HIPAA Privacy and Security Training For Employees Compliance




- Slides: 73
HIPAA Privacy and Security Training For Employees Compliance is Everyone’s Job University Medical Center UNIVERSITY OF ALABAMA V 2012. 1 INTERNAL USE ONLY 1
Topics to Cover • • • General HIPAA Privacy and Security Overview HIPAA Privacy ARRA of 2009: HIPAA Breach Notification Rules and Procedures HIPAA Security Questions/Acknowledgment of Training INTERNAL USE ONLY 2
What is HIPAA? The Health Insurance Portability and Accountability Act (HIPAA) is federal legislation which addresses issues ranging from health insurance coverage to national standard identifiers for healthcare providers. The portions that are important for our purposes are those that deal with protecting the privacy and security of health data, which HIPAA calls Protected Health Information or PHI. INTERNAL USE ONLY 3
Question 1 HIPAA addresses a) Privacy b) Security c) Both A and B INTERNAL USE ONLY 4
Correct Answer c: HIPAA establishes requirements for both the privacy and security of PHI. Privacy refers to the confidentiality of protected information. Security addresses the safekeeping of both paper and electronic (computer-based) records. INTERNAL USE ONLY 5
Applicability of HIPAA to UA • HIPAA Applies to: University Medical Center Brewer-Porch Children's Center The Speech & Hearing Center Autism Clinic Departments that have signed Business Associate Agreements Group Health Insurance/Flexible Spending Plan/EAP UA Administrative Departments supporting the above entities (like Legal Office, Auditing, Financial Affairs, Risk Management, OIT, UA Privacy/Security Officer, etc. ) • Research involving PHI from a HIPAA covered entity • • Does not apply to Psychology Clinic, Student Health Center/Pharmacy, ODS records, Counseling Center, WRC, Athletic Dept health records INTERNAL USE ONLY 6
What is Protected Health Information (PHI) • Any information, transmitted or maintained in any medium, including demographic information; • Created/received by covered entity or business associate; • Relates to/describes past, present or future physical or mental health or condition; or past, present or future payment for provision of healthcare; and • Can be used to identify the patient INTERNAL USE ONLY 7
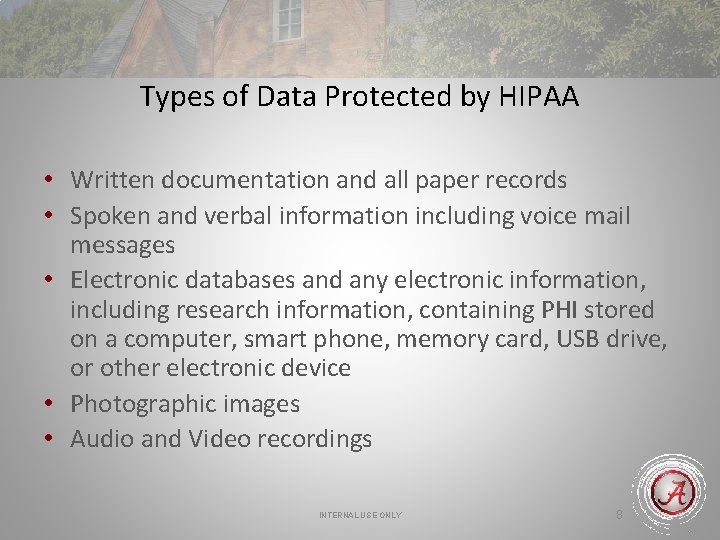
Types of Data Protected by HIPAA • Written documentation and all paper records • Spoken and verbal information including voice mail messages • Electronic databases and any electronic information, including research information, containing PHI stored on a computer, smart phone, memory card, USB drive, or other electronic device • Photographic images • Audio and Video recordings INTERNAL USE ONLY 8
Question 2 Jenny, a pediatric nurse, needs to report lab results to the mother of a 3 year old child who is sitting in the waiting room. She sticks her head in the waiting room door and says, “Good news. The lab results are normal. ” Is this a privacy breach? a) Yes b) No INTERNAL USE ONLY 9
Correct Answer c: Yes, unless no one else was in the waiting room. The nurse should have asked the mother to step out into the hallway or taken other steps to be certain that no one else would overhear the conversation. INTERNAL USE ONLY 10
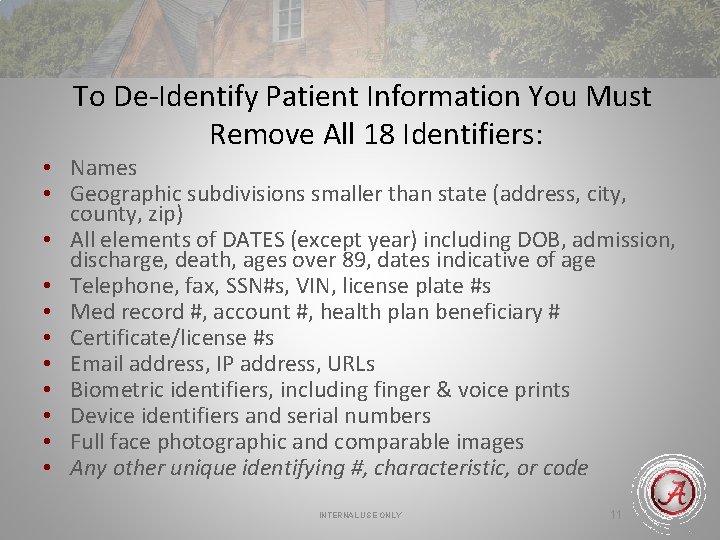
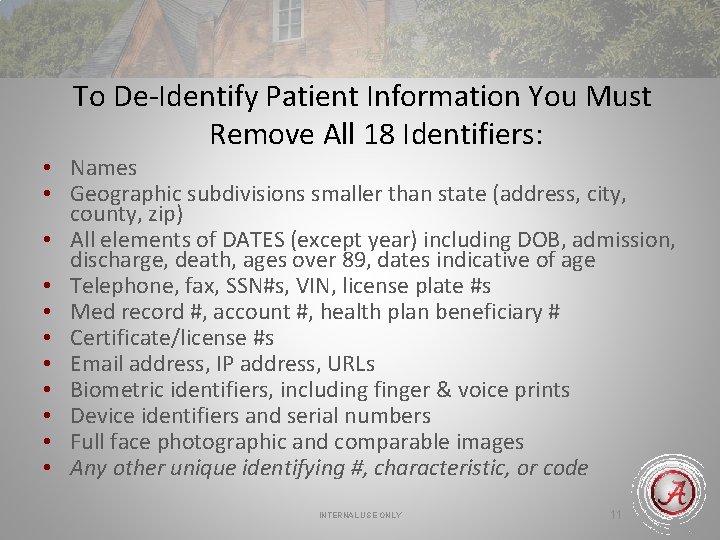
To De-Identify Patient Information You Must Remove All 18 Identifiers: • Names • Geographic subdivisions smaller than state (address, city, county, zip) • All elements of DATES (except year) including DOB, admission, discharge, death, ages over 89, dates indicative of age • Telephone, fax, SSN#s, VIN, license plate #s • Med record #, account #, health plan beneficiary # • Certificate/license #s • Email address, IP address, URLs • Biometric identifiers, including finger & voice prints • Device identifiers and serial numbers • Full face photographic and comparable images • Any other unique identifying #, characteristic, or code INTERNAL USE ONLY 11
Question 3 Photographs are considered PHI. a) True b) False INTERNAL USE ONLY 12
Correct Answer a: Photographs as well as video and audio recordings are protected under HIPAA regulations. INTERNAL USE ONLY 13
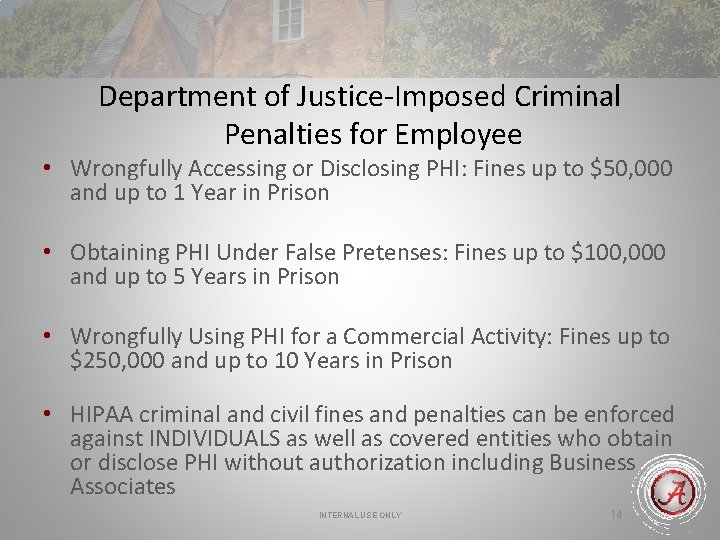
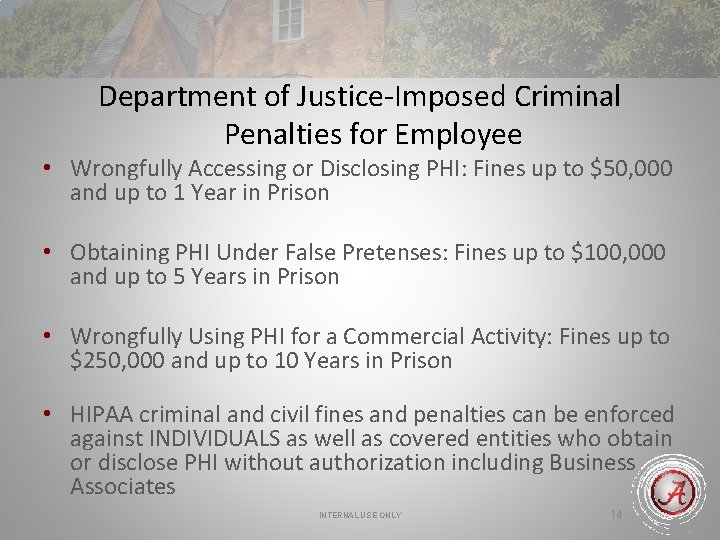
