Population Health Readiness SelfAssessment Financial Indicators NC Critical


- Slides: 48
Population Health Readiness Self-Assessment Financial Indicators NC Critical Access Hospital Network Regional Meeting May 22, 2019 1
Goals for Today § To stimulate your thinking regarding transformational shift from the current “sick care” to future “health care” delivery model § To share your self-assessment readiness level for navigating towards population health delivery model § To encourage proactive planning and engagement related to population health positioning 2
Project Summary • Online survey • Available to all NC CAHs • One response per hospital • Administered in 2017 • 16 CAHs participated • Administered in 2019 • 11 CAHs participated 3
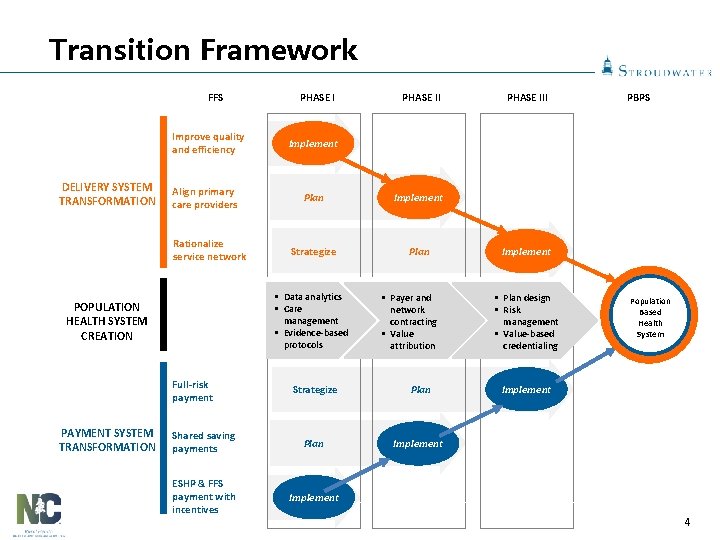
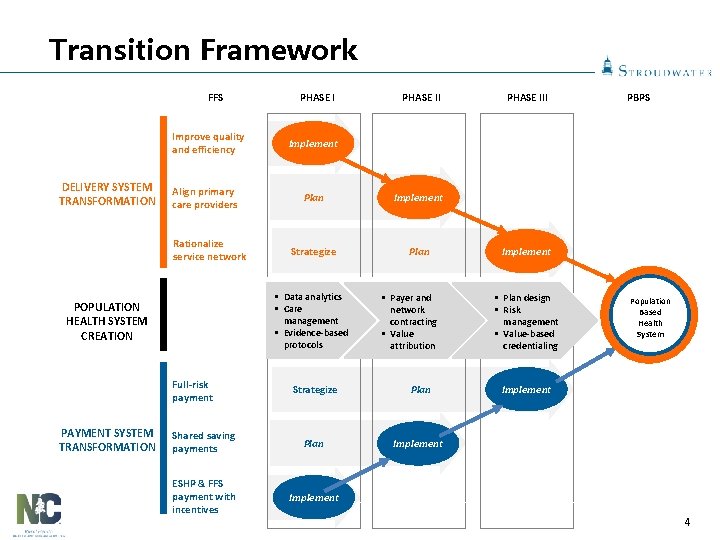
Transition Framework FFS Improve quality and efficiency DELIVERY SYSTEM TRANSFORMATION Align primary care providers Rationalize service network Full-risk payment PHASE III PBPS Implement Plan Implement Strategize Plan § Data analytics § Care management § Evidence-based protocols POPULATION HEALTH SYSTEM CREATION PAYMENT SYSTEM TRANSFORMATION PHASE I § Payer and network contracting § Value attribution Strategize Plan Shared saving payments Plan Implement ESHP & FFS payment with incentives Implement § Plan design § Risk management § Value-based credentialing Population Based Health System Implement 4
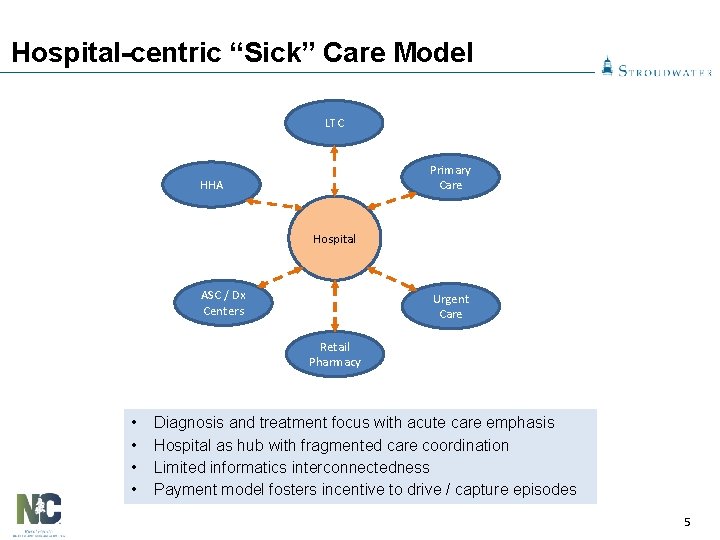
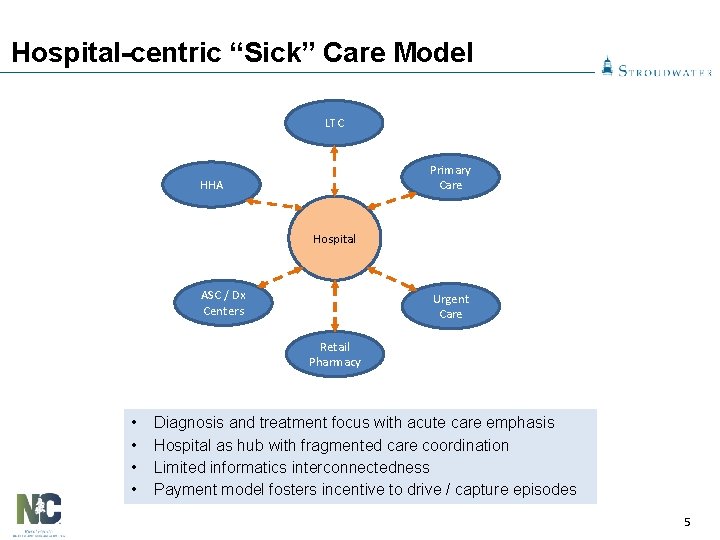
Hospital-centric “Sick” Care Model LTC Primary Care HHA Hospital ASC / Dx Centers Urgent Care Retail Pharmacy • • Diagnosis and treatment focus with acute care emphasis Hospital as hub with fragmented care coordination Limited informatics interconnectedness Payment model fosters incentive to drive / capture episodes 5
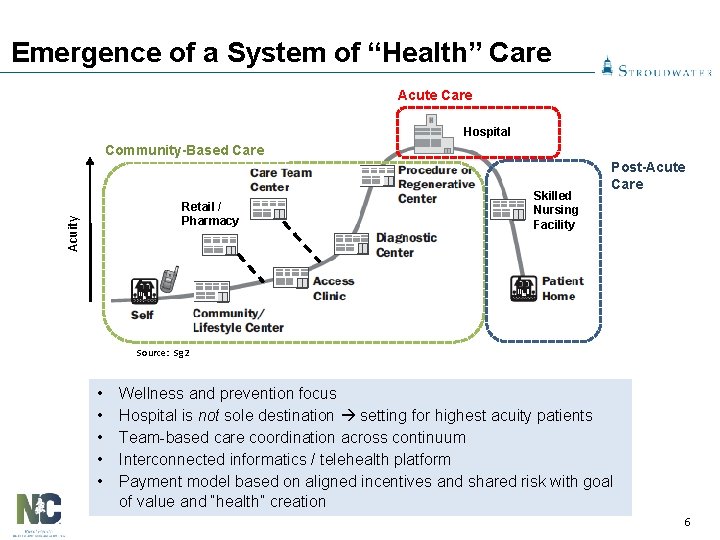
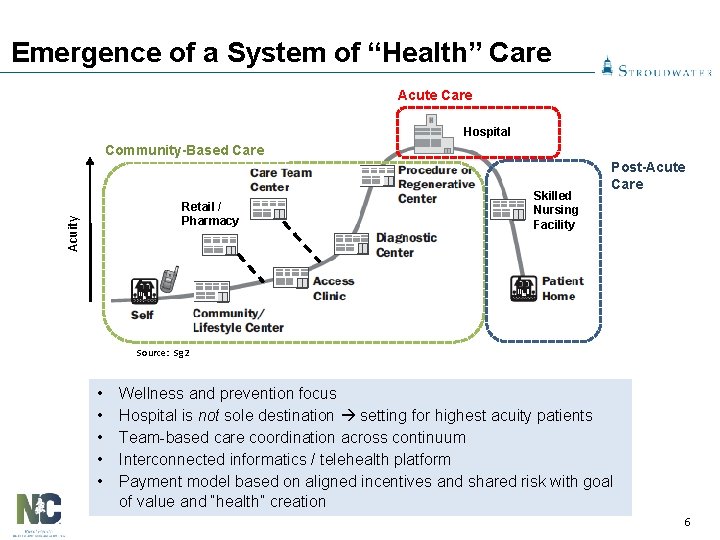
Emergence of a System of “Health” Care Acute Care Hospital Community-Based Care Acuity Retail / Pharmacy Skilled Nursing Facility Post-Acute Care Source: Sg 2 • • • Wellness and prevention focus Hospital is not sole destination setting for highest acuity patients Team-based care coordination across continuum Interconnected informatics / telehealth platform Payment model based on aligned incentives and shared risk with goal of value and “health” creation 6
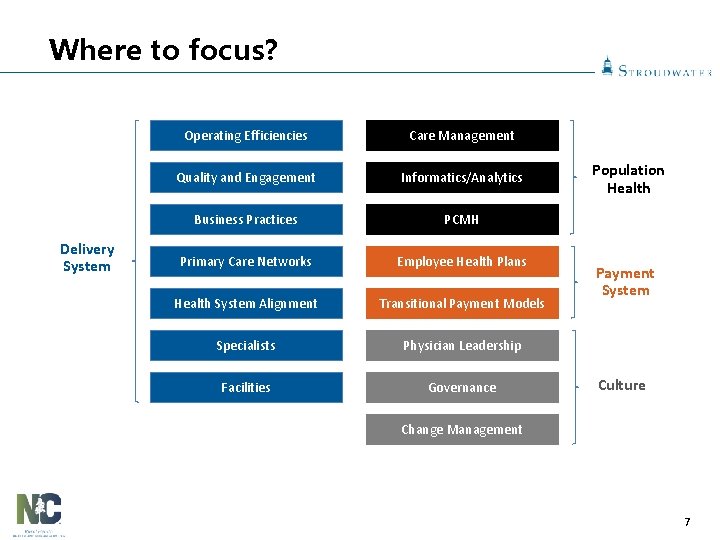
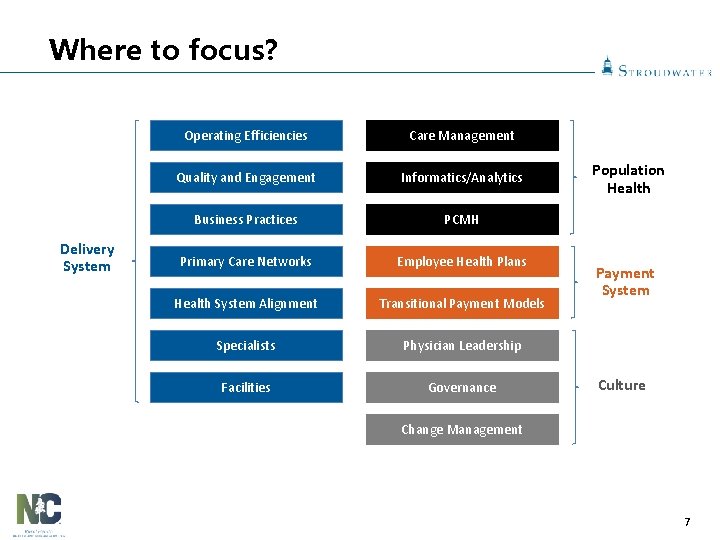
Where to focus? Delivery System Operating Efficiencies Care Management Quality and Engagement Informatics/Analytics Business Practices PCMH Primary Care Networks Employee Health Plans Health System Alignment Transitional Payment Models Specialists Physician Leadership Facilities Governance Population Health Payment System Culture Change Management 7
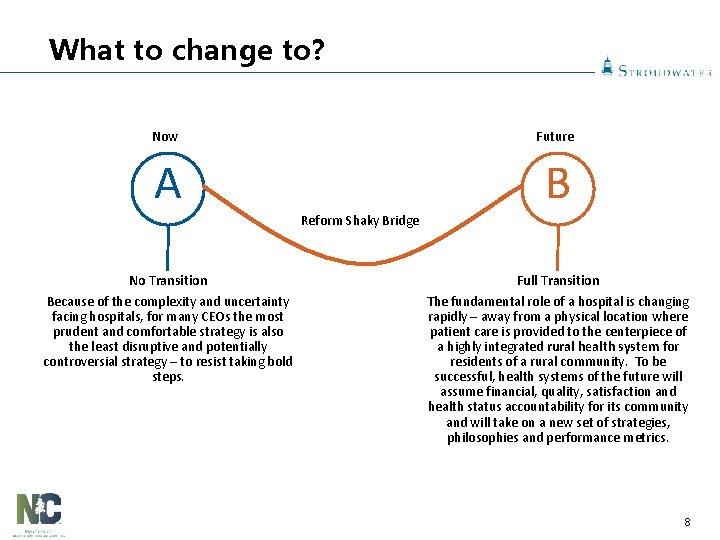
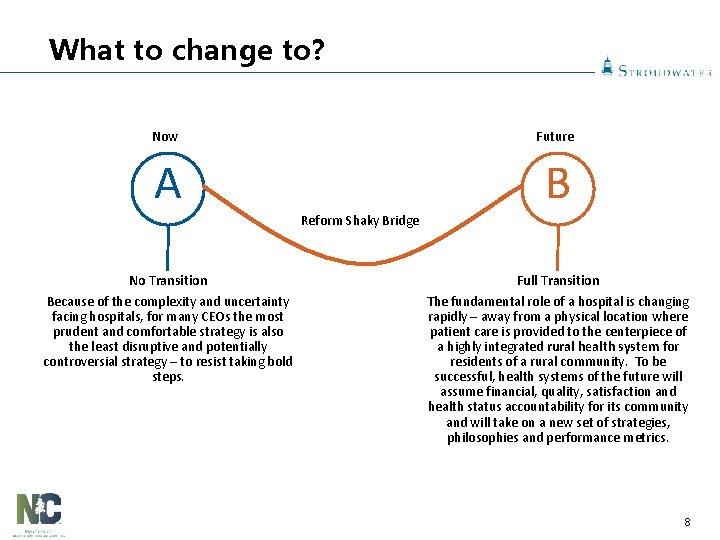
