SARAH AWAISHEH ANTEPARTUM HEMORRHAGE ANATOMY OF THE UTERUS



- Slides: 25

SARAH AWAISHEH ANTEPARTUM HEMORRHAGE
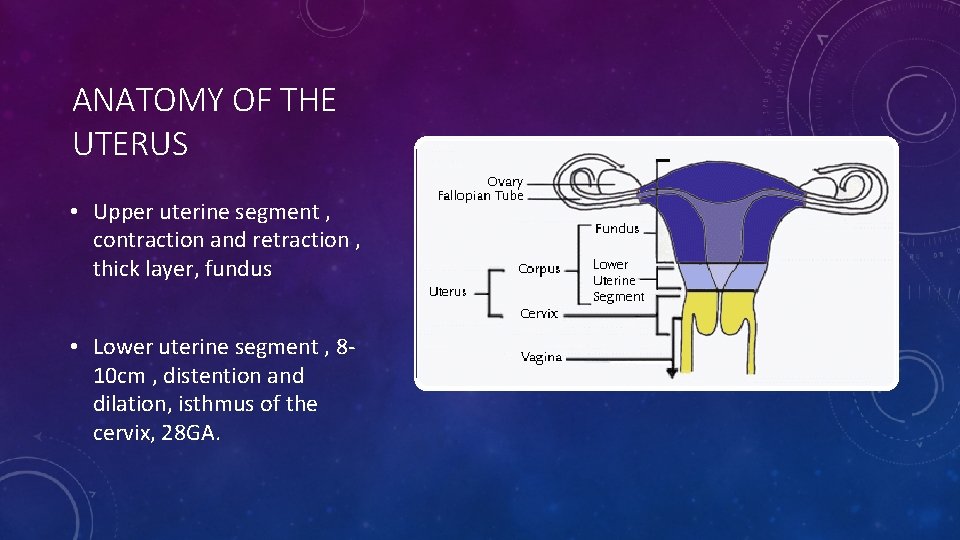
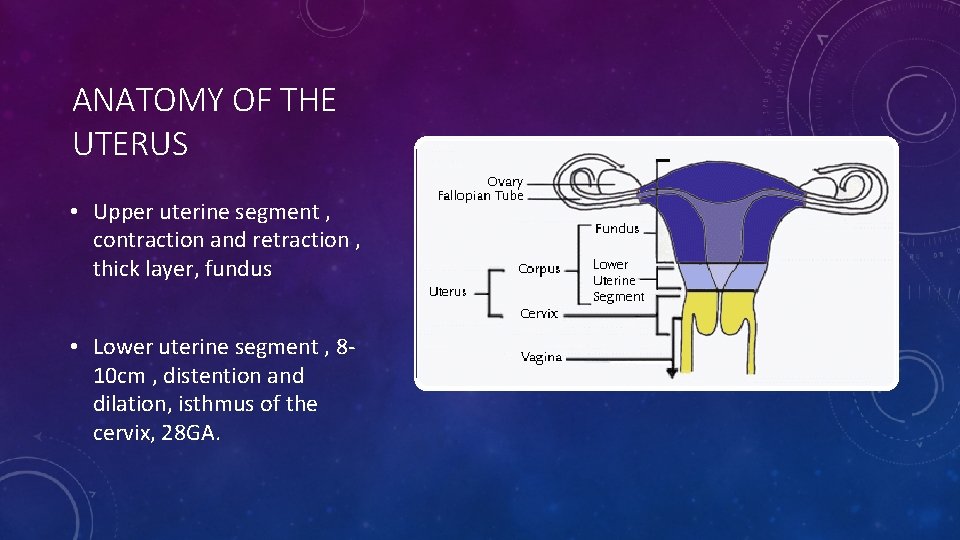
ANATOMY OF THE UTERUS • Upper uterine segment , contraction and retraction , thick layer, fundus • Lower uterine segment , 8‐ 10 cm , distention and dilation, isthmus of the cervix, 28 GA.
