PRESSURE ULCER AWARENESS TRAINING The Frightening Statistics Every




- Slides: 27
PRESSURE ULCER AWARENESS TRAINING
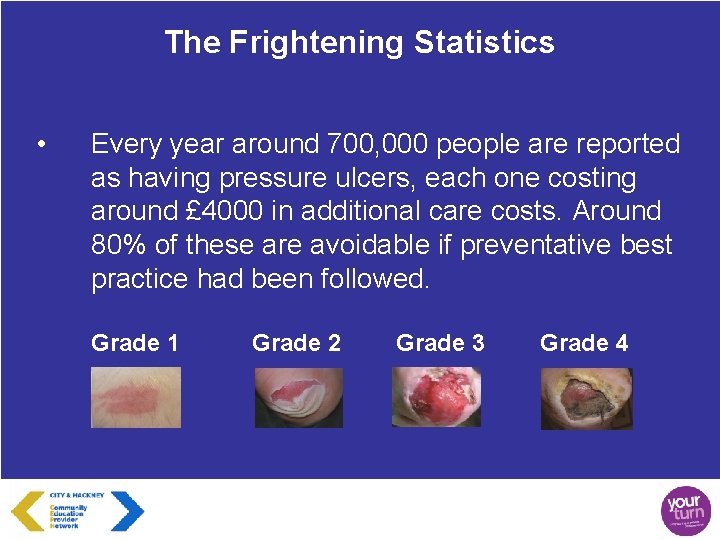
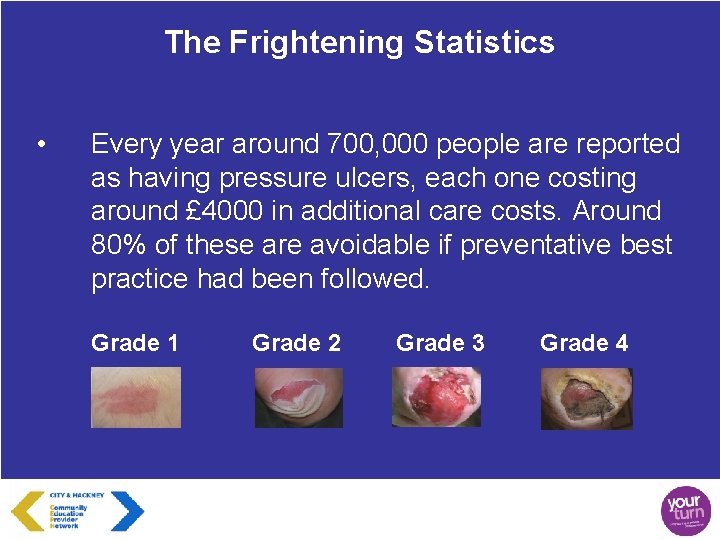
The Frightening Statistics • Every year around 700, 000 people are reported as having pressure ulcers, each one costing around £ 4000 in additional care costs. Around 80% of these are avoidable if preventative best practice had been followed. Grade 1 Grade 2 Grade 3 Grade 4
WARNING!! It only takes 2 hours to damage the skin with pressure Fit and healthy people move approximately every 7 minutes to relieve pressure
Blood supply • • • Think of the blood supply like a hosepipe If you stand on it or kink it, it stops flowing Blood vessels are squashed by a persons weight pushing their bone through the tissue against a surface (chair or bed)
What Are Pressure Ulcers (a dictionary definition) • • Pressure ulcers are caused when an area of skin and the tissues below are damaged as a result of being placed under pressure sufficient to impair its blood supply A pressure ulcer is a localised injury to the skin and underlying tissue usually over a bony prominence as a result of pressure or pressure in combination with shear
Who Is At Risk? • • • The sad reality is that we are all at risk The greatest risk is to those who are immobile Any person who is unable to change position without help People unable to feel pain due to nerve damage Diabetics and people with arterial disease Elderly people in general are at greater risk because the skin is thinner and more fragile

