PATIENTS FUNDERS PHYSICIANS Physician Retirement Patient Experience A






- Slides: 58
PATIENTS FUNDERS PHYSICIANS Physician Retirement & Patient Experience: A Shared Responsibility
Presenters Marty Crapper: Executive Director Cheryl English: Director of Programs and Services Brandice Hartin: Manager of Primary Care Relationships with Commercial Interests: none Grants/Research Support: none Speakers Bureau/Honoraria: none Consulting Fees: We wish! none Other: none
Mr. and Mrs. Crapper

Clients of a bank in Brighton for 40 years Longstanding relationship based on trust Personal relationship with manager
Ways in which the bank offered help We notified patients with a prominent ad in the newspaper 3 months before we closed We could not possibly contact each of our clients directly You will need to seek a new bank who will accept you on your own. Here is a list of bank manager names Good luck!
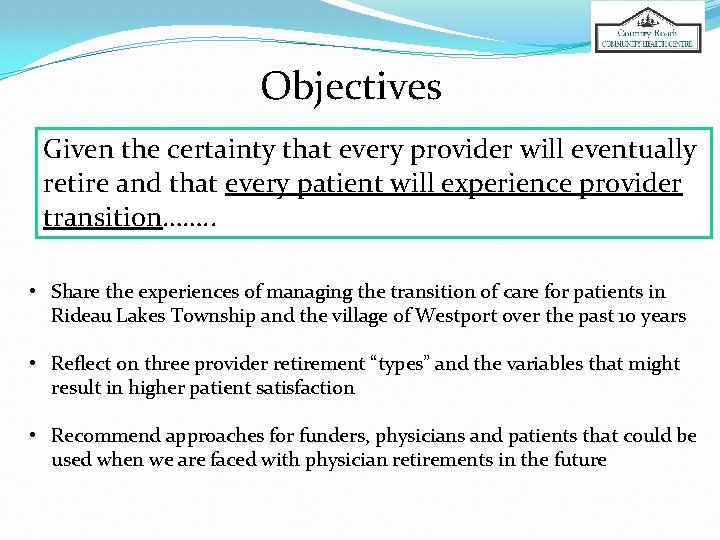
Objectives Given the certainty that every provider will eventually retire and that every patient will experience provider transition……. . • Share the experiences of managing the transition of care for patients in Rideau Lakes Township and the village of Westport over the past 10 years • Reflect on three provider retirement “types” and the variables that might result in higher patient satisfaction • Recommend approaches for funders, physicians and patients that could be used when we are faced with physician retirements in the future
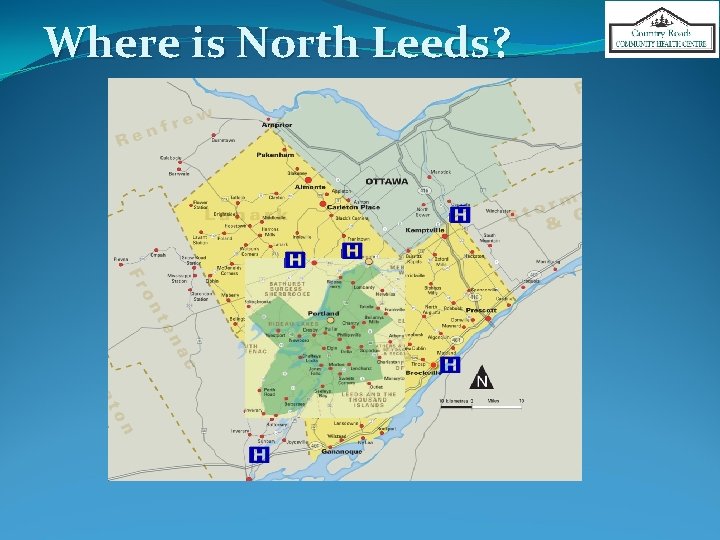
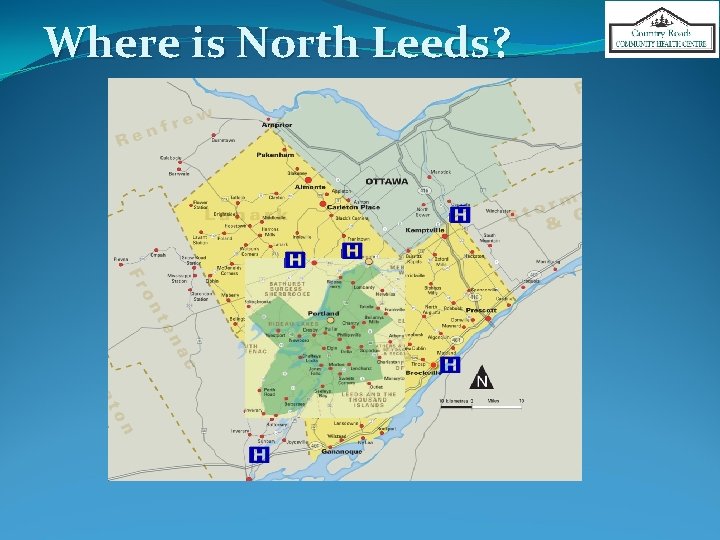
Where is North Leeds?
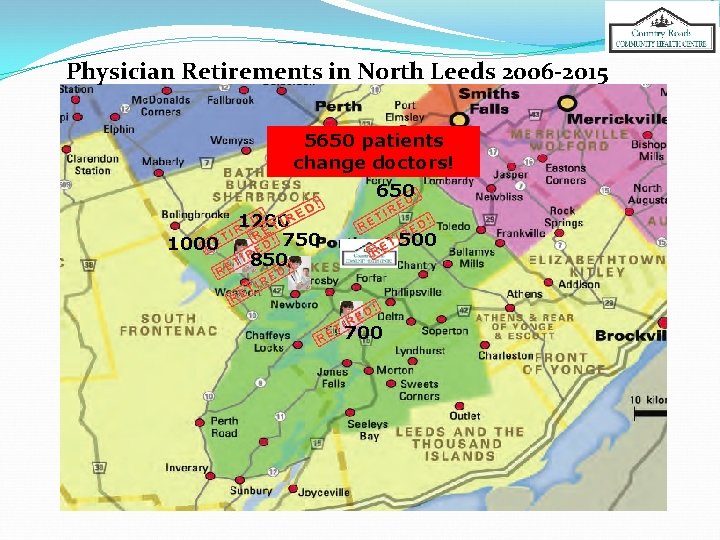
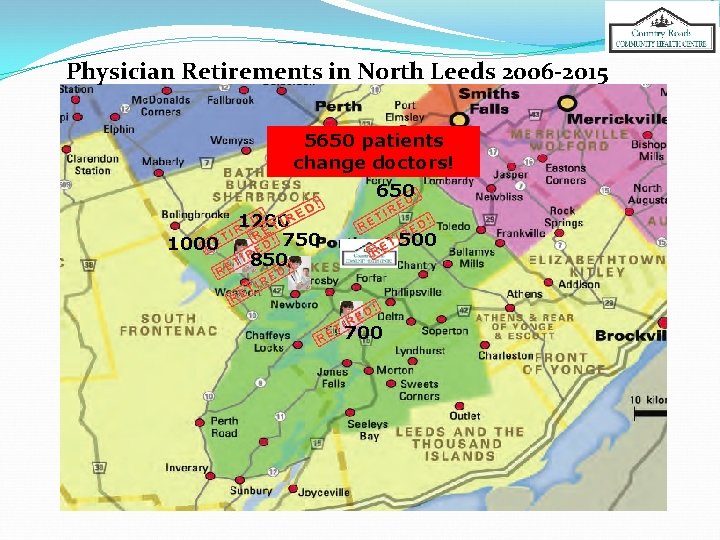
Physician Retirements in North Leeds 2006 -2015 5650 patients change doctors! 650 1000 1200 750 850 500 700


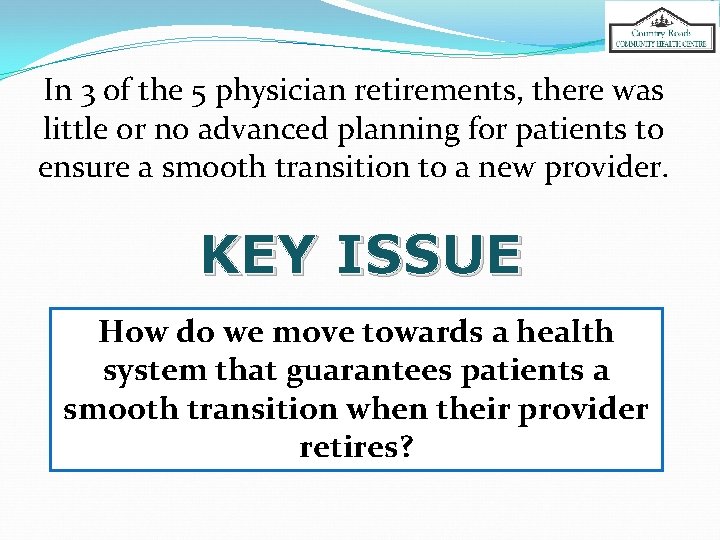
In 3 of the 5 physician retirements, there was little or no advanced planning for patients to ensure a smooth transition to a new provider. KEY ISSUE How do we move towards a health system that guarantees patients a smooth transition when their provider retires?
5 MD RETIREMENTS RESULTED IN TOTAL SHIFT OF 3, 000 PEOPLE IN NORTH LEEDS IN PAST 3 -5 YEARS 3 of 5 had no advanced planning
Impacts �Anxiety �Continuity of care �Provider Client therapeutic relationship * �Trust breakdown �Provider burdens �Confusion �Misinformation *American Medical Association, 2003
Limited literature on effect of health outcomes & continuity of care when a provider leaves, however……… “Comfort with a provider and trust were the attributes of therapeutic relationship that are most poignantly mentioned by patients” Journal of General Internal Medicine, 2008
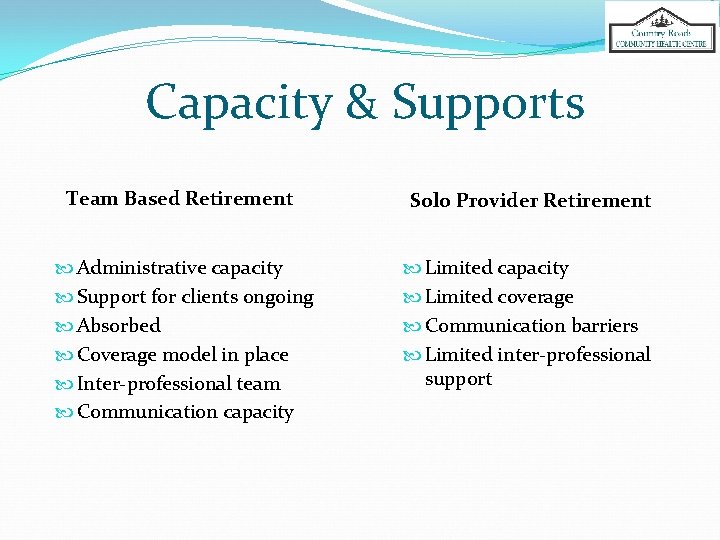
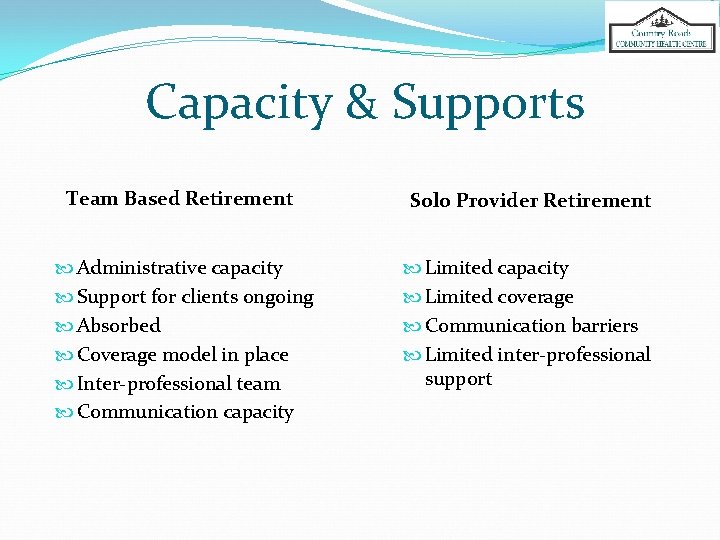
Capacity & Supports Team Based Retirement Solo Provider Retirement Administrative capacity Support for clients ongoing Absorbed Coverage model in place Inter-professional team Communication capacity Limited coverage Communication barriers Limited inter-professional support
Our Experiences ü Team based practice (internal CHC) ü Solo Practice setting (less common in 2016 but still out there!) ü LHIN funded pilot

Client Experience
What did we want to know? Were there any differences in experiences for people who had providers from different models? What type of supports best help people who experience a loss of provider?
What We Asked �Age (age 70 average) �What support did you receive? �Specific experience (how they learned of their doctor leaving) �Emotional impact �What additional support would have helped you?
How We Asked Random telephone survey 20 from each of the 3 types: solo (unsupported), team (CHC) and LHIN funded pilot. �Name of previous doctor (for “type” assignment) � 3 questions about overall satisfaction with the way they learned about and were supported through the transition to a new provider.
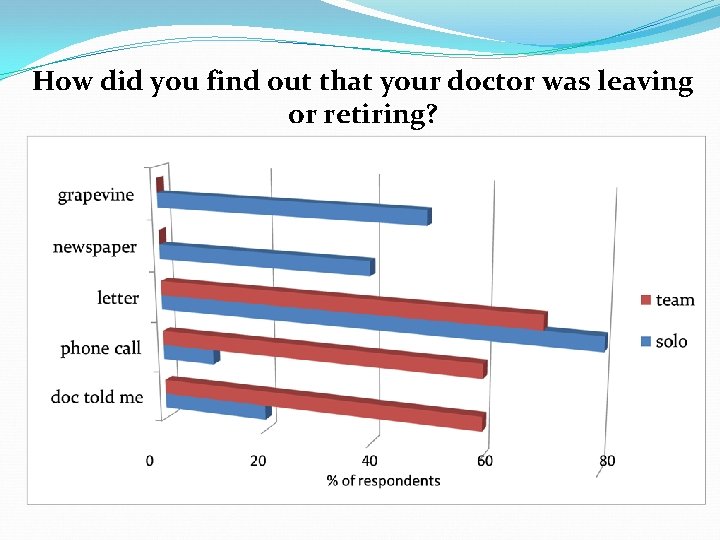
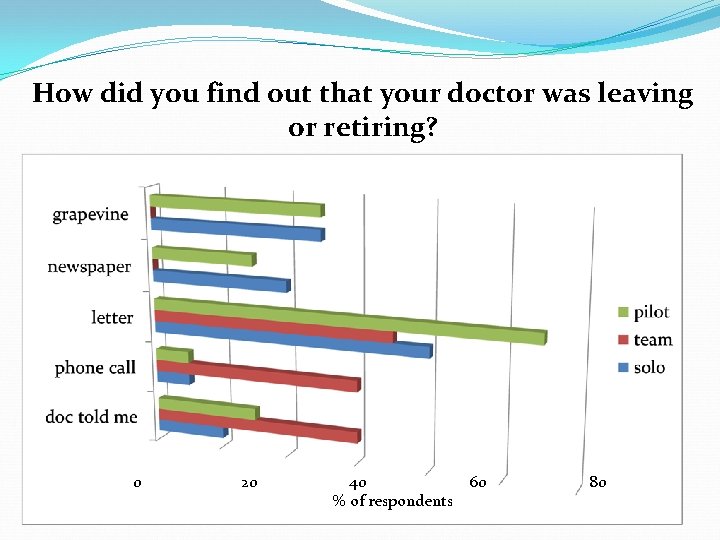
How did you find out your doctor was leaving? � Doctor told me directly � I received a letter � I received a phone call � I read it in the newspaper � I heard it informally through a friend or neighbour � Other
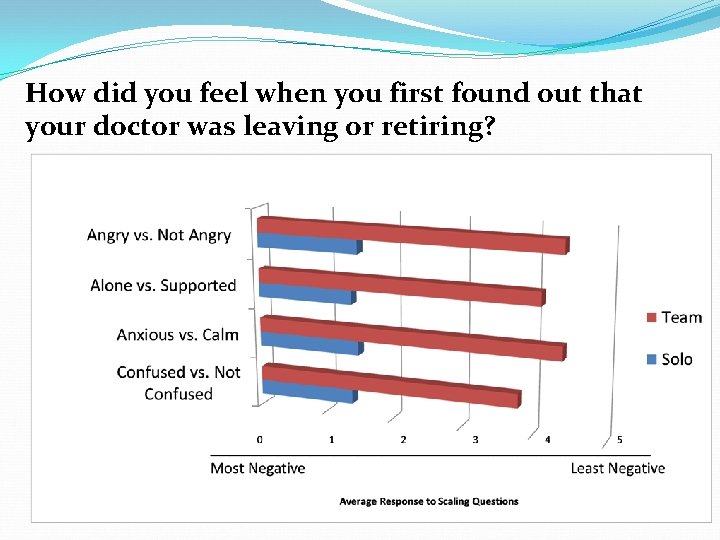
How did you feel when you first found out that your doctor was leaving? (Scale 0 to 5) � Confused vs. Not Confused � Anxious vs. Calm � Alone vs. Supported � Angry vs. Not Angry � Other Feelings
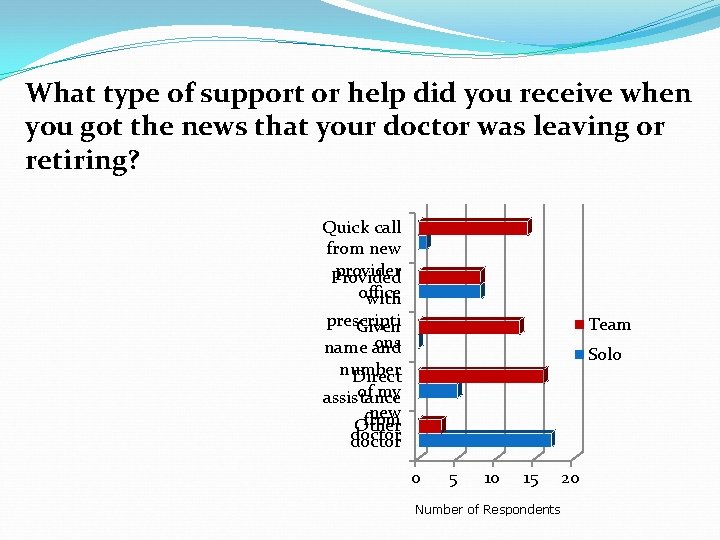
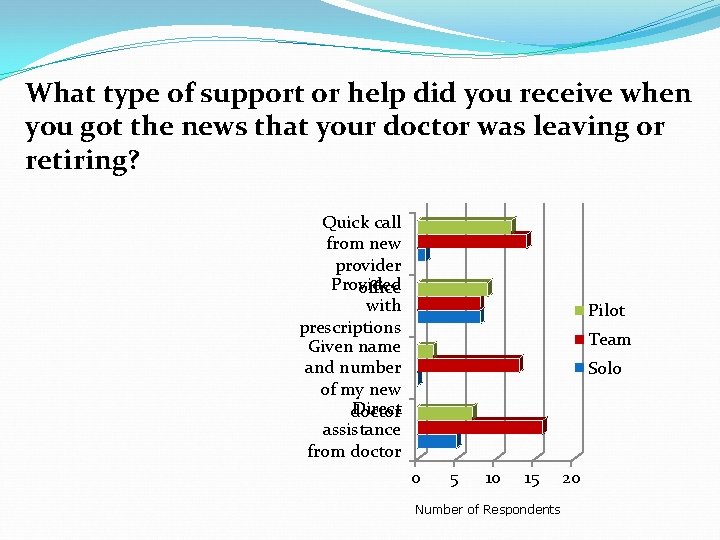
What types of support did you receive when you found out that your doctor was leaving? I received direct assistance from my doctor’s office I was given the name and number of my new doctor I was provided enough medication for the length of time needed I got a call from someone at the new provider office quickly Other
Given your experience this past year, what do you think should happen when a doctor leaves or retires to make it a better process for the patient?

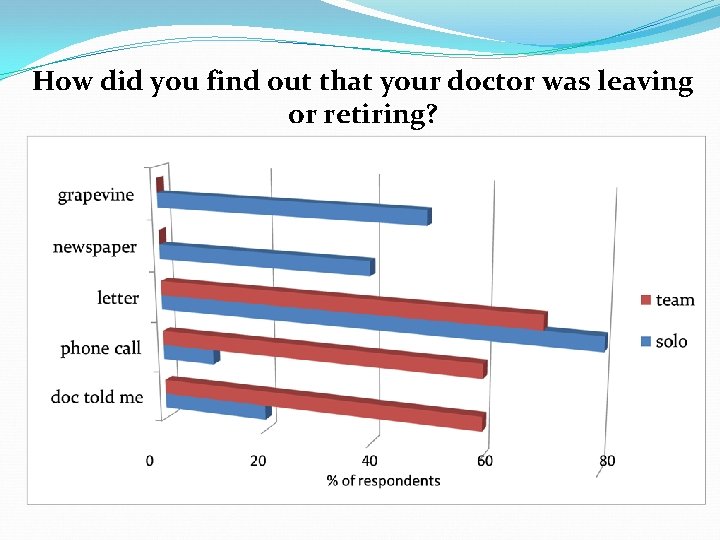
How did you find out that your doctor was leaving or retiring?
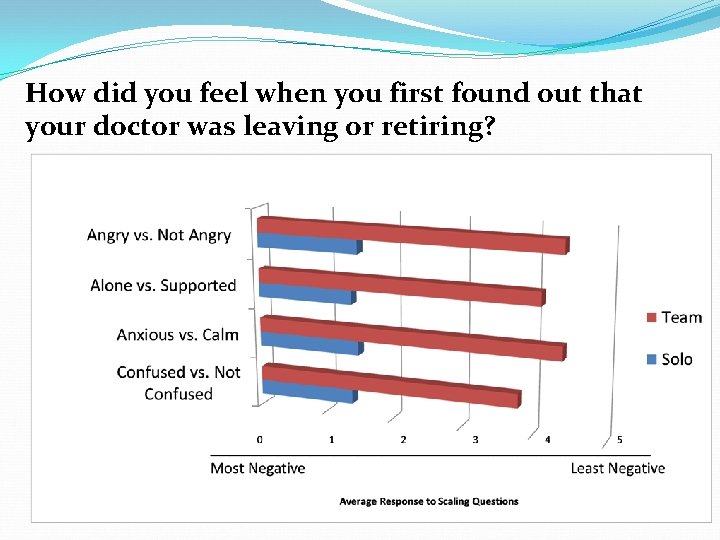
How did you feel when you first found out that your doctor was leaving or retiring?
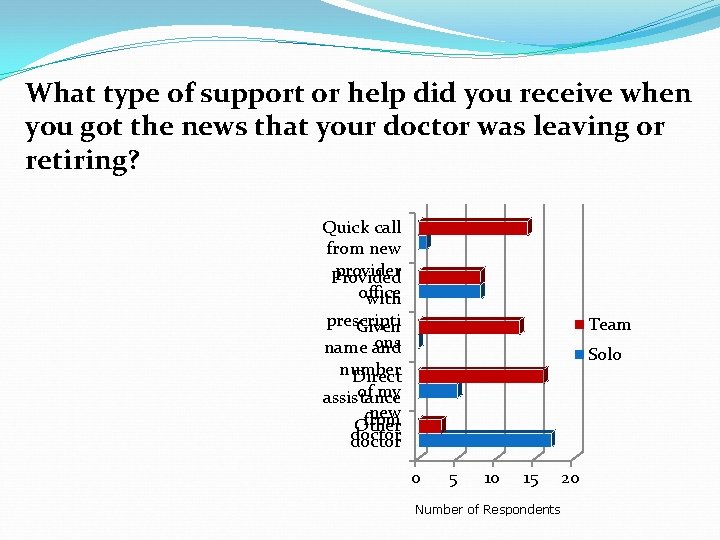
What type of support or help did you receive when you got the news that your doctor was leaving or retiring? Quick call from new provider Provided office with prescripti Given ons name and Team Solo number Direct of my assistance new from Other doctor 0 5 10 15 Number of Respondents 20
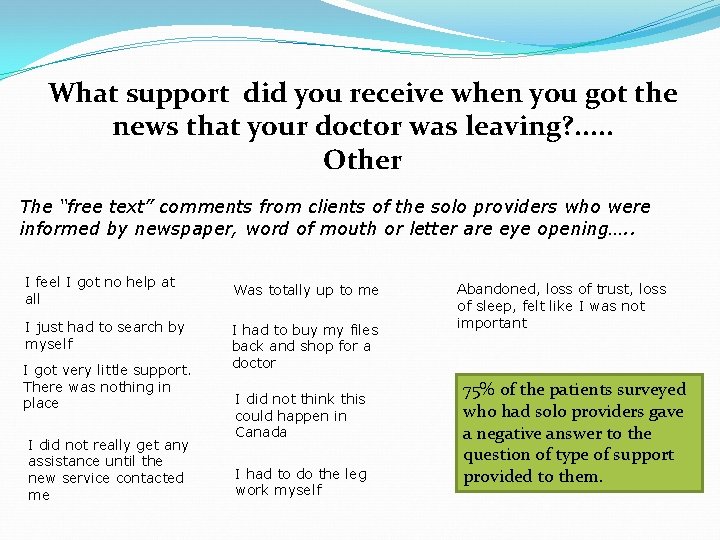
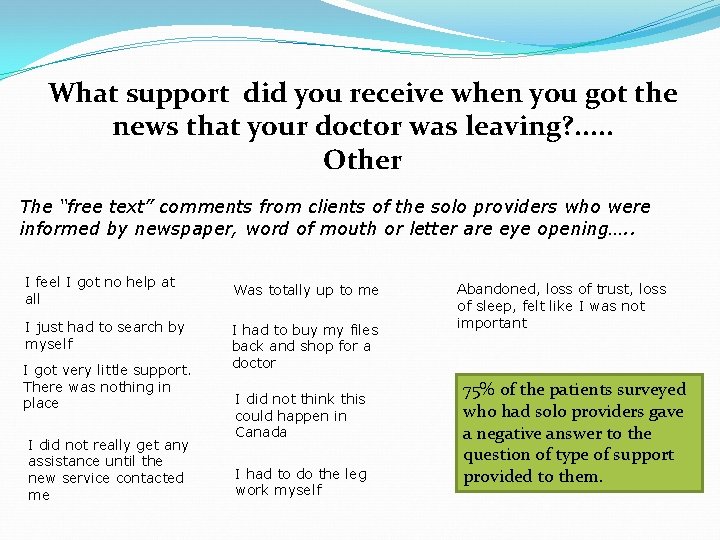
What support did you receive when you got the news that your doctor was leaving? . . . Other The “free text” comments from clients of the solo providers who were informed by newspaper, word of mouth or letter are eye opening…. . I feel I got no help at all I just had to search by myself I got very little support. There was nothing in place I did not really get any assistance until the new service contacted me Was totally up to me I had to buy my files back and shop for a doctor I did not think this could happen in Canada I had to do the leg work myself Abandoned, loss of trust, loss of sleep, felt like I was not important 75% of the patients surveyed who had solo providers gave a negative answer to the question of type of support provided to them.
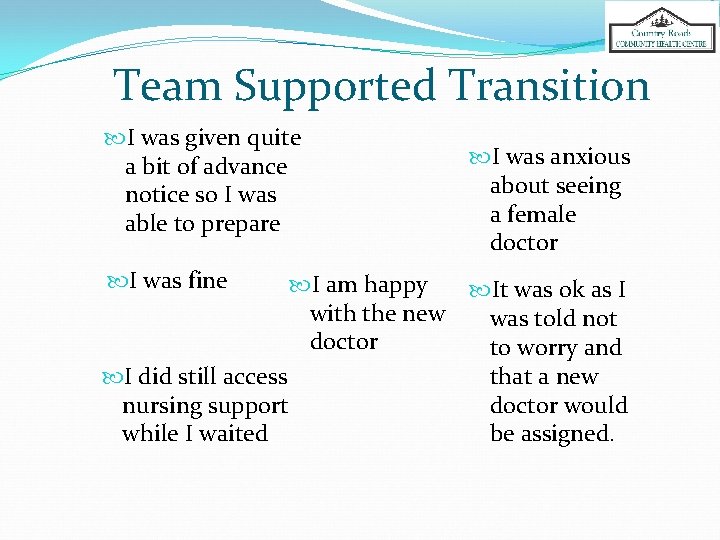
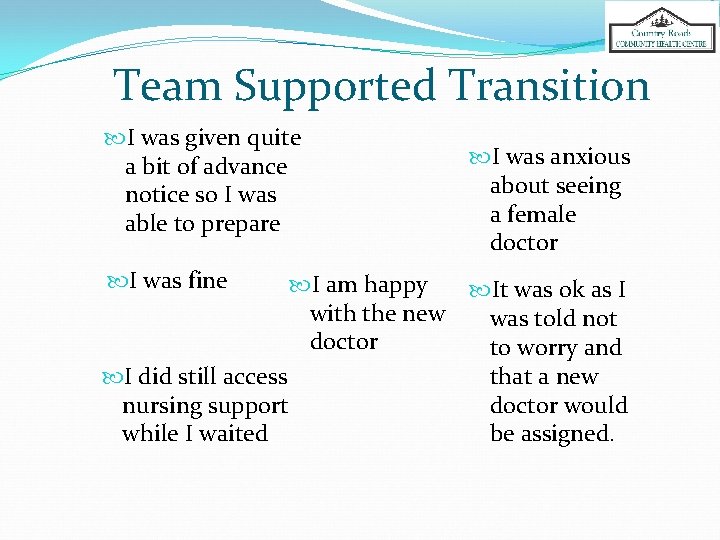
Team Supported Transition I was given quite a bit of advance notice so I was able to prepare I was fine I was anxious about seeing a female doctor I am happy It was ok as I with the new was told not doctor to worry and I did still access that a new nursing support doctor would while I waited be assigned.
What We Heard…. There should be a plan & provider responsibility that results in immediate access It should not be up to me to find another MD Planned assistance and direct help for patients Much better communication when providers retire
What We Heard cont’d…. The government should not let physicians decide on their own that they will not see a complex patient, there should be a process Someone needs to be in charge of making sure patients get service The MD on their own did not have the resource to figure out the solution, support from the system is needed!
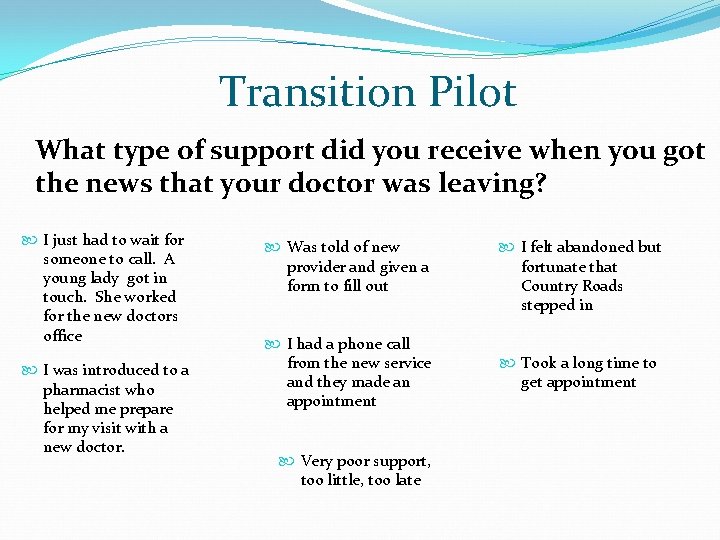
Transition Pilot
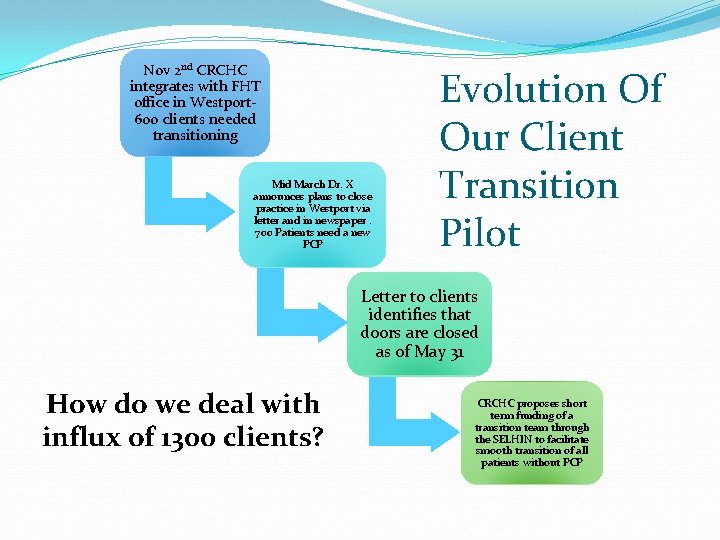
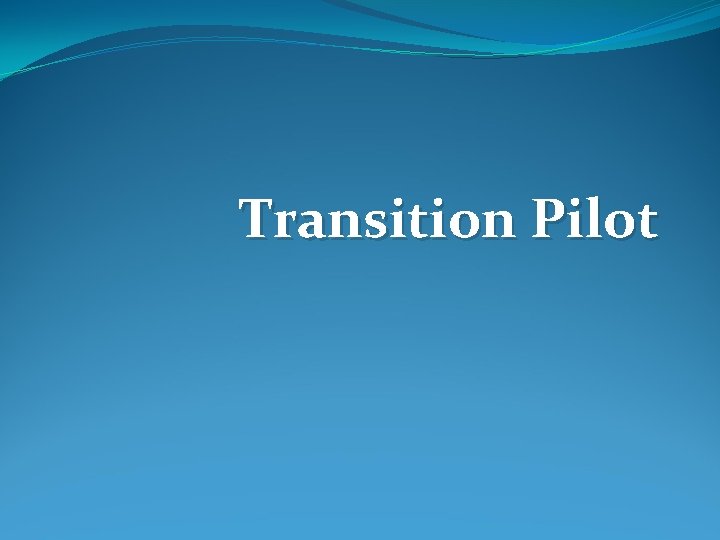
Nov 2 nd CRCHC integrates with FHT office in Westport 600 clients needed transitioning Mid March Dr. X announces plans to close practice in Westport via letter and in newspaper. 700 Patients need a new PCP Evolution Of Our Client Transition Pilot Letter to clients identifies that doors are closed as of May 31 How do we deal with influx of 1300 clients? CRCHC proposes short term funding of a transition team through the SELHIN to facilitate smooth transition of all patients without PCP
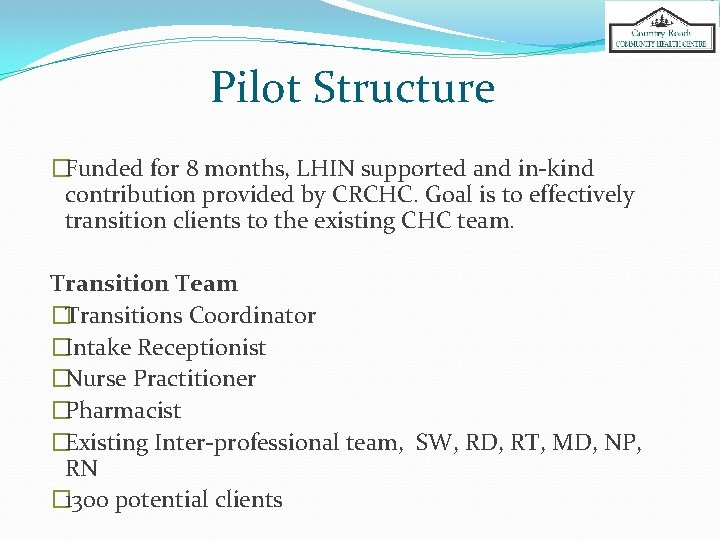
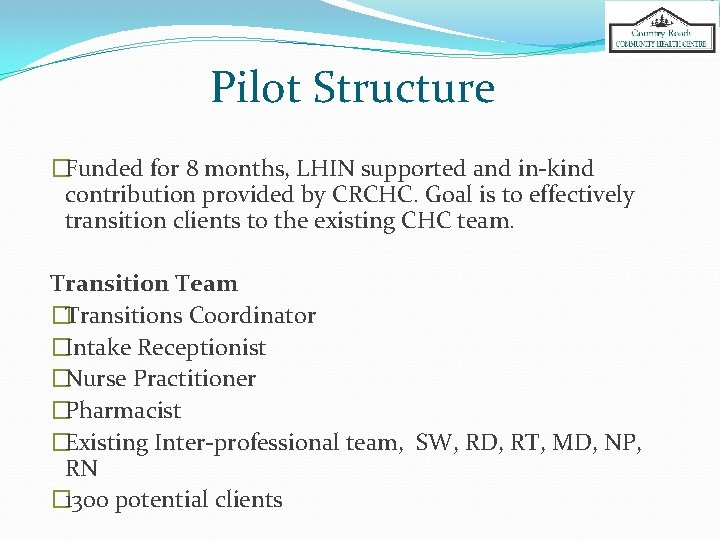
Pilot Structure �Funded for 8 months, LHIN supported and in-kind contribution provided by CRCHC. Goal is to effectively transition clients to the existing CHC team. Transition Team �Transitions Coordinator �Intake Receptionist �Nurse Practitioner �Pharmacist �Existing Inter-professional team, SW, RD, RT, MD, NP, RN � 1300 potential clients
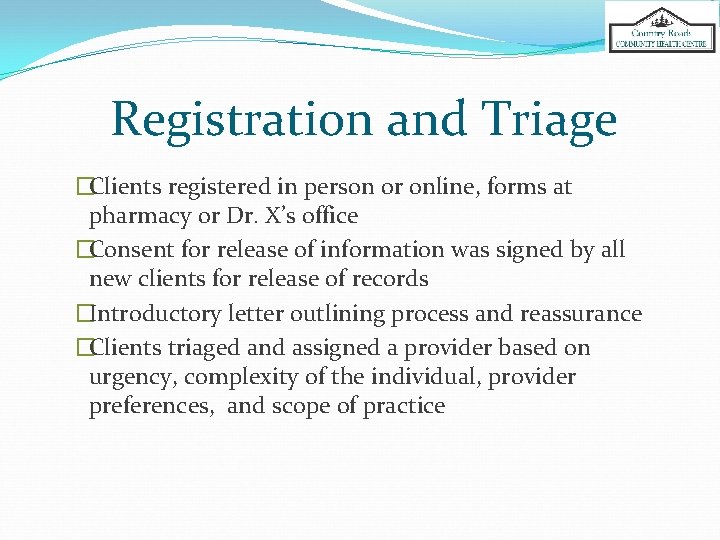
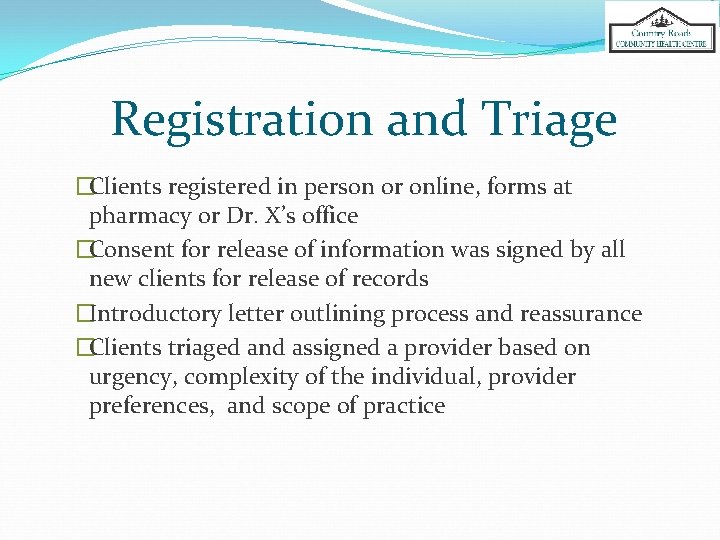
Registration and Triage �Clients registered in person or online, forms at pharmacy or Dr. X’s office �Consent for release of information was signed by all new clients for release of records �Introductory letter outlining process and reassurance �Clients triaged and assigned a provider based on urgency, complexity of the individual, provider preferences, and scope of practice
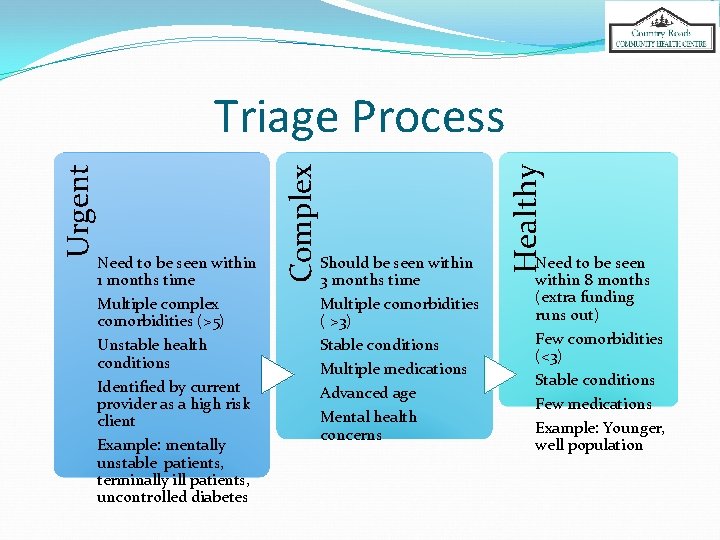
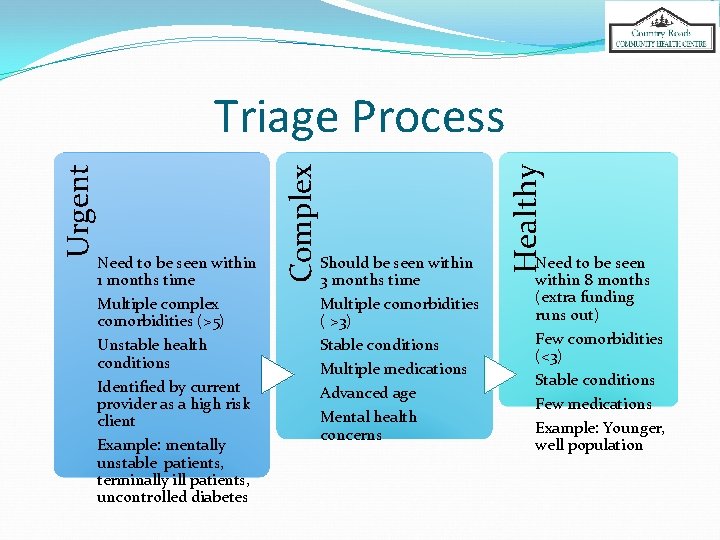
Should be seen within 3 months time Multiple comorbidities ( >3) Stable conditions Multiple medications Advanced age Mental health concerns Healthy Need to be seen within 1 months time Multiple complex comorbidities (>5) Unstable health conditions Identified by current provider as a high risk client Example: mentally unstable patients, terminally ill patients, uncontrolled diabetes Complex Urgent Triage Process Need to be seen within 8 months (extra funding runs out) Few comorbidities (<3) Stable conditions Few medications Example: Younger, well population
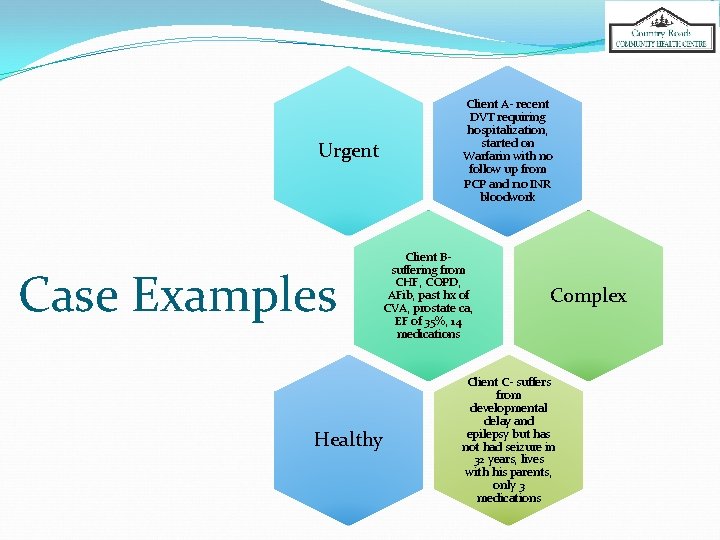
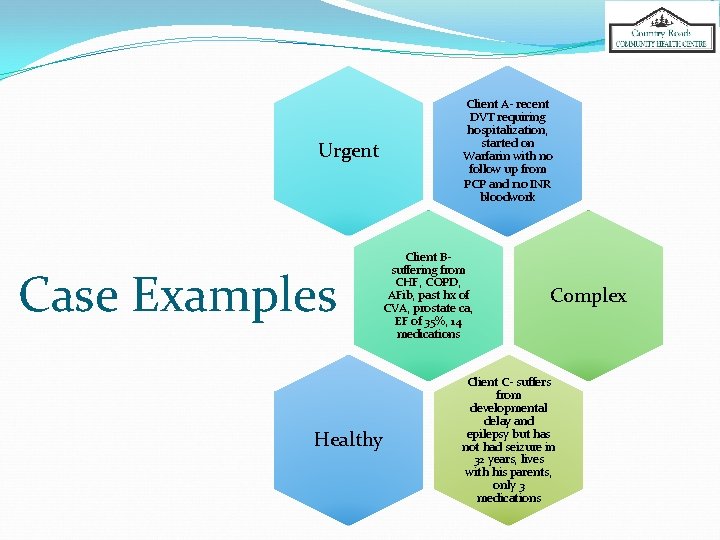
Urgent Case Examples Healthy Client A- recent DVT requiring hospitalization, started on Warfarin with no follow up from PCP and no INR bloodwork Client Bsuffering from CHF, COPD, AFib, past hx of CVA, prostate ca, EF of 35%, 14 medications Complex Client C- suffers from developmental delay and epilepsy but has not had seizure in 32 years, lives with his parents, only 3 medications
Content of Intake Interviews * Introduction to the CHC * Health Questionnaire * EHR Entry and Chart Review
Barriers to Transition Time and number of clients needing service Communication Access for existing clients Needs of new clients Lack of trust from new clients
Timelines How did we deal with lack of time? • ~600 clients need to be seen from Apr to Nov • Six 30 min. intake assessments per day starting in April by the Transition Coordinator How did we schedule appointments? Clients called in order of urgency and complexity for each assigned provider � Intake assessments completed prior to the Meet and Greet with the provider � Need for Meet and Greet appointment was determined during the intake assessment
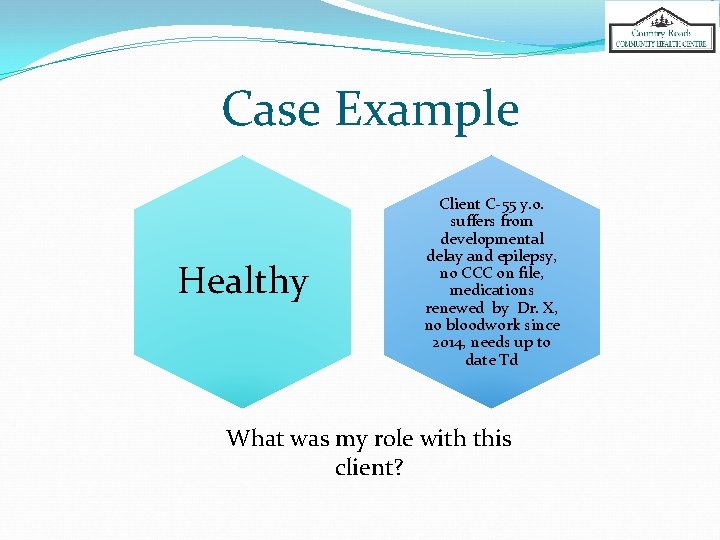
Case Example Healthy Client C-55 y. o. suffers from developmental delay and epilepsy, no CCC on file, medications renewed by Dr. X, no bloodwork since 2014, needs up to date Td What was my role with this client?
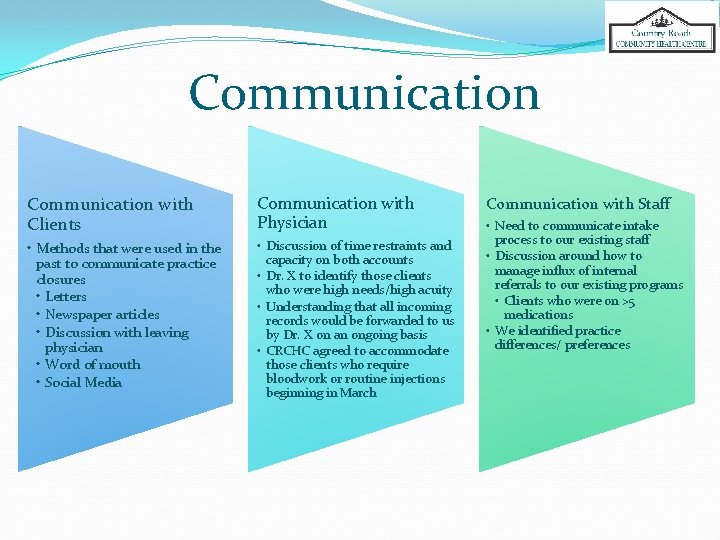
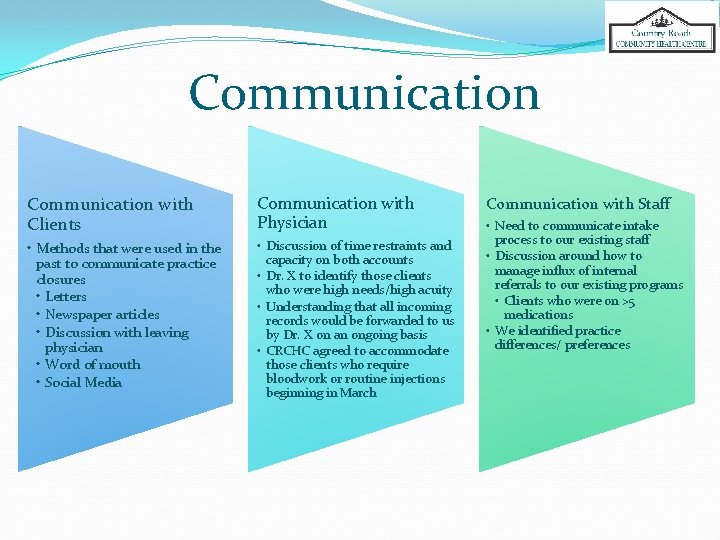
Communication with Clients Communication with Physician • Methods that were used in the past to communicate practice closures • Letters • Newspaper articles • Discussion with leaving physician • Word of mouth • Social Media • Discussion of time restraints and capacity on both accounts • Dr. X to identify those clients who were high needs/high acuity • Understanding that all incoming records would be forwarded to us by Dr. X on an ongoing basis • CRCHC agreed to accommodate those clients who require bloodwork or routine injections beginning in March Communication with Staff • Need to communicate intake process to our existing staff • Discussion around how to manage influx of internal referrals to our existing programs • Clients who were on >5 medications • We identified practice differences/ preferences
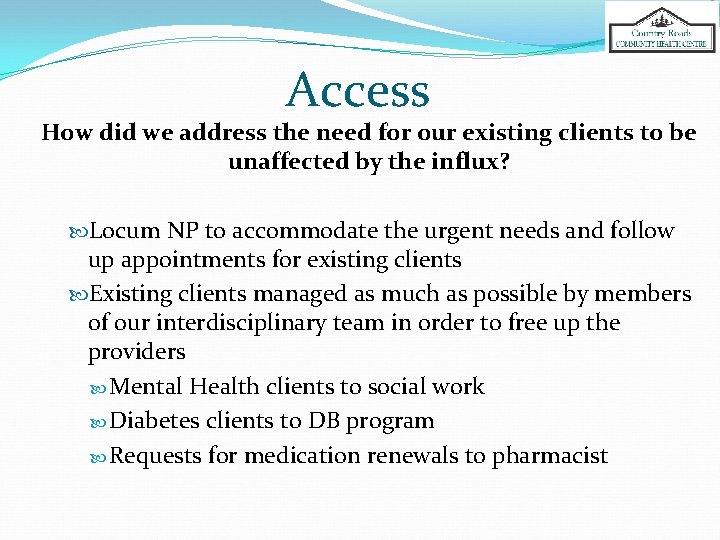
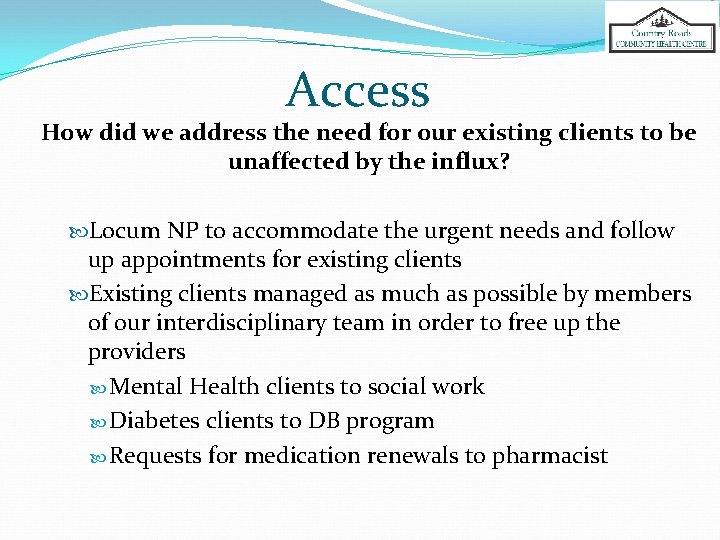
Access How did we address the need for our existing clients to be unaffected by the influx? Locum NP to accommodate the urgent needs and follow up appointments for existing clients Existing clients managed as much as possible by members of our interdisciplinary team in order to free up the providers Mental Health clients to social work Diabetes clients to DB program Requests for medication renewals to pharmacist
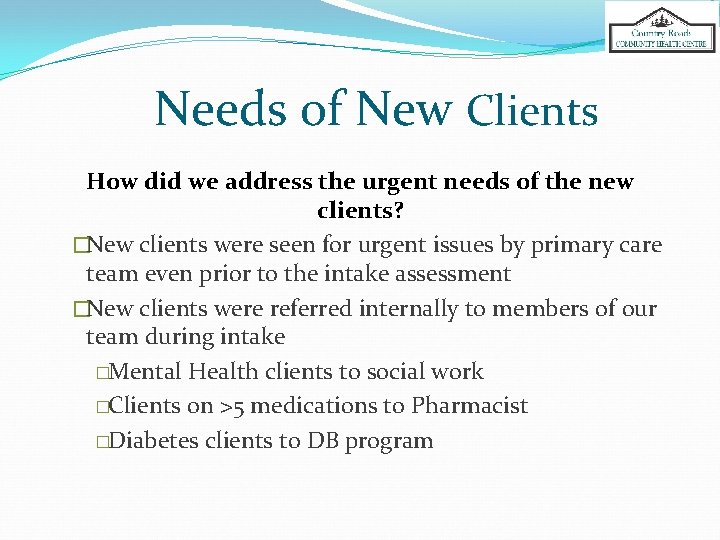
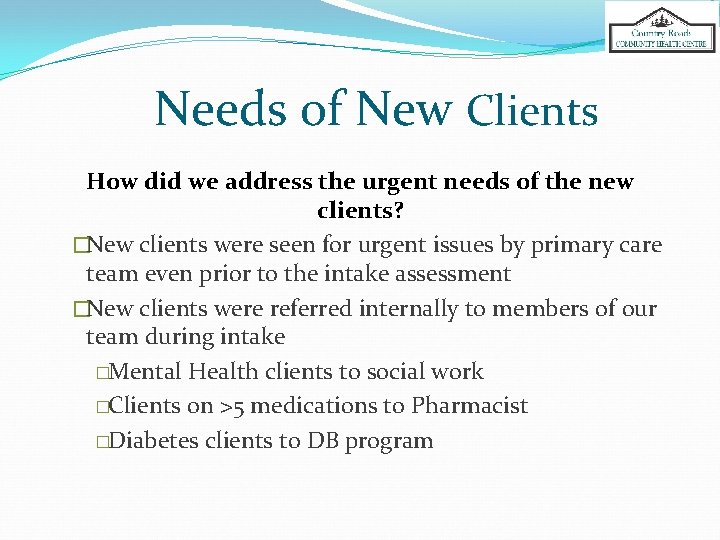
Needs of New Clients How did we address the urgent needs of the new clients? �New clients were seen for urgent issues by primary care team even prior to the intake assessment �New clients were referred internally to members of our team during intake �Mental Health clients to social work �Clients on >5 medications to Pharmacist �Diabetes clients to DB program
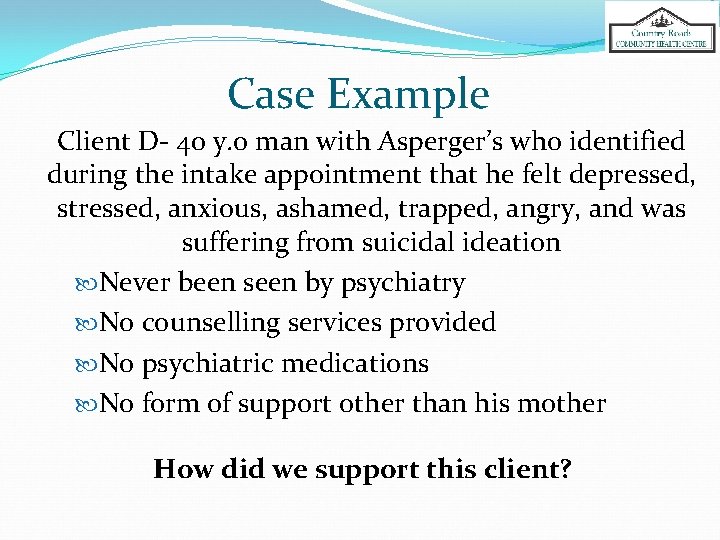
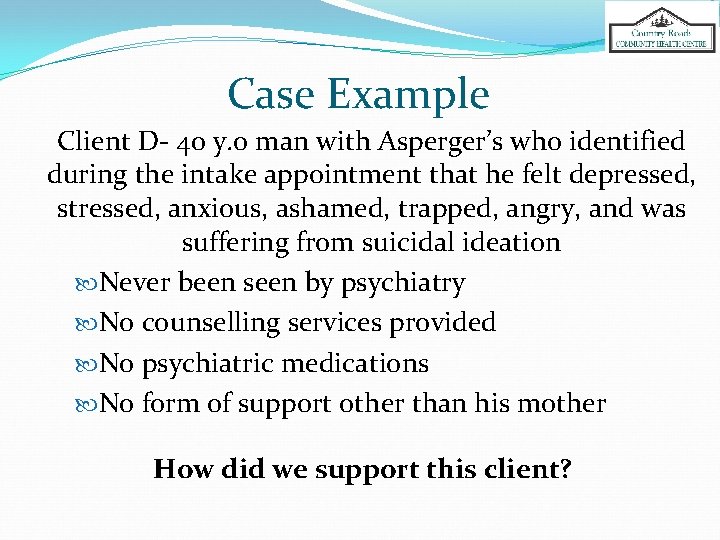
Case Example Client D- 40 y. o man with Asperger’s who identified during the intake appointment that he felt depressed, stressed, anxious, ashamed, trapped, angry, and was suffering from suicidal ideation Never been seen by psychiatry No counselling services provided No psychiatric medications No form of support other than his mother How did we support this client?
Trust How did we address the lack of trust? By addressing the issues as the client brought them up By identifying what is important to the client What is important to you? What are you worried about right now? Why is it important to ask these questions?
Case Example Client E- 50 y. o female with hypertension, bipolar disorder, and fibromyalgia. Biggest concern? Teeth! She reported constant taste of blood in her mouth, and teeth breaking off anytime she tries to eat something solid.
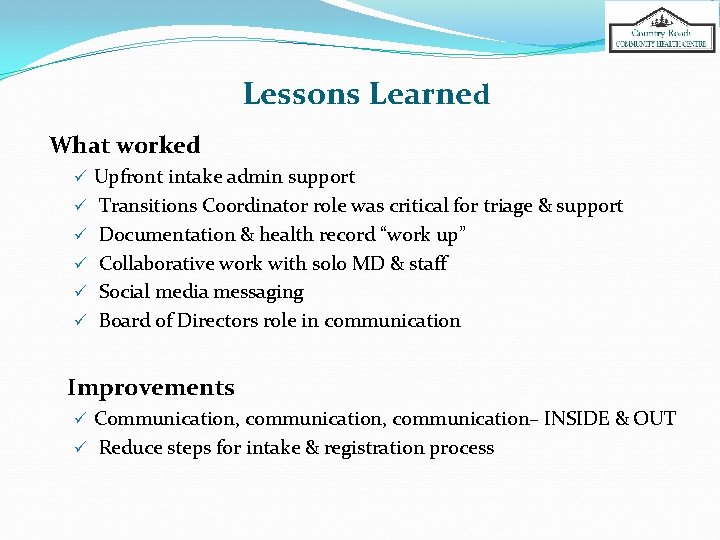
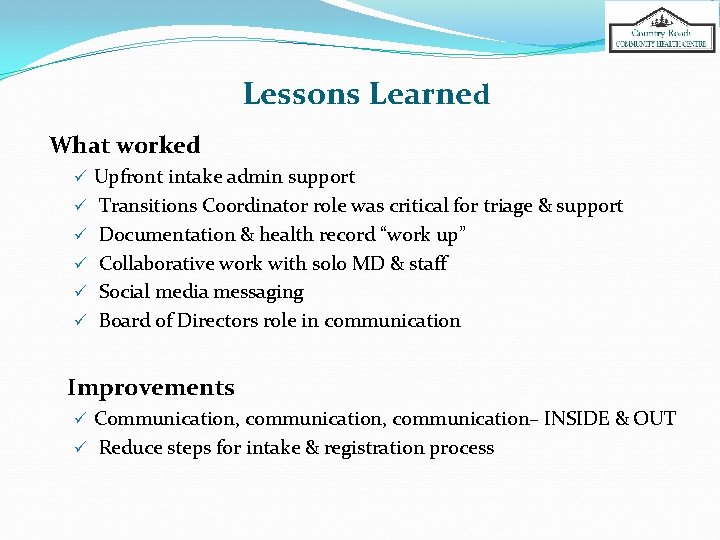
Lessons Learned What worked ü Upfront intake admin support ü Transitions Coordinator role was critical for triage & support ü Documentation & health record “work up” ü Collaborative work with solo MD & staff ü Social media messaging ü Board of Directors role in communication Improvements ü Communication, communication– INSIDE & OUT ü Reduce steps for intake & registration process

Transition Pilot Client Experience
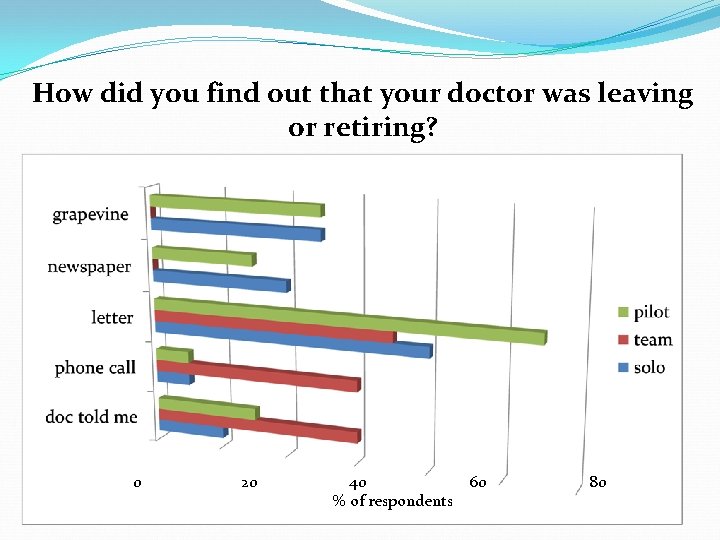
How did you find out that your doctor was leaving or retiring? 0 20 40 60 % of respondents 80
How did you feel when you first found out that your doctor was leaving or retiring? 0 1 2 3 4 5 ____________________________ Most Negative Least Negative Average Response to Scaling Questions
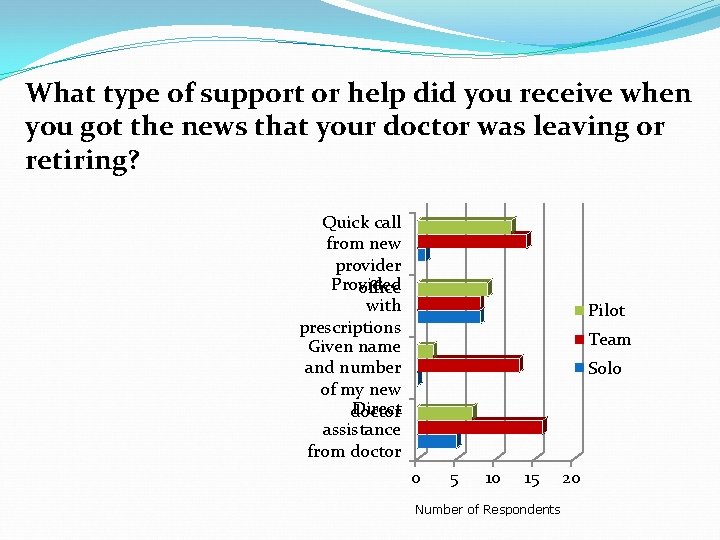
What type of support or help did you receive when you got the news that your doctor was leaving or retiring? Quick call from new provider Provided office with prescriptions Given name and number of my new Direct doctor assistance from doctor Pilot Team Solo 0 5 10 15 Number of Respondents 20
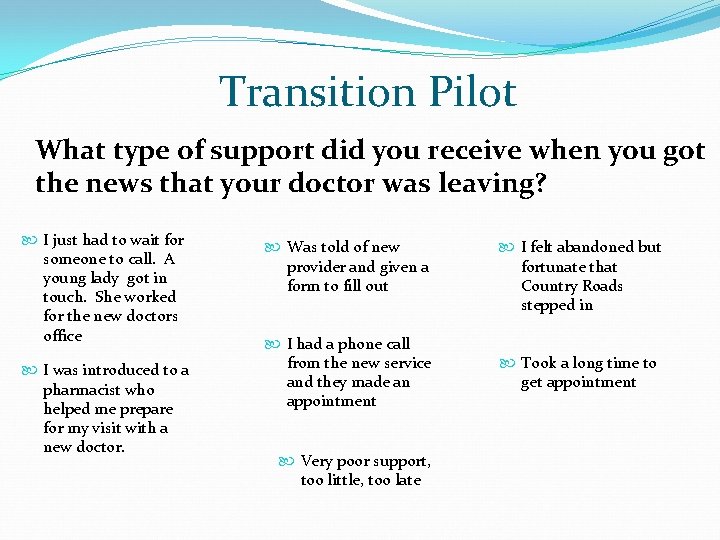
Transition Pilot What type of support did you receive when you got the news that your doctor was leaving? I just had to wait for someone to call. A young lady got in touch. She worked for the new doctors office I was introduced to a pharmacist who helped me prepare for my visit with a new doctor. Was told of new provider and given a f 0 rm to fill out I had a phone call from the new service and they made an appointment Very poor support, too little, too late I felt abandoned but fortunate that Country Roads stepped in Took a long time to get appointment
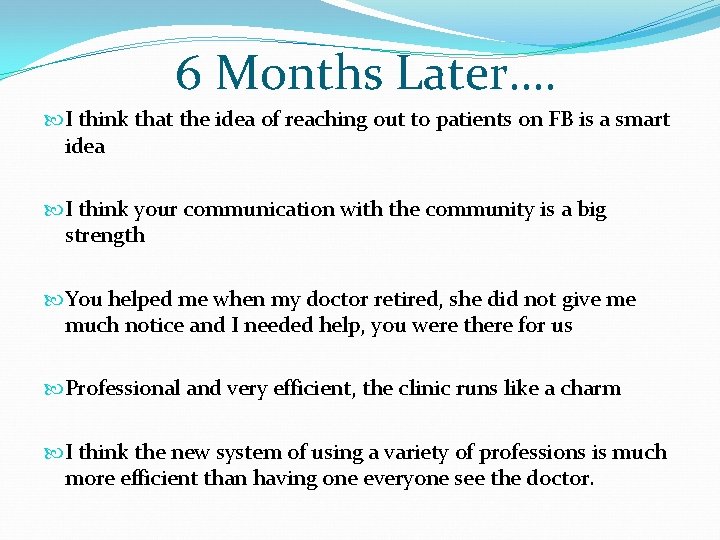
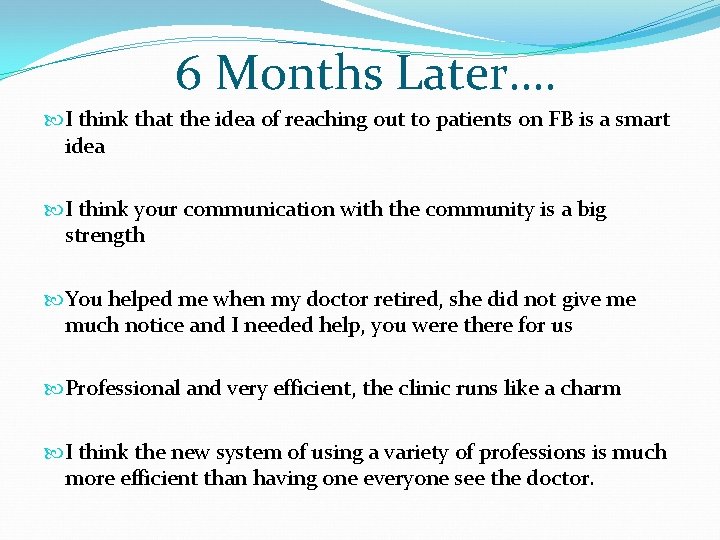
6 Months Later…. I think that the idea of reaching out to patients on FB is a smart idea I think your communication with the community is a big strength You helped me when my doctor retired, she did not give me much notice and I needed help, you were there for us Professional and very efficient, the clinic runs like a charm I think the new system of using a variety of professions is much more efficient than having one everyone see the doctor.
KEY ISSUE How do we move towards a health system that guarantees patients a smooth transition when their provider retires?
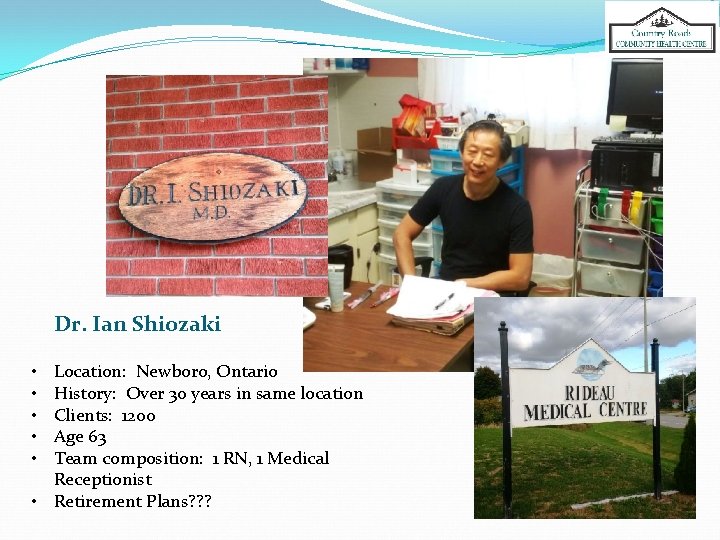
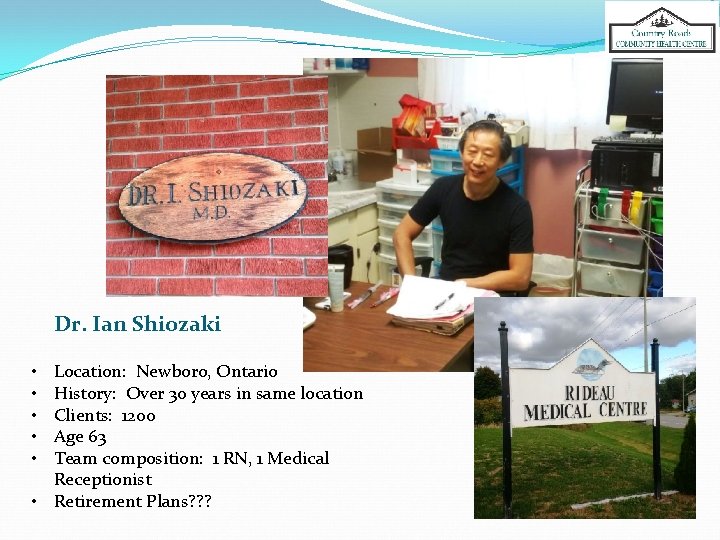
Dr. Ian Shiozaki Location: Newboro, Ontario History: Over 30 years in same location Clients: 1200 Age 63 Team composition: 1 RN, 1 Medical Receptionist • Retirement Plans? ? ? • • •
SHARED RESPONSIBILITY? ? Patient Provider System
 Open research funders group
Open research funders group Deliberative model of doctor-patient relationship
Deliberative model of doctor-patient relationship Early experience vs later experience debate
Early experience vs later experience debate Direct and indirect experience examples
Direct and indirect experience examples Imprinting meaning psychology
Imprinting meaning psychology Patient experience program
Patient experience program Caspa achievements examples
Caspa achievements examples Transforming patient experience
Transforming patient experience Why patient experience matters
Why patient experience matters Patient 2 patient
Patient 2 patient University of cincinnati physicians inc
University of cincinnati physicians inc Central washington hospital pharmacy
Central washington hospital pharmacy American college of private physicians
American college of private physicians Maryland physician health program
Maryland physician health program Jrcptb eportfolio
Jrcptb eportfolio Retaining millennial physicians
Retaining millennial physicians Kentucky physicians health foundation
Kentucky physicians health foundation Group 1 vs group 2 specialties
Group 1 vs group 2 specialties Jh community physicians
Jh community physicians University of cincinnati physicians inc
University of cincinnati physicians inc Gateway marketing inc
Gateway marketing inc Ghana physicians and surgeons foundation
Ghana physicians and surgeons foundation Primary care physician wellstar
Primary care physician wellstar Coalition for physician enhancement
Coalition for physician enhancement Elisha goodman prayer points for breakthrough
Elisha goodman prayer points for breakthrough A physician claims that joggers maximum volume
A physician claims that joggers maximum volume Daniel stok
Daniel stok Ohio association of physician assistants
Ohio association of physician assistants Physician time study
Physician time study Physician mohh
Physician mohh Designated civil surgeon locator
Designated civil surgeon locator Physician burnout retreat
Physician burnout retreat A physician claims that joggers maximum volume
A physician claims that joggers maximum volume Physician recruitment onboarding and retention
Physician recruitment onboarding and retention Pa ieb physician certification form
Pa ieb physician certification form Family medicine fellowship
Family medicine fellowship Physician associate lecturer
Physician associate lecturer Advanced hcp targeting
Advanced hcp targeting Computerized physician order entry definition
Computerized physician order entry definition The good physician treats the disease
The good physician treats the disease Physician employment models
Physician employment models Physician reentry programs
Physician reentry programs Cphp
Cphp University of new england physician assistant program
University of new england physician assistant program Physician sign out
Physician sign out Physician competency reference set
Physician competency reference set Oklahoma board of nursing lpn scope of practice
Oklahoma board of nursing lpn scope of practice Stanford physician wellness survey
Stanford physician wellness survey Sachin khullar
Sachin khullar Physician consortium for performance improvement
Physician consortium for performance improvement Physician wellness academic consortium
Physician wellness academic consortium Physician personas
Physician personas Retirement plan limerick
Retirement plan limerick Ucf retirement plan
Ucf retirement plan Tcg retirement
Tcg retirement Shakespeare lived almost entirely during the reign of
Shakespeare lived almost entirely during the reign of Fresno county employees retirement association
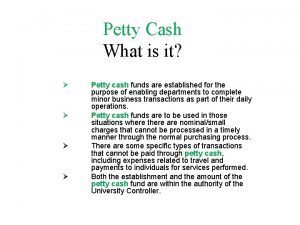
Fresno county employees retirement association Petty cash retirement
Petty cash retirement Caltech retiree benefits
Caltech retiree benefits