PTSD Emma Mathews Aims To increase recognition of

![What is PTSD? The American Psychiatric Association [APA], in the Diagnostic and Statistical Manual What is PTSD? The American Psychiatric Association [APA], in the Diagnostic and Statistical Manual](https://slidetodoc.com/presentation_image_h2/b0c5bf2273a11a10946a8f17702985f0/image-14.jpg)

![Situationally accessible memories… �The other set of representations are the situationally accessible memories [SAMS]. Situationally accessible memories… �The other set of representations are the situationally accessible memories [SAMS].](https://slidetodoc.com/presentation_image_h2/b0c5bf2273a11a10946a8f17702985f0/image-32.jpg)




- Slides: 64
PTSD Emma Mathews
Aims �To increase recognition of presentations and appropriate referral to services �To increase understanding of how psychological trauma can impact on students �To raise awareness of the diagnosis PTSD �To discuss implications for treatment
Examples of traumatic events �Natural disasters (e. g. earthquake) �Man-made disaster s (e. g. terrorist attacks) �Accidents (e. g. Fall, RTA, train crash, medical) �Physical assault �Robbery �Murder �Sexual assault or rape �War �Ethnic cleansing �Torture
Outcomes After Trauma �Acute Stress Disorder �PTSD �Phobias �Somatization �Depression �OCD �Suicide �Substance Abuse �Pain
Prevalence of violent crime �The police recorded 1. 2 million (1, 167, 998) violence against the person offences in the year ending March 2017, an increase of 18% compared with the year ending March 2016 (992, 246 offences): �violence without injury accounted for 41% (474, 006 offences) �violence with injury accounted for 40% (465, 765 offences) �stalking and harassment accounted for 19% (226, 754 offences) �death or serious injury – unlawful driving accounted for 0. 06% (749 offences) �homicide accounted for 0. 06% (724 offences)
Prevalence for young people �Adults aged 16 to 24 were more likely to be victims of violence (4. 1%) than those in older age groups. This was particularly pronounced for stranger violence (2. 1%) and acquaintance violence (1. 5%). �Reference: Crime survey England Wales
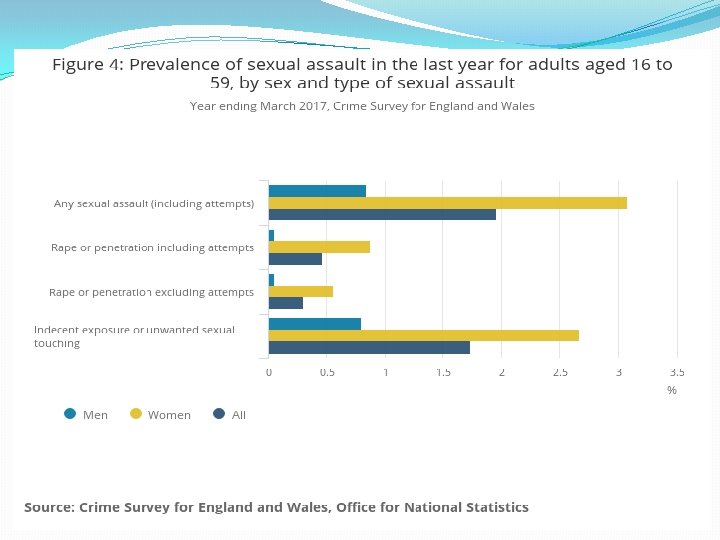
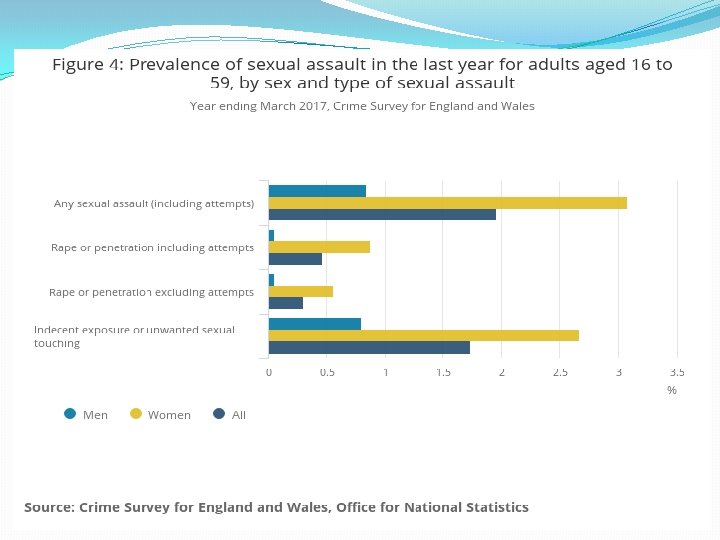
Prevalence… �An estimated 3. 1% of women (510, 000) and 0. 8% of men (138, 000) aged 16 to 59 experienced sexual assault in the last year �Students (6. 4%) were more likely to have been a victim of sexual assault in the last year than adults of other occupations.
