #1) http: //www. youtube. com/watch? v=Kno. Tw. OUb 0 a. Q Diagnosing and Treating Schizophrenia (Schizophrenia #2) http: //www. youtube. com/watch? v=Wwl. M 1 px. Iba. I
Introduction • The word schizophrenia is derived from the Greek words skhizo (split) and phren (mind). • Schizophrenia is probably caused by a combination of factors, including: • Of all mental illnesses, schizophrenia probably causes more – Lengthy hospitalizations – Chaos in family life – Exorbitant costs to people and governments – Fears
Nature of the Disorder • Schizophrenia disturbs Thought processes, Perception and Affect • With schizophrenia, there is a severe deterioration of social and occupational functioning * In the United States, the lifetime prevalence of schizophrenia is about 1 percent.
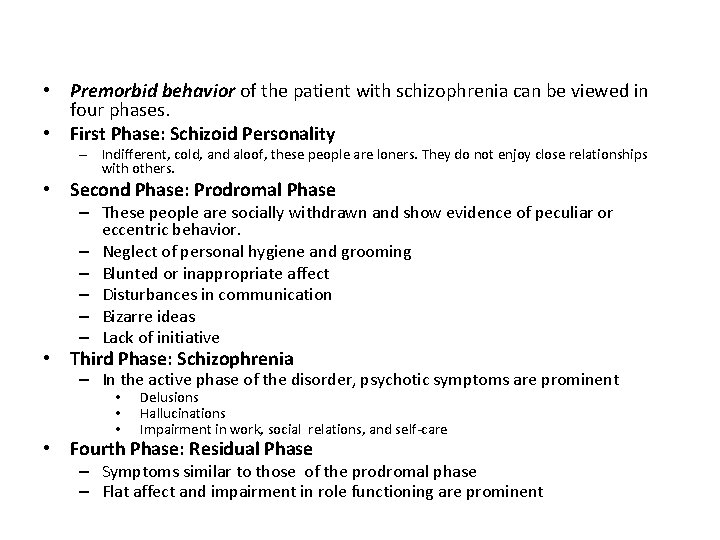
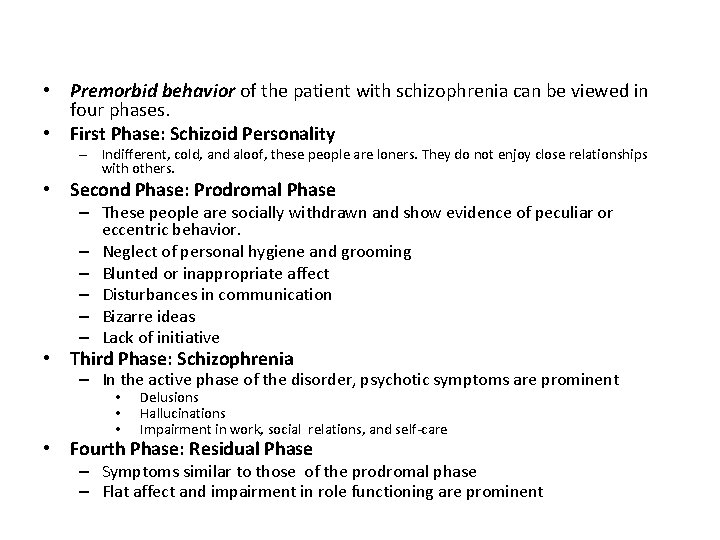
• Premorbid behavior of the patient with schizophrenia can be viewed in four phases. • First Phase: Schizoid Personality – Indifferent, cold, and aloof, these people are loners. They do not enjoy close relationships with others. • Second Phase: Prodromal Phase – These people are socially withdrawn and show evidence of peculiar or eccentric behavior. – Neglect of personal hygiene and grooming – Blunted or inappropriate affect – Disturbances in communication – Bizarre ideas – Lack of initiative • Third Phase: Schizophrenia – In the active phase of the disorder, psychotic symptoms are prominent • • • Delusions Hallucinations Impairment in work, social relations, and self-care • Fourth Phase: Residual Phase – Symptoms similar to those of the prodromal phase – Flat affect and impairment in role functioning are prominent