What to change to? Now Future A B Reform Shaky Bridge No Transition Because of the complexity and uncertainty facing hospitals, for many CEOs the most prudent and comfortable strategy is also the least disruptive and potentially controversial strategy – to resist taking bold steps. Full Transition The fundamental role of a hospital is changing rapidly – away from a physical location where patient care is provided to the centerpiece of a highly integrated rural health system for residents of a rural community. To be successful, health systems of the future will assume financial, quality, satisfaction and health status accountability for its community and will take on a new set of strategies, philosophies and performance metrics. 8
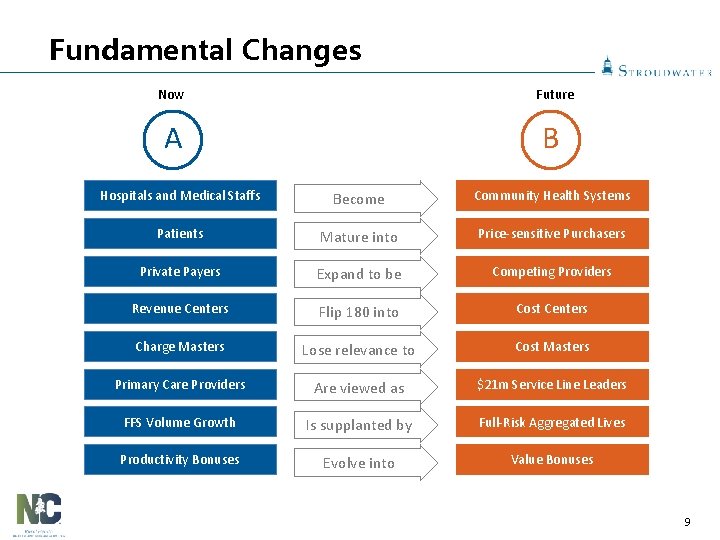
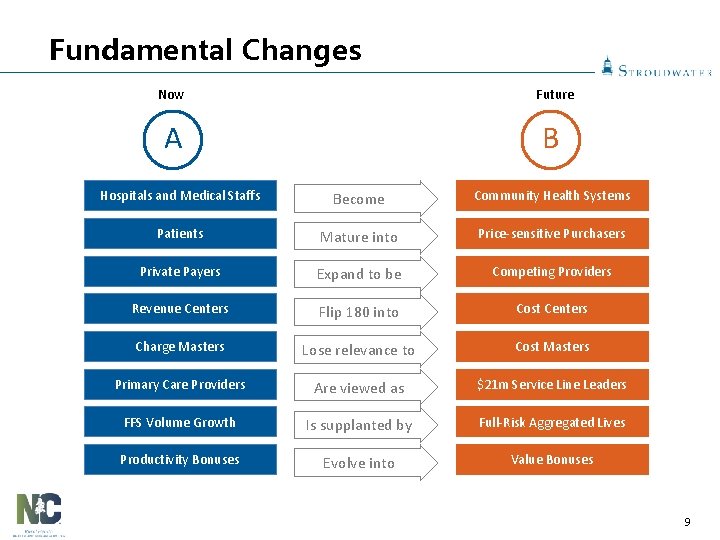
Fundamental Changes Now Future A B Hospitals and Medical Staffs Become Community Health Systems Patients Mature into Price-sensitive Purchasers Private Payers Expand to be Competing Providers Revenue Centers Flip 180 into Cost Centers Charge Masters Lose relevance to Cost Masters Primary Care Providers Are viewed as $21 m Service Line Leaders FFS Volume Growth Is supplanted by Full-Risk Aggregated Lives Productivity Bonuses Evolve into Value Bonuses 9
Group Questions 1. Are you discussing the transition to Population Based Payment with key stakeholder groups (e. g. Board, Medical Staff, Hospital Associates and Community) 10
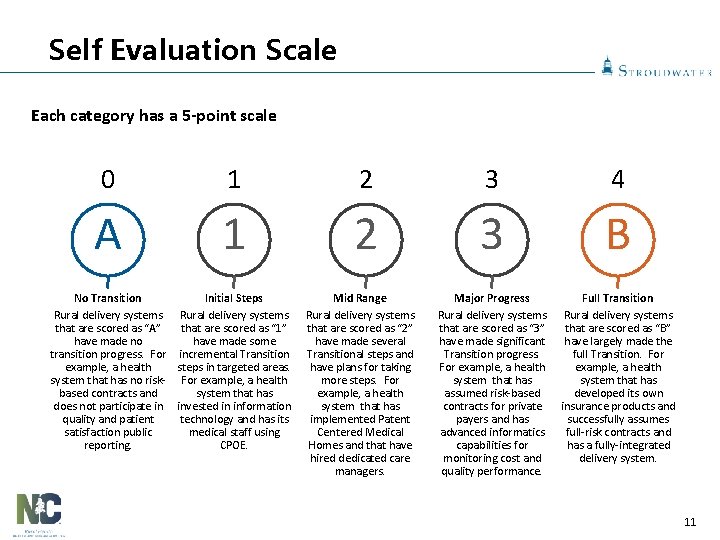
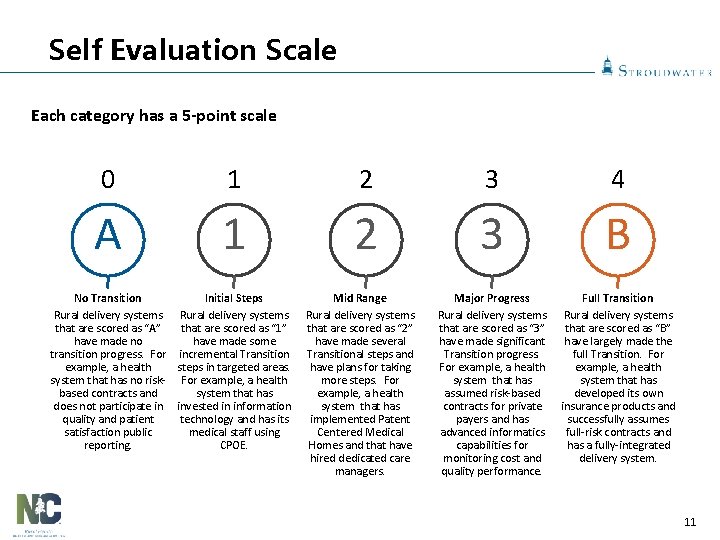
Self Evaluation Scale Each category has a 5 -point scale 0 1 2 3 4 A 1 2 3 B Major Progress Rural delivery systems that are scored as “ 3” have made significant Transition progress. For example, a health system that has assumed risk-based contracts for private payers and has advanced informatics capabilities for monitoring cost and quality performance. Full Transition Rural delivery systems that are scored as “B” have largely made the full Transition. For example, a health system that has developed its own insurance products and successfully assumes full-risk contracts and has a fully-integrated delivery system. No Transition Initial Steps Rural delivery systems that are scored as “A” that are scored as “ 1” have made no have made some transition progress. For incremental Transition example, a health steps in targeted areas. system that has no risk- For example, a health based contracts and system that has does not participate in invested in information quality and patient technology and has its satisfaction public medical staff using reporting. CPOE. Mid Range Rural delivery systems that are scored as “ 2” have made several Transitional steps and have plans for taking more steps. For example, a health system that has implemented Patent Centered Medical Homes and that have hired dedicated care managers. 11
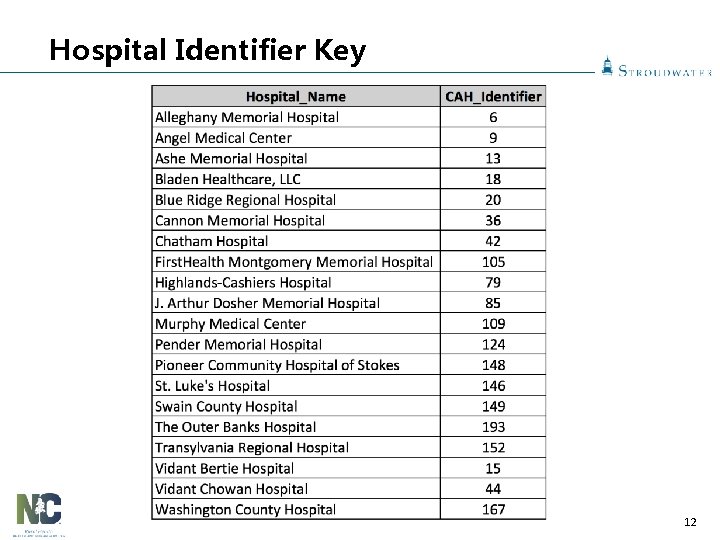
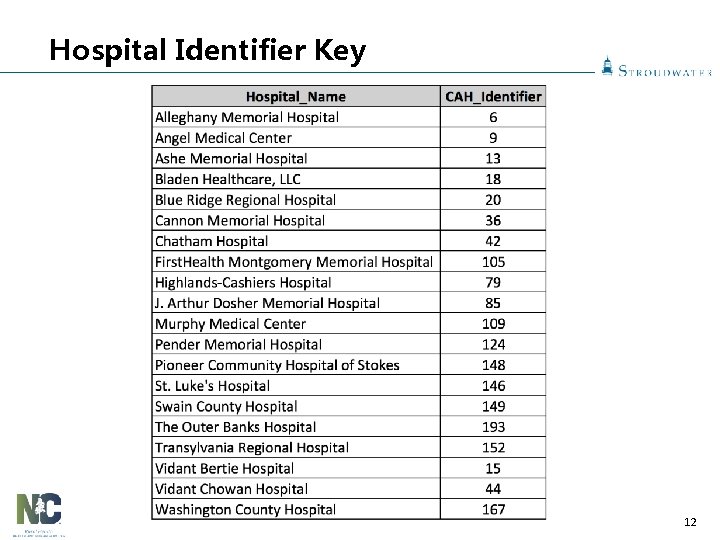
Hospital Identifier Key 12
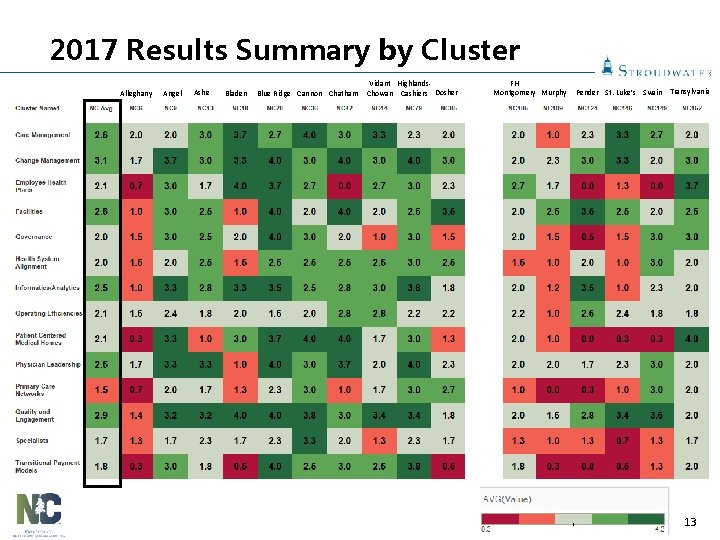
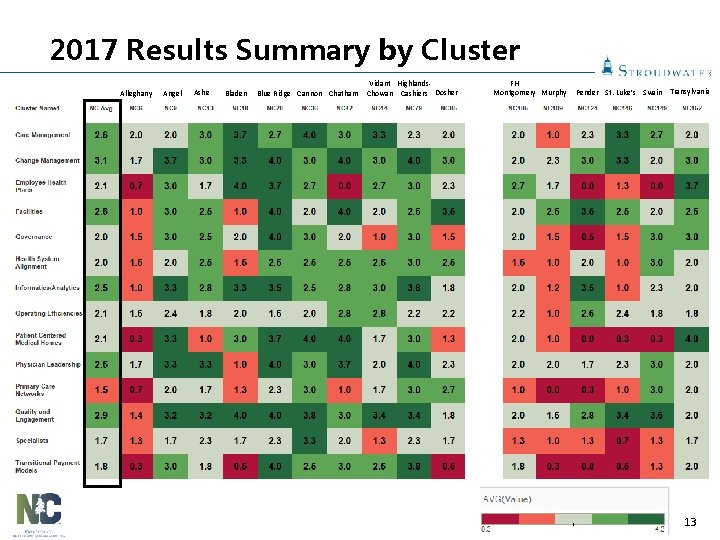
2017 Results Summary by Cluster Alleghany Angel Ashe Bladen Blue Ridge Cannon Chatham Vidant Highlands. Chowan Cashiers Dosher FH Montgomery Murphy Pender St. Luke’s Swain Transylvania 13