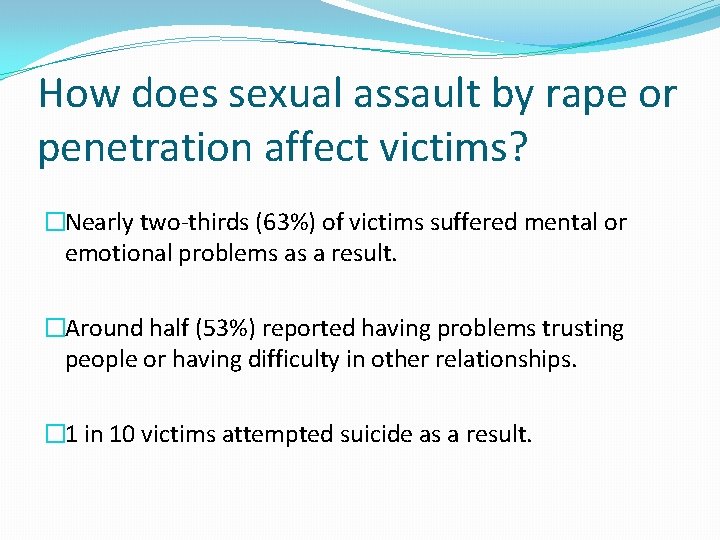
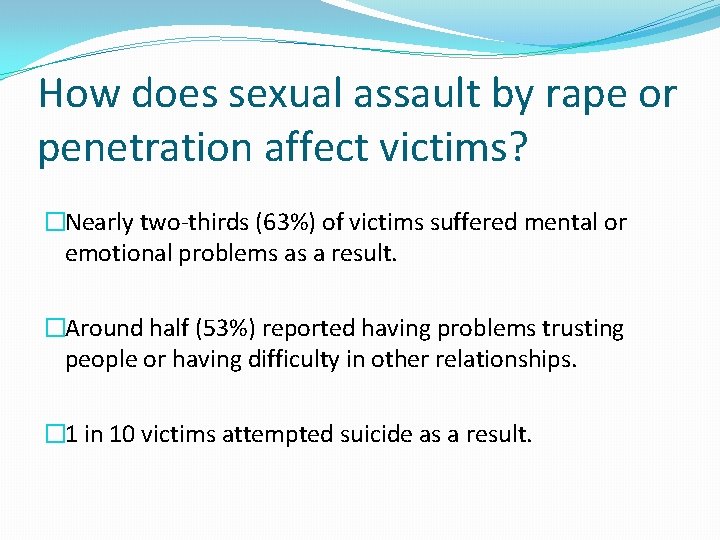
How does sexual assault by rape or penetration affect victims? �Nearly two-thirds (63%) of victims suffered mental or emotional problems as a result. �Around half (53%) reported having problems trusting people or having difficulty in other relationships. � 1 in 10 victims attempted suicide as a result.
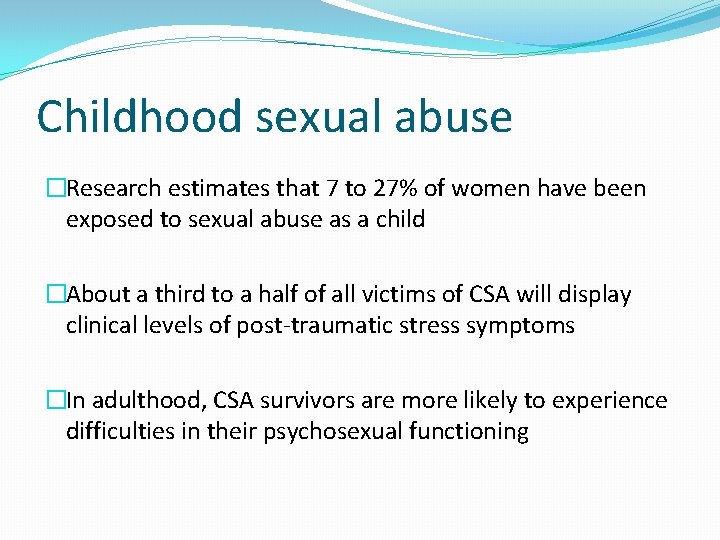
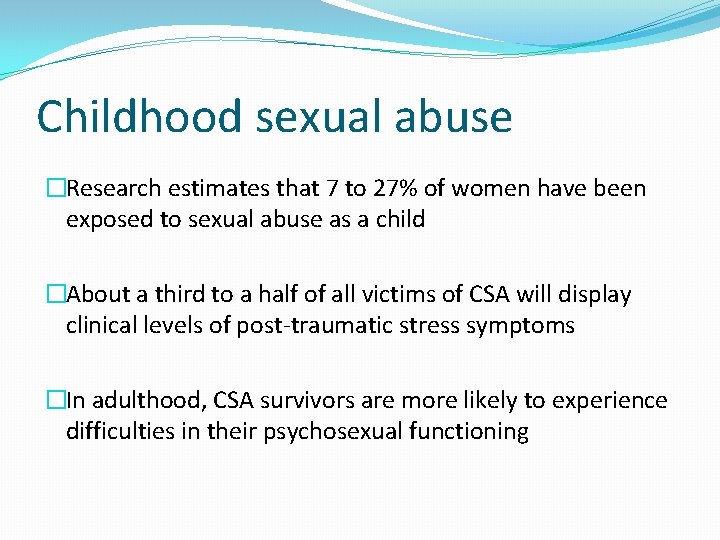
Childhood sexual abuse �Research estimates that 7 to 27% of women have been exposed to sexual abuse as a child �About a third to a half of all victims of CSA will display clinical levels of post-traumatic stress symptoms �In adulthood, CSA survivors are more likely to experience difficulties in their psychosexual functioning

![What is PTSD The American Psychiatric Association APA in the Diagnostic and Statistical Manual What is PTSD? The American Psychiatric Association [APA], in the Diagnostic and Statistical Manual](https://slidetodoc.com/presentation_image_h2/b0c5bf2273a11a10946a8f17702985f0/image-14.jpg)
What is PTSD? The American Psychiatric Association [APA], in the Diagnostic and Statistical Manual of Mental Disorders
Early History of PTSD �The Iliad of Homer and The Odyssey both describe soldiers traumatized by war �Shakespeare's King Henry IV, written in 1598, the character of Hotspur suffers from post-traumatic nightmares �Crimean War 1853 -1856 �U. S. Civil War 1861 -1865 �Boer War 1899 -1902 �World War I 1914 -1918 �World War II 1939 -1945 �Korean War 1950 -1953 �Vietnam War 1955 -1975

Early definitions �DSM-I (1952) - recognized both civilian and military experiences could cause Posttraumatic Stress Disorder, although it was described as a brief reaction rather than a potentially long-term disorder. �DSM-II (1968) - PTSD was combined with adjustment disorders and placed in the Transient Situational Disturbances category. �DSM-III (1980) - Existence of a recognizable stressor that would evoke significant symptoms of distress in almost everyone.
