Toilet training for children with autism POSITIVE BEHAVIOUR

Toilet training for children with autism POSITIVE BEHAVIOUR SUPPORT SERVICES TRASNA TRAINING SERVICE
Overview of Toileting Workshop ➲Evening 1 ‘Getting everything in place’ ➲Evening 2 ‘Planning implementation’ ➲Evening 3 ‘Reviewing implementation and planning further steps’
Agenda Evening 1 ➲Welcome and Introduction ➲Goal setting ➲General information on toileting ➲Break ➲Homework
Setting Goals!!! What do you want to get out of this workshop? ?
Delays in learning to toilet are common in the general population. With Day time wetting ‘Affecting approximately 1 in 75 children over the age of five’ and approximately 15% of 5 year old experiencing night time wetting. Source ERIC (The UK Childhood Continence Charity)
Toileting: a complex skill ● ● ● ● Motor functions Muscle control Understanding of directions Understanding of toileting process Understanding of process of elimination Ability to learn a new skill Able to observe modeling & follow
The learning process ● Developmental delay might have impacted on various milestones, toileting one of these ○ Frustration, sadness, pressure ● Setbacks and accidents are part of the process ○ What to do: ■ Do not scold ■ Remain as neutral and calm as possible ● Is difficult - What could you do? Plan ahead!
Developmental Patterns: Bladder and Bowel Functioning ➲Bowel and bladder grow bigger so that more waste can be held – that’s why babies need so frequent nappy changes! ➲When growth happens, reflex to hold and pass is triggered ➲We must learn to control this reflex for successful toilet training
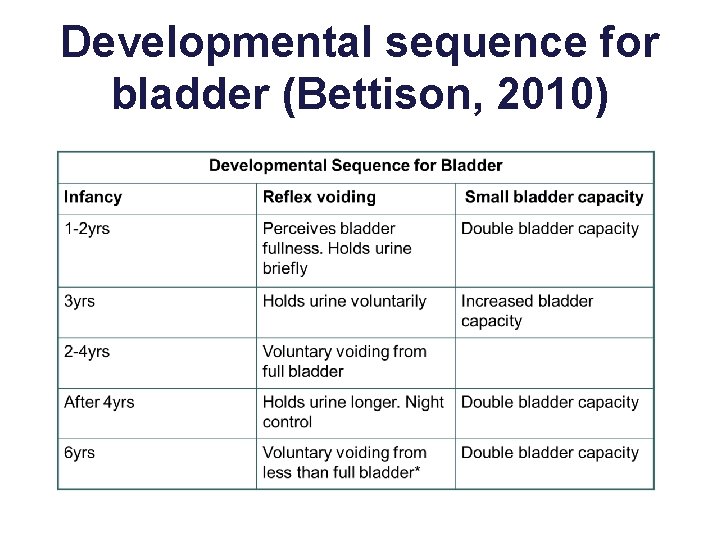
Developmental sequence for bladder (Bettison, 2010)
Any time before 6, a child does not have full control over their bladder i. e. cannot always voluntarily produce urine – that’s why you put child on the toilet when you know they have a full bladder but they don’t go, they may have an accident two minutes later!!
BREAK
The common challenges experienced ➲Day time wetting (Diurnal enuresis) ➲Night time wetting (Nocturnal enuresis) ➲Soiling (Encopresis)

Before toilet training begins ➲ Let the child get used to the bathroom, make it a fun place! ➲ Start changing the child's nappy in the bathroom so they begin to associate the two. ➲ Modelling- let the child see a parent or sibling use the toilet. ➲ Autonomy and control for child is important – no pressure
You will receive a toileting pack to take home which contains: ➲The medical checklist ➲The readiness checklist ➲Blank data sheets

Interaction with physical illness & medical conditions Checklist 1 1. Children with autism are more than 3. 5 times more likely to suffer chronic diarrhea or constipation (Centre for Disease Control and Prevention, CDC) 2. Frequent gastrointestinal problems can result in abdominal pain, gaseousness, and pain on stooling. 3. Seizure activity and medications for seizures and other illness can impact toileting.
