Pulmonary venous anomalies DOLLY MATHEW Anatomy of pulm






- Slides: 86
Pulmonary venous anomalies DOLLY MATHEW
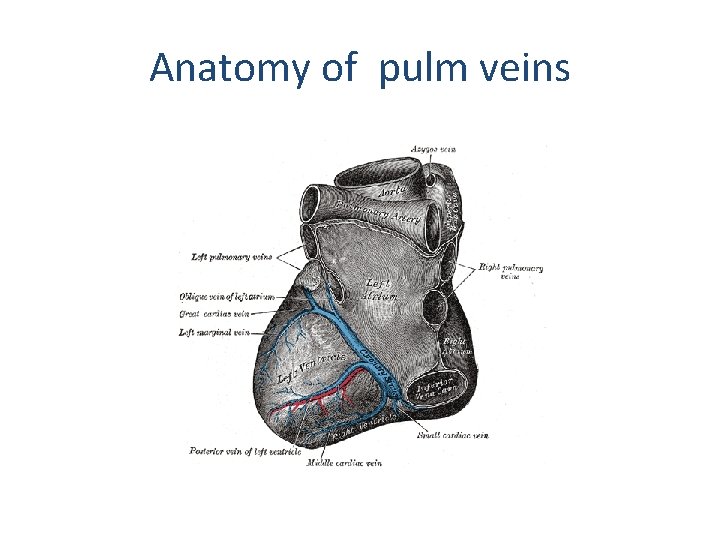
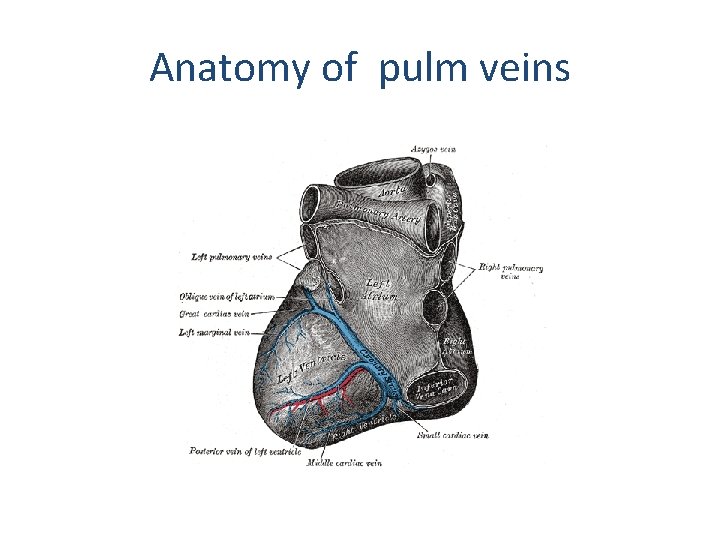
Anatomy of pulm veins
Venous anomalies • • Anomalous connections Anomalous drainage with normal connections Stenotic connections Abnormal number of pulmonary veins
Anomalous connections & drainage • TAPVC : all the veins connect anomalously • PAPVC : 1 or more, not all , of the veins connect anomalously • TAPVD/PAPVD: all or some of the pulmonary veins drain anomalously into the RA, without being abnormally connected Stenotic connections • Produce obstruction to pulmonary venous return to LA (N connection) / RA ( Ano conn)
Embryology
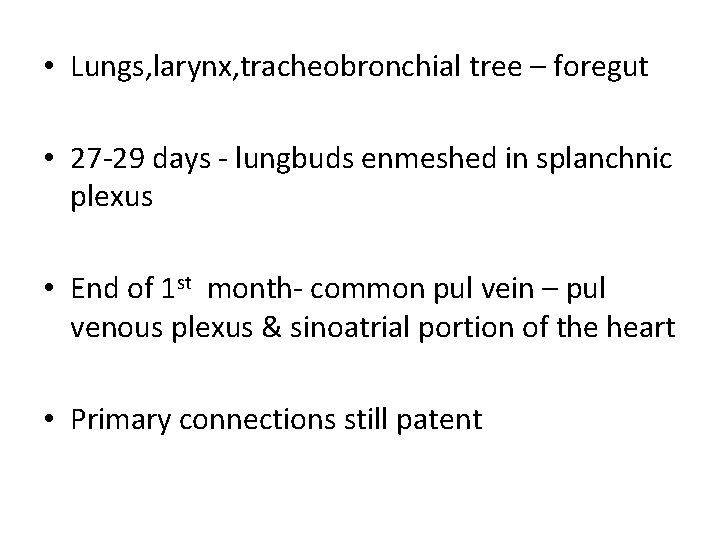
• Lungs, larynx, tracheobronchial tree – foregut • 27 -29 days - lungbuds enmeshed in splanchnic plexus • End of 1 st month- common pul vein – pul venous plexus & sinoatrial portion of the heart • Primary connections still patent


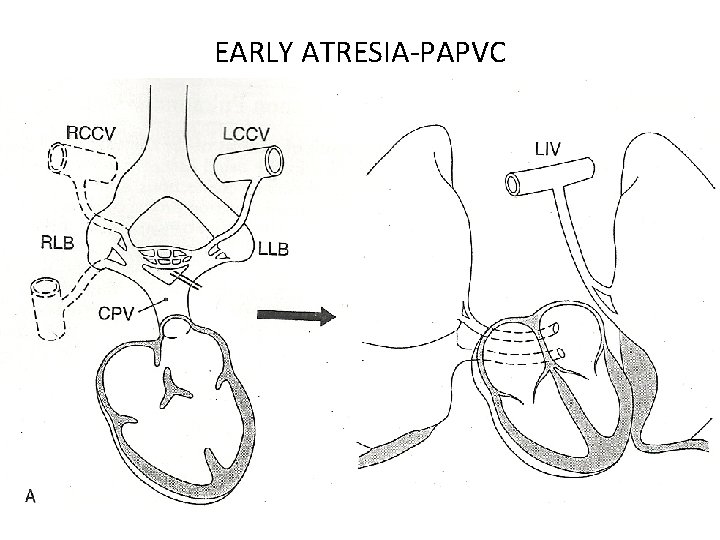
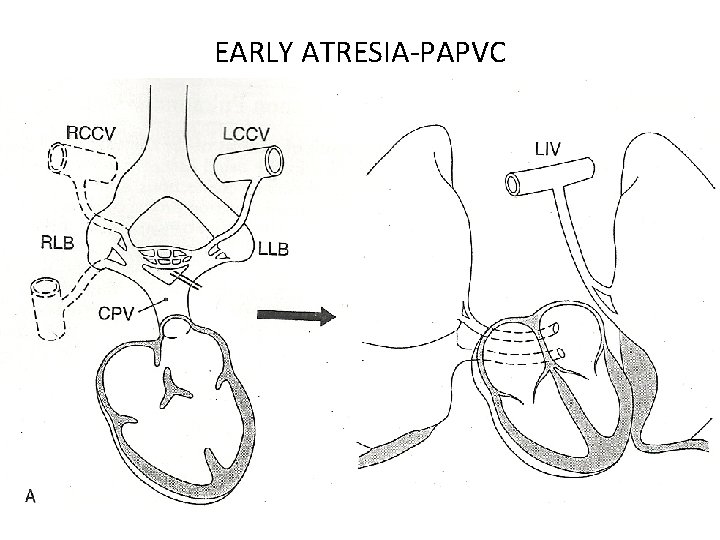
EARLY ATRESIA-PAPVC
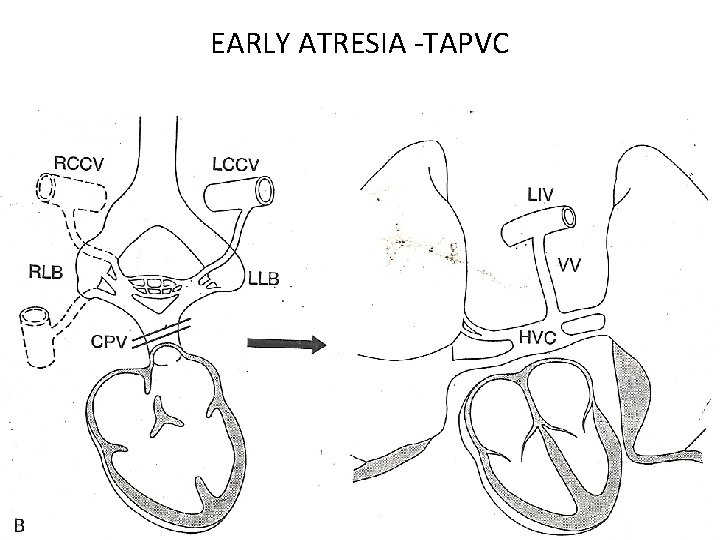
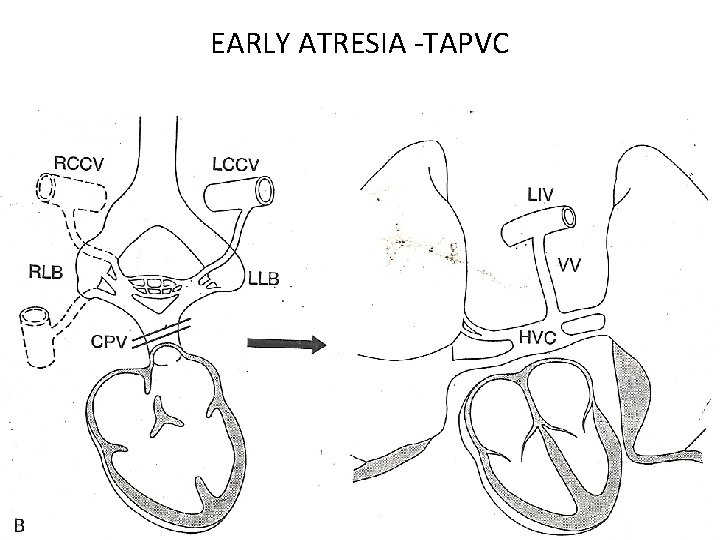
EARLY ATRESIA -TAPVC
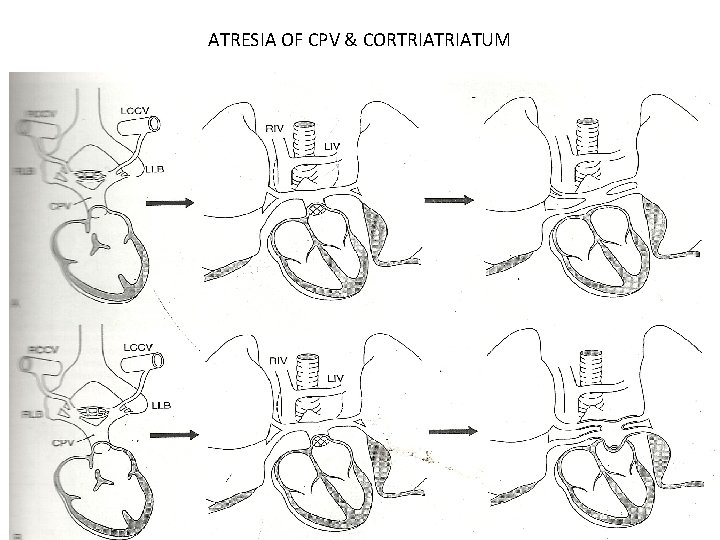
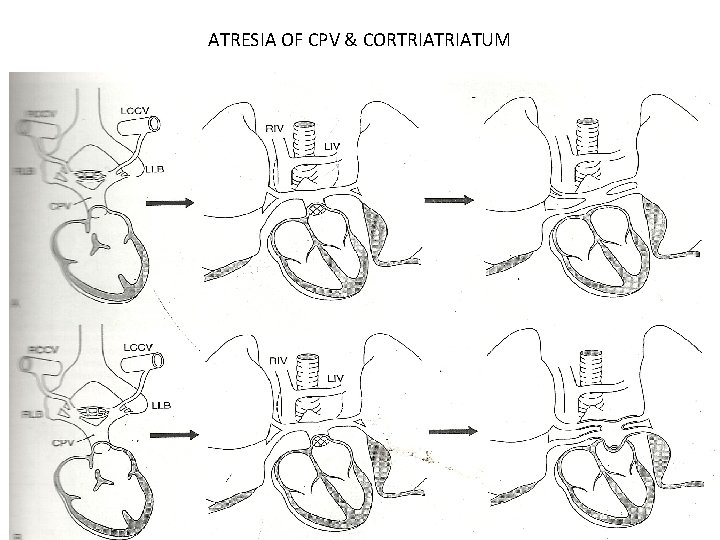
ATRESIA OF CPV & CORTRIATUM
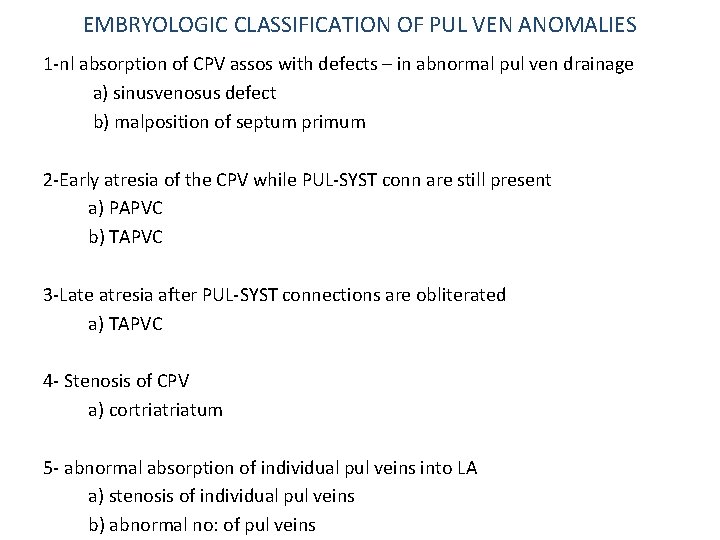
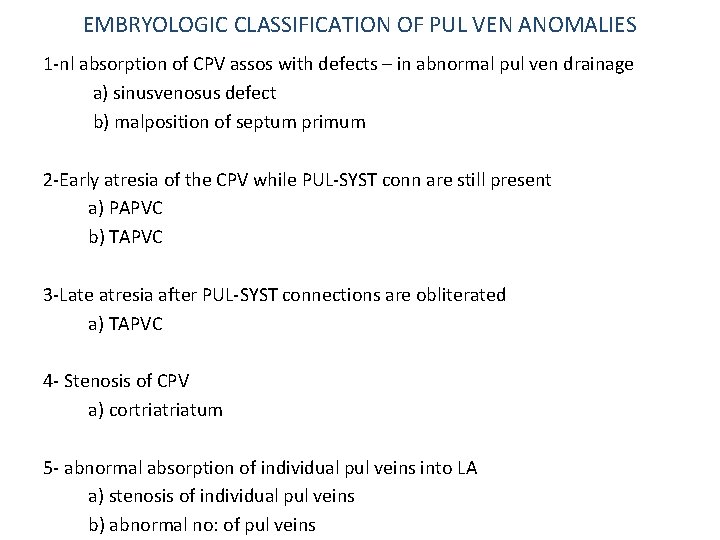
EMBRYOLOGIC CLASSIFICATION OF PUL VEN ANOMALIES 1 -nl absorption of CPV assos with defects – in abnormal pul ven drainage a) sinusvenosus defect b) malposition of septum primum 2 -Early atresia of the CPV while PUL-SYST conn are still present a) PAPVC b) TAPVC 3 -Late atresia after PUL-SYST connections are obliterated a) TAPVC 4 - Stenosis of CPV a) cortriatum 5 - abnormal absorption of individual pul veins into LA a) stenosis of individual pul veins b) abnormal no: of pul veins
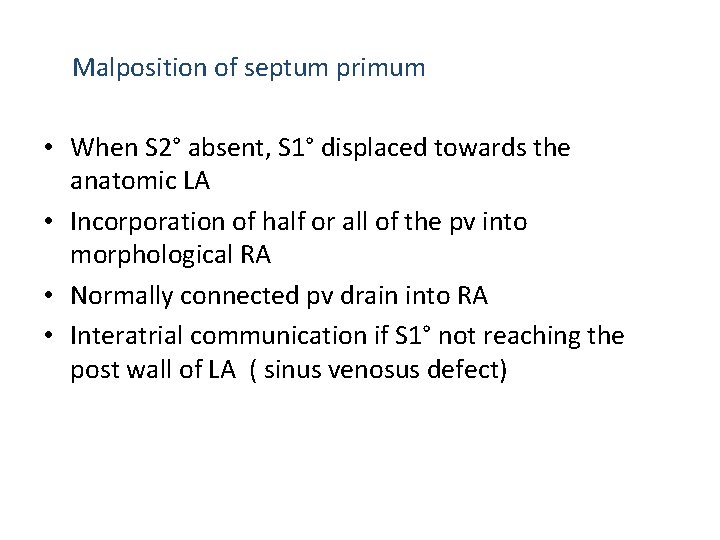
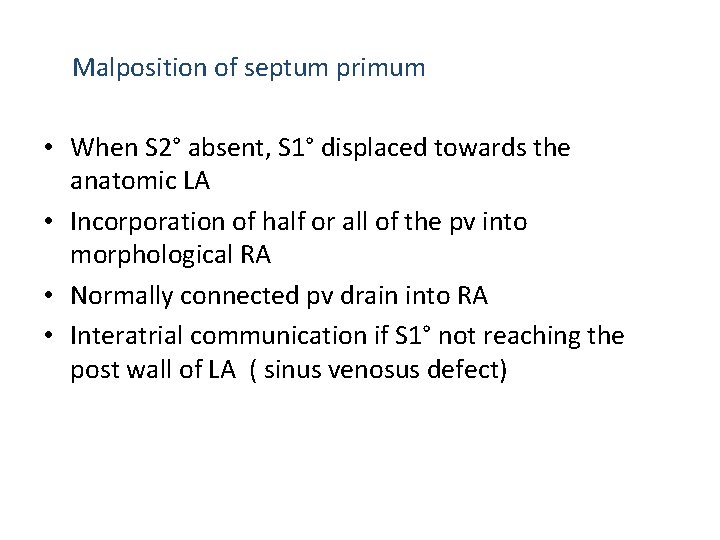
Malposition of septum primum • When S 2° absent, S 1° displaced towards the anatomic LA • Incorporation of half or all of the pv into morphological RA • Normally connected pv drain into RA • Interatrial communication if S 1° not reaching the post wall of LA ( sinus venosus defect)
PAPVC • Less than four pulmonary veins connected to RA or systemic vein(s) • Sex ratio is equal • Associations Asplenia and polysplenia Turner and Noonan ASD and TOF -Present in 9 % of ASDs. -Present in all cases of sinus venosus ASD Tricuspid atresia and single ventricle
PAPVC RPVs to SVC – without abn connection RPVs to IVC – more primitive anomaly LPVs IVC LPVs to LIV – veins from Lt upper lobe or whole Lt lung connect to LIV via vertical vein/ LSVC • Uncommon sites of PAPVC of LPVs to coronary sinus, Rt SVC, Lt subclavian , azygos vein • •
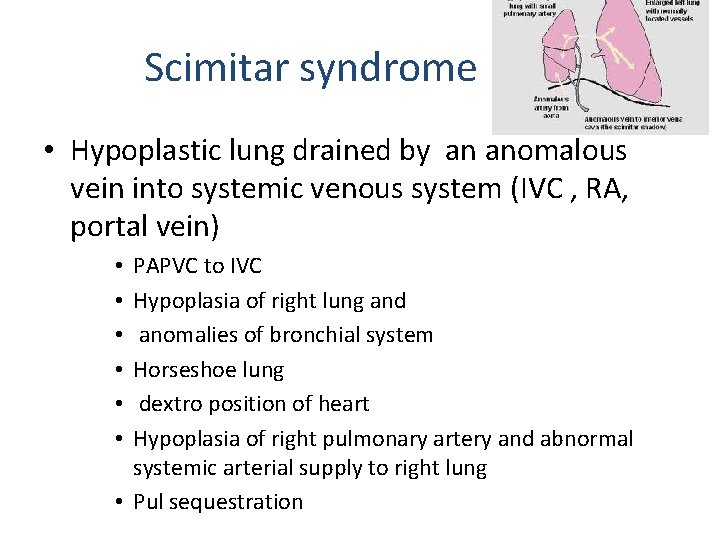
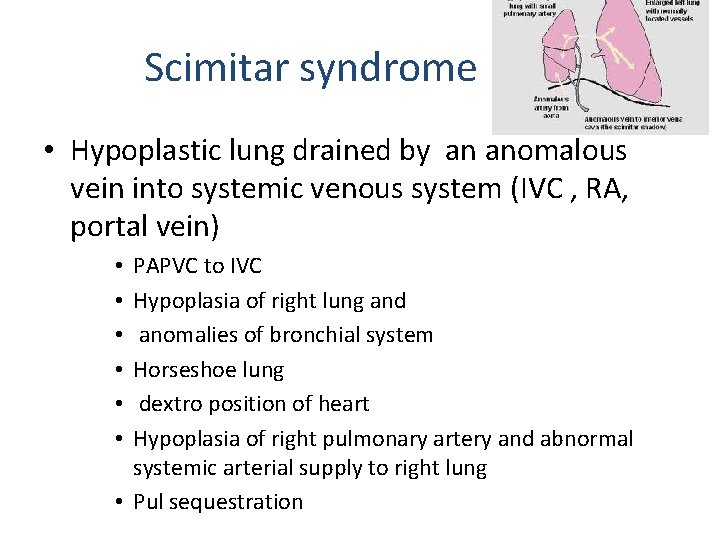
