Palliative Care MINA KIM PHARMD PAIN MANAGEMENT CLINICAL
- Slides: 39
Palliative Care MINA KIM, PHARMD PAIN MANAGEMENT CLINICAL PHARMACIST
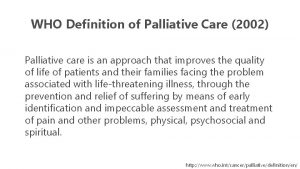
Palliative Care �The goal of palliative care is to prevent and relieve suffering and to support the best possible quality of life for patients and their families, regardless of the stage of the disease or the need for otherapies. American Academy of Hospice and Palliative Medicine
Goals of Palliative Care �Provides relief from pain and other distressing symptoms �Affirms life and regards dying as a normal process – Intends neither to hasten or postpone death �Integrates the psychological and spiritual aspects of patient care �Offers a support system to help patients and their family cope during the illness and in the family’s bereavement �Uses a team approach to address the needs of patients and their families
Team Members �Providers (Physicians, ARNPs, PAs) �Pharmacists �Nurses �Health Aides �Social Workers �Chaplains �Physical/Occupational Therapists �Music Therapists
Hospice �Palliative care for individuals who have life-limiting or incurable conditions in their last year of life �Hospice care can be provided wherever a patient resides: Home Inpatient hospice Long term care facilities (SNF, nursing homes) Hospital �Medication focus: what is necessary to make them comfortable (not all medications are relevant in hospice, i. e. , cholesterol medications)
Common Diseases in Palliative Care �Cancer �Organ Failure (Heart, Liver, Renal, Pulmonary) �Progressive Neurological Diseases (i. e. Dementia, Alzheimers) �Failure to Thrive
Symptom Management �Pain �Dyspnea �Constipation �Nausea/Vomiting �Appetite �Delirium/Agitation �Anxiety
Pain �Refer to previous lecture on assessment (KEY!) �Tylenol, NSAIDs and Opioids (standard) �Opioids Best route of administration for patient (PO, IV, SC, transdermal, PR) Scheduled dosing for patients with continuous pain Breakthrough dose should be 10% of the 24 hour dose of the scheduled opioid Know conversion between different drugs and routes �Use adjuvant medications as indicated: i. e. , anticonvulsants, antidepressants, steroids �Consider nonpharmacological therapy