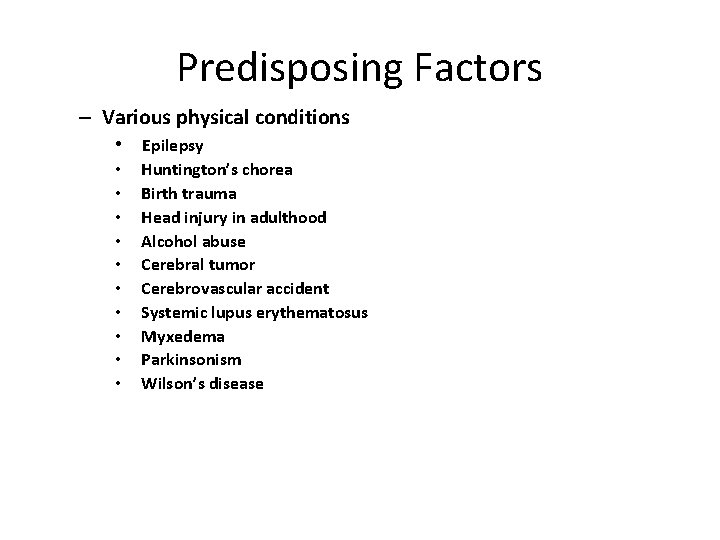
Predisposing Factors – Various physical conditions • Epilepsy • • • Huntington’s chorea Birth trauma Head injury in adulthood Alcohol abuse Cerebral tumor Cerebrovascular accident Systemic lupus erythematosus Myxedema Parkinsonism Wilson’s disease
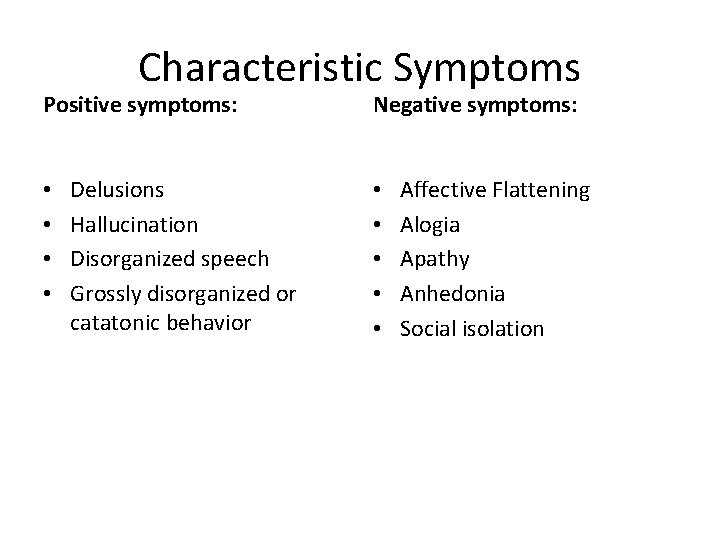
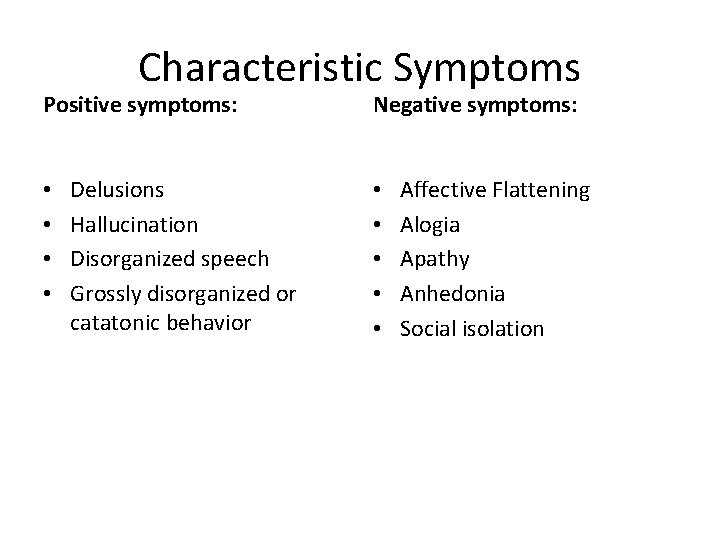
Characteristic Symptoms Positive symptoms: • • Delusions Hallucination Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms: • • • Affective Flattening Alogia Apathy Anhedonia Social isolation
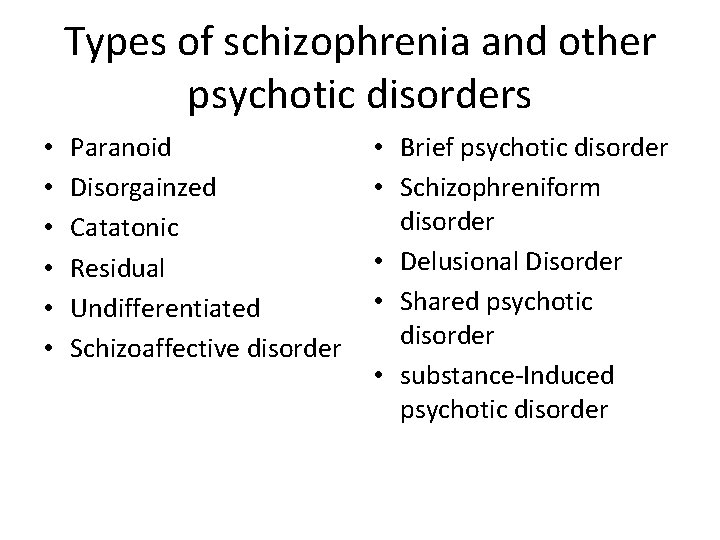
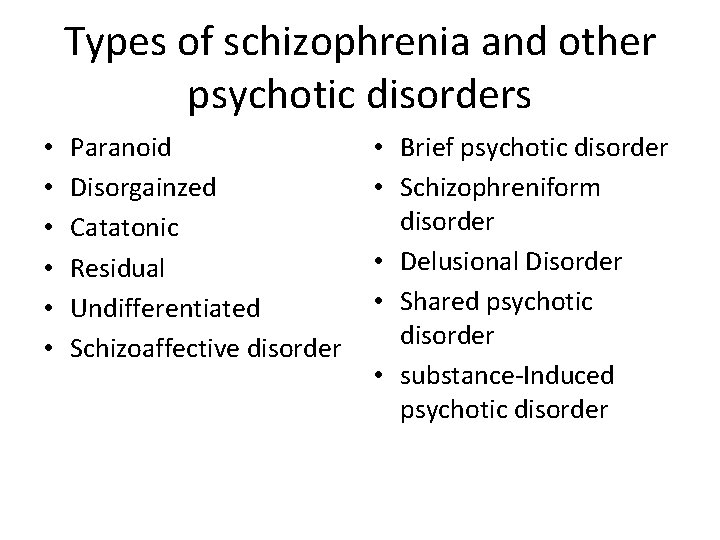
