Physician Retraining and Reentry Programs Ethics Seminar June







- Slides: 54

Physician Retraining and Reentry Programs Ethics Seminar June 12, 2010 at Round Rock, TX Anita R. Webb, Ph. D Joane G. Baumer, MD JPS Family Medicine, Fort Worth Roy S. Martin, D. Min, UNT-HSC, Fort Worth
Goals and Objectives n n n n Explain the need for retraining programs. Discuss physician “impairment”. Describe AMA’s position on retraining/reentry. Review some existing reentry programs. Describe the JPS reentry curriculum. Review reentry physician behavioral issues. Discuss ethical issues.
Key Points n n Physicians with extended practice interruptions have few options to resume clinical practice. Extended interruptions raise important ethical issues about the physician-patient relationship. The AMA supports the need for retraining and reentry programs. A limited number of programs are offered.
The Need: Physician Shortage n n n Expected to worsen, multiple factors. Midlevel clinicians are not filling all the gaps. Returning dormant physicians to practice will benefit the community. Faster, cheaper than training new physicians. Experienced physicians have more insight.
The Problem: Stressful Profession n High patient-to-physician ratio n n Running a “business” n n Time pressures in clinical environment Increasing costs, decreasing compensation Nonproductive encounters with patients, staff, colleagues, administrators. . . 75% of physicians are moving to employed positions Public demands and expectations
Stressors: On the Job n n n n Fractured healthcare environment in U. S. Eroding public image of physicians Eroding doctor-patient relationships, with payers driving doctor hopping Increasing government regulations, paperwork Loss of control over practice, income, time… Litigious society: Malpractice fears Isolated practice: No professional support system post-training
Stressors: Personal n n n n High achievers, high personal expectations Perfectionists, expect to be less vulnerable Need for control Exaggerated sense of responsibility Difficulty asking for help Workaholic: No fun, no vacations, etc. Conflicting roles and responsibilities

High Risk for Problems Burnout n Stress-related illness n Family problems n Depression n Suicide n Substance abuse n
“Problem Doctors” n “Physician performance failures are not rare, and pose substantial threats to patient welfare and safety. ” n Leape LL, Fromson JA. Problem doctors: Is there a system-level solution? Ann Intern Med 2006; 144: 107 -115.
Result: Practice Interruptions Personal medical problems, illness n Family responsibilities: e. g. childrearing, caretaking for ill parents n Transition to a non-clinical medical position (e. g. administrative) n Mistakes, sanctions, loss of privileges n “Impairment” n
Returning to Practice Previously, it was customary to enlist a colleague for informal proctoring. n However, this process is no longer acceptable to licensing bodies. n Formal Reentry/Retraining Programs n n n International movement But major barriers to initiating these programs
Re-Entry Barriers Concerns about erosion of competence n Expired medical license n May be difficult for dormant physician to “catch up” after extended interruption. n No formal mechanism to repatriate the physician. n How to help the “impaired” physician? n
“Impaired Physician”: Definition n n “A physician who is unable to practice medicine “With reasonable skill and safety to patients “Because of physical or mental illness, “Including deterioration through the aging process or loss of motor skill, or “Excessive use or abuse of drugs including alcohol. ” n American College of Emergency Physicians
Impairment: Substance Abuse n Substance abuse is leading impairment cause. n n Physicians do well in recovery programs. n n More favorable outcomes than general population American with Disabilities Act (1990) n n 10% prevalence: But only 1 -2 % recognized Cannot discriminate against impaired physician Requires changing the “punitive culture” of medicine.
Treatment versus Punishment n Movement toward treatment n n n Encourage self-reporting, treatment, and earlier return-to-work. Specialist treatment facilities for physicians Why are family physicians over-represented among impaired physicians? n E. g. solo practice/isolation
Joint Commission on Accreditation of Hospitals Effective 2001 n Hospitals must identify and manage physician impairment, and demonstrate how impaired physicians are monitored. n Physician Well-Being Committees n Mandatory for all hospital medical staffs n For health and behavioral problems n
Physician Health Programs (PHP) n Every state has some type of physician assistance program. Example: n n 1978 Tennessee Medical Foundation: substance abuse, depression, psychosexual disorder, etc. 98% with substance use disorder achieve “persistent recovery”, able to return to practice Also assistance program for the families International movement
Example: Spain Medical College of Barcelona: 1999 n “Psychiatric disorders” and “drug addiction” n Treatment team: three psychiatrists, two psychologists, one internist, nurses n n n Therapeutic contract Identity is disguised. n Lives at unmarked center during treatment.
Spain (continued) “High quality” center: 10 “single” rooms, library, computers, leisure facilities n Medical conferences, skills retraining, personal tutor n Free for local physicians n n Funded by Health Dept. Financial compensation: Physician & family (Bosch. JAMA. 2000; 283(24): 3186 -3187)
Problem Doctors: Research Disciplinary action by a medical board n Was strongly associated with prior n Unprofessional behavior in medical school. n n Papadakis MA, Teherani A, Banach MA et al. Disciplinary Action by Medical Boards and Prior Behavior in Medical School. New England Journal of Med 2005; 353: 2673 -2682.

