Pathogenesis and treatment of joint pain Aims Origins





- Slides: 33
Pathogenesis and treatment of joint pain
Aims • Origins of joint pain – inflammation tissue damage central mechanisms • Major rheumatic conditions • Autoimmune • crystal-related • Crystal arthropathies • Fibromyalgia • Therapeutic options and mechanisms of action • Analgesia (simple, NSAIDs) • Disease modifying (MTX, biologicals) • Corticosteroids
Therapeutic aims ↓ Pain ↓ Stiffness ↓ progressive joint damage ? Repair joint damage Maintain functional capacity and quality of life
Origin of joint pain; inflammatory or non-inflammatory? Inflammatory: redness, heat, pain, swelling and loss of function Symptoms worse in morning Eased by exercise Non-inflammatory: bone and cartilage damage Worse in evening Exacerbated by use
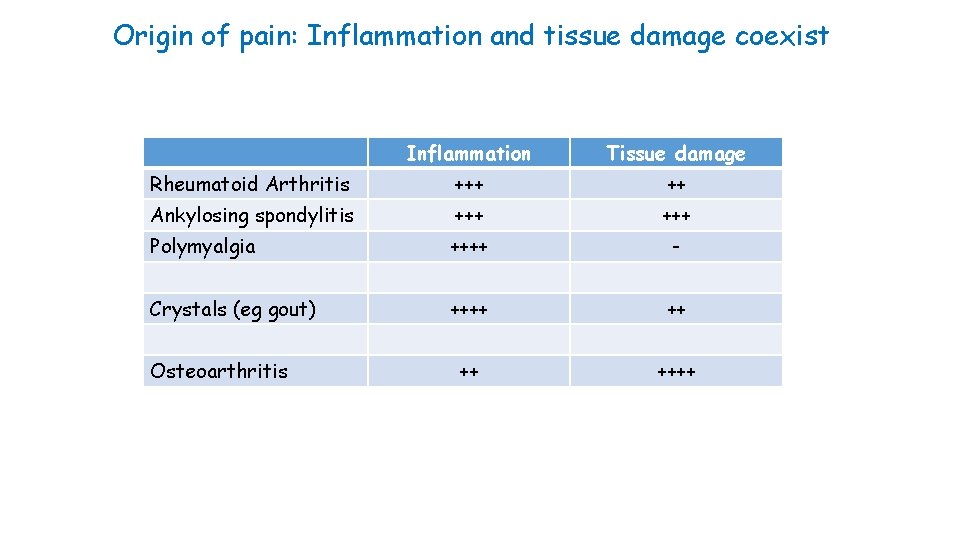
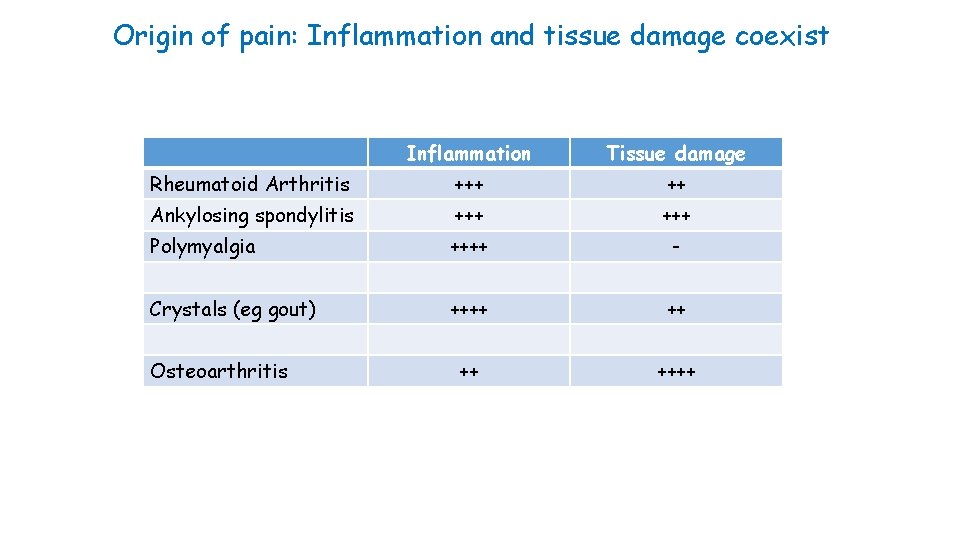
