Overview of CAQH Index and Value of CAQH


- Slides: 65
Overview of CAQH Index and Value of CAQH CORE Operating Rules to the Dental Industry Reid Kiser and Taha Anjarwalla May 1, 2018 © 2018 CAQH, All Rights Reserved.
Session Topics § About CAQH § Overview of CAQH Index § Value of CAQH CORE Operating Rules © 2018 CAQH, All Rights Reserved. 2
About CAQH © 2018 CAQH, All Rights Reserved. 3
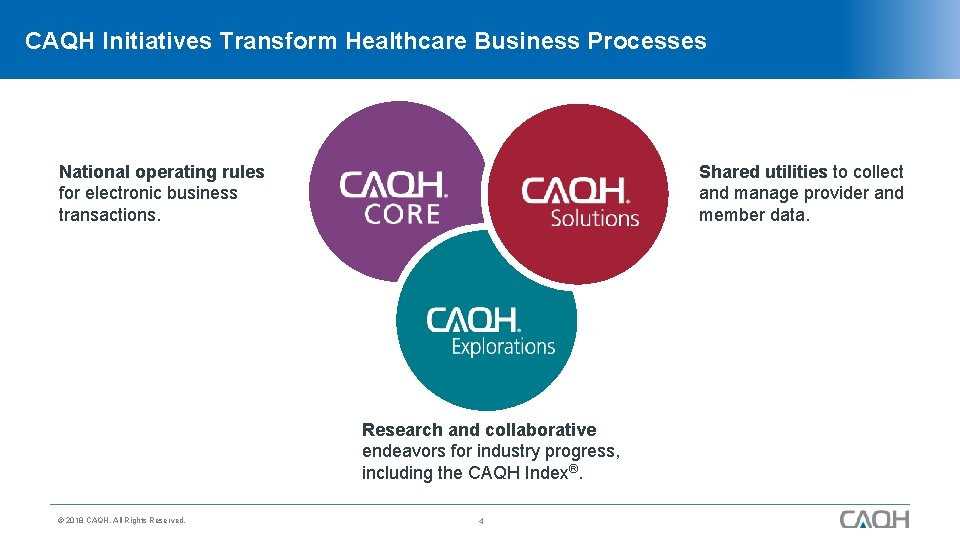
CAQH Initiatives Transform Healthcare Business Processes National operating rules for electronic business transactions. Shared utilities to collect and manage provider and member data. Click to add title Research and collaborative endeavors for industry progress, including the CAQH Index®. © 2018 CAQH, All Rights Reserved. 4
5 CAQH Solutions for Healthcare Provider Data: § CAQH Pro. View® is the industry standard for provider data collection and distribution. § Direct. Assure® increases the accuracy of provider directories. § Veri. Fide™ streamlines provider credentialing by standardizing and automating data verification. Click tomulti-state add title information on provider licensure disciplinary § Sanctions. Track® delivers comprehensive, actions. § Enroll. Hub® reduces costly paper checks with provider enrollment for EFT and ERA. Solution for Coordination of Benefits: § COB Smart® identifies health plan members with overlapping coverage. © 2018 CAQH, All Rights Reserved. 5
Highlights of CAQH Dental Industry Touchpoints § CORE Participation: HHS-mandated CORE Operating Rules apply to dental plans; dental plans have a direct voice in operating rule development. § CORE Certification: Dental plans are certifying conformance with the operating rules. © 2018 CAQH, All Rights Reserved. § § CAQH Index: Dental plans are contributing data to track industry adoption of the HIPAAmandated electronic administrative transactions; 2015 report began tracking adoption by the dental health industry. 6 Pro. View: ADA and CAQH § have formed a strategic alliance to help streamline the credentialing process for dentists, dental plans and employers. Powered by Pro. View®, it enables dentists to enter their professional and practice information one time in an easy-to-use, fast and protected digital platform. Enroll. Hub: Dental plans are increasingly using EFT/ERA through standardized enrollments.
2017 CAQH Index® A Report of Healthcare Industry Adoption of Electronic Business Transactions and Cost Savings Reid Kiser May 1, 2018 © 2018 CAQH, All Rights Reserved.
Objectives § About the CAQH Index § Findings Adoption Rates Cost of Transactions for Healthcare Providers Cost of Transactions for Health Plans National Potential Cost Savings § How to Participate in the 2018 Index § Q&A © 2018 CAQH, All Rights Reserved. 8
What is the CAQH Index? § A voluntary nationwide survey of: Commercial medical health plans. Commercial dental health plans. Healthcare providers. § The industry source for: Tracking adoption of fully electronic administrative transactions. Estimating the cost savings opportunity. § Guided by the CAQH Index Advisory Council. Experts in administrative transactions, data analysis, and healthcare management. Representing providers, health plans, vendors and other industry partners. © 2018 CAQH, All Rights Reserved. 9