Department of Justice-Imposed Criminal Penalties for Employee • Wrongfully Accessing or Disclosing PHI: Fines up to $50, 000 and up to 1 Year in Prison • Obtaining PHI Under False Pretenses: Fines up to $100, 000 and up to 5 Years in Prison • Wrongfully Using PHI for a Commercial Activity: Fines up to $250, 000 and up to 10 Years in Prison • HIPAA criminal and civil fines and penalties can be enforced against INDIVIDUALS as well as covered entities who obtain or disclose PHI without authorization including Business Associates INTERNAL USE ONLY 14
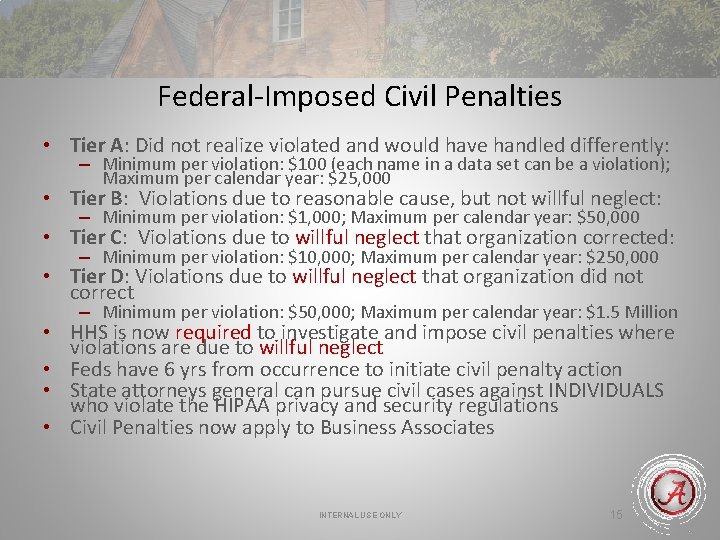
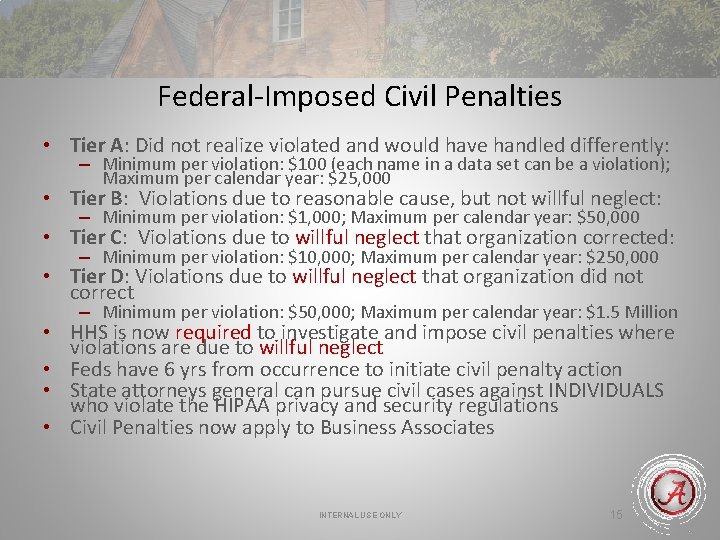
Federal-Imposed Civil Penalties • Tier A: Did not realize violated and would have handled differently: – Minimum per violation: $100 (each name in a data set can be a violation); Maximum per calendar year: $25, 000 • Tier B: Violations due to reasonable cause, but not willful neglect: – Minimum per violation: $1, 000; Maximum per calendar year: $50, 000 • Tier C: Violations due to willful neglect that organization corrected: – Minimum per violation: $10, 000; Maximum per calendar year: $250, 000 • Tier D: Violations due to willful neglect that organization did not correct – Minimum per violation: $50, 000; Maximum per calendar year: $1. 5 Million • HHS is now required to investigate and impose civil penalties where violations are due to willful neglect • Feds have 6 yrs from occurrence to initiate civil penalty action • State attorneys general can pursue civil cases against INDIVIDUALS who violate the HIPAA privacy and security regulations • Civil Penalties now apply to Business Associates INTERNAL USE ONLY 15
Question 4 An individual convicted of HIPAA violation might be subject to a) Fine b) Jail term c) Both A and B INTERNAL USE ONLY 16
Correct Answer c: HIPAA is federal legislation. Sanctions for violators can include both fines and incarceration. INTERNAL USE ONLY 17
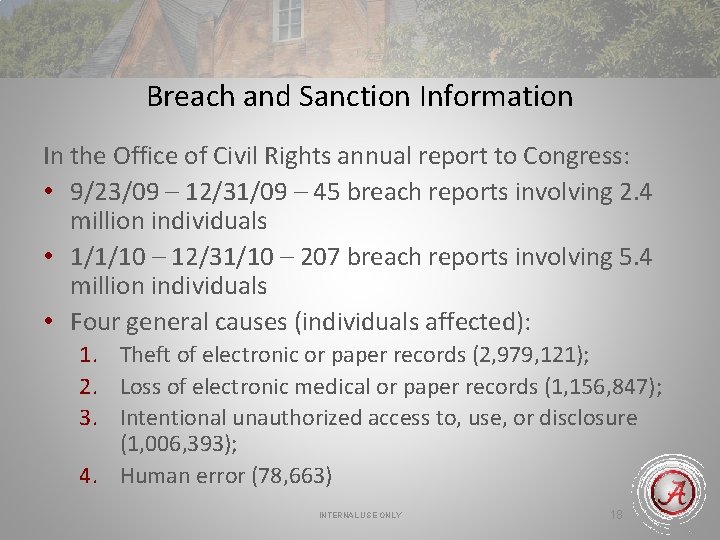
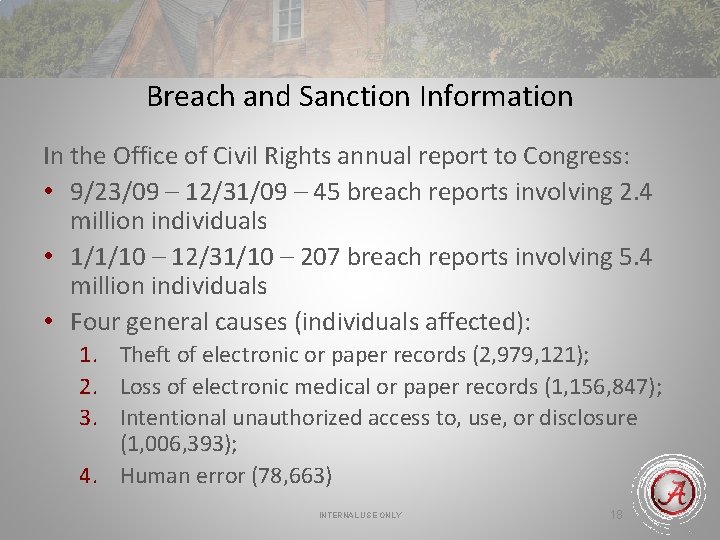
Breach and Sanction Information In the Office of Civil Rights annual report to Congress: • 9/23/09 – 12/31/09 – 45 breach reports involving 2. 4 million individuals • 1/1/10 – 12/31/10 – 207 breach reports involving 5. 4 million individuals • Four general causes (individuals affected): 1. Theft of electronic or paper records (2, 979, 121); 2. Loss of electronic medical or paper records (1, 156, 847); 3. Intentional unauthorized access to, use, or disclosure (1, 006, 393); 4. Human error (78, 663) INTERNAL USE ONLY 18
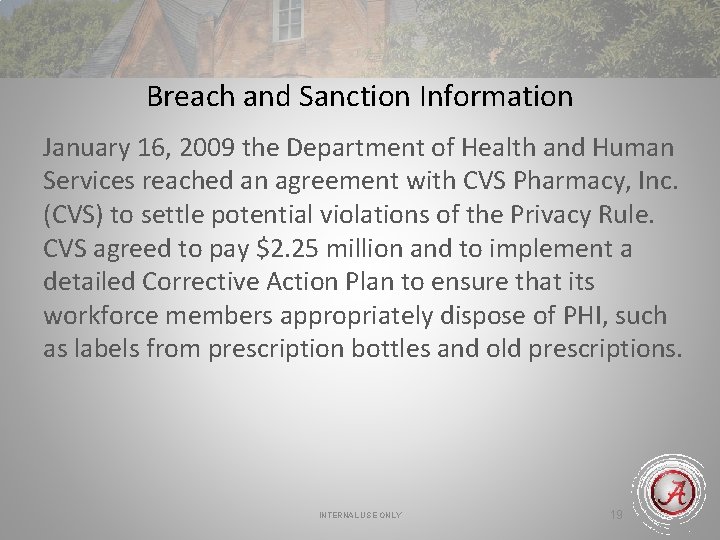
Breach and Sanction Information January 16, 2009 the Department of Health and Human Services reached an agreement with CVS Pharmacy, Inc. (CVS) to settle potential violations of the Privacy Rule. CVS agreed to pay $2. 25 million and to implement a detailed Corrective Action Plan to ensure that its workforce members appropriately dispose of PHI, such as labels from prescription bottles and old prescriptions. INTERNAL USE ONLY 19
Breach and Sanction Information On July 27, 2010, the Department of Health and Human Services (HHS) reached an agreement with Rite Aid Corporation and its 40 affiliated entities (Rite Aid) to settle potential violations of the Privacy Rule. Rite Aid agreed to pay $1 million and to take corrective action to improve policies and procedures to safeguard the privacy of its customers when disposing PHI on pill bottle labels and other health information. INTERNAL USE ONLY 20
Breach and Sanction Information July 6, 2011 The Department of Health and Human Services (HHS) entered into its third largest settlement for potential HIPAA privacy and security rule violations, reaching a resolution agreement of $865, 500 with the University of California at Los Angeles Health System (UCLAHS) associated with 2 complaints of intentional unauthorized access to/use/disclosure of PHI. INTERNAL USE ONLY 21
UA HIPAA Sanctions • Employees who do not follow Privacy and Security Policies and related workplace rules and policies are subject to disciplinary action, up to and including dismissal • Type of sanction depends on severity of violation, intent, pattern/practice of improper activity, etc. INTERNAL USE ONLY 22
Question 5 A University of Alabama employee who violates HIPAA Policies can be fired. a) True b) False INTERNAL USE ONLY 23