Additional risks to elderly • The older person is more susceptible to: • Bruising and haematomas • Maceration (fluid retention in the skin) • Skin tears • Moisture lesions • Leg ulcers ALL DUE TO AGEING SKIN
How does the skin change with age? • • The epidermis becomes thinner, reduced elastin fibres, more easy to stretch, increasing the risk of tearing and trauma and is more susceptible to moisture damage Thinning of the dermis sees a reduction in blood vessels, nerve endings and collagen leading to decreased sensation, temperature control, rigidity and moisture retention
How Pressure Ulcers Can Affect People’s Lives • • • They can be painful Can cause depression and anxiety Stop people taking part in activities Possible hospital admission due to infection May cause death
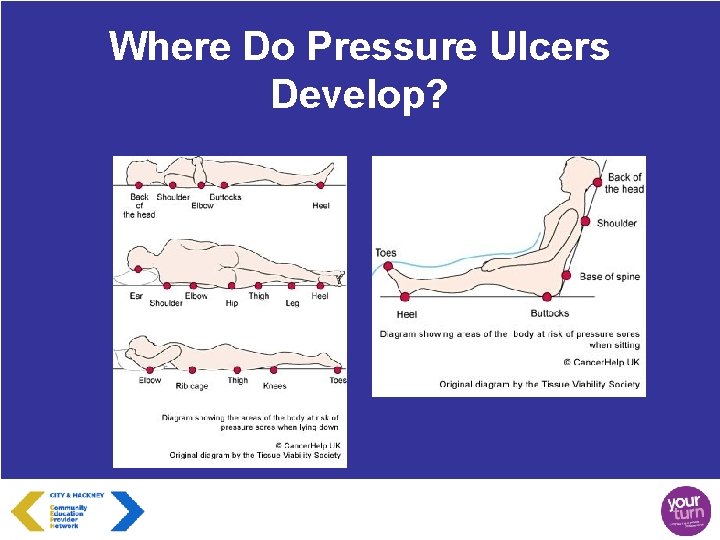
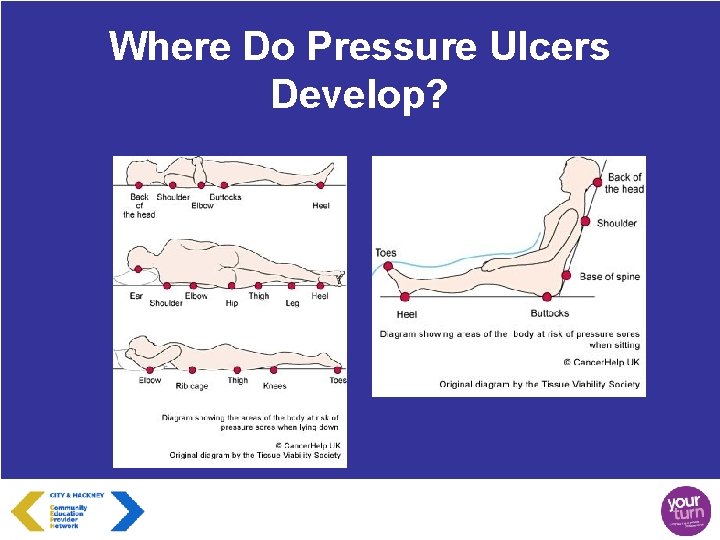
Where Do Pressure Ulcers Develop?
Medication and Pressure Ulcers • • Some medication can inadvertently increase the risk of a pressure ulcer if it reduces sensitivity to pain or pressure Care plans should be clearly noted with details of sedatives or other medication being given in order that correct pressure area care is undertaken
Five Simple Steps S – SURFACE S – SKIN INSPECTION K – KEEP MOVING I – INCONTINENCE N – NUTRITION AND HYDRATION
Surface • • • Pressure mattresses and cushions are used by people at risk of or who have pressure ulcers – cut foam, memory foam, air alternating (not cushions) Check covers for damage Remove slide sheets and hoist slings Reposition on mattresses If there is a problem consult the instruction booklet and/or call the engineer
Skin Inspection • • Vulnerable areas – bony prominence Discolouration, blisters, changes in skin temperature (hot = damaged), swelling (boggy feel), discomfort (pain, hardness, itching, loss of sensation) Document what is found even if skin is normal Report any concerns through the PUT form which we will go over later
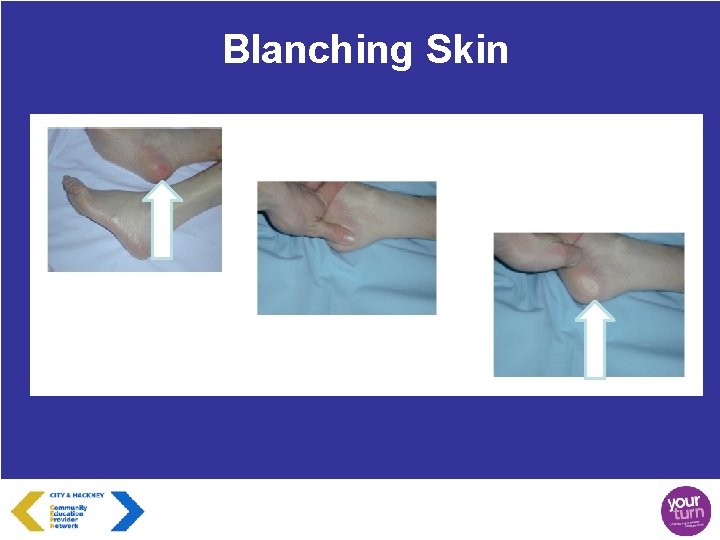
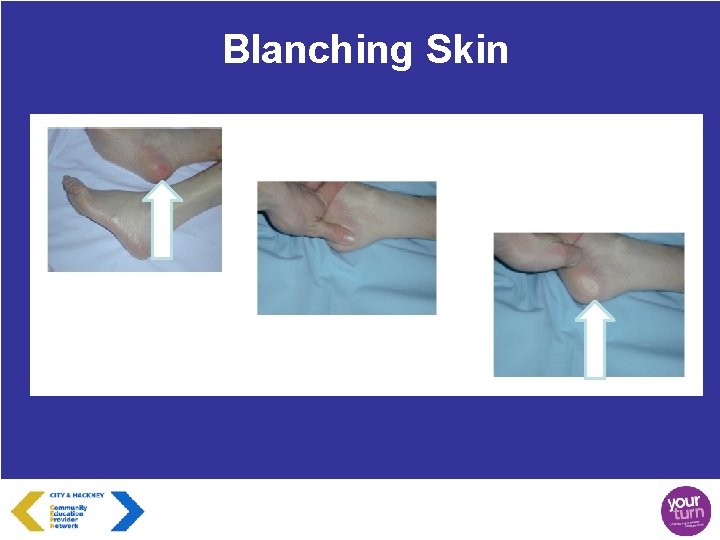
Blanching Skin

