Johns Hopkins Community Physicians Presentation to MCMS October
Johns Hopkins Community Physicians Presentation to MCMS October 25, 2012 Presented by: Matt Poffenroth, MD, MBA Director of Clinical Integration, JHCP 1
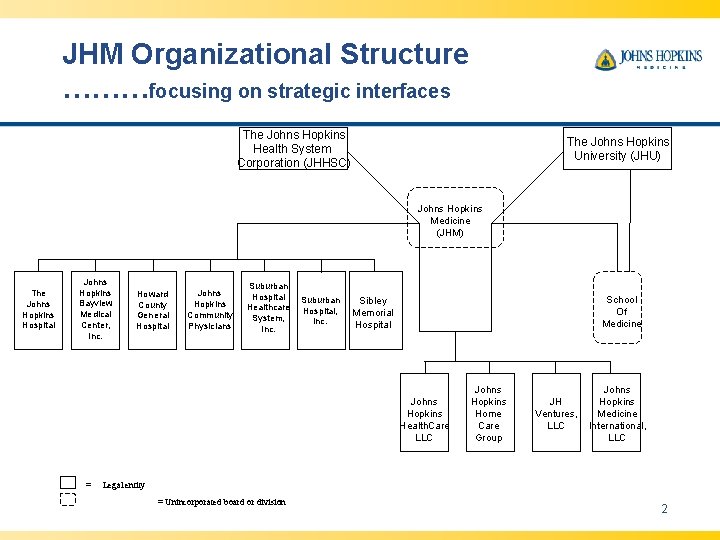
JHM Organizational Structure ………focusing on strategic interfaces The Johns Hopkins Health System Corporation (JHHSC) The Johns Hopkins University (JHU) Johns Hopkins Medicine (JHM) The Johns Hopkins Hospital Johns Hopkins Bayview Medical Center, Inc. Howard County General Hospital Johns Hopkins Community Physicians Suburban Hospital Healthcare System, Inc. Suburban Hospital, Inc. School Of Medicine Sibley Memorial Hospital Johns Hopkins Health. Care LLC = Johns Hopkins Home Care Group JH Ventures, LLC Johns Hopkins Medicine International, LLC Legal entity = Unincorporated board or division 2
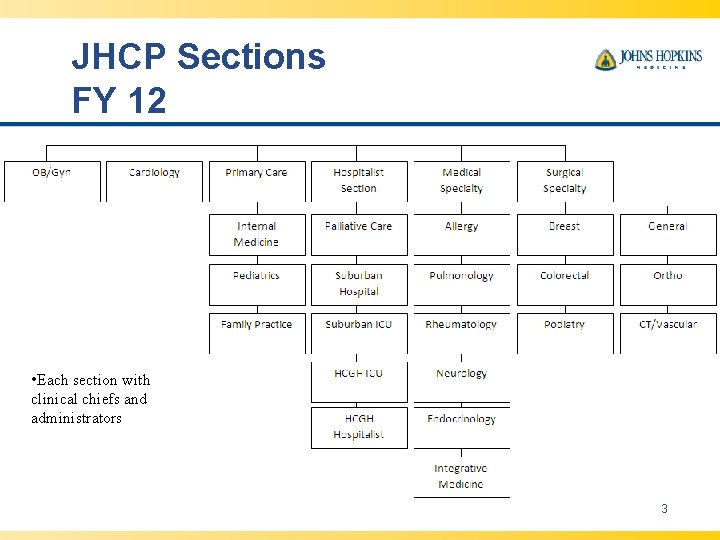
JHCP Sections FY 12 • Each section with clinical chiefs and administrators 3
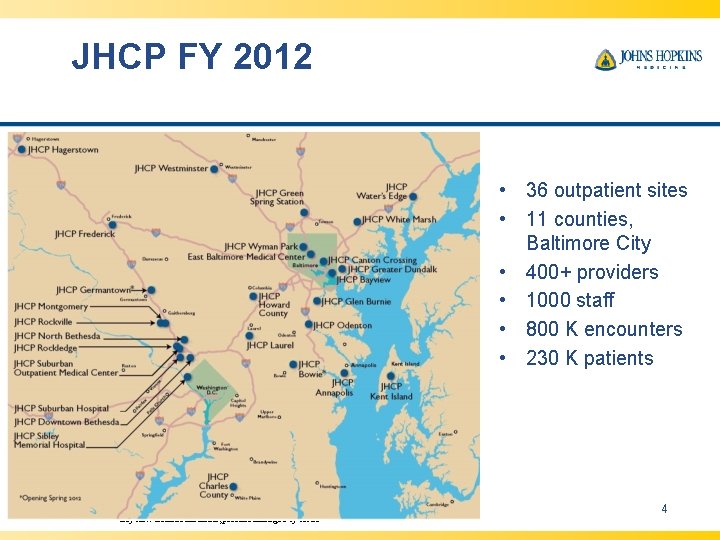
JHCP FY 2012 • 36 outpatient sites • 11 counties, Baltimore City • 400+ providers • 1000 staff • 800 K encounters • 230 K patients ** Bayview Internal Medicine, practice managed by JHCP 4
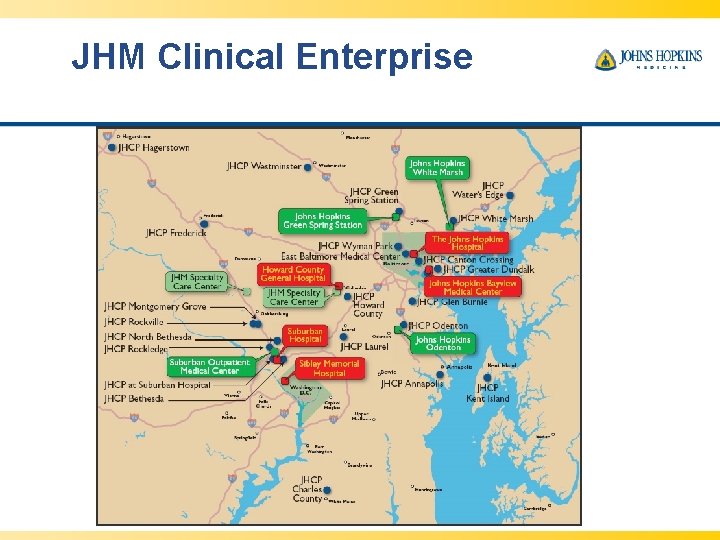
JHM Clinical Enterprise
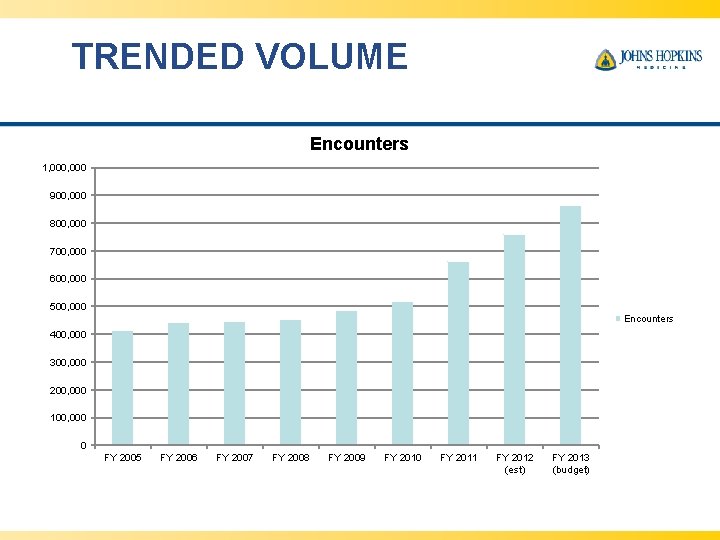
TRENDED VOLUME Encounters 1, 000 900, 000 800, 000 700, 000 600, 000 500, 000 Encounters 400, 000 300, 000 200, 000 100, 000 0 FY 2005 FY 2006 FY 2007 FY 2008 FY 2009 FY 2010 FY 2011 FY 2012 (est) FY 2013 (budget)
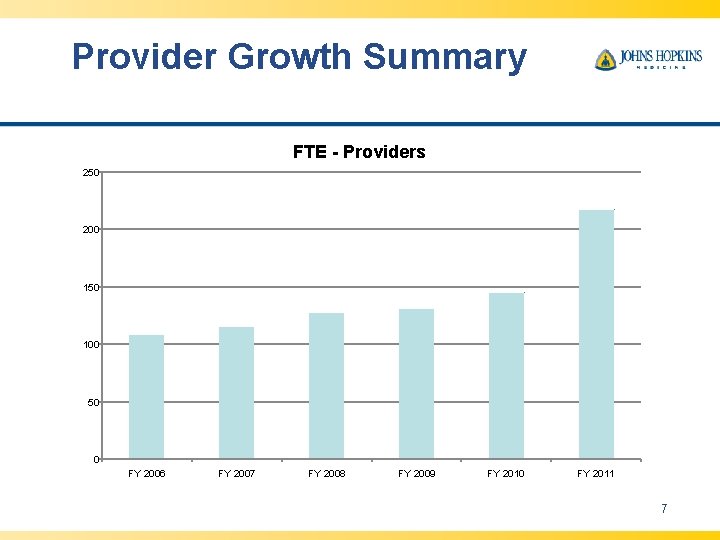