Correct Answer a: True: The University of Alabama is legally obligated to enforce HIPAA Policies. Employees who violate policy will be subject to sanctions which can included termination of employment. The nature of the sanction is determined by the severity of the policy breach. INTERNAL USE ONLY 24
HIPAA Permitted Uses and Disclosures of PHI • A covered entity can always use and disclose PHI for any purpose if it gets the person’s signed HIPAA-valid authorization • Only designated, HIPAA trained personnel are permitted to approve disclosure of PHI per the person’s HIPAA-valid authorization • For a complete list of permitted uses and disclosures of PHI, see your entity’s notice of health information practices INTERNAL USE ONLY 25
HIPAA Permitted Uses and Disclosures of PHI • The HIPAA Privacy Rule states that PHI may be used and disclosed to facilitate treatment, payment, and healthcare operations (TPO) which means: – PHI may be disclosed to other providers for treatment – PHI may be disclosed to other covered entities for payment – PHI may be disclosed to other covered entities that have a relationship with the patient for certain healthcare operations such as quality improvement, credentialing, and compliance – PHI may be disclosed to individuals involved in a patient’s care or payment for care unless the patient objects INTERNAL USE ONLY 26
Minimum Necessary Standard • When HIPAA permits use or disclosure of PHI, a covered entity must use or disclose only the minimum necessary PHI required to accomplish the purpose of the use or disclosure. • The only exceptions to the minimum necessary standard are those times when a covered entity is disclosing PHI for the following reasons: – – Treatment Purposes for which an authorization is signed Disclosures required by law Sharing information to the patient about himself/herself INTERNAL USE ONLY 27
What HIPAA Did Not Change: • Family and friends can still pick up prescriptions for sick people • Physicians and Nurses do not have to whisper • State laws still govern the disclosure of minor’s health information to parents (a minor is under the age of 19 in Alabama) INTERNAL USE ONLY 28
Other Privacy Safeguards • Avoid conversations involving PHI in public or common areas such as hallways or elevators • Keep documents containing PHI in locked cabinets or locked rooms when not in use • During work hours, place written materials in secure areas that are not in view or easily accessed by unauthorized persons • Do not leave materials containing PHI on desks or counters, in conference rooms, or in public areas • Do not remove PHI in any form from the designated work site unless authorized to do so by management • Never take photographs in patient care areas INTERNAL USE ONLY 29
Required Forms and Documents Used at UA • • Notice of Health Information Practices Acknowledgement of Receipt of Notice Confidentiality Statement Authorization for Use or Disclosure of Information Accounting of Disclosures Documentation Business Associate Agreements Fax Coversheet Data Use Agreement INTERNAL USE ONLY 30
Question 6 TPO stands for a) Therapy, patient, outcome b) Treatment, payment, operation c) Training, participation, organization INTERNAL USE ONLY 31
Correct Answer b: Treatment, payment, operation. Once the Acknowledgement of Health Information Practices has been signed by the patient, PHI can be disclosed as necessary to complete treatment, bill for services, and manage healthcare operations. INTERNAL USE ONLY 32
Question 7 PHI can never be released for any reason except TPO (treatment, payment, operations). a) True b) False INTERNAL USE ONLY 33
Correct Answer b: False. PHI can be released for reasons other than TPO if additional release forms have been signed by the patient. INTERNAL USE ONLY 34
Question 8 Charlie works at a medical center and is responsible for entering billing data into the computer system. He looks at his mother-in-law’s medical records, because he is concerned that she has not been fully honest with her family about some recent health problems. Since he has been HIPAA trained, is this a breach of privacy? a) Yes b) No INTERNAL USE ONLY 35