DSM-IV (1994) �The person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others �The person's response involved intense fear, helplessness, or horror.
DSM-V (2013) Being exposed to death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence.
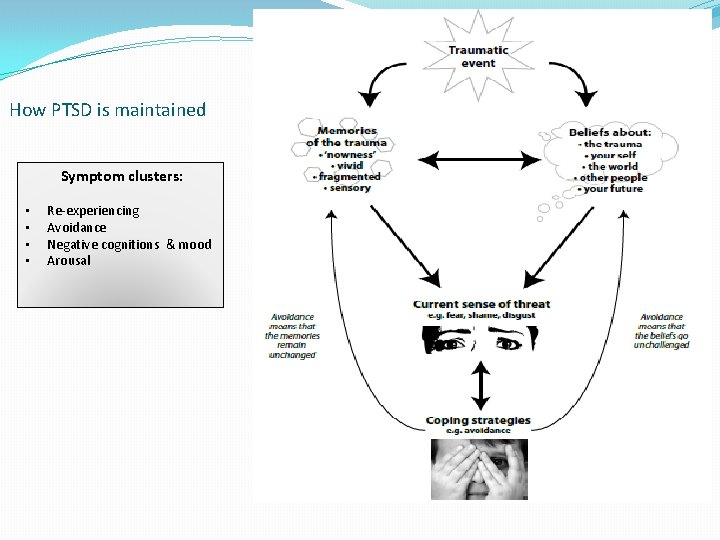
DSM-V diagnostic criteria for PTSD �DSM-V focuses on four diagnostic clusters … �Re-experiencing �Avoidance �Negative cognitions and mood �Arousal.
Psychological reactions �Anxiety �Hyper-vigilance �Sleep disturbance �Intrusive memories �Guilt �Shame and embarrassment �Sadness �Irritability �Emotional numbness �Mental avoidance �Behavioural avoidance �Increased startle response
Physical reactions �Shakiness & trembling �Tension & muscular aches (especially in head & neck) �Insomnia, tiredness & fatigue �Poor concentration & forgetfulness �Palpitations, shallow & rapid breathing, dizziness �Gastrointestinal symptoms �Disturbance of menstrual cycle & loss of interest in sex
Following disaster �In 1987 the Herald of Free Enterprise sank � 193 people died �Survey of survivors found: � 73% increased alcohol consumption � 44% increased cigarette consumption � 40% use of sleeping tablets increased � 28% use of antidepressants increased � 21% use of tranquillisers increased
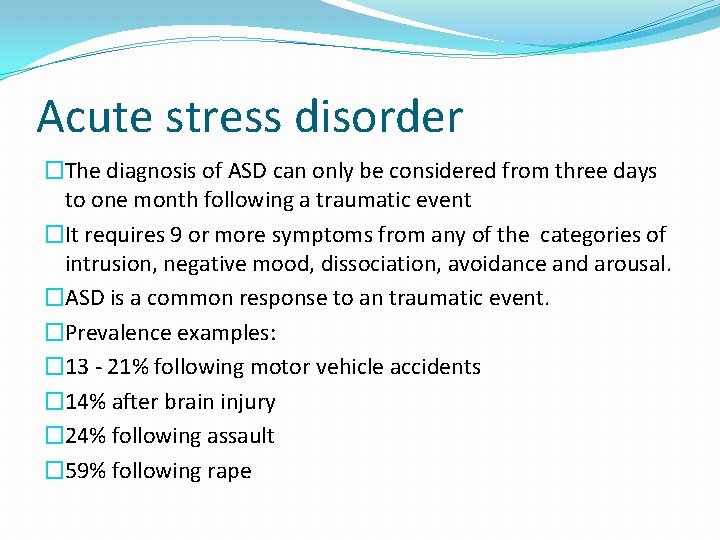
Lockerbie Disaster: The Crash of Pan Am Flight 103 (1988) �A terrorist bomb caused an airline explosion that killed 270 people. �Almost three quarters of a group of people seeking psychological damages following the crash reported PTSD. �Over 50% continued to have PTSD three years after the crash.