Types of schizophrenia and other psychotic disorders • • • Paranoid Disorgainzed Catatonic Residual Undifferentiated Schizoaffective disorder • Brief psychotic disorder • Schizophreniform disorder • Delusional Disorder • Shared psychotic disorder • substance-Induced psychotic disorder
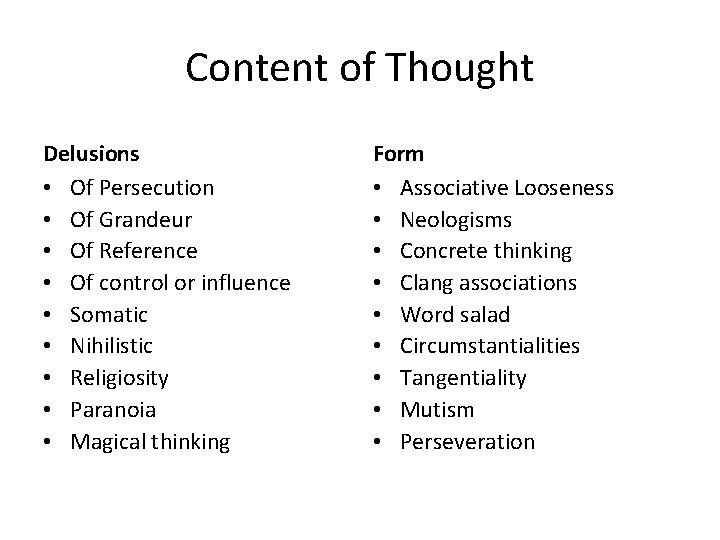
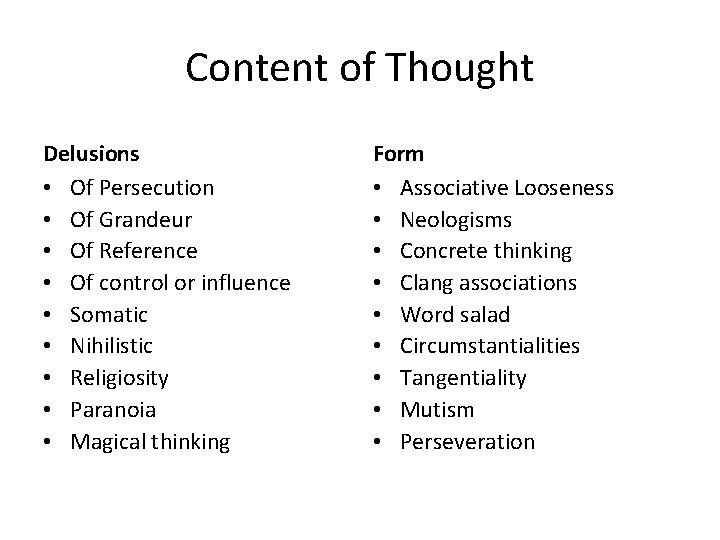
Content of Thought Delusions • Of Persecution • Of Grandeur • Of Reference • Of control or influence • Somatic • Nihilistic • Religiosity • Paranoia • Magical thinking Form • Associative Looseness • Neologisms • Concrete thinking • Clang associations • Word salad • Circumstantialities • Tangentiality • Mutism • Perseveration

Perception • • • Hallucination Auditory Visual Tactile Olfactory Affects • Inappropriate affect • Bland or flat affect • Apathy