Correct Answer a: Yes. Although Charlie has been HIPAA trained, his access is based on the minimum necessary requirement to complete his job. He does not need to access health records to enter billing data. Unless his mother-in-law has given permission, in writing, for him to access her records, this action was a violation of Privacy Policies. INTERNAL USE ONLY 36
Business Associate Agreements • Are required before a covered entity can contract with a third party individual or vendor (subcontractor) to perform activities or functions which will involve the use or disclosure of the covered entity’s PHI • Binds the third party individual or vendor to the HIPAA regulations when performing the contracted services • Must be approved in accordance with appropriate UA policies and procedures Individual employees are NOT authorized to sign contracts on behalf of UA. INTERNAL USE ONLY 37
HIPAA Put New Requirements on Research: • If you work for a Health Care Provider under HIPAA, do not release PHI for research unless: – The patient has signed a valid HIPAA authorization, or – The IRB at UA has approved a waiver of authorization; or – The IRB agrees that an exception applies Information regarding HIPAA and Research is available through Office of Research Compliance – Director is Tanta Myles INTERNAL USE ONLY 38
American Recovery and Reinvestment Act of 2009 (ARRA) • Expanded privacy and security provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) • One new requirement is that we must notify affected individuals and federal officials when a breach or potential breach of privacy has occurred • The following slides discuss our obligation under these rules INTERNAL USE ONLY 39
Question 9 _______ requires that individuals and federal officials be notified when a breach or potential breach of PHI Privacy or Security regulations has occurred a) HIPAA b) AARA c) FERPA INTERNAL USE ONLY 40
Correct Answer b: AARA, or the American Recovery and Reinvestment Act of 2009, expanded HIPAA to establish regulations for notification of a breach or potential breach of PHI. INTERNAL USE ONLY 41
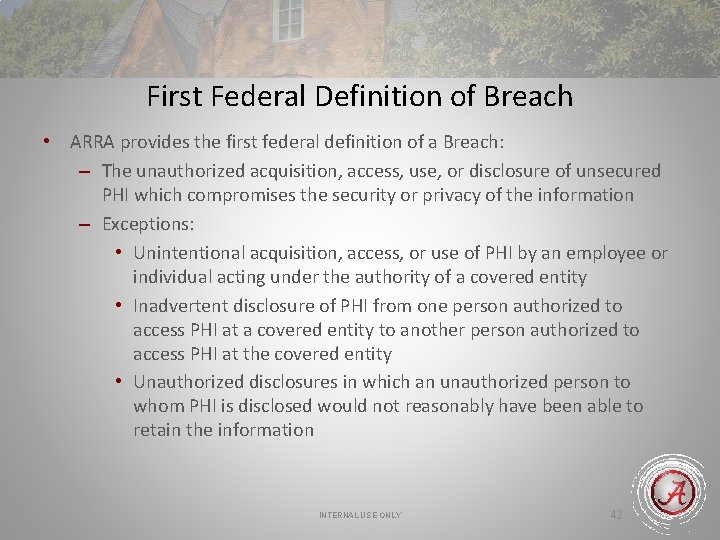
First Federal Definition of Breach • ARRA provides the first federal definition of a Breach: – The unauthorized acquisition, access, use, or disclosure of unsecured PHI which compromises the security or privacy of the information – Exceptions: • Unintentional acquisition, access, or use of PHI by an employee or individual acting under the authority of a covered entity • Inadvertent disclosure of PHI from one person authorized to access PHI at a covered entity to another person authorized to access PHI at the covered entity • Unauthorized disclosures in which an unauthorized person to whom PHI is disclosed would not reasonably have been able to retain the information INTERNAL USE ONLY 42
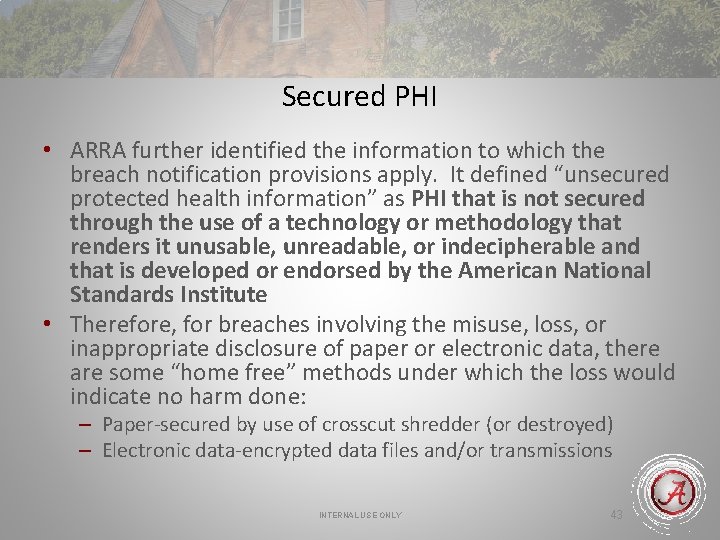
Secured PHI • ARRA further identified the information to which the breach notification provisions apply. It defined “unsecured protected health information” as PHI that is not secured through the use of a technology or methodology that renders it unusable, unreadable, or indecipherable and that is developed or endorsed by the American National Standards Institute • Therefore, for breaches involving the misuse, loss, or inappropriate disclosure of paper or electronic data, there are some “home free” methods under which the loss would indicate no harm done: – Paper-secured by use of crosscut shredder (or destroyed) – Electronic data-encrypted data files and/or transmissions INTERNAL USE ONLY 43
Encryption • Security Rules require Covered Entity/Business Associate to consider implementing encryption as a method for safeguarding Electronic Protected Health Information (PHI) • If you choose to encrypt, then not required to notify in event of breach INTERNAL USE ONLY 44
What Constitutes a Breach? • A breach could result from many activities. Some examples are – – – Failing to log off when leaving a workstation Unauthorized access to PHI Sharing confidential information, including passwords Having patient-related conversations in public settings Improper disposal of confidential materials in any form Copying or removing PHI from the appropriate area • Why? – – Curiosity…about a co-worker or friend Laziness…so shared sign-on to information systems Compassion…the desire to help someone Greed or malicious intent…for personal gain INTERNAL USE ONLY 45