Dyspnea �Difficult or labored breathing �Incidence in terminal illness ranges from 12 -74% Most common in lung cancer and COPD Tends to worsen as death approaches �Common descriptions Cannot get enough air - “air hunger” Tightness in the chest Feeling a need to gasp or pant Feeling suffocated
Dyspnea: Treatment from Etiology �End-of-life respiratory failure: opioids Morphine is the standard treatment Decreases patient’s perception of breathlessness, reduces respiratory needs and oxygen consumption �COPD or asthma: bronchodilators, steroid �CHF leading to volume overload: diuretics Adjust doses according to patient response Signs of volume overload include: SOB, crackles in lungs, peripheral edema �Pleural effusion: consider thoracentesis �Anxiety associated dyspnea: anxiolytics
Dyspnea: Treatment �Oxygen to achieve O 2 saturation > 90% �Non-pharmacological Fans Positioning Breathing exercises, relaxation techniques Rest/conserve energy
Constipation � 2 -10% of general population �Increases with age �Effects more than 50% of patients in a palliative care unit or in hospice �Frequently seen symptom at the end of life �Undertreated by providers
Constipation: Causes �Immobility �Diet/hydration �Medications Opioids, anticholinergics, TCAs �Disease Cancer (hypercalcemia, bowel cancers, tumors invading GI tract) Chronic diseases (i. e , IBS, neurologic diseases, diverticular disease)
Constipation: Assessment �Characteristic �Frequency �Physical Examination Diagnostic �Medications �Fluid/food intake
Constipation: Treatment �Prevention is key! �Always prescribe constipation medications with opioids �Encourage fluid intake and dietary fiber �Physical activity �Disimpaction
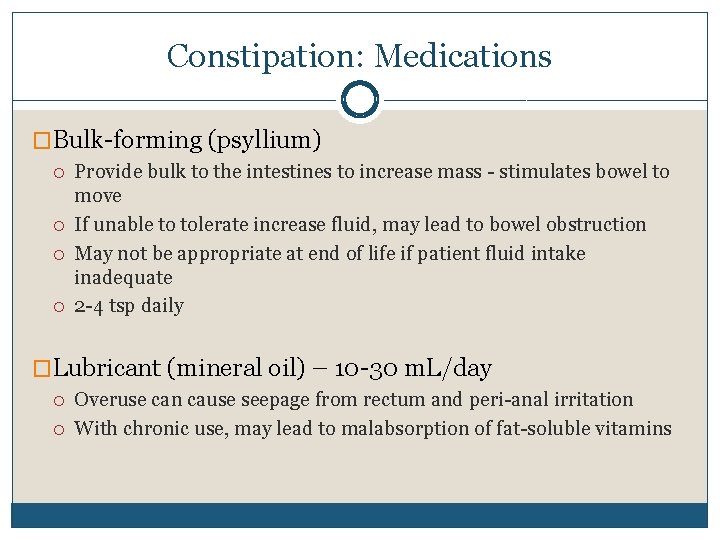
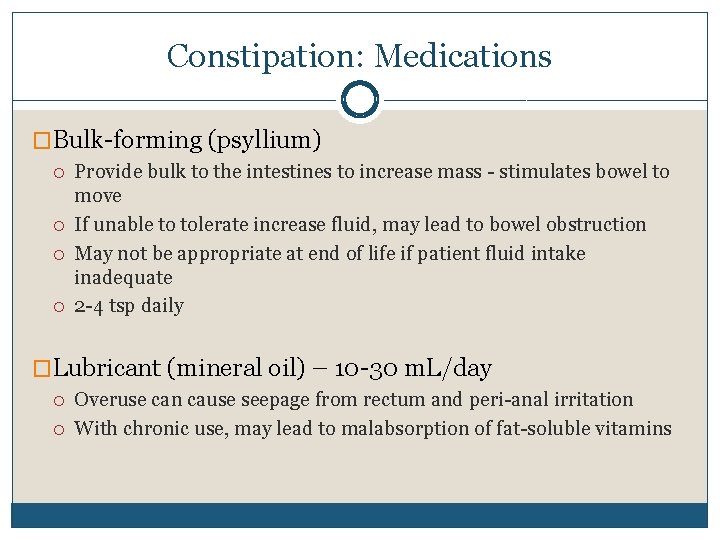
Constipation: Medications �Bulk-forming (psyllium) Provide bulk to the intestines to increase mass - stimulates bowel to move If unable to tolerate increase fluid, may lead to bowel obstruction May not be appropriate at end of life if patient fluid intake inadequate 2 -4 tsp daily �Lubricant (mineral oil) – 10 -30 m. L/day Overuse can cause seepage from rectum and peri-anal irritation With chronic use, may lead to malabsorption of fat-soluble vitamins
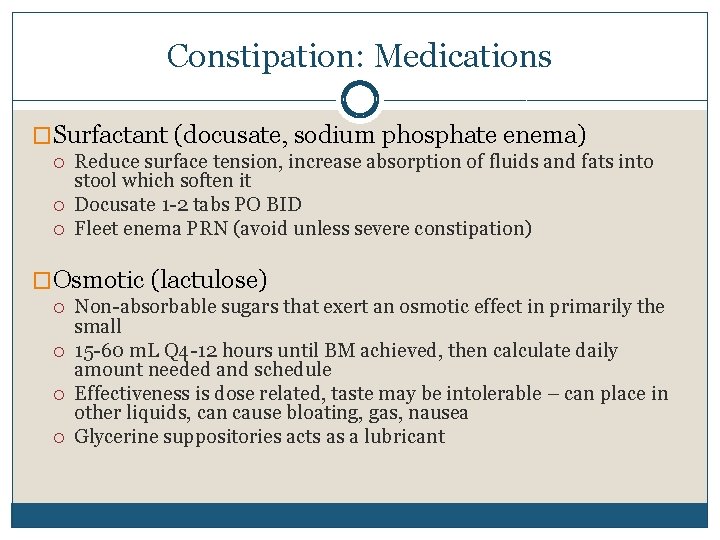
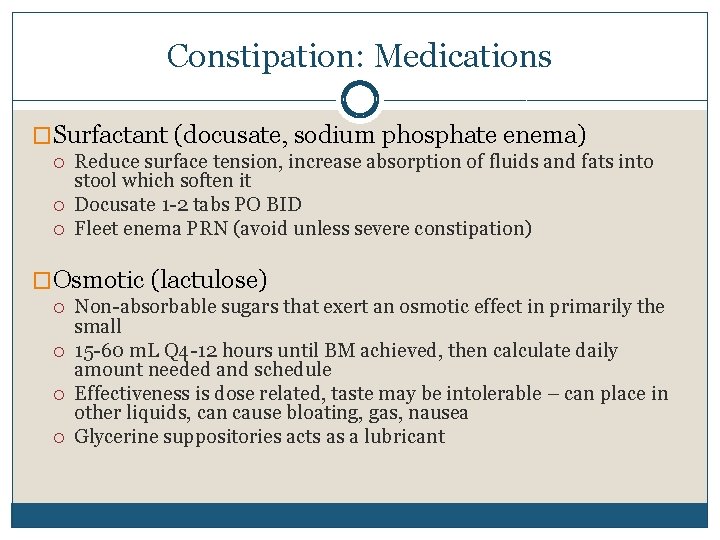