Why Does the CAQH Index Matter? § Tracking is critical to monitoring progress and identifying specific opportunities for further improvement. § Industry-wide transition to electronic transactions is a critical component to a modern healthcare system. Reduces unnecessary healthcare costs. > More than $31 billion spent annually by healthcare providers alone conducting basic business transactions with health plans. > Electronic transactions are significantly less expensive than manual. Eases provider administrative burden. > Electronic transactions require less staff time. Reduces friction between providers and health plans. > Needed information communicated more rapidly and easily, reducing errors. Complements revolution of clinical use of Health IT. > Results in more efficient, integrated healthcare ecosystem. © 2018 CAQH, All Rights Reserved. 10
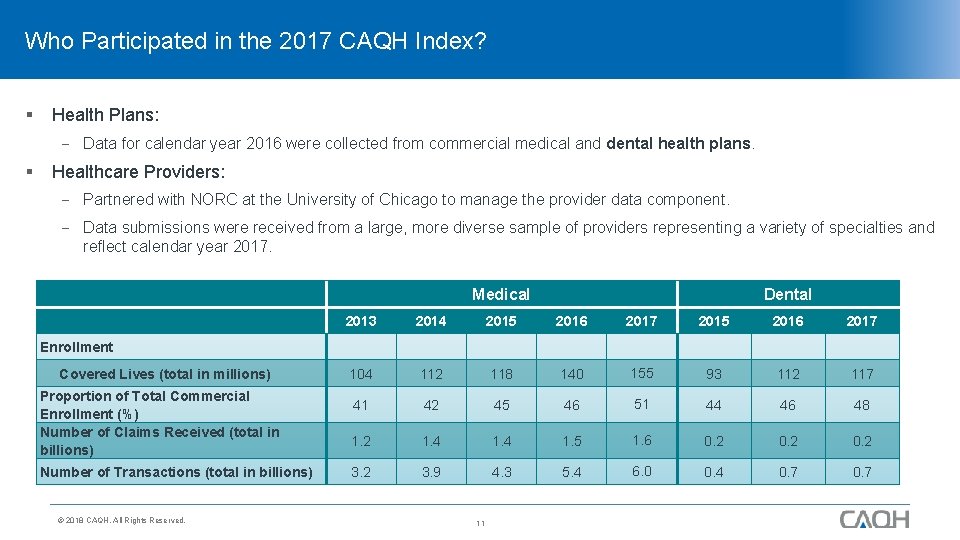
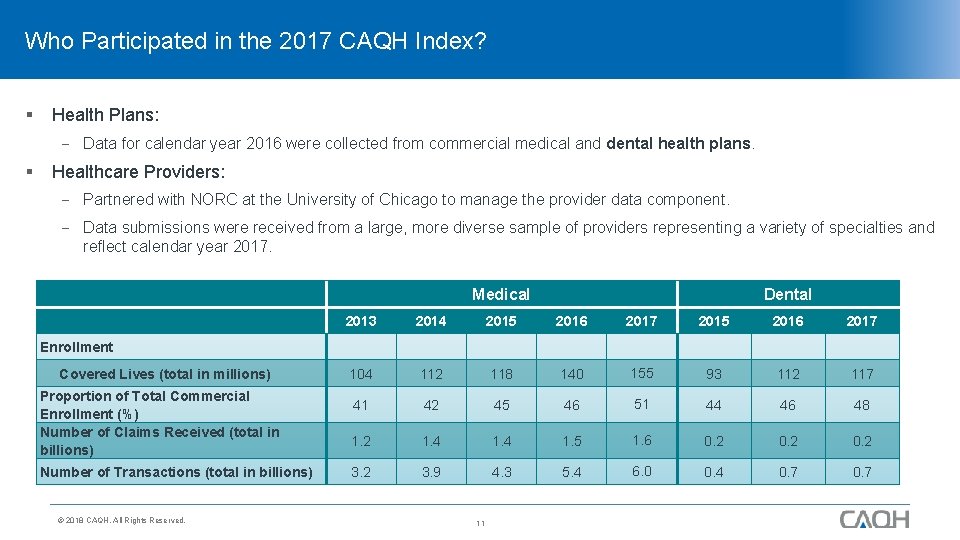
Who Participated in the 2017 CAQH Index? § Health Plans: Data for calendar year 2016 were collected from commercial medical and dental health plans. § Healthcare Providers: Partnered with NORC at the University of Chicago to manage the provider data component. Data submissions were received from a large, more diverse sample of providers representing a variety of specialties and reflect calendar year 2017. Medical Dental 2013 2014 2015 2016 2017 104 112 118 140 155 93 112 117 41 42 45 46 51 44 46 48 1. 2 1. 4 1. 5 1. 6 0. 2 3. 9 4. 3 5. 4 6. 0 0. 4 0. 7 Enrollment Covered Lives (total in millions) Proportion of Total Commercial Enrollment (%) Number of Claims Received (total in billions) Number of Transactions (total in billions) © 2018 CAQH, All Rights Reserved. 11
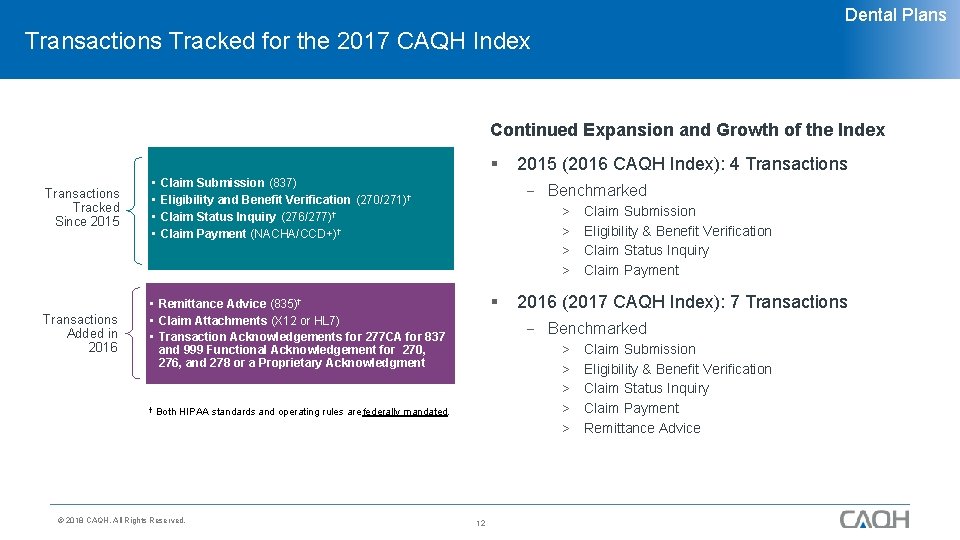
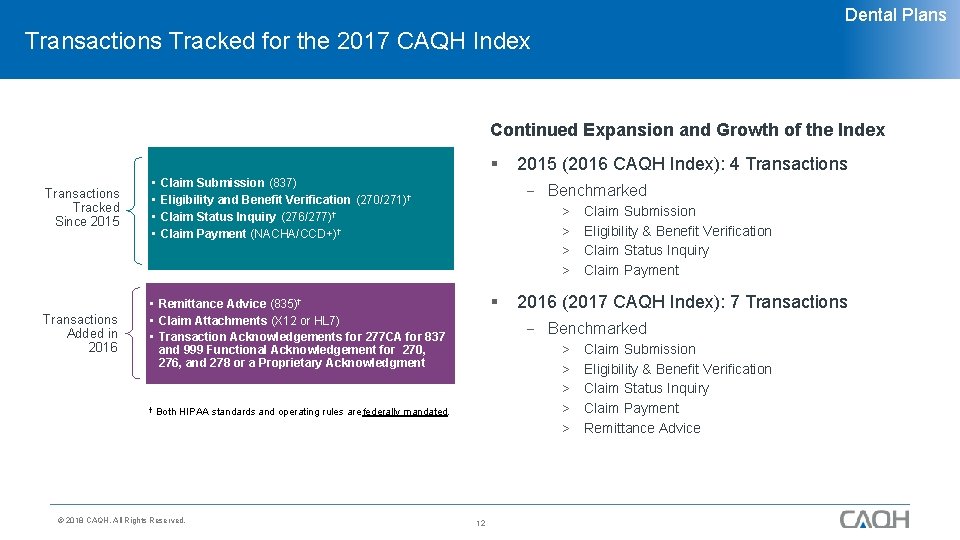
Dental Plans Transactions Tracked for the 2017 CAQH Index Continued Expansion and Growth of the Index § Transactions Tracked Since 2015 • • Transactions Added in 2016 • Remittance Advice (835)† • Claim Attachments (X 12 or HL 7) • Transaction Acknowledgements for 277 CA for 837 and 999 Functional Acknowledgement for 270, 276, and 278 or a Proprietary Acknowledgment † Claim Submission (837) Eligibility and Benefit Verification (270/271)† Claim Status Inquiry (276/277)† Claim Payment (NACHA/CCD+)† Benchmarked > > § Claim Submission Eligibility & Benefit Verification Claim Status Inquiry Claim Payment 2016 (2017 CAQH Index): 7 Transactions Benchmarked > > > Both HIPAA standards and operating rules are federally mandated. © 2018 CAQH, All Rights Reserved. 2015 (2016 CAQH Index): 4 Transactions 12 Claim Submission Eligibility & Benefit Verification Claim Status Inquiry Claim Payment Remittance Advice
When Will the 2017 CAQH Index Be Available? § Information shared with you today is embargoed until June 13, 2018, including for the media. § Webinar in mid-June. § Rolling out promotional emails soon. © 2018 CAQH, All Rights Reserved. 13

Adoption of Electronic Transactions © 2018 CAQH, All Rights Reserved. 14
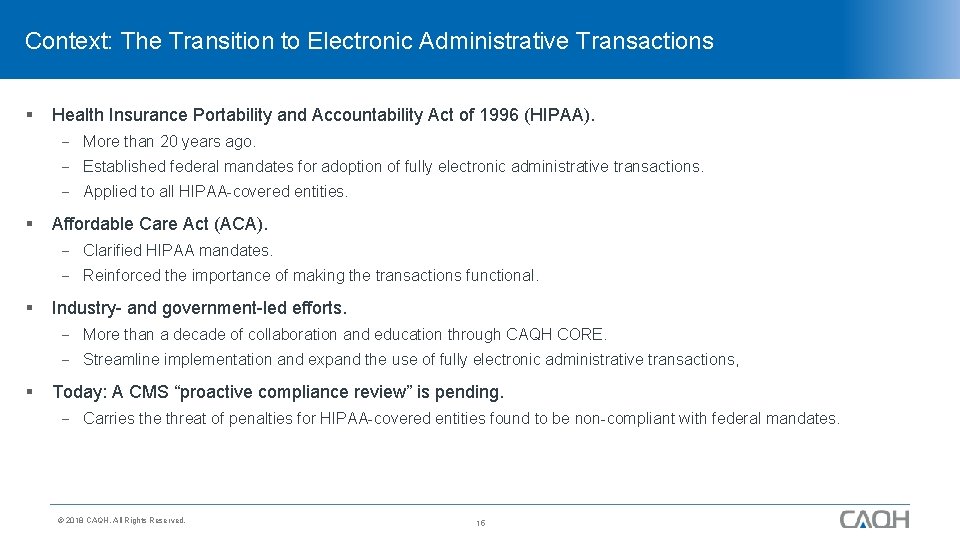