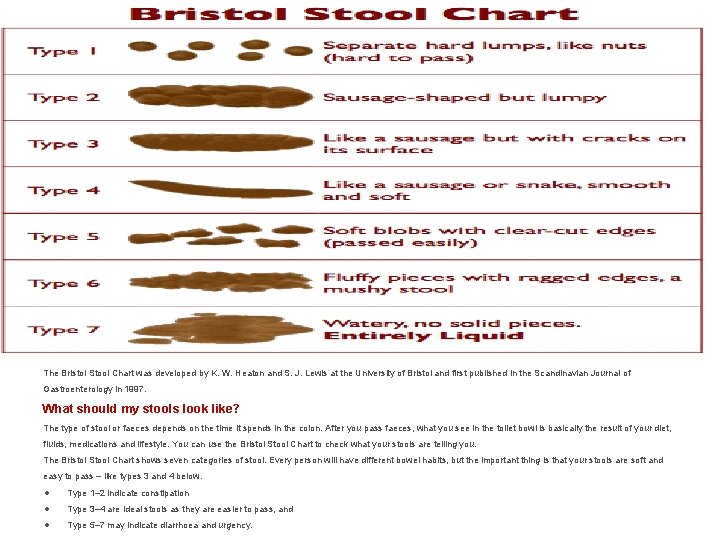
The Bristol Stool Chart was developed by K. W. Heaton and S. J. Lewis at the University of Bristol and first published in the Scandinavian Journal of Gastroenterology in 1997. What should my stools look like? The type of stool or faeces depends on the time it spends in the colon. After you pass faeces, what you see in the toilet bowl is basically the result of your diet, fluids, medications and lifestyle. You can use the Bristol Stool Chart to check what your stools are telling you. The Bristol Stool Chart shows seven categories of stool. Every person will have different bowel habits, but the important thing is that your stools are soft and easy to pass – like types 3 and 4 below. ● Type 1– 2 indicate constipation ● Type 3– 4 are ideal stools as they are easier to pass, and ● Type 5– 7 may indicate diarrhoea and urgency.
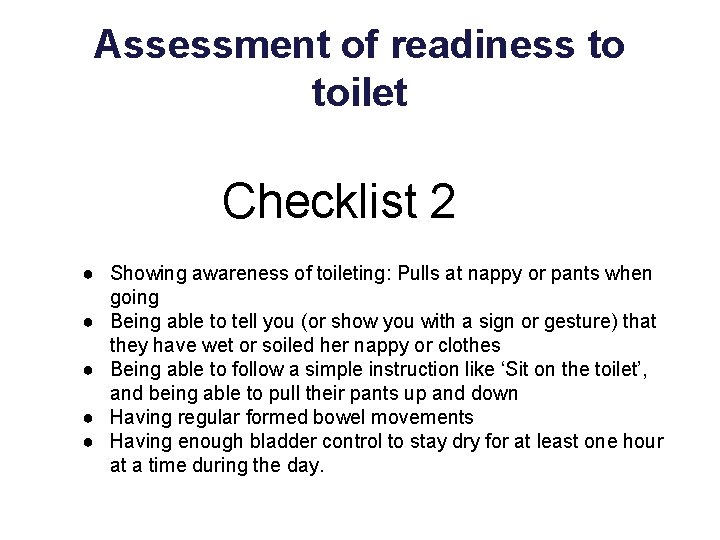
Assessment of readiness to toilet Checklist 2 ● Showing awareness of toileting: Pulls at nappy or pants when going ● Being able to tell you (or show you with a sign or gesture) that they have wet or soiled her nappy or clothes ● Being able to follow a simple instruction like ‘Sit on the toilet’, and being able to pull their pants up and down ● Having regular formed bowel movements ● Having enough bladder control to stay dry for at least one hour at a time during the day.
