Recanalization of Central Venous Total Occlusions Dr Steven



- Slides: 31
Recanalization of Central Venous Total Occlusions Dr. Steven Abramowitz, MD Med. Star Washington Hospital Washington, DC
Steven Abramowitz, MD I have no relevant financial relationships
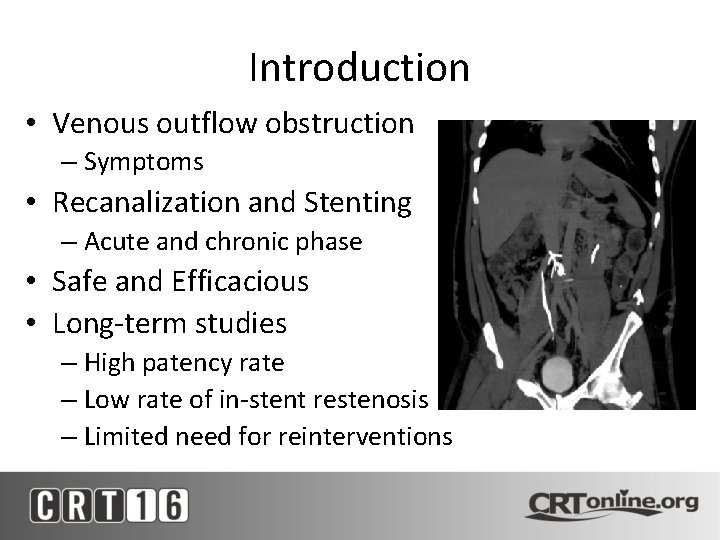
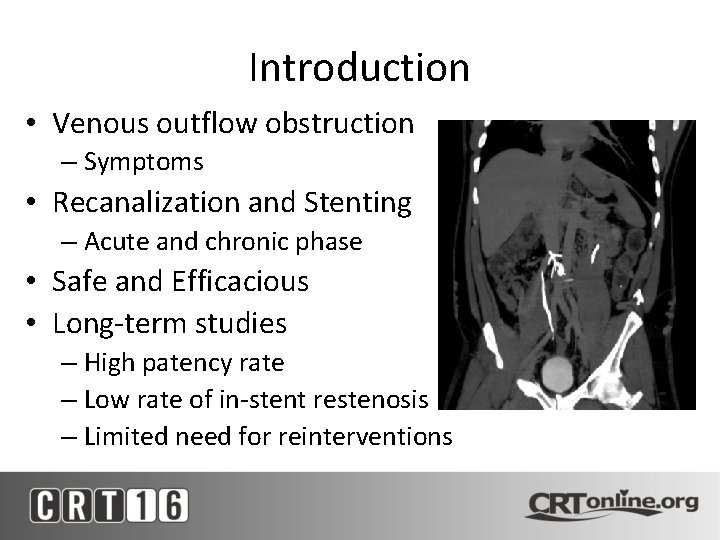
Introduction • Venous outflow obstruction – Symptoms • Recanalization and Stenting – Acute and chronic phase • Safe and Efficacious • Long-term studies – High patency rate – Low rate of in-stent restenosis – Limited need for reinterventions