Origin of pain: Inflammation and tissue damage coexist Inflammation Tissue damage Rheumatoid Arthritis +++ ++ Ankylosing spondylitis +++ Polymyalgia ++++ - Crystals (eg gout) ++++ ++++ Osteoarthritis
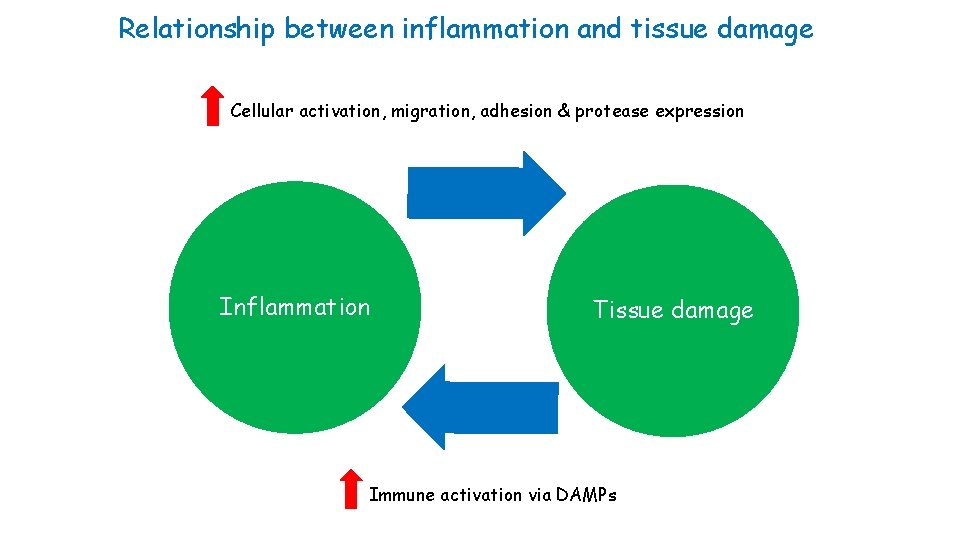
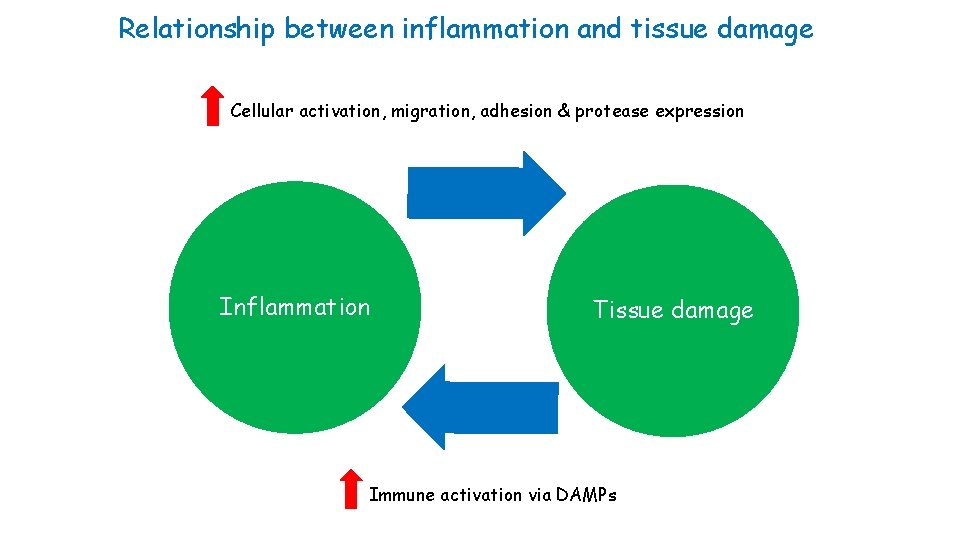
Relationship between inflammation and tissue damage Cellular activation, migration, adhesion & protease expression Inflammation Tissue damage Immune activation via DAMPs
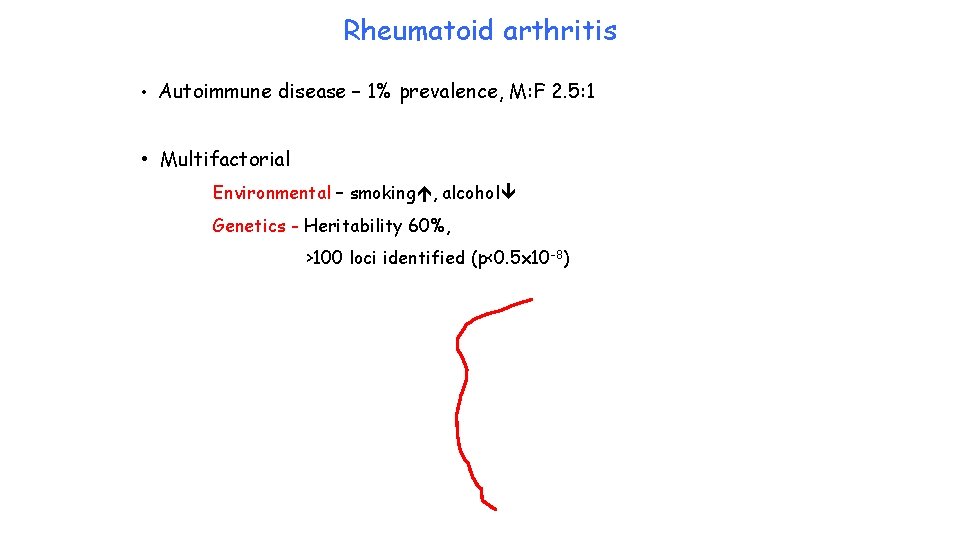
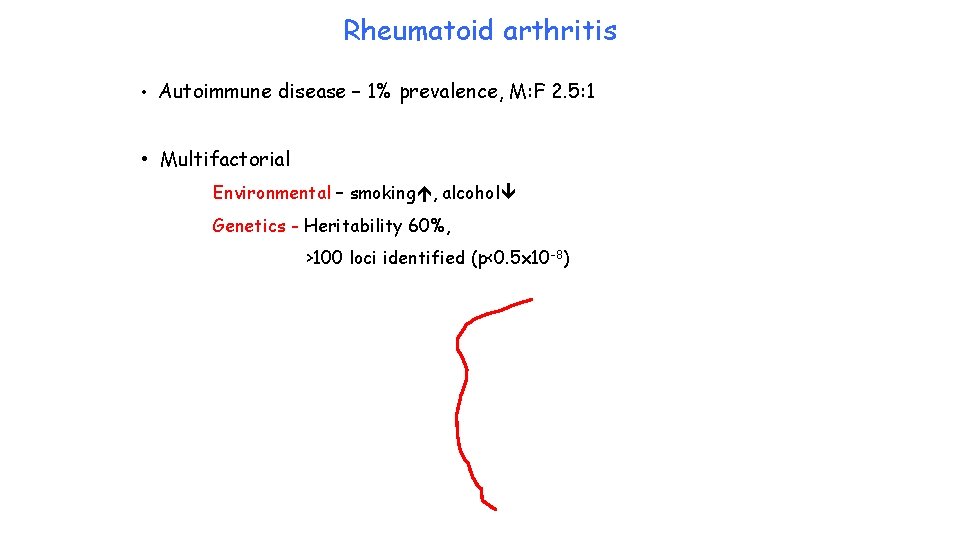
Rheumatoid arthritis • Autoimmune disease – 1% prevalence, M: F 2. 5: 1 • Multifactorial Environmental – smoking , alcohol Genetics - Heritability 60%, >100 loci identified (p<0. 5 x 10 -8)
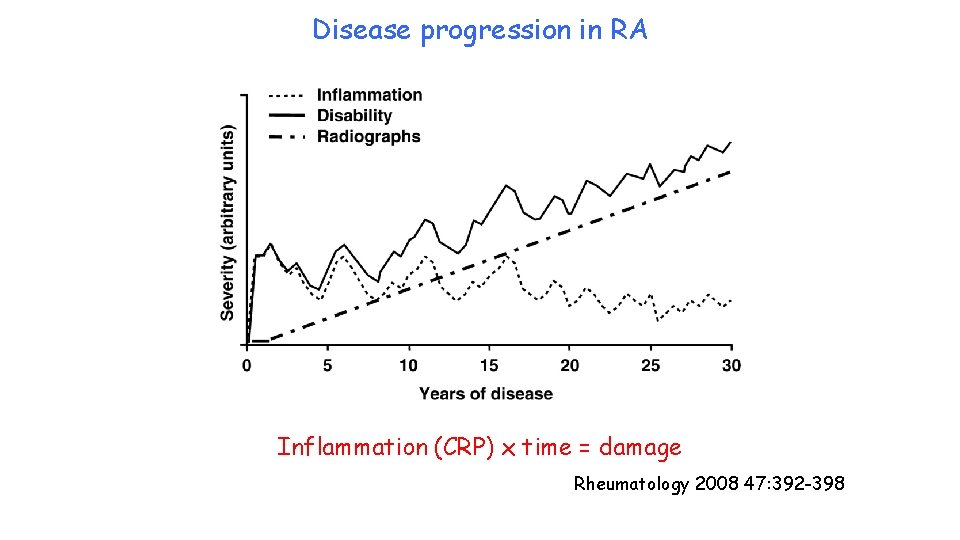
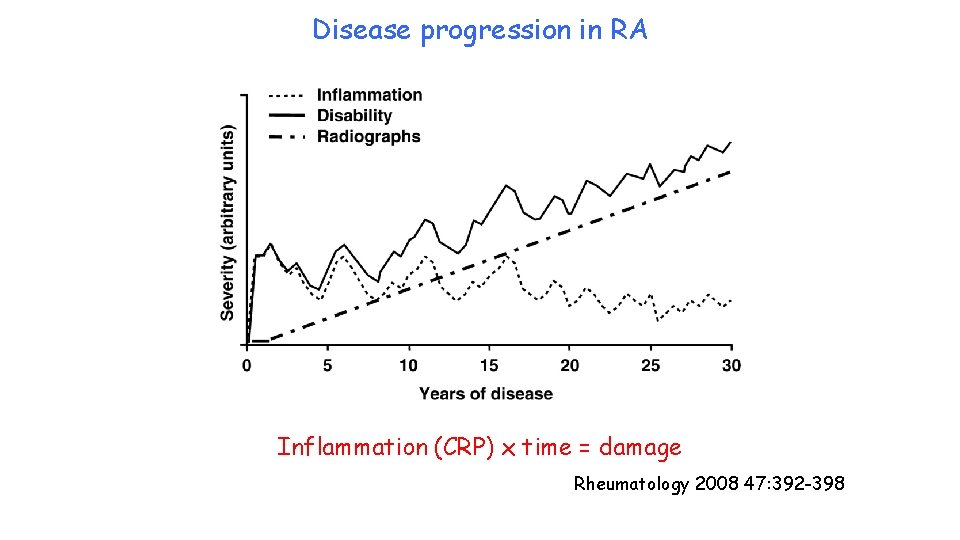
Disease progression in RA Inflammation (CRP) x time = damage Rheumatology 2008 47: 392 -398
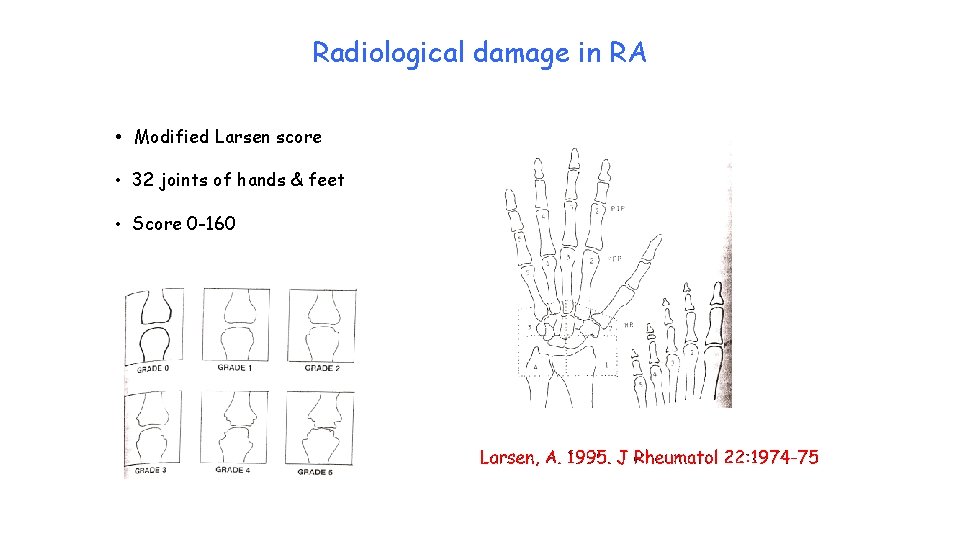
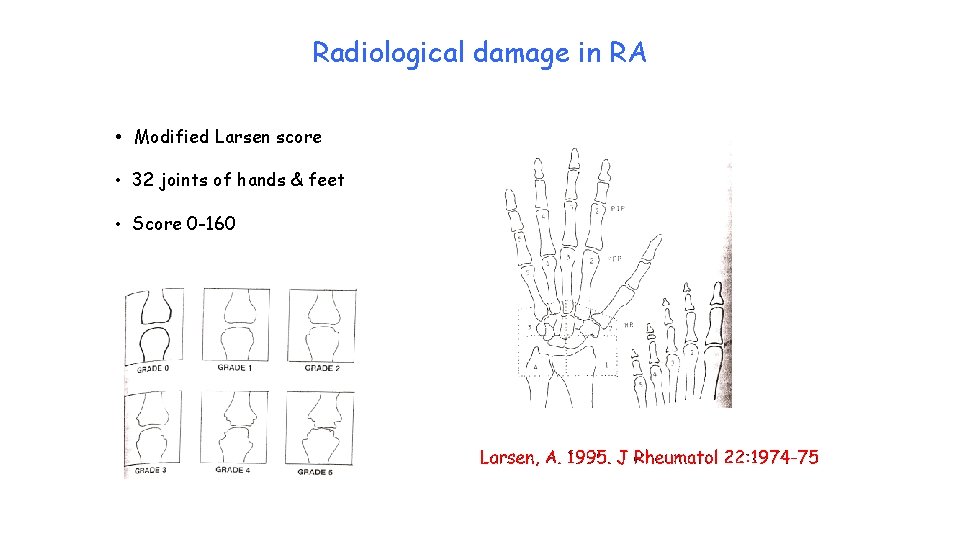