Question 10 Bill, a billing employee, receives and opens an email containing PHI which a nurse, Nancy, mistakenly sent to Bill notices that he is not the intended recipient, alerts Nancy to the misdirected email, and deletes it. • Was this a breach of PHI? a) Yes b) No INTERNAL USE ONLY 46
Correct Answer b: No. Bill unintentionally accessed PHI that he was not authorized to access. However, he opened the email within the scope of his job for the covered entity. He did not further use or disclose the PHI. This was not a breach of PHI as long as Bill did not further use or disclose the information accessed in a manner not permitted by the Privacy Rule. INTERNAL USE ONLY 47
Question 11 Rhonda is a receptionist for a covered entity, and, due to her work responsibilities, she is not authorized to access PHI. Rhonda decides to look through patient files to learn about a friend’s last visit to the doctor. • Does Rhonda’s action constitute a breach? a) Yes b) No INTERNAL USE ONLY 48

Correct Answer a: Yes. Rhonda accessed PHI without a workrelated need to know. This access was not unintentional, done in good faith, or within the scope of her job for the covered entity. INTERNAL USE ONLY 49
Question 12 Rob, a research assistant, wanted to get ahead on some statistical work, so he copied the information from 240 research participants to his thumb drive. The information included PHI, and the thumb drive was not encrypted. On his way home to continue his work, he stopped by the store to get some snacks. When he returned to his car, he found it had been broken into. Missing were his GPS, dozens of CDs, and his book bag containing the thumb drive. • Does this event constitute a breach? a) Yes b) No INTERNAL USE ONLY 50

Correct Answer a: Yes. Unsecured PHI was stolen because thumb drive was unencrypted. Actually, Rob violated many UA policies: – Removed confidential information from the unit without approval – Used his personal portable computing device for UA business without senior management approval – Copied confidential information to a portable computing device without senior management approval – Used a portable computing device that was not encrypted INTERNAL USE ONLY 51
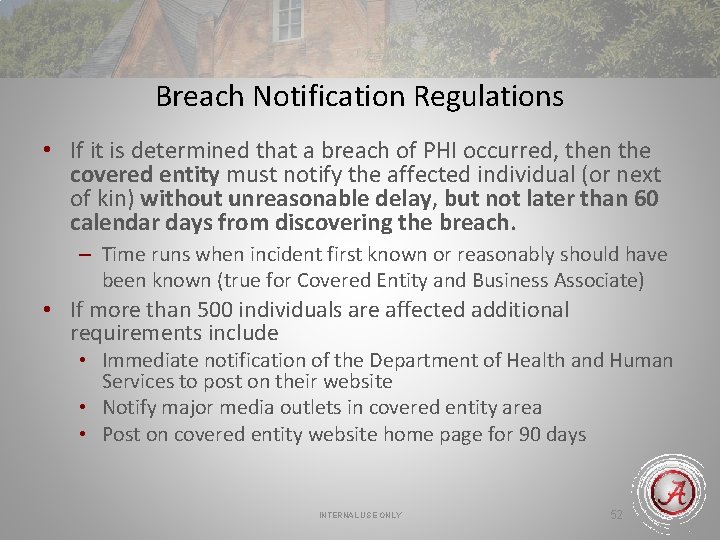
Breach Notification Regulations • If it is determined that a breach of PHI occurred, then the covered entity must notify the affected individual (or next of kin) without unreasonable delay, but not later than 60 calendar days from discovering the breach. – Time runs when incident first known or reasonably should have been known (true for Covered Entity and Business Associate) • If more than 500 individuals are affected additional requirements include • Immediate notification of the Department of Health and Human Services to post on their website • Notify major media outlets in covered entity area • Post on covered entity website home page for 90 days INTERNAL USE ONLY 52
Responsibility to Report • When receiving a privacy complaint, learning of a suspected breach in privacy or security, or noticing something is “just not right, ” we must work together • Immediately; cooperatively; efficiently; carefully; and confidentially • If you notice, hear, see, or witness any activity that you think might be a breach of privacy or security, please let your organization’s privacy and/or security officer know immediately • It is much better to investigate and discover no breach than to wait and later discover that something DID happen INTERNAL USE ONLY 53

Question 13 If you suspect that there has been a breach of HIPAA Policies in your workplace, you should report your suspicions to a) University Police b) University Office of Legal Counsel c) HIPAA Privacy or Security Officer assigned to your workplace INTERNAL USE ONLY 54
Correct Answer c: The HIPAA Privacy or Security Officer for your workplace should be notified of any possible breach of HIPAA Policies. The employee who reports such suspicions is protected from any repercussions for making his/her concerns known to the HIPAA Officer. INTERNAL USE ONLY 55