General Principles • Anesthesia – Sedation v General • Foley Catheter • Position – Prone or Supine
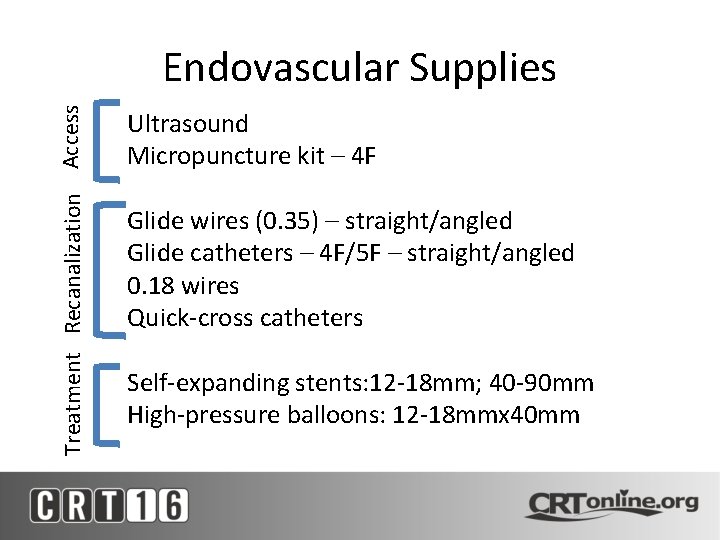
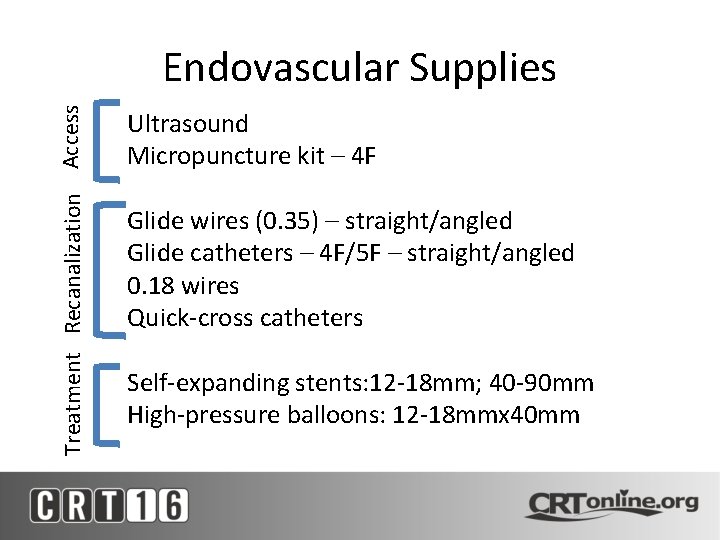
Treatment Recanalization Access Endovascular Supplies Ultrasound Micropuncture kit – 4 F Glide wires (0. 35) – straight/angled Glide catheters – 4 F/5 F – straight/angled 0. 18 wires Quick-cross catheters Self-expanding stents: 12 -18 mm; 40 -90 mm High-pressure balloons: 12 -18 mmx 40 mm
Access • US Guided – Femoral – Popliteal – Internal jugular • Chronicity – May or may not have backbleeding