Radiological damage in RA • Modified Larsen score • 32 joints of hands & feet • Score 0 -160
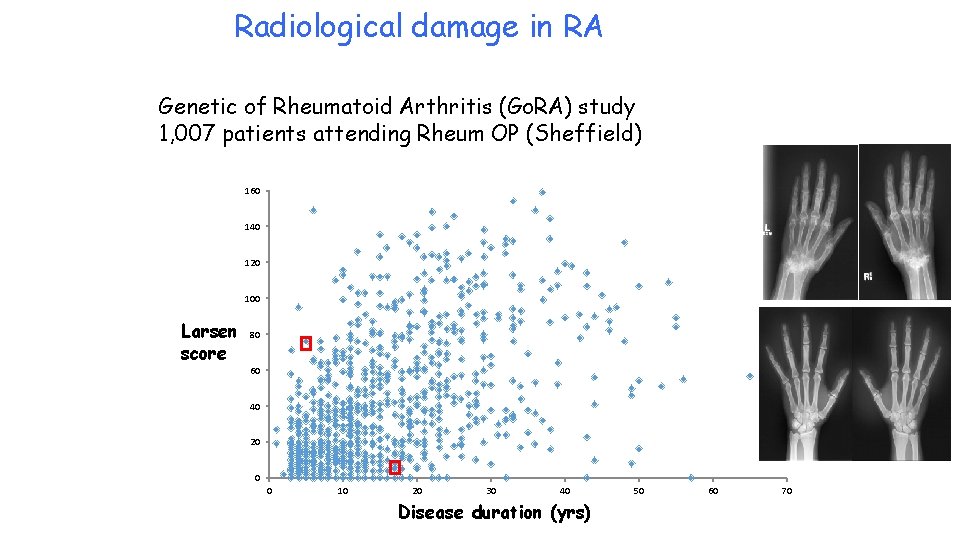
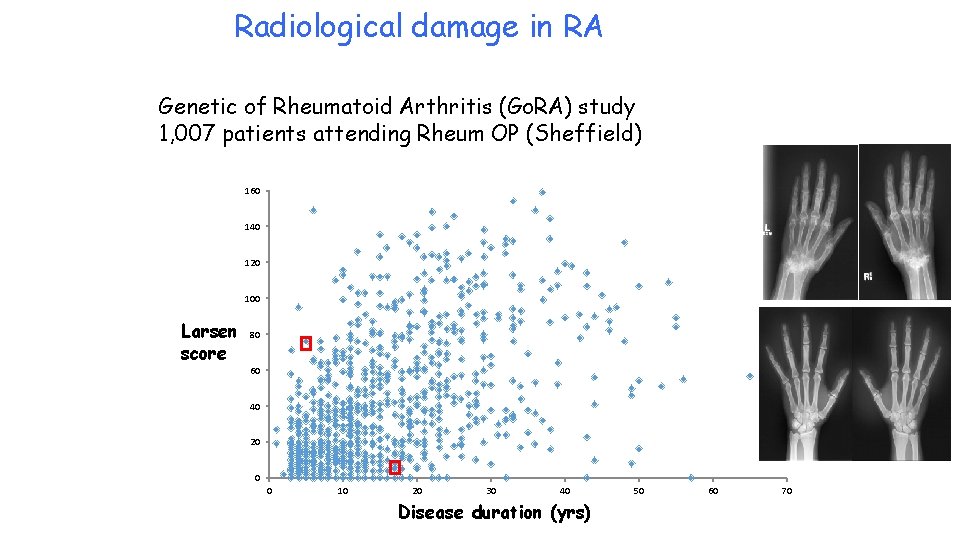
Radiological damage in RA Genetic of Rheumatoid Arthritis (Go. RA) study 1, 007 patients attending Rheum OP (Sheffield) 160 140 120 100 Larsen score 80 60 40 20 0 0 10 20 30 40 Disease duration (yrs) 50 60 70

Analgesia for RA NICE guidelines (2015) • Paracetamol, codeine or compound agents initially • Oral NSAIDs/COX-2 inhibitors should be used at the lowest effective dose for the shortest possible period of time. • Initially standard NSAID or a COX-2 inhibitor • Oral NSAIDs/COX-2 inhibitors have analgesic effects of a similar magnitude but vary in their potential gastrointestinal, liver and cardio-renal toxicity • If NSAIDs or COX-2 inhibitors are not providing satisfactory symptom control, review the disease-modifying or biological drug regimen