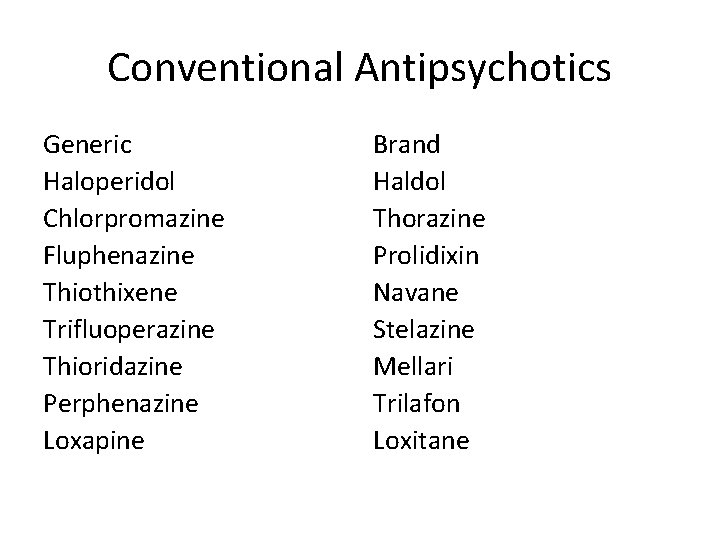
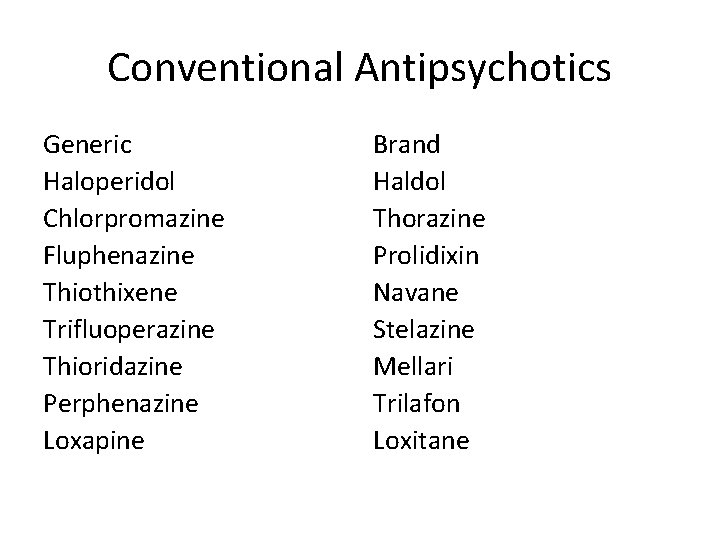
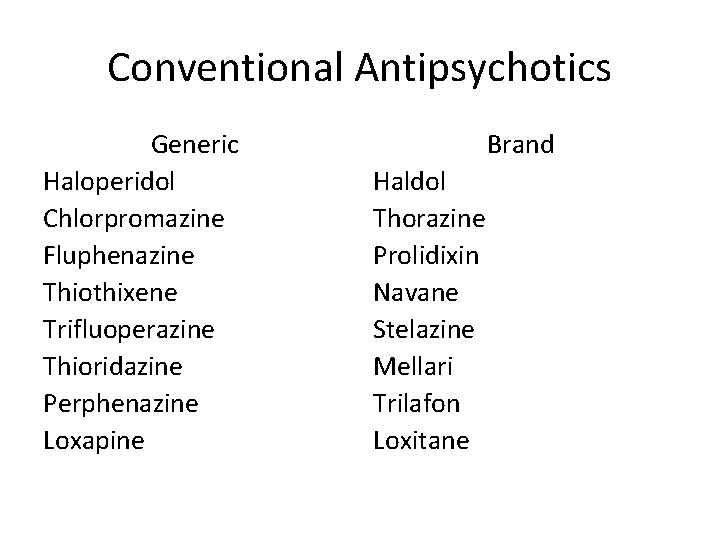
Conventional Antipsychotics Generic Haloperidol Chlorpromazine Fluphenazine Thiothixene Trifluoperazine Thioridazine Perphenazine Loxapine Brand Haldol Thorazine Prolidixin Navane Stelazine Mellari Trilafon Loxitane
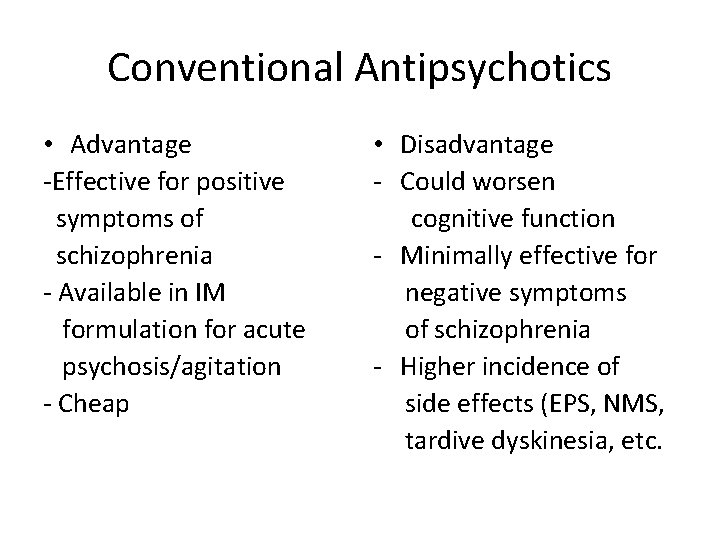
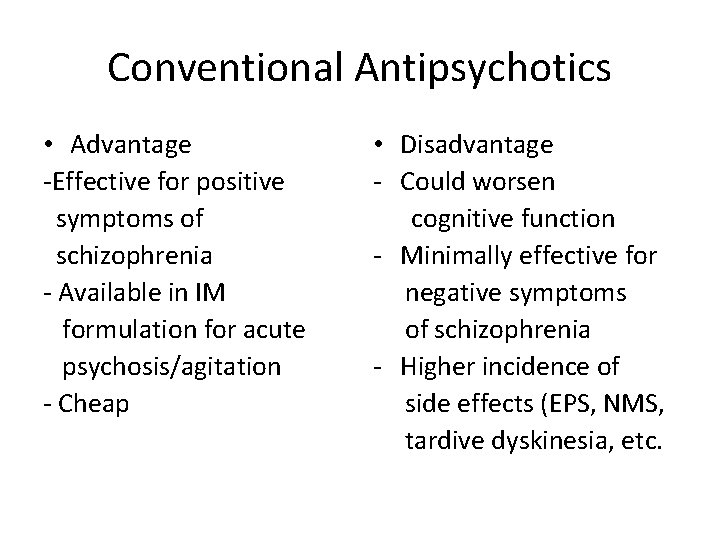
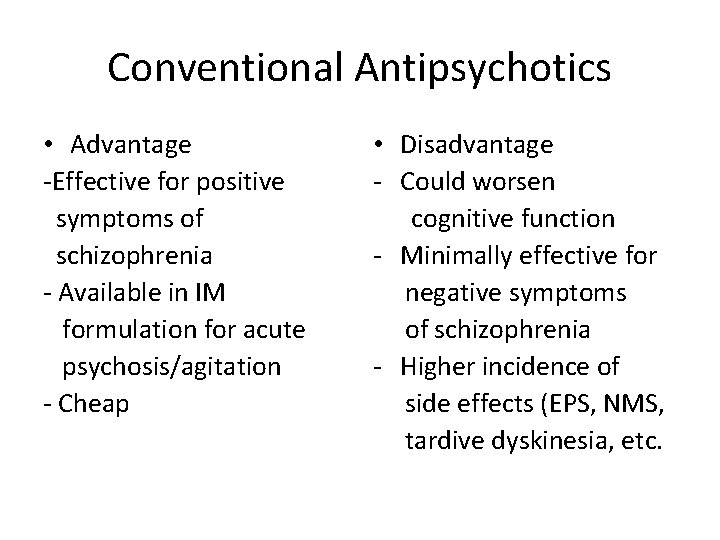
Conventional Antipsychotics • Advantage -Effective for positive symptoms of schizophrenia - Available in IM formulation for acute psychosis/agitation - Cheap • Disadvantage - Could worsen cognitive function - Minimally effective for negative symptoms of schizophrenia - Higher incidence of side effects (EPS, NMS, tardive dyskinesia, etc.