Crossing Techniques • Acute occlusions – Cross occlusion – Thrombolysis • Chronic occlusions – Cross occlusion – can be challenging – Pre-dilate 6 -8 mm
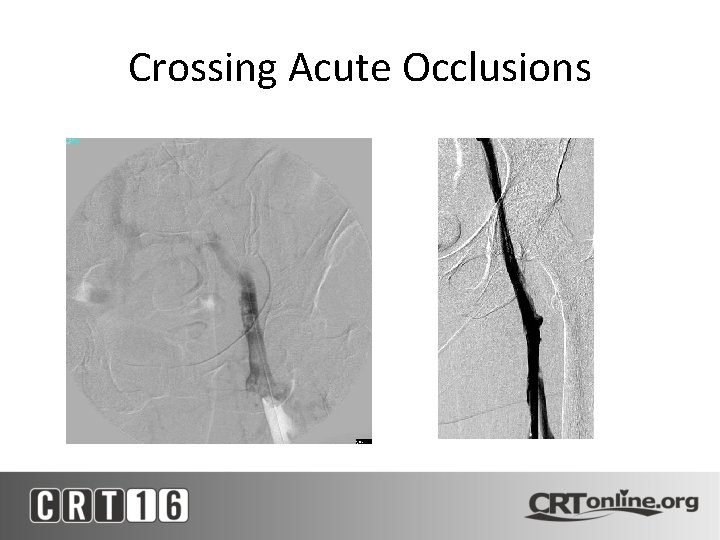
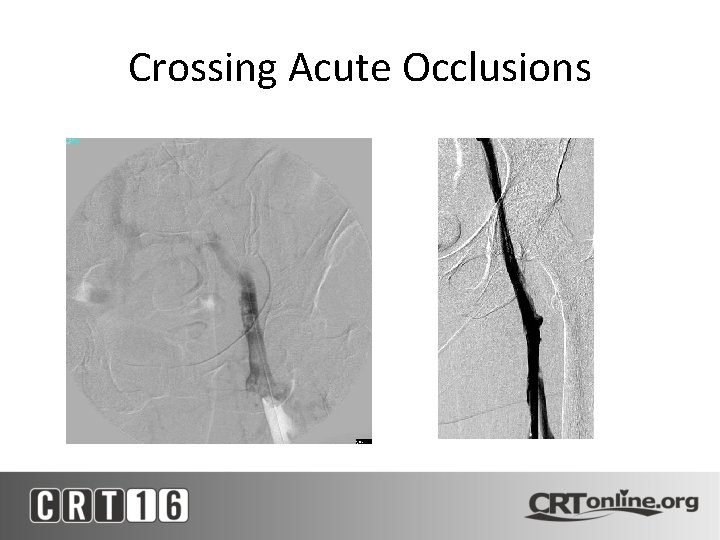
Crossing Acute Occlusions
Crossing Chronic Occlusions • Hydrophilic Wire/Catheter • Multiple Access Points – Prepare to Snare • Adequate System – Long Sheath • Telescoping Sheaths • Patience

Crossing Chronic Occlusions • Crossing – Advanced: • Glide/Amplatz Back End • Telescoping Catheters • Sharp Recanalization (Chiba or Rosch-Uchida)
Crossing Chronic Occlusions • Pre-Dilate – Use 6 -8 mm balloons – 30 sec inflation times – Do not dilate to desired diameter – Enough to deliver stent