9/11 US Terrorist Attacks (2001) �Within two months of incident, in the cities attacked prevalence of PTSD was 8% and prevalence of depression was 10%. �Higher prevalence of PTSD was reported for those closer to the disaster (14 -20%), and for those actually in the building or injured (30%). �Prevalence of PTSD decreased during the six months following the disaster, alcohol and substance use remained high. �Depression was related to alcohol use increase, and along with PTSD was related to increased cigarette and marijuana use. �Manhattan residents overall showed significant increase in the use of all three substances.
Acute stress disorder �The diagnosis of ASD can only be considered from three days to one month following a traumatic event �It requires 9 or more symptoms from any of the categories of intrusion, negative mood, dissociation, avoidance and arousal. �ASD is a common response to an traumatic event. �Prevalence examples: � 13 - 21% following motor vehicle accidents � 14% after brain injury � 24% following assault � 59% following rape
NICE Guidelines Draft guideline for consultation 2018
Drug treatments �Do not offer drug treatments, including benzodiazepines, to prevent PTSD in adults �Consider a selective serotonin reuptake inhibitor (SSRI) or venlafaxine for adults with a diagnosis of PTSD if the person has a preference for drug treatment �Consider antipsychotics such as risperidone, quetiapine and olanzapine to manage symptoms for adults with a diagnosis of PTSD in a secondary care setting �Ensure that regular reviews are carried out
Treatment �Offer individual trauma-focused CBT to adults with a diagnosis of PTSD or clinically important symptoms of PTSD more than 1 month after a traumatic event �Offer eye movement desensitisation and reprocessing (EMDR) as an option for non-combat-related trauma to adults with a diagnosis of PTSD or clinically important symptoms of PTSD more than 3 months after a traumatic event
Concepts and theories of posttraumatic stress
Verbally accessible memories… �Brewin (1989) suggested that there will be more than one representation of a traumatic experience. �One set of representations will be of the individual’s conscious experience of the trauma, he termed these verbally accessible memories [VAMS]. �These are stored as autobiographical experiences, are likely to be fairly detailed, will contain some information regarding the sensory features, emotional and physiological reactions, and perceived meaning of the event. �Detail may be selective as anxiety tends to increase attentional selectivity and decreases short term memory capacity.
![Situationally accessible memories The other set of representations are the situationally accessible memories SAMS Situationally accessible memories… �The other set of representations are the situationally accessible memories [SAMS].](https://slidetodoc.com/presentation_image_h2/b0c5bf2273a11a10946a8f17702985f0/image-32.jpg)
Situationally accessible memories… �The other set of representations are the situationally accessible memories [SAMS]. �SAMS contain information that cannot be deliberately accessed, and therefore cannot be edited. �These memories are activated by sounds, smells, tastes and sight. �SAMS are not subject to the same processing capacity as VAMS, and the meaning that is automatically ascribed to the SAMS does not always correspond to the verbally retrievable meanings.
Shattered assumptions �Posttraumatic stress is due to the disruption of core assumptions about the self, the world and others… �These being that the self is worthy, and the world is benevolent and meaningful. �Those who hold more positive beliefs are more vulnerable as their beliefs become ‘shattered’ following a traumatic event.
Some have mainly primary emotions relating to their experience, such as fear, with symptoms which can include avoidance and arousal. Others have mainly secondary emotions, such as guilt and shame, influenced by their appraisals of events, with symptoms which can include avoidance, anger, self-blame or strong negative feelings about themselves and others.
Evidence based treatment for PTSD



Freeze response �Dissociation can occur when escape is not possible (e. g. CSA, torture, etc) �States of depersonalization and derealization are examples of how consciousness can be altered to accommodate overwhelming experience that allows the person to continue functioning during traumatic experiences �Depersonalization - individuals often see themselves observing their own body from above �Derealization - individuals experience that ‘things are not real’ ‘it is just a dream’ �Both are protective and create the perception that ‘this is not really happening to me’ and are often associated with the experience of decreased emotional intensity
Fight, flight or freeze https: //youtu. be/Rv 9 hn 4 IGof. M https: //youtu. be/H 0 RHSX_9 c-U
Evidence based treatment for PTSD �TFCBT helps people to work through the memories and make sense of the feelings they are having. It helps them to think about how their symptoms fit together, affect each other, and keep the problem going. �EMDR helps the brain’s memory networks to connect, and allows the brain to process the traumatic memory.