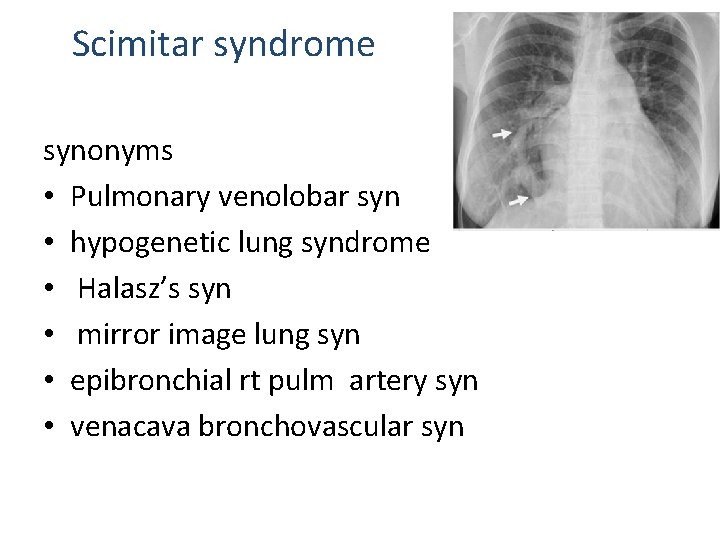
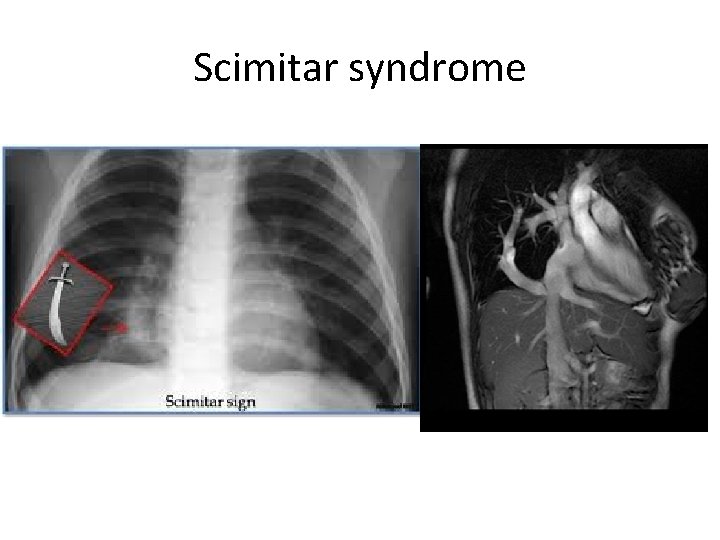
Scimitar syndrome • Hypoplastic lung drained by an anomalous vein into systemic venous system (IVC , RA, portal vein) PAPVC to IVC Hypoplasia of right lung and anomalies of bronchial system Horseshoe lung dextro position of heart Hypoplasia of right pulmonary artery and abnormal systemic arterial supply to right lung • Pul sequestration • • •
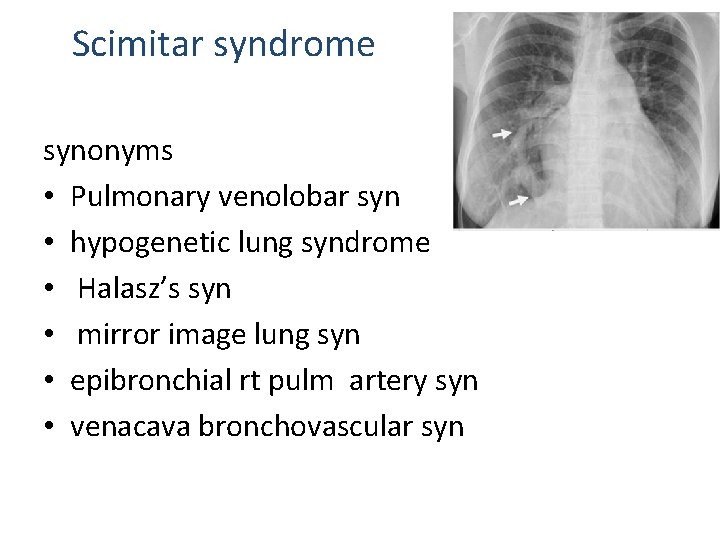
Scimitar syndrome synonyms • Pulmonary venolobar syn • hypogenetic lung syndrome • Halasz’s syn • mirror image lung syn • epibronchial rt pulm artery syn • venacava bronchovascular syn
Associations • • • CHD- ASD, VSD, TOF, PDA Ipsilateral diaphragmatic anomalies Localised bronchiectasis Vertebral anomalies Genitourinary tract abn
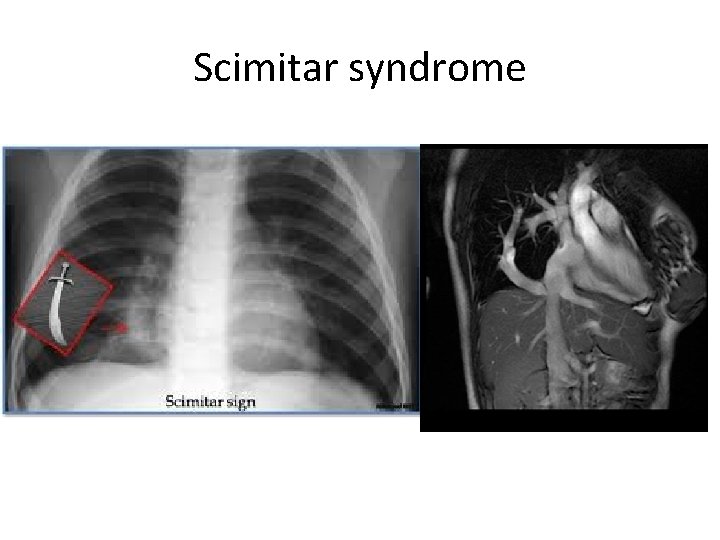
Scimitar syndrome
Treatment • Surgical correction – sig L R shunting , PHTN • Interatrial baffle to redirect pv retrn to LA • Anomalous vein replanted directly into LA
Physiology • • • PAPVC with intact IAS Single pv – anomalous bld flow 20 -25% TPBF RA pressure < LA pressure All but one pv – 80% TPBF ; phys & CF comparable with TAPVC PAPVC with ASD PBF: SBF - 3. 5: 1 Bld from both lungs drained anomalously Preferential shunting from rt lung in ASD more- proximity of rt pulm venous orifices to ASD
Clinical features • Cyanosis uncommon in childhood • Cyanosis during 3 rd & 4 th decades – changes in the pulmonary vascular bed, pulmonary HTN, increasing R L shunt
ECG • r. R’ , r. SR’ pattern • Peaked p , RVH – older patients with PHTN • CXR - increased pulmonary bld flow - RV dilation • Dilation of lower portion of SVC • Azygos vein- rounded bulge in rt sup mediastinum at rt heart border • LIV – snowman appearance of the mediastinum
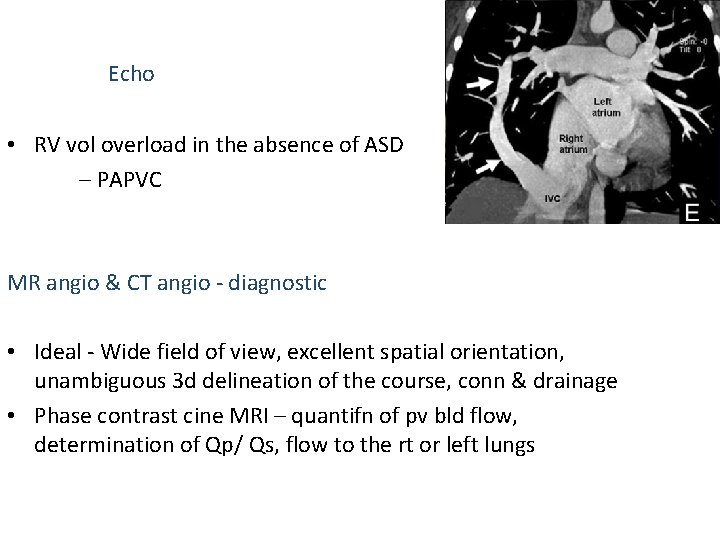
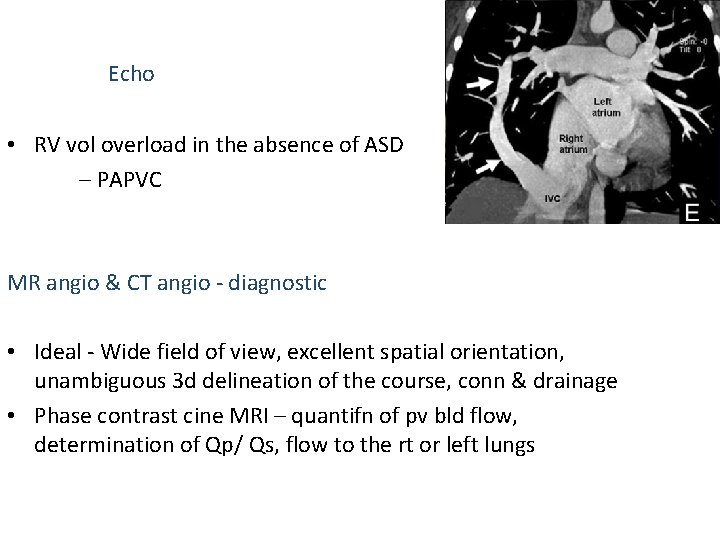
Echo • RV vol overload in the absence of ASD – PAPVC MR angio & CT angio - diagnostic • Ideal - Wide field of view, excellent spatial orientation, unambiguous 3 d delineation of the course, conn & drainage • Phase contrast cine MRI – quantifn of pv bld flow, determination of Qp/ Qs, flow to the rt or left lungs
Cardiac catheterization • Inability to pass Catheter from RA to LA or a difference between RA pressure and pulmonary wedge pressure – s/o PAPVC with intact IAS • Selective pulmonary angiography shows the anomalous pulmonary vein in levophase.
• Management • Indications for surgery– Qp/Qs more than 2: 1 – Scimitar syndrome • Timing- 2 to 5 years
Sinus venosus defect • Atrial level shunt • Deficiency of common wall between Rt SVC & RUPV & RLPV • Unroofing of PV into SVC or RA • Closure of defect between svc & rpv • Enlargement of interatrial communication& baffling rpvs to LA via enlarged comm used for rt atrial sv defects