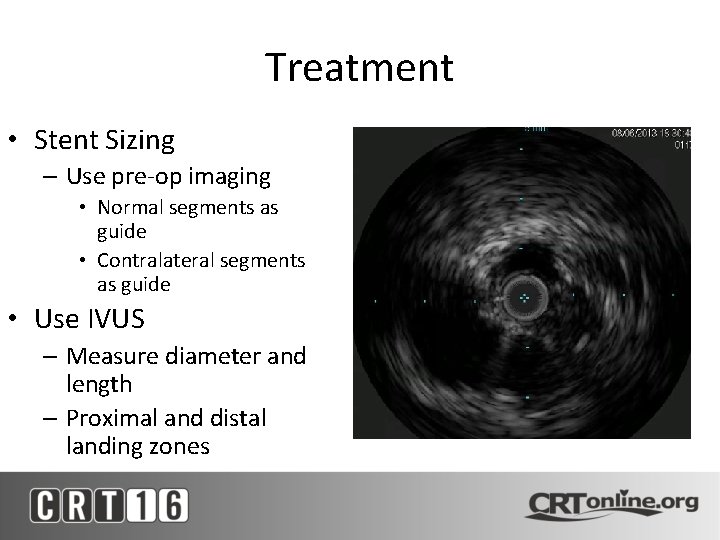
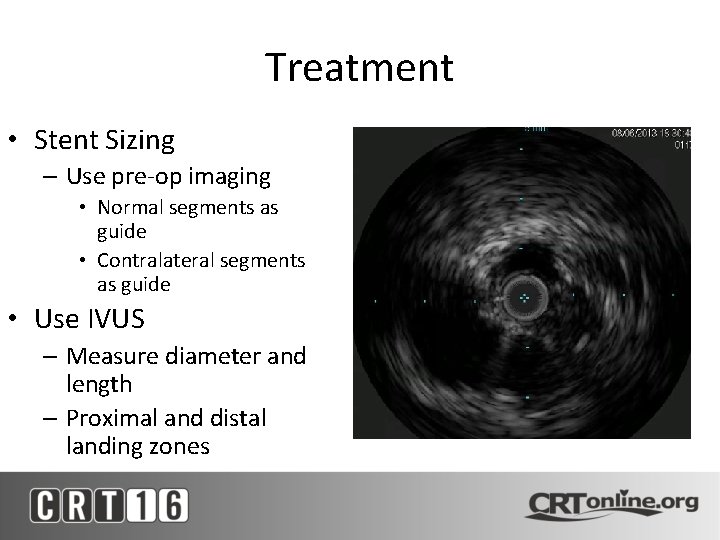
Treatment • Stent Sizing – Use pre-op imaging • Normal segments as guide • Contralateral segments as guide • Use IVUS – Measure diameter and length – Proximal and distal landing zones
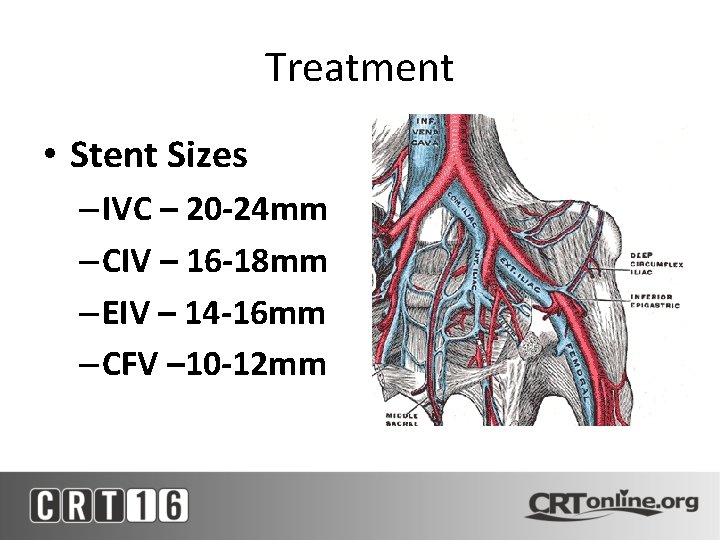
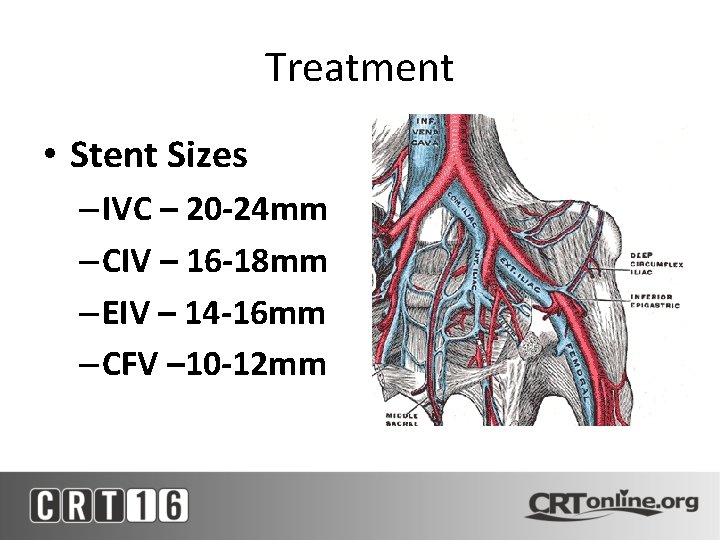
Treatment • Stent Sizes – IVC – 20 -24 mm – CIV – 16 -18 mm – EIV – 14 -16 mm – CFV – 10 -12 mm
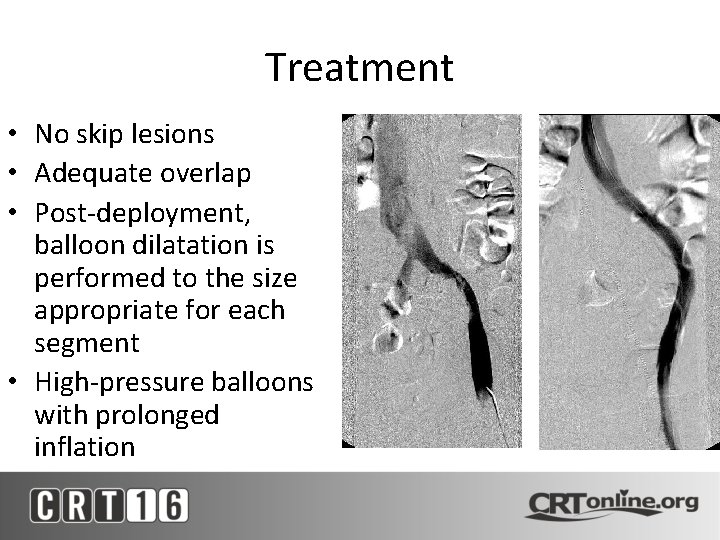
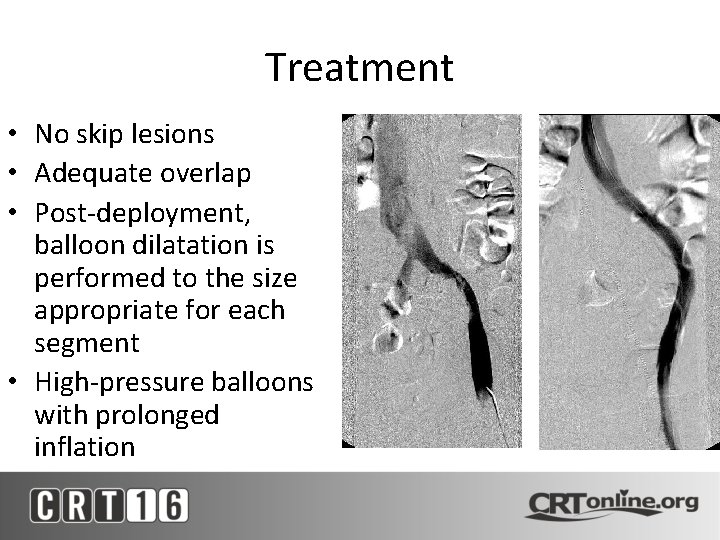