Security Standards – General Rules • HIPAA security standards ensure the confidentiality, integrity, and availability of PHI created, received, maintained, or transmitted electronically (PHI –Protected Health Information) by and with all facilities • Protect against any reasonably anticipated threats or hazards to the security or integrity or such information • Protect against any reasonably anticipated uses or disclosures of such information that are not permitted INTERNAL USE ONLY 56
Rules for Access • Access to computer systems and information is based on your work duties and responsibilities • Access privileges are limited to only the minimum necessary information you need to do your work • Access to an information system does not automatically mean that you are authorized to view or use all the data in that system • Different levels of access for personnel to PHI is intentional • If job duties change, clearance levels for access to PHI is reevaluated • Access is eliminated if employee is terminated • Accessing PHI for which you are not cleared or for which there is no job-related purpose will subject you to sanctions INTERNAL USE ONLY 57
Question 14 Once employees have completed HIPAA training, their access to PHI is a) Unlimited b) Based on work duties and responsibilities c) Limited to the minimum necessary information to complete required work d) Both B and C INTERNAL USE ONLY 58
Correct Answer d: Access to PHI is based on need-to-know which is determined by the employee’s duties and responsibilities. The employee should access the minimum PHI necessary to complete the required task. INTERNAL USE ONLY 59
Rules for Protecting Information • Do not allow unauthorized persons into restricted areas where access to PHI could occur • Arrange computer screens so they are not visible to unauthorized persons and/or patients; use security screens in areas accessible to public • Log in with password, log off prior to leaving work area, and do not leave computer unattended • Close files not in use/turn over paperwork containing PHI • Do not duplicate, transmit, or store PHI without appropriate authorization • Storage of PHI on unencrypted removable devices (Disk/CD/DVD/Thumb Drives) is prohibited without prior authorization INTERNAL USE ONLY 60
Encryption of PHI • Encryption is generally necessary to protect information outside of the Electronic Medical Records (EMR) system • Use of other mobile media for accessing and transporting PHI such as smart phones, i. Pads, Netbooks, thumb drives, CDs, DVDs, etc. , presents a very high risk of exposure and requires appropriate authorization • Use of any personally owned laptops, desktops or other mobile devices (non-UA equipment) for accessing PHI requires appropriate authorization INTERNAL USE ONLY 61
Password Management • Do not allow coworkers to use your computer without first logging off your user account • Do not share passwords or reuse expired passwords • Do not use passwords that can be easily guessed (dictionary words, pets name, birthday, etc. ) • Choose new passwords when they must be reset • Should not be written down, but if writing down the password is required, must be stored in a secured location • Should be changed if you suspect someone else knows it • Disable passwords or delete accounts when employees leave • Passwords: – – Should be minimum 8 characters long Include 3 of 4 data types (upper/lower case, numeric, special characters) Should be changed periodically Good password scheme is critical for complex passwords – R 0 llt!de (don’t use this, just an example) INTERNAL USE ONLY 62
Question 15 Is it acceptable to share your computer password with your fellow employees if they have received HIPAA training. a) Yes b) No INTERNAL USE ONLY 63
Correct Answer b: No. You should not share you computer password. INTERNAL USE ONLY 64
Protection from Malicious Software • • Malicious software can be thought of as any virus, worm, malware, adware, etc. As a result of an unauthorized infiltration, PHI and other data can be damaged or destroyed Notify your supervisor, system support representative, and/or security officer immediately if you believe your computer has been compromised or infected with a virus—do not continue using computer until resolved The University provides standard, managed anti virus and other security software Do not disable anti-virus or other security software on individual workstations Any personal devices used for access to PHI must have appropriate anti virus software Do not open e-mail or attachments from an unknown, suspicious, or untrustworthy source or if the subject line is questionable or unexpected—DELETE THEM IMMEDIATELY INTERNAL USE ONLY 65