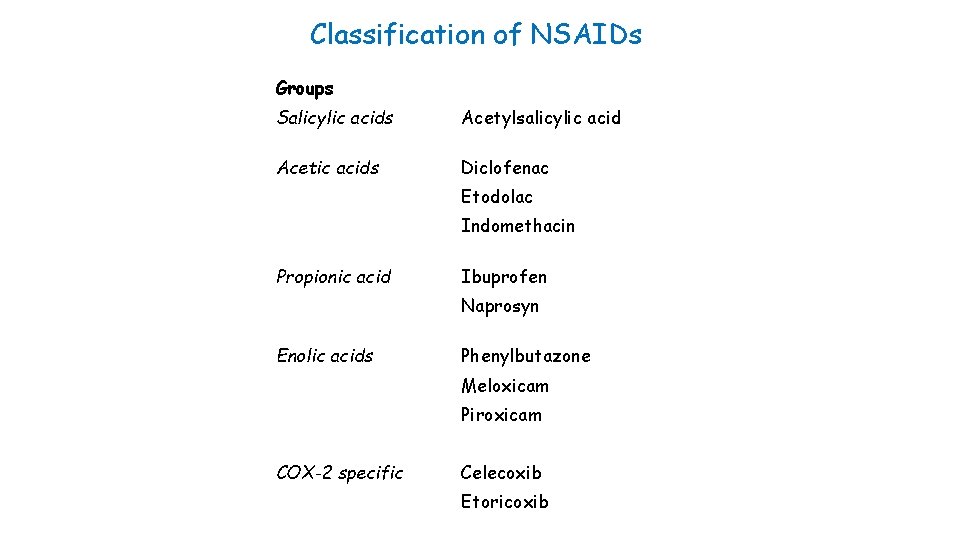
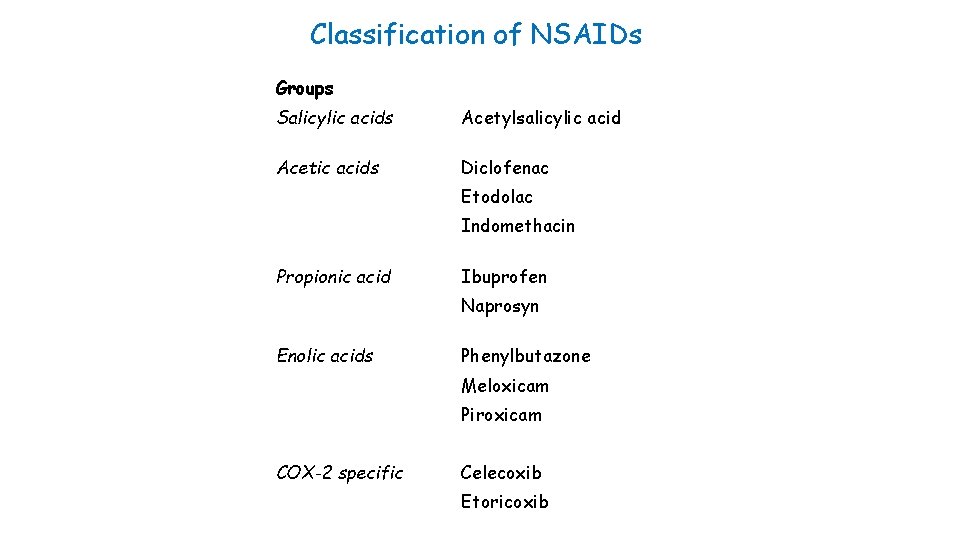
Classification of NSAIDs Groups Salicylic acids Acetylsalicylic acid Acetic acids Diclofenac Etodolac Indomethacin Propionic acid Ibuprofen Naprosyn Enolic acids Phenylbutazone Meloxicam Piroxicam COX-2 specific Celecoxib Etoricoxib
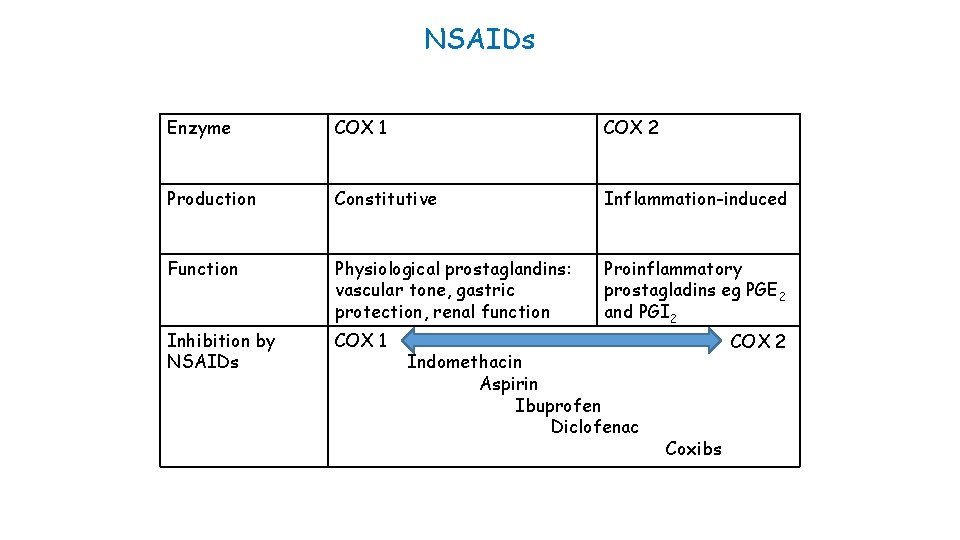
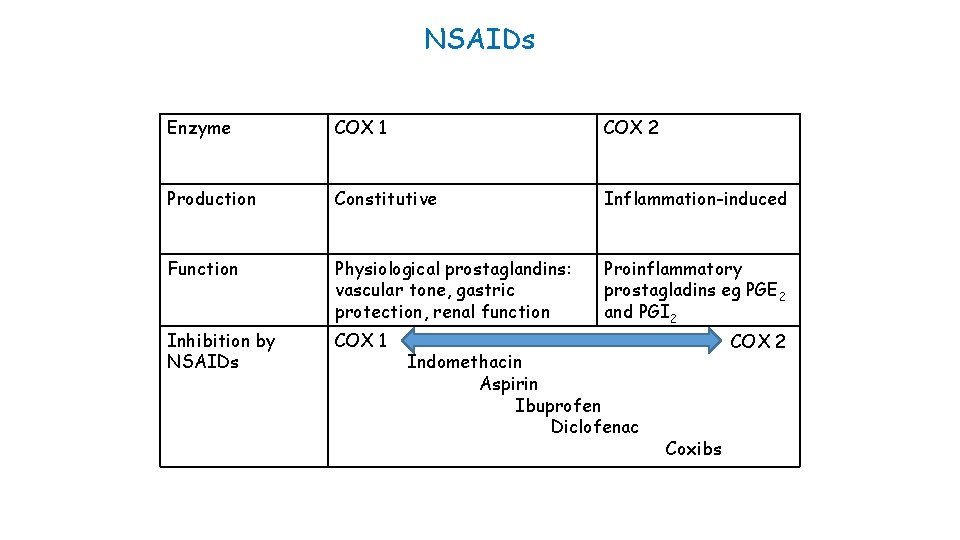
NSAIDs Enzyme COX 1 COX 2 Production Constitutive Inflammation-induced Function Physiological prostaglandins: vascular tone, gastric protection, renal function Proinflammatory prostagladins eg PGE 2 and PGI 2 Inhibition by NSAIDs COX 1 Indomethacin Aspirin Ibuprofen Diclofenac COX 2 Coxibs
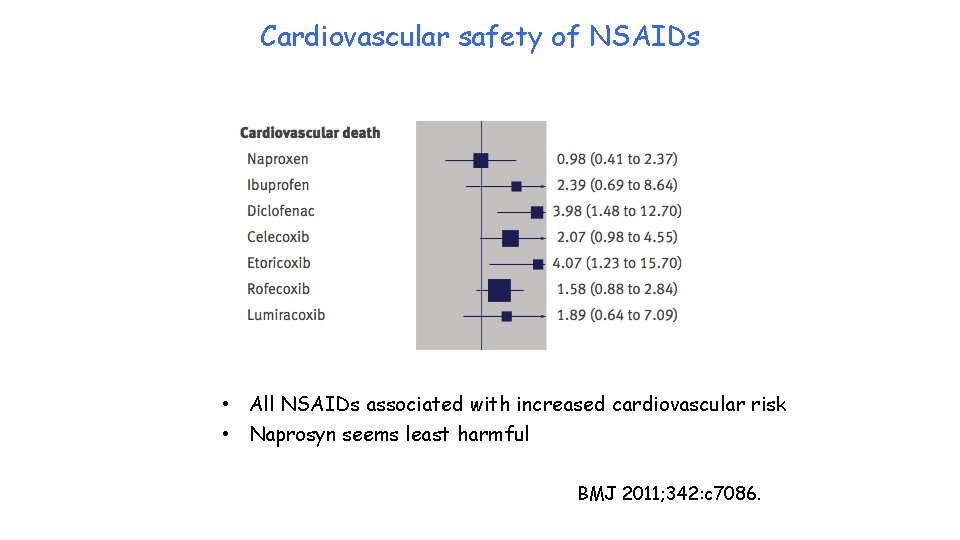
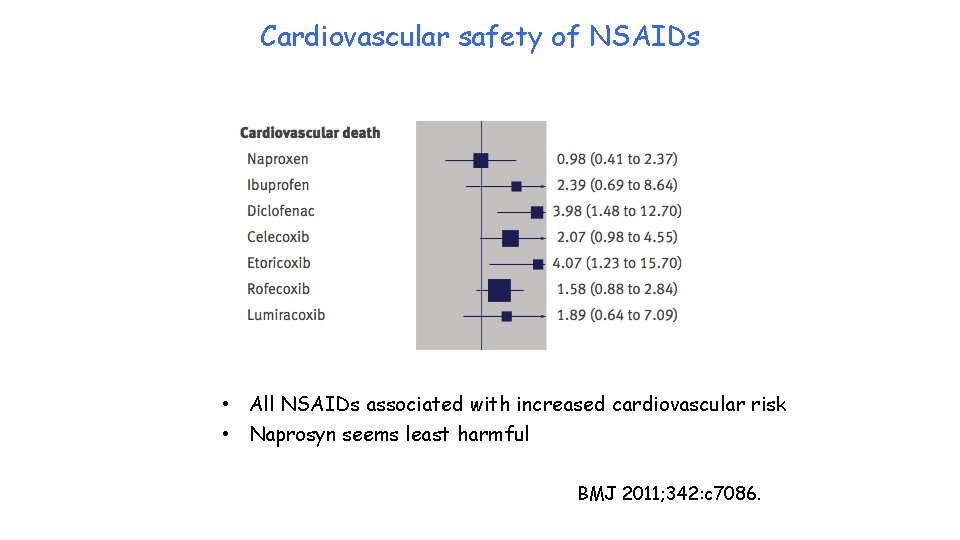
Cardiovascular safety of NSAIDs • All NSAIDs associated with increased cardiovascular risk • Naprosyn seems least harmful BMJ 2011; 342: c 7086.
