Coma head injury Judita Capkova MD Ph D
![PRESSURE [mm. Hg] INTRACRANIAL PRESSURE (ICP) 40 De-compensation phase Compensation Phase Transition phase 0 PRESSURE [mm. Hg] INTRACRANIAL PRESSURE (ICP) 40 De-compensation phase Compensation Phase Transition phase 0](https://slidetodoc.com/presentation_image_h/1ecbea85a3f3a604e88d8ad28e251aa3/image-19.jpg)


- Slides: 42
Coma, head injury Judita Capkova, MD. Ph. D. Jozef Firment, MD. Ph. D. Department of Anaesthesiology & Intensive Care Medicine Šafárik University Faculty of Medicine, Košice
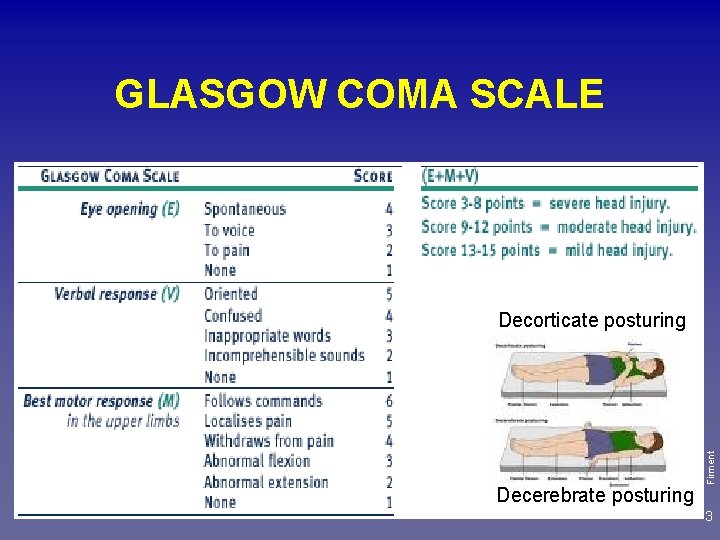
Coma Is a „state of unarousable unresposiviness“ (of unconsciousness from which the patient cannot be aroused) • No evidence of arousal: no spontaneous eye opening, no speech, voluntary limb movement • Unresponsive to external stimuli, although abnormal postures may be • GCS – level of consciousness, coma: GCS ≤ 8 Firment • Involuntary movements (seizures) may occur 2
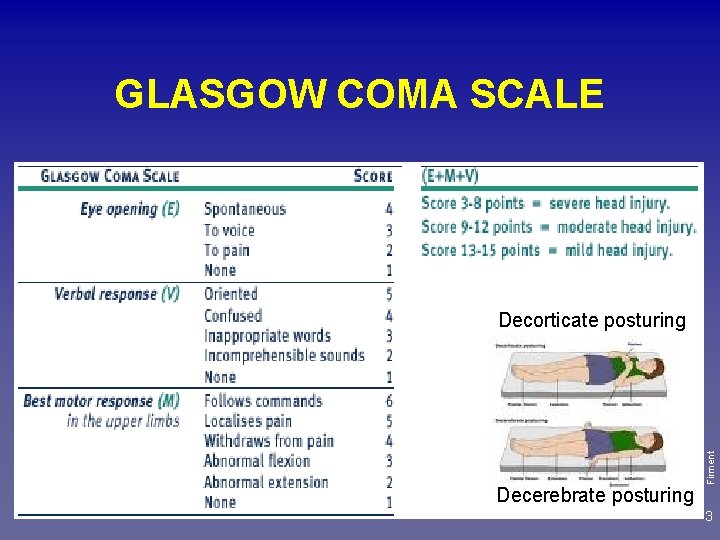
GLASGOW COMA SCALE Decerebrate posturing Firment Decorticate posturing 3
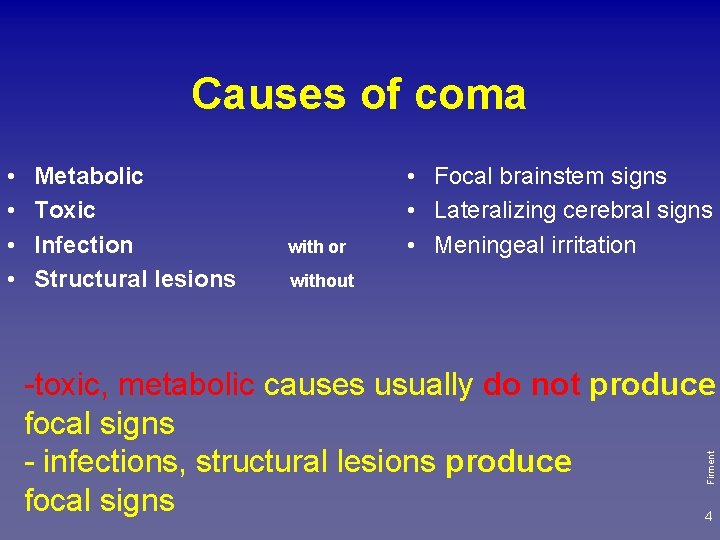
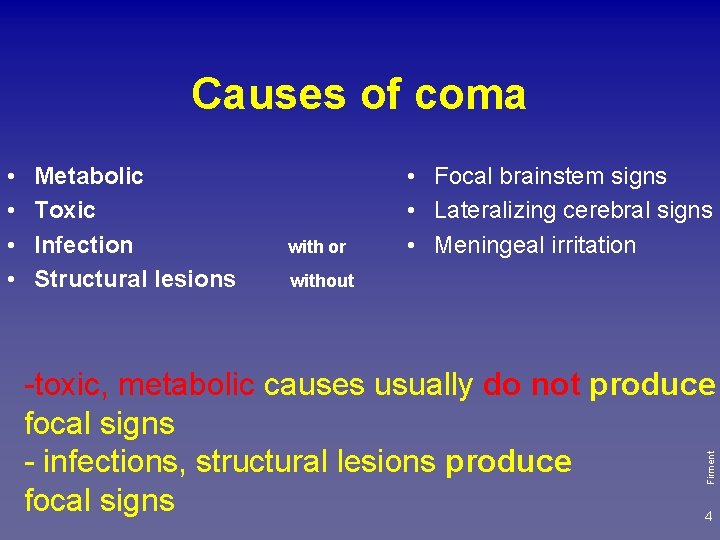
Causes of coma Metabolic Toxic Infection Structural lesions with or • Focal brainstem signs • Lateralizing cerebral signs • Meningeal irritation without -toxic, metabolic causes usually do not produce focal signs - infections, structural lesions produce focal signs 4 Firment • •
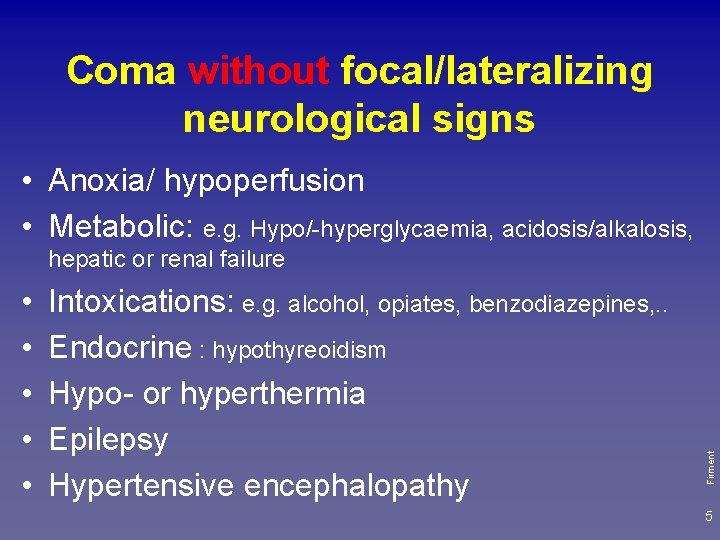
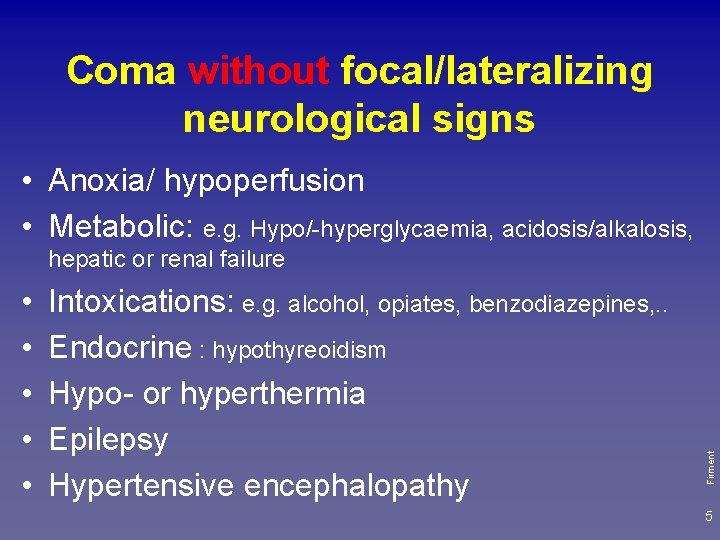
Coma without focal/lateralizing neurological signs • Anoxia/ hypoperfusion • Metabolic: e. g. Hypo/-hyperglycaemia, acidosis/alkalosis, • • • Intoxications: e. g. alcohol, opiates, benzodiazepines, . . Endocrine : hypothyreoidism Hypo- or hyperthermia Epilepsy Hypertensive encephalopathy Firment hepatic or renal failure 5
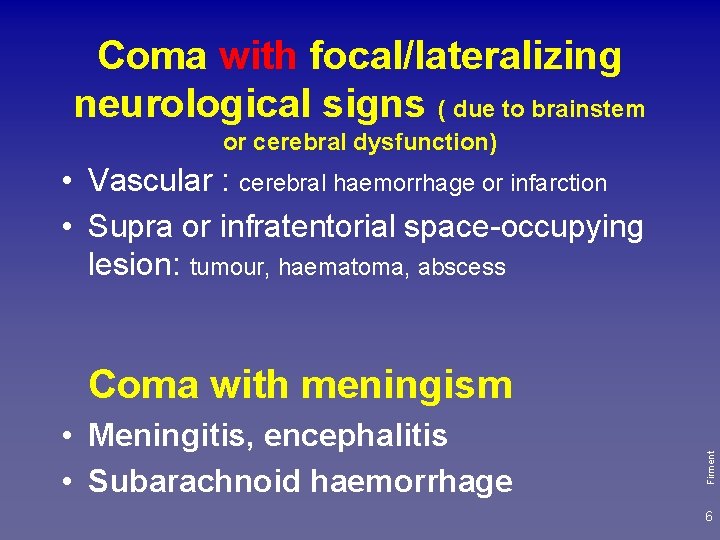
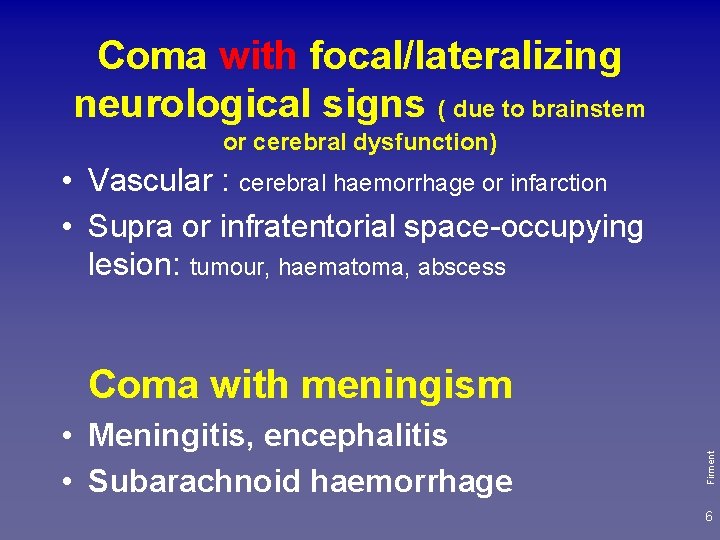