Context: The Transition to Electronic Administrative Transactions § Health Insurance Portability and Accountability Act of 1996 (HIPAA). More than 20 years ago. Established federal mandates for adoption of fully electronic administrative transactions. Applied to all HIPAA-covered entities. § Affordable Care Act (ACA). Clarified HIPAA mandates. Reinforced the importance of making the transactions functional. § Industry- and government-led efforts. More than a decade of collaboration and education through CAQH CORE. Streamline implementation and expand the use of fully electronic administrative transactions, § Today: A CMS “proactive compliance review” is pending. Carries the threat of penalties for HIPAA-covered entities found to be non-compliant with federal mandates. © 2018 CAQH, All Rights Reserved. 15
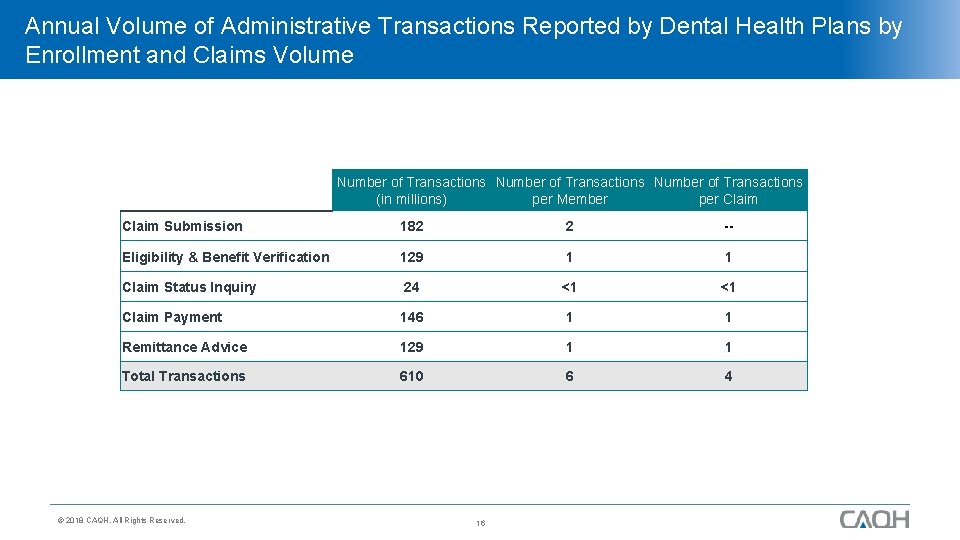
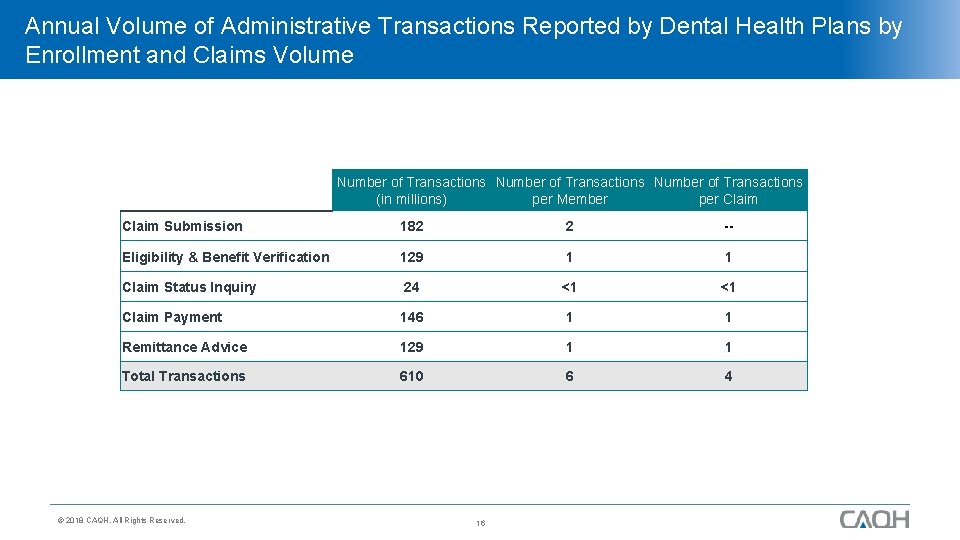
Annual Volume of Administrative Transactions Reported by Dental Health Plans by Enrollment and Claims Volume Number of Transactions (in millions) per Member per Claim Submission 182 2 -- Eligibility & Benefit Verification 129 1 1 Claim Status Inquiry 24 <1 <1 Claim Payment 146 1 1 Remittance Advice 129 1 1 Total Transactions 610 6 4 © 2018 CAQH, All Rights Reserved. 16
Data Overview § Participating health plans reported the volume of administrative transactions by type and method. § Transactions are classified as: Fully Electronic – conducted using the adopted HIPAA standard. Partially Electronic – conducted using web portals or interactive voice response (IVR) systems. Fully Manual – conducted using telephone, fax, or postal mail. © 2018 CAQH, All Rights Reserved. 17
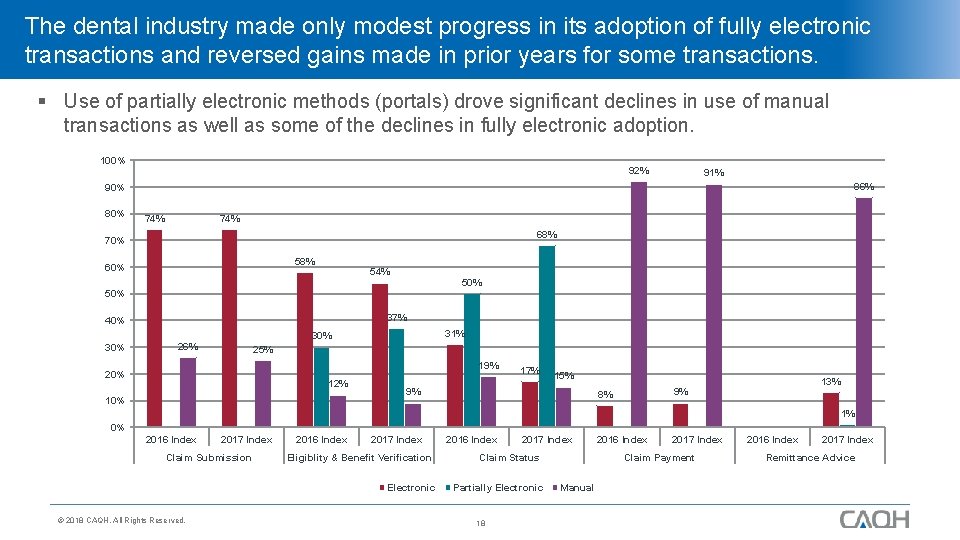
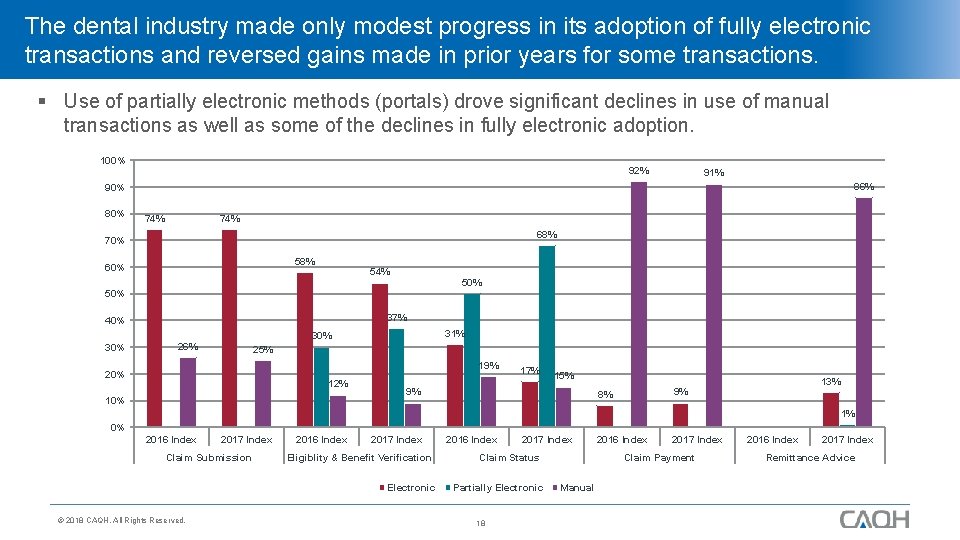
The dental industry made only modest progress in its adoption of fully electronic transactions and reversed gains made in prior years for some transactions. § Use of partially electronic methods (portals) drove significant declines in use of manual transactions as well as some of the declines in fully electronic adoption. 100% 92% 91% 86% 90% 80% 74% 68% 70% 58% 60% 54% 50% 37% 40% 31% 30% 26% 25% 19% 20% 12% 10% 17% 15% 9% 13% 9% 8% 1% 0% 2016 Index 2017 Index Claim Submission 2016 Index 2017 Index Eligiblity & Benefit Verification Electronic © 2018 CAQH, All Rights Reserved. 2016 Index 2017 Index Claim Status Partially Electronic 18 2016 Index 2017 Index Claim Payment Manual 2016 Index 2017 Index Remittance Advice
The dental industry has not yet caught up with its medical peers for any of the five transactions tracked for both sectors. § On average, dental industry adoption was still 30 percentage points lower than adoption levels by medical plans and providers. § The transaction with the highest level of fully electronic adoption was claim submission. § Similar to medical health plans, portals played an important role in the 2017 Index for dental health plans. There were increases in use of portals for eligibility and benefit verifications and claim status inquiries and corresponding decreases in adoption of fully electronic and use of manual for these two transactions. § Electronic claim status, payment and remittance advice all lag that of medical with a 43 to 52 percentage-point difference. © 2018 CAQH, All Rights Reserved. 19
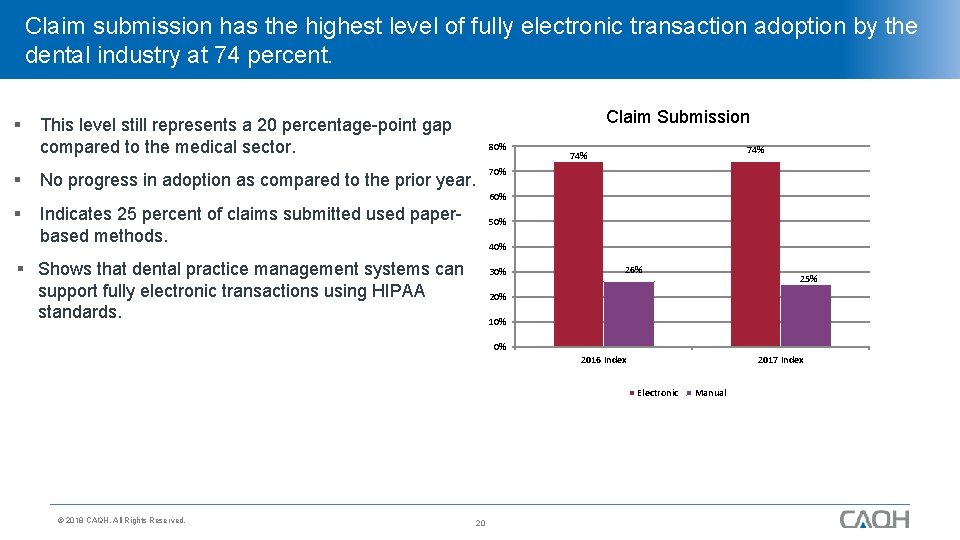
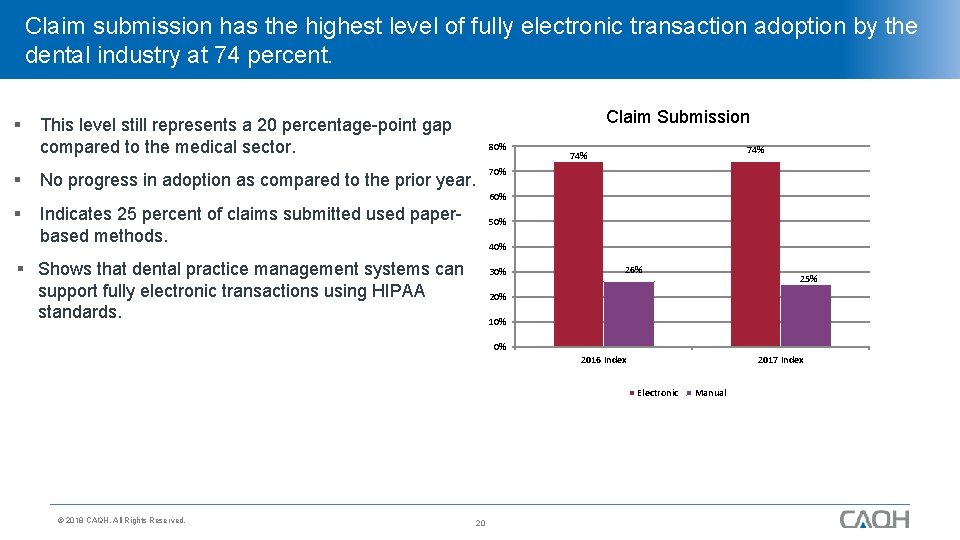