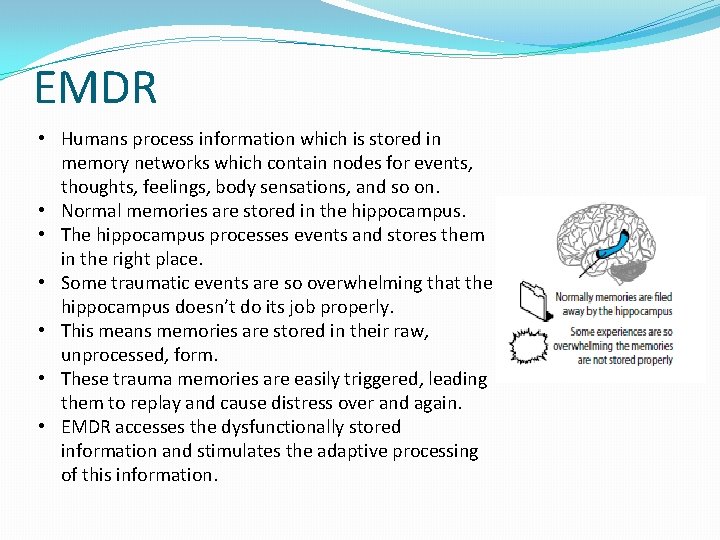
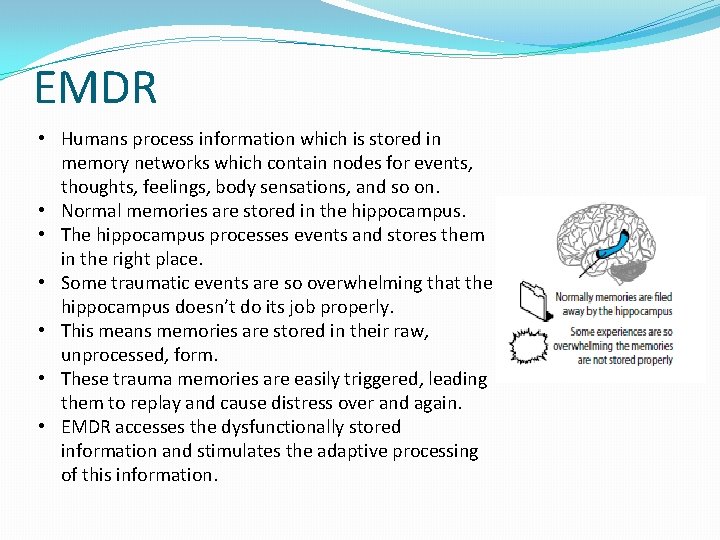
EMDR • Humans process information which is stored in memory networks which contain nodes for events, thoughts, feelings, body sensations, and so on. • Normal memories are stored in the hippocampus. • The hippocampus processes events and stores them in the right place. • Some traumatic events are so overwhelming that the hippocampus doesn’t do its job properly. • This means memories are stored in their raw, unprocessed, form. • These trauma memories are easily triggered, leading them to replay and cause distress over and again. • EMDR accesses the dysfunctionally stored information and stimulates the adaptive processing of this information.
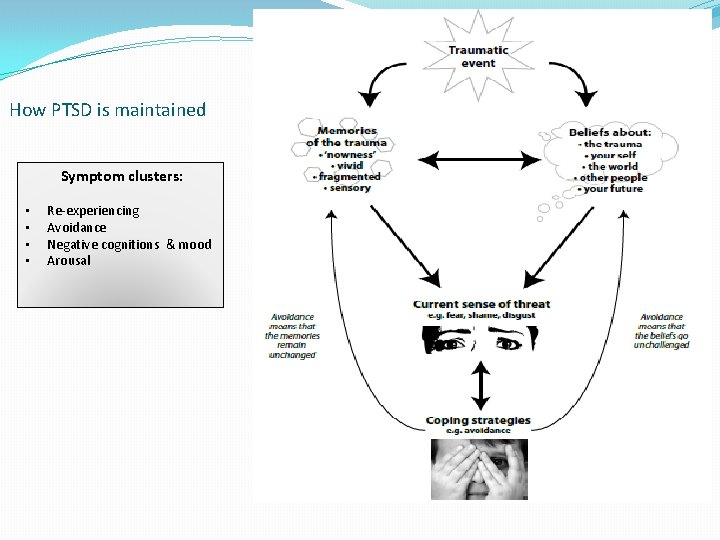
How PTSD is maintained Symptom clusters: • • Re-experiencing Avoidance Negative cognitions & mood Arousal
TFCBT sessions include… �Grounding and stabilization �Working with memories �Working with beliefs �Reclaiming your life
Working with memories �Reliving with cognitive restructuring: �Helps the person to elaborate on the trauma memory, and put it in an appropriate context �Identifies trauma hot spots and the appraisals made about these hot spots �It also tests beliefs regarding what may happen if the person stops avoiding the memory (e. g. I’ll fall apart, I’ll go crazy, etc…)

Working with beliefs �People try to make sense of what happens to them. Sometimes events happen that are so difficult to process that they come to see themselves and the world in a very negative way. �Belief work in TFCBT is about making sense of what the person thought at the time of the trauma, and deciding what is a more balanced way to think about them self and the situation now.
Body memories �Body memories can be described as a physical re-experiencing of the traumatic event(s). �The nervous system and the body experience the feelings and sensations experienced during the original traumatic event. �These memories may be explicit (always remembered) or implicit (not connected to a linear story line). �Implicit memories can happen for any traumatic event and may be particularly common if someone was under the influence of alcohol or drugs, were a child during the abuse, or if the abuse happened over a prolonged period of time.