Coma with focal/lateralizing neurological signs ( due to brainstem or cerebral dysfunction) • Vascular : cerebral haemorrhage or infarction • Supra or infratentorial space-occupying lesion: tumour, haematoma, abscess • Meningitis, encephalitis • Subarachnoid haemorrhage Firment Coma with meningism 6
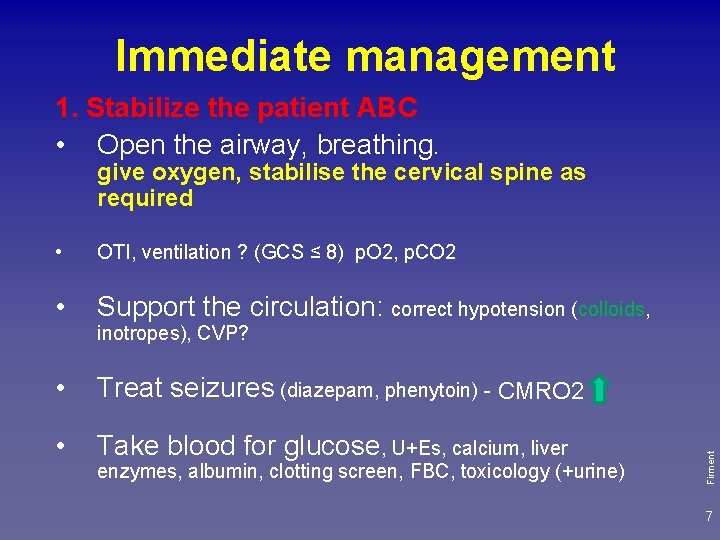
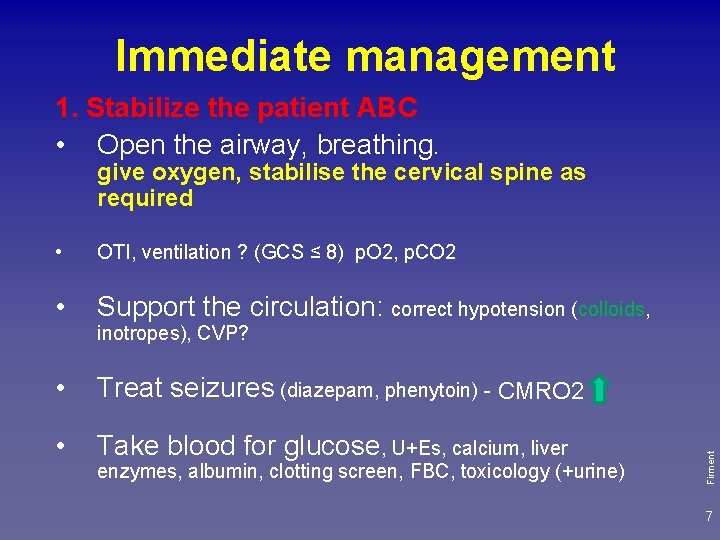
Immediate management 1. Stabilize the patient ABC • Open the airway, breathing. give oxygen, stabilise the cervical spine as required • OTI, ventilation ? (GCS ≤ 8) p. O 2, p. CO 2 • Support the circulation: correct hypotension (colloids, • Treat seizures (diazepam, phenytoin) - CMRO 2 • Take blood for glucose, U+Es, calcium, liver enzymes, albumin, clotting screen, FBC, toxicology (+urine) Firment inotropes), CVP? 7
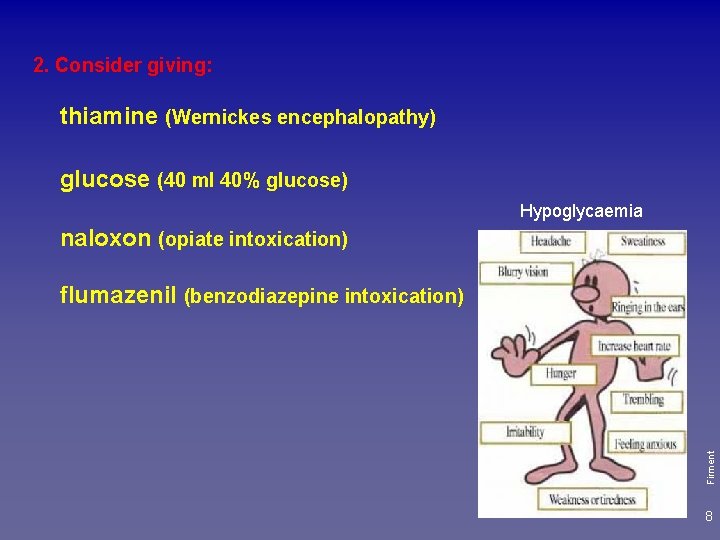
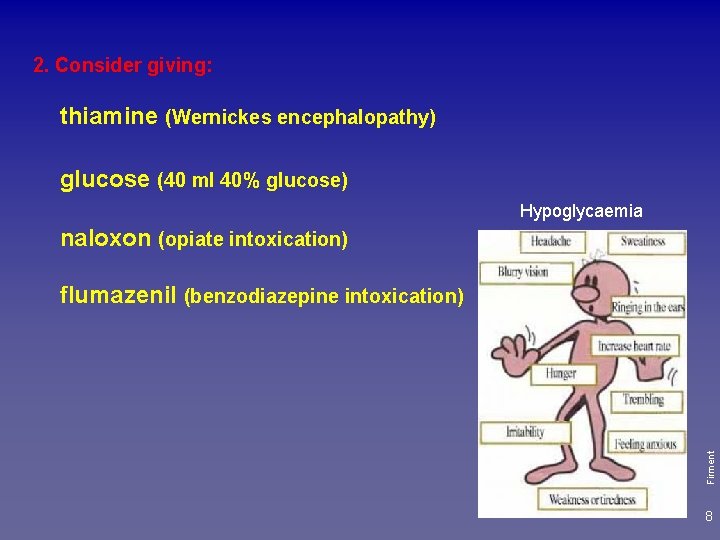
2. Consider giving: thiamine (Wernickes encephalopathy) glucose (40 ml 40% glucose) Hypoglycaemia naloxon (opiate intoxication) Firment flumazenil (benzodiazepine intoxication) 8
3. Examine patient: History General examination • Core temperature, heart rate, rhythm, BP, respiratory pattern, breath, skin, heart, abdomen, fundi Is there meningism? – neck stiffness (inflammation, Asses GCS Look for evidence of brainstem dysfunction Are there lateralizing signs? Firment blood) 9
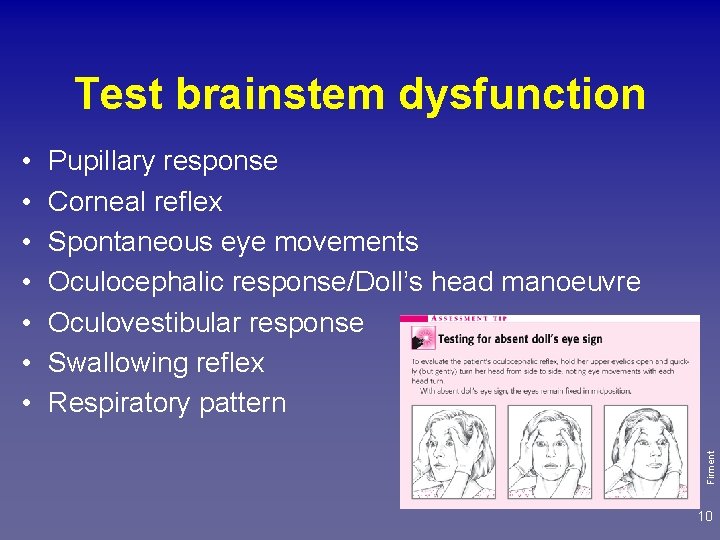
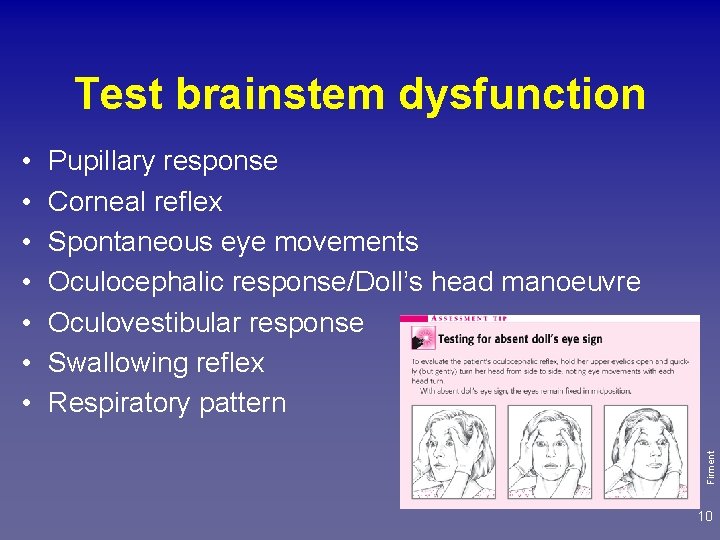
Test brainstem dysfunction Pupillary response Corneal reflex Spontaneous eye movements Oculocephalic response/Doll’s head manoeuvre Oculovestibular response Swallowing reflex Respiratory pattern Firment • • 10
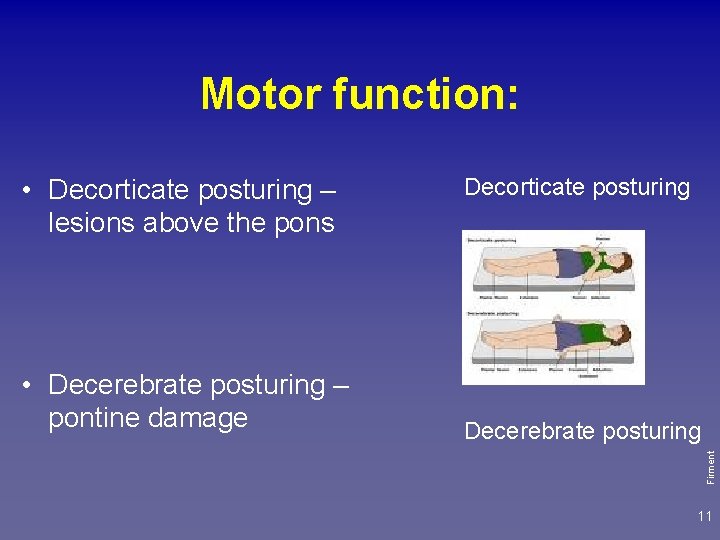
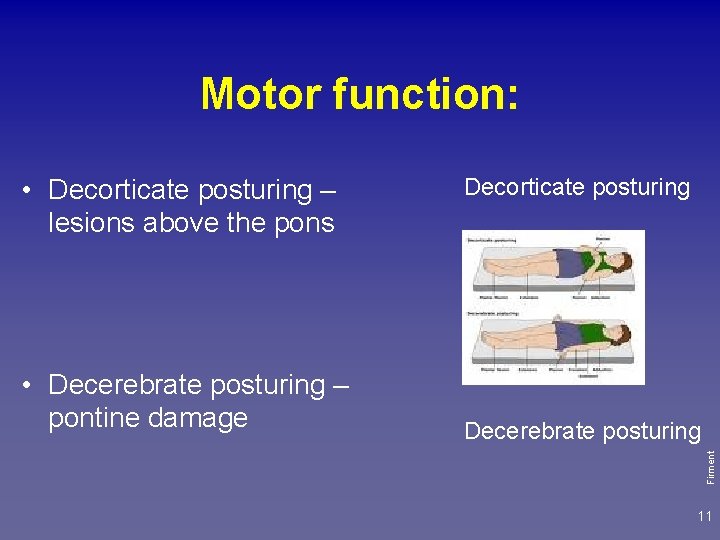
Motor function: • Decerebrate posturing – pontine damage Decorticate posturing Decerebrate posturing Firment • Decorticate posturing – lesions above the pons 11
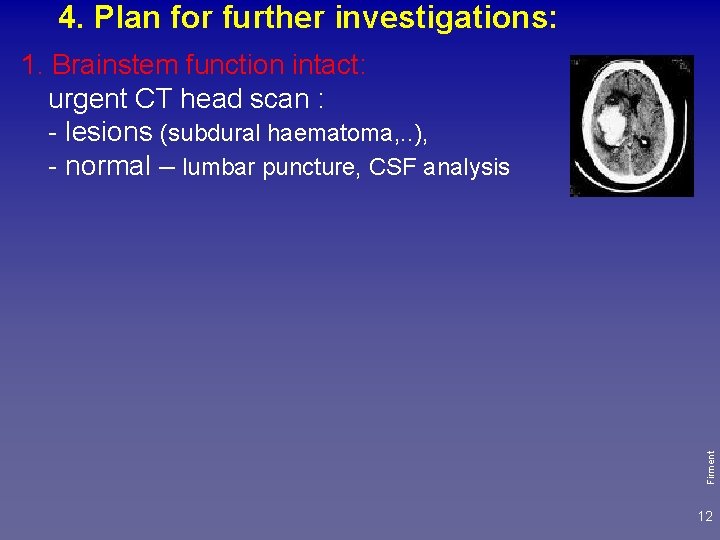
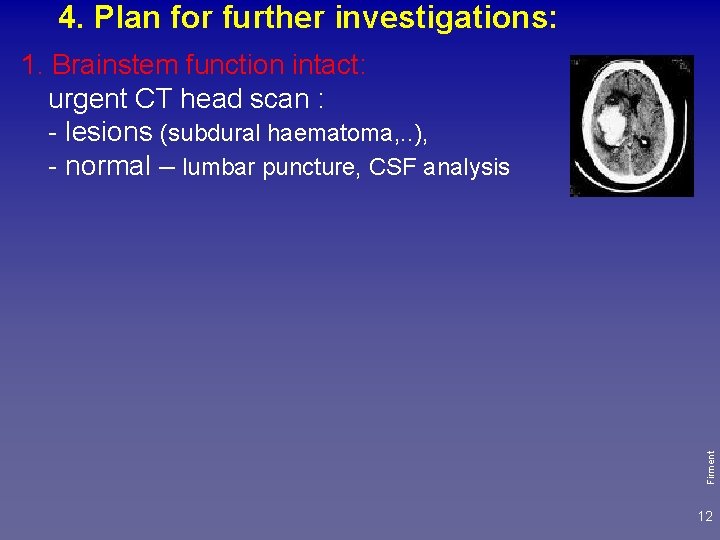