Rules for Disposal of Computer Equipment • • Only authorized employees should dispose of PHI in accordance with retention policies Documents containing PHI or other sensitive information must be shredded when no longer needed. Shred immediately or place in securely locked boxes or rooms to await shredding. All questions concerning media reallocation and disposal should be directed to your HIPAA Security Officer; OIT systems representatives are responsible for sanitization and destruction methods Media, such as CDs, disks, or thumb drives, containing PHI/sensitive information must be cleaned or sanitized before reallocating or destroying “Sanitize” means to eliminate confidential or sensitive information from computer/electronic media by either overwriting the data or magnetically erasing data from the media If media are to be destroyed, then once they are sanitized, place them in specially marked secure containers for destruction NOTES: Deleting a file does not actually remove the data from the media. Formatting does not constitute sanitizing the media INTERNAL USE ONLY 66
Use of Technology • Use of other mobile media for accessing and transporting PHI such as smart phones, i. Pads, Netbooks, thumb drives, CDs, DVDs, etc. , presents a very high risk of exposure and requires appropriate authorization • Email, internet use, fax and telephones are to be used for UA business purposes (see UA policies) • Fax of PHI should only be done when the recipient can be reliably identified; Verify fax number and recipient before transmitting • No PHI is permitted to leave facility in any format without prior approval • Where technically feasible, email should be avoided when communicating unencrypted sensitive PHI - follow your organization’s email policy for PHI • No PHI is permitted on any social networking sites (Twitter, Facebook, My. Space, etc. ) • No PHI is permitted on any texting or chat platforms (AOL, MSN, cell phones) INTERNAL USE ONLY 67
Question 16 Your office computer is being replaced. You should a) Delete all files that might contain sensitive information b) Have the computer sent to surplus for secure storage c) Contact your HIPAA Security Officer to initiate steps to sanitize the computer INTERNAL USE ONLY 68
Correct Answer c: Contact your HIPAA Security Officer. Deleting files from a hard drive will not permanently remove the files from the computer. Computers should not be taken to surplus until they have been sanitized. Not all used computers go to surplus. Some are reassigned for further use. INTERNAL USE ONLY 69
Facility Access Controls • Help to monitor the controls we have for Facility Access – Sign-in Visitors and Vendors (as required) – Insure that locks, card access, or any other physical access controls are working as expected • Report any problems or possible problems to your security officer INTERNAL USE ONLY 70
Reporting Security Incidents • Notify your Security Officer of any unusual or suspicious incident • Security incidents include the following: – – – – Theft of or damage to equipment Unauthorized use of a password Unauthorized use of a system Violations of standards or policy Computer hacking attempts Malicious software Security Weaknesses Breaches to patient, employee, or student privacy INTERNAL USE ONLY 71
Contacts and References • Know Your Security and Privacy Officer: – – – – Medical Center Privacy/Security Officer is Jan Chaisson Brewer Porch Privacy/Security Officer is Warren Williams Speech and Hearing Privacy/Security Officer is Becca Brooks Autism Spectrum Disorders Clinic Privacy/Security Officer is Kelly Mc. Kinnon UA Group Health Plan/FSA Privacy/Security Officer is Dave Bertanzetti Youth Services Institute Privacy/Security Officer is Karan Singley UA Privacy Officer: Jan Chaisson UA Security Officer: Ashley Ewing • Other References – Privacy: • www. hhs. gov/ocr/hipaa – Security: • www. cms. hhs. gov/Security. Standard INTERNAL USE ONLY 72

Training Certification • Please Complete the Training Acknowledgement Form to Obtain Credit for Completing the Annual Training INTERNAL USE ONLY 73