Claim submission has the highest level of fully electronic transaction adoption by the dental industry at 74 percent. § Claim Submission This level still represents a 20 percentage-point gap compared to the medical sector. § No progress in adoption as compared to the prior year. § Indicates 25 percent of claims submitted used paperbased methods. 80% 74% 70% 60% 50% 40% § Shows that dental practice management systems can support fully electronic transactions using HIPAA standards. 30% 26% 25% 20% 10% 0% 2016 Index 2017 Index Electronic © 2018 CAQH, All Rights Reserved. 20 Manual
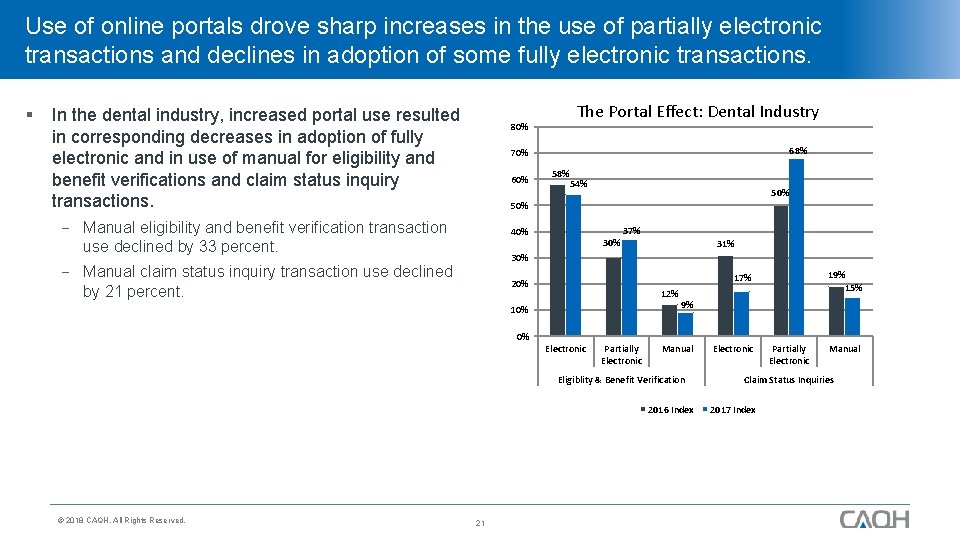
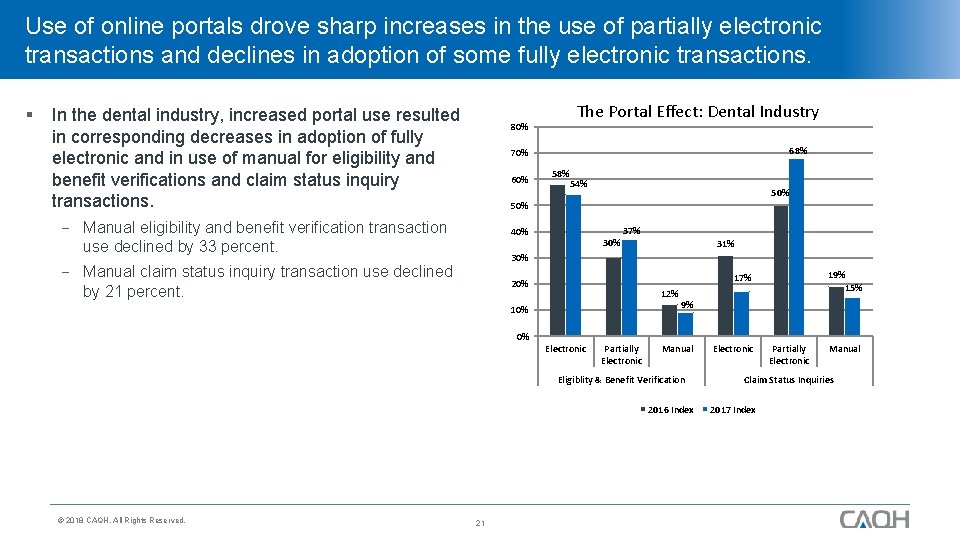
Use of online portals drove sharp increases in the use of partially electronic transactions and declines in adoption of some fully electronic transactions. § In the dental industry, increased portal use resulted in corresponding decreases in adoption of fully electronic and in use of manual for eligibility and benefit verifications and claim status inquiry transactions. 80% The Portal Effect: Dental Industry 68% 70% 60% 58% 54% 50% Manual eligibility and benefit verification transaction use declined by 33 percent. 37% 40% 31% 30% Manual claim status inquiry transaction use declined by 21 percent. 19% 15% 17% 20% 12% 10% 9% 0% Electronic Partially Electronic Manual Eligiblity & Benefit Verification 2016 Index © 2018 CAQH, All Rights Reserved. 21 Electronic Partially Electronic Manual Claim Status Inquiries 2017 Index
Portals may be a bridge, a barrier or have no effect at all on the ultimate success of the transition to fully electronic administrative transactions. § Portals had a mixed effect in the medical industry. § For one transaction (Remittance Advice), portal use increased, while adoption of fully electronic transactions remained steady and fully manual declined. § For another (Prior Authorization), portal use increased as adoption of fully electronic transactions declined and use of manual remained steady. § For two others (Claim Status/Eligibility & Benefits Verification), a more hopeful sign: A small decline in portal use was matched by an increase in fully electronic adoption. © 2018 CAQH, All Rights Reserved. 22
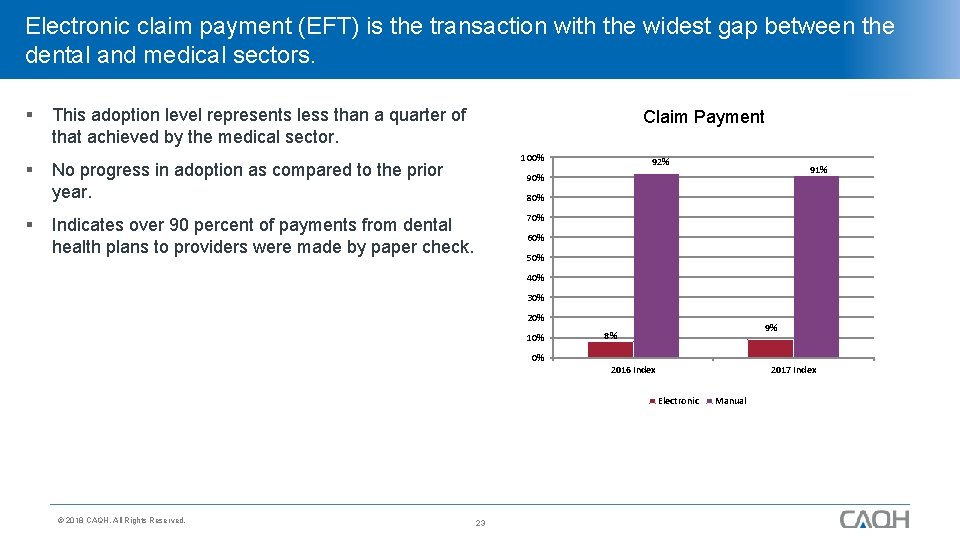
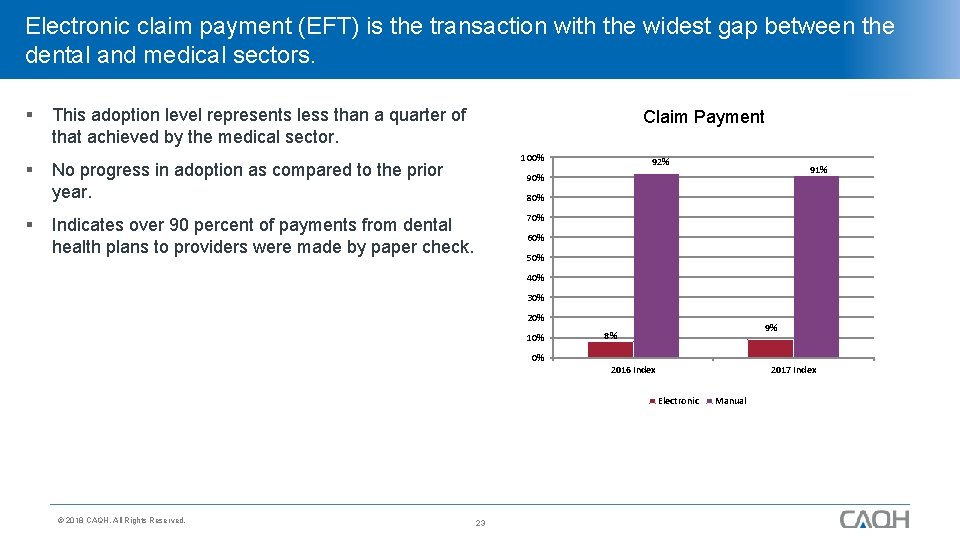
Electronic claim payment (EFT) is the transaction with the widest gap between the dental and medical sectors. § § § This adoption level represents less than a quarter of that achieved by the medical sector. Claim Payment 100% No progress in adoption as compared to the prior year. 92% 91% 90% 80% 70% Indicates over 90 percent of payments from dental health plans to providers were made by paper check. 60% 50% 40% 30% 20% 10% 9% 8% 0% 2016 Index 2017 Index Electronic © 2018 CAQH, All Rights Reserved. 23 Manual
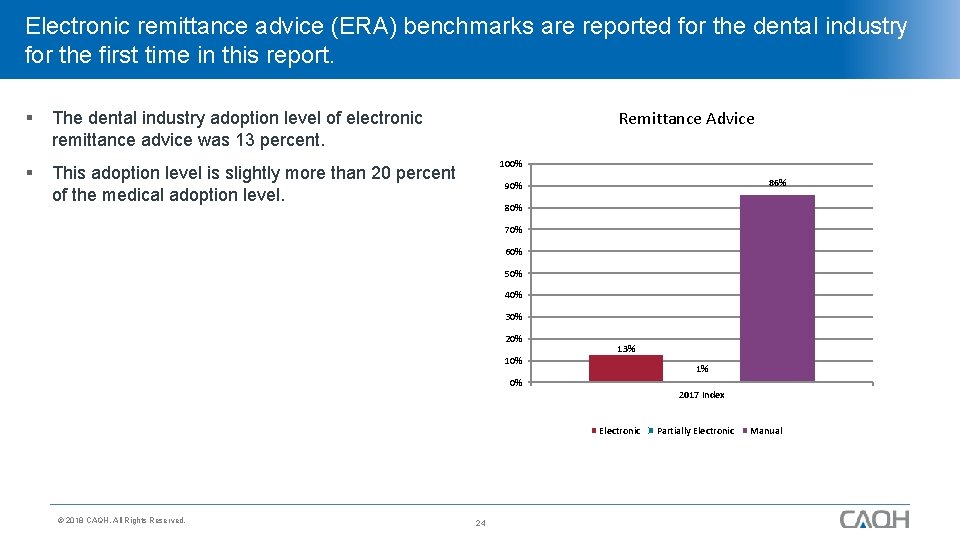
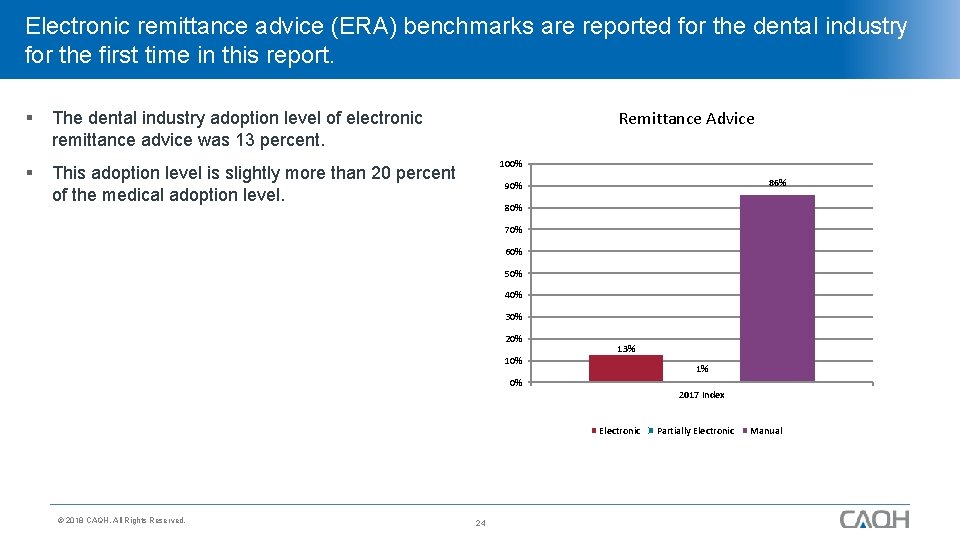
Electronic remittance advice (ERA) benchmarks are reported for the dental industry for the first time in this report. § The dental industry adoption level of electronic remittance advice was 13 percent. § This adoption level is slightly more than 20 percent of the medical adoption level. Remittance Advice 100% 86% 90% 80% 70% 60% 50% 40% 30% 20% 13% 1% 0% 2017 Index Electronic © 2018 CAQH, All Rights Reserved. 24 Partially Electronic Manual
Cost of Electronic Transactions © 2018 CAQH, All Rights Reserved. 25