Anti-inflammatory treatments - corticosteroids Potent anti-inflammatory agents Down-regulate production of many inflammatory molecules Hydrocortisone (produced by adrenal) is short acting Act through specific cytoplasmic receptors Disease modifying – reduce CRP and x-ray progression Oral, intra-muscular or intra-articular
Anti-inflammatory treatment: Disease-modifying anti-rheumatic drugs (DMARDs) • Slow onset (6 weeks +) • Systemic inflammatory response (CRP) • Improve functional status • Slow radiological progression • Monotherapy or combination • Use at onset since early 1990 s v after 2 -3 yrs 1980 s • Hydroxychloroquine, sulphasalazine, methotrexate
Anti-inflammatory treatments: biological agents Anti-TNF agents: infliximab, etanercept, adalimumab, golimumab, certulizumab Anti-IL-6: tocilizumab Anti-IL-17: secukinumab Anti-IL 12/23: ustekinumab B cell depletion: rituximab Immune cell cross-talk: abatacept
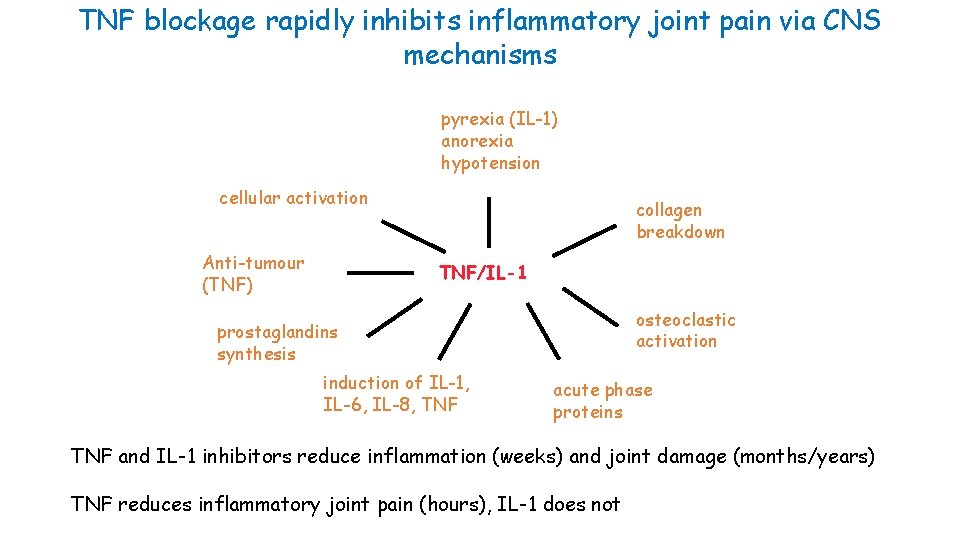
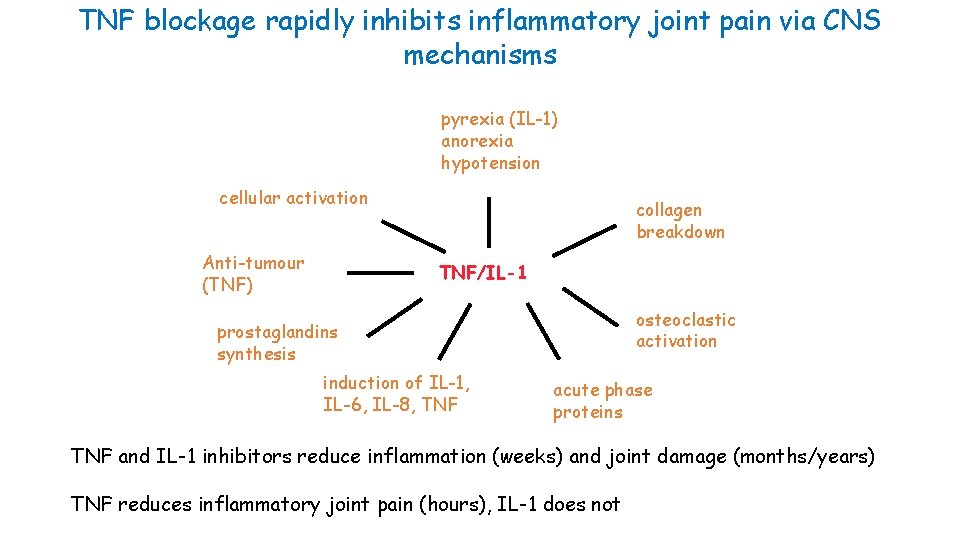
TNF blockage rapidly inhibits inflammatory joint pain via CNS mechanisms pyrexia (IL-1) anorexia hypotension cellular activation Anti-tumour (TNF) collagen breakdown TNF/IL-1 osteoclastic activation prostaglandins synthesis induction of IL-1, IL-6, IL-8, TNF acute phase proteins TNF and IL-1 inhibitors reduce inflammation (weeks) and joint damage (months/years) TNF reduces inflammatory joint pain (hours), IL-1 does not
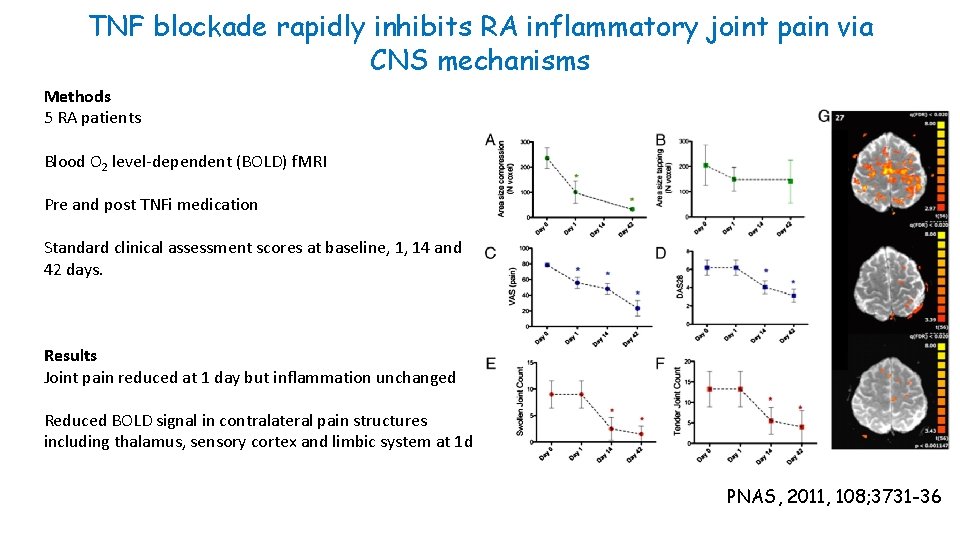
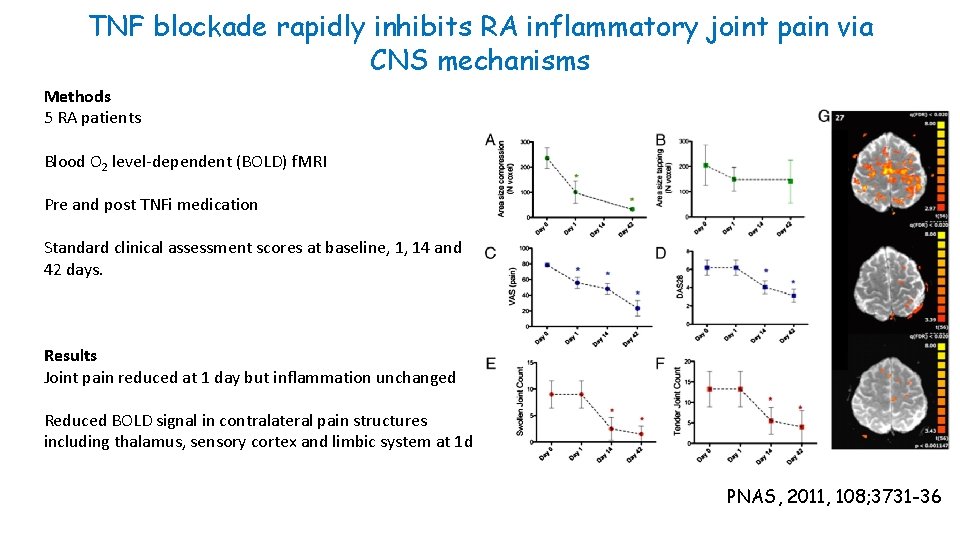
TNF blockade rapidly inhibits RA inflammatory joint pain via CNS mechanisms Methods 5 RA patients Blood O 2 level-dependent (BOLD) f. MRI Pre and post TNFi medication Standard clinical assessment scores at baseline, 1, 14 and 42 days. Results Joint pain reduced at 1 day but inflammation unchanged Reduced BOLD signal in contralateral pain structures including thalamus, sensory cortex and limbic system at 1 d PNAS, 2011, 108; 3731 -36
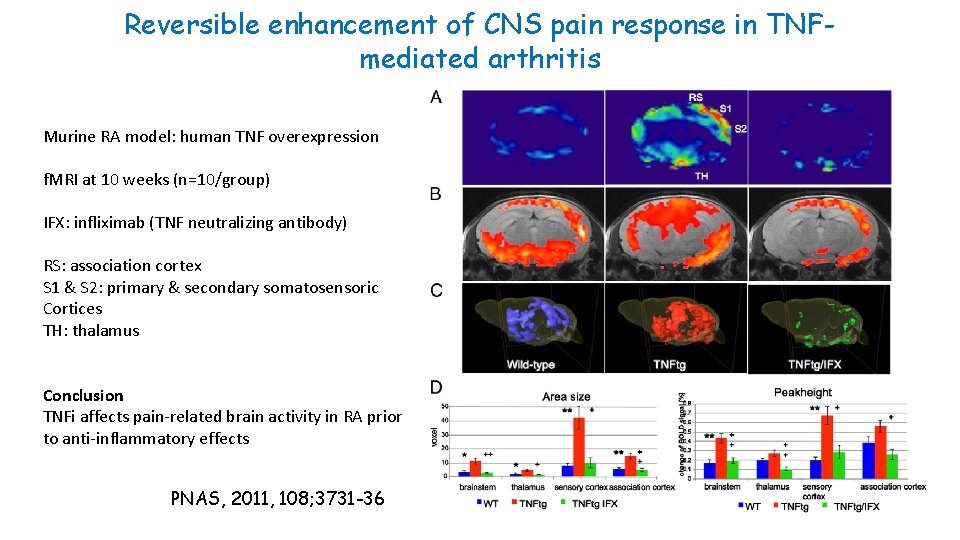
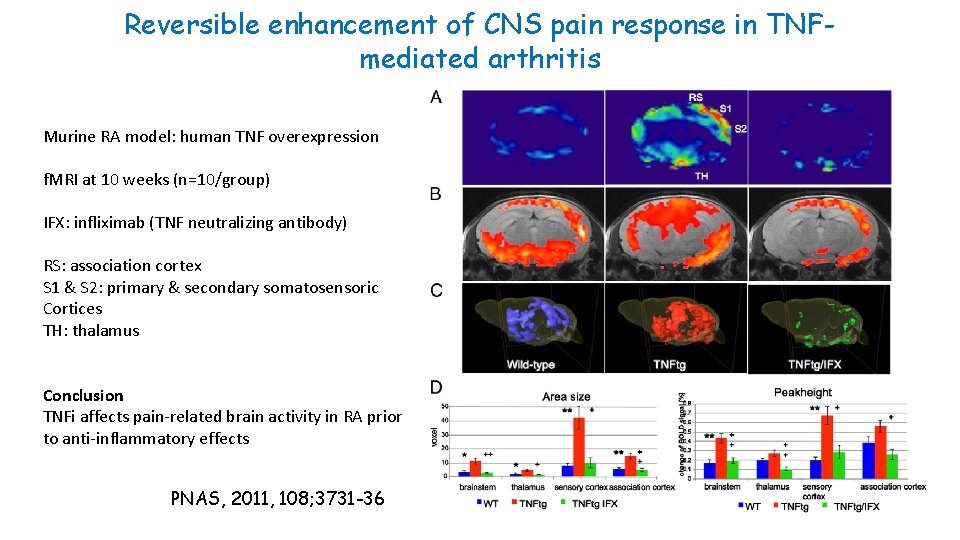
Reversible enhancement of CNS pain response in TNFmediated arthritis Murine RA model: human TNF overexpression f. MRI at 10 weeks (n=10/group) IFX: infliximab (TNF neutralizing antibody) RS: association cortex S 1 & S 2: primary & secondary somatosensoric Cortices TH: thalamus Conclusion TNFi affects pain-related brain activity in RA prior to anti-inflammatory effects PNAS, 2011, 108; 3731 -36