Constipation: Medications �Surfactant (docusate, sodium phosphate enema) Reduce surface tension, increase absorption of fluids and fats into stool which soften it Docusate 1 -2 tabs PO BID Fleet enema PRN (avoid unless severe constipation) �Osmotic (lactulose) Non-absorbable sugars that exert an osmotic effect in primarily the small 15 -60 m. L Q 4 -12 hours until BM achieved, then calculate daily amount needed and schedule Effectiveness is dose related, taste may be intolerable – can place in other liquids, can cause bloating, gas, nausea Glycerine suppositories acts as a lubricant
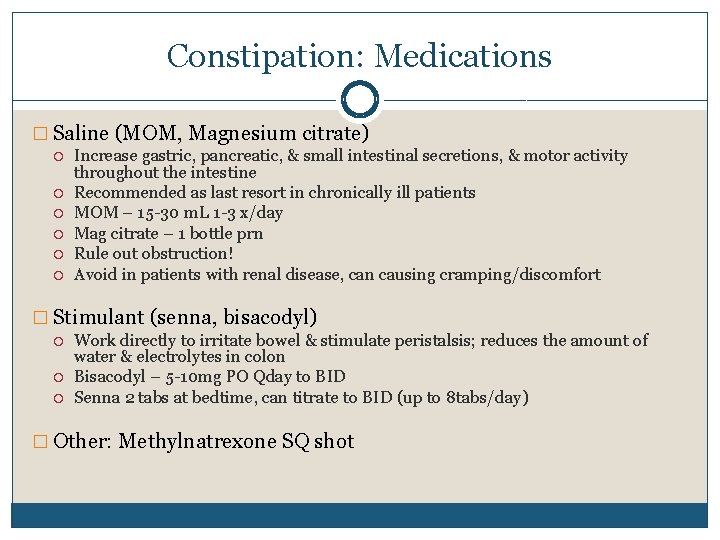
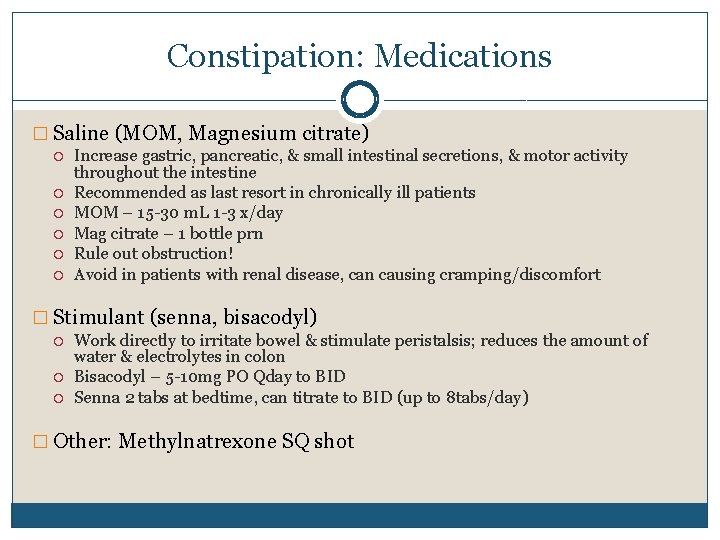
Constipation: Medications � Saline (MOM, Magnesium citrate) Increase gastric, pancreatic, & small intestinal secretions, & motor activity throughout the intestine Recommended as last resort in chronically ill patients MOM – 15 -30 m. L 1 -3 x/day Mag citrate – 1 bottle prn Rule out obstruction! Avoid in patients with renal disease, can causing cramping/discomfort � Stimulant (senna, bisacodyl) Work directly to irritate bowel & stimulate peristalsis; reduces the amount of water & electrolytes in colon Bisacodyl – 5 -10 mg PO Qday to BID Senna 2 tabs at bedtime, can titrate to BID (up to 8 tabs/day) � Other: Methylnatrexone SQ shot
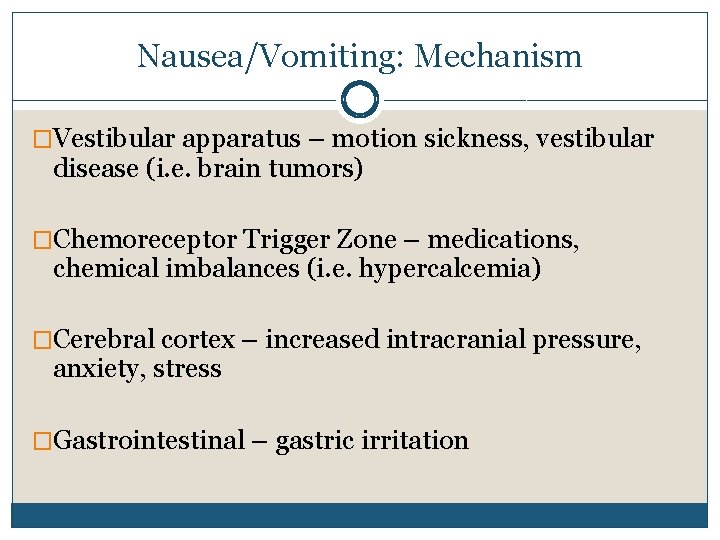
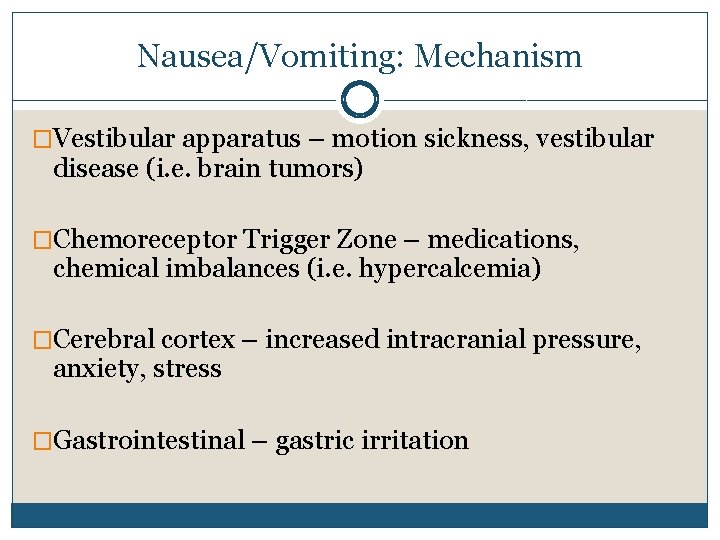
Nausea/Vomiting: Mechanism �Vestibular apparatus – motion sickness, vestibular disease (i. e. brain tumors) �Chemoreceptor Trigger Zone – medications, chemical imbalances (i. e. hypercalcemia) �Cerebral cortex – increased intracranial pressure, anxiety, stress �Gastrointestinal – gastric irritation
Nausea/Vomiting: Assessment �Good assessment is very important �Precipitating/palliating �Quality �Temporal �Previous treatment or therapy
Nausea/Vomiting: Nonpharmacologic �Acupuncture �Relaxation therapy �Interventions if needed (stents, NG tube, etc) �Changing food/eating patterns 6 -8 small meals a day Food selection Eat slowly Stay upright at least 1 hour after eating
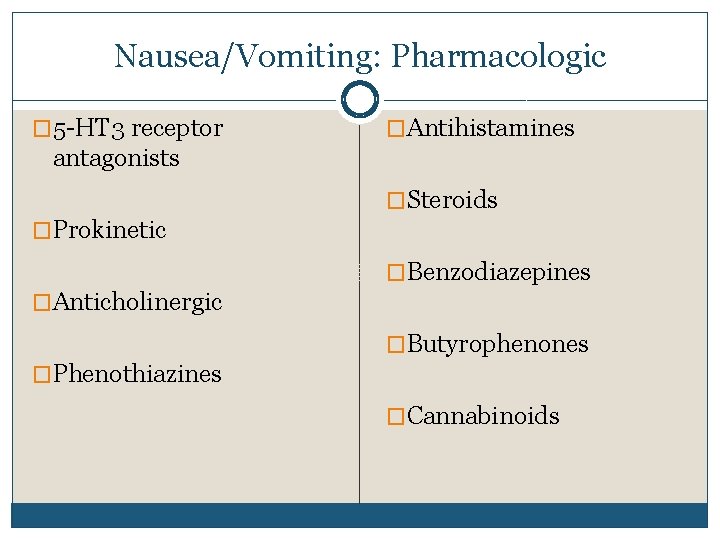
Nausea/Vomiting: Pharmacologic � 5 -HT 3 receptor �Antihistamines antagonists �Steroids �Prokinetic �Benzodiazepines �Anticholinergic �Butyrophenones �Phenothiazines �Cannabinoids