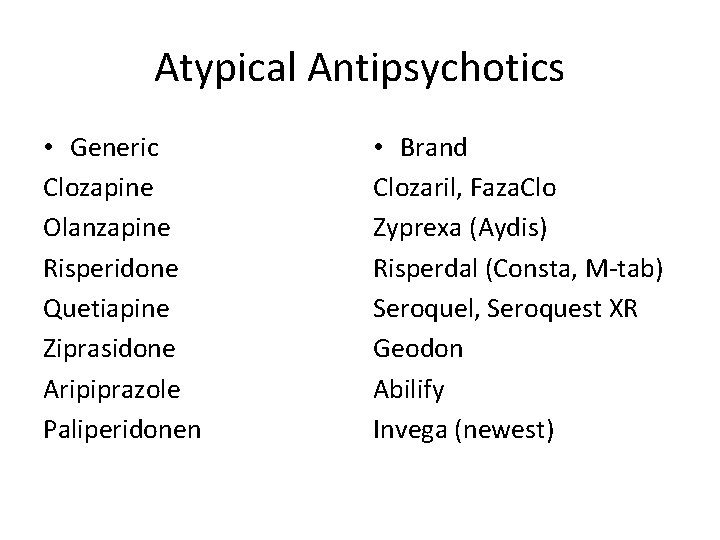
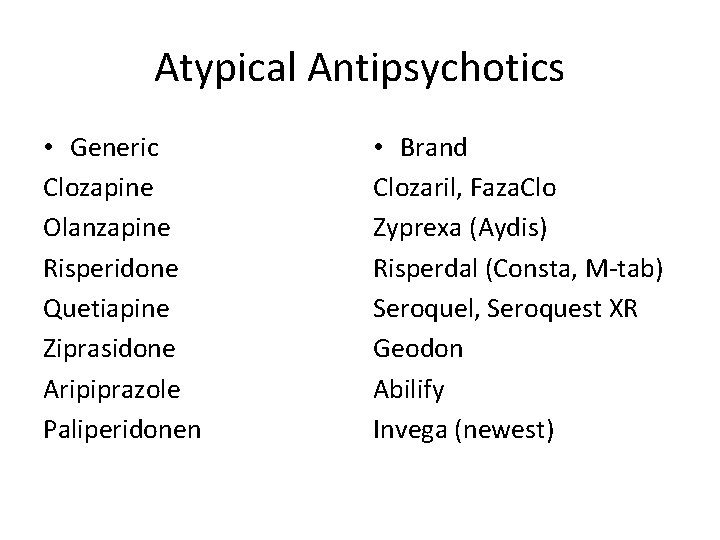
Atypical Antipsychotics • Generic Clozapine Olanzapine Risperidone Quetiapine Ziprasidone Aripiprazole Paliperidonen • Brand Clozaril, Faza. Clo Zyprexa (Aydis) Risperdal (Consta, M-tab) Seroquel, Seroquest XR Geodon Abilify Invega (newest)

Atypical Antipsychotics • Advantage - Effective for positive of symptoms of schizophrenia - May improve negative symptoms of schizophrenia - Lower incidence of side effects compared to conventional antipsychotics • Disadvantage - Higher incidence of weight gain - Higher incidence of diabets - Expensive
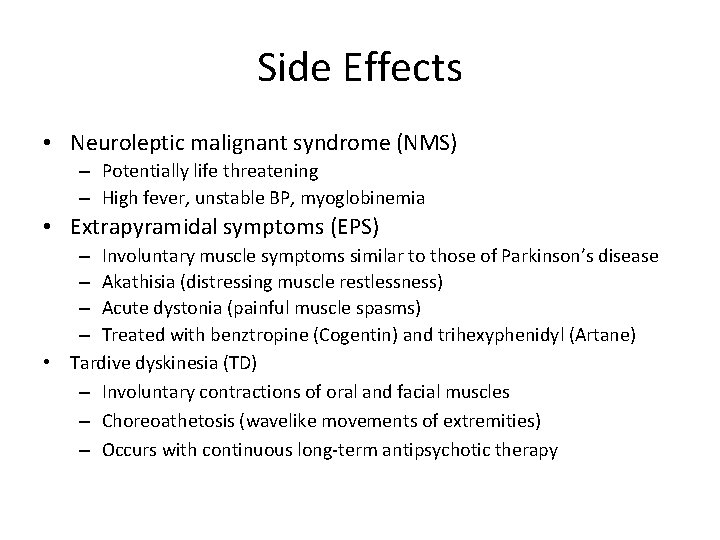
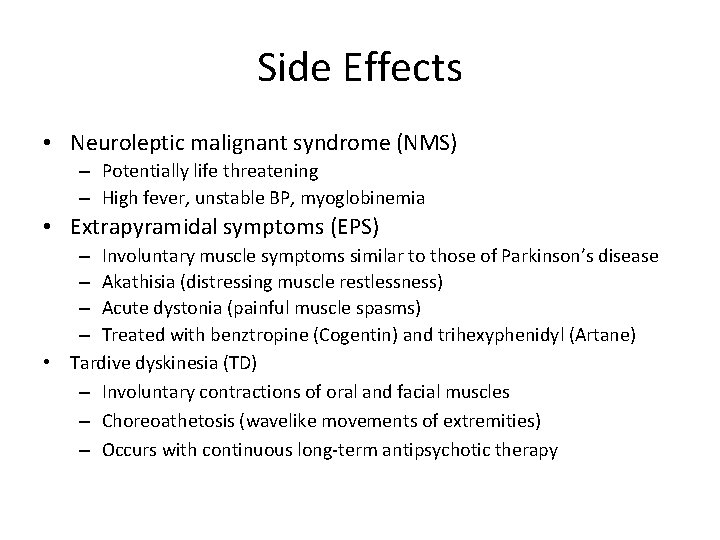
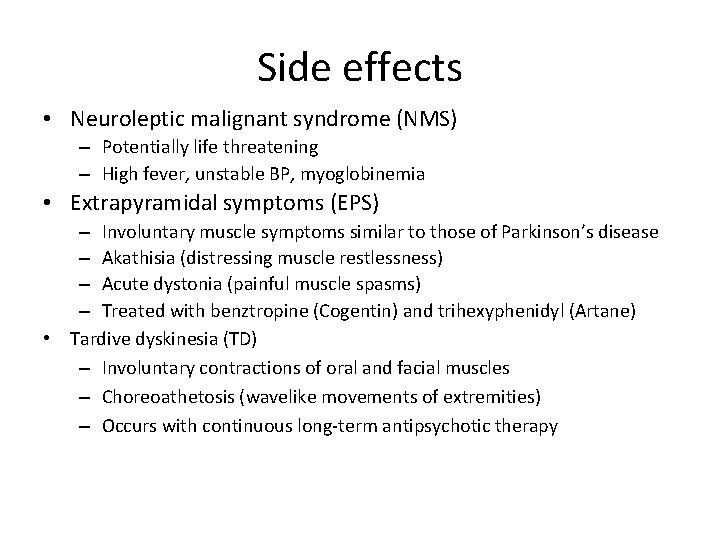
Side Effects • Neuroleptic malignant syndrome (NMS) – Potentially life threatening – High fever, unstable BP, myoglobinemia • Extrapyramidal symptoms (EPS) – Involuntary muscle symptoms similar to those of Parkinson’s disease – Akathisia (distressing muscle