4. Plan for further investigations: Firment 1. Brainstem function intact: urgent CT head scan : - lesions (subdural haematoma, . . ), - normal – lumbar puncture, CSF analysis 12
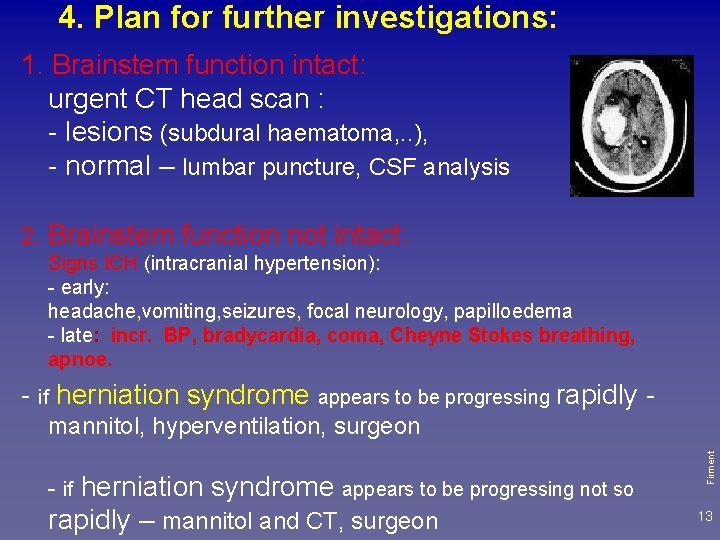
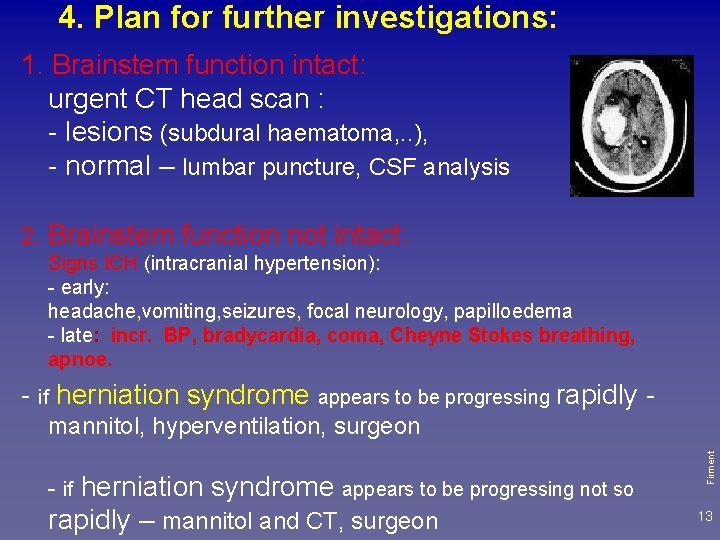
4. Plan for further investigations: 1. Brainstem function intact: urgent CT head scan : - lesions (subdural haematoma, . . ), - normal – lumbar puncture, CSF analysis 2. Brainstem function not intact: Signs ICH (intracranial hypertension): - early: headache, vomiting, seizures, focal neurology, papilloedema - late: incr. BP, bradycardia, coma, Cheyne Stokes breathing, apnoe. - if herniation syndrome appears to be progressing rapidly - if herniation syndrome appears to be progressing not so rapidly – mannitol and CT, surgeon Firment mannitol, hyperventilation, surgeon 13
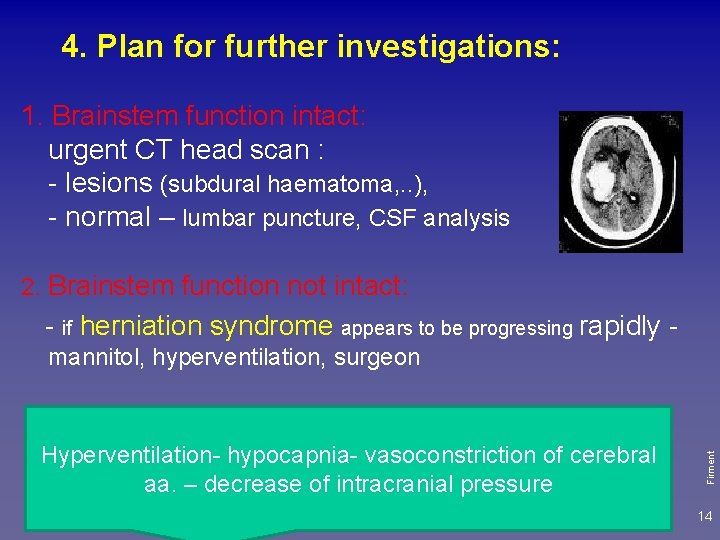
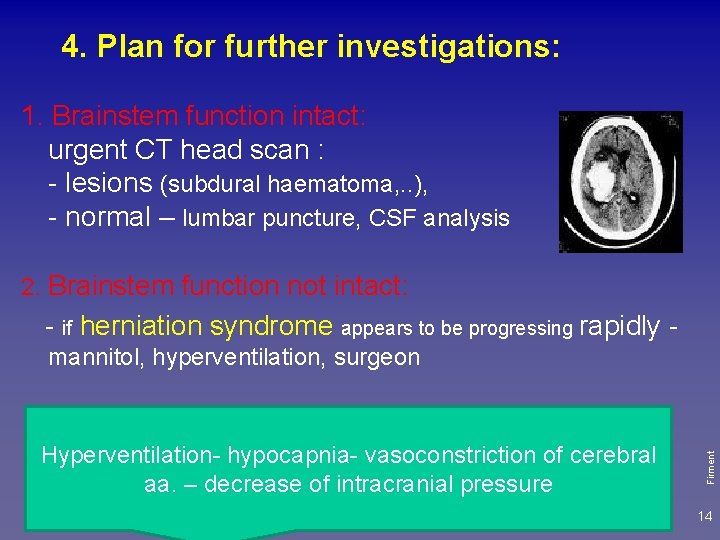
4. Plan for further investigations: 1. Brainstem function intact: urgent CT head scan : - lesions (subdural haematoma, . . ), - normal – lumbar puncture, CSF analysis 2. Brainstem function not intact: - if herniation syndrome appears to be progressing rapidly - if herniation syndrome appears to be progressing not so rapidly – mannitol and CT vasoconstriction of cerebral Hyperventilationhypocapniaaa. – decrease of intracranial pressure Firment mannitol, hyperventilation, surgeon 14
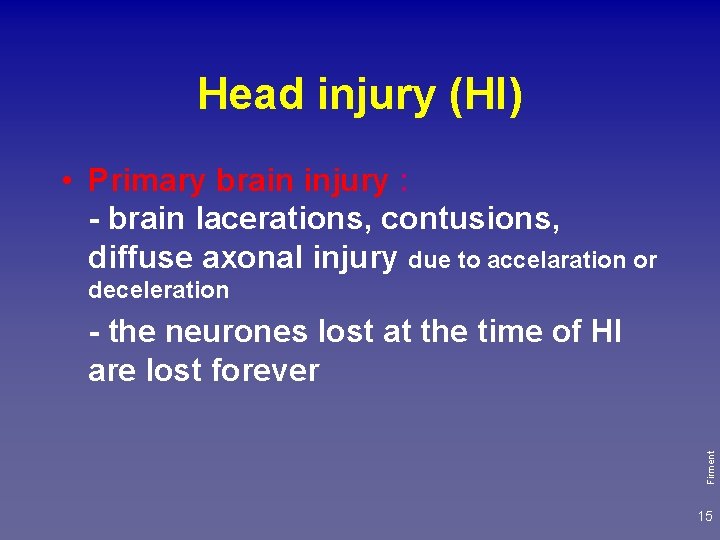
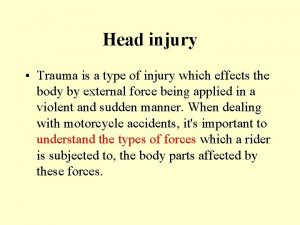
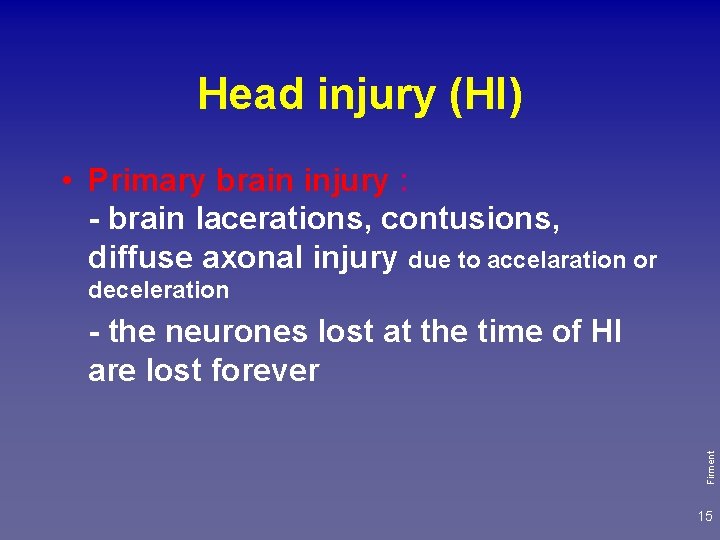
Head injury (HI) • Primary brain injury : - brain lacerations, contusions, diffuse axonal injury due to accelaration or deceleration Firment - the neurones lost at the time of HI are lost forever 15
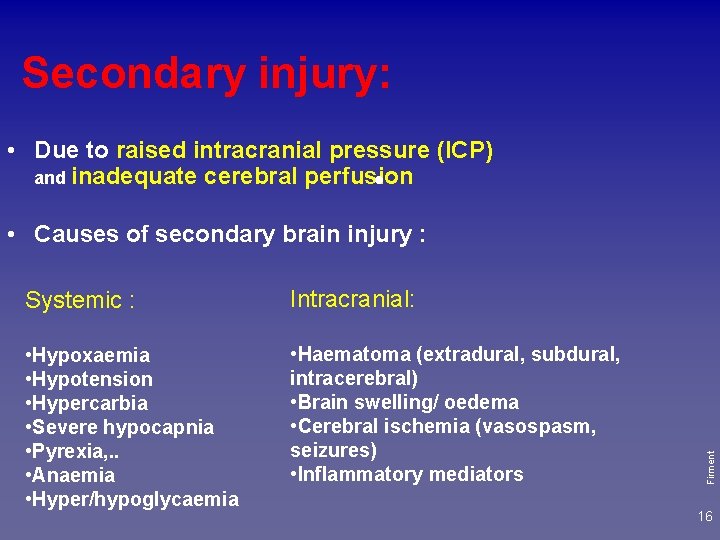
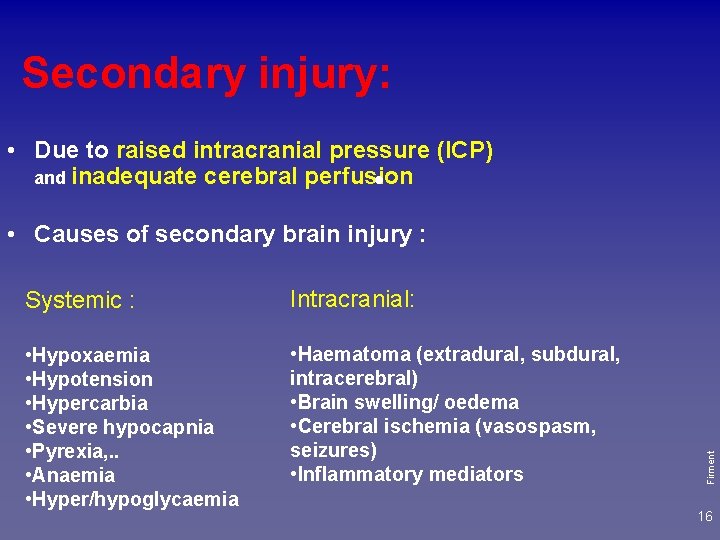