Nausea/Vomiting: Pharmacologic � 5 -HT 3 receptor antagonists – ondansetron, granisetron, dolasetron �Prokinetic – metoclopramide �Anticholinergic – scopolamine �Phenothiazines – prochlorperazine
Nausea/Vomiting: Pharmacologic �Steroids – dexamethasone �Benzodiazepines – lorazepam �Butyrophenones - haloperidol, droperidol �Cannabinoids – dronabinol, marijuana
Appetite �Anorexia vs. Cachexia �Causes Metabolic imbalances Secondary to physical symptoms (i. e. pain, dysphagia, alcoholism) Medication side effects Physiological / Spiritual distress
Appetite: Treatment �Medications Megestrol acetate (Megace) Metoclopramide (Reglan) Dexamethasone (Decadron) Dronabinol (Marinol) �Non-pharmacological Emotional and nutritional support Enteral and parenteral nutrition Support for family
Delirium/Agitation �Delirium – change in cognition that is relatively acute in onset and generally reversible �Presentation Disorientation Change in consciousness Distress Paranoia, nightmares, hallucination can often occur at end of life
Delirium/Agitation �Agitation – excessive restlessness accompanied by increased mental and physical activity Inability to concentrate/relax Disturbances in sleep/rest Fluctuating levels of consciousness, cognitive dysfunction �Often referred to as “terminal restlessness” or “terminal agitation” at the end of life
Delirium/Agitation �Almost half of patients experience delirium/agitation in their last 48 hours �Causes include (as defined by the American Psychiatric Association DSM-IV) Organic: malignancies, infection, renal/hepatic failure, metabolic abnormalities, hypoxemia Non-organic: sensory deprivation, changes in environment, medications, withdrawal
Delirium/Agitation: Assessment Tools �Mini-Mental Status Exam �Delirium rating scale �Memorial Delirium Assessment Scale �Confusion Assessment Method �Neecham Confusion Scale
Delirium/Agitation: Treatment �Is treatment necessary? Delirium vs. Agitation �Treatment Correct underlying cause Symptomatic and supportive therapy if necessary
Delirium/Agitation: Nonpharmacological �Environment Avoid excessive stimulation Reorient patient as needed Create familiar and comfortable setting Presence of family/friends �Complementary therapy Therapeutic touch Spiritual support
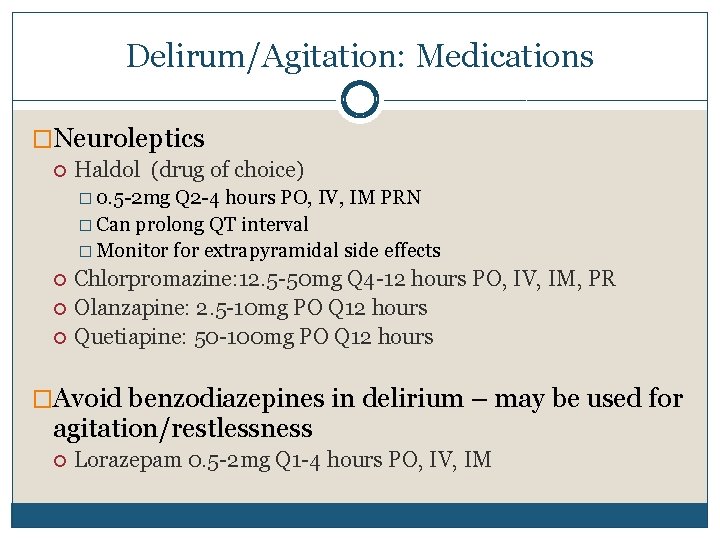