restlessness) – Acute dystonia (painful muscle spasms) – Treated with benztropine (Cogentin) and trihexyphenidyl (Artane) • Tardive dyskinesia (TD) – Involuntary contractions of oral and facial muscles – Choreoathetosis (wavelike movements of extremities) – Occurs with continuous long-term antipsychotic therapy
Nursing Process • • • Nursing Assessment Nursing Diagnosis Related to Evidenced by Interventions Education
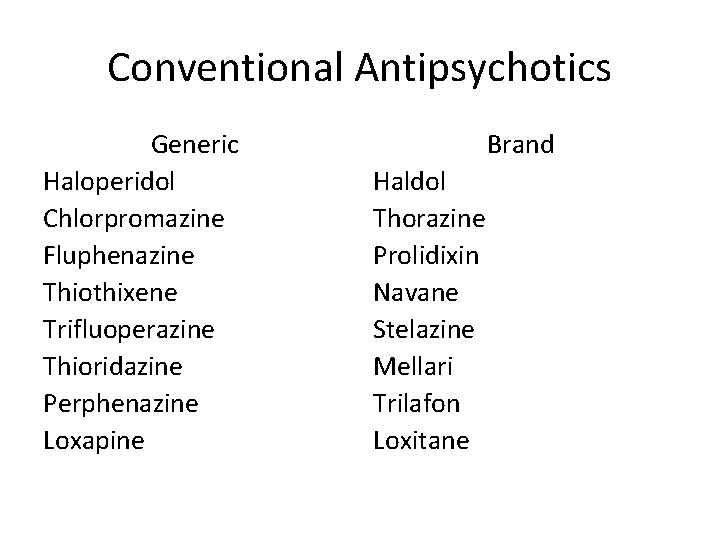
Conventional Antipsychotics Generic Haloperidol Chlorpromazine Fluphenazine Thiothixene Trifluoperazine Thioridazine Perphenazine Loxapine Brand Haldol Thorazine Prolidixin Navane Stelazine Mellari Trilafon Loxitane
Conventional Antipsychotics • Advantage -Effective for positive symptoms of schizophrenia - Available in IM formulation for acute psychosis/agitation - Cheap • Disadvantage - Could worsen cognitive function - Minimally effective for negative symptoms of schizophrenia - Higher incidence of side effects (EPS, NMS, tardive dyskinesia, etc.