2017 Index Industry Cost Estimates § In the prior year, the 2016 CAQH Index expanded cost estimates to include: Cost per transaction for seven of the twelve medical health plan transactions with the addition of costs for claim attachments. First time reporting initial four transactions for dental health plans. Claim Submission Eligibility and Benefit Verification Claim Status Inquiries Claim Payment Potential savings opportunity for dental health plans and providers for four of the seven transactions for medical health plans. § The 2017 CAQH Index expands even further: Cost per transaction for remittance advice added for dental health plans. Deeper exploration and more robust analysis of the practice management system and provider-facing clearinghouse vendor fees and pricing models. © 2018 CAQH, All Rights Reserved. 26
Producing Cost Per Transaction Estimates for Health Plans § § Participating health plans provide cost-per-transaction estimates, which are weighted and averaged. Health plans use a variety of internal reporting systems to estimate fully loaded, direct cost for each transaction factoring: Staffing. > Number of employees working on specific transaction types. > Salaries associated with employees. Transactions. > Volume of transactions by type and mode. > Percent of time spent processing each transaction type by mode. Vendor Fees. © 2018 CAQH, All Rights Reserved. 27
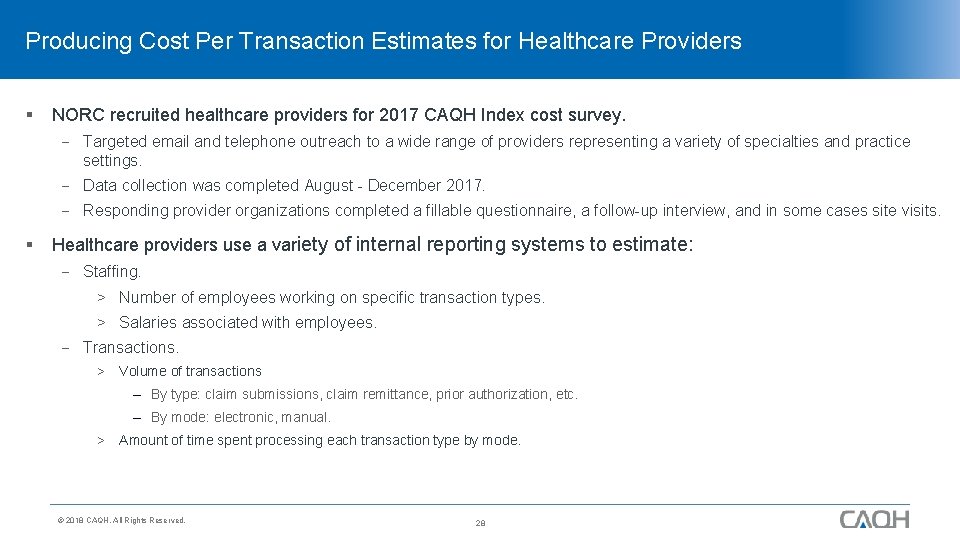
Producing Cost Per Transaction Estimates for Healthcare Providers § NORC recruited healthcare providers for 2017 CAQH Index cost survey. Targeted email and telephone outreach to a wide range of providers representing a variety of specialties and practice settings. Data collection was completed August - December 2017. Responding provider organizations completed a fillable questionnaire, a follow-up interview, and in some cases site visits. § Healthcare providers use a variety of internal reporting systems to estimate: Staffing. > Number of employees working on specific transaction types. > Salaries associated with employees. Transactions. > Volume of transactions – By type: claim submissions, claim remittance, prior authorization, etc. – By mode: electronic, manual. > Amount of time spent processing each transaction type by mode. © 2018 CAQH, All Rights Reserved. 28
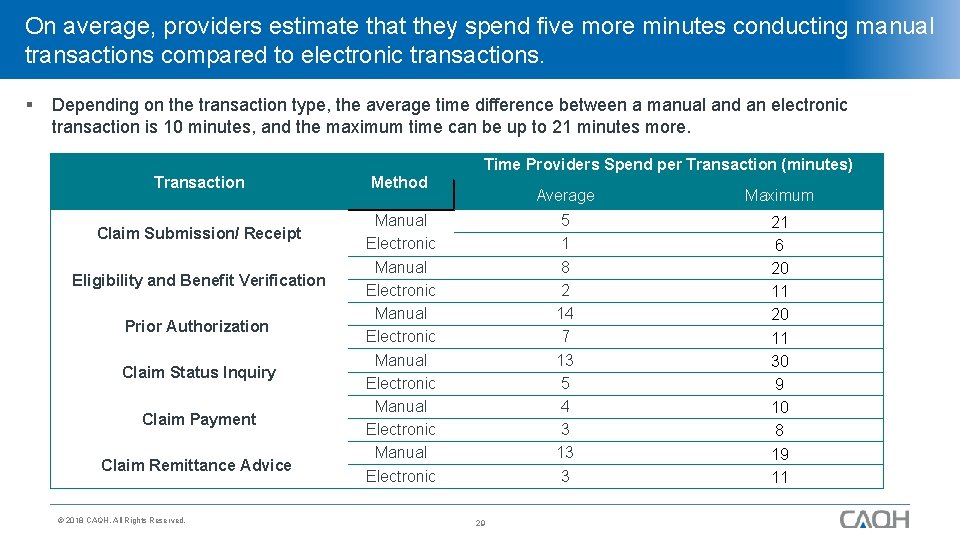
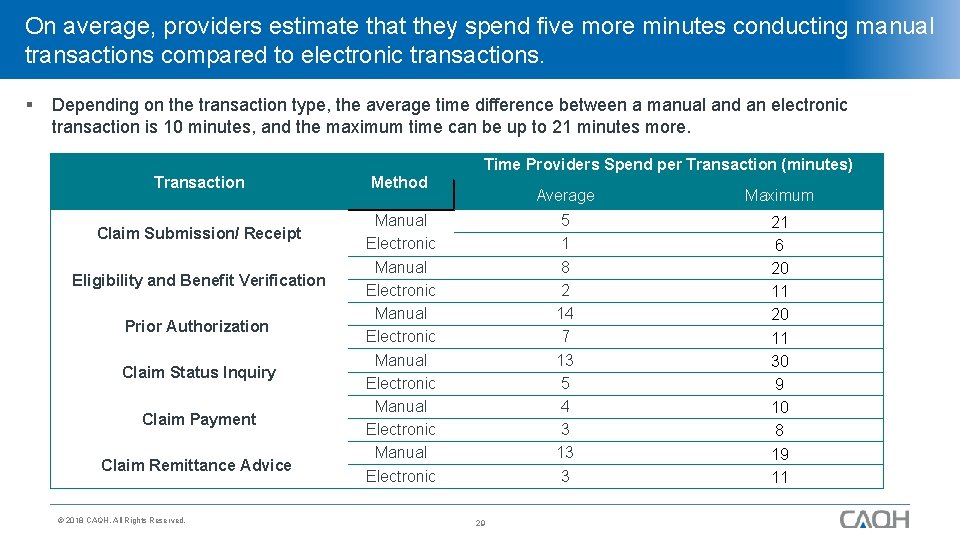
On average, providers estimate that they spend five more minutes conducting manual transactions compared to electronic transactions. § Depending on the transaction type, the average time difference between a manual and an electronic transaction is 10 minutes, and the maximum time can be up to 21 minutes more. Time Providers Spend per Transaction (minutes) Transaction Claim Submission/ Receipt Eligibility and Benefit Verification Prior Authorization Claim Status Inquiry Claim Payment Claim Remittance Advice © 2018 CAQH, All Rights Reserved. Method Manual Electronic Manual Electronic 29 Average Maximum 5 1 8 2 14 7 13 5 4 3 13 3 21 6 20 11 30 9 10 8 19 11
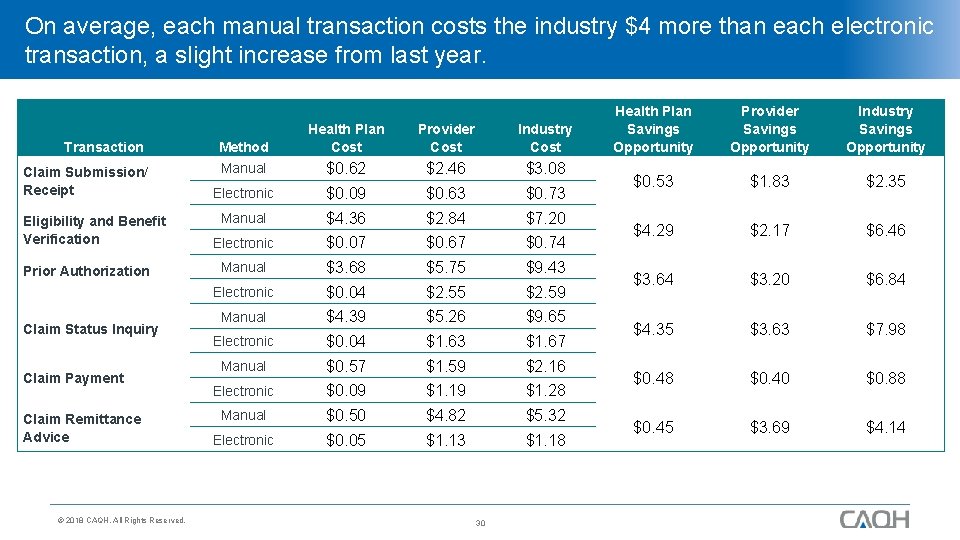
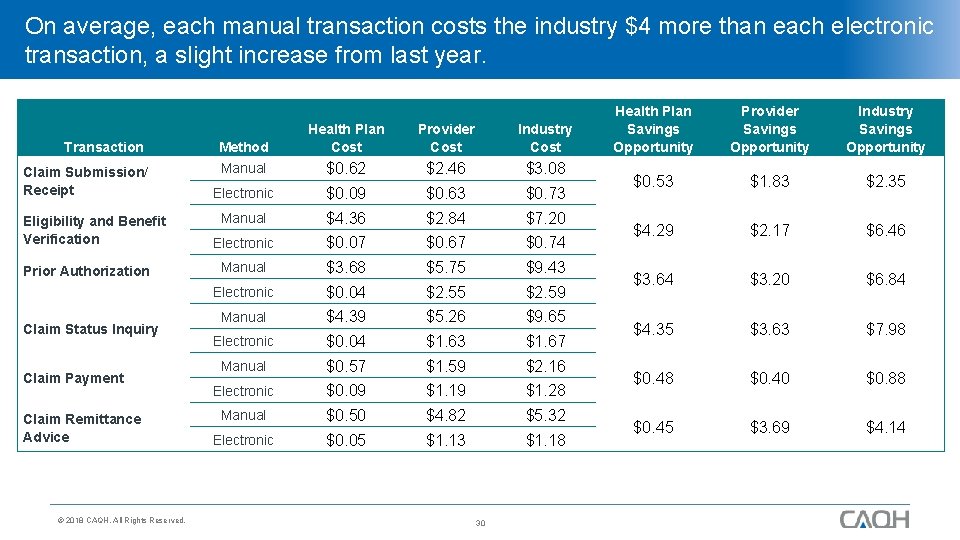