Remediation? n n Apparently, neither medical school nor residency training resolved the problem of unprofessional behavior for these delinquent medical students. What kind of remediation or educational intervention should be instituted? n In medical school? n In residency? n After residency?
Post-Residency: “Retraining” Physicians who were either interrupted or disciplined can get a second chance to practice via reentry programs. n An international movement to retrain physicians has spawned a number of reentry programs in the U. S. n
Example: Syracuse, New York n n n “Physician Prescribed Educational Program” n Launched 1992 within FMRP n Target: “lapsed knowledge and skills” Accepts only physicians with “educationally remedial deficits” Excludes: substance abuse, sexual violations, psychiatric diagnosis, or judicially mandated
Example: Tennessee 1999 Vanderbilt University Medical Center n “The Center for Professional Health” n “Program for Distressed Physicians” n 46. 5 hours CME n 3 days + 3 follow-up group sessions n
Vanderbilt (cont. ) Didactics, role-play, feedback, testing, “group accountability: n Excluded: Ongoing psychiatric, substance abuse, sexual addiction n $3500 + $1500 workplace assessment + fee for psychological assessment n
REENTRY PROGRAMS Three reentry programs in U. S. n Oregon n Pennsylvania n Texas n (Soon: Wisconsin) n
Example: Oregon Health/Science University n 2006 Portland n 2 -3 month individualized fellowship n $2500 - $8000/month n Accepts only Oregon physicians “in good standing” n 12 physicians per year n
Example: Pennsylvania 2006 Drexel University, Philadelphia n Six-week internal medicine preceptorship n Added ob-gyn, surgery, pediatrics n Average: $7500 n

Coalition for Physician Enhancement: CPE n n n “A consortium of professionals with expertise in “Quality assurance, medical education, and “The assessment, licensing, and accreditation of “Referred physicians seeking higher levels “Of performance in patient care. ” n North America n www. physicianenhancement. org
CPE: Mission Statement “To support and develop expertise n “In assessment and enhancement n “When competence and/or performance n “Are to be assessed. ” n Six members that offer retraining n n California, Colorado, New York, Texas, Toronto (Canada) and Wisconsin
CPE Members n n n New York: Albany Medical College Denver: Center for Personalized Education for Physicians Toronto, Canada: Clinician Assessment and Professional Enhancement University of California at San Diego University of Wisconsin School of Medicine JPS/Texas A&M University partnership
Example: Texas n n n Newest re-entry program: 2008 Application and assessment through KSTAR at Texas A&M University n Extensive, intensive assessment Re-training at JPS in Fort Worth n n Twelve-week structured program Based on the six ACGME Competencies
KSTAR: Assessing Physicians Capacity: Physical, cognitive, “personality” n Motivation: Why return to practice? n “Distractors”: e. g. marital, substance abuse n Alienation from medical community n Disruptive behavior n Organizational skills n Emotional intelligence n

JPS Reentry Program n n Referral: TMB, hospital, lawyer, self Three full sessions to date plus two physicians who attended solo = 20 physicians 16 physicians graduated to date Preferable to enroll as small groups (3 - 5) n n Enhances professionalism discussions Functions as de facto support group
Medical Specialties Family Med (6) n Surgery (3) n OB/Gyn (3) n Internal Medicine (5) n Anesthesiology n Emergency Medicine n Physicians from Texas, Ohio, California n
“Mini-Residency” Curriculum n n n Weekly activities n Clinical: Five half-days with preceptor (a. m. ) n Redacted chart review group session n Behavioral Science group n Noon conference daily with residents n Didactic modules on computer Procedure Log Individual QI Project
Performance Evaluation n 360 degree evaluations at end of program n n By preceptor, nurse(s), and patients (N=10) Brief 10 -item Likert scale surveys Limitation: No “pre-test” scores for comparison n Approved by JPS Internal Review Board n