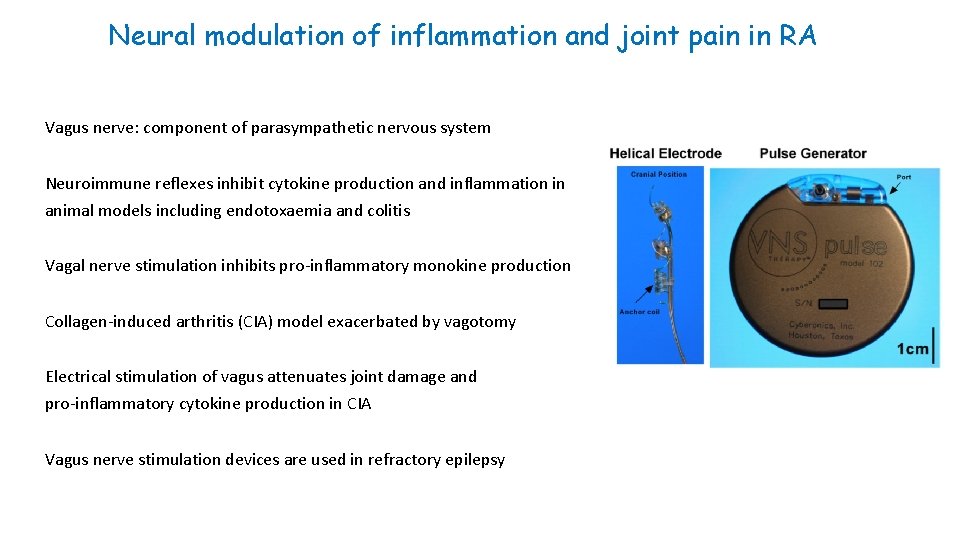
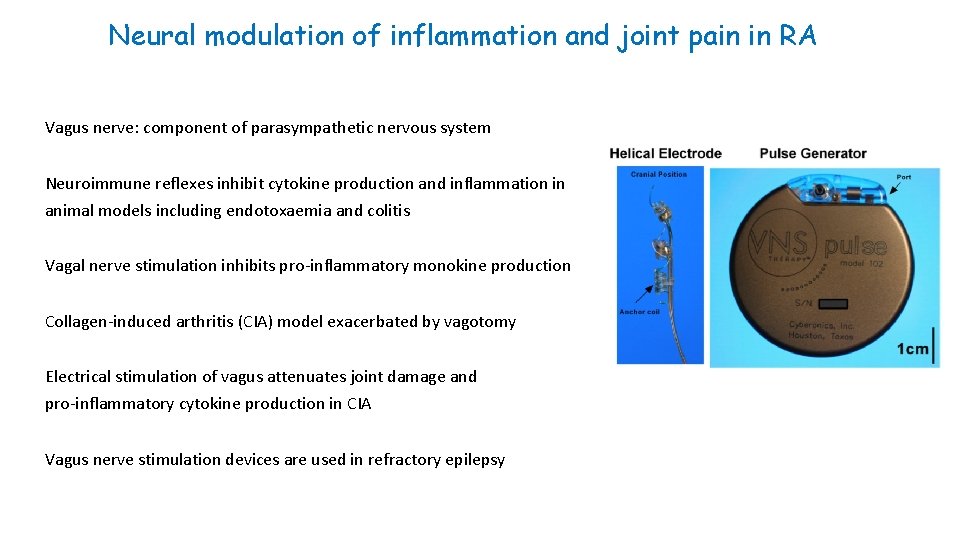
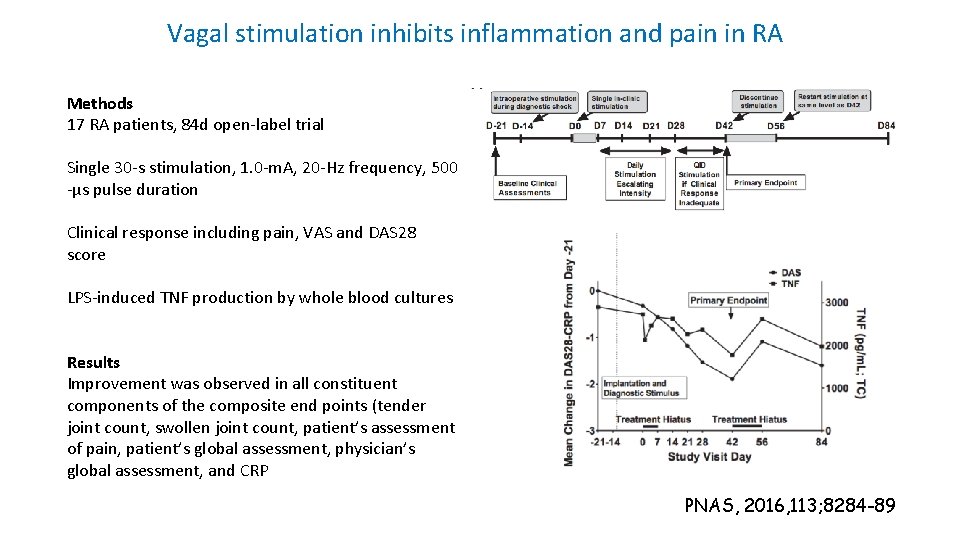
Neural modulation of inflammation and joint pain in RA Vagus nerve: component of parasympathetic nervous system Neuroimmune reflexes inhibit cytokine production and inflammation in animal models including endotoxaemia and colitis Vagal nerve stimulation inhibits pro-inflammatory monokine production Collagen-induced arthritis (CIA) model exacerbated by vagotomy Electrical stimulation of vagus attenuates joint damage and pro-inflammatory cytokine production in CIA Vagus nerve stimulation devices are used in refractory epilepsy
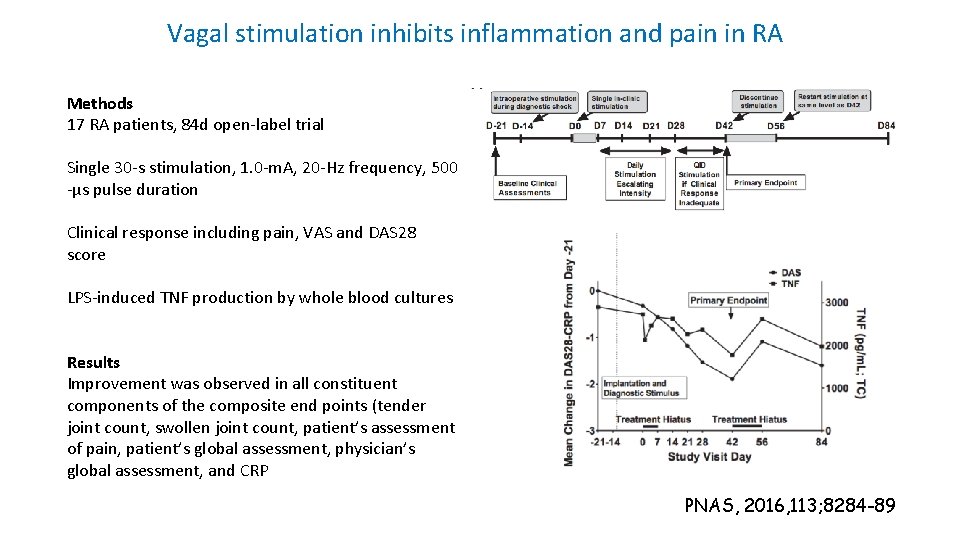
Vagal stimulation inhibits inflammation and pain in RA Methods 17 RA patients, 84 d open-label trial Single 30 -s stimulation, 1. 0 -m. A, 20 -Hz frequency, 500 -μs pulse duration Clinical response including pain, VAS and DAS 28 score LPS-induced TNF production by whole blood cultures Results Improvement was observed in all constituent components of the composite end points (tender joint count, swollen joint count, patient’s assessment of pain, patient’s global assessment, physician’s global assessment, and CRP PNAS, 2016, 113; 8284 -89
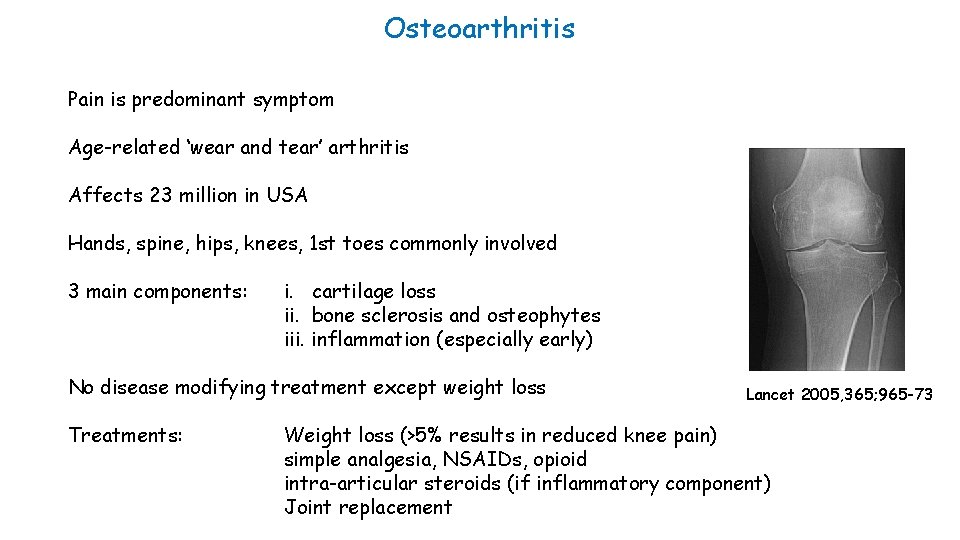
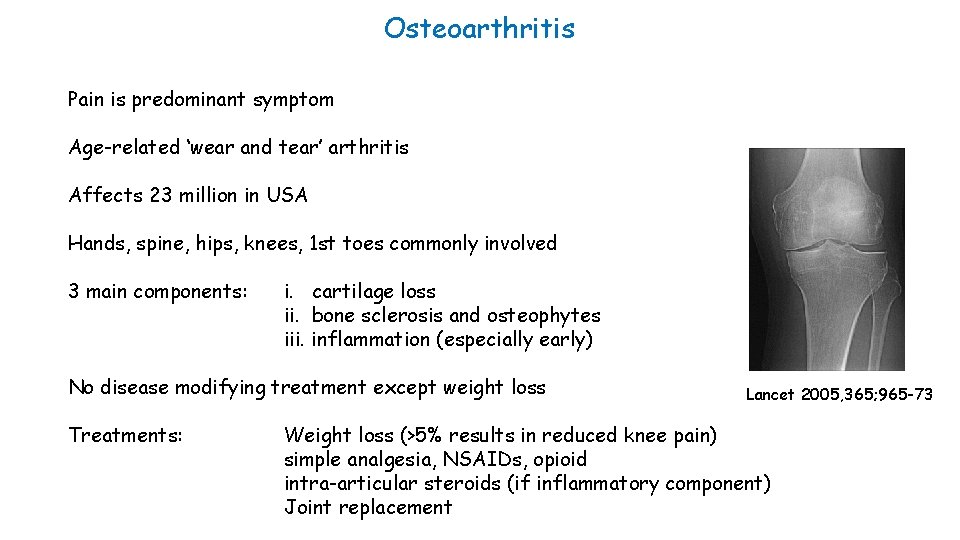
Osteoarthritis Pain is predominant symptom Age-related ‘wear and tear’ arthritis Affects 23 million in USA Hands, spine, hips, knees, 1 st toes commonly involved 3 main components: i. cartilage loss ii. bone sclerosis and osteophytes iii. inflammation (especially early) No disease modifying treatment except weight loss Treatments: Lancet 2005, 365; 965 -73 Weight loss (>5% results in reduced knee pain) simple analgesia, NSAIDs, opioid intra-articular steroids (if inflammatory component) Joint replacement
Poor correlation between structural damage and joint pain in OA Pain is primary clinical symptom in OA Origin and mechanism of pain in OA poorly understood Frequent discordance between OA tissue damage and joint pain • • 30 -50% patients with moderate-severe x-ray damage are asymptomatic 10% patients with severe knee pain have normal x-rays Variants in pathway genes associated with asymptomatic v symptomatic OA including COMT, SCN 9 A and TRPV 1 “The … data … suggest that in some individuals, central factors are superimposed upon the more traditional peripheral factors (targeted by NSAIDs, for example) leading to the need for a broader and more flexible approach to diagnosis and treatment. ” Arthritis Rheum 2013; 65: 291 -302