TAPVC • TAPVC - all four pulmonary veins drain directly or indirectly into the right atrium • • • INCIDENCE- rare ( 4/1000 cases) 1. 5 - 3% of CHDs no sex predliction (males in TAPVC to portal vein) Asplenia, polysplenia , cat’s eye syndrome ASD/ PFO necessory to sustain life
• DARLING’s classification type 1 - conn at supracardiac level type 2 - at cardiac level ( coronary sinus) type 3 - at infracardiac level type 4 - at two /> of the above levels • SMITH classification supracardiac ( without pul ven obstruction) Infradiaphragmatic(with pul ven obstruction) • Burroughs Edwards classification Long, intermediate, short
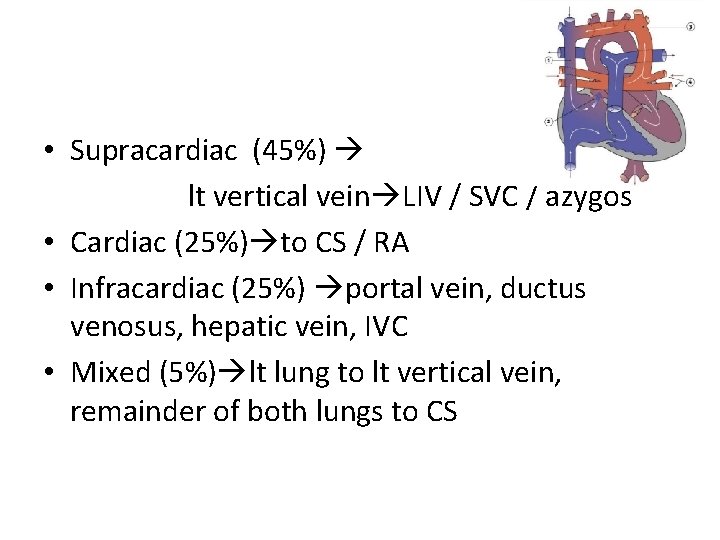
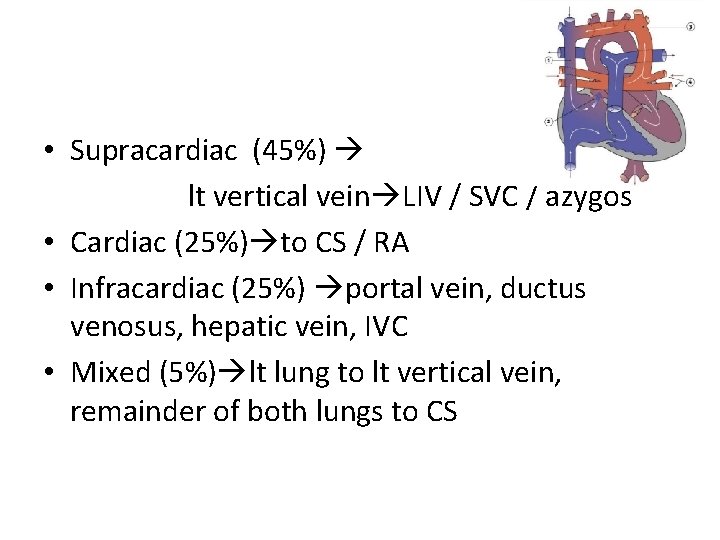
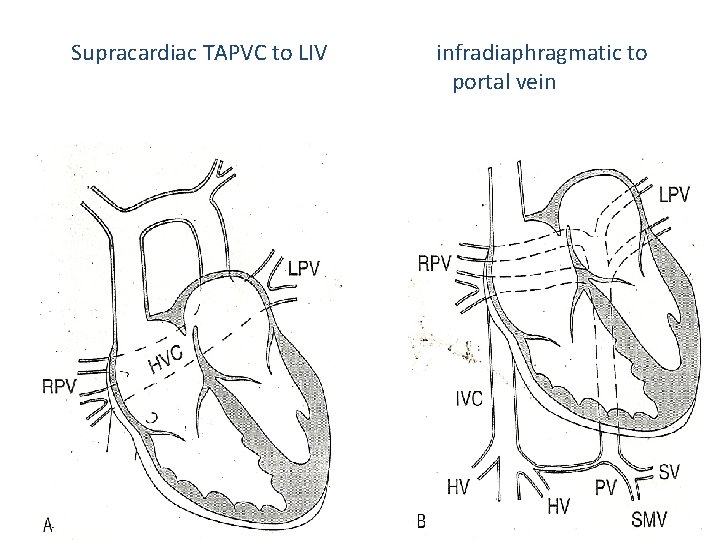
• Supracardiac (45%) lt vertical vein LIV / SVC / azygos • Cardiac (25%) to CS / RA • Infracardiac (25%) portal vein, ductus venosus, hepatic vein, IVC • Mixed (5%) lt lung to lt vertical vein, remainder of both lungs to CS
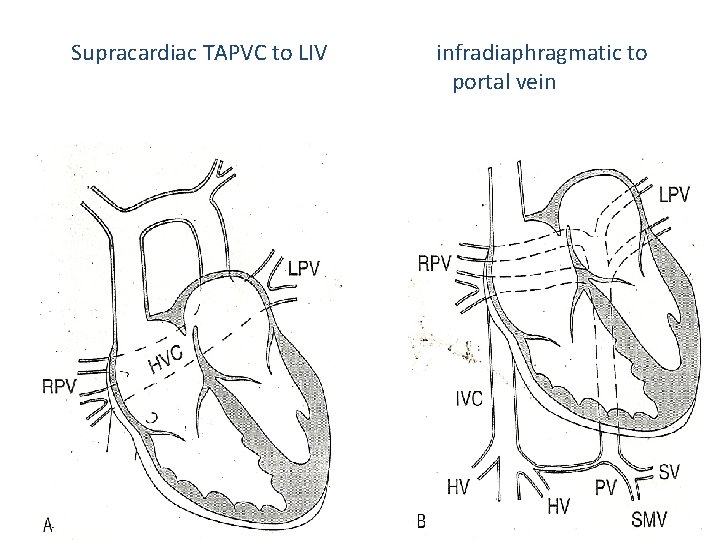
Supracardiac TAPVC to LIV infradiaphragmatic to portal vein
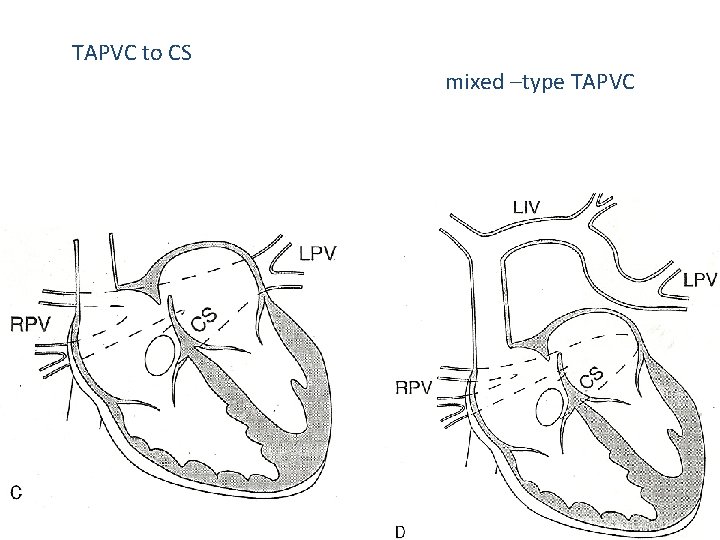
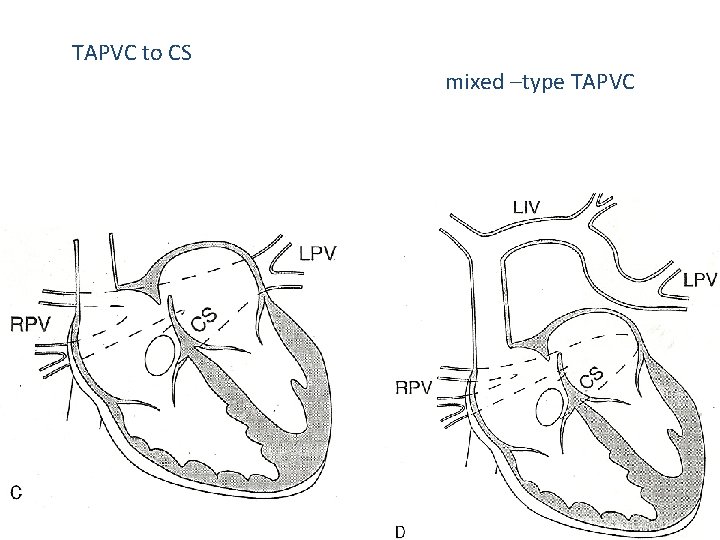
TAPVC to CS mixed –type TAPVC
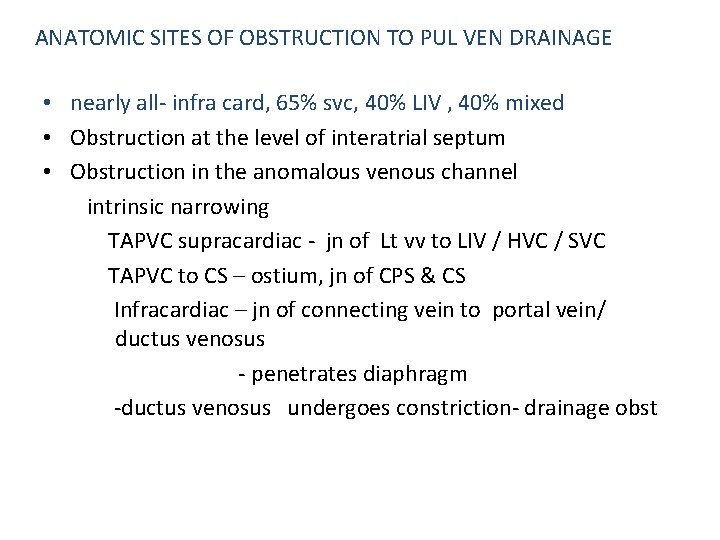
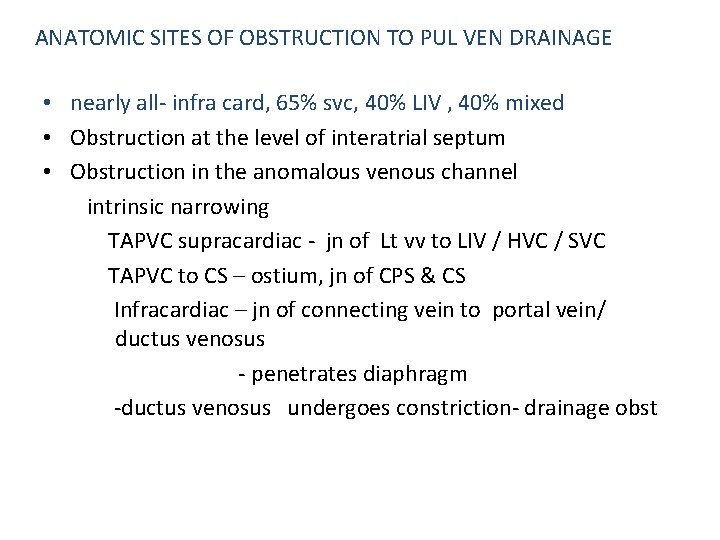
ANATOMIC SITES OF OBSTRUCTION TO PUL VEN DRAINAGE • nearly all- infra card, 65% svc, 40% LIV , 40% mixed • Obstruction at the level of interatrial septum • Obstruction in the anomalous venous channel intrinsic narrowing TAPVC supracardiac - jn of Lt vv to LIV / HVC / SVC TAPVC to CS – ostium, jn of CPS & CS Infracardiac – jn of connecting vein to portal vein/ ductus venosus - penetrates diaphragm -ductus venosus undergoes constriction- drainage obst
extrinsic pressure - vertical vein to LIV passing bet L main pul art & L main stem bronchus – vascular vise - TAPVC to SVC - RPA & trachea -to portal vein- hepatic sinusoids interposed, results in inc resistance to venous return
TAPVC without pv obstruction • The mixed venous pool receives 3 -5 parts of fully saturated blood for each part of systemic venous blood • RA saturation ≥ 90% • Progr RV hypertrophy & dilation • TAPVC with pvo • Elevated pressure in the pv channels freely transmitted to capillary bed • Osmotic pressure of blood > hydrostatic pressure in the capillaries pulm edema • RV vol & pr overload, decreased LV vol, low systemic output
Hemodynamic considerations • Severe pv obstrn – pv HTN – pulm lymphangiectasia • LA/ LV small – lack of pv drainage to LA • Narrowing of aortic isthmus & Co. A
After birth • Pv severely obstructed, pulm bld flow reduced & if systemic flow is maintained, pulm to syst flow ratio decreases, arterial O 2 sat falls • Unobstructed pv – as PVR falls, pulm bld flow increased – high pulm to syst flow ratios – high syst o 2 saturations
PVR & pulm bld flow • Fall in PVR -↑pulm bld flow - ↑flow in PVs- if veins obstructed, pulm venous pressure elevated • If plasma oncotic pressure exceeded , transudation of fluid - pulm oedema