Delirum/Agitation: Medications �Neuroleptics Haldol (drug of choice) � 0. 5 -2 mg Q 2 -4 hours PO, IV, IM PRN � Can prolong QT interval � Monitor for extrapyramidal side effects Chlorpromazine: 12. 5 -50 mg Q 4 -12 hours PO, IV, IM, PR Olanzapine: 2. 5 -10 mg PO Q 12 hours Quetiapine: 50 -100 mg PO Q 12 hours �Avoid benzodiazepines in delirium – may be used for agitation/restlessness Lorazepam 0. 5 -2 mg Q 1 -4 hours PO, IV, IM
Anxiety �Causes Poorly controlled pain Medical conditions causing physiological/emotional/spiritual distress �Interview of the patient is key Find physical cause and treat if possible Support through counseling, spiritual care, relaxation techniques and coping skills
Anxiety: Treatment �Benzodiazepines (most commonly used) Numerous agents that can be given IV/PO Use as needed and schedule if needed Lorazepam, alprazolam, clonazepam, diazepam �Barbiturates Phenobarbital 60 mg PR Q 4 -12 hours PRN Use when benzodiazepines ineffective Rapid onset and sedating �Neuroleptics Useful when anxiety occurs with delirium/agitation �Tricyclic Antidepressants Useful when anxiety occurs with depression
Palliative Sedation or Comfort Care �Terminally ill patients with expected life of hours to days �Usually takes place usually in an inpatient setting (hospital, hospice) �Stop all medications and procedures that are not necessary for comfort �Continuous drips (opioids, benzodiazepine) titrated for comfort
Double Effect �Medical decision that may result in both desirable and undesirable effects: allowing an unintended bad event to happen in the course of trying to do a good thing �Ethically permissible if Action itself is good or indifferent Agent intends the good effects The good effect must not occur via the bad effect �Example: giving opioids for pain in terminal cancer but…this may also lead to respiratory depression which may cause death sooner
Washington Death with Dignity Act � Terminally ill, competent, adult Washington residents � Prognosis of ≤ 6 months � Request & self-administer lethal medication prescribed by a physician � 2 physicians diagnose the patient and determine if the patient has the capacity to make an informed decision � Optional referral to a psychologist/psychiatrist if concerned about mental health affecting capacity to make decisions � Two oral and one written request � A 15 -day waiting period between oral requests � Physicians, patients and others acting in good faith have criminal and civil immunity