Secondary injury: • Due to raised intracranial pressure (ICP) and inadequate cerebral perfusion • Systemic : Intracranial: • Hypoxaemia • Hypotension • Hypercarbia • Severe hypocapnia • Pyrexia, . . • Anaemia • Hyper/hypoglycaemia • Haematoma (extradural, subdural, intracerebral) • Brain swelling/ oedema • Cerebral ischemia (vasospasm, seizures) • Inflammatory mediators Firment • Causes of secondary brain injury : 16
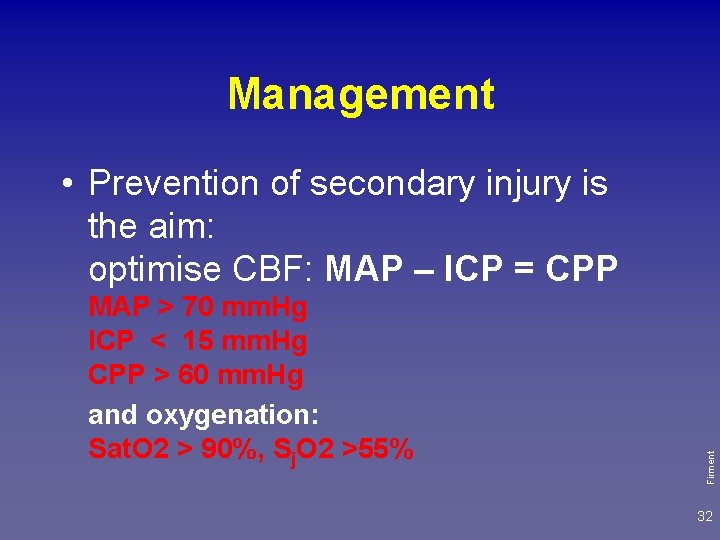
Prevention of secondary injury is the aim of the treatment. Firment Prevention therapy may improve outcome. 17
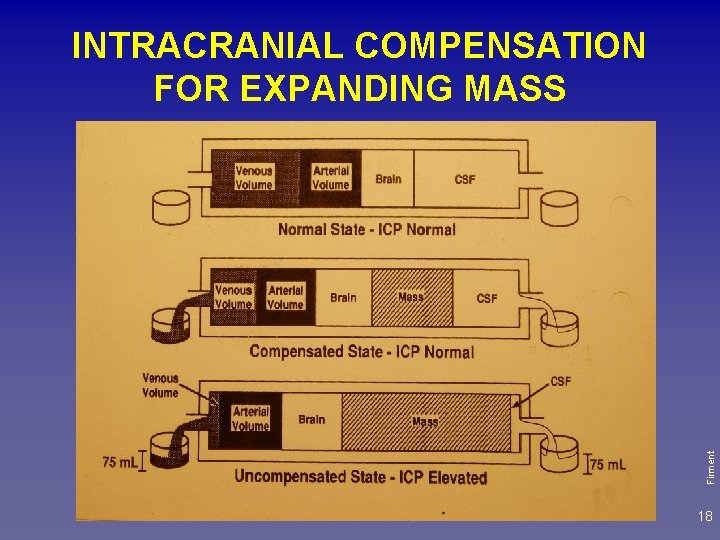
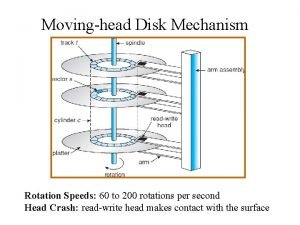
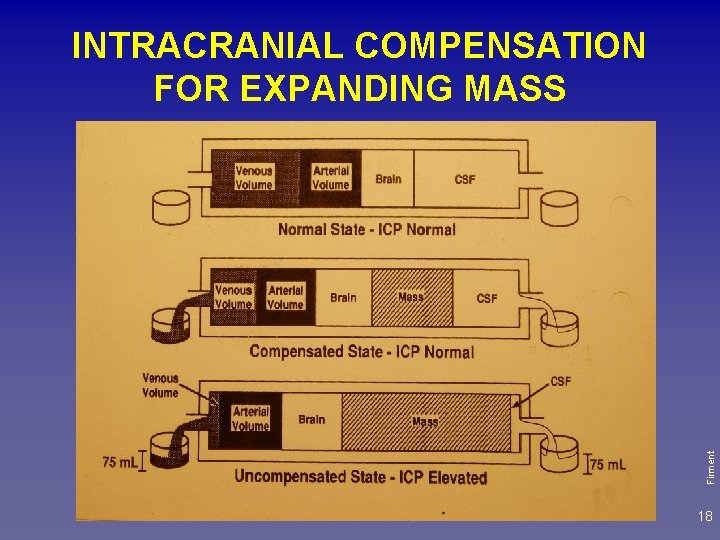
Firment INTRACRANIAL COMPENSATION FOR EXPANDING MASS 18
![PRESSURE mm Hg INTRACRANIAL PRESSURE ICP 40 Decompensation phase Compensation Phase Transition phase 0 PRESSURE [mm. Hg] INTRACRANIAL PRESSURE (ICP) 40 De-compensation phase Compensation Phase Transition phase 0](https://slidetodoc.com/presentation_image_h/1ecbea85a3f3a604e88d8ad28e251aa3/image-19.jpg)
PRESSURE [mm. Hg] INTRACRANIAL PRESSURE (ICP) 40 De-compensation phase Compensation Phase Transition phase 0 VOLUME Up to 15 mm. Hg, above 40 malignant oedema Firment 20 19
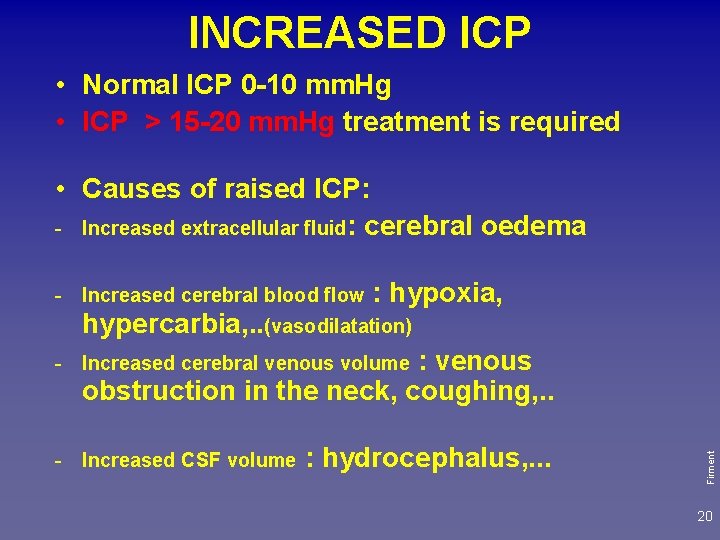
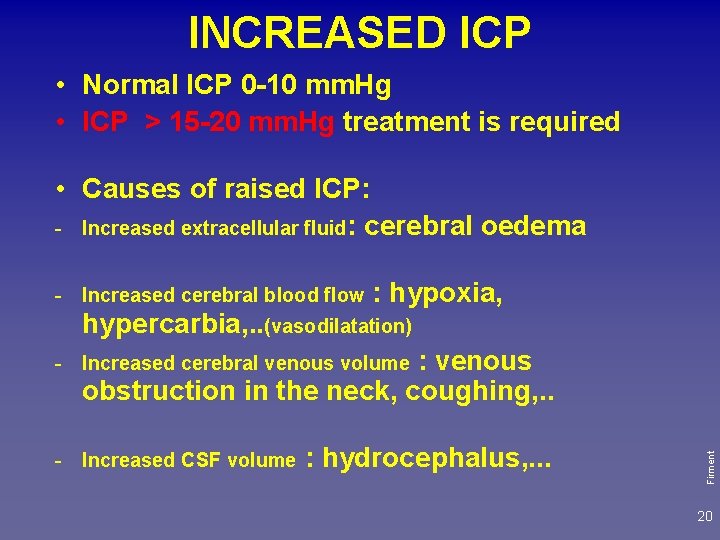
INCREASED ICP • Normal ICP 0 -10 mm. Hg • ICP > 15 -20 mm. Hg treatment is required • Causes of raised ICP: - Increased extracellular fluid: cerebral oedema - Increased cerebral blood flow : hypoxia, hypercarbia, . . (vasodilatation) : venous obstruction in the neck, coughing, . . - Increased CSF volume : hydrocephalus, . . . Firment - Increased cerebral venous volume 20
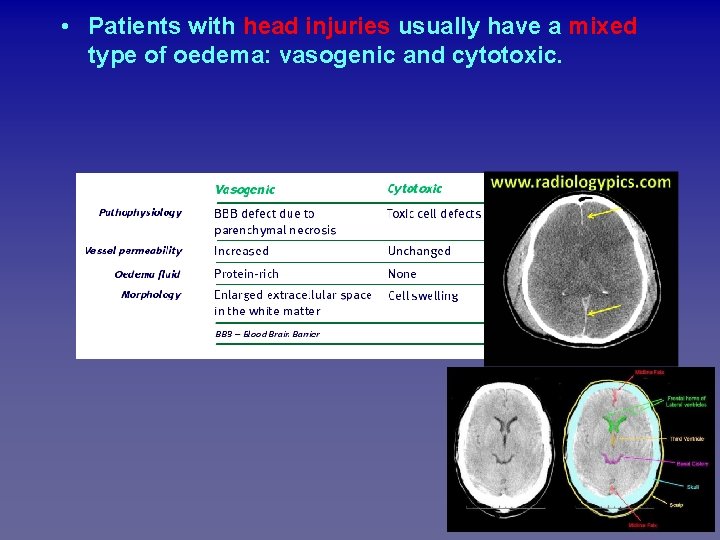
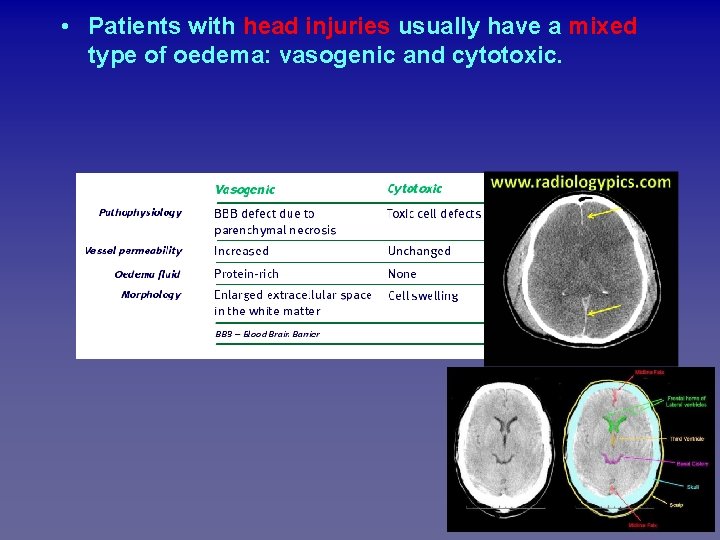
Firment • Patients with head injuries usually have a mixed type of oedema: vasogenic and cytotoxic. 21
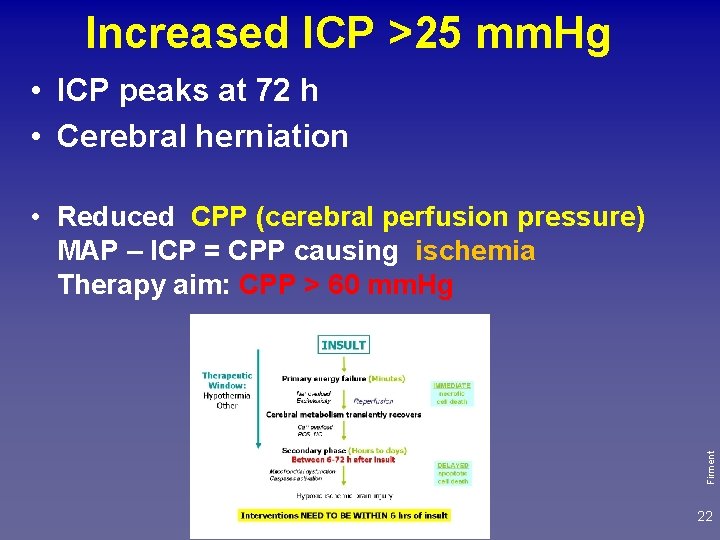
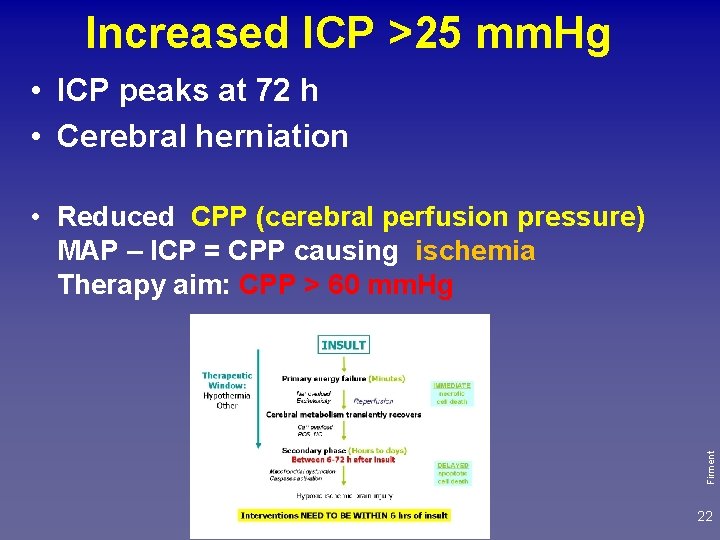
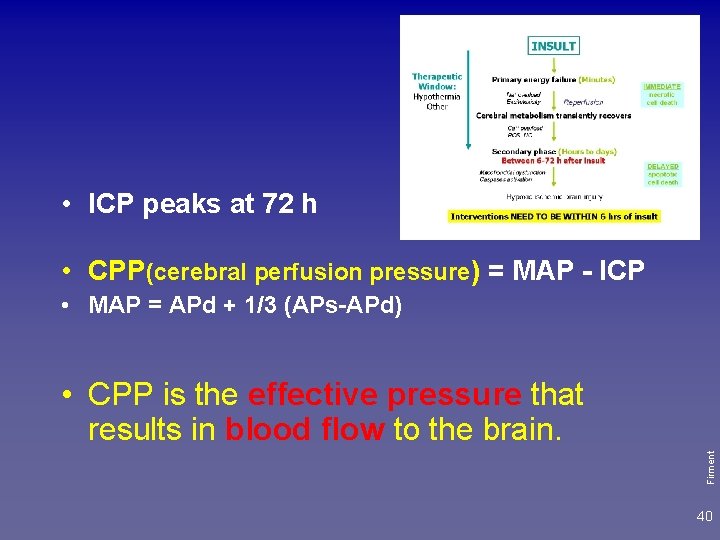
Increased ICP >25 mm. Hg • ICP peaks at 72 h • Cerebral herniation Firment • Reduced CPP (cerebral perfusion pressure) MAP – ICP = CPP causing ischemia Therapy aim: CPP > 60 mm. Hg 22