Role of foramen ovale • In the absence of pulmonary venous return to LA, RA pr > LA pr, R L flow thru foramen ovale • Severe obstruction – large foramen ovaleprovide adequate systemic bld flow without significant elevation of RA pressure • Restriction of foramen ovale with moderate – no PVO
Role of ductus arteriosus • As PVR high, bld shunts from PA Ao thru ductus ↓flow thru’ pulmonary circulation • Pulm venous flow ↓, pulm venous pr ↓, less likely pulm edema • Ductus closes – R L shunt eliminated – PA pr & lung perfusion ↑- pulm venous flow, pr & pulm edema ↑
Role of ductus venosus • Pulm venous bld returning to portal vein IVC • Pulm venous HTN & pulm edema will not dev • Closure of ductus flow thru’ hepatic microcirculation portal , pv pressure ↑pulm edema
Effect of feeding • ↑gastrointestinal & portal flow • Portal & pulm venous pr will rise – pulm edema aggravated
Effect of PGE 1 infusion • -Dilating the ductus - ↑ R L shunt , ↑ cyanosis - Pulm vasodilatation, ↑pulm bld flow, ↑pulm edema, improve cyanosis • Beneficial – infra diaphragmatic • Relaxes smooth muscle in ductus venosus & relieves constriction- lower the pulm venous pressure – improvement of pulm edema
Natural history • • • Assymptomatic at birth 56% syptomatic at 1 st month of life Failure at 6 months of age Severe obstrn- pulm edema 1 st few hrs Cyanosis mild, more with failure & pulm vascular changes
Natural history • Death – 1 st few wks or months of life in most neonates • 90% death – 1 st year of life • Survivors of 1 st few wks of life – incr pulm bld flow mild cyanosis, PHTN • 50% survive beyond 3/12 • 20% surviving the 1 st yr • Median survival 3 wks (obst) , 2. 5 months in (non obstr) • Infracardiac- worse prognosis- 3 wks survival
• Pulses – weak, BP reduced, small pulse pr • Prominent RV heave • Loud s 1, s 2 wide fixed split , loud p 2, s 3 at apex, s 4 frequently in older patients • Cont mr if Lt vertical vein obstructed • 2/6 soft blowing systolic mr pulm area ( turbulence in the pulm outflow tract) • TR murmur at LLSB
• ECG- RA enlargement , RAD, RVH • • CXR- RA, RV enlarged PA segment prominent Figure of 8 or snowman – TAPVC to LIV Lung fields reflect increased pulm bld flow
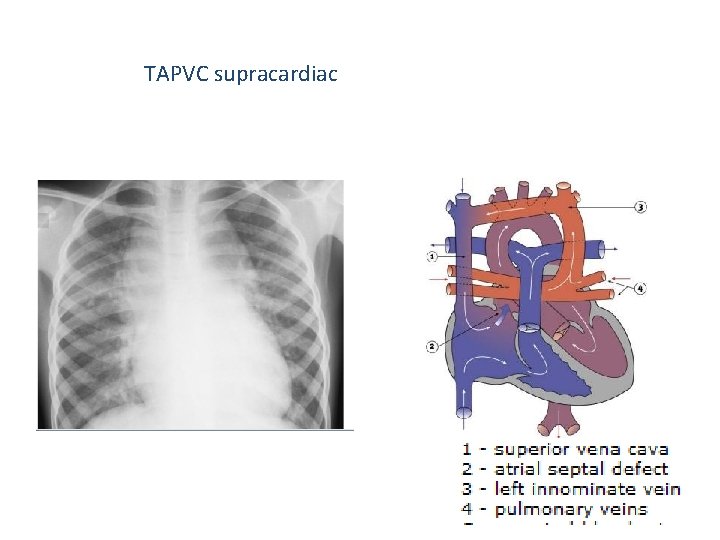
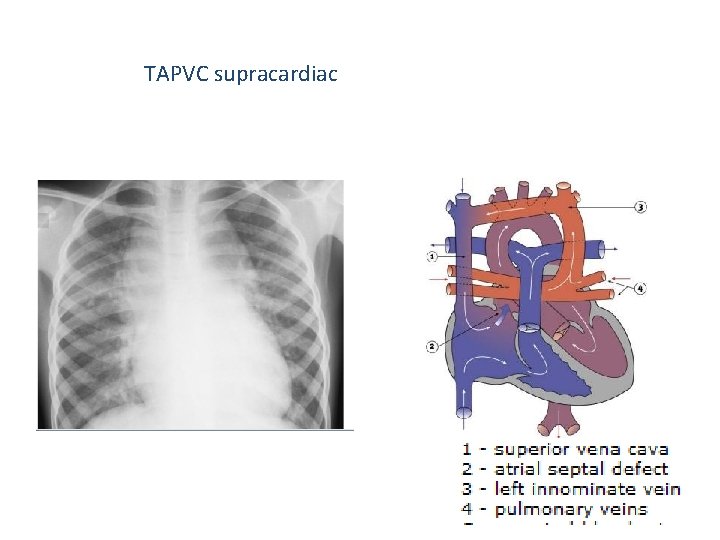
TAPVC supracardiac
Echo PVs are farthest from the transducer (most posterior structures) • • RA/RV vol overload LV vol decreased Pulm venous confluence & individual pv imaged Cs dilated, if TAPVC conn to cs
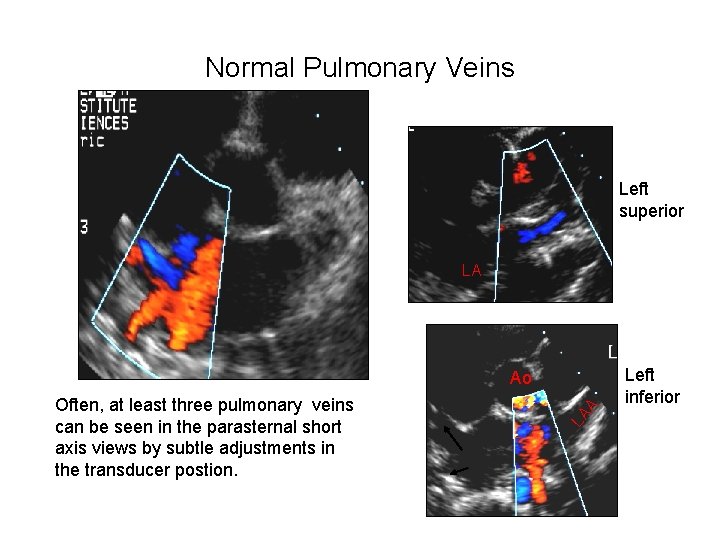
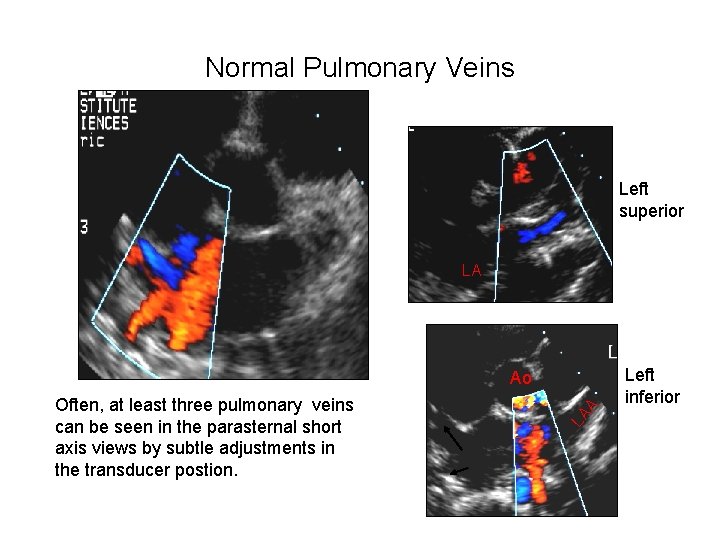
Normal Pulmonary Veins Left superior LA LA Often, at least three pulmonary veins can be seen in the parasternal short axis views by subtle adjustments in the transducer postion. A Ao Left inferior

Suspecting TAPVC – dilated RA, RV - Dilated SVC(supracardiac)
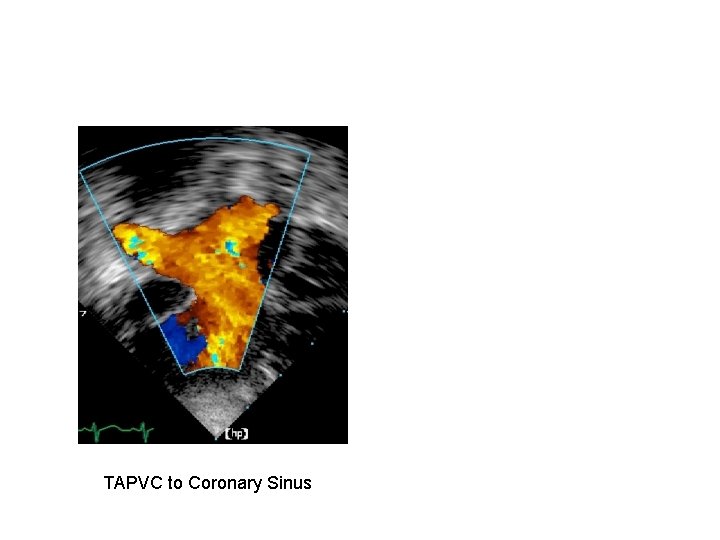
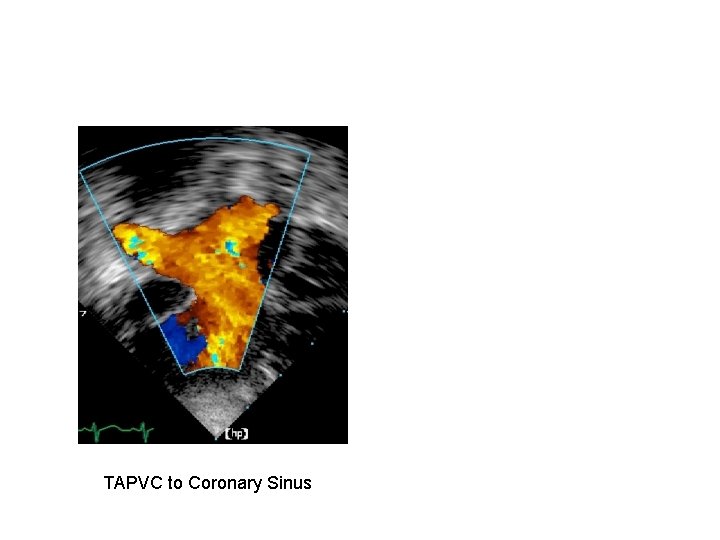