Treatment • No skip lesions • Adequate overlap • Post-deployment, balloon dilatation is performed to the size appropriate for each segment • High-pressure balloons with prolonged inflation
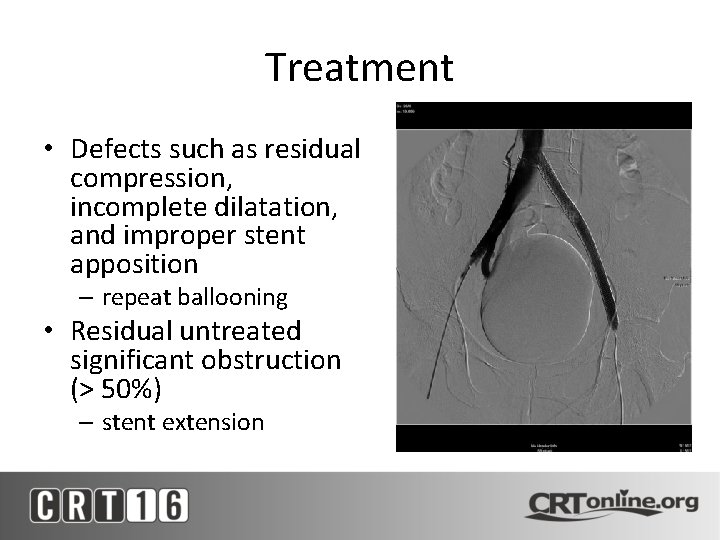
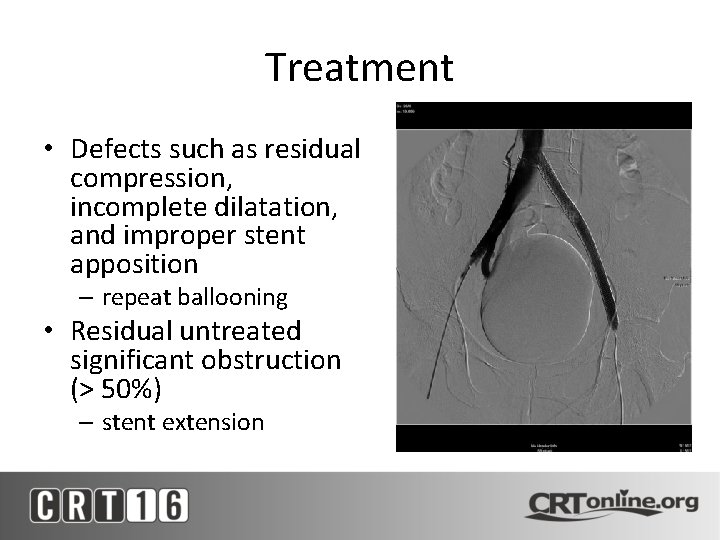
Treatment • Defects such as residual compression, incomplete dilatation, and improper stent apposition – repeat ballooning • Residual untreated significant obstruction (> 50%) – stent extension
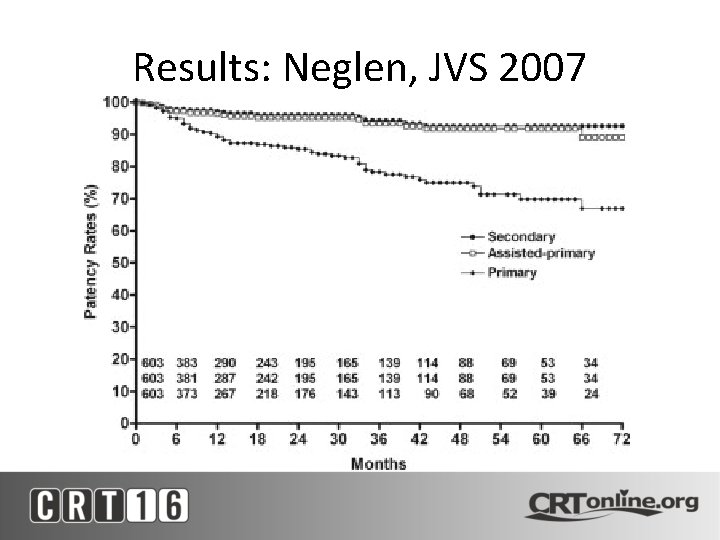
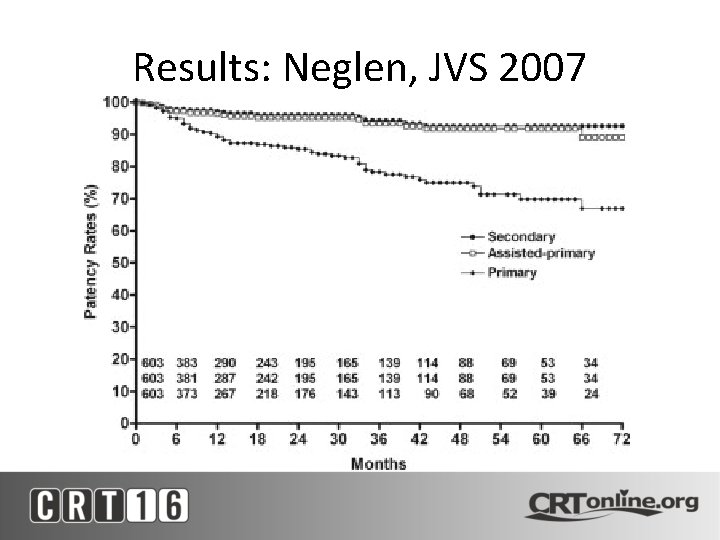
Results: Neglen, JVS 2007
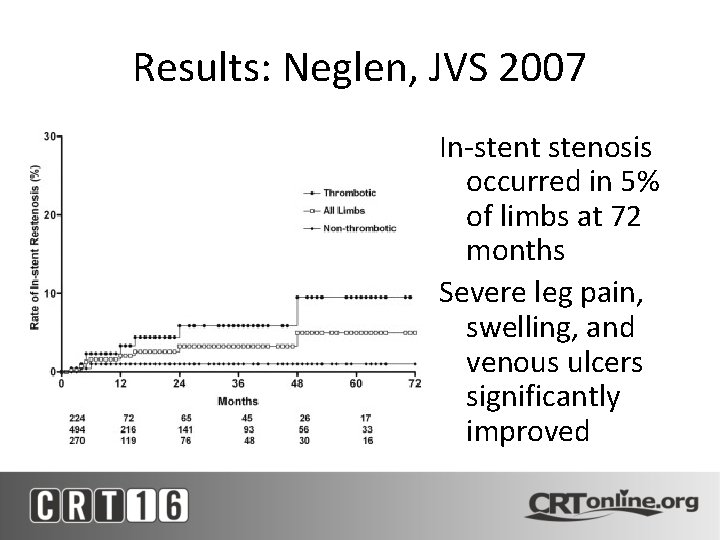
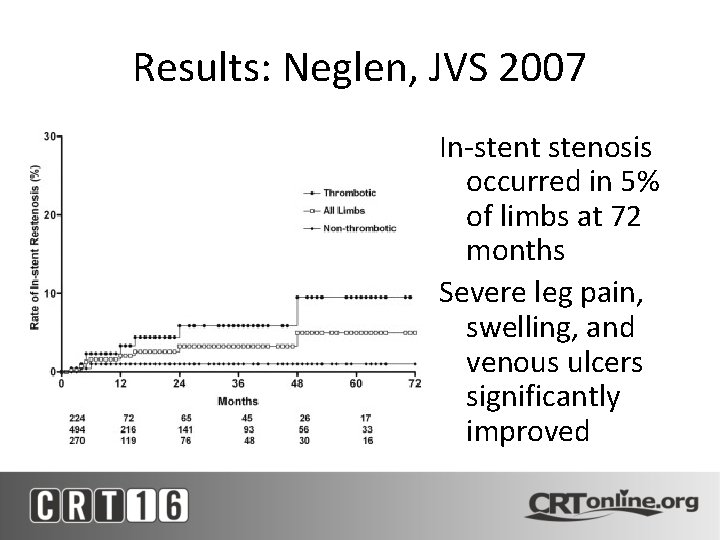