DEFINITION ANTEPARTUM HEMORRHAGE TYPICALLY REFERS TO VAGINAL BLEEDING AFTER 24 WEEKS OF GESTATION THAT IS UNRELATED TO LABOR AND DELIVERY. IT IS ASSOCIATED WITH SIGNIFICANT MATERNAL AND FETAL MORBIDITY AND MORTALITY.
• COMMON CAUSES OF ANTEPARTUM BLEEDING • Placenta previa (20 percent) • Abruptio placentae (30 percent) • UNCOMMON • Uterine rupture • VASA PREVIA
• Definition PLACENTA PREVIA • Presence of the placenta in lower uterine segment, which might lead to partial or full obstruction of the neck of the uterus with high risk of hemorrhage (rupture of placental vessels) and birth complications. • Epidemiology • ∼ 0. 5% AT TERM of all pregnancies

• WHAT DO YOU THINK THE RELATION BETWEEN THE GESTATIONAL AGE AND THE INCIDENCE?
PLACENTA PREVIA • Risk factors • MULTIPLE GESTATIONS (dichorionic vs monochorionic) • Previous placenta previa, previous/recurrent abortion • Previous cesarean delivery
PLACENTA PREVIA • Clinical features • asymptomatic • Sudden, painless, recurrent bright red vaginal bleeding (90%) • Often causes preterm delivery (∼ 45% of cases) • Soft, nontender uterus • Usually no fetal distress • 10 to 20 %of women present with uterine contractions, pain, and bleeding, similar to the presentation of abruptio placenta • About 10 percent of women reach term without bleeding • Diagnostics • Transvaginal ultrasound to assess the position of the placenta (Transvaginal ultrasound is the most sensitive imaging modality. Transabdominal ultrasound can be performed in conjunction with transvaginal ultrasound. ) • Digital vaginal examinations are contraindicated in cases of hemorrhage of unknown cause!
ASSOCIATED FINDINGS • Placenta previa‐accreta • Malpresentation
• Treatment • Approach PLACENTA PREVIA V • • Gestational age < 37 weeks • No active bleeding AND no evidence of fetal distress ‐‐‐‐ ‐‐> postpond 37 w and do expectant managment • Severe, active bleeding OR evidence of fetal distress: stabilization and emergency cesarian section Gestational age > 37 weeks: immediate delivery