Non-Blanching Skin
Keep Moving • • • Assist those who cannot reposition/move themselves Reposition people on mattresses Limit chair sitting – 2 hours maximum Use 2 hours as a guide – may be able to go longer, particularly at night Encourage regular, gentle movements – chair based exercise every 30 mins
Incontinence and Moisture • • • Ensure people are clean and dry Limit the use of vigorous movements when washing and drying – they are not a dirty saucepan If soiled wash using a soap substitute (soap increases the skin’s p. H level and puts it at greater risk of dehydration and bacteria colonisation) Apply barrier cream/spray if prescribed but only if you know how to use it properly. If you don’t ask to be shown Report any concerns
Nutrition and Hydration • • Ensure people are eating and drinking Monitor intake of food and fluid where possible Check mouths for any problems such as thrush, ill fitting dentures, are their dentures their own? Ensure supplements are offered where prescribed but with meals rather than on their own
Four Steps of Prevention
Step 1 • Training – Simple advice and knowledge that can improve the outcomes for the people you are caring for – Will be recorded on your employment history (certificates will be made available soon) – Demonstrates a commitment and willingness to prevent pressure ulcers with simple techniques
Step 2 • Policy – Agree what is your ‘Policy on Pressure Ulcer prevention’? – Publish your policy for relatives to see – Put it on your website – Tell the commissioners about your proactivity in this area – We have a template policy available on the website for organisations to download
Step 3 • • Using The New Tools We have produced some tools to make your jobs easier when it comes to pressure ulcer prevention – General information leaflets – – Posters Workbooks Pressure Ulcer Trigger checklists Safety Cross (available online)

Step 4 • Keep It Going – Pressure Ulcer Prevention needs to become part of your day to day lives – Get used to using the tools to help record the work that you are doing – Publish your pressure ulcer prevention policy on your website – Keep a log of how many days ‘Pressure Ulcer Free’ you are in your area and communicate it regularly to staff using the Safety Cross – Visit the website for advice and support – www. reacttoredskin. co. uk/hackney
26

PRESSURE ULCER AWARENESS TRAINING www. reacttoredskin. co. uk/hackney
 Privacy awareness and hipaa privacy training cvs answers
Privacy awareness and hipaa privacy training cvs answers Disease definition
Disease definition Pauchet gastrectomy
Pauchet gastrectomy Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Tuberculous ulcer and typhoid ulcer
Tuberculous ulcer and typhoid ulcer Ulcer niche and ulcer notch
Ulcer niche and ulcer notch Gastric ulcer vs duodenal ulcer
Gastric ulcer vs duodenal ulcer Pressure ulcer prevention bundle
Pressure ulcer prevention bundle Bedsore grade
Bedsore grade Sskin bundle template
Sskin bundle template Pressure ulcer pico question
Pressure ulcer pico question Nasal cannula pressure ulcer prevention
Nasal cannula pressure ulcer prevention Braden score meaning
Braden score meaning Category 4 pressure ulcer
Category 4 pressure ulcer Pressure ulcer clipart
Pressure ulcer clipart Depuap
Depuap Every nation and every country
Every nation and every country Microsoft vision statement
Microsoft vision statement Every knee shall bow every tongue confess
Every knee shall bow every tongue confess Every rotarian every year
Every rotarian every year Every nation and every country
Every nation and every country Every picture has a story and every story has a moment
Every picture has a story and every story has a moment Every child every day
Every child every day How is hyde presented as a frightening outsider
How is hyde presented as a frightening outsider Chapter 4-6 summary to kill a mockingbird
Chapter 4-6 summary to kill a mockingbird Although frieda is typically very reserved as
Although frieda is typically very reserved as Introduction to statistics what is statistics
Introduction to statistics what is statistics Peer pressure statistics
Peer pressure statistics