Results: Neglen, JVS 2007 In-stent stenosis occurred in 5% of limbs at 72 months Severe leg pain, swelling, and venous ulcers significantly improved
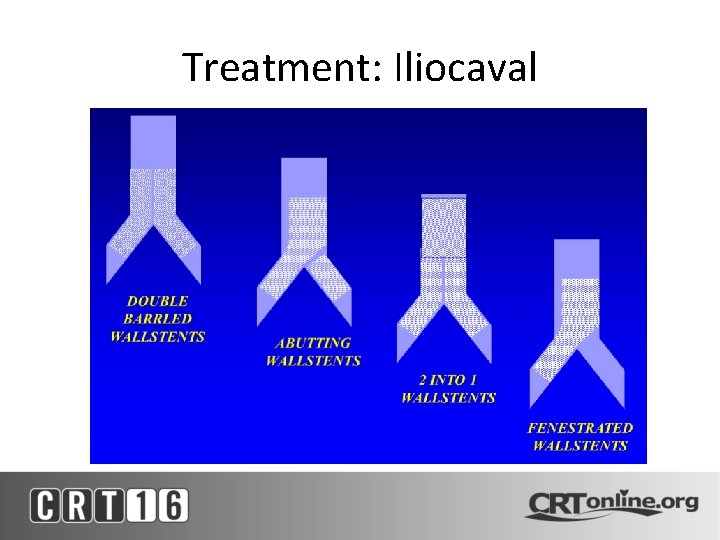
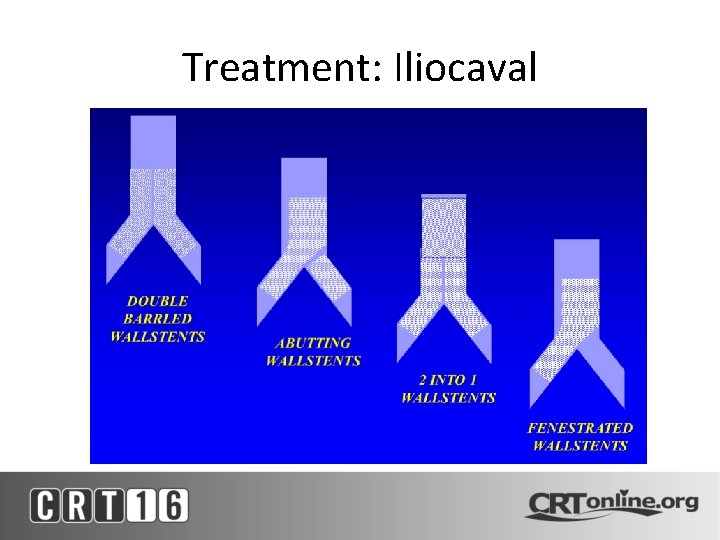
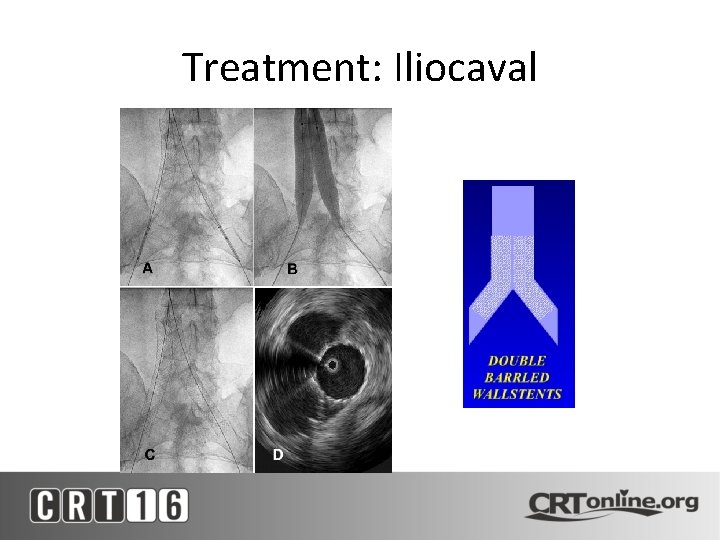
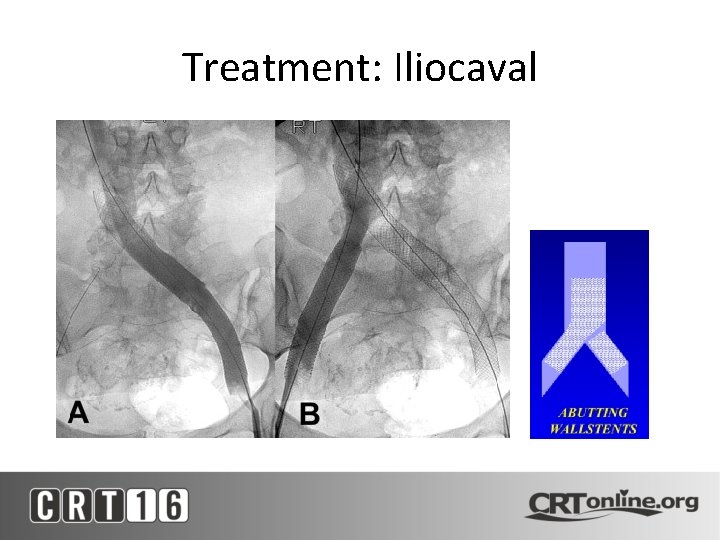
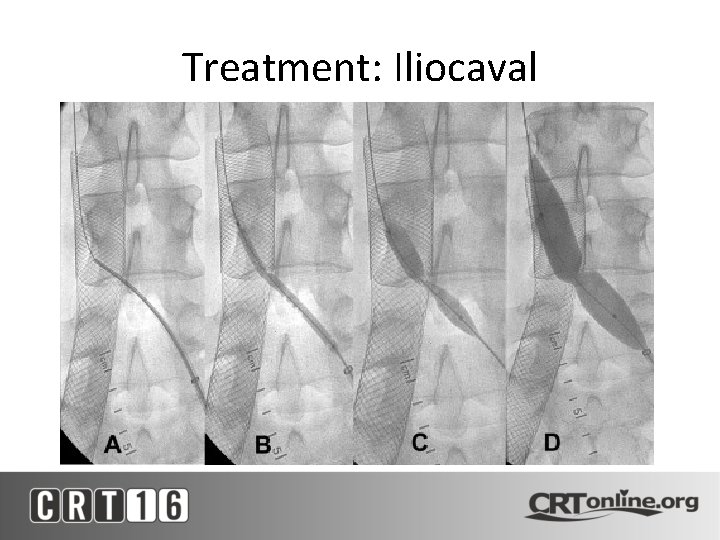
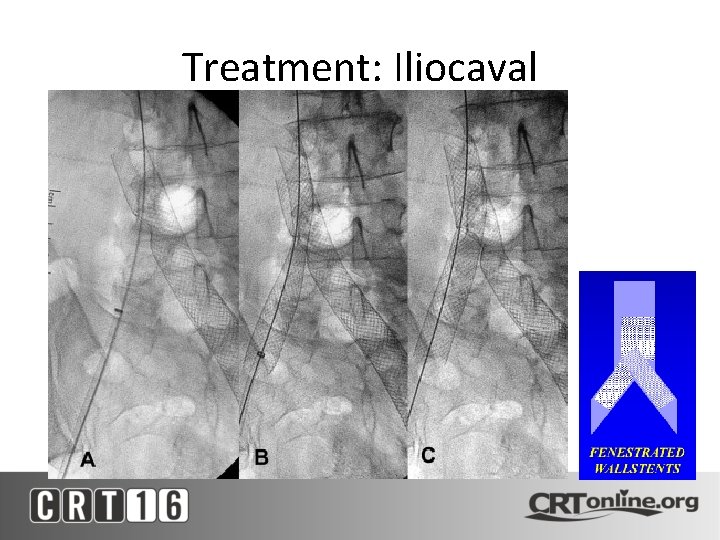
Treatment: Iliocaval
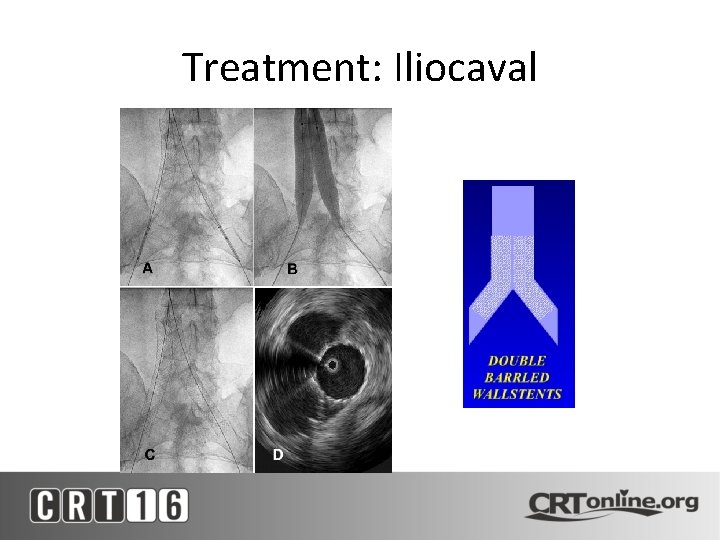
Treatment: Iliocaval
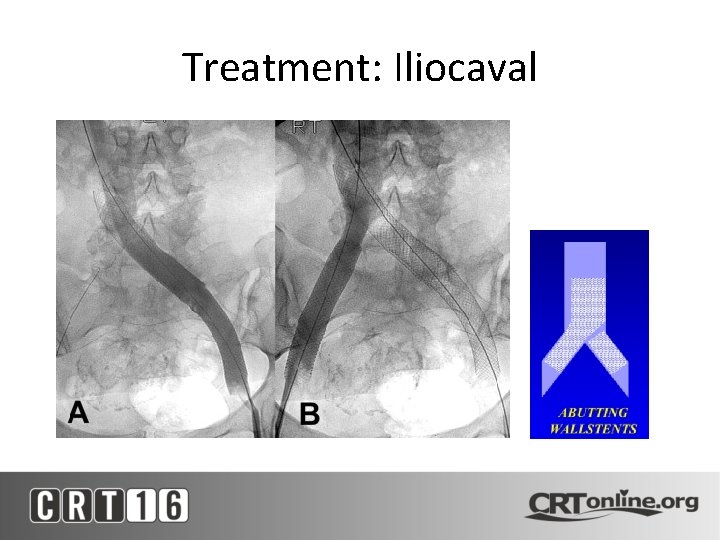
Treatment: Iliocaval
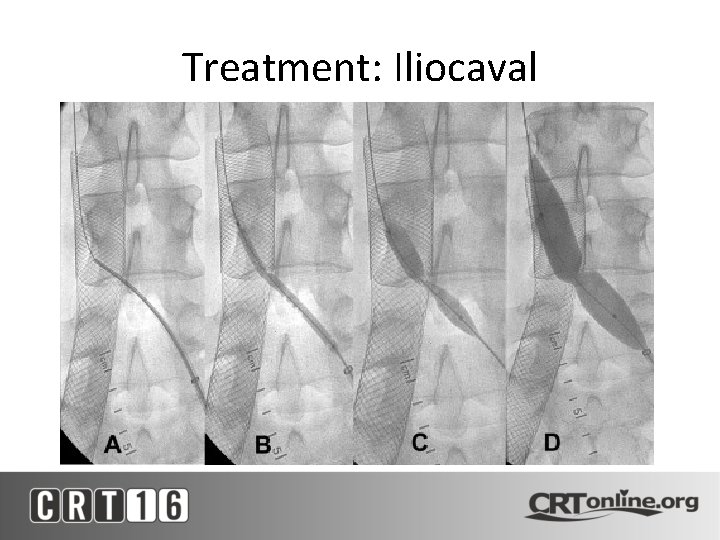
Treatment: Iliocaval
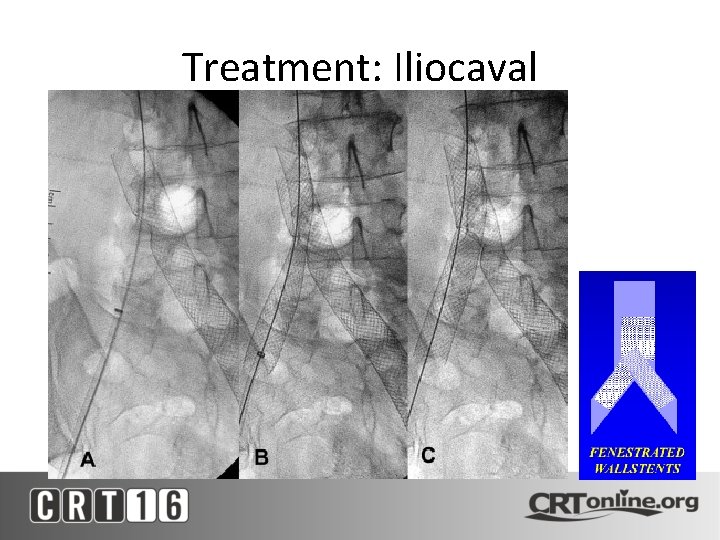