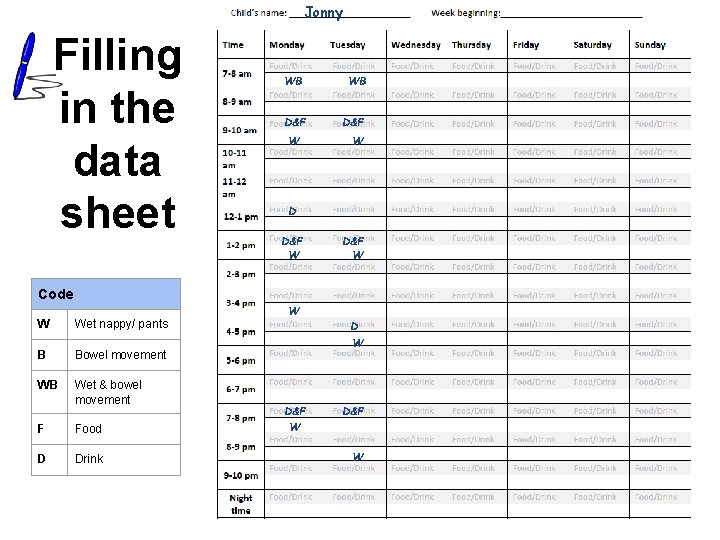
Jonny Filling in the data sheet WB D&F W D D&F W Code W Wet nappy/ pants B Bowel movement WB Wet & bowel movement F Food D Drink W D&F W
Our recommendations for the next week • Checklist 1, ensuring that all the common medical concerns are addressed. • Complete Checklist 2. To give a better idea of your child's level of readiness for toilet training. • Bring your child to the bathroom so that they get used to it, make it a positive place! • Watch and record, using the sheets provided.

Thank you for giving your time and attention to this workshop

Toilet training for children with autism POSITIVE BEHAVIOUR SUPPORT SERVICES TRASNA TRAINING SERVICE
Agenda Evening 2 ➲Check in ➲Toilet training interventions ➲Break ➲Development of individualised toileting programmes
Quick reminder ● Aim of this workshop: ○ Provision of information ● Readiness ○ Is your child ticking all the boxes in the readiness checklist? ○ Is this the right time to teach toileting (for you and your child)? ○ The information can be used at a more appropriate time.
Interventions ➲Modeling and use of reinforcement ➲Visual Sequences ➲Social Stories ➲Fading/shaping ➲Task analysis ▪ Backward chaining ▪ Forward chaining
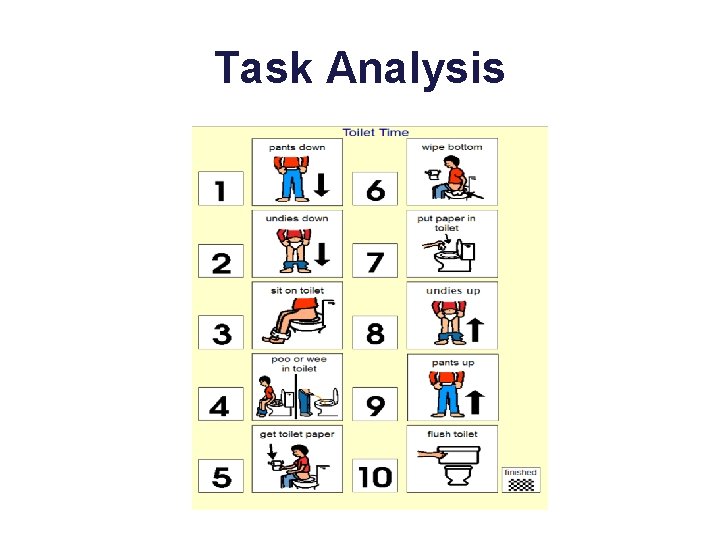
Task Analysis
Interventions ➲Increase fluid intake ▪ ▪ Can increase bladder capacity Increase opportunities for learning Emphasise feeling of full bladder Use salty snacks for children who are less likely to take fluids. ➲About 30 mins for drink to pass ➲This is the optimal time to take your child to the bathroom. ➲This does not mean you take your child to the bathroom every 30 minutes!!