Provider Growth Summary FTE - Providers 250 200 150 100 50 0 FY 2006 FY 2007 FY 2008 FY 2009 FY 2010 FY 2011 7
JHCP Challenges In many ways, similar to private practice: • Insure access to growing volume of patients • Coordinate care for patients in a fragmented delivery system • Meet demands of payers to measure and report data • How to position ourselves for payment reform • Physician work: life balance 8
How is JHCP meeting these challenges? • Strategically adding capacity, based on access needs • Partnering with other private practice physicians in the community • New models of care – PCMH, extended hours, etc. • Participating with various P 4 P programs • Implementing EPIC in April, 2013 • Evaluating physician compensation model 9
Pay for Performance Programs at JHCP • Value Based Purchasing (JHHC) • Meaningful Use of EHR’s • Patient Centered Medical Home (PCMH) – Maryland Multi-Payer Pilot (MMPP)- 5 sites – Care. First – USFHP • ACO-prepared • PQRS • e. Prescribing • Maryland State-Regulated Payer EHR Adoption Incentive Program 10
Future of healthcare in Maryland • Payment reform is happening – providers increasingly will be asked to take risk • Quality and transparency is be demanded by payers and patients • Shift towards population health management • Uncertainty about HSCRC waiver and how this could affect providers 11
How will the system respond? • Continued and accelerated consolidation – Physicians increasingly seeking “safe haven” of employment – Hospitals increasingly reliant on physicians to meet access and quality needs – Bundled payments, shared savings programs, etc. • Alignment of incentives between providers, patients, payers and purchasers (is this a dream? ) 12