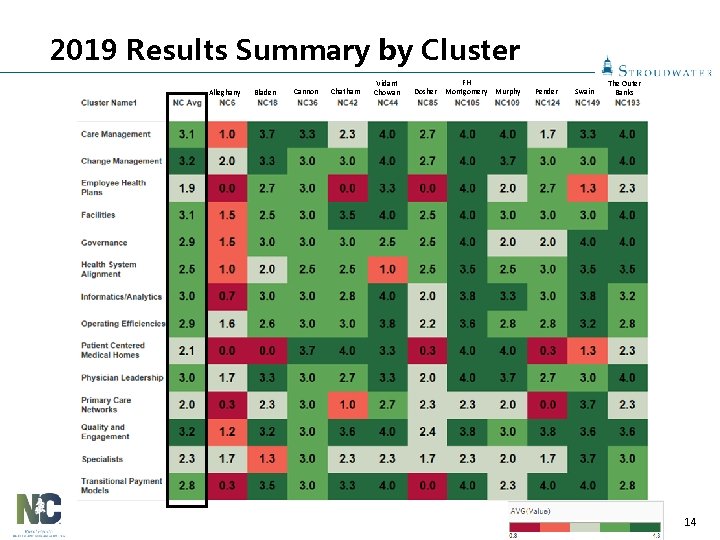
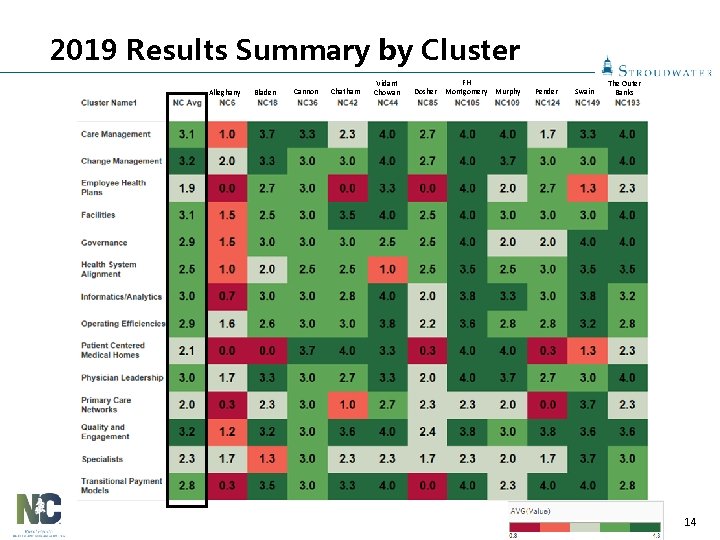
2019 Results Summary by Cluster Alleghany Bladen Cannon Chatham Vidant Chowan Dosher FH Montgomery Murphy Pender Swain The Outer Banks 14
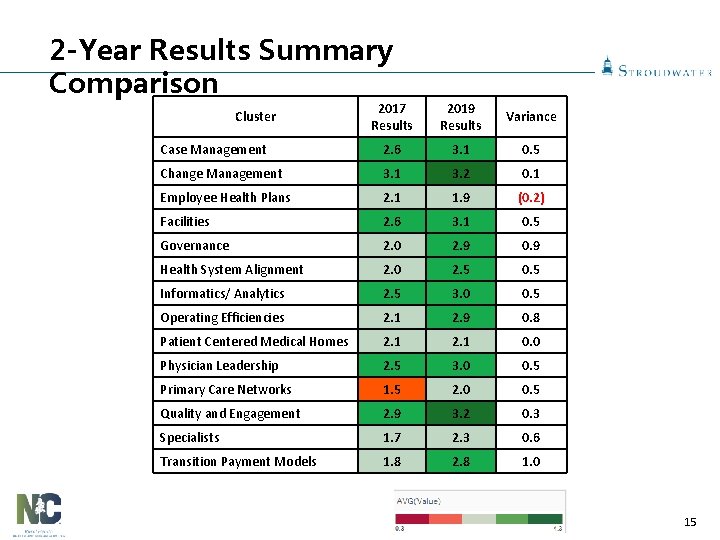
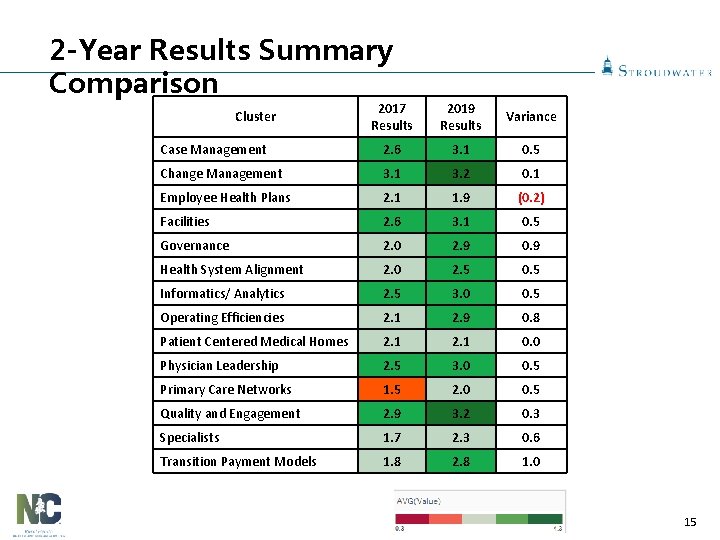
2 -Year Results Summary Comparison 2017 Results 2019 Results Variance Case Management 2. 6 3. 1 0. 5 Change Management 3. 1 3. 2 0. 1 Employee Health Plans 2. 1 1. 9 (0. 2) Facilities 2. 6 3. 1 0. 5 Governance 2. 0 2. 9 0. 9 Health System Alignment 2. 0 2. 5 0. 5 Informatics/ Analytics 2. 5 3. 0 0. 5 Operating Efficiencies 2. 1 2. 9 0. 8 Patient Centered Medical Homes 2. 1 0. 0 Physician Leadership 2. 5 3. 0 0. 5 Primary Care Networks 1. 5 2. 0 0. 5 Quality and Engagement 2. 9 3. 2 0. 3 Specialists 1. 7 2. 3 0. 6 Transition Payment Models 1. 8 2. 8 1. 0 Cluster 15
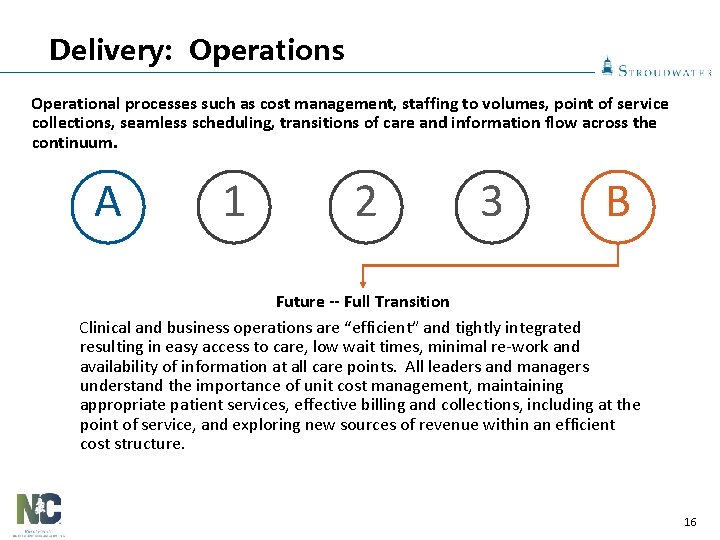
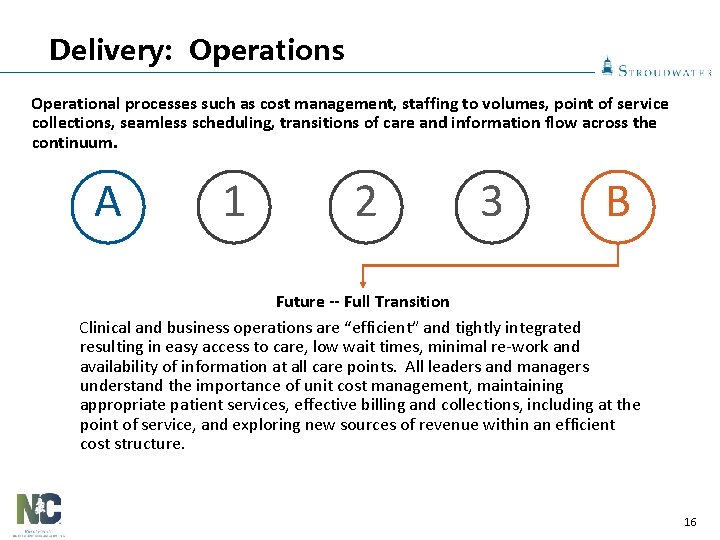
Delivery: Operations Operational processes such as cost management, staffing to volumes, point of service collections, seamless scheduling, transitions of care and information flow across the continuum. A 1 2 3 B Future -- Full Transition Clinical and business operations are “efficient” and tightly integrated resulting in easy access to care, low wait times, minimal re-work and availability of information at all care points. All leaders and managers understand the importance of unit cost management, maintaining appropriate patient services, effective billing and collections, including at the point of service, and exploring new sources of revenue within an efficient cost structure. 16
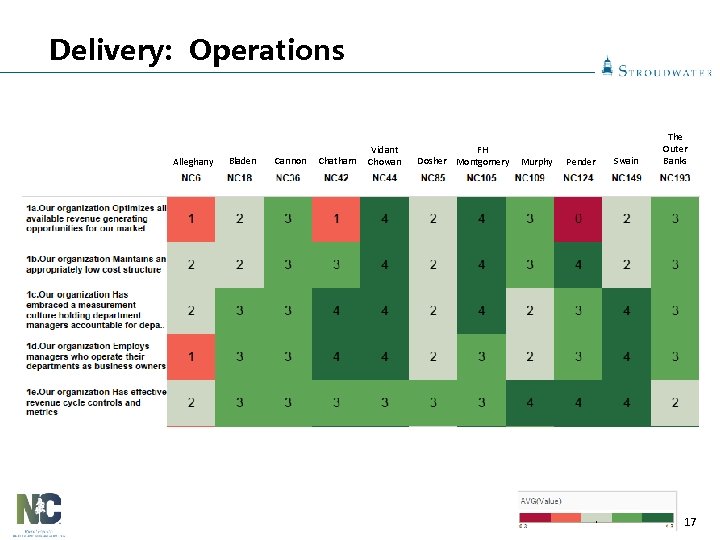
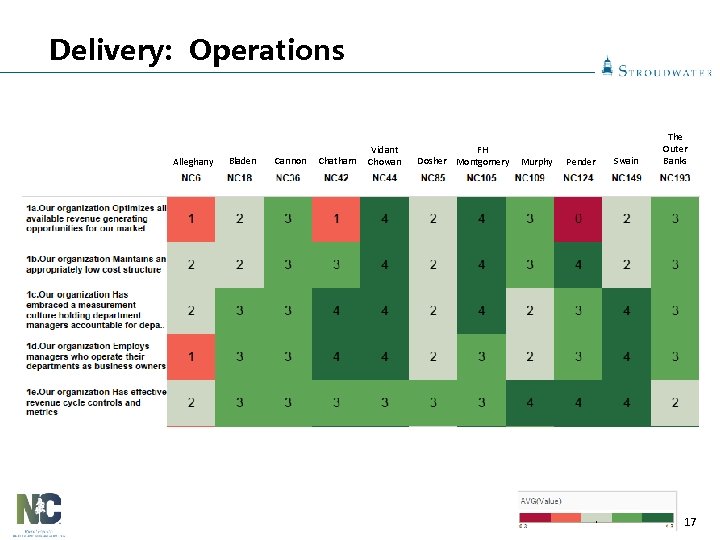
Delivery: Operations Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 17
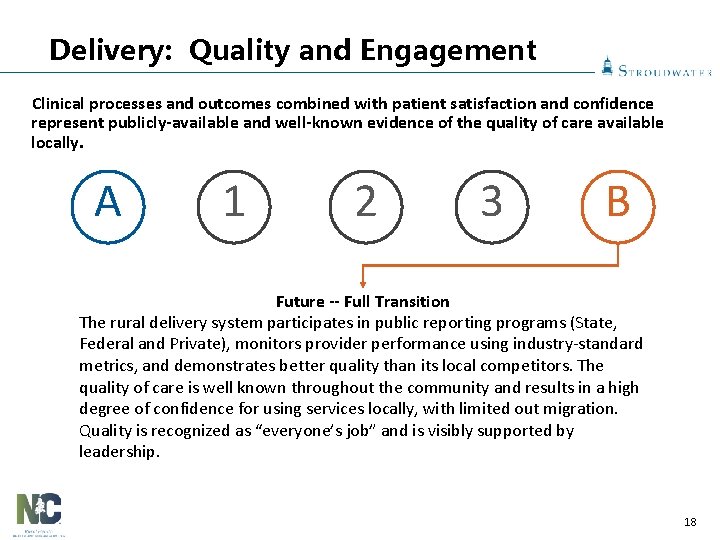
Delivery: Quality and Engagement Clinical processes and outcomes combined with patient satisfaction and confidence represent publicly-available and well-known evidence of the quality of care available locally. A 1 2 3 B Future -- Full Transition The rural delivery system participates in public reporting programs (State, Federal and Private), monitors provider performance using industry-standard metrics, and demonstrates better quality than its local competitors. The quality of care is well known throughout the community and results in a high degree of confidence for using services locally, with limited out migration. Quality is recognized as “everyone’s job” and is visibly supported by leadership. 18
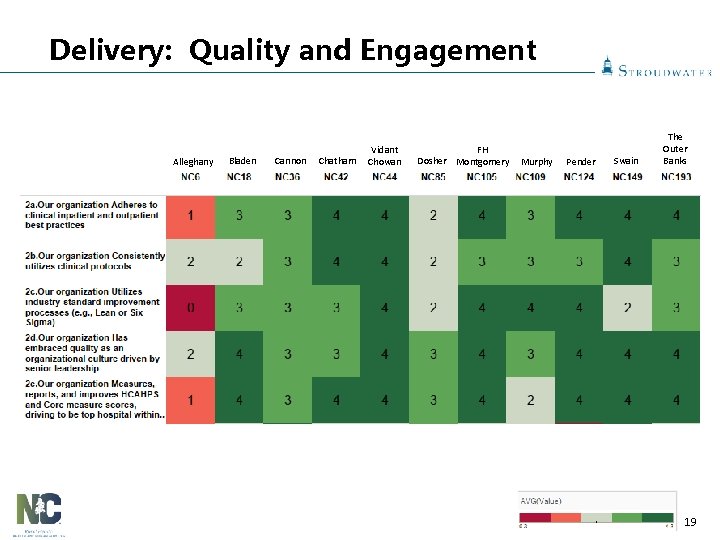
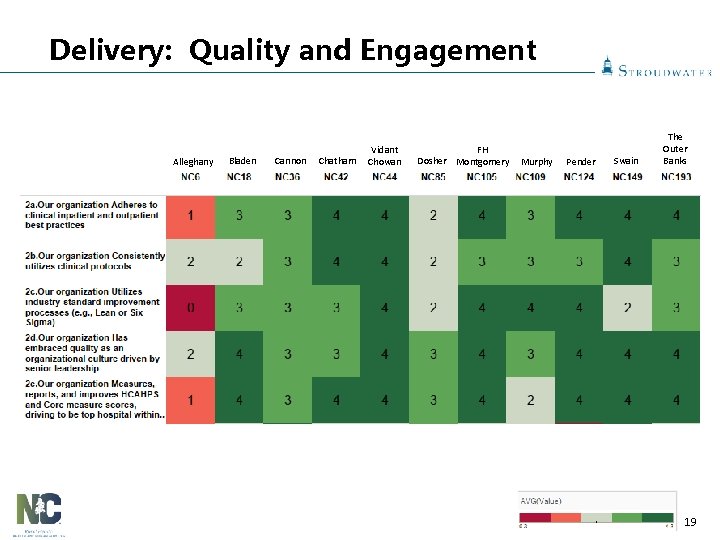
Delivery: Quality and Engagement Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 19
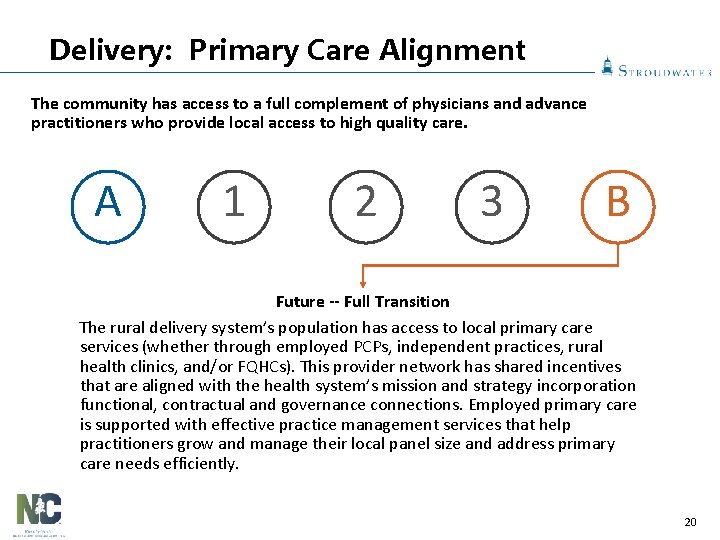