Toilet training protocol ● Remove nappy and increase fluid intake. ● Only let your child sit on the toilet for a maximum of 3 minutes (sing songs together etc). ● Minimally train during a 4 hour period to be considered toilet training. ● There will be accidents!! remember to change your child in the toilet. ● Consider highly reinforcing items (access to I-pad, sweet) that can be given immediately on the toileting step you have decided upon. ● Set realistic steps to be achieved by your child e. g. treat for going into the toilet, or sitting on the toilet etc. .
BREAK
Designing a Toileting Plan for your child ● We are going to include the information on toilet training in your toileting pack. . This will assist in the next stage of designing a toileting plan for your child. ● We are now going to divide into groups where Rachel, Mareike and myself will take a group each and support each person to outline a possible toileting plan for your child. ● Because of time constraints we will divide the time evenly for each child so that everyone goes away with an outline of a plan. Each group will also support in the process of designing each child's plan. ● Let's go!!

Thank you for giving your time and attention to this workshop

Toilet training for children with autism POSITIVE BEHAVIOUR SUPPORT SERVICES TRASNA TRAINING SERVICE
Agenda Evening 3 ➲Check in ➲Toilet training troubleshooting ➲Break ➲Check in on goals ➲Further toileting resources

BREAK
Helpful resources for toilet training • Urine alarms- used for nocturnal enuresis • A bedwetting alarm is a device that wakes a child who wets the bed. Many have a sensor which is worn in the pyjamas or pants. The sensor is linked to an alarm. If the sensor gets wet, it immediately activates the alarm. • Toilet training Apps • Free apps which can be downloaded from the app store to help with potty training. These include The Potty Book, Potty Training — Learning with the animals. • Toilet training videos • Useful videos to encourage your child to use the potty. They can help normalise the potty and provide helpful visual cues. Videos include Elmo’s Potty Time song and Tom & Emily going to the bathroom. • Links to all of the above resources can be found in the Toilet training pack.
References Ardiç, A. , & Cavkaytar, A. (2014). Effectiveness of the modified intensive toilet training method on teaching toilet skills to children with autism. Education and Training in Autism and Developmental Disabilities, 263 -276. Azrin, N. H. , & Foxx, R. M. (1971). A rapid method of toilet training the institutionalized retarded. Journal of applied behavior analysis, 4(2), 89 -99. DOI: 10. 1901/jaba. 1971. 4 -89 Bainbridge, N. , & Smith Myles, B. (1999). The use of priming to introduce toilet training to a child with autism. Focus on Autism and Other Developmental Disabilities, 14(2), 106 -109. DOI: 10. 1177/108835769901400206 Bettison, S. (1978). Toilet training the retarded: analysis of the stages of development and procedures for designing programs. Australian Journal of Mental Retardation, 5(3), 95 -100. DOI: 10. 3109/13668257809010176 Brazelton, T. B. (1962). A child-oriented approach to toilet training. Pediatrics, 29(1), 121 -128. Call, N. A. , Mevers, J. L. , Mc. Elhanon, B. O. , & Scheithauer, M. C. (2017). A multidisciplinary treatment for encopresis in children with developmental disabilities. Journal of Applied Behavior Analysis, 50(2), 332 -344. DOI: 10. 1002/jaba. 379 Chaidez, V. , Hansen, R. L. , & Hertz-Picciotto, I. (2014). Gastrointestinal problems in children with autism, developmental delays or typical development. Journal of autism and developmental disorders, 44(5), 1117 -1127. DOI: 10. 1007/s 10803 -013 -1973 -x Cicero, F. R. , & Pfadt, A. (2002). Investigation of a reinforcement-based toilet training procedure for children with autism. Research in Developmental Disabilities, 23(5), 319 -331. DOI: 10. 1016/SO 8914222(02)00136 -1