On average, each manual transaction costs the industry $4 more than each electronic transaction, a slight increase from last year. Transaction Claim Submission/ Receipt Eligibility and Benefit Verification Prior Authorization Claim Status Inquiry Claim Payment Claim Remittance Advice © 2018 CAQH, All Rights Reserved. Method Health Plan Cost Provider Cost Industry Cost Manual $0. 62 $2. 46 $3. 08 Electronic $0. 09 $0. 63 $0. 73 Manual $4. 36 $2. 84 $7. 20 Electronic $0. 07 $0. 67 $0. 74 Manual $3. 68 $5. 75 $9. 43 Electronic $0. 04 $2. 55 $2. 59 Manual $4. 39 $5. 26 $9. 65 Electronic $0. 04 $1. 63 $1. 67 Manual $0. 57 $1. 59 $2. 16 Electronic $0. 09 $1. 19 $1. 28 Manual $0. 50 $4. 82 $5. 32 Electronic $0. 05 $1. 13 $1. 18 30 Health Plan Savings Opportunity Provider Savings Opportunity Industry Savings Opportunity $0. 53 $1. 83 $2. 35 $4. 29 $2. 17 $6. 46 $3. 64 $3. 20 $6. 84 $4. 35 $3. 63 $7. 98 $0. 40 $0. 88 $0. 45 $3. 69 $4. 14
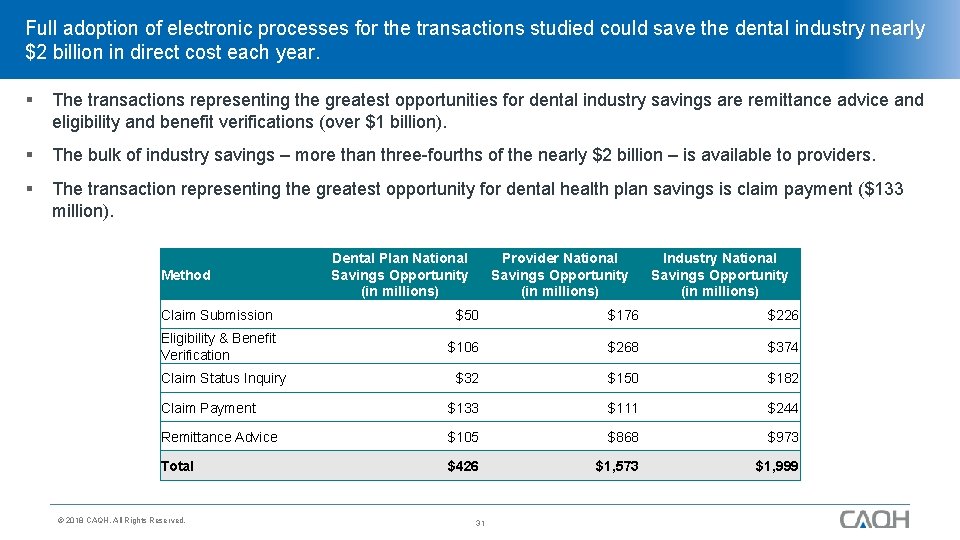
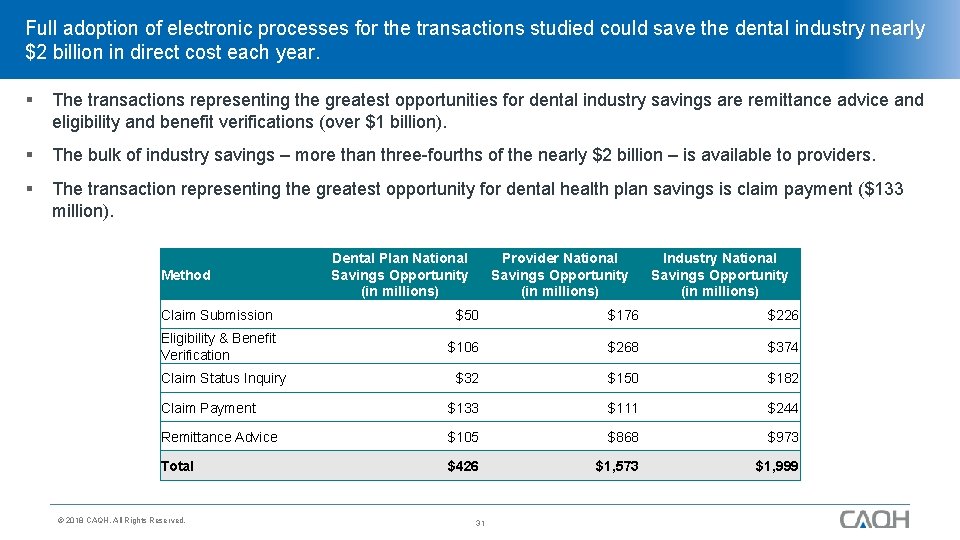
Full adoption of electronic processes for the transactions studied could save the dental industry nearly $2 billion in direct cost each year. § The transactions representing the greatest opportunities for dental industry savings are remittance advice and eligibility and benefit verifications (over $1 billion). § The bulk of industry savings – more than three-fourths of the nearly $2 billion – is available to providers. § The transaction representing the greatest opportunity for dental health plan savings is claim payment ($133 million). Method Dental Plan National Savings Opportunity (in millions) Provider National Savings Opportunity (in millions) Industry National Savings Opportunity (in millions) Claim Submission $50 $176 $226 Eligibility & Benefit Verification $106 $268 $374 $32 $150 $182 Claim Payment $133 $111 $244 Remittance Advice $105 $868 $973 Total $426 $1, 573 $1, 999 Claim Status Inquiry © 2018 CAQH, All Rights Reserved. 31
The 2017 Index features expanded research on practice management system and clearinghouse vendor costs. § Partnered with Milliman to complete an environmental scan of pricing models of PMS and provider clearinghouse vendors. The information was acquired through systematic review of available web resources and requests for pricing and quotes from 16 vendors. A brief overview will be noted in the 2016 Index Report, and actual estimates of vendor costs will be integrated into overhead costs for providers in 2017. § Describes the complex nature of vendor pricing models. § Surveys vendor support for electronic administrative transactions and finds gaps. © 2018 CAQH, All Rights Reserved. 32
Participate in the 2018 CAQH Index § Health plans and healthcare providers (practices and health systems) can participate in the 2018 Index by submitting data for calendar year 2017. § Vendors may also participate in the Index by: Sharing the call for data submissions with healthcare providers in your network. Completing the new 2018 vendor cost survey. § For more information: Contact Reid Kiser (explorations@caqh. org). Visit www. caqhindex. org. § All participants receive benchmark reports, which provide important information specific to your organization: How your company compares to the industry at-large. How much time and effort your staff spends on electronic and manual transactions. Potential for efficiency gains by further transition to electronic transactions. © 2018 CAQH, All Rights Reserved. 33
Questions? © 2018 CAQH, All Rights Reserved. 34
Value of CAQH CORE Operating Rules to Dental Industry May 1, 2018 Taha Anjarwalla CAQH CORE Manager © 2018 CAQH, All Rights Reserved.
