Skin preparation draping and patient positioning Module 1
- Slides: 11
Skin preparation, draping, and patient positioning Module 1: Principles of soft-tissue management Faculty name Affiliation Fundamentals of Soft-Tissue Management Date
Disclosures I have no financial relationships with commercial entities that produce health-care related products. OR The commercial entities with which I have a financial relationship do not produce health-care related products or services relevant to the content of my presentation. OR I disclose the following financial relationships with commercial entities that produce health-care related products or services: Consultant for: Advisory Board for: Employee of: Grant/Research support from: Honoraria from: Stockholder in: Speaker/teacher for: 2
Learning objectives 1. Describe procedure for skin preparation. I. Washing in general II. Hair removal III. Skin preparation in particular a. Selection of antiseptics b. Application of antiseptics c. Safe handling, storage, and disposal of antiseptics 2. Describe principles of patient draping. 3. Describe basic strategies of patient positioning. 4
Skin preparation: Why do we need it? • Prevention of Surgical Site Infections (SSI): 5 • 2 nd most common hospital-acquired infection • Doubles patient’s mortality • Need for intensive care treatment increases by 60% • Prolongs hospital stay and hospital cost • Can interact with pre- and perioperative risk factors
Skin preparation: Why do we need it? • Reduce patient-based skin flora • Decrease bacterial-load, that may penetrate into the depth (wounds) • Solution of choice: alcohol-based • Solutions need to completely dry prior to the next prep/incision • To allow for adherence of draping to the skin & to be effective • Ideally it lasts for 48 hours despite evaporation of the alcohol base • Combination of Chlorhexidine- and Povidone-iodine result in purple skin discoloration 6
Skin preparation: 1. Preoperative washing • Bathe or shower before surgery with either plain soap or antimicrobial soap at least the night before or on the day of surgery. [Moderate Evidence] • The use of Chlorhexidine gluconate-impregnated clothes does not seem to be superior in reducing SSI [Low Evidence] 7
Skin preparation: 2. Hair removal • Hair at the surgical site to be left in place. [Strong Evidence] • Patient to be instructed to leave hair in place at surgical site before surgery. [Moderate Evidence] • If removal necessary, use clipping devices (instead depilation or shaver). [Strong Evidence] • When not feasible (e. g. , emergency, patient anxiety), remove in order to prevent hair dispersal in the OR (e. g. wet clipping & suction). 8
Skin preparation: 3. Selection of antiseptics • No one antiseptic is more effective than another for preventing SSI [Strong Evidence] • Octenidin > PVP-iodine and chlorhexidine [Moderate Evidence] • For (screened) patients with a history of multi-resistant bacteria, selection of antiseptics does not change, but may guide antibiotic choice 9
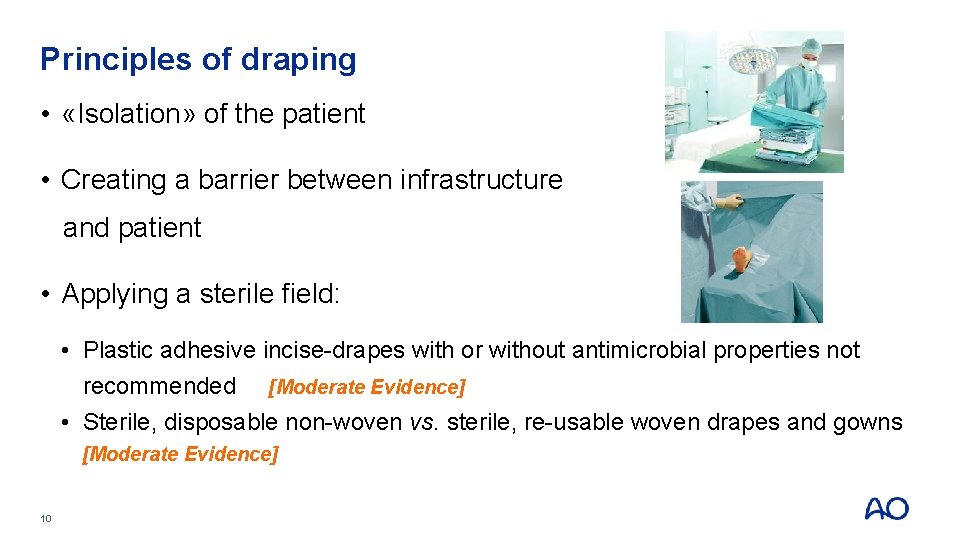
Principles of draping • «Isolation» of the patient • Creating a barrier between infrastructure and patient • Applying a sterile field: • Plastic adhesive incise-drapes with or without antimicrobial properties not recommended [Moderate Evidence] • Sterile, disposable non-woven vs. sterile, re-usable woven drapes and gowns [Moderate Evidence] 10
Strategies of safe patient positioning • Anatomical knowledge • E. g. positioning of extremities and padding of pressure points to avoid skin breakdown and neuropathy • Meticulous planning • E. g. correct alignment (in particular extremities) and exposure of surgical site • Team work • 11 Coordination duties of paramedical and medical staff
Take home messages • Bath or shower before surgery • Do not shave (if necessary to remove hair, use clippers immediately before surgery) • Commercially available antiseptics are all effective (must dry prior to surgery) • Safe patient positioning needs anatomical knowledge, correct padding and teamwork 12