• PLACENTA PREVIA Expectant management • Hospitalization and observation for 48 hours • If gestational age is < 34 weeks: fetal lung maturity induction with corticosteroids (e. g. , betamethasone) • If gestational age is between 34 and 37 weeks and delivery is likely within 7 days: fetal lung maturity induction with corticosteroids • If mild uterine contractions are present: tocolysis with magnesium sulfate may be performed (especially if the fetus is extremely premature) • Route of delivery • Lower segment cesarean section is almost always preferred; ideally scheduled at 36– 37 weeks gestation
VAGINAL DELIVERY SHOULD NEVER BE ATTEMPTED OUTSIDE THE OPERATING ROOM IN A PATIENT WITH PLACENTA PREVIA
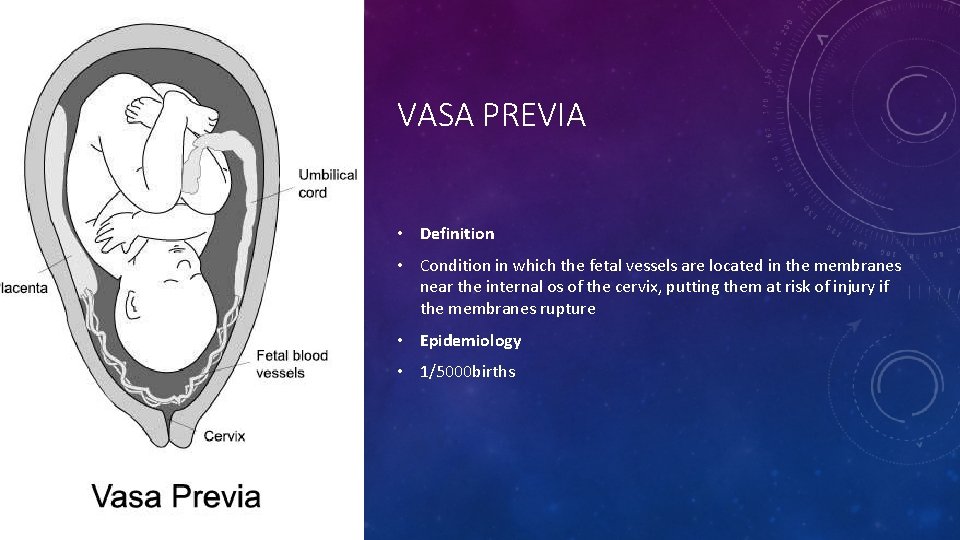
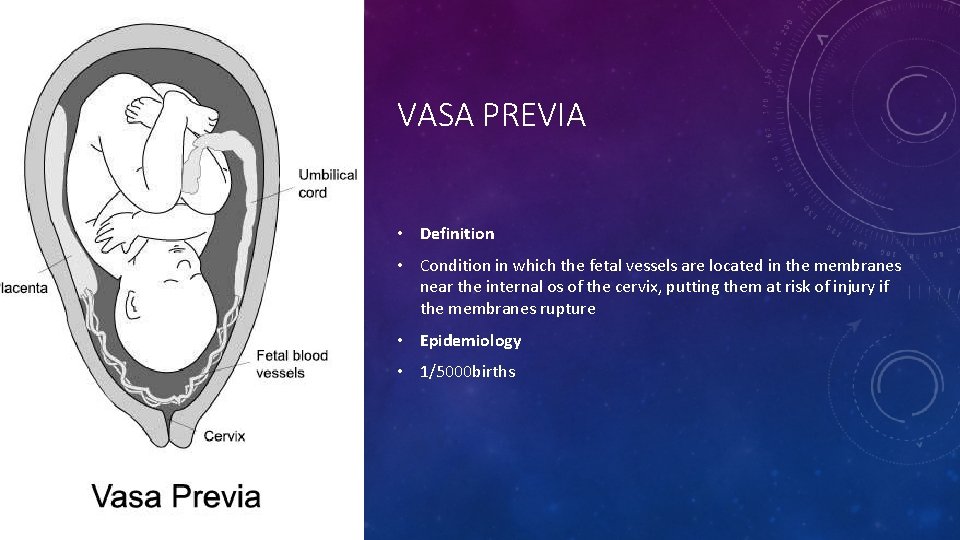
VASA PREVIA • Definition • Condition in which the fetal vessels are located in the membranes near the internal os of the cervix, putting them at risk of injury if the membranes rupture • Epidemiology • 1/5000 births
• a vasa praevia is likely to rupture in active labour, or when amniotomy is performed to induce or augment labour, in particular when located near or over the cervix, under the fetal presenting part. • Vasa praevia may be diagnosed during early labour by vaginal examination, detecting the pulsating fetal vessels inside the internal os, or by the presence of dark‐red vaginal bleedin, Transabdominal or transvaginal ultrasound with color Doppler shows fetal vessels overlying the internal os and decreased blood flow within fetal vessels. • The fetal mortality rate in this situation is at least 60% despite urgent caesarean delivery.
VASA PREVIA • Treatment • Emergency cesarean if there are signs of fetal distress
PLACENTA ABRUPTION • The partial or complete separation of the placenta from the uterus prior to delivery. Subsequent hemorrhage occurs from both maternal and fetal vessels. • Epidemiology • Incidence: ∼ 0. 2– 1% of pregnancies. • Occurs most often in the third trimester. • The recurrence rate in subsequent pregnancies is 3– 15%.