Delivery: Primary Care Alignment The community has access to a full complement of physicians and advance practitioners who provide local access to high quality care. A 1 2 3 B Future -- Full Transition The rural delivery system’s population has access to local primary care services (whether through employed PCPs, independent practices, rural health clinics, and/or FQHCs). This provider network has shared incentives that are aligned with the health system’s mission and strategy incorporation functional, contractual and governance connections. Employed primary care is supported with effective practice management services that help practitioners grow and manage their local panel size and address primary care needs efficiently. 20

Delivery: Primary Care Alignment Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 21
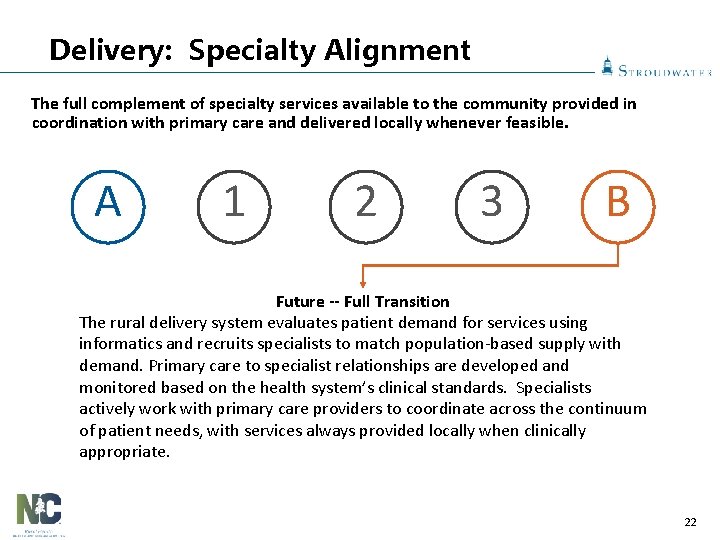
Delivery: Specialty Alignment The full complement of specialty services available to the community provided in coordination with primary care and delivered locally whenever feasible. A 1 2 3 B Future -- Full Transition The rural delivery system evaluates patient demand for services using informatics and recruits specialists to match population-based supply with demand. Primary care to specialist relationships are developed and monitored based on the health system’s clinical standards. Specialists actively work with primary care providers to coordinate across the continuum of patient needs, with services always provided locally when clinically appropriate. 22
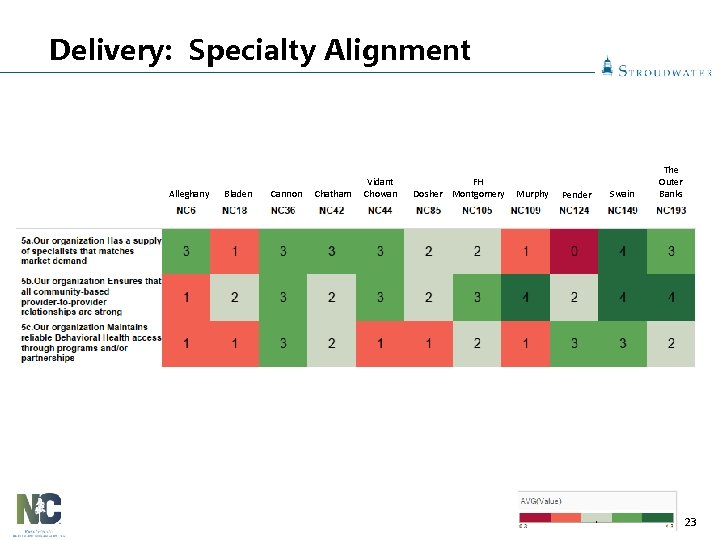
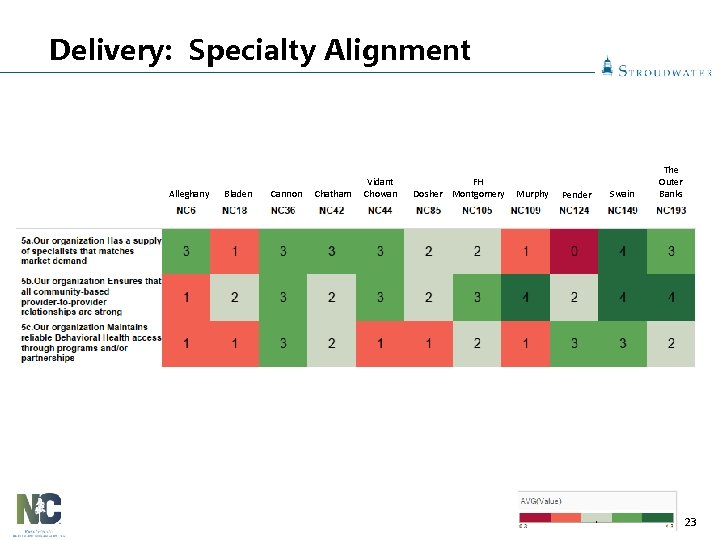
Delivery: Specialty Alignment Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 23
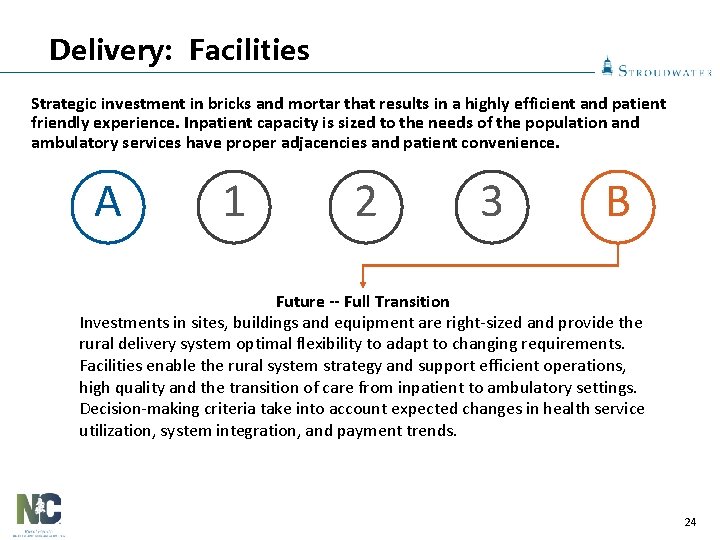
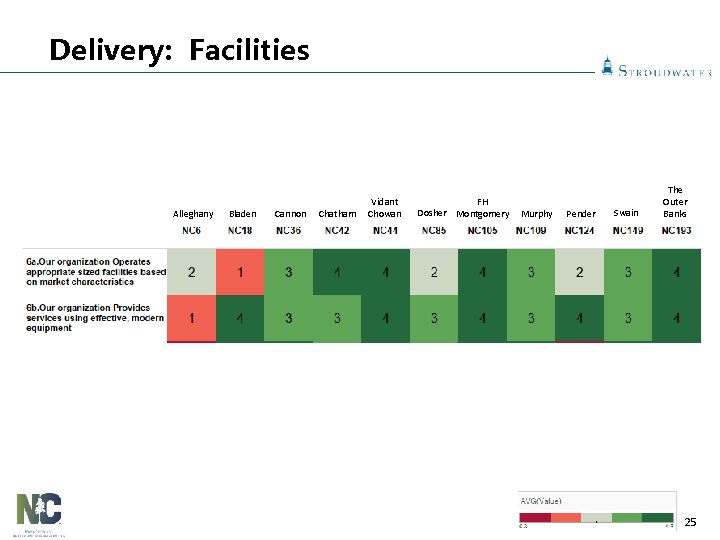
Delivery: Facilities Strategic investment in bricks and mortar that results in a highly efficient and patient friendly experience. Inpatient capacity is sized to the needs of the population and ambulatory services have proper adjacencies and patient convenience. A 1 2 3 B Future -- Full Transition Investments in sites, buildings and equipment are right-sized and provide the rural delivery system optimal flexibility to adapt to changing requirements. Facilities enable the rural system strategy and support efficient operations, high quality and the transition of care from inpatient to ambulatory settings. Decision-making criteria take into account expected changes in health service utilization, system integration, and payment trends. 24
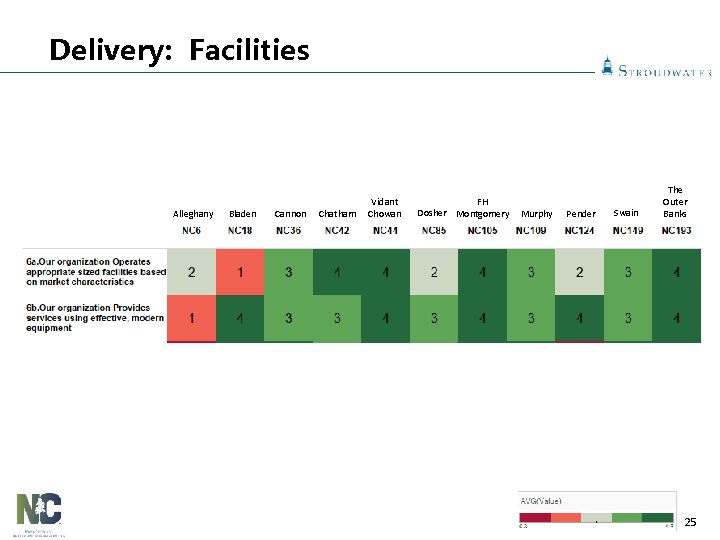
Delivery: Facilities Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 25
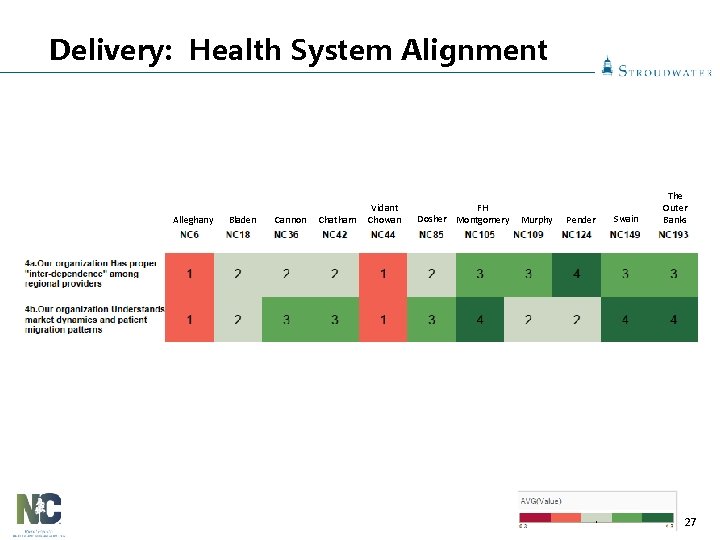
Delivery: Health System Alignment The rural health delivery system uses a proactive strategy to develop its affiliation strategy to enhance the sustainability of service availability and rationalize services across the spectrum of care. A 1 2 3 B Future -- Full Transition The rural delivery system has a regional alignment strategy that includes other providers and/or payers to ensure patients receive all necessary services at the optimal time, place, quality, and cost. The rural system’s partners recognize the value of the rural delivery system, have processes to enhance it, and attribute value back to the primary care site(s). The scale provided through its partnership(s) enable the rural system to access transitional and population-based payment approaches that enhance sustainability. 26