Trauma informed care – primary care
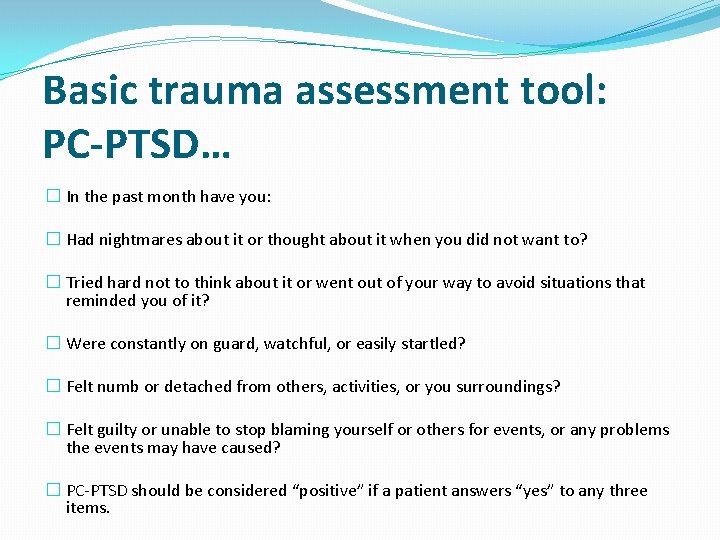
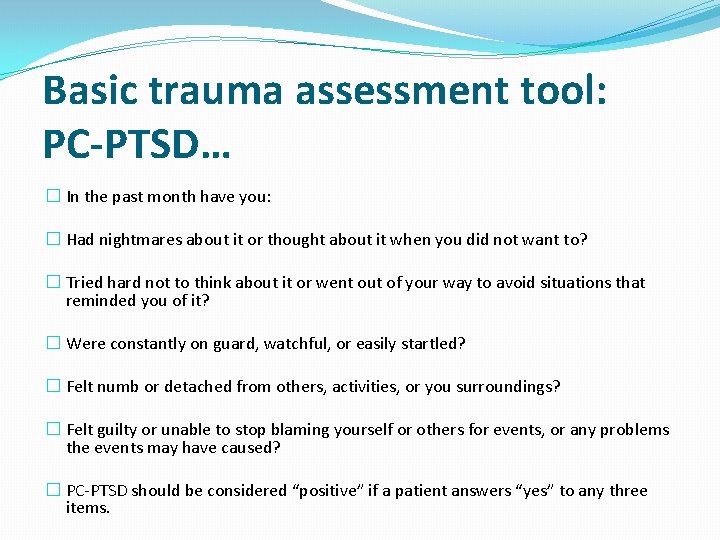
Basic trauma assessment tool: PC-PTSD… � In the past month have you: � Had nightmares about it or thought about it when you did not want to? � Tried hard not to think about it or went out of your way to avoid situations that reminded you of it? � Were constantly on guard, watchful, or easily startled? � Felt numb or detached from others, activities, or you surroundings? � Felt guilty or unable to stop blaming yourself or others for events, or any problems the events may have caused? � PC-PTSD should be considered “positive” if a patient answers “yes” to any three items.
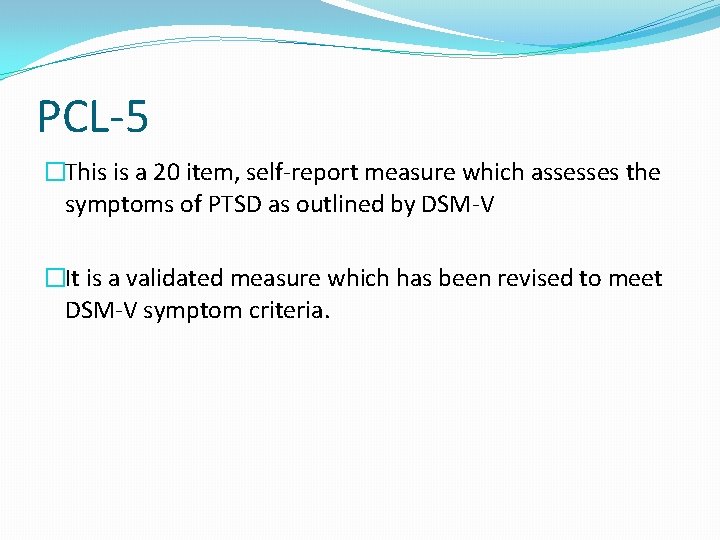
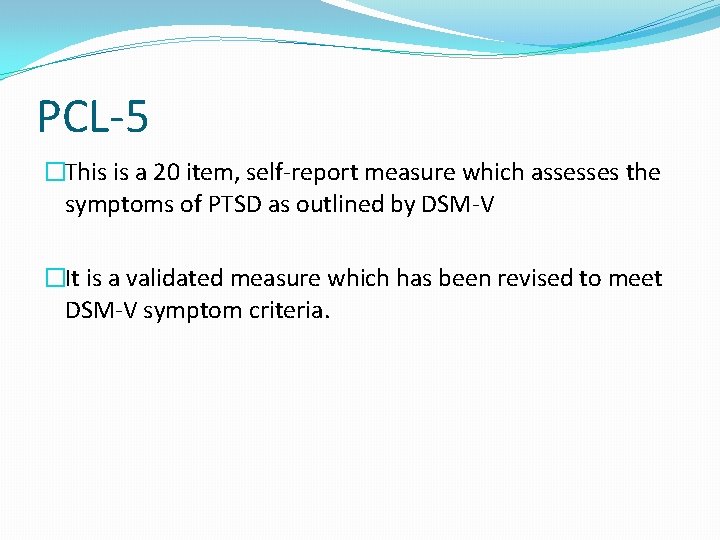
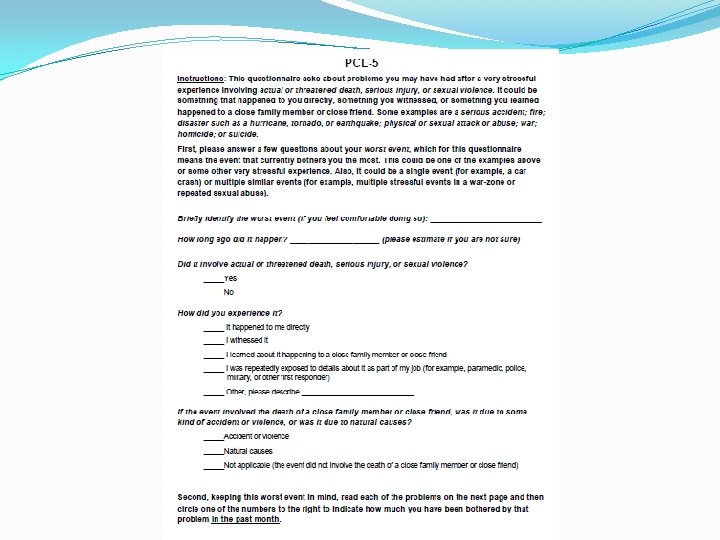
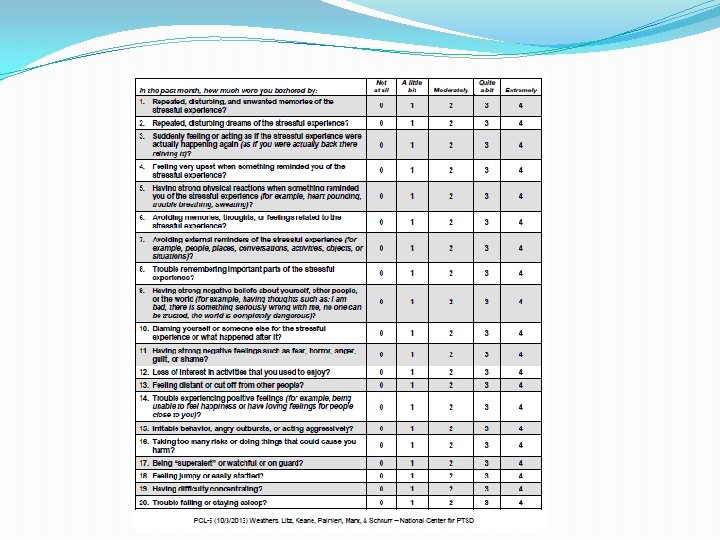