Atypical Antipsychotics • Generic Clozapine Olanzapine Risperidone Quetiapine Ziprasidone Aripiprazole Paliperidonen • Brand Clozaril, Faza. Clo Zyprexa (Aydis) Risperdal (Consta, M-tab) Seroquel, Seroquest XR Geodon Abilify Invega (newest)

Atypical Antipsychotics • Advantage - Effective for positive of symptoms of schizophrenia - May improve negative symptoms of schizophrenia - Lower incidence of side effects compared to conventional antipsychotics • Disadvantage - Higher incidence of weight gain - Higher incidence of diabets - Expensive
Antipsychotics Background Assessment Data • Indications: Treatment of acute and chronic psychoses; selected agents are also used as antiemetics in the treatment of intractable hiccoughs and for control of tics and vocal utterances in Tourette’s disorder • Actions: Unknown; thought to block postsynaptic dopamine receptors in the basal ganglia, hypothalamus, limbic system, brainstem, and medulla. Newer antipsychotics may block action on receptors specific to dopamine, serotonin, and other neurotransmitters.
• Contraindications/precautions – Contraindicated with known hypersensitivity; with CNS depression; when blood dyscrasias exist; in clients with Parkinson’s disease; or those with liver, renal, or cardiac insufficiency – Caution with elderly, debilitated, or diabetic clients or those with respiratory insufficiency, prostatic hypertrophy, or intestinal obstructio • Interactions – Additive anticholinergic effects with other drugs that produce these properties – Additive hypotensive effects with beta-blockers – Decreased absorption of antipsychotics with antacids and antidiarrheals – Decreased effectiveness of antipsychotics with barbiturates – Additive CNS depression with alcohol, antihistamines, antidepressants, sedative-hypnotics, and anxiolytics
Nursing Diagnosis • • Risk for other-directed violence Risk for injury Risk for activity intolerance Noncompliance
Neuroleptic Malignant Syndrome • Signs and symptoms of NMS are: muscle rigidity, hyperthermia, decreased ventilation, cardiovascular collapse, and an elevate CPK
Side effects • Neuroleptic malignant syndrome (NMS) – Potentially life threatening – High fever, unstable BP, myoglobinemia • Extrapyramidal symptoms (EPS) – Involuntary muscle symptoms similar to those of Parkinson’s disease – Akathisia (distressing muscle restlessness) – Acute dystonia (painful muscle spasms) – Treated with benztropine (Cogentin) and trihexyphenidyl (Artane) • Tardive dyskinesia (TD) – Involuntary contractions of oral and facial muscles – Choreoathetosis (wavelike movements of extremities) – Occurs with continuous long-term antipsychotic therapy

A 29 year old woman is being discharged in 2 days form the hospital after her first psychotic break (paranoid schizophrenia). She is recently divorced and has been working as a legal secretary, although her work had become erratic, and her suspicious behavior was calling attention to herself at work. She will be discharged in her mother’s care until she is able to resume working. Her mother is overwhelmed and asked the nurse how she is going to cope. “She has become so distant and she always takes thing the wrong way. I can hardly say anything to her with her misconstruing everything. She is very mad at me because I called 911 and had her admitted after she told me she was going to get justice back in the world by blowing up evil forces that have been haunting her life and then proceeded to try to run over her ex-husband, thinking he was the devil. She told me there is nothing wrong with her and I am concerned she won’t take her medication once she is discharge.

1. What are some of the priority concern that nurse could address in the hospital setting before she is discharge? 2. How would you explain to the mother some of the symptoms that she is experience in? What suggestion could you give her to handle some of the immediate concerns? 3. What issues could you bring up to the staff about her medication compliance? What would be some ways to deal with this issue? 4. What do you think of the prognosis for her? Support your hypothesis with data regarding influences on the course of schizophrenia.
 Associative looseness
Associative looseness Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Is schizophrenia on a spectrum
Is schizophrenia on a spectrum Chapter 31 schizophrenia and other psychoses
Chapter 31 schizophrenia and other psychoses Difference between neurosis and psychosis
Difference between neurosis and psychosis Traits of a psychopath
Traits of a psychopath Schizophreniform disorder icd-10
Schizophreniform disorder icd-10 Types of delusion
Types of delusion Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Types of somatic disorder
Types of somatic disorder Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Elsevier
Elsevier Chapter 10 nail disorders and diseases
Chapter 10 nail disorders and diseases Nail diseases and disorders milady
Nail diseases and disorders milady Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Eating disorder in which people overeat compulsively
Eating disorder in which people overeat compulsively