About CAQH CORE © 2018 CAQH, All Rights Reserved. 36

CAQH CORE Mission & Vision MISSION VISION DESIGNATION Drive the creation and adoption of healthcare operating rules that support standards, accelerate interoperability and align administrative and clinical activities among providers, payers and consumers. An industry-wide facilitator of a trusted, simple and sustainable healthcare data exchange that evolves and aligns with market needs. Named by Secretary of HHS to be national author for operating rules to cover all HIPAA-mandated transactions. © 2018 CAQH, All Rights Reserved. 37
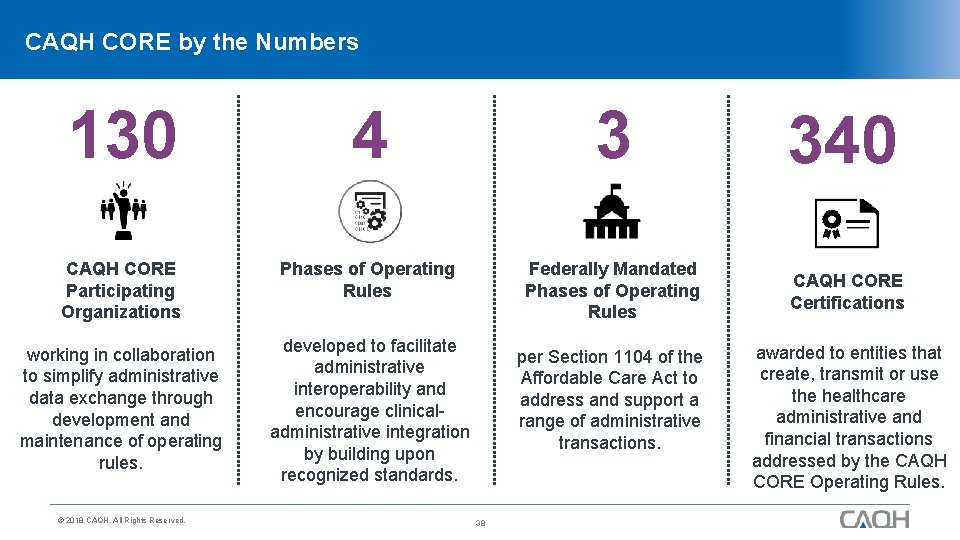
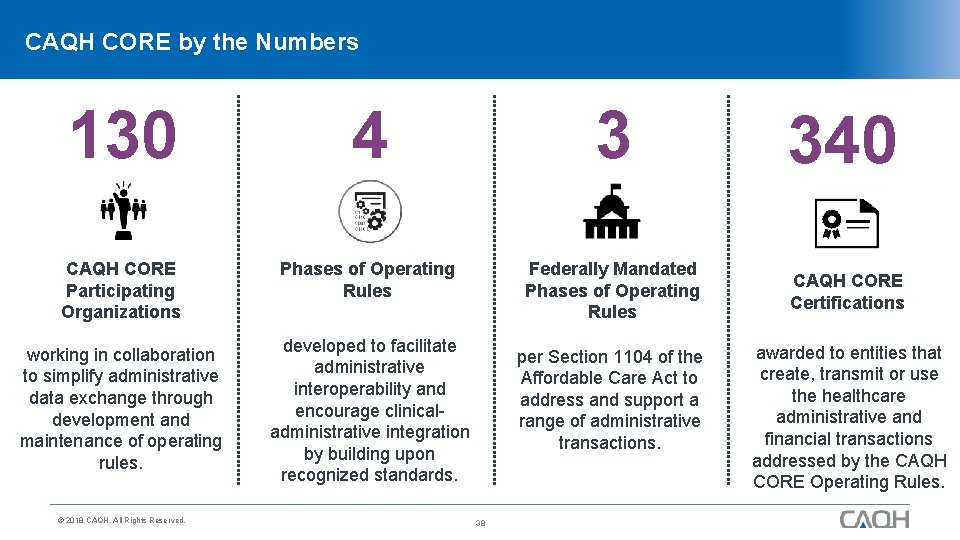
CAQH CORE by the Numbers 130 4 3 340 CAQH CORE Participating Organizations Phases of Operating Rules Federally Mandated Phases of Operating Rules CAQH CORE Certifications working in collaboration to simplify administrative data exchange through development and maintenance of operating rules. developed to facilitate administrative interoperability and encourage clinicaladministrative integration by building upon recognized standards. © 2018 CAQH, All Rights Reserved. per Section 1104 of the Affordable Care Act to address and support a range of administrative transactions. 38 awarded to entities that create, transmit or use the healthcare administrative and financial transactions addressed by the CAQH CORE Operating Rules.
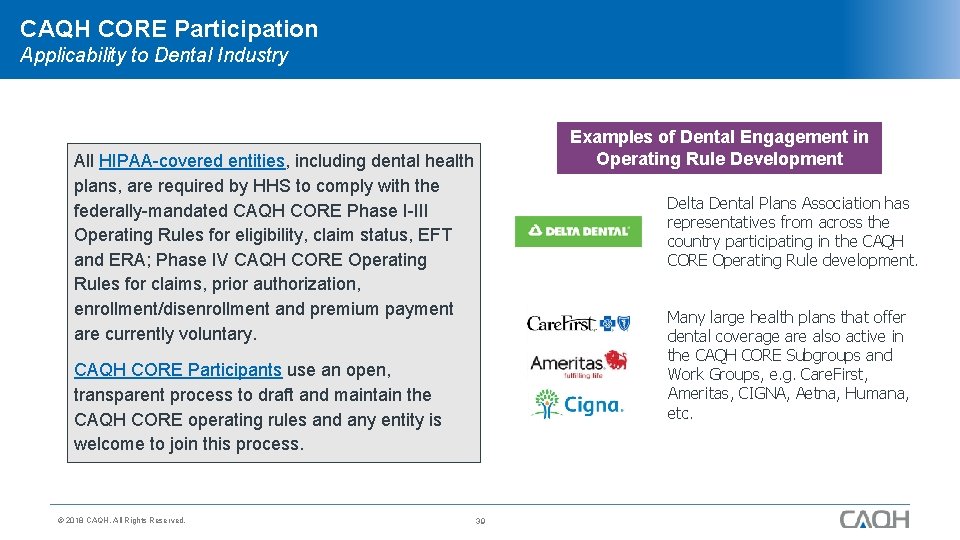
CAQH CORE Participation Applicability to Dental Industry All HIPAA-covered entities, including dental health plans, are required by HHS to comply with the federally-mandated CAQH CORE Phase I-III Operating Rules for eligibility, claim status, EFT and ERA; Phase IV CAQH CORE Operating Click to add Rules for claims, prior authorization, enrollment/disenrollment and premium payment are currently voluntary. CAQH CORE Participants use an open, transparent process to draft and maintain the CAQH CORE operating rules and any entity is welcome to join this process. © 2018 CAQH, All Rights Reserved. 39 Examples of Dental Engagement in Operating Rule Development title Delta Dental Plans Association has representatives from across the country participating in the CAQH CORE Operating Rule development. Many large health plans that offer dental coverage are also active in the CAQH CORE Subgroups and Work Groups, e. g. Care. First, Ameritas, CIGNA, Aetna, Humana, etc.