TAPVC to Coronary Sinus
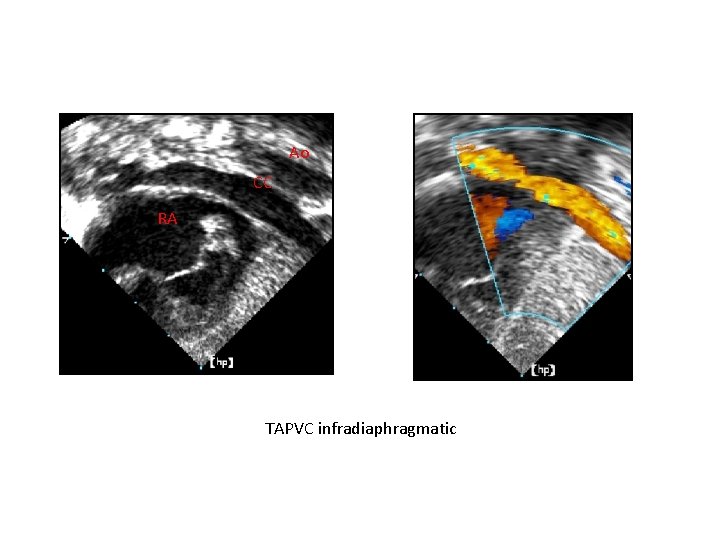
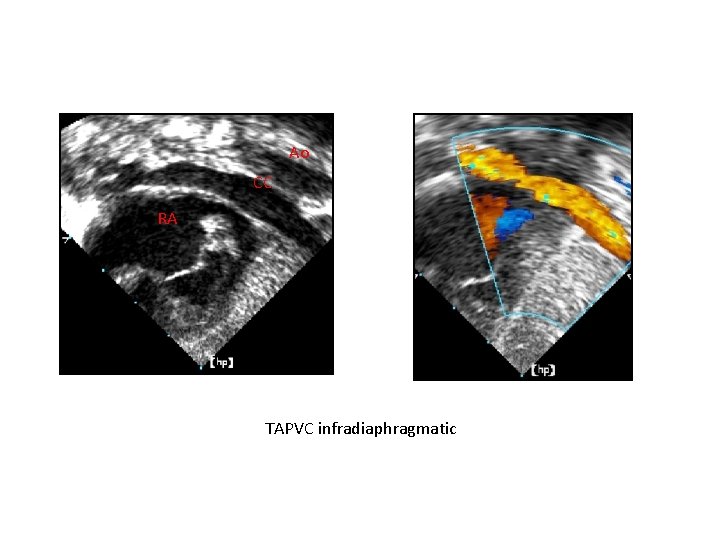
Ao CC RA TAPVC infradiaphragmatic
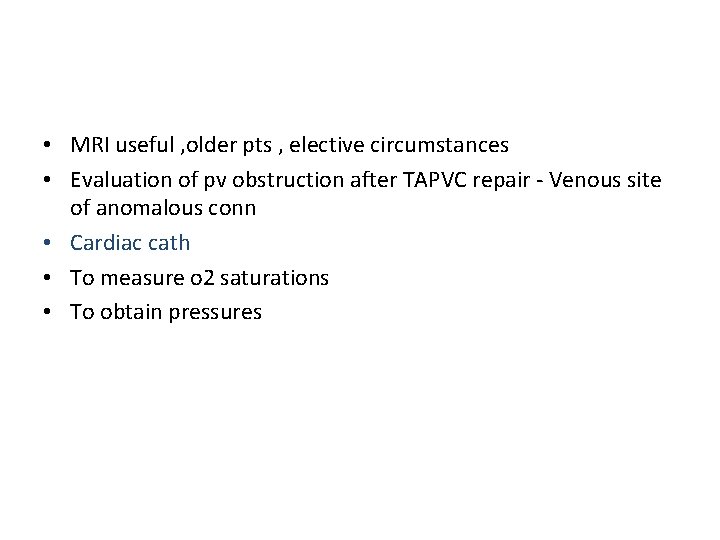
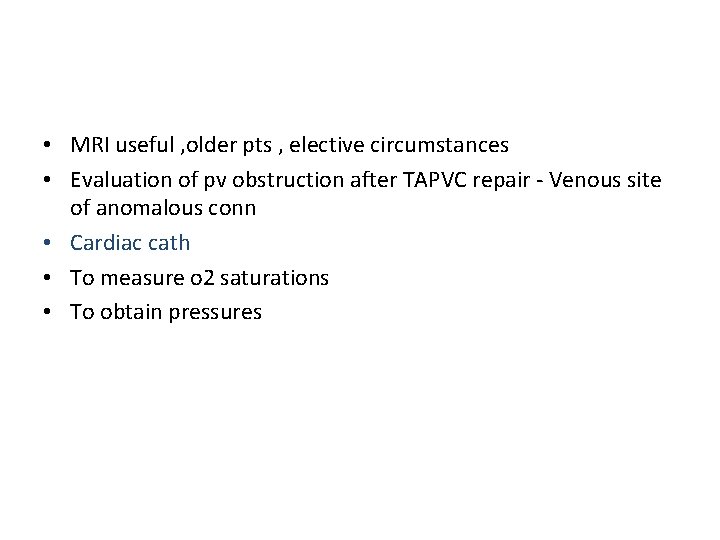
• MRI useful , older pts , elective circumstances • Evaluation of pv obstruction after TAPVC repair - Venous site of anomalous conn • Cardiac cath • To measure o 2 saturations • To obtain pressures
• When pv trunk enters vv/ svc , saturation higher in svc • Infradiaphragmatic – o 2 saturation in systemitc veins • To cs – diff small
Principles of treatment • With obstruction – urgent surgery • Lesser degrees of obstruction, failure several wks / months after birth - can be delayed to beyond 12 - 18 months • PGE 1 – pv drainage to portal vein
Treatment • Corrective surgery as soon as possible • Balloon atrial septostomy, blade atrial septostomy – palliative procedures • TAPVC to cs- common wall of cs & LA excised thru’ rt atriotomy approach drainage pv flow into LA , orifice of cs closed by direct suture/ patch, ASD closed
• TAPVC to LIV – creation of a large side to side anastomosis between LA & pv confluence, ASD closure • Prognosis untreated • Size of IAS defect, obstructive lesions in the anomalous venous pathways, state of pulm vascular bed
Stenosis of cpv • Cor Triatum- pv enter an accessory chamber that joins the LA thru’ a narrow opening • Accessory chamber communicate with RA • Cor triatum sinister - Failure of incorporation of cpv into LA - most accepted theory • Cor triatum dexter- persistence of rt valve of sinus venosus
Anatomic classification of cor triatum • I. accessory atrial chamber receives all pvs, comm with LA A. No other conn- classic cortriatum B. other ano conn 1. to RA directly 2. with TAPVC • II. accessory atrial chamber receives all pvs, doesn’t comm with LA A. ano conn to RA directly B. with TAPVC • III. Subtotal cor triatritum A. Accessory atrial chamber receives part of pvs & conn to LA 1. remaining pv conn normally 2. remaining pv conn anomalously B. accessory atrial chamber receives part of pv, conn to RA 1. remaining pvs conn normally
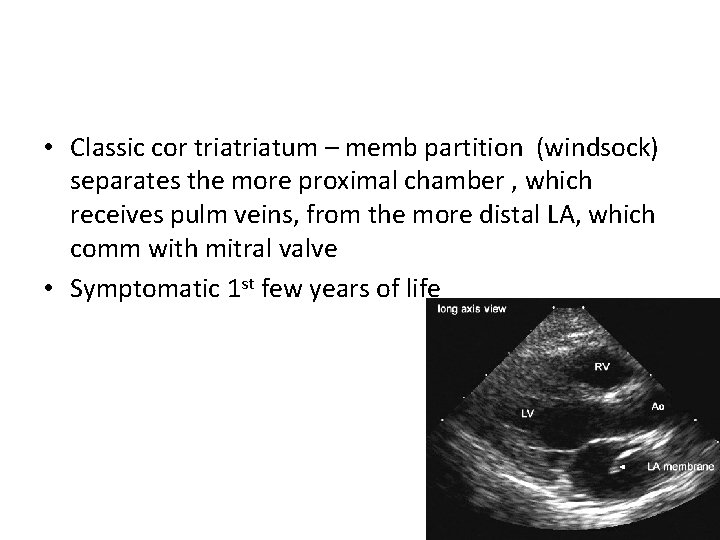
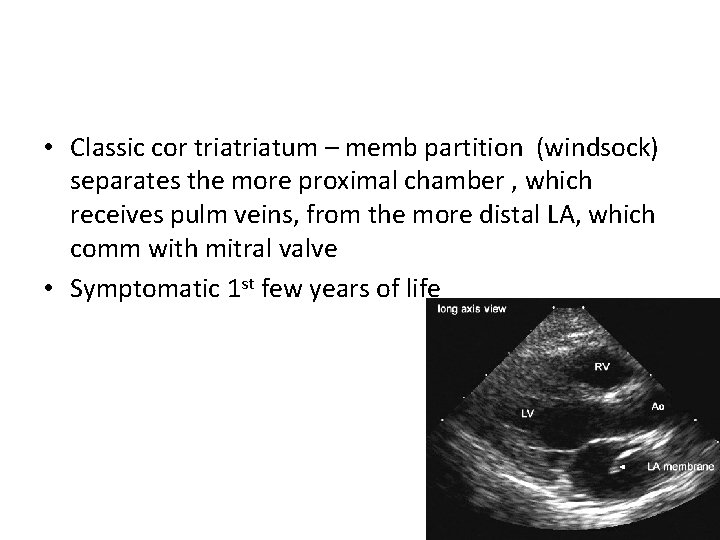
• Classic cor triatum – memb partition (windsock) separates the more proximal chamber , which receives pulm veins, from the more distal LA, which comm with mitral valve • Symptomatic 1 st few years of life

Cor triatum sinistrum • Incidence - 0. 1 0. 4% • No sex difference • Clinical features dep on size of opening in the septum • Incidental detection • Symptomatic if obstn severe/ dev of MR , AF
Cor triatum dextrum • Asymptomatic • Symptomatic – degree of septation RA - size of sinoatrial orifice • Diagnosis – echo - Cardiac MRI -angio • Sympt pts – control of fluid retention, atrial arrhythmias • Balloon septostomy of atrial membrane • Surgical resection of accessory membrane
Abnormal absorption of cpv into LA • • Localised stenosis of pv Hypoplasia of individual pv Respiratory symptoms, RHF , failure to thrive, hemoptysis Reanastomosis of stenotic pv into LA
Thank you
Abnormal systemic venous connections
Venous system 3 basic venous system Cardinal veins- SVC & IVC Umblical , vitelline, omphalomesentriccarry bld from placenta , yolksac & intestine Pulmonary veins- returning bld from lungs

VENOUS SYSTEM
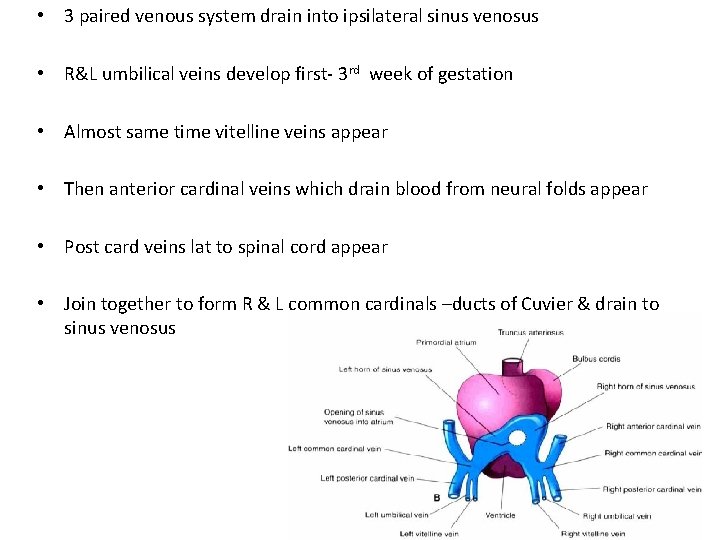
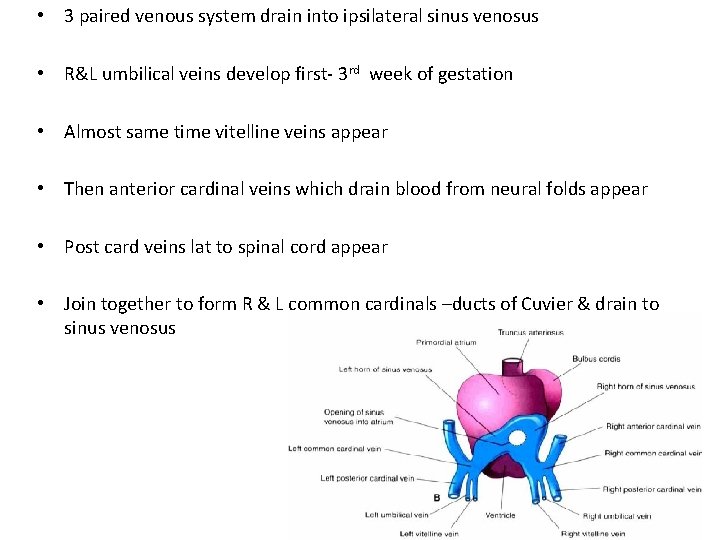
• 3 paired venous system drain into ipsilateral sinus venosus • R&L umbilical veins develop first- 3 rd week of gestation • Almost same time vitelline veins appear • Then anterior cardinal veins which drain blood from neural folds appear • Post card veins lat to spinal cord appear • Join together to form R & L common cardinals –ducts of Cuvier & drain to sinus venosus
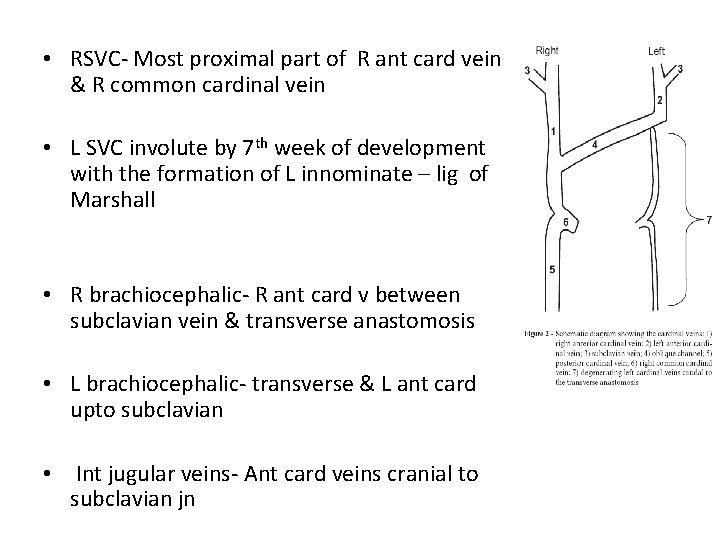
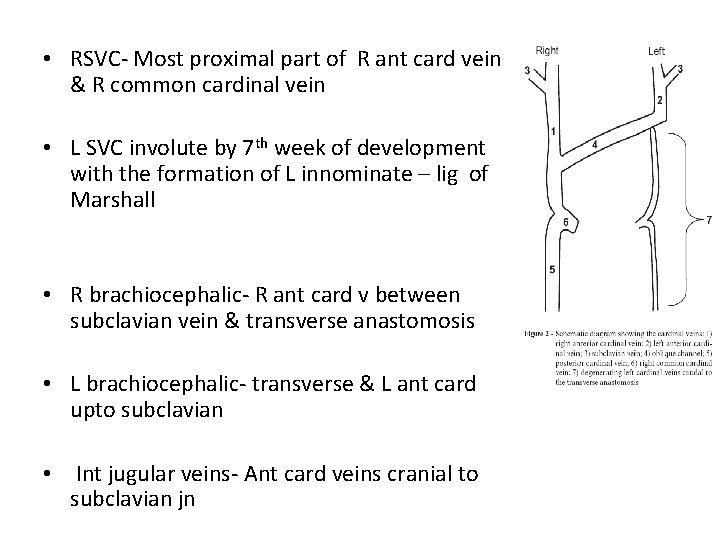
• RSVC- Most proximal part of R ant card vein & R common cardinal vein • L SVC involute by 7 th week of development with the formation of L innominate – lig of Marshall • R brachiocephalic- R ant card v between subclavian vein & transverse anastomosis • L brachiocephalic- transverse & L ant card upto subclavian • Int jugular veins- Ant card veins cranial to subclavian jn
Coronary sinus • Lt horn of sinus venosus & adjacent part of CCV - receive cardiac veins & form coronary sinus • Orifice always in the anatomical RA • Persistant LSVC always continues with CS, since Lt CCV is part of CS & LSVC
DVT OF IVC & PORTALS

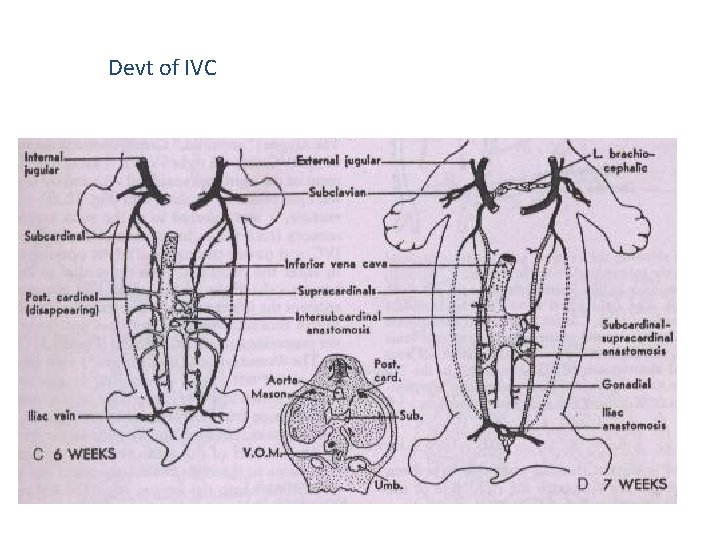
Devt of IVC • 5 diff venous systems • Posterior cardinal veins • Subcardinal sinus – new unpaired venous channel develops, hepatic segment IVC • 7 th wk- new venous channel connects the subcardinal sinus with confluence of hepatic veins & ductus venosus • Postr card veins involute, supracardinals appear, which connects subcardinal sinus with cephalic remnant of post cardinal via azygos & hemiazygos • Infra renal portion of rt supracardinal infra renal portion of IVC
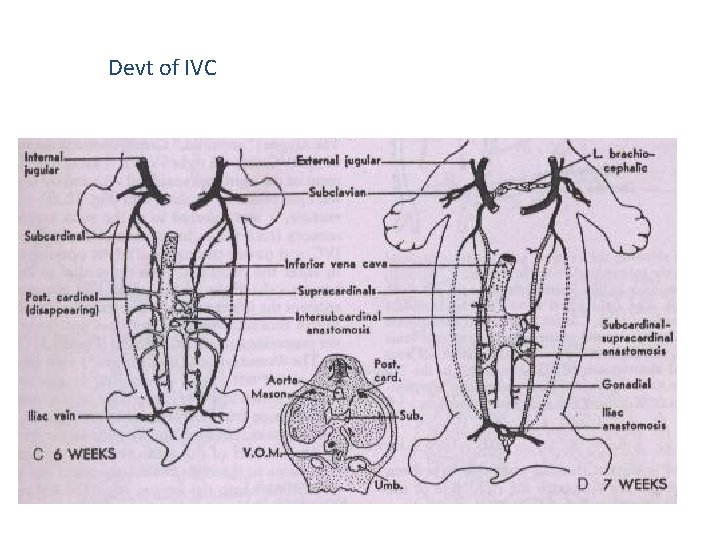
Devt of IVC
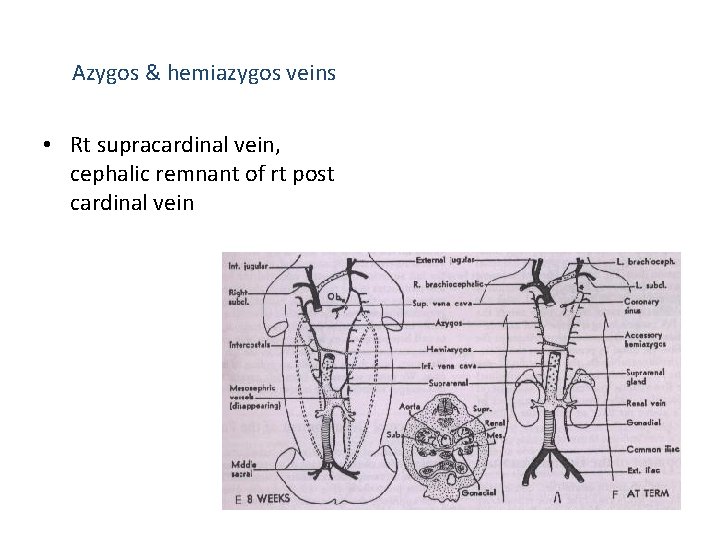
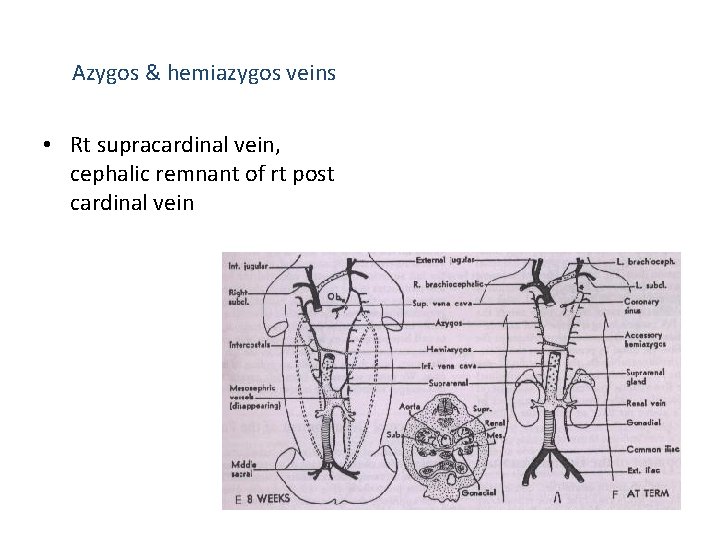
Azygos & hemiazygos veins • Rt supracardinal vein, cephalic remnant of rt post cardinal vein
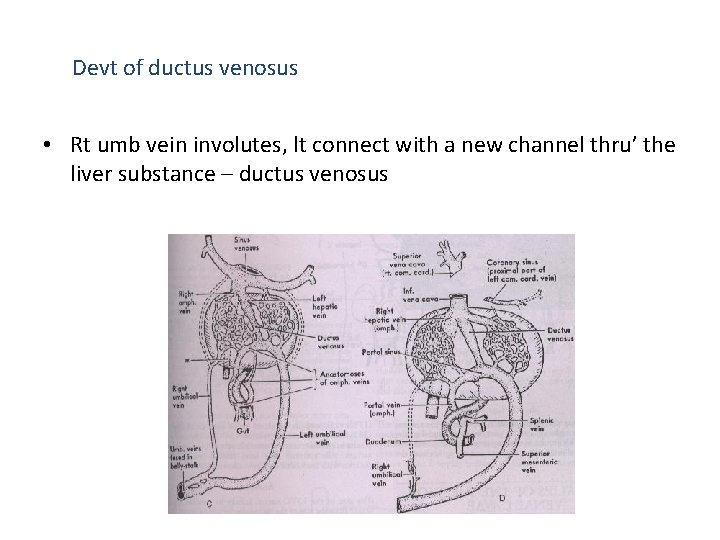
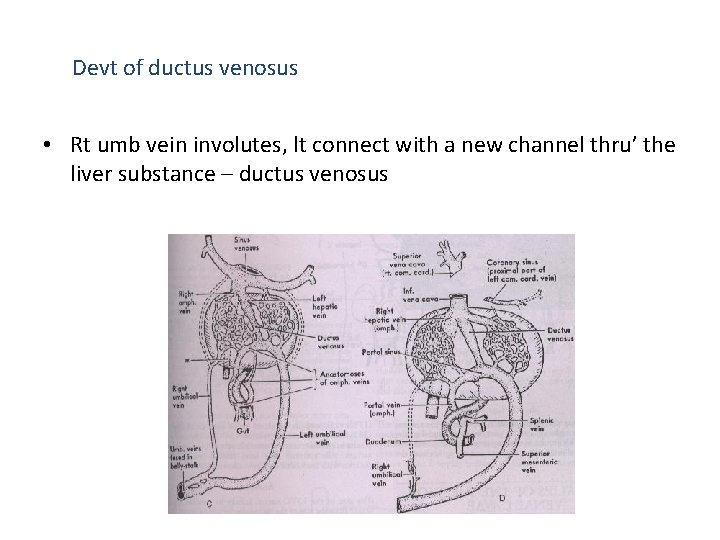
Devt of ductus venosus • Rt umb vein involutes, lt connect with a new channel thru’ the liver substance – ductus venosus
Devt of portal vein • Vitelline veins of the primitive gut become confluent with rt & lt omphalomescenteric veins sinus venosus • Omphalic part disappears, mesenteric part grows, anastomose • Lt mesenteric vein involute cephalad to the anastomosis • Rt – caudal to the anastomosis
Anomalies of SVC B/L SVC with normal drainage to RA • Persistence of LSVC - failure of Lt ant & CCV to involute Drains to RA thru’ CS (92%) Drains to LA - unroofed CS Absent RSVC in visceroatrial situs solitus (0. 07 -0. 13%) • LSVC draining to RA via the CS B/L SVC with unroofed CS • LSVC drains to LA • RA orifice of CS enlarged , allows inter atrial communication Left atrial / B/L drainage of RSVC • Sinus venosus defect of SVC type a/w atresia of Rt SVC orifice
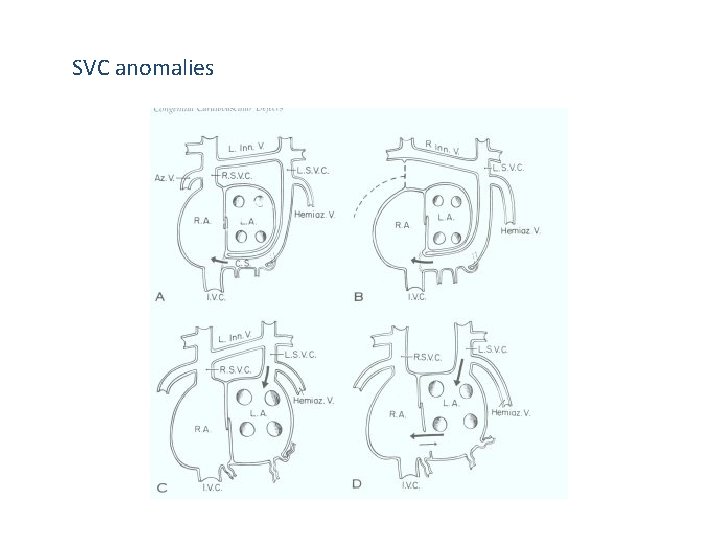
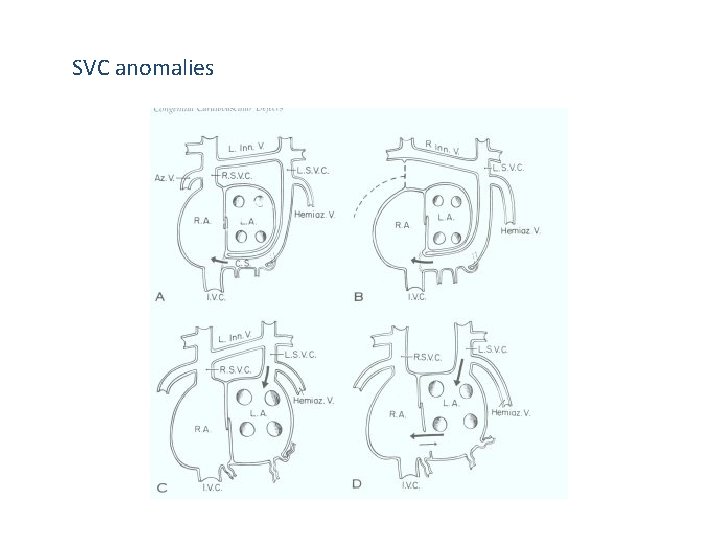
SVC anomalies
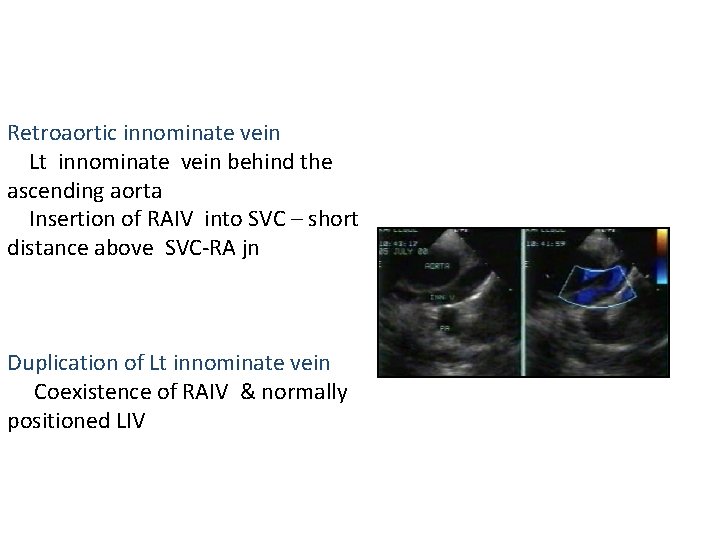
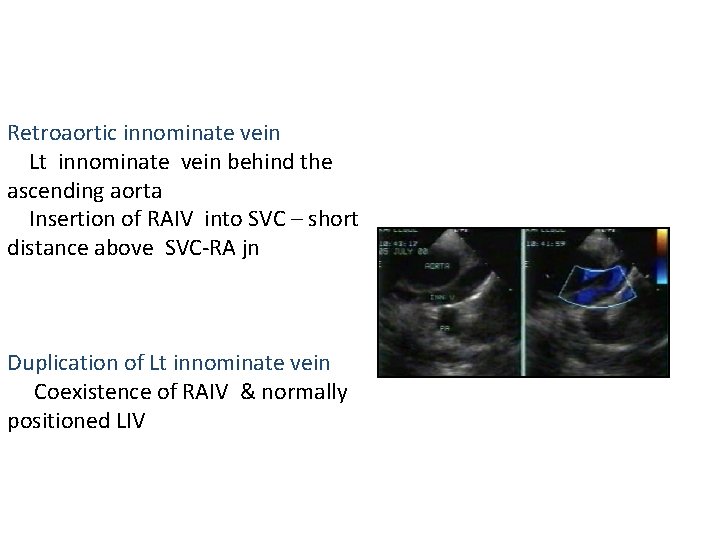
Retroaortic innominate vein Lt innominate vein behind the ascending aorta Insertion of RAIV into SVC – short distance above SVC-RA jn Duplication of Lt innominate vein Coexistence of RAIV & normally positioned LIV
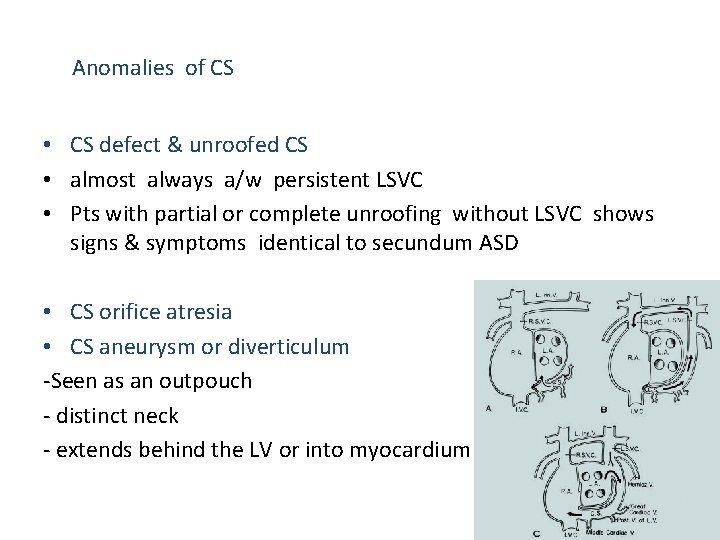
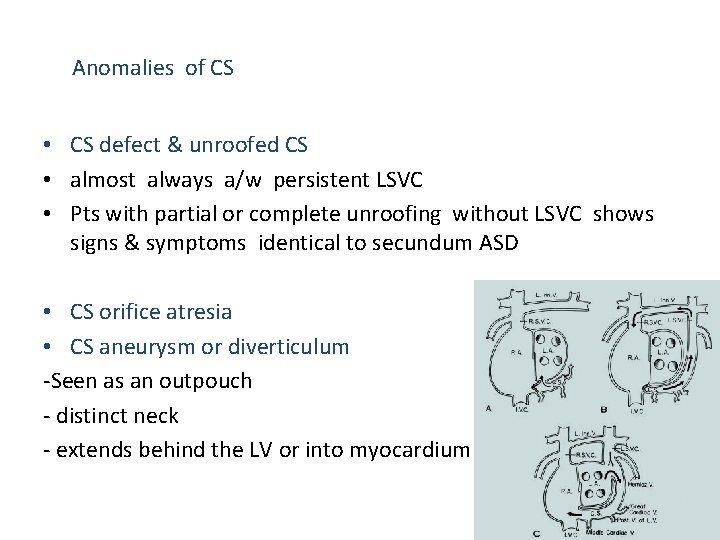
Anomalies of CS • CS defect & unroofed CS • almost always a/w persistent LSVC • Pts with partial or complete unroofing without LSVC shows signs & symptoms identical to secundum ASD • CS orifice atresia • CS aneurysm or diverticulum -Seen as an outpouch - distinct neck - extends behind the LV or into myocardium
Anomalies of IVC • Interrupted IVC – absence of hepatic segment of IVC with azygos continuation into Rt or Lt SVC - When renal to hepatic segment of IVC is absent, no IVC is seen below the liver - Azygos vein is enlarged , followed cranially until its connection with SVC • B/L IVC - B/L suprahepatic IVC, B/L infrarenal IVC • IVC drainage to LA - eustachian valve persist - patent foramen ovale
Anomalies of ductus venosus • Anomalous termination of umbilical veins & absent ductus venosus - rare, donot produce symptoms • Post natal persistence of ductus venosus • Persistent valves of sinus venosus Results in obstruction of blood flow into the RA or thru’ the RA
Significance of Common Venous Anomalies • Prior knowledge helps planning of interventions and diagnostic cath procedures – E. g. Pulmonary valve stenosis in IVC interruption: Elective Jugular or subclavian approach – LSVC to coronary sinus: pacemaker implantation on the right side preferred
Systemic Venous Anomalies That Result in Cyanosis • • LSVC to LA (absent coronary sinus) RSVC to LA IVC to LA Total anomalous systemic venous drainage
 Cortriatum
Cortriatum Robert sarv pulm
Robert sarv pulm Total anomalous pulmonary venous return
Total anomalous pulmonary venous return Cephalic vein
Cephalic vein What do dolly grips do
What do dolly grips do Dolly foundation
Dolly foundation Prednosti kloniranja
Prednosti kloniranja Dolly krishnaswamy
Dolly krishnaswamy Clonazione di dolly
Clonazione di dolly Paper
Paper Dolly pull off test
Dolly pull off test Dolly grip salary
Dolly grip salary Brebie dolly clonage
Brebie dolly clonage Isabelle boulay dolly parton
Isabelle boulay dolly parton What is a crab dolly? when is it most often used?
What is a crab dolly? when is it most often used? Dolly hoist
Dolly hoist Dolly bhargava
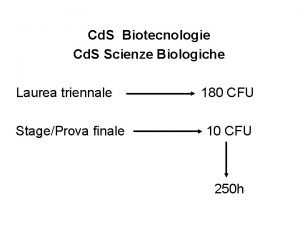
Dolly bhargava Tfa unimore
Tfa unimore Dolly in storyboard
Dolly in storyboard Biologia
Biologia Dolly busterporn
Dolly busterporn Goodfellas dolly zoom
Goodfellas dolly zoom Dolly unimore scienze naturali
Dolly unimore scienze naturali Dolly
Dolly Cừu dolly được sinh ra bằng phương pháp
Cừu dolly được sinh ra bằng phương pháp Sonny bolger
Sonny bolger Cfsv2 monthly prec anomalies
Cfsv2 monthly prec anomalies Oddball: spotting anomalies in weighted graphs
Oddball: spotting anomalies in weighted graphs Anomalies of vitellointestinal duct
Anomalies of vitellointestinal duct Modification anomalies
Modification anomalies Disease penis
Disease penis Biolateral macostomia
Biolateral macostomia Convex population pyramid
Convex population pyramid Moral anomalies by raffaele garofalo
Moral anomalies by raffaele garofalo Mcgovern nipple
Mcgovern nipple Attention anomalies finance
Attention anomalies finance Elliptocytosis
Elliptocytosis Spina bifida
Spina bifida Anomalies du rcf pendant le travail
Anomalies du rcf pendant le travail Défauts et anomalies du bois
Défauts et anomalies du bois Most common congenital anomalies
Most common congenital anomalies Ralentissement variable atypique
Ralentissement variable atypique Data redundancy and update anomalies
Data redundancy and update anomalies Kode icd palatoschisis
Kode icd palatoschisis Database anomalies
Database anomalies Andrea frazzini aqr
Andrea frazzini aqr Anomali refraksi
Anomali refraksi Matthew chapter 8
Matthew chapter 8 Major beliefs in buddhism
Major beliefs in buddhism Tisson mathew
Tisson mathew Astra greek hacker
Astra greek hacker Matthew 5 nkjv
Matthew 5 nkjv Avin mathew
Avin mathew Mathew 13:13
Mathew 13:13 Bessie mathew
Bessie mathew Mathew duncan method
Mathew duncan method Fs71i
Fs71i Enganche de mathieu
Enganche de mathieu 22*46
22*46 Mathew pereira
Mathew pereira Mathew 17:1-8
Mathew 17:1-8 Matthew 7:28
Matthew 7:28 Introduction of dover beach
Introduction of dover beach Pediatrician job descriptions
Pediatrician job descriptions Matthew 28 19-20
Matthew 28 19-20 Benjamin matthew victor
Benjamin matthew victor Matthew 6 12
Matthew 6 12 Ee5358
Ee5358 Mattew chapter 5
Mattew chapter 5 Mathew williams md
Mathew williams md Ephesians 6:10-13 kjv
Ephesians 6:10-13 kjv Matthew 10:34
Matthew 10:34 Mk mathew
Mk mathew Matthew 17 nkjv
Matthew 17 nkjv Propchain crypto
Propchain crypto Mathew 12 36
Mathew 12 36 Mathew 24:44
Mathew 24:44 Mathew 6:25
Mathew 6:25 Mathew 26:36-44
Mathew 26:36-44 Mathew pletcher
Mathew pletcher Modified brandt andrews technique
Modified brandt andrews technique Jose manuel mathew
Jose manuel mathew Mathew 2:1-12
Mathew 2:1-12 Julie anderson mary poppins
Julie anderson mary poppins Mathews v eldridge case brief
Mathews v eldridge case brief Galavni
Galavni Matthew 28 19-20
Matthew 28 19-20