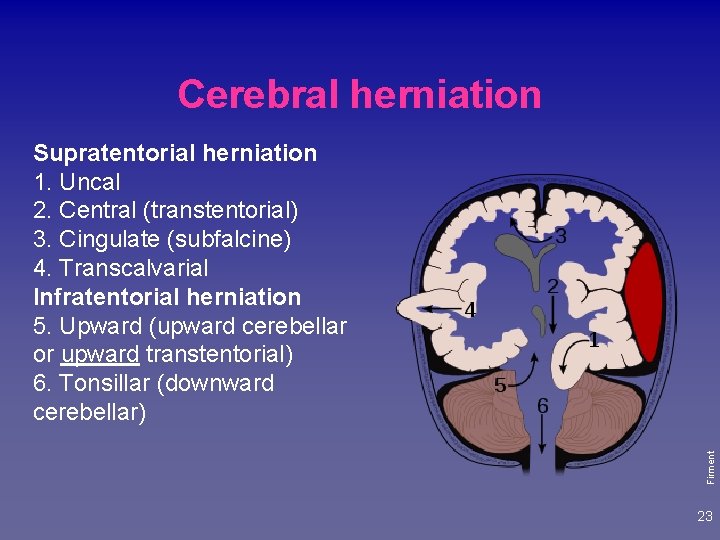
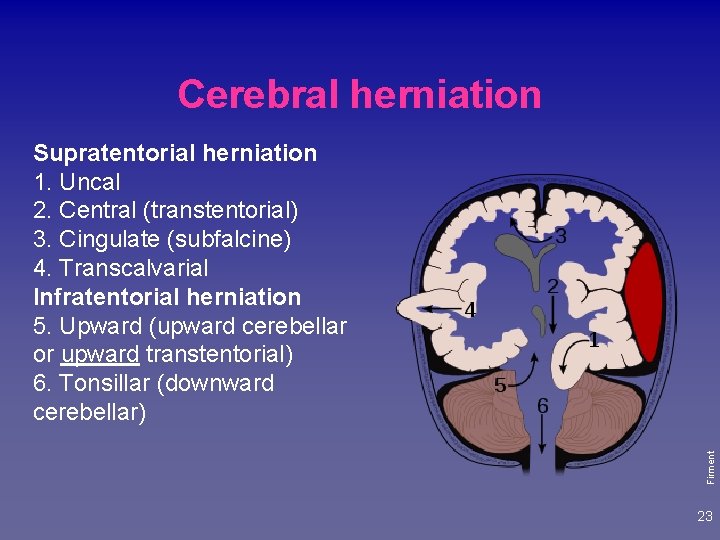
Cerebral herniation Firment Supratentorial herniation 1. Uncal 2. Central (transtentorial) 3. Cingulate (subfalcine) 4. Transcalvarial Infratentorial herniation 5. Upward (upward cerebellar or upward transtentorial) 6. Tonsillar (downward cerebellar) 23
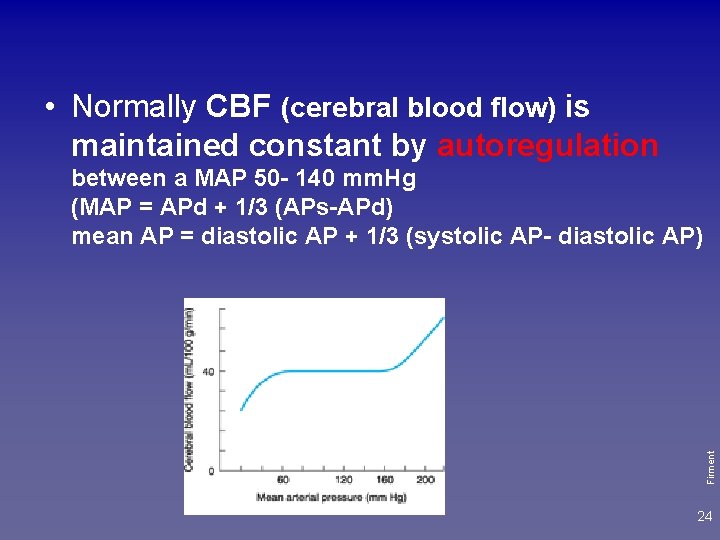
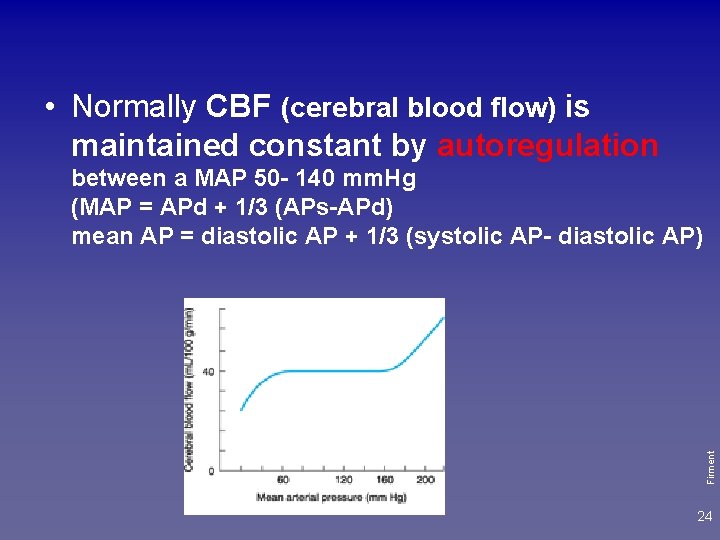
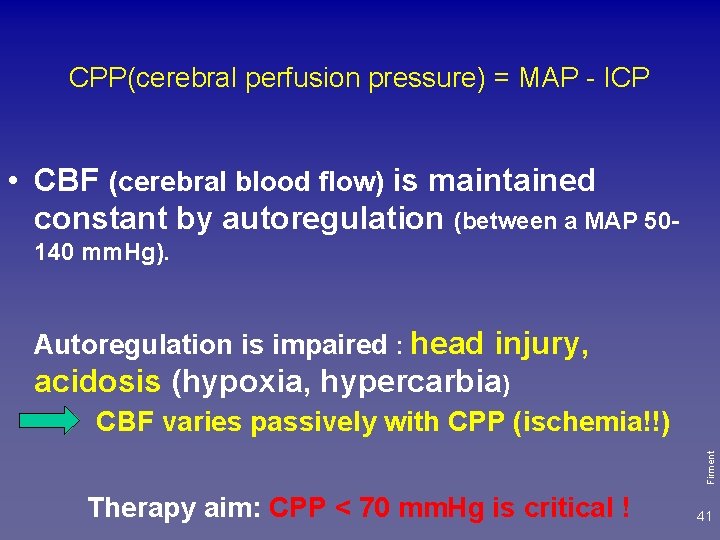
• Normally CBF (cerebral blood flow) is maintained constant by autoregulation Firment between a MAP 50 - 140 mm. Hg (MAP = APd + 1/3 (APs-APd) mean AP = diastolic AP + 1/3 (systolic AP- diastolic AP) 24
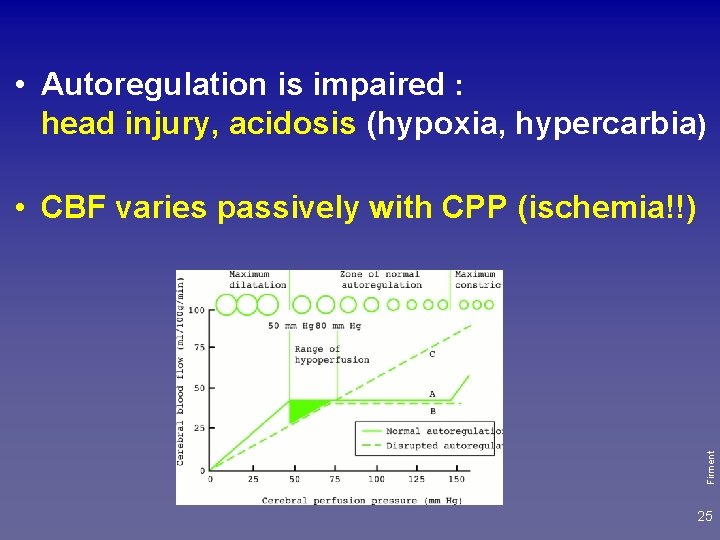
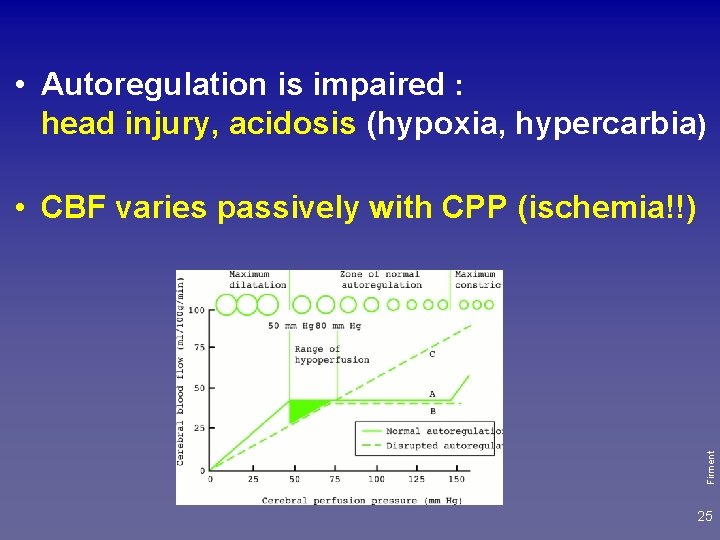
• Autoregulation is impaired : head injury, acidosis (hypoxia, hypercarbia) Firment • CBF varies passively with CPP (ischemia!!) 25
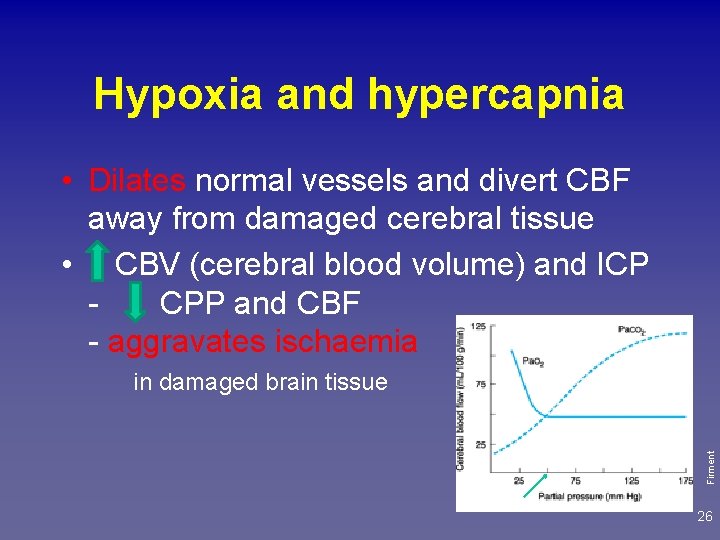
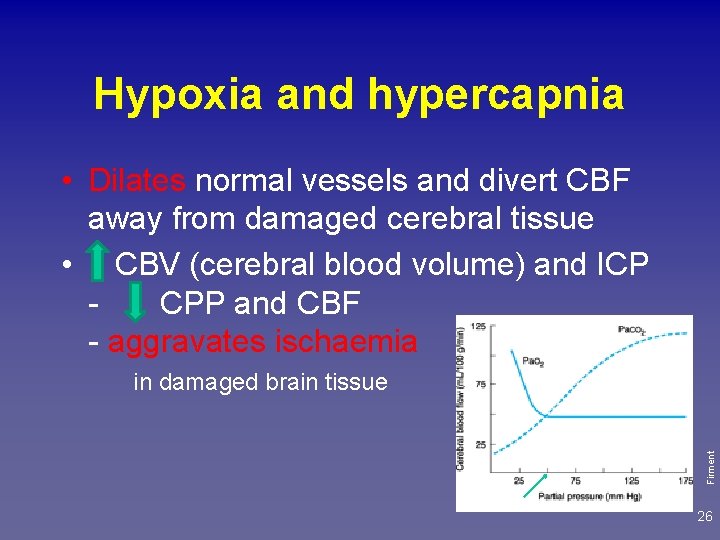
Hypoxia and hypercapnia • Dilates normal vessels and divert CBF away from damaged cerebral tissue • CBV (cerebral blood volume) and ICP CPP and CBF - aggravates ischaemia Firment in damaged brain tissue 26
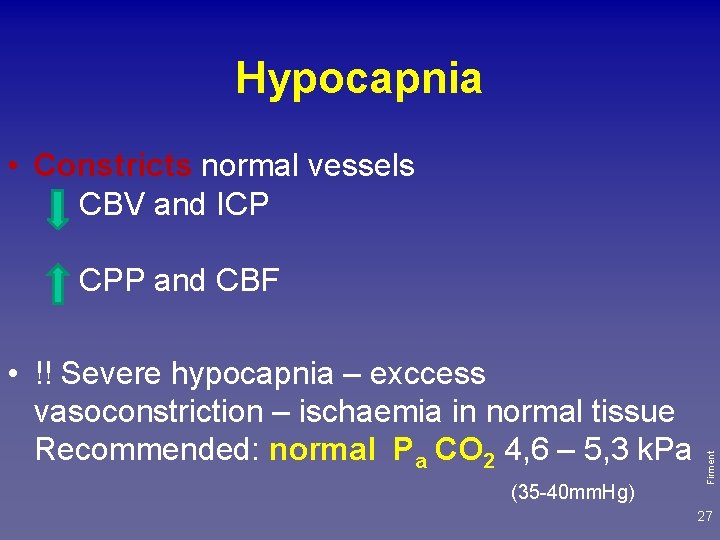
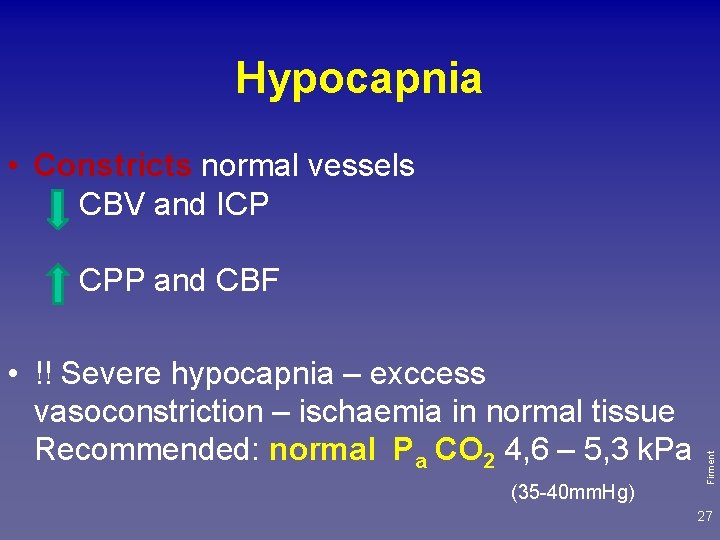
Hypocapnia • Constricts normal vessels CBV and ICP • !! Severe hypocapnia – exccess vasoconstriction – ischaemia in normal tissue Recommended: normal Pa CO 2 4, 6 – 5, 3 k. Pa (35 -40 mm. Hg) Firment CPP and CBF 27
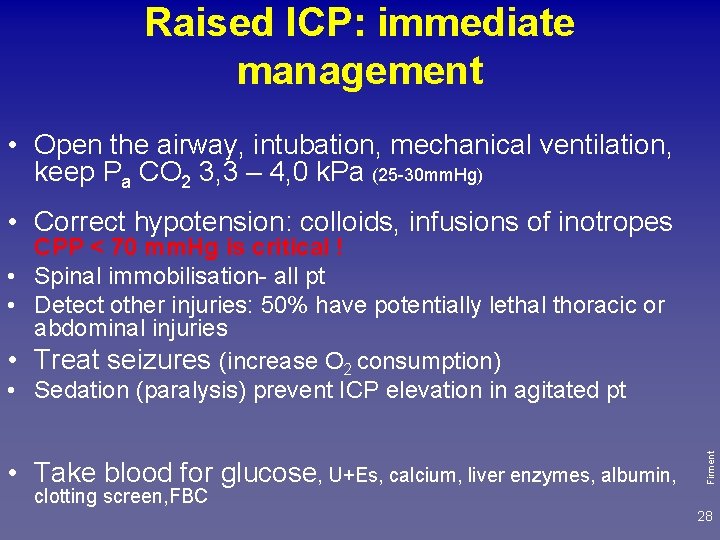
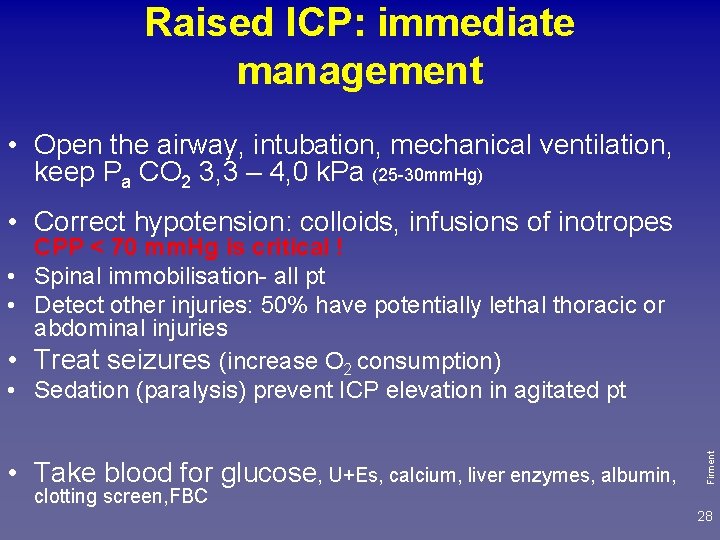
Raised ICP: immediate management • Open the airway, intubation, mechanical ventilation, keep Pa CO 2 3, 3 – 4, 0 k. Pa (25 -30 mm. Hg) • Correct hypotension: colloids, infusions of inotropes • • • Take blood for glucose, U+Es, calcium, liver enzymes, albumin, clotting screen, FBC Firment • • CPP < 70 mm. Hg is critical ! Spinal immobilisation- all pt Detect other injuries: 50% have potentially lethal thoracic or abdominal injuries Treat seizures (increase O 2 consumption) Sedation (paralysis) prevent ICP elevation in agitated pt 28