Potential Pitfalls n n Enforcement of curriculum requirements n Example: Physician who missed most of the Behavioral sessions, delaying graduation Difficulties with credentialing Board ordered participants Lack of longitudinal data to evaluate program n Graduates are not returning follow-up questionnaires
Successes: Employment n n Some physicians retained their practice or nonclinical employment during retraining. Most of the physicians found positions prior to finishing the reentry program. n Variety of medical settings: clinic, inpatient, military, urgent care, locum tenums n Two were hired by JPS: Win/win n Five resumed current positions
Reasons for Leaving Practice n n n Life stress: “I ran away. ” n One physician left practice, spouse, country n One traveled U. S. in RV with family: Jobless Early retirement: “It wasn’t fun any more. ” Stressful hospital environment Lost license due to substance abuse Lost license due to bipolar disorder Disruptive behavior, terminated from residency

Professionalism/Ethics n Physician’s commitment to the patient? n n Is there a “Commitment Boundary”? n n Physician’s oath is similar to clergy’s vow. Unspoken, unacknowledged, unaddressed Violation of physician-patient relationship?
Abandonment? n “I felt compelled to leave practice. ” How do physicians reach drastic dead end? n What alternatives were considered? Did they seek assistance, advice, counseling? Did they perceive departure as abandonment? n n n
RESEARCH n n n Survey of Arizona physicians N=13, 215 licensed physicians in state 604 returned to practice 2003 -2006 n n 4. 6% of all licensees: “Much more than expected” 45 changed specialties: 37 left obstetrics n n n Mary Rimsza MD, Medical Director Center of Health Information and Research Arizona State University in Tempe
Research (continued) n Reentry n n barriers 22 physician organizations formed a national working group in 2006 to examine barriers The AMA in collaboration with multiple associations studied reentry. n Issued a report in 2008.
AMA Report “Physician Reentry to Practice: Data to Guide Program Development” n Ten recommendations n Including: “Make physician career paths more flexible” n n (12/01/09)