Value of CAQH CORE Operating Rules © 2018 CAQH, All Rights Reserved. 40
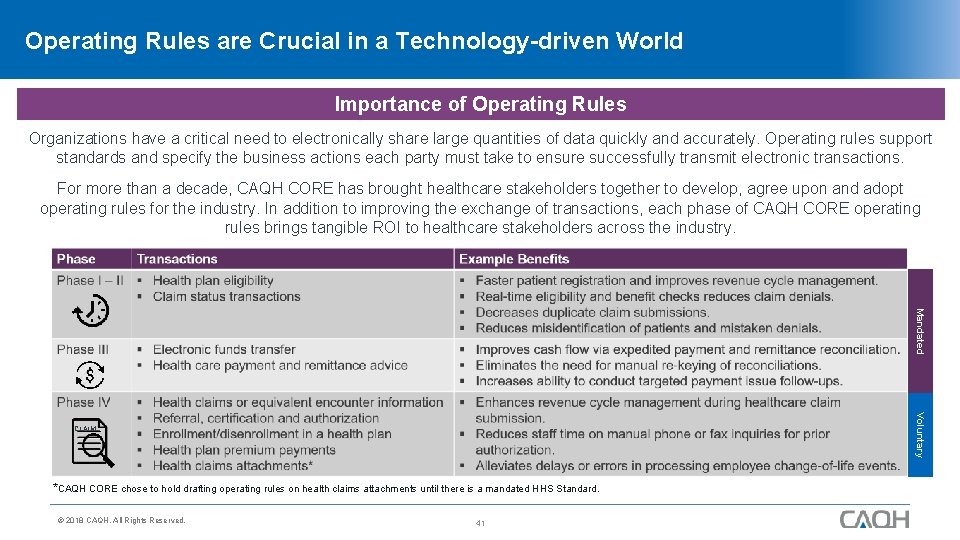
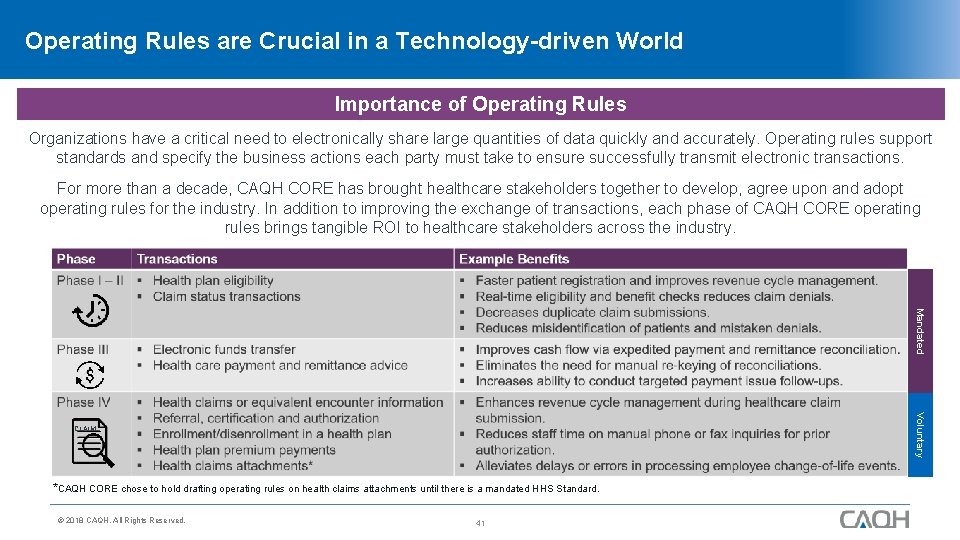
Operating Rules are Crucial in a Technology-driven World Importance of Operating Rules Organizations have a critical need to electronically share large quantities of data quickly and accurately. Operating rules support standards and specify the business actions each party must take to ensure successfully transmit electronic transactions. For more than a decade, CAQH CORE has brought healthcare stakeholders together to develop, agree upon and adopt operating rules for the industry. In addition to improving the exchange of transactions, each phase of CAQH CORE operating rules brings tangible ROI to healthcare stakeholders across the industry. Mandated Voluntary CLAIM *CAQH CORE chose to hold drafting operating rules on health claims attachments until there is a mandated HHS Standard. © 2018 CAQH, All Rights Reserved. 41
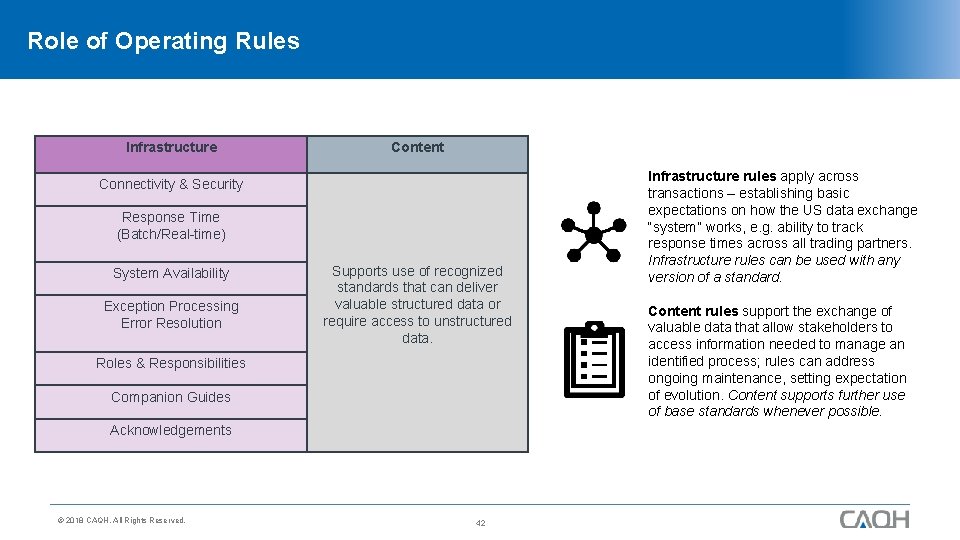
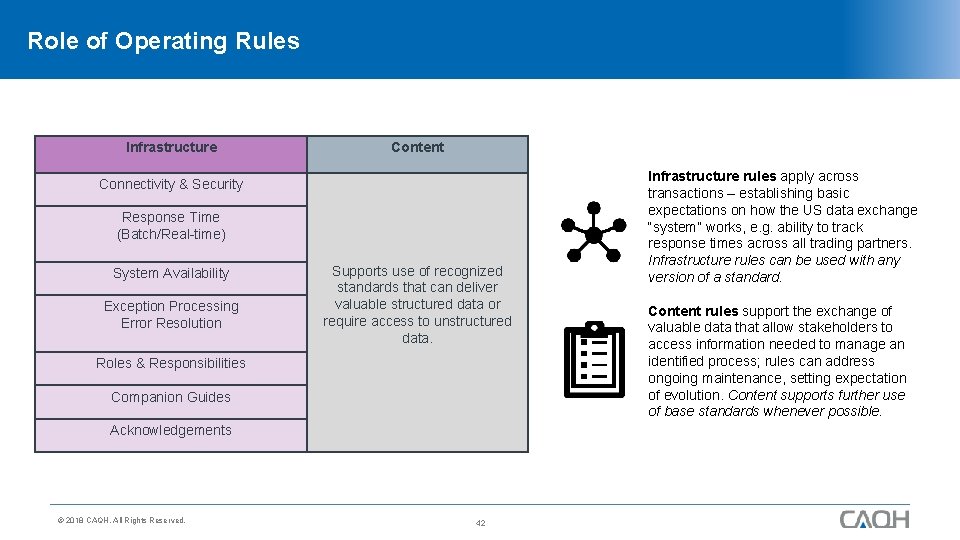
Role of Operating Rules Infrastructure Content Connectivity & Security Response Time (Batch/Real-time) System Availability Exception Processing Error Resolution Supports use of recognized standards that can deliver valuable structured data or require access to unstructured data. Roles & Responsibilities Companion Guides Acknowledgements © 2018 CAQH, All Rights Reserved. 42 Infrastructure rules apply across transactions – establishing basic expectations on how the US data exchange “system” works, e. g. ability to track response times across all trading partners. Infrastructure rules can be used with any version of a standard. Content rules support the exchange of valuable data that allow stakeholders to access information needed to manage an identified process; rules can address ongoing maintenance, setting expectation of evolution. Content supports further use of base standards whenever possible.
Voluntary CORE Certification © 2018 CAQH, All Rights Reserved. 43
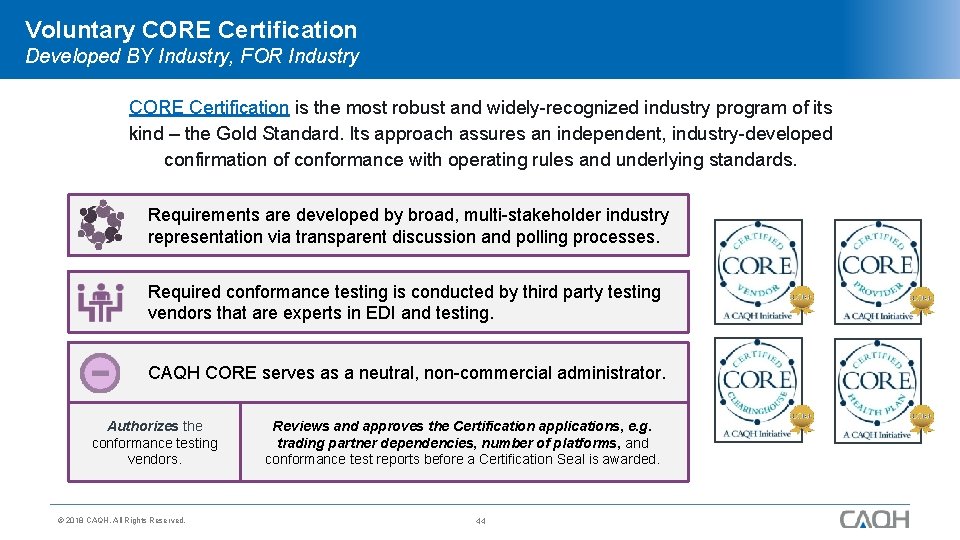
Voluntary CORE Certification Developed BY Industry, FOR Industry CORE Certification is the most robust and widely-recognized industry program of its kind – the Gold Standard. Its approach assures an independent, industry-developed confirmation of conformance with operating rules and underlying standards. Requirements are developed by broad, multi-stakeholder industry representation via transparent discussion and polling processes. Required conformance testing is conducted by third party testing vendors that are experts in EDI and testing. CAQH CORE serves as a neutral, non-commercial administrