Positioning Draping Amanda La Londe PT DPT GCS




- Slides: 33
Positioning / Draping Amanda La. Londe, PT, DPT, GCS PT 6280 Ch. 6 -7 in text
Objectives Understand the purpose of draping and positioning u Demonstrate correct draping techniques u Identify properly supported patient position for supine, sidelying, and prone u Understand supported positioning for sitting in a w/c u Understand the complications of improper long-term positioning u
Key Terms u Draping – The covering of patients to only expose only the body parts needed for treatment u Contracture – Shortening or tightening of the skin, muscle, fascia and/or joint capsule – Prevents normal movement u Shear – A force that causes an opposite, but parallel sliding motion of the planes of an object u Spasticity - A form of hypertonicity - Gradual increase in resistance to movement
Short-Term Positioning u Safety u u Comfort u u Safe, protected, non-restrictive position Maintain spinal alignment PT Access u Position so intervention can be performed
Short-Term Positioning Checklist: u Is the patient safe? u Do they have good alignment? u Are the necessary areas accessible (and only the necessary areas)? u Are the trunk and extremities supported for comfort?
Treatment Preparation u Gather needed items ahead of time u Linen, u Prepare pillows, modalities the treatment table u Minimal adjustment after the patient gets on the table u Drape areas not needed to be exposed u Inform your patient
Preparation of the Table u Materials needed – 2 full sized sheets – 2 pillows and pillow cases – 2 towels
Table Preparation, cont. – Place one full size sheet (folded lengthwise) on plinth – Place a towel at each end of table – Place a folded sheet on the table to be used as a drape – Have additional pillows, towels, blankets, etc. ready
Preparation of the Patient: – Instruct the patient in what they are to take off u Provide gowns & a dressing room – Tell the person how to position on the table u Easily understood terms – Assist them as much as needed to support weak or injured parts u Help patient “keep their dignity”
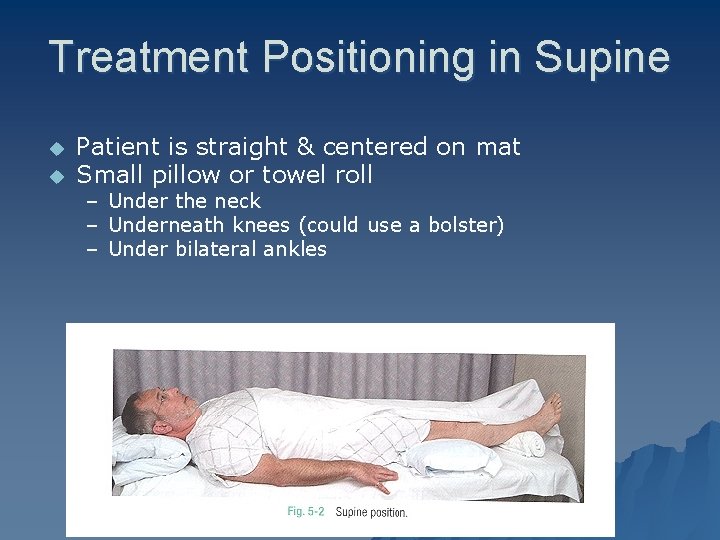
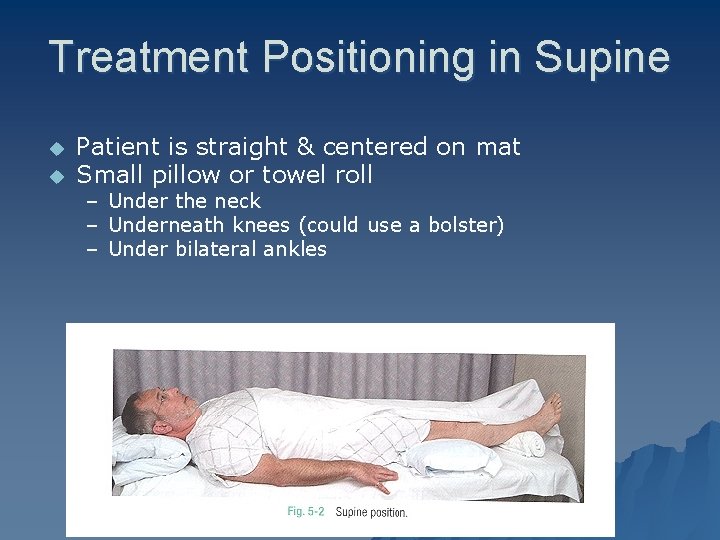
Treatment Positioning in Supine u u Patient is straight & centered on mat Small pillow or towel roll – Under the neck – Underneath knees (could use a bolster) – Under bilateral ankles
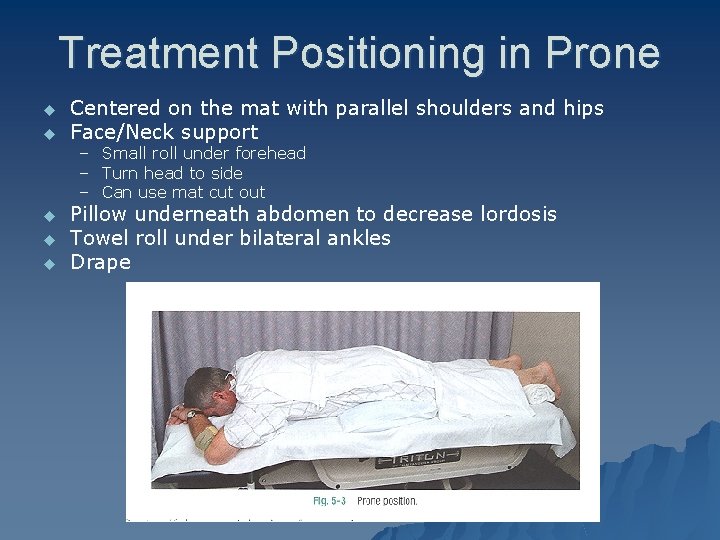
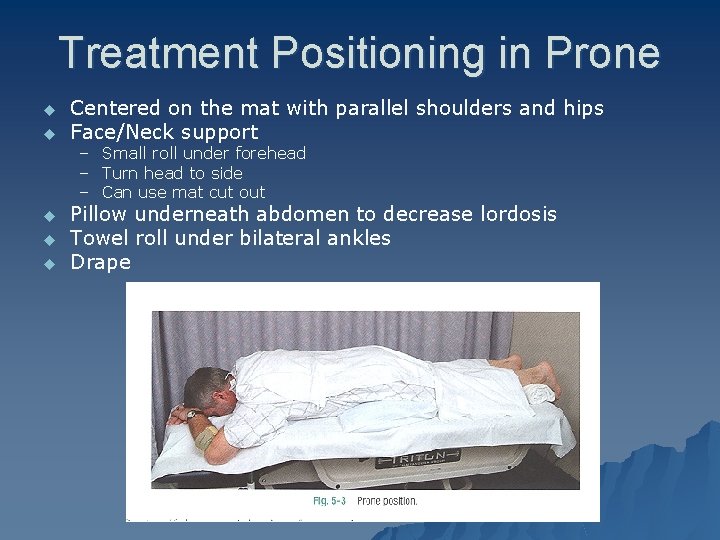
Treatment Positioning in Prone u u Centered on the mat with parallel shoulders and hips Face/Neck support – Small roll under forehead – Turn head to side – Can use mat cut out u u u Pillow underneath abdomen to decrease lordosis Towel roll under bilateral ankles Drape
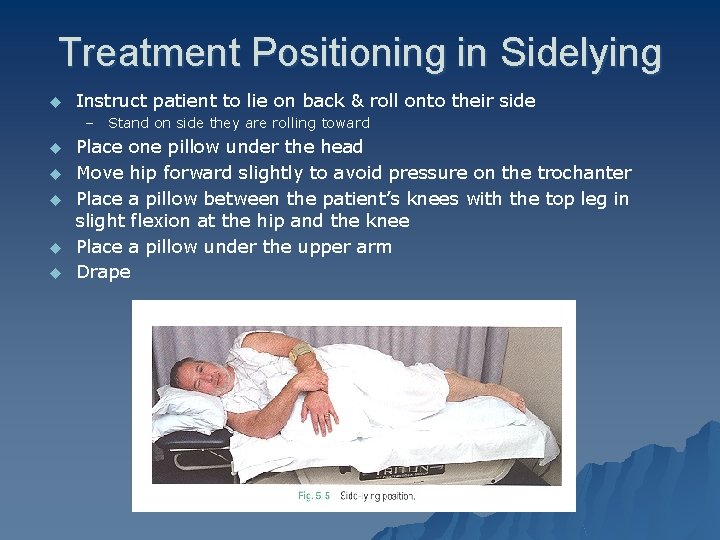
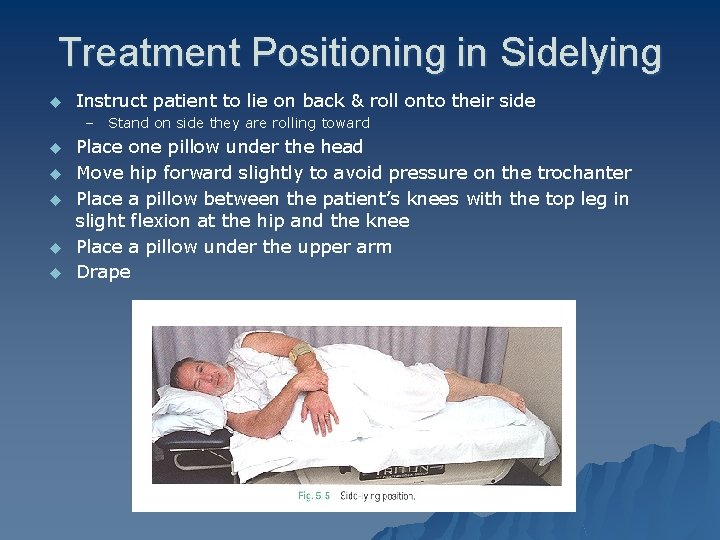
Treatment Positioning in Sidelying u Instruct patient to lie on back & roll onto their side – Stand on side they are rolling toward u u u Place one pillow under the head Move hip forward slightly to avoid pressure on the trochanter Place a pillow between the patient’s knees with the top leg in slight flexion at the hip and the knee Place a pillow under the upper arm Drape
Draping u Reposition u Access a body part for treatment u After completing treatment Don’t forget about what is (or could be) exposed during your treatment ANTICIPATE
Long-Term Positioning u Also called “Preventative Positioning” u Objectives – Prevent negative effects of long-term immobility u Safety: Maintain open airways, avoid falls, accommodate medical limitations u Prevention: Prevent pressure ulcers, contractures, edema and promote function of body systems u Comfort: Normal alignment, and relieve jt stress
Assessing the Patient – Level of consciousness – Medical or surgical precautions – Are they in pain – Do they have a loss of sensation – What is their muscular function – Do they have spasticity or other abnormal muscle tone
Assessing the Patient – Amount of tissue to protect bony prominences – Any bowel or bladder incontinence – Can they assist – Do they have contractures u Acute (developing) or chronic – Do they have edema, skin rashes, redness, irritation, infection
Preventing Pressure Ulcers u Lesion caused by unrelieved pressure – Damage of the underlying tissue Healthy person should reposition in bed at least every 2 hours u Maximum repositioning time in sitting u – 15 minutes u Patients who are medically unstable need to be repositioned more frequently
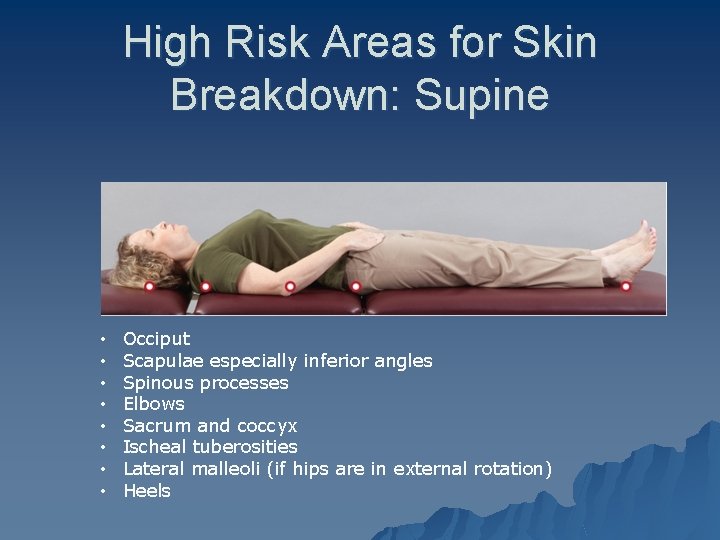
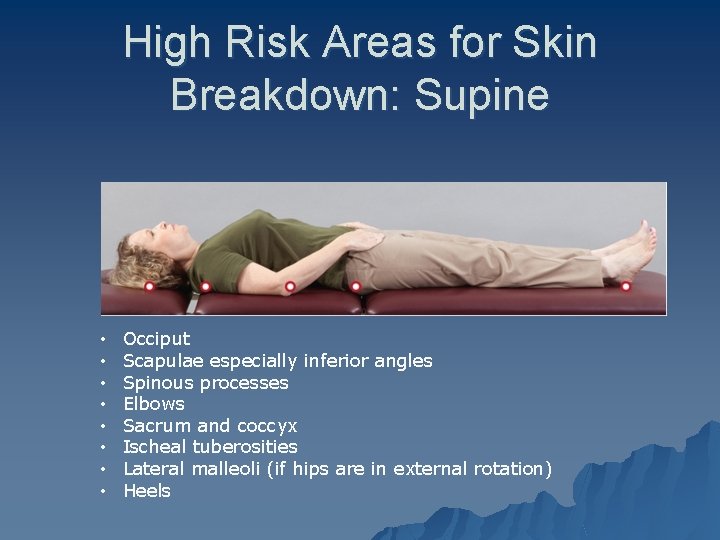
High Risk Areas for Skin Breakdown: Supine Johansson & Chinworth text page 161 • • Occiput Scapulae especially inferior angles Spinous processes Elbows Sacrum and coccyx Ischeal tuberosities Lateral malleoli (if hips are in external rotation) Heels
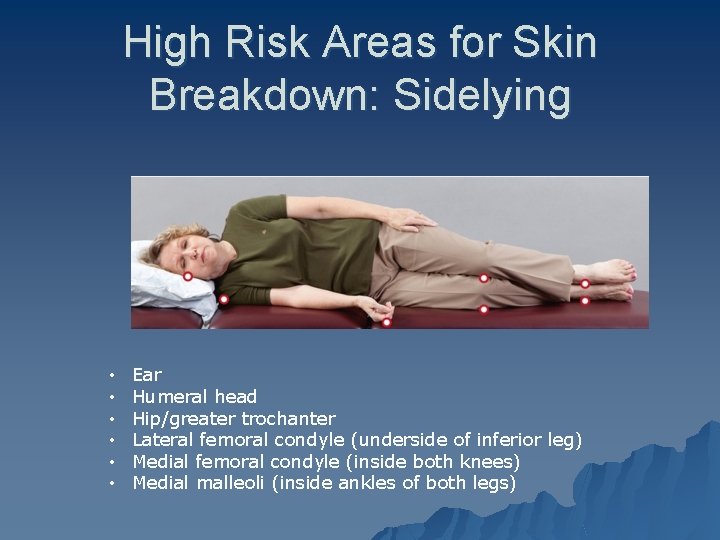
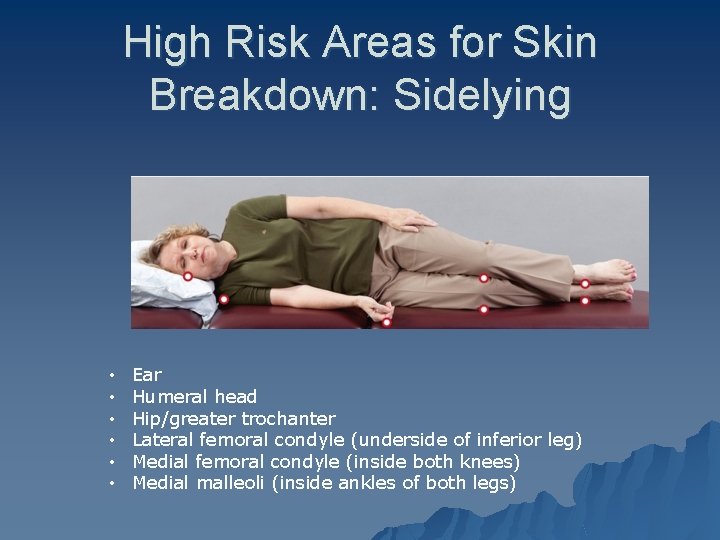
High Risk Areas for Skin Breakdown: Sidelying Johansson & Chinworth text page 162 • • • Ear Humeral head Hip/greater trochanter Lateral femoral condyle (underside of inferior leg) Medial femoral condyle (inside both knees) Medial malleoli (inside ankles of both legs)

High Risk Areas for Skin Breakdown: Sitting u u u u Johansson & Chinworth text page 162 Occiput (in a high back chair) Scapulae (inf. Angles) Spinous processes Elbows (when resting on armrests) Sacrum and coccyx Ischial tuberosities Heels

Precautions: Pressure Ulcers – Avoid folded linens underneath a patient u Remote, cell phone, pens, comb, bed pan, syringe caps, pills, spirometers, pads, sheets, soiled briefs, lines, food, drains. . – Protect bony prominences – Don’t position extremities off of surface – Caution with u Confusion u Decreased sensation u Poor circulation u Altered consciousness

Preventing Contractures u Without movement, stiffness occurs u. Muscles, tendons & ligaments u Physiological changes within a joint cause stiffness u Muscle in a shortened range – Agonist has decrease in sarcomeres – Adhesions form – Antagonist becomes over-lengthened
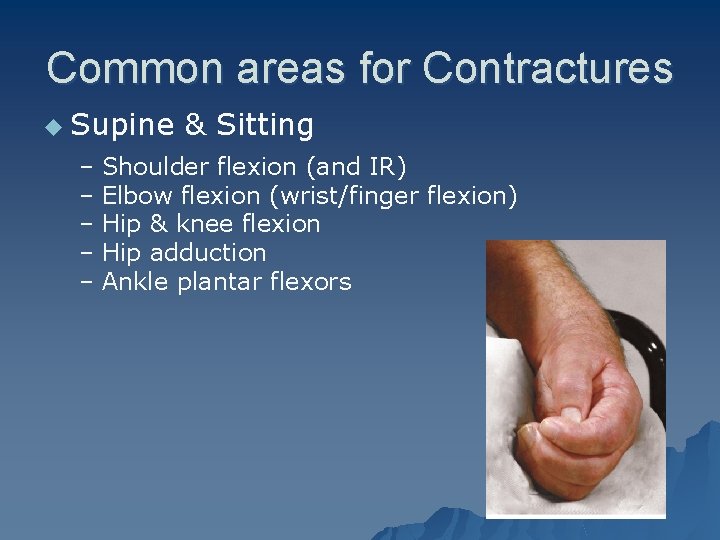
Common areas for Contractures u Supine & Sitting – Shoulder flexion (and IR) – Elbow flexion (wrist/finger flexion) – Hip & knee flexion – Hip adduction – Ankle plantar flexors
Edema & Cardiopulmonary Complications u Return of fluid is facilitated by muscle contractions – Skeletal pumps u Orthostatic Hypotension u Deep vein thrombosis (DVT) u Breathing – With immobility air exchange is ↓ – Body must rely on gravity to drain moisture from lungs

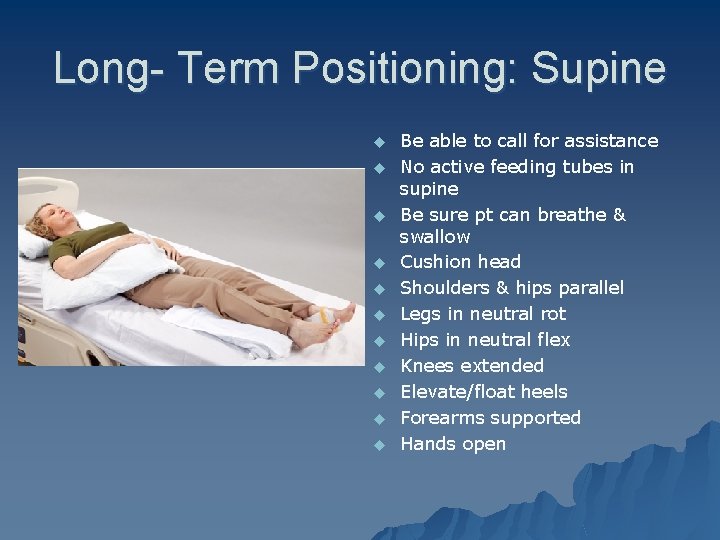
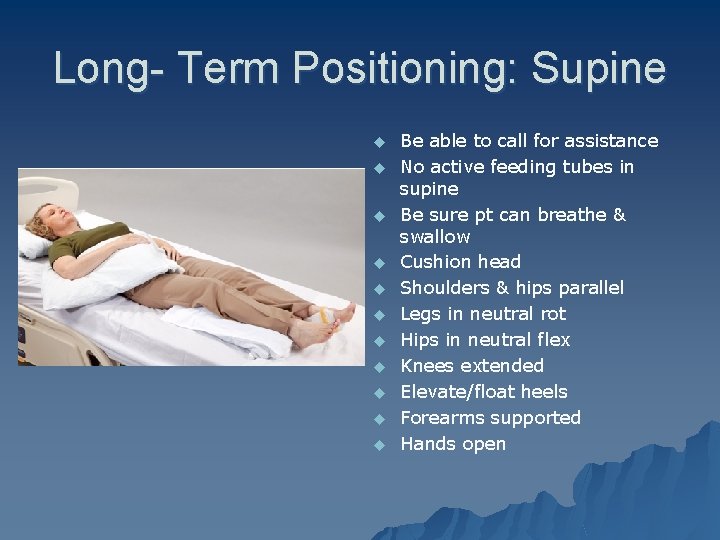
Long- Term Positioning: Supine u u u Johansson & Chinworth text page 166 u u u Be able to call for assistance No active feeding tubes in supine Be sure pt can breathe & swallow Cushion head Shoulders & hips parallel Legs in neutral rot Hips in neutral flex Knees extended Elevate/float heels Forearms supported Hands open
Long-Term Positioning: Sidelying u Be able to call for assistance u Airway clear u Head cushioned u Body aligned and centered on bed u Rotate trunk slightly forward/underside hip forward u Underside knee straight/top leg flexed u Pillow between knees & ankles u Upper arm abducted u Underneath scapula int. rot. (protracted) u Elbow straight u Arm and hand supported u Can tuck pillow behind the pt to maintain position
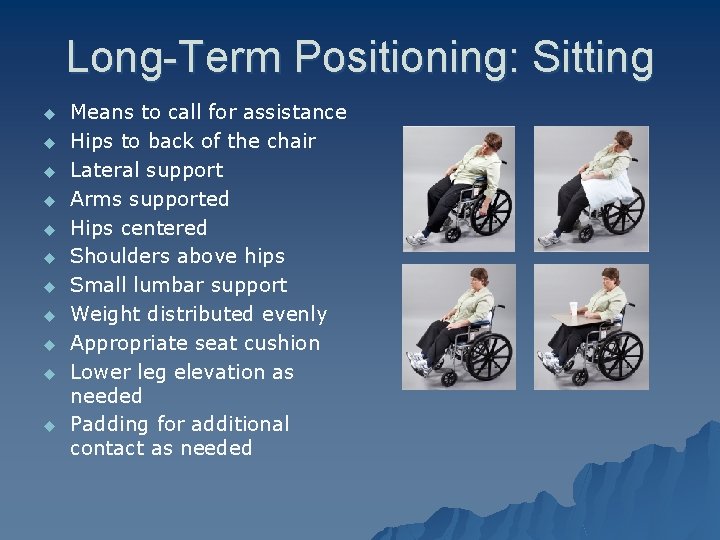
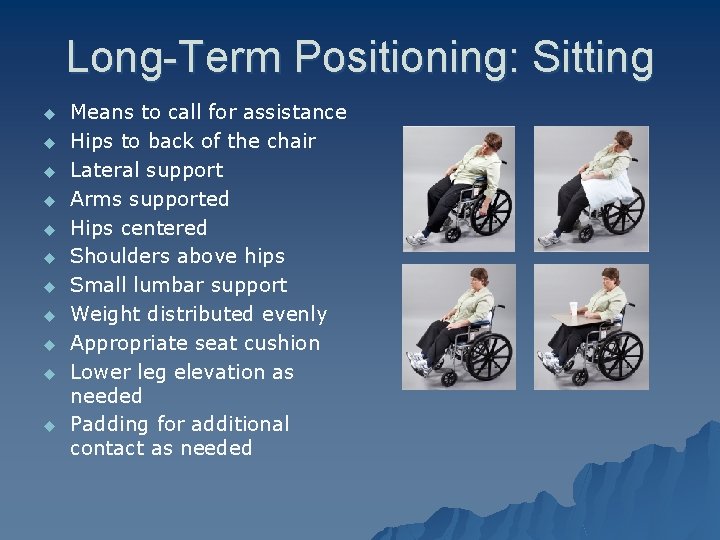
Long-Term Positioning: Sitting u u u Means to call for assistance Hips to back of the chair Lateral support Arms supported Hips centered Shoulders above hips Small lumbar support Weight distributed evenly Appropriate seat cushion Lower leg elevation as needed Padding for additional contact as needed
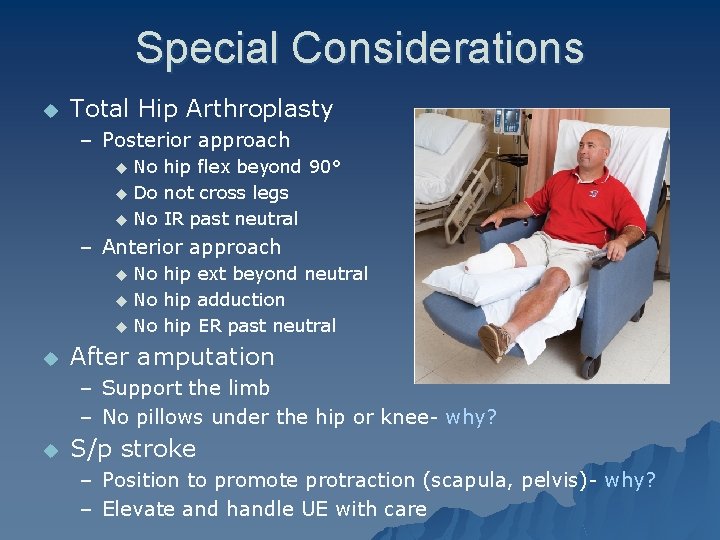
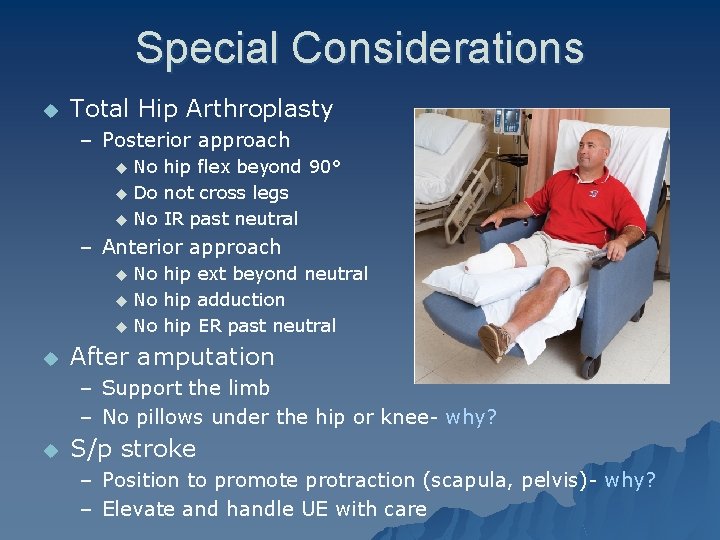
Special Considerations u Total Hip Arthroplasty – Posterior approach No hip flex beyond 90° u Do not cross legs u No IR past neutral u – Anterior approach No hip ext beyond neutral u No hip adduction u No hip ER past neutral u u After amputation – Support the limb – No pillows under the hip or knee- why? u S/p stroke – Position to promote protraction (scapula, pelvis)- why? – Elevate and handle UE with care
Objectives Re-Visited Understand the purpose of draping and positioning u Demonstrate correct draping techniques u Identify properly supported patient position for supine, sidelying, and prone u Understand supported positioning for sitting in a w/c u Understand the complications of improper long-term positioning u
Lab u Review each of the scenarios u Complete as therapist and patient