Main Message Is your treatment consistent with the patient’s goals of care?
 Palliative care versus hospice care
Palliative care versus hospice care Elizabeth farrington pharmd
Elizabeth farrington pharmd Rutgers pharmd fellowship
Rutgers pharmd fellowship Hip fracture clinical care standard
Hip fracture clinical care standard Esas-r
Esas-r Rug-adl
Rug-adl Tarek mahdi md
Tarek mahdi md Principles of palliative care
Principles of palliative care Palliative care in nepal
Palliative care in nepal Palliative care assistant
Palliative care assistant European certificate in palliative care
European certificate in palliative care Parallel planning palliative care
Parallel planning palliative care Franciscan hospice and palliative care
Franciscan hospice and palliative care Traduzione
Traduzione Symptom assessment scale palliative care
Symptom assessment scale palliative care Palliative care quality collaborative
Palliative care quality collaborative Antiemetic ladder
Antiemetic ladder Just in case bag palliative care
Just in case bag palliative care Amber care bundle nice
Amber care bundle nice Goscote palliative care centre
Goscote palliative care centre Barry laird
Barry laird Bluegrass care navigators hazard ky
Bluegrass care navigators hazard ky Calvary palliative care
Calvary palliative care Anorexia, nausea and vomiting
Anorexia, nausea and vomiting Palliative care matters
Palliative care matters Dr hong-phuc tran
Dr hong-phuc tran Goc palliative care
Goc palliative care Npcrc
Npcrc Driver diagram palliative care
Driver diagram palliative care Anergia definition
Anergia definition Textbook of palliative care communication
Textbook of palliative care communication Oacc palliative care
Oacc palliative care Ethical issues in palliative care
Ethical issues in palliative care Mad pain martian pain
Mad pain martian pain Period or pregnant
Period or pregnant Signs of period vs pregnancy
Signs of period vs pregnancy Primary secondary and tertiary health care
Primary secondary and tertiary health care Angina pectoris nursing diagnosis
Angina pectoris nursing diagnosis Mina tajvidi
Mina tajvidi Kuka määrittelee toimintatavat yhteisellä työpaikalla
Kuka määrittelee toimintatavat yhteisellä työpaikalla