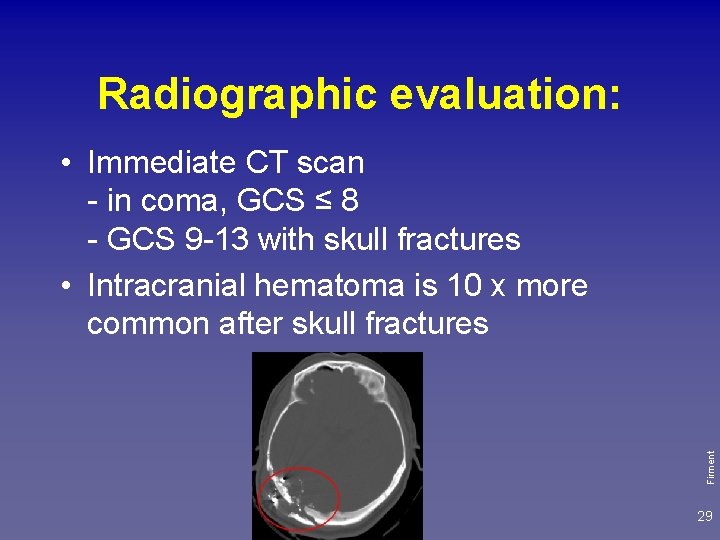
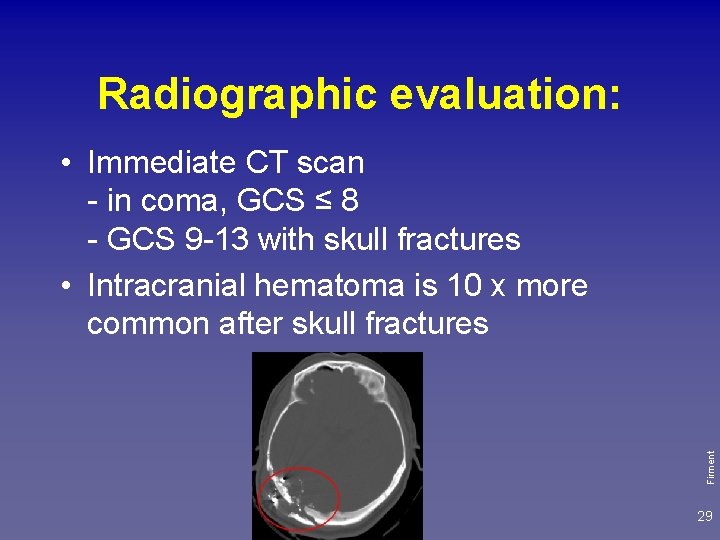
Radiographic evaluation: Firment • Immediate CT scan - in coma, GCS ≤ 8 - GCS 9 -13 with skull fractures • Intracranial hematoma is 10 x more common after skull fractures 29
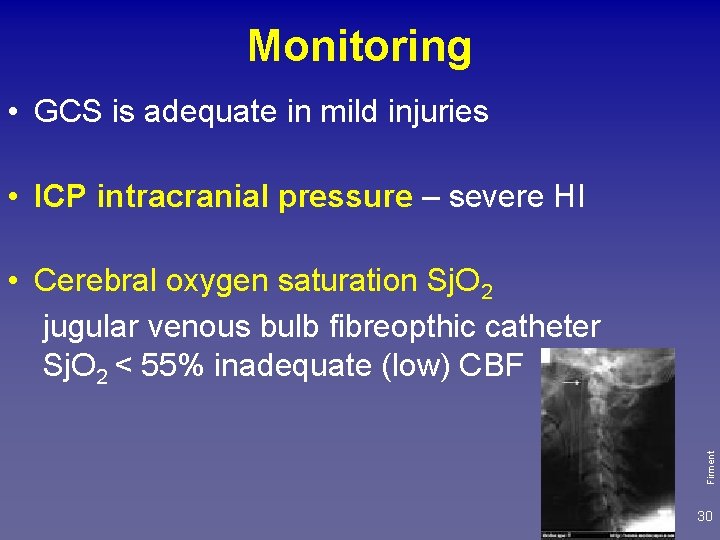
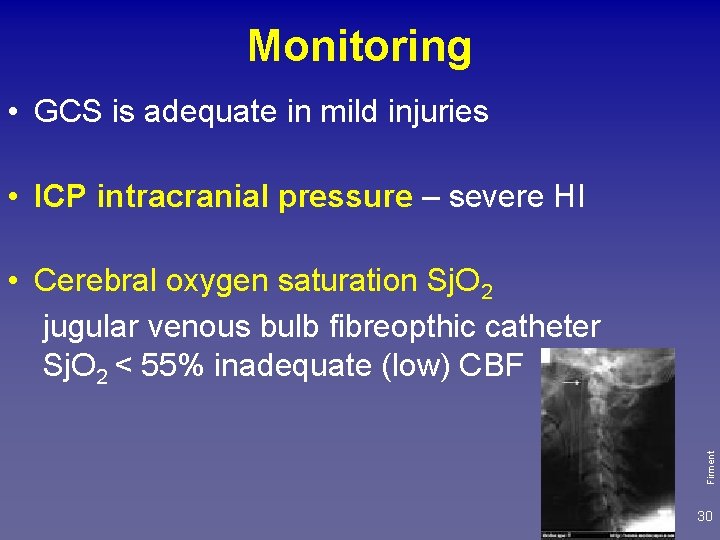
Monitoring • GCS is adequate in mild injuries • ICP intracranial pressure – severe HI Firment • Cerebral oxygen saturation Sj. O 2 jugular venous bulb fibreopthic catheter Sj. O 2 < 55% inadequate (low) CBF 30
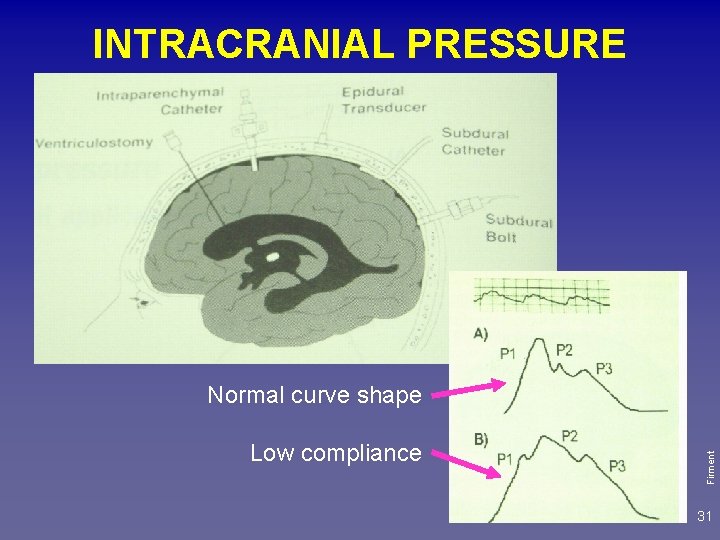
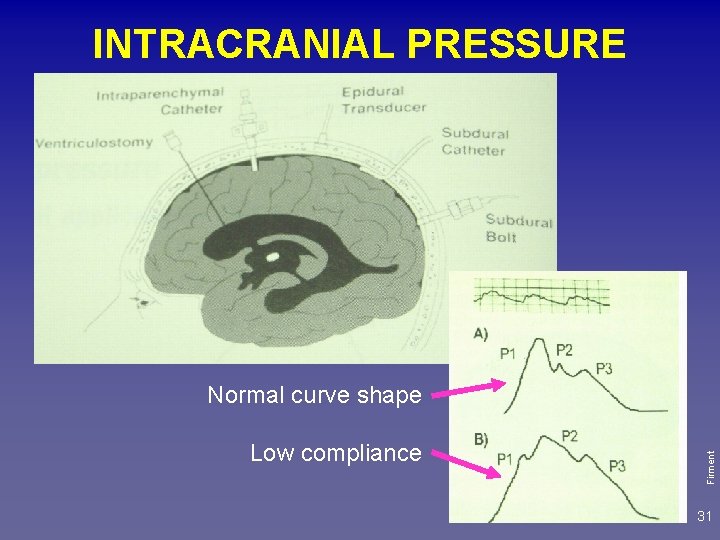
INTRACRANIAL PRESSURE Low compliance Firment Normal curve shape 31
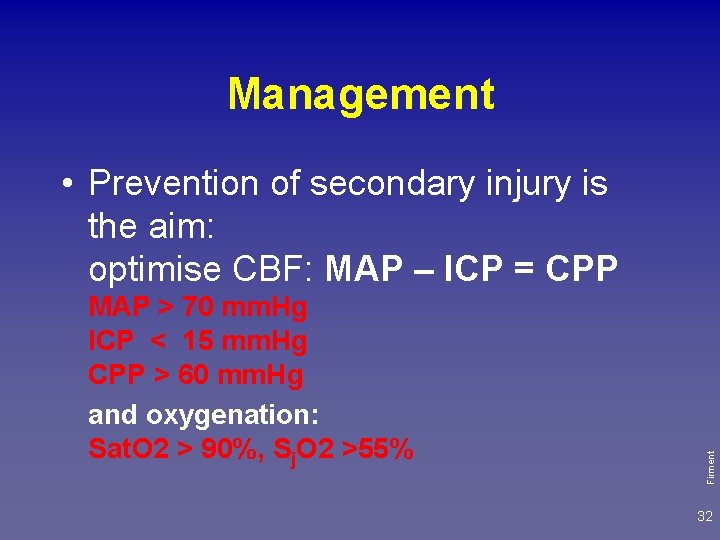
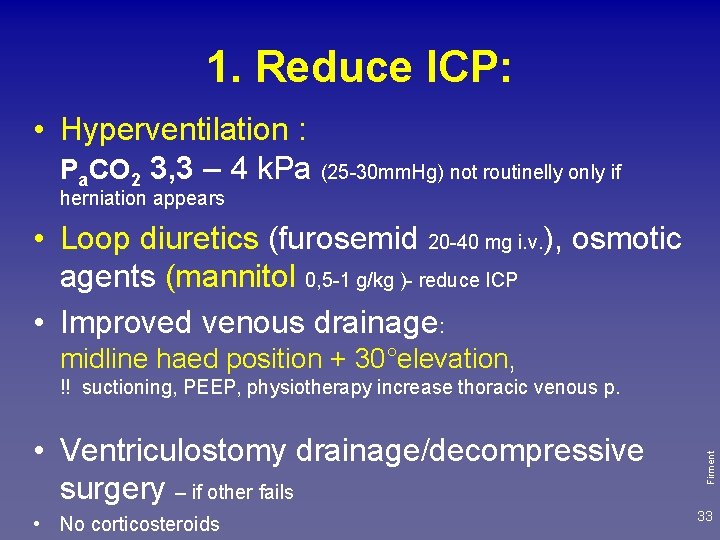
Management MAP > 70 mm. Hg ICP < 15 mm. Hg CPP > 60 mm. Hg and oxygenation: Sat. O 2 > 90%, Sj. O 2 >55% Firment • Prevention of secondary injury is the aim: optimise CBF: MAP – ICP = CPP 32
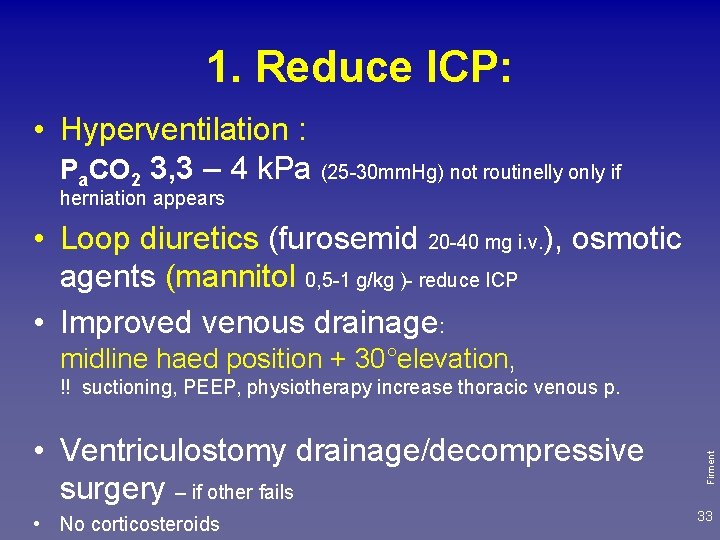
1. Reduce ICP: • Hyperventilation : Pa. CO 2 3, 3 – 4 k. Pa (25 -30 mm. Hg) not routinelly only if herniation appears • Loop diuretics (furosemid 20 -40 mg i. v. ), osmotic agents (mannitol 0, 5 -1 g/kg )- reduce ICP • Improved venous drainage: midline haed position + 30°elevation, • Ventriculostomy drainage/decompressive surgery – if other fails • No corticosteroids Firment !! suctioning, PEEP, physiotherapy increase thoracic venous p. 33
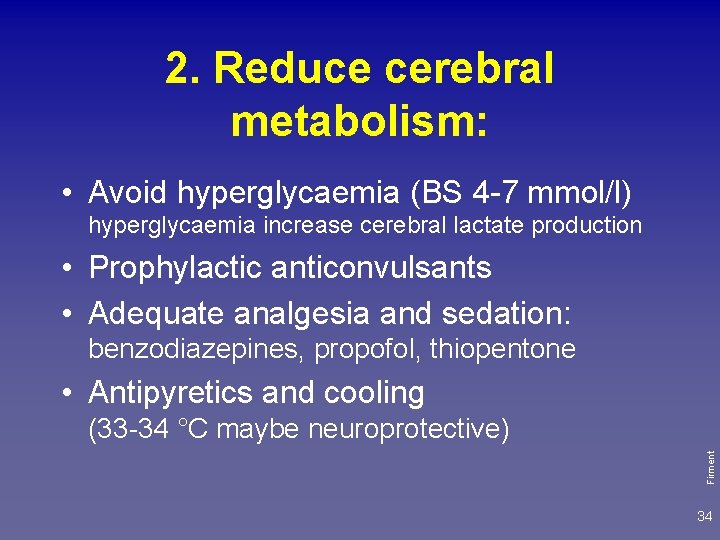
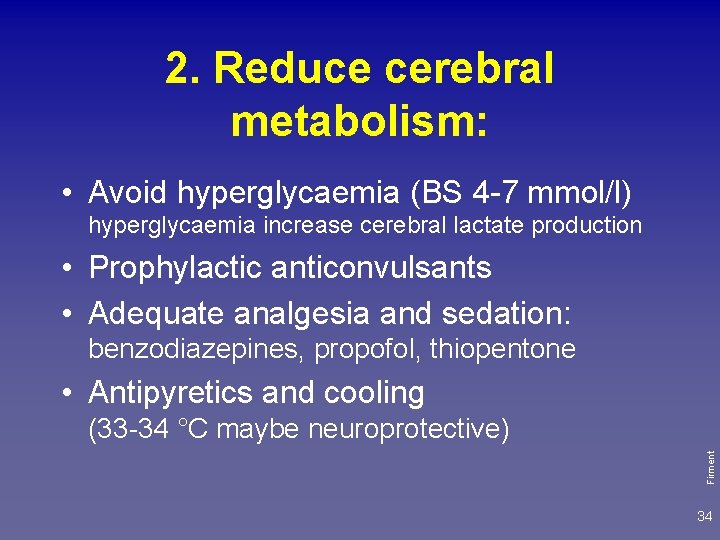
2. Reduce cerebral metabolism: • Avoid hyperglycaemia (BS 4 -7 mmol/l) hyperglycaemia increase cerebral lactate production • Prophylactic anticonvulsants • Adequate analgesia and sedation: benzodiazepines, propofol, thiopentone • Antipyretics and cooling Firment (33 -34 °C maybe neuroprotective) 34