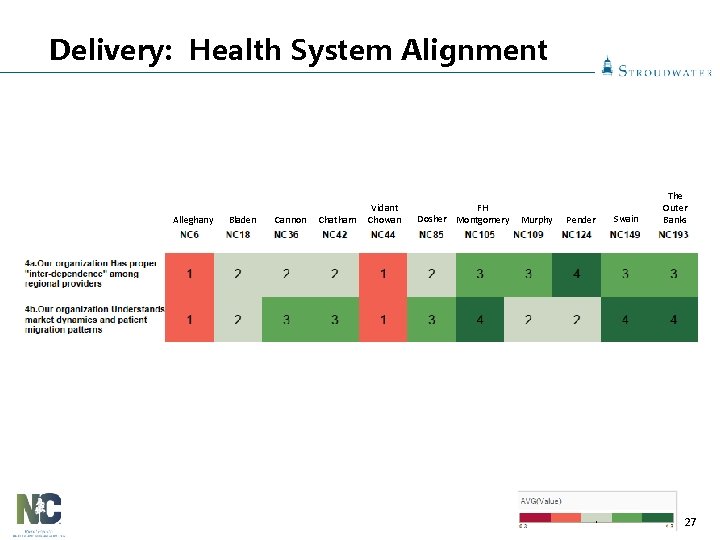
Delivery: Health System Alignment Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 27
Group Questions 2. Do you have a transition plan for Population Health? If so, please share what progress has been made. 28
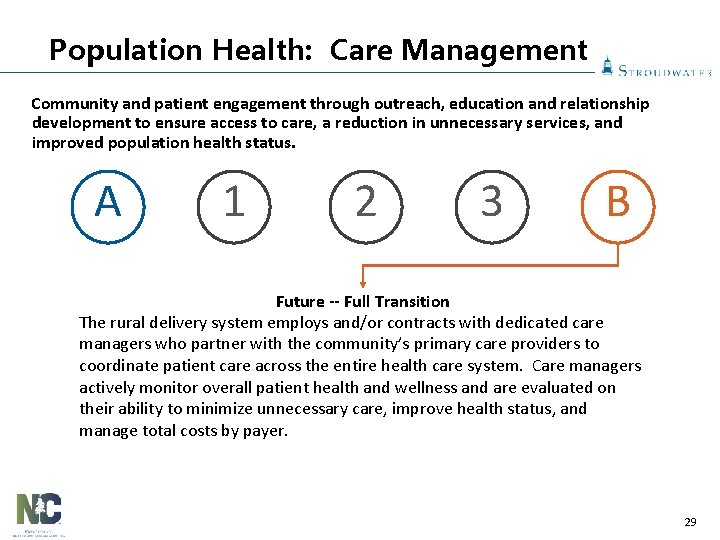
Population Health: Care Management Community and patient engagement through outreach, education and relationship development to ensure access to care, a reduction in unnecessary services, and improved population health status. A 1 2 3 B Future -- Full Transition The rural delivery system employs and/or contracts with dedicated care managers who partner with the community’s primary care providers to coordinate patient care across the entire health care system. Care managers actively monitor overall patient health and wellness and are evaluated on their ability to minimize unnecessary care, improve health status, and manage total costs by payer. 29
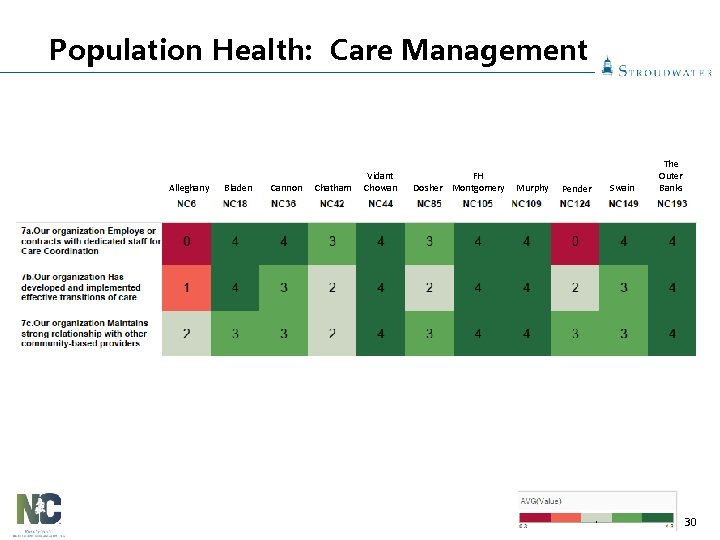
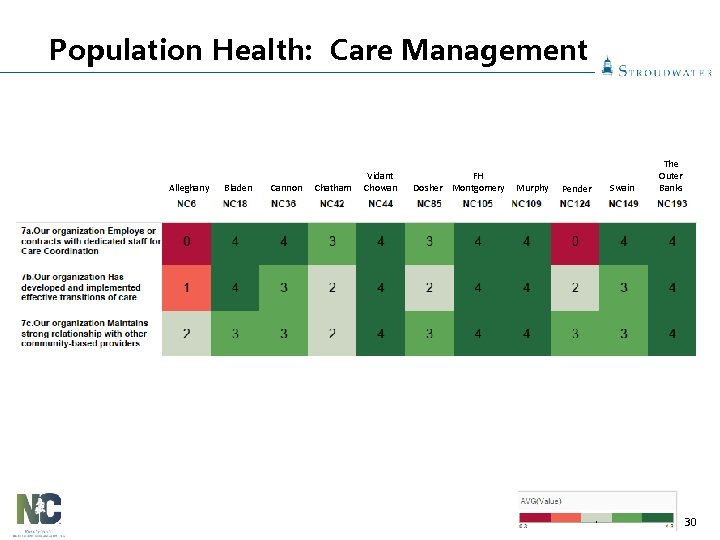
Population Health: Care Management Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 30
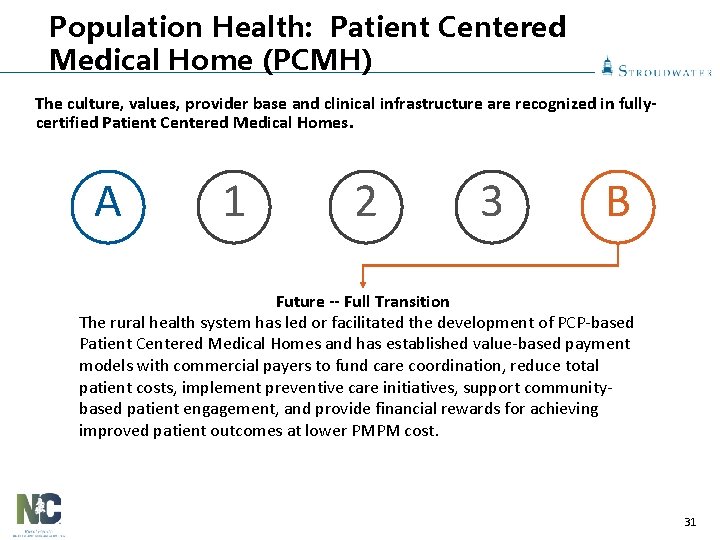
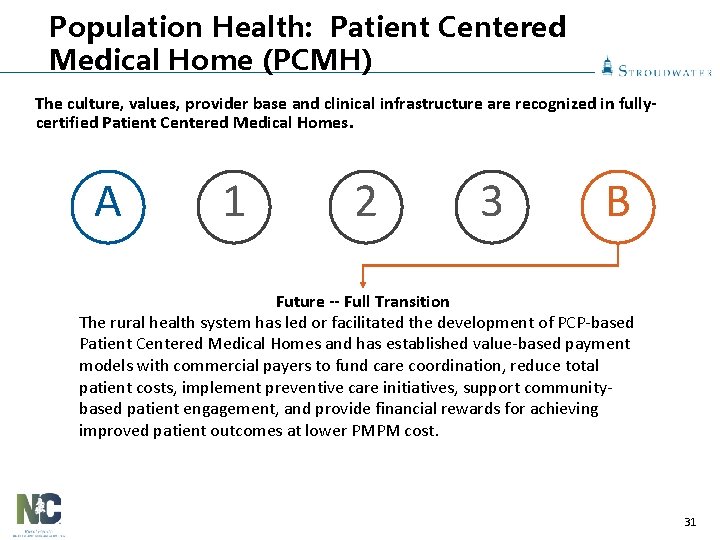
Population Health: Patient Centered Medical Home (PCMH) The culture, values, provider base and clinical infrastructure are recognized in fullycertified Patient Centered Medical Homes. A 1 2 3 B Future -- Full Transition The rural health system has led or facilitated the development of PCP-based Patient Centered Medical Homes and has established value-based payment models with commercial payers to fund care coordination, reduce total patient costs, implement preventive care initiatives, support communitybased patient engagement, and provide financial rewards for achieving improved patient outcomes at lower PMPM cost. 31
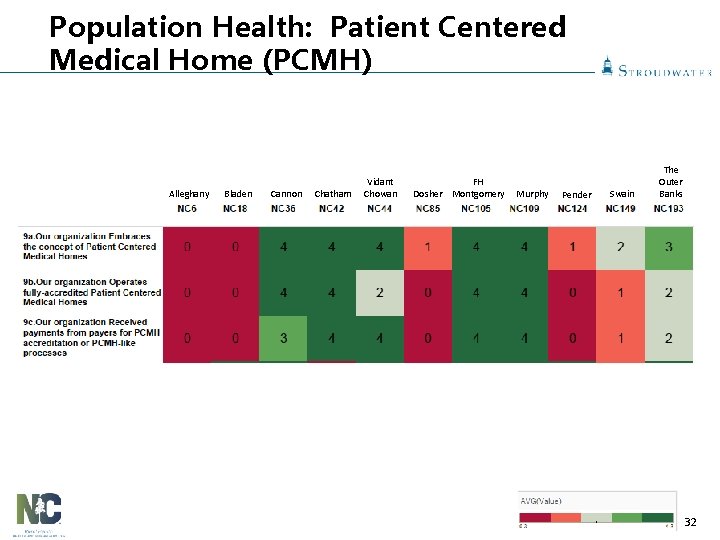
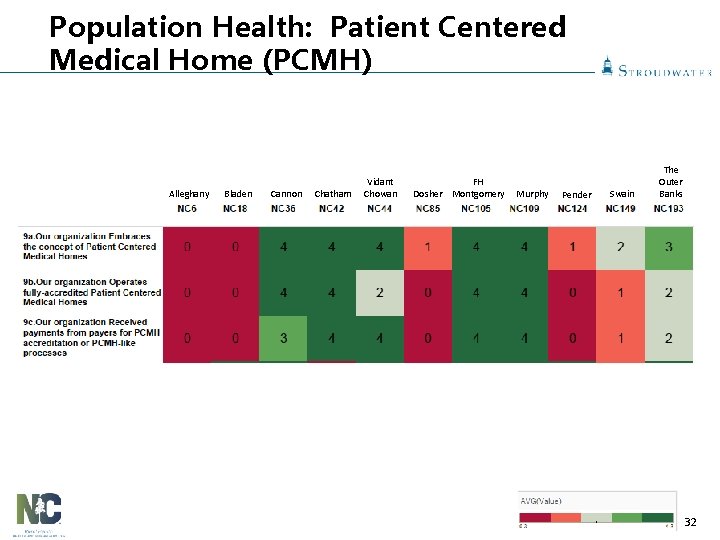
Population Health: Patient Centered Medical Home (PCMH) Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 32
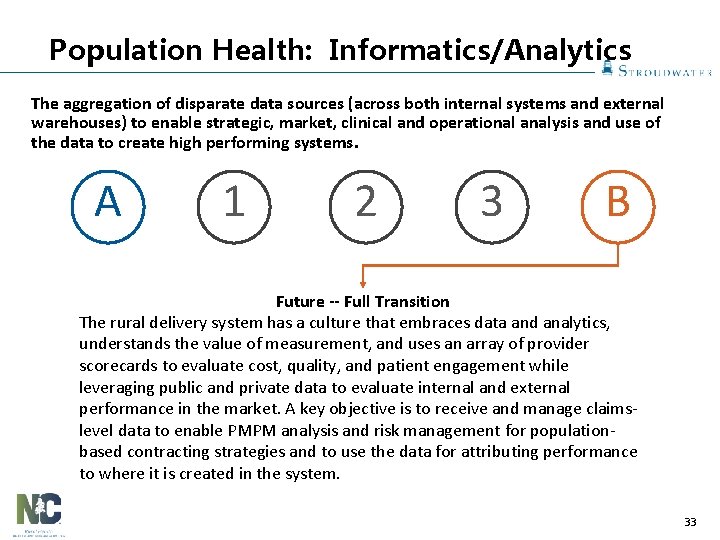
Population Health: Informatics/Analytics The aggregation of disparate data sources (across both internal systems and external warehouses) to enable strategic, market, clinical and operational analysis and use of the data to create high performing systems. A 1 2 3 B Future -- Full Transition The rural delivery system has a culture that embraces data and analytics, understands the value of measurement, and uses an array of provider scorecards to evaluate cost, quality, and patient engagement while leveraging public and private data to evaluate internal and external performance in the market. A key objective is to receive and manage claimslevel data to enable PMPM analysis and risk management for populationbased contracting strategies and to use the data for attributing performance to where it is created in the system. 33