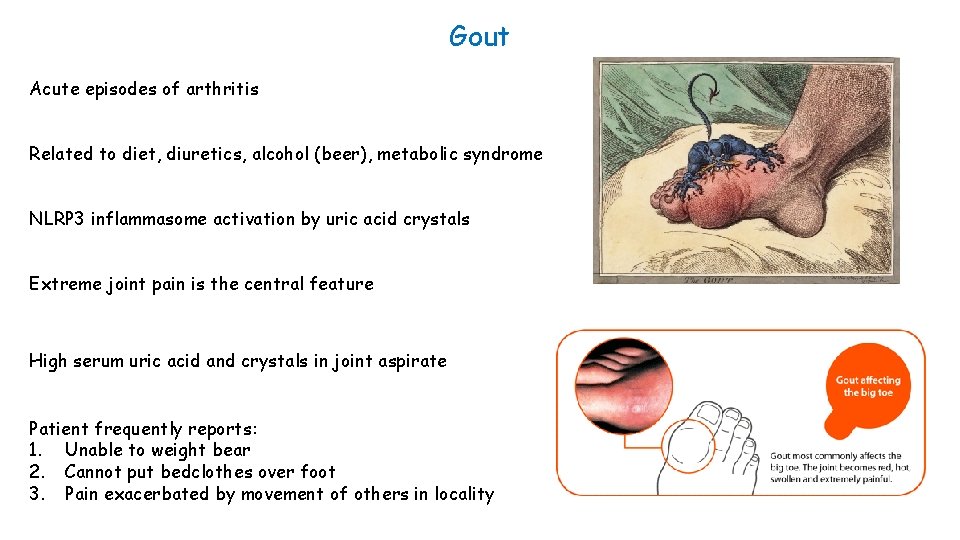
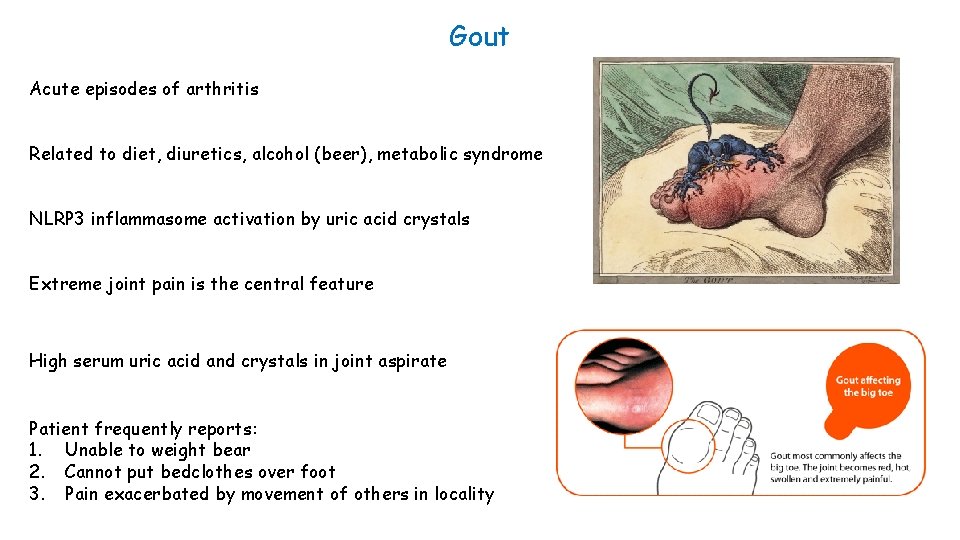
Gout Acute episodes of arthritis Related to diet, diuretics, alcohol (beer), metabolic syndrome NLRP 3 inflammasome activation by uric acid crystals Extreme joint pain is the central feature High serum uric acid and crystals in joint aspirate Patient frequently reports: 1. Unable to weight bear 2. Cannot put bedclothes over foot 3. Pain exacerbated by movement of others in locality
Pain management in acute gout NSAIDs Corticosteroids orally or intra-articular Colchicine – inhibits microtubule formation resulting in: I. ↓ NLRP 3 activation II. ↓ NFk. B activation III. ↓ adhesion molecule expression on endothelium IV. ↓ superoxide radicle production

Fibromyalgia Chronic widespread pain Prevalence of 2% to 8% Accompanied by fatigue, memory problems, and sleep disturbances Not related to inflammation or tissue damage


EULAR management recommendations of fibromyalgia Full understanding requires comprehensive assessment of pain, function and psychosocial context. … a complex and heterogeneous condition where there is abnormal pain processing and other secondary features. Optimal treatment requires a multidisciplinary approach including non-pharmacological and pharmacological treatment modalities tailored according to pain intensity, function, associated features, such as depression, fatigue and sleep disturbance in discussion with the patient. Simple analgesics such as paracetamol and other weak opioids can also be considered in the treatment of fibromyalgia. Corticosteroids and strong opioids are not recommended. Antidepressants/pregabalin frequently used Exercise, hydrotherapy, cognitive behavioural therapy Ann Rheum Dis 2008; 67: 536 -541
Weather and joint pain ‘‘Whoever would study medicine aright must learn of the following subjects. First he must consider the effect of each of the seasons of the year and the differences between them. Secondly he must study the warm and the cold winds, both those which are common to every country and those peculiar to a particular locality. . ’’ Hippocrates, ”Air, Waters, Places” 400 BCE Many patients report increased joint pain in cold, wet weather Some supporting evidence. . However it is probably due to selective matching and is a not real phenomenon…