Treat complications: • Avoid nasogastic tubes in basilar skull fracture Firment • Hypotalamic injury : inappropriate ADH secretion – diabetes insipidus • Meningitis – ATB 35

Firment TBI, maxillofaciálne poranenie, haemothorax Tracheostómia – UVP, PEG, drenáž hrudníka 36
jcapkova@capko. sk Firment Thank you! 37
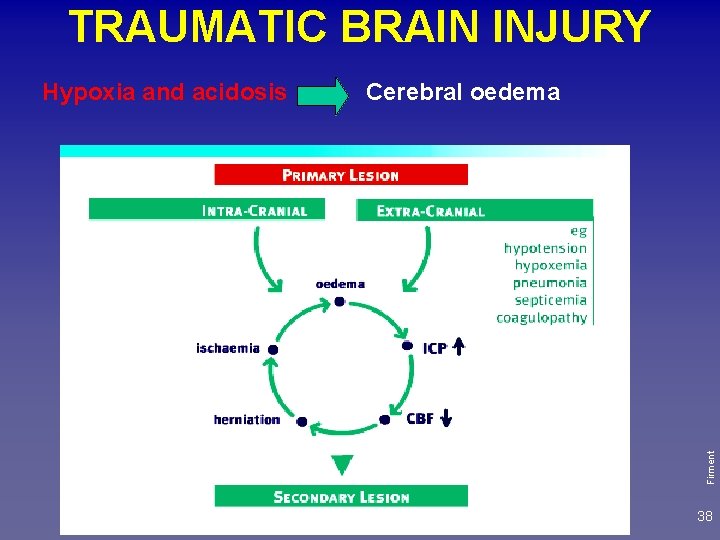
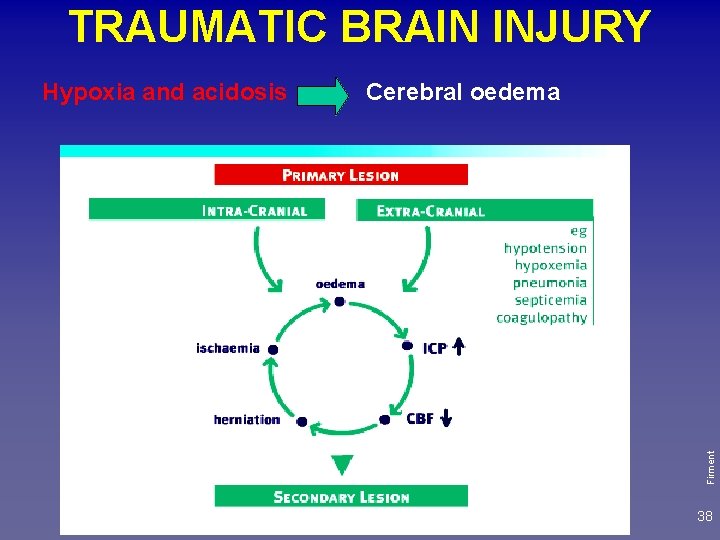
TRAUMATIC BRAIN INJURY Cerebral oedema Firment Hypoxia and acidosis 38
1. Stabilize the patient: ABC give oxygen, support circulation, treat seizures, stabilise the cervical spine as required 2. Consider giving thiamine, glucose (40 ml 40% glucose), naloxon, flumazenil 3. Examine patient 4. Plan for further investigations Firment Immediate management 39
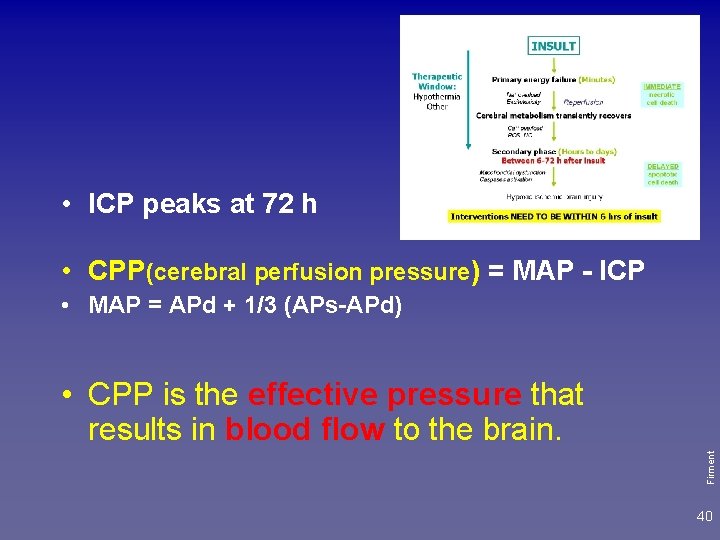
• ICP peaks at 72 h • CPP(cerebral perfusion pressure) = MAP - ICP • MAP = APd + 1/3 (APs-APd) Firment • CPP is the effective pressure that results in blood flow to the brain. 40
CPP(cerebral perfusion pressure) = MAP - ICP • CBF (cerebral blood flow) is maintained constant by autoregulation (between a MAP 50140 mm. Hg). Autoregulation is impaired : head injury, acidosis (hypoxia, hypercarbia) Firment CBF varies passively with CPP (ischemia!!) Therapy aim: CPP < 70 mm. Hg is critical ! 41
5. Progress in monitoring • Regular and frequent observations of vital signs and neurological state • Emergency treatment of raised ICP (intracranial pressure) headache, vomiting, seizures, focal neurology, papilloedema - late: incr. BP, bradycardia, coma, Cheyne Stokes breathing, apnoe. Firment Signs ICH (intracranial hypertension): - early: 42
 Raya funcion
Raya funcion Intentional and unintentional injury
Intentional and unintentional injury Head injury assessment
Head injury assessment Battle's sign
Battle's sign Cholesteatoma