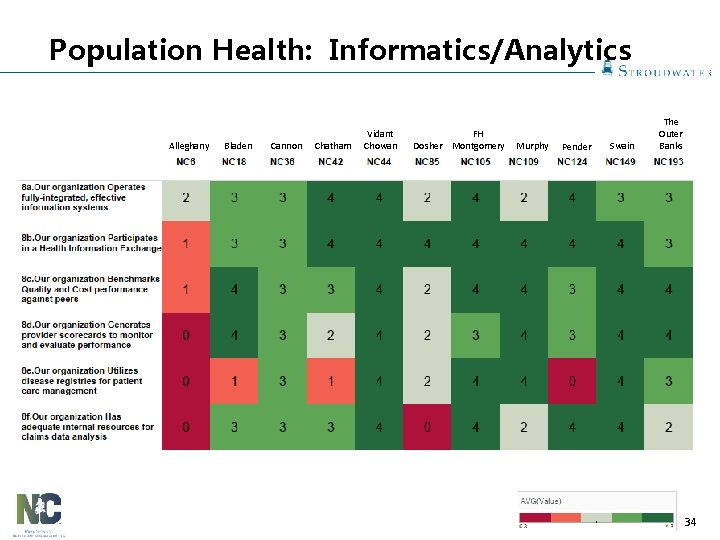
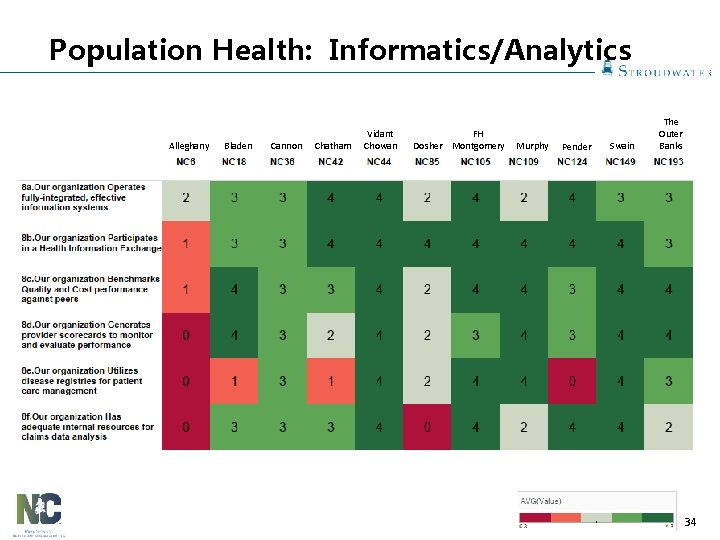
Population Health: Informatics/Analytics Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 34
Culture: Physician Leadership Aligned medical staff buy-into and actively lead, support and/or reinforce health system delivery transformation. A 1 2 3 B Future -- Full Transition The rural delivery system’s medical staff and regional providers are closely aligned with the organization’s mission and strategy, collaborate well as a team and actively embrace system-wide change to preserve the organization’s mission and to fulfill the overarching goal of optimal health outcomes for the community. Key members of the medical staff have assumed leadership roles in the organization and have buy-in from other members of the medical staff. 35
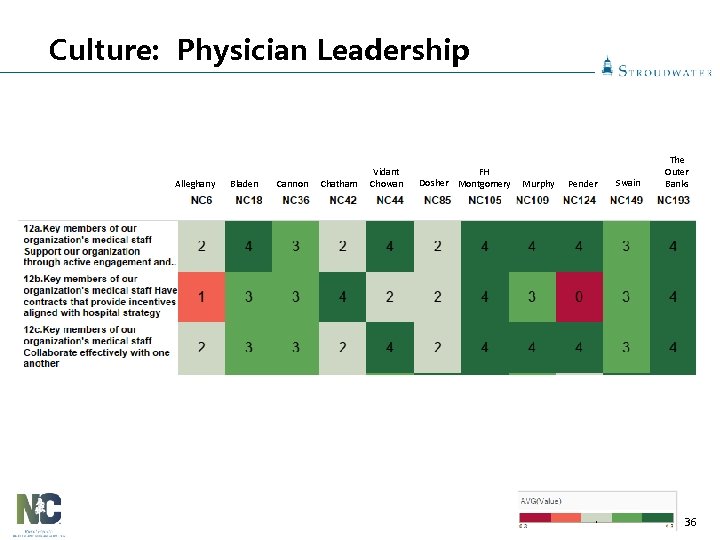
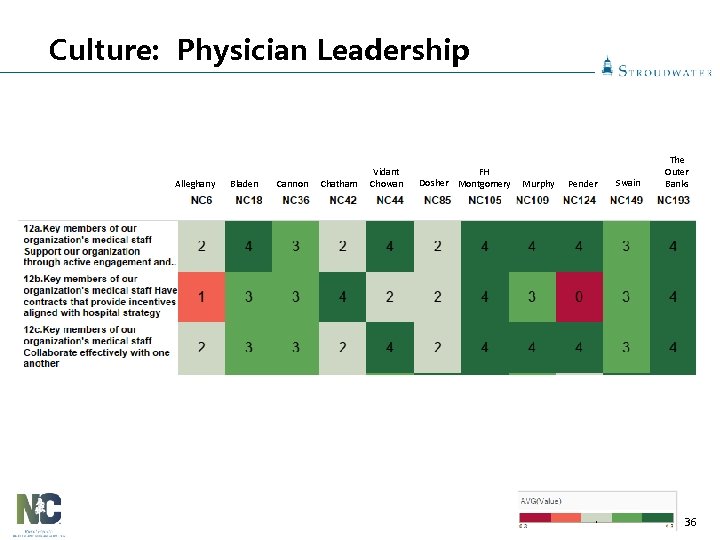
Culture: Physician Leadership Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 36
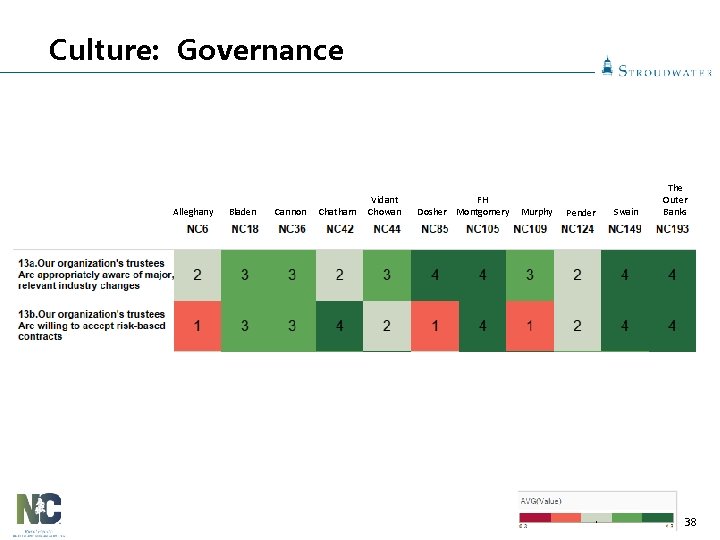
Culture: Governance Hospital trustees understand the urgency and complexity surrounding healthcare transformation and play a fiduciary role in fostering organizational change. A 1 2 3 B Future -- Full Transition The rural delivery system’s Trustees are well educated on the future challenges and impending changes, have endorsed and are monitoring a formal strategy to prepare for the future and are equipped to facilitate and support the management team’s decision making process. Trustees understand execute their fiduciary responsibility consistently. 37
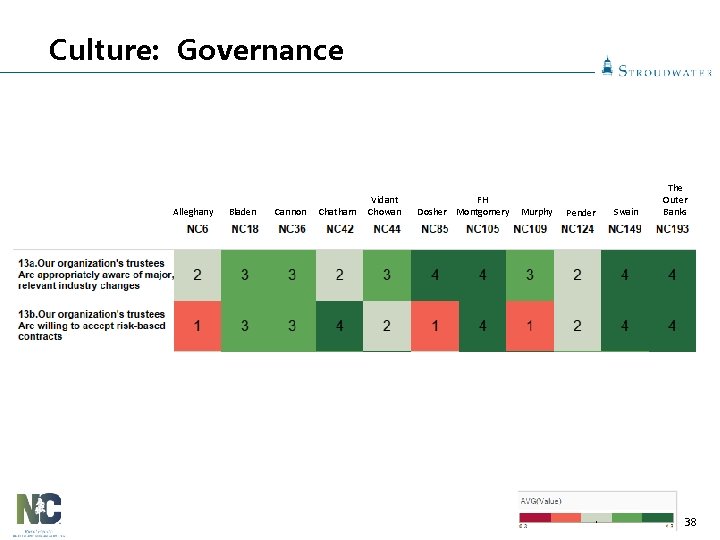
Culture: Governance Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 38
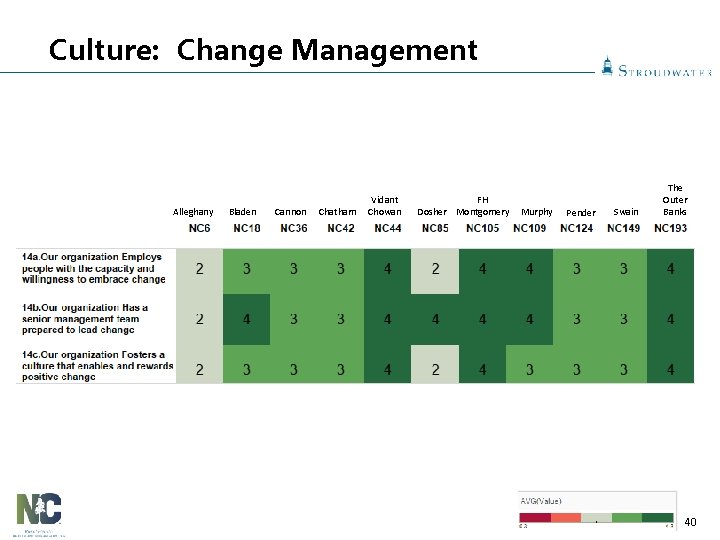
Culture: Change Management Hospital employees, executives, medical staff and trustees recognize the importance of culture and learner styles on the organization’s ability to affect change. A 1 2 3 B Future -- Full Transition Change is viewed as a natural, positive phenomenon that signals the vitality of the rural health system. Staff, physicians and Trustees all embrace the opportunity to improve processes and to grow in ways that are respectful, effective, equitable and efficient. Communication across the system flows seamlessly (vertically and horizontally) based on intentional Organizational Design principles that balance incentives, performance monitoring and decision rights. Growth occurs intentionally with empowered managers who operate as “pitchers” vs. “catchers”. 39
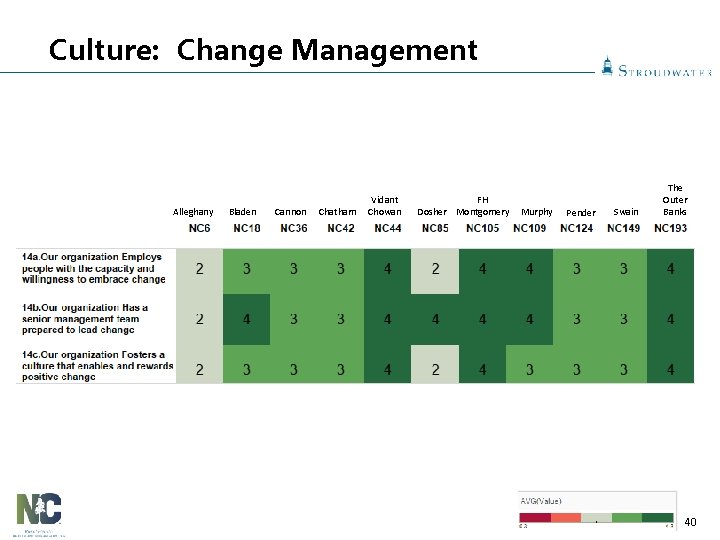
Culture: Change Management Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 40
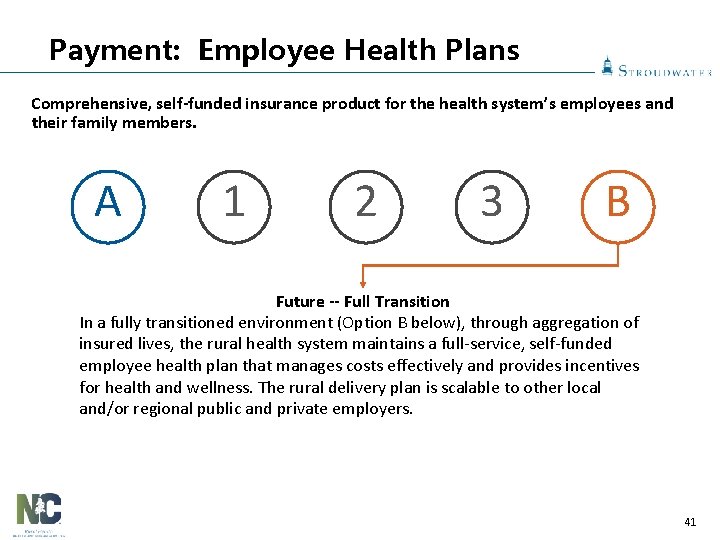
Payment: Employee Health Plans Comprehensive, self-funded insurance product for the health system’s employees and their family members. A 1 2 3 B Future -- Full Transition In a fully transitioned environment (Option B below), through aggregation of insured lives, the rural health system maintains a full-service, self-funded employee health plan that manages costs effectively and provides incentives for health and wellness. The rural delivery plan is scalable to other local and/or regional public and private employers. 41