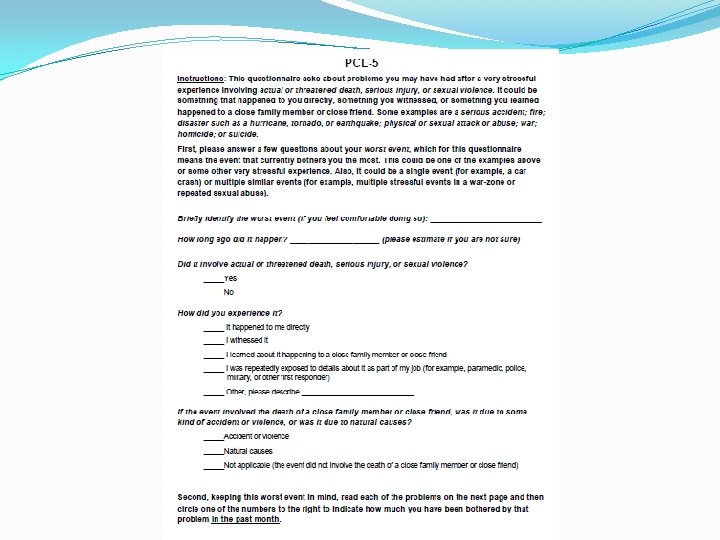
PCL-5 �This is a 20 item, self-report measure which assesses the symptoms of PTSD as outlined by DSM-V �It is a validated measure which has been revised to meet DSM-V symptom criteria.
Planning treatment and supporting engagement �Give information about treatment interventions �Take into account any previous treatment, associated functional impairment and any coexisting conditions. �Take into account any social or personal factors that may have a role in the development or maintenance of the disorder �Be aware that people with PTSD may be apprehensive, anxious and may avoid treatment or have difficulty developing trust. �Engagement strategies could include following up when people miss appointments.
What should GPs/Primary care providers do immediately following a traumatic event?