Etiology • Predisposing factors • Vascular changes • Hypertension (most common cause) • Preeclampsia/eclampsia • (Abdominal) trauma (up to 10% of cases): car accidents, falls, iatrogenic (e. g. , post‐amniocentesis) • Sudden decrease in intrauterine pressure (After delivery of the first child in multiple pregnancy or in premature rupture of the membrane) • Previous abruption • Alcohol and cigarette consumption, cocaine use • Clinical picture • Continuous, dark, vaginal bleeding (revealed abruptio placentae) • In ∼ 20% of cases, the hemorrhage is mainly retroplacental; vaginal bleeding does not occur (concealed abruptio placentae) • Abdominal pain or back pain • , uterine tenderness • Hypertonic contractions (rigid uterus), premature labor • Fetal distress (60% of cases) • Possible diminished or absent fetal movement • Decelerations seen on fetal heart monitor • Vaginal exam contraindicated: may worsen bleeding
* RAPID DIAGNOSIS AND IMMEDIATE TREATMENT ARE VITAL FOR THE SURVIVAL OF BOTH MOTHER AND CHILD! • Diagnostics • • Placental abruption is a clinical diagnosis. Ultrasound (transabdominal, transvaginal): only 25% sensitivity! • Presentation of the placental position and a possible retroplacental hematoma • Monitoring vital signs of the fetus (heartbeat, fetal movement) • To rule out placenta previa in unclear cases • Fetal heart rate monitoring • Laboratory tests: CBC, coagulation factors • Treatment
UTERINE RUPTURE • Uterine rupture is a pregnancy complication that is life‐threatening for the mother and the baby. It occurs in approximately one in every 4, 000 births, and in most cases, during labor. • Incidence: 1/4000 births(As a result of the rising number of C‐sections and labor induction, uterine ruptures have increased in frequency)
UTERINE RUPTURE • Clinically significant uterine rupture after a previous cesarean delivery refers to complete disruption of all uterine layers, including the serosa, leading to changes in maternal or fetal status. • most common in women with a prior hysterotomy • usually occurs during labor.
CLINICAL PICTURE • Severe abdominal pain • Sudden pause in contractions • Fetal distress (e. g. , deteriorating fetal heart rate) • Vaginal bleeding • Hemodynamic instability (as a result of abdominal bleeding) • Loss of fetal station • Palpable fetal parts through the ruptur
TREATMENT • Uterine rupture: • Immediate laparotomy with emergency C‑section • Hysterectomy necessary if the bleeding does not cease • Uterine dehiscence: Cesarean delivery before labor begins is recommended to avoid a complete rupture. • prognosis • Traumatic and spontaneous ruptures increase the mortality rate of the mother and the baby. • Open ruptures lead to hypovolemia and hypoxia; as a result, the fetal mortality rate is between 50– 75%
THANK YOU.
 Antepartum hemorrhage definition
Antepartum hemorrhage definition Klasifikasi perdarahan antepartum
Klasifikasi perdarahan antepartum Tanya zakrison
Tanya zakrison Subconjunctival hemorrhage
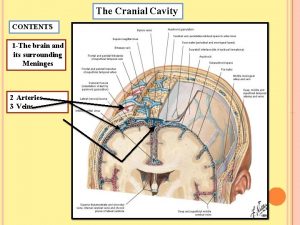
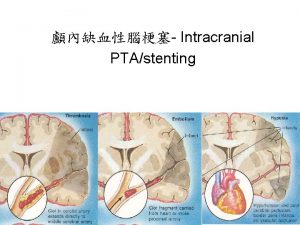
Subconjunctival hemorrhage Middle meningeal artery
Middle meningeal artery Hemorrhage
Hemorrhage Raina flores
Raina flores Management of hemorrhage
Management of hemorrhage Hunt and hess score
Hunt and hess score Stamca
Stamca Vertical
Vertical Hemorrhage
Hemorrhage Subgaleal hemorrhage
Subgaleal hemorrhage 4t postpartum hemorrhage
4t postpartum hemorrhage Gastroesophageal sphincter
Gastroesophageal sphincter Brain hemorrhage
Brain hemorrhage Management of hemorrhage
Management of hemorrhage Post tonsillectomy hemorrhage
Post tonsillectomy hemorrhage Postpartum hemorrhage
Postpartum hemorrhage Pph management
Pph management Antipartum hemorrhage
Antipartum hemorrhage Venous beading
Venous beading Postnatal nursing diagnosis slideshare
Postnatal nursing diagnosis slideshare External loss
External loss Trauma triad of death
Trauma triad of death Post tonsillectomy hemorrhage
Post tonsillectomy hemorrhage