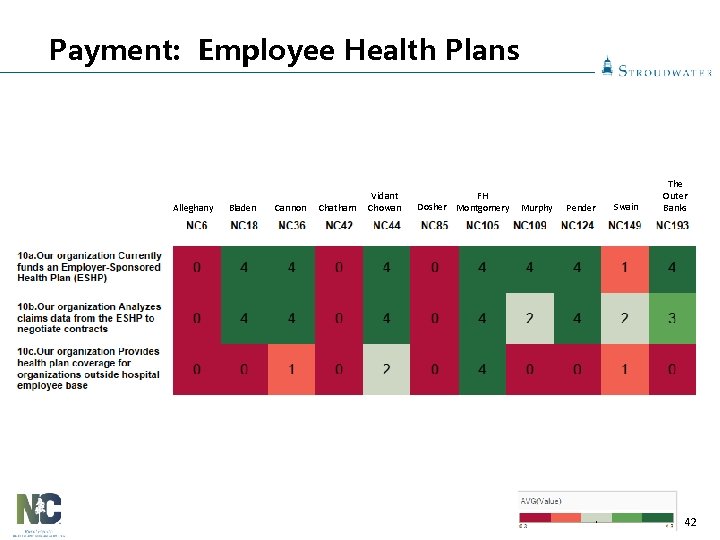
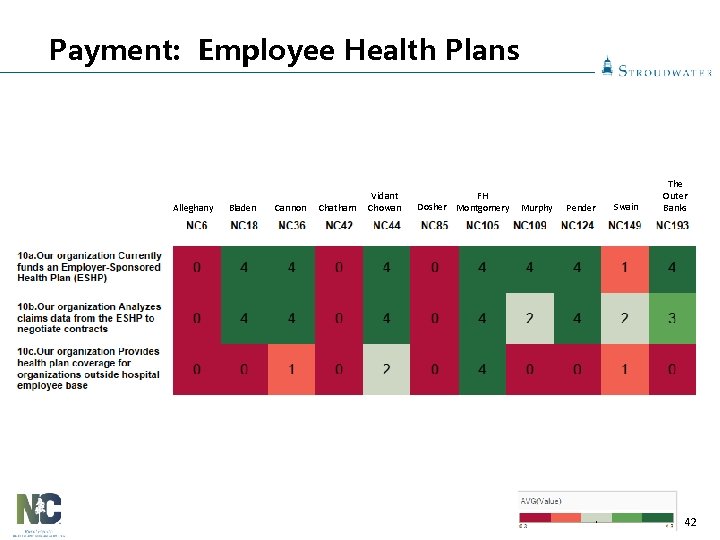
Payment: Employee Health Plans Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 42
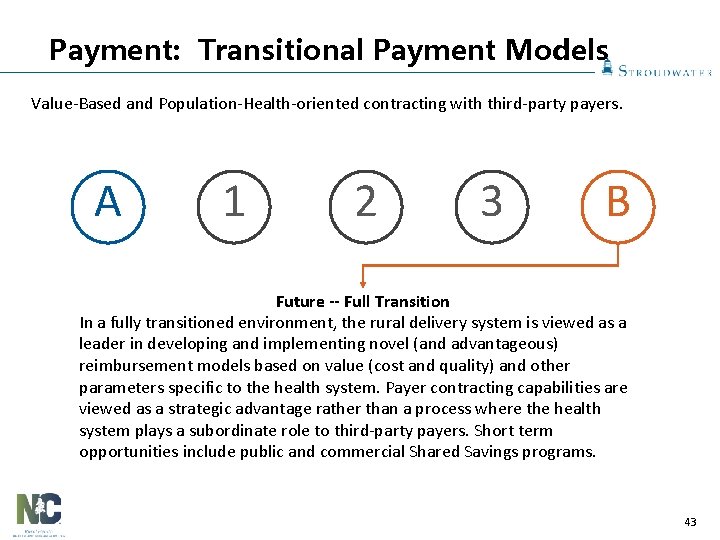
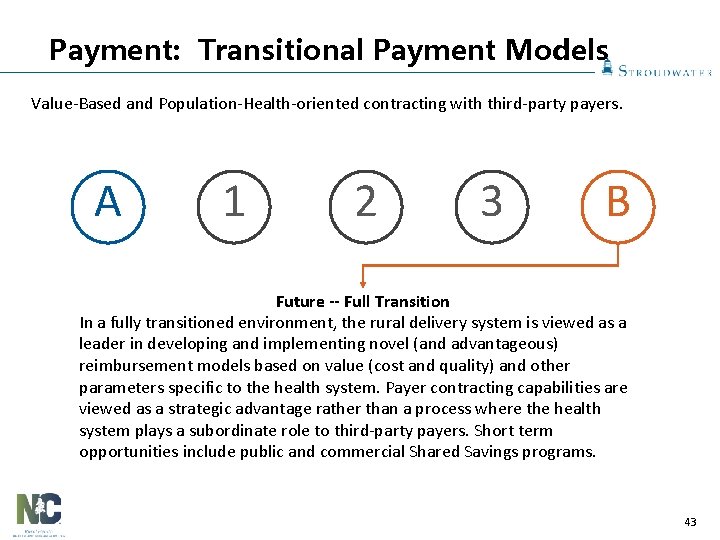
Payment: Transitional Payment Models Value-Based and Population-Health-oriented contracting with third-party payers. A 1 2 3 B Future -- Full Transition In a fully transitioned environment, the rural delivery system is viewed as a leader in developing and implementing novel (and advantageous) reimbursement models based on value (cost and quality) and other parameters specific to the health system. Payer contracting capabilities are viewed as a strategic advantage rather than a process where the health system plays a subordinate role to third-party payers. Short term opportunities include public and commercial Shared Savings programs. 43
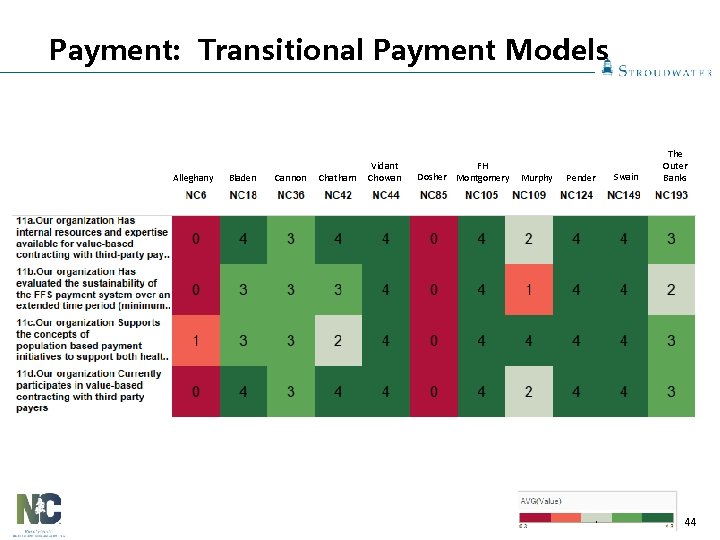
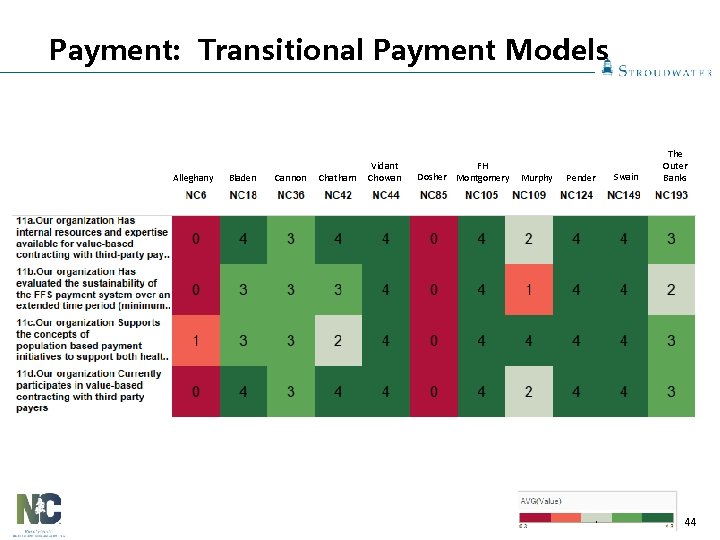
Payment: Transitional Payment Models Alleghany Bladen Cannon Chatham Vidant Chowan FH Dosher Montgomery Murphy Pender Swain The Outer Banks 44
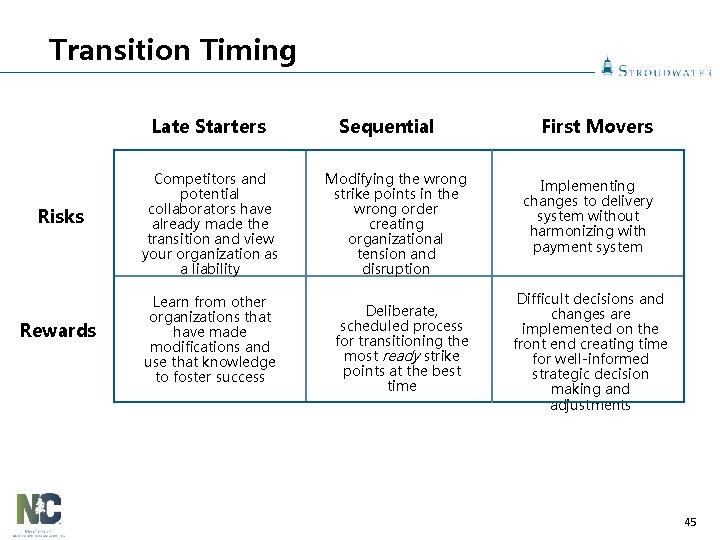
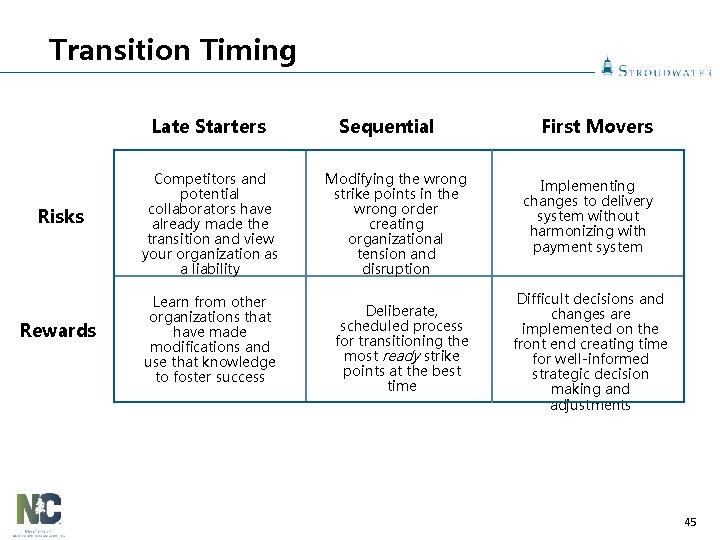
Transition Timing Late Starters Risks Rewards Competitors and potential collaborators have already made the transition and view your organization as a liability Learn from other organizations that have made modifications and use that knowledge to foster success Sequential Modifying the wrong strike points in the wrong order creating organizational tension and disruption Deliberate, scheduled process for transitioning the most ready strike points at the best time First Movers Implementing changes to delivery system without harmonizing with payment system Difficult decisions and changes are implemented on the front end creating time for well-informed strategic decision making and adjustments 45

Addressing your Bottlenecks Operating Efficiencies Assess, benchmark and develop focused action plans Value and Engagement Maximize performance on public reporting programs Care Management Employ or contract for care coordinators Business Practices Ensure high performance revenue cycle management Facilities Health System Alignment Drive out unnecessary PP&E fixed costs Define criteria and monitoring systems for collaborators Physician Leadership Identify, empower and support physician leaders Change Management Educate people and invest in processes to facilitate change 46
Group Questions 3. What actions will you take following this meeting to better prepare your organization for the transition to Population Based payment? 47
Questions? Financial Indicators 1685 Congress St. Suite 202 Portland, Maine 04102 (207) 221 -8250 www. stroudwater. com 48
 Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Semicritical