Summary Inflammatory joint diseases • Joint pain arises from inflammation and/or tissue damage • Rapid resolution of inflammation reduces pain and prevents tissue damage • Revolutionary therapeutic advances over past 20 years for inflammatory joint diseases • TNFi reduces joint pain rapidly by action on CNS Osteoarthritis • Osteoarthritis increasing prevalence with no disease-modifying treatments • Pain and joint damage not correlated in many patients • Related to genetic variants in pathway genes Fibromyalgia • Major area of unmet need in understanding causes of fibromyalgia

 Pain x mad
Pain x mad Period or pregnant
Period or pregnant Symptoms before period
Symptoms before period Pathogenesis of pleomorphic adenoma
Pathogenesis of pleomorphic adenoma Uremia pathogenesis
Uremia pathogenesis Chronic calculous cholecystitis
Chronic calculous cholecystitis Acute cholecystitis clinical features
Acute cholecystitis clinical features Bacterial pathogenesis
Bacterial pathogenesis Cholecystitis pathophysiology
Cholecystitis pathophysiology Bacterial pathogenesis
Bacterial pathogenesis Risus sardonicus
Risus sardonicus Jaundice pathogenesis
Jaundice pathogenesis Pathogenesis dengue fever
Pathogenesis dengue fever Rabies pathogenesis
Rabies pathogenesis Pathogenesis steps
Pathogenesis steps Pathogenesis game
Pathogenesis game Left parasternal heave
Left parasternal heave Cirrhosis pathogenesis
Cirrhosis pathogenesis Histoplasma capsulatum pathogenesis
Histoplasma capsulatum pathogenesis Pathogenesis of chronic pyelonephritis
Pathogenesis of chronic pyelonephritis Pathophysiology of anemia
Pathophysiology of anemia Mechanism of ischemic stroke
Mechanism of ischemic stroke Pathogenesis of tuberculosis
Pathogenesis of tuberculosis Pain treatment satisfaction scale
Pain treatment satisfaction scale Chronic pain management irwin
Chronic pain management irwin Mechanical vs inflammatory back pain
Mechanical vs inflammatory back pain Which is permanent joint
Which is permanent joint Symphyses
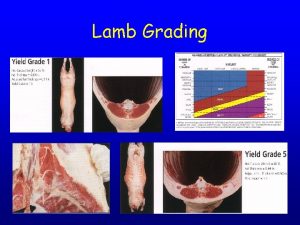
Symphyses Spool joint in lambs
Spool joint in lambs Ligamentum nuchae
Ligamentum nuchae Memorandum joint venture account
Memorandum joint venture account Break joint vs spool joint
Break joint vs spool joint Hip and leg muscles
Hip and leg muscles Comparison between virtual circuit and datagram network
Comparison between virtual circuit and datagram network