Cocchiola, M. A. , Martino, G. M. , Dwyer, L. J. , & Demezzo, K. (2012). Toilet training children with autism and developmental delays: an effective program for school settings. Behavior analysis in practice, 5(2), 60 -64. DOI: 10. 1007/BF 03391824 Doan, D. , & Toussaint, K. A. (2017). A parent-oriented approach to rapid toilet training. International Electronic Journal of Elementary Education, 9(2), 473 -486. DOI: 10. 1177/10883576050200020601 Friman, P. C. (1986). A preventive contexttfor enuresis. Pediatric Clinics of North America, 33(4), 871 -886. DOI: 10. 1016/S 0031 -3955(16)36078 -3 Gorrindo, P. , Williams, K. C. , Lee, E. B. , Walker, L. S. , Mc. Grew, S. G. , & Levitt, P. (2012). Gastrointestinal dysfunction in autism: parental report, clinical evaluation, and associated factors. Autism Research, 5(2), 101 -108. DOI: 10. 1002/aur. 237 Greer, B. D. , Neidert, P. L. , & Dozier, C. L. (2016). A component analysis of toilet‐training procedures recommended for young children. Journal of applied behavior analysis, 49(1), 69 -84. DOI: 10. 1002/jaba. 275 Gorzki, P. A. (1999). Toilet training guidelines: The role of the parent in toilet training. Pediatrics, 103(6, suppl. ), 1362 -1363. Kroeger, K. , & Sorensen, R. (2010). A parent training model for toilet training children with autism. Journal of Intellectual Disability Research, 54(6), 556 -567. DOI: 10. 1111/j. 1365 -2788. 2010. 01286. x Levato, L. E. , Aponte, C. A. , Wilkins, J. , Travis, R. , Aiello, R. , Zanibbi, K. , . . . & Mruzek, D. W. (2016). Use of urine alarms in toilet training children with intellectual and developmental disabilities: A review. Research in developmental disabilities, 53, 232 -241. DOI: 10. 1016/j. ridd. 2016. 02. 007 Mack, A. H. (2011). Association of Hospitalization for Infection in Childhood With Diagnosis of Autism Spectrum Disorders. Year Book of Psychiatry & Applied Mental Health, 2011(C), 58 -59. DOI: 10. 1016/j. ypsy. 2010. 09. 005 Mahoney, K. , Wagenen, R. , & Meyerson, L. (1971). Toilet training of normal and retarded children. Journal of Applied Behavior Analysis, 4(3), 173 -181. DOI: 10. 1901/jaba. 1971. 4 -173
Mannion, A. , & Leader, G. (2013). Comorbidity in autism spectrum disorder: A literature review. Research in Autism Spectrum Disorders, 7(12), 1595 -1616. DOI: 10. 1016/j. rasd. 2013. 09. 006 Mc. Elhanon, B. O. , Mc. Cracken, C. , Karpen, S. , & Sharp, W. G. (2014). Gastrointestinal symptoms in autism spectrum disorder: a meta-analysis. Pediatrics, 133(5), 872 -883. Nikolov, R. N. , Bearss, K. E. , Lettinga, J. , Erickson, C. , Rodowski, M. , Aman, M. G. & Arnold, L. E. (2009). Gastrointestinal symptoms in a sample of children with pervasive developmental disorders. Journal of autism and developmental disorders, 39(3), 405 -413. DOI: 10. 1007/s 10803 -008 -0637 -8 Rinald, K. , & Mirenda, P. (2012). Effectiveness of a modified rapid toilet training workshop for parents of children with developmental disabilities. Research in Developmental Disabilities, 33(3), 933 -943. DOI: 10. 1016/j. ridd. 2012. 01. 003 Schieve, L. A. , Gonzalez, V. , Boulet, S. L. , Visser, S. N. , Rice, C. E. , Braun, K. V. N. , & Boyle, C. A. (2012). Concurrent medical conditions and health care use and needs among children with learning and behavioral developmental disabilities, National Health Interview Survey, 2006– 2010. Research in developmental disabilities, 33(2), 467 -476. DOI: 10. 1016/j. ridd. 2011. 10. 008 Warzak, W. J. , Forcino, S. S. , Sanberg, S. A. , & Gross, A. C. (2016). Advancing Continence in Typically Developing Children: Adapting the Procedures of Foxx and Azrin for Primary Care. Journal of Developmental & Behavioral Pediatrics, 37(1), 83 -87. DOI: 10. 1097/DBP. 0000000232
- Slides: 37