Semicritical Key risk indicators for vendor management
Key risk indicators for vendor management Indicators of financial abuse
Indicators of financial abuse Key financial indicators
Key financial indicators Chapter test a chapter 4 population ecology answer key
Chapter test a chapter 4 population ecology answer key Section 1 population dynamics
Section 1 population dynamics Population ecology section 1 population dynamics
Population ecology section 1 population dynamics Study guide section 1 population dynamics
Study guide section 1 population dynamics Critical reading meaning
Critical reading meaning What is health indicators
What is health indicators Indicator of health
Indicator of health Community health status indicators
Community health status indicators Population health risk assessment and management
Population health risk assessment and management Chapter 2 population and health key issue 3
Chapter 2 population and health key issue 3 Population health
Population health Paula stewart medical officer of health
Paula stewart medical officer of health Population health program manager
Population health program manager Financial and non financial motivation
Financial and non financial motivation Unit 2 lesson 3 health insurance and financial planning
Unit 2 lesson 3 health insurance and financial planning Unit 2 lesson 3 health insurance and financial planning
Unit 2 lesson 3 health insurance and financial planning Young workers readiness certificate
Young workers readiness certificate Workplace readiness skills positive work ethics
Workplace readiness skills positive work ethics School readiness goals
School readiness goals What is the importance of follower readiness?
What is the importance of follower readiness? Employment readiness scale
Employment readiness scale Bge mirror settings will
Bge mirror settings will Potty training readiness checklist
Potty training readiness checklist Trl calculator excel
Trl calculator excel Test readiness review
Test readiness review School readiness goals
School readiness goals Production readiness review
Production readiness review Postsecondary education readiness test
Postsecondary education readiness test Lexile levels by grade
Lexile levels by grade Pai readiness
Pai readiness Organizational readiness to change assessment
Organizational readiness to change assessment What is operational readiness testing
What is operational readiness testing Horrid hent
Horrid hent College lexile level
College lexile level Material condition of readiness
Material condition of readiness Peek readiness to learn
Peek readiness to learn Kindergarten readiness checklist colorado
Kindergarten readiness checklist colorado Jen piaget
Jen piaget Cisco ise urt
Cisco ise urt Ipo readiness roadmap
Ipo readiness roadmap National career readiness certificate
National career readiness certificate Emdr readiness checklist
Emdr readiness checklist Implementation readiness checklist
Implementation readiness checklist Cmdb implementation checklist
Cmdb implementation checklist