Treatment: Iliocaval
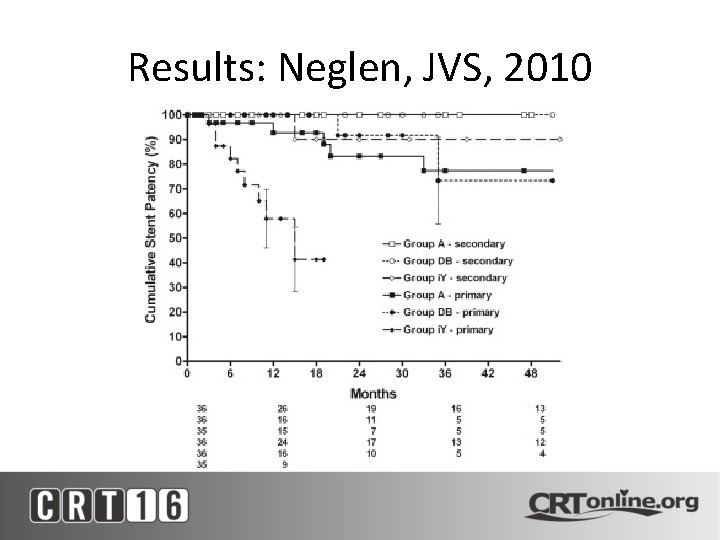
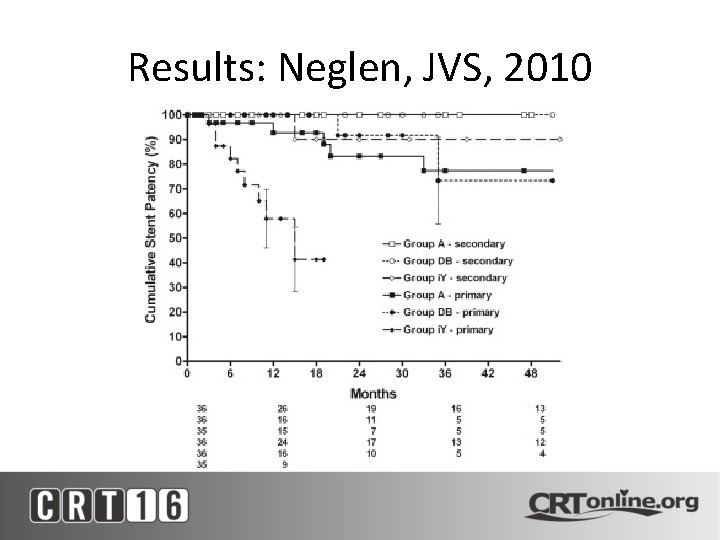
Results: Neglen, JVS, 2010
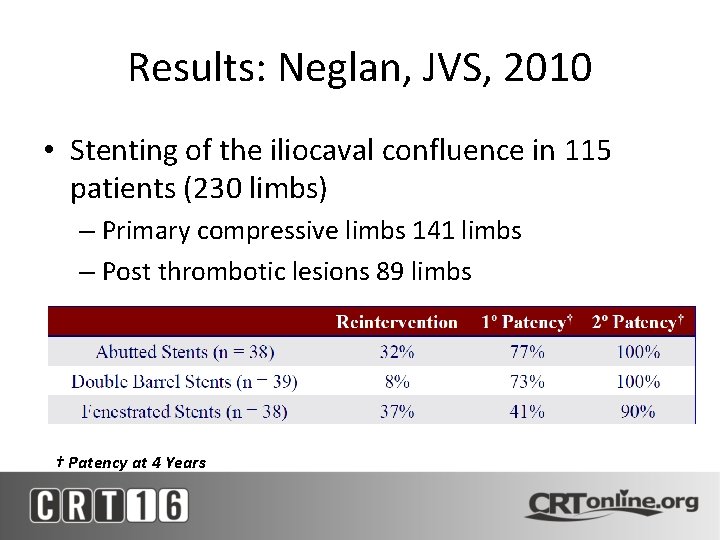
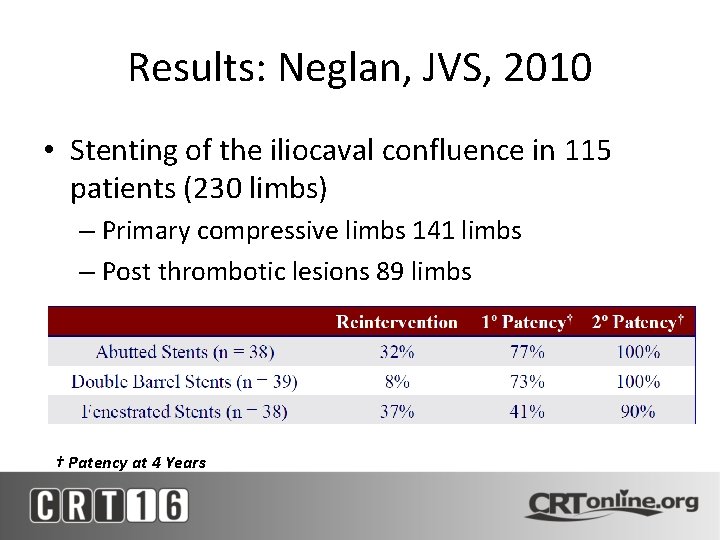
Results: Neglan, JVS, 2010 • Stenting of the iliocaval confluence in 115 patients (230 limbs) – Primary compressive limbs 141 limbs – Post thrombotic lesions 89 limbs † Patency at 4 Years

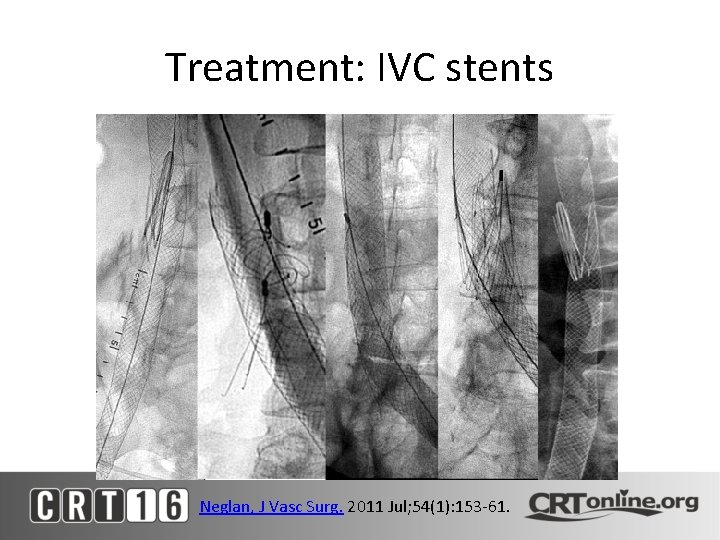
Treatment: IVC stents
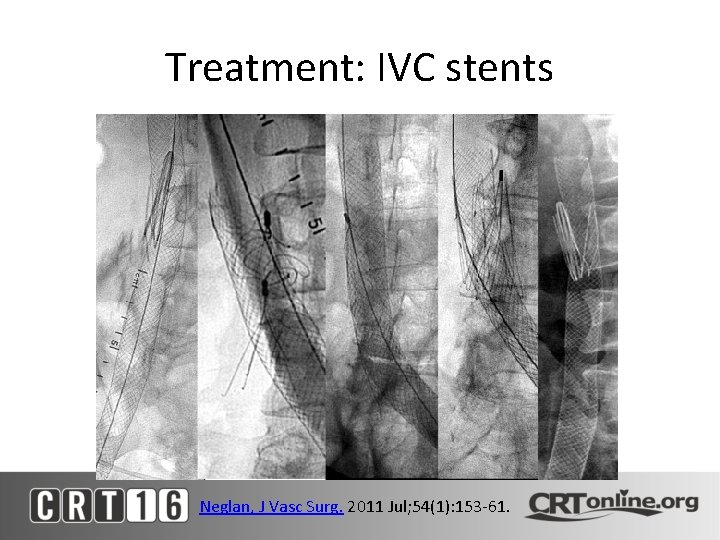
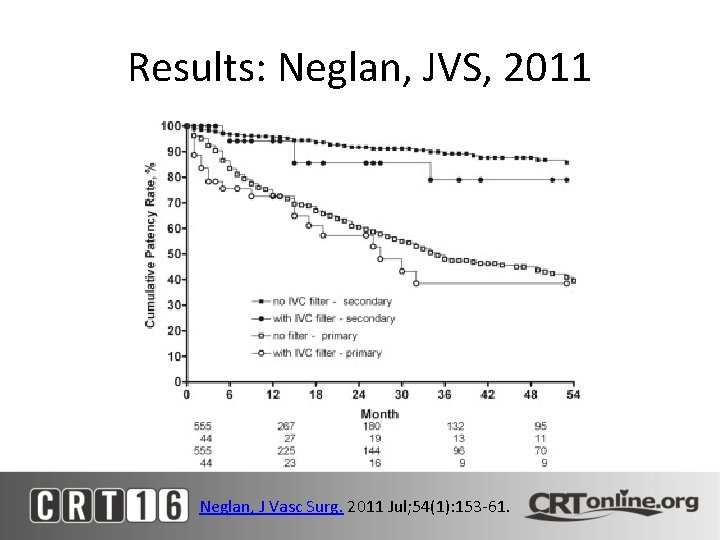
Treatment: IVC stents Neglan, J Vasc Surg. 2011 Jul; 54(1): 153 -61.