 Cvs privacy awareness and hipaa privacy training
Cvs privacy awareness and hipaa privacy training Hipaa privacy and security awareness training
Hipaa privacy and security awareness training Azure pci dss responsibility matrix
Azure pci dss responsibility matrix Air force hipaa training
Air force hipaa training Jcaho standards
Jcaho standards Ada hipaa compliance kit
Ada hipaa compliance kit Hipaa security rule self assessment toolkit
Hipaa security rule self assessment toolkit Hipaa objectives
Hipaa objectives Chapter 9 privacy security and ethics
Chapter 9 privacy security and ethics Chapter 9 privacy security and ethics
Chapter 9 privacy security and ethics Chapter 9 privacy security and ethics
Chapter 9 privacy security and ethics What is the destructive event or prank the virus delivers
What is the destructive event or prank the virus delivers Private securit
Private securit Hipaa training georgia
Hipaa training georgia Accountable hipaa training
Accountable hipaa training Hipaa training strategies
Hipaa training strategies Hipaa training for nurses
Hipaa training for nurses Chapter 8 training and developing employees
Chapter 8 training and developing employees Chapter 8 training and development
Chapter 8 training and development The process of selecting training and evaluating employees
The process of selecting training and evaluating employees Ibp training
Ibp training Personal information lifecycle
Personal information lifecycle Grooming ppt
Grooming ppt Iso 9001 awareness
Iso 9001 awareness Code of conduct training presentation
Code of conduct training presentation Gmp training modules
Gmp training modules Need analysis example
Need analysis example Compliance training for managers
Compliance training for managers Eeo compliance training
Eeo compliance training Medicare parts c and d general compliance training answers
Medicare parts c and d general compliance training answers Security compliance monitoring
Security compliance monitoring Oeaa baa
Oeaa baa Product compliance training
Product compliance training Overt discrimination
Overt discrimination Auto dealership compliance training
Auto dealership compliance training Board of directors compliance training
Board of directors compliance training Danaher connect compliance training
Danaher connect compliance training Utsa compliance training
Utsa compliance training Plu campus safety
Plu campus safety Compliance training strategies
Compliance training strategies Epa compliance training
Epa compliance training Geisingerconnect
Geisingerconnect Wireless security in cryptography and network security
Wireless security in cryptography and network security Integrity in e commerce
Integrity in e commerce Chapter 10 motivating and satisfying employees and teams
Chapter 10 motivating and satisfying employees and teams Motivating and satisfying employees and teams
Motivating and satisfying employees and teams Chapter 10 motivating and satisfying employees and teams
Chapter 10 motivating and satisfying employees and teams Motivating and satisfying employees and teams
Motivating and satisfying employees and teams Copyright
Copyright Hippa secure now
Hippa secure now Joint commission accreditation standards
Joint commission accreditation standards Hipaa pre-existing condition protections
Hipaa pre-existing condition protections Gillman hipaa progress note
Gillman hipaa progress note Hippa cow
Hippa cow Jira hipaa
Jira hipaa Gillman hipaa progress note
Gillman hipaa progress note Certified hipaa administrator
Certified hipaa administrator Hipaa summit
Hipaa summit What does tpo stand for in hipaa
What does tpo stand for in hipaa When should you promote hipaa awareness
When should you promote hipaa awareness What is hipaa
What is hipaa What is hipaa
What is hipaa Hipaa vs hippocratic oath
Hipaa vs hippocratic oath Hipaa vs hippa
Hipaa vs hippa Hipaa law louisiana
Hipaa law louisiana Hipaa summit
Hipaa summit Hipaa frequently asked questions
Hipaa frequently asked questions Hipaa breach notification decision tree
Hipaa breach notification decision tree Hipaa principles
Hipaa principles Ferpa hipaa
Ferpa hipaa Gremote.geisinger
Gremote.geisinger Becoming hipaa compliant
Becoming hipaa compliant Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Typiska drag för en novell
Typiska drag för en novell