JHM Strategic Response • Developing an integrated delivery system is one of JHM’s Mission Imperatives • Alignment with private physicians is a JHM priority to achieve clinical integration • Strategies include: 1. 2. 3. 4. Employment Shared EHR Accountable Care Organizations Other 13
Employment • Typically not “purchasing” practices • Not always an appealing option for either side – Financial risk – Culture • Requires a shared Mission and Vision 14
Shared EHR • JHM begins transitioning to EPIC in April 2013, beginning with our ambulatory practices • JH Community Division to offer EPIC Community Connect to private practices • Full EHR and practice management system, without billing module • Marketing to begin late fall 2012, implementation fall 2013 15
ACOs • CMMI grant approval for J-CHi. P in June 2012 – “academic ACO” • Exploring community ACO model with intent to file letter of intent by June 2013 with implementation January 2014 • Success (i. e. improved quality at lower cost) will require: – Infrastructure – Resources – Expertise in population health management • Not all “ACOs” will succeed 16
Other methods to enhance alignment • • Improved access to JH clinics Part-time faculty appointments CME Shared purchasing agreements Networking with JH health plans MSO services “True” clinical integration model with shared contracting 17
Questions? Matt Poffenroth, MD, MBA mpoffen 1@jhmi. edu 240 -235 -9130 18
- Slides: 18