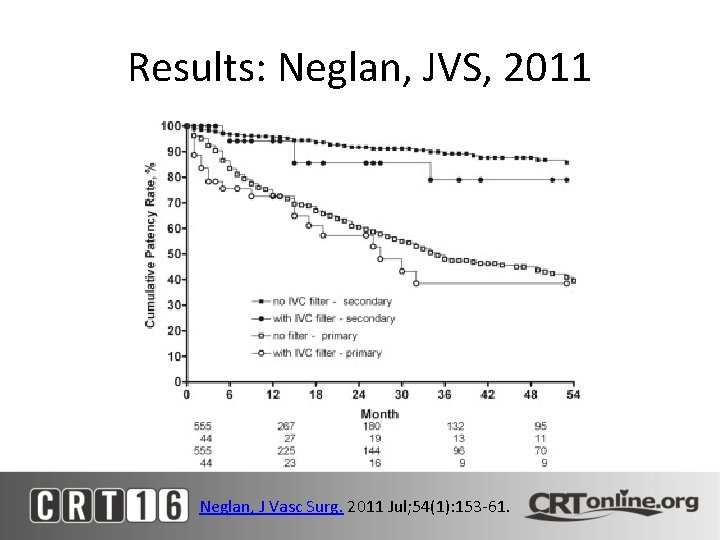
Results: Neglan, JVS, 2011 Neglan, J Vasc Surg. 2011 Jul; 54(1): 153 -61.
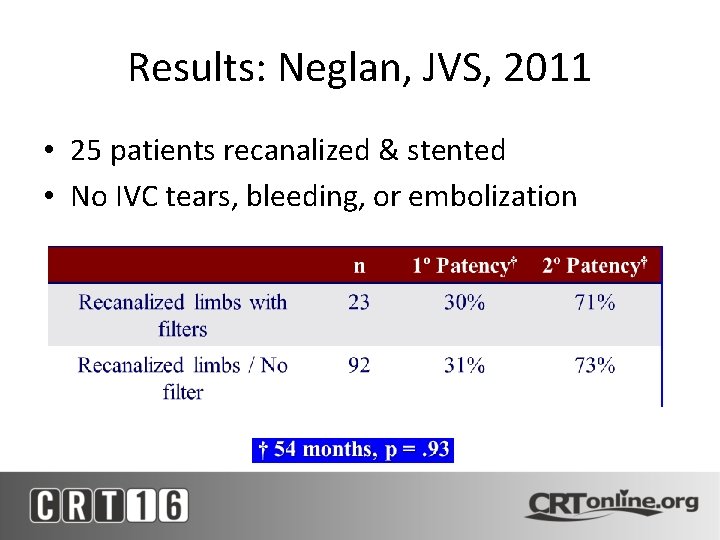
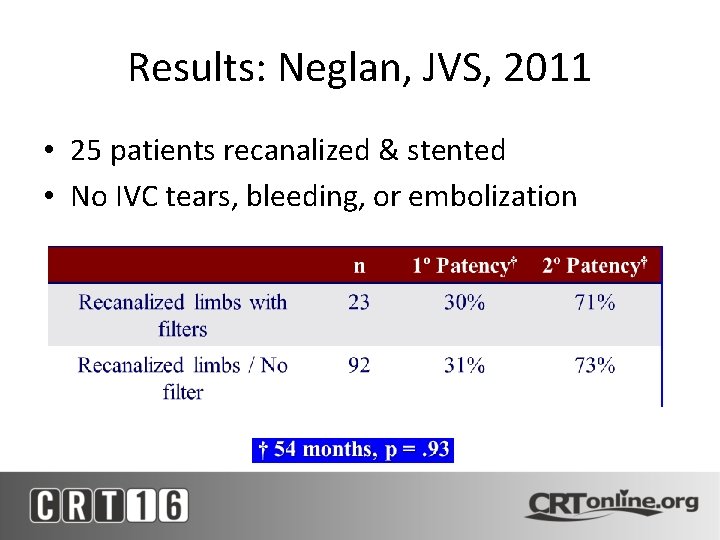
Results: Neglan, JVS, 2011 • 25 patients recanalized & stented • No IVC tears, bleeding, or embolization
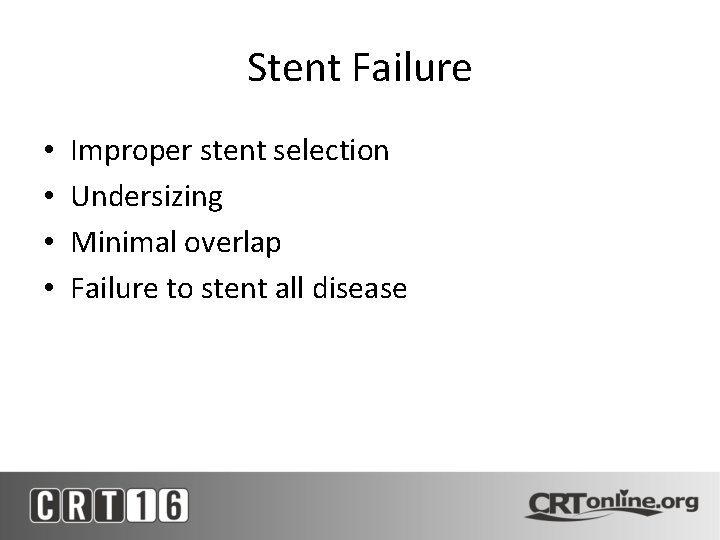
Stent Failure • • Improper stent selection Undersizing Minimal overlap Failure to stent all disease
Conclusions • Endovascular recanalization of chronic venous occlusions are safe and effective • Cover all diseased segments • Need good inflow and outflow • Knowledge of available catheters, wires, stents and IVUS
 Portal vein recanalization
Portal vein recanalization Tapvd
Tapvd Phlebostatic axis
Phlebostatic axis Broviac catheter
Broviac catheter Groshung
Groshung Most common complication of central venous catheter
Most common complication of central venous catheter Hob 60 degrees
Hob 60 degrees Broviac vs hickman
Broviac vs hickman Total revenues minus total costs equals
Total revenues minus total costs equals Total revenues minus total costs equals
Total revenues minus total costs equals Unidad 3 razones financieras
Unidad 3 razones financieras Total revenue minus total expenses
Total revenue minus total expenses Total revenues minus total costs equals
Total revenues minus total costs equals Origin of vascular cambium
Origin of vascular cambium Mudpiles
Mudpiles Venous beading
Venous beading Retrohyaloid hemorrhage
Retrohyaloid hemorrhage Absent x descent
Absent x descent Venous vs arterial blood
Venous vs arterial blood Posterior thorax lecture
Posterior thorax lecture Venous loop
Venous loop Recurrent ulnar artery
Recurrent ulnar artery Deep venous system
Deep venous system Venous ulcer grading
Venous ulcer grading Venous and lymphatic drainage
Venous and lymphatic drainage Blood vessels
Blood vessels Indibulum
Indibulum Hunter perforator
Hunter perforator Hard exudates vs cotton wool spots
Hard exudates vs cotton wool spots Superficial temporal vein
Superficial temporal vein Peripheral venous thrombolysis
Peripheral venous thrombolysis Parts of oesophagus
Parts of oesophagus