Cholesteatoma Nrl head injury recognition and referral form
Nrl head injury recognition and referral form Copyright
Copyright Patrick lynch head injury colorado
Patrick lynch head injury colorado Pass and decal north island
Pass and decal north island Gustav klimt judita
Gustav klimt judita Kavinukas su pastoralem
Kavinukas su pastoralem Judita miro gavran karakterizacija likova
Judita miro gavran karakterizacija likova Miro gavran zaljubljen do ušiju lektira
Miro gavran zaljubljen do ušiju lektira Miro gavran najpoznatija djela
Miro gavran najpoznatija djela Invokacija judita
Invokacija judita Kneevi
Kneevi Saulegraza vaiciunaite
Saulegraza vaiciunaite What is tonic syllable
What is tonic syllable The head of moving head disk with 100 tracks
The head of moving head disk with 100 tracks Html teksta noformēšana
Html teksta noformēšana Negative suction head
Negative suction head Moving head disk mechanism in os
Moving head disk mechanism in os Biceps femoris innervation
Biceps femoris innervation Dividing head calculation formula
Dividing head calculation formula Parts of the leg
Parts of the leg What is tone unit
What is tone unit The attacking firm goes head-to-head with its competitor.
The attacking firm goes head-to-head with its competitor. Astrowise
Astrowise Glasgow coma scale
Glasgow coma scale Hyperthyroidism hypokalemia
Hyperthyroidism hypokalemia Coma hiperosmolar fisiopatologia
Coma hiperosmolar fisiopatologia Glasgow coma scale chart
Glasgow coma scale chart Coma diabetica
Coma diabetica Coma hyperosmolaire
Coma hyperosmolaire La coma en los conectores
La coma en los conectores Aeiou tips coma
Aeiou tips coma Multiplicacion de decimales
Multiplicacion de decimales Inokuchi shunt
Inokuchi shunt Coma cluster
Coma cluster Coma psicogeno
Coma psicogeno Contusio capitis reg frontalis
Contusio capitis reg frontalis Neurological observations glasgow coma scale
Neurological observations glasgow coma scale Lateralizing signs
Lateralizing signs