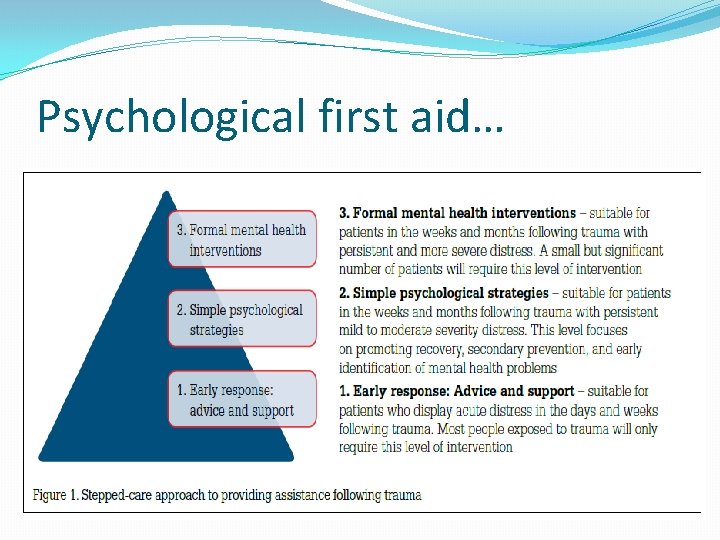
Psychological first aid… �Early assistance to those who have experienced trauma, the aim being to reduce initial distress and maximise the likelihood of a natural spontaneous recovery. �It ensures basic needs are met, providing practical and emotional support and information, and promotes adaptive coping; encouraging engagement with social supports. �It aims to ensure a sense of safety, calming, self-efficacy, connectedness and hope. �Reference: Wade, D. , Howard, A. , Fletcher, S. , Cooper, J. , Forbes, D. (2013). Early response to psychological trauma. What GPs can do. Australian Family Physician 42 (9), 610 -614.
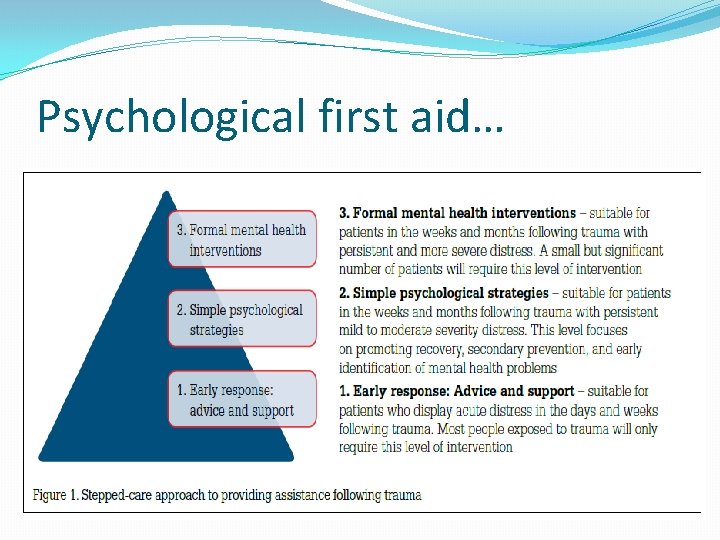
Psychological first aid…
Sense of safety �Be realistic and specific, rather than provide vague and potentially inaccurate reassurances �Provide simple and accurate information on how to meet the person’s basic needs (eg. food and shelter) �Repeat information as often as needed �Encourage the person to limit exposure to media coverage of the event, particularly graphic coverage that can lead to increased distress
Calming �Teaching patients to use controlled breathing when anxious �‘Normalising’ psychological reactions to such events �Encouraging sufficient rest, exercise and a healthy diet �Assisting patients to schedule enjoyable and relaxing activities �Encourage the patient to avoid unhelpful coping strategies such as substance use and social withdrawal
Self efficacy �Highlight those aspects of the situation that the person has some control over �Remind the person about past experiences of successfully coping with stressful situations �Encourage the person to actively address problems and solve one problem at a time �Assist the person to ‘recalibrate’ their expectations of themselves
Connectedness �Explaining the known benefits of social support �Encouraging the person to identify opportunities to spend time with family and friends �Telling the person that they may find talking to others helpful, but should do so when they feel ready �Directing and referring the person to appropriate community support services �Anticipating that some people will not feel deserving of assistance
Promoting hope �Most people recover with time by using helpful coping strategies and with the support of family and others �For many people, distressing psychological reactions are transient �The patient has strengths, such as their ability to cope under stress or their available social supports
Self care �Providing care in the aftermath of a traumatic event can place significant demands on GPs/Primary care providers �They may face repeated exposure to traumatic and distressing experiences of others, and in some large scale events, may themselves be members of the affected community �It is important that they look after their own mental health, by employing the self-management strategies that they encourage their patients to use
Key points �Only a minority of people develop chronic mental health problems following exposure to a traumatic event. �GPs are well placed to support and monitor primary care patients �following trauma exposure. �Psychological first aid is the preferred approach to providing early assistance to people who have experienced a traumatic event. �Early advice and support provided by GPs can be guided by the �following principles: a sense of safety, calming, self efficacy, �connectedness and hope. �GP self care is an important aspect of providing post-trauma patient care.
Questions? Contact details emmamathewstherapy@outlook. com emma. mathews@gmmh. nhs. uk