DEFINITIONS n REENTRY n n Return to clinical practice following extended period of clinical inactivity not resulting from discipline or impairment RETRAINING n Updating one’s skills or learning new skills to move into a new clinical area
Two AMA National Surveys n n n Survey #1: n Sent to 68 state boards of medicine n Re: reentry regulations Survey #2: n Sent to 10 reentry program directors. n Re: requirements, participant demographics, cost, etc. Reports available at www. ama-assn. org
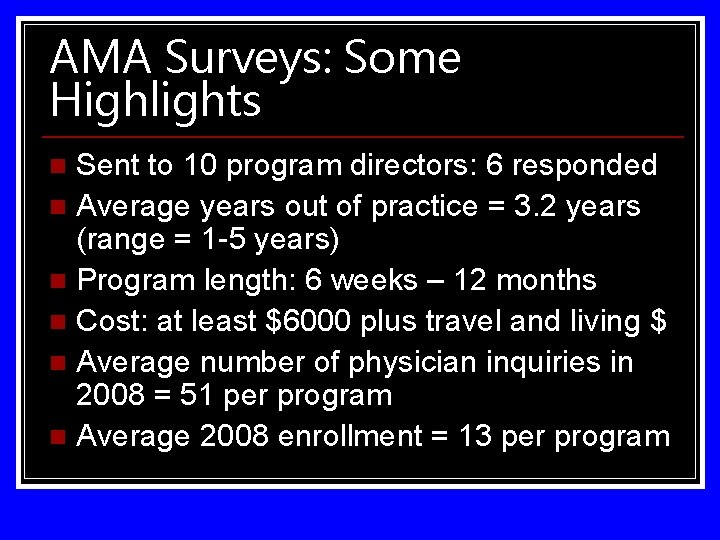
AMA Surveys: Some Highlights Sent to 10 program directors: 6 responded n Average years out of practice = 3. 2 years (range = 1 -5 years) n Program length: 6 weeks – 12 months n Cost: at least $6000 plus travel and living $ n Average number of physician inquiries in 2008 = 51 per program n Average 2008 enrollment = 13 per program n
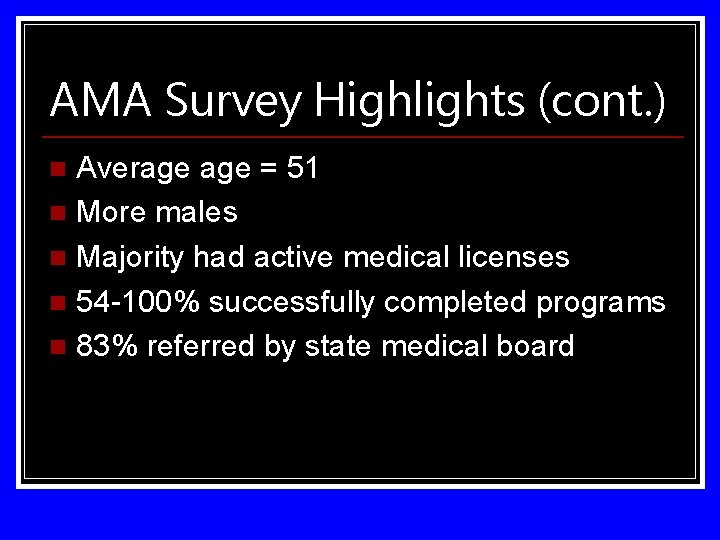
AMA Survey Highlights (cont. ) Average = 51 n More males n Majority had active medical licenses n 54 -100% successfully completed programs n 83% referred by state medical board n
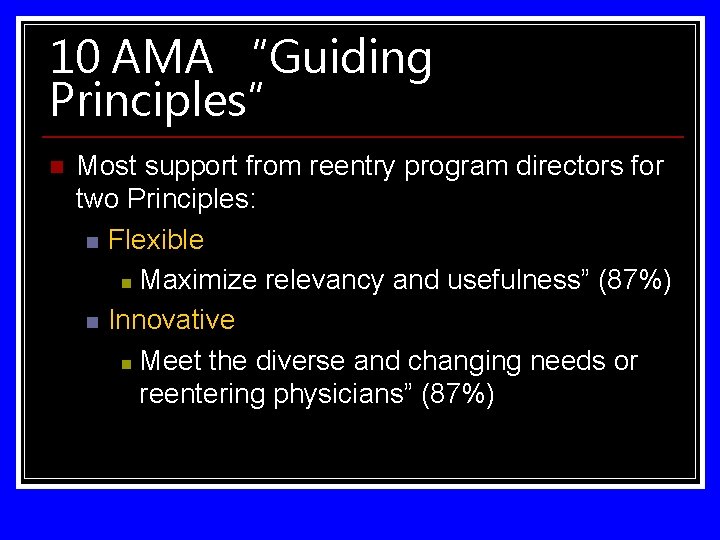
10 AMA “Guiding Principles” n Most support from reentry program directors for two Principles: n Flexible n Maximize relevancy and usefulness” (87%) n Innovative n Meet the diverse and changing needs or reentering physicians” (87%)
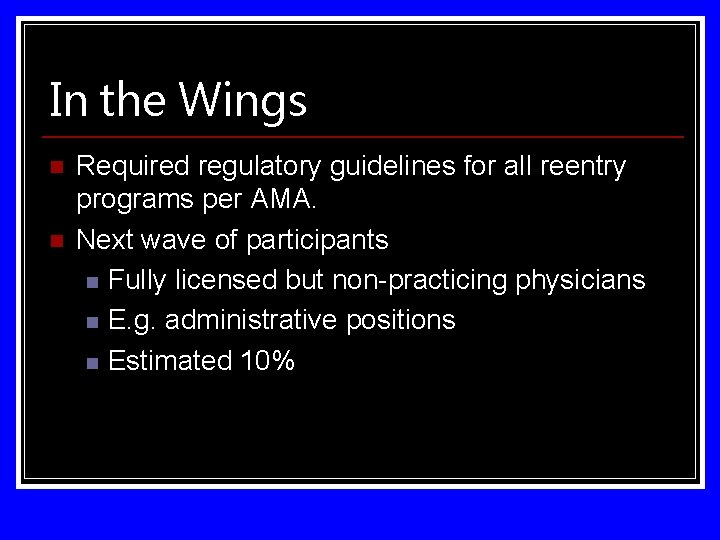
In the Wings n n Required regulatory guidelines for all reentry programs per AMA. Next wave of participants n Fully licensed but non-practicing physicians n E. g. administrative positions n Estimated 10%
Summary Reentry programs serve a function for physicians and for society. n Intensive screening assessment is required by some programs. n Programs can be as brief as 46. 5 hours. n Reentry programs in U. S. are costly. n
Key Points n n Physicians who experience extended practice interruptions have few options to resume clinical practice. Extended interruptions raise important ethical issues about the physician-patient relationship. The AMA supports the need for retraining and reentry programs. A limited number of programs are offered.
THE END Thank You! jbaumer@jpshealth. org awebb@jpshealth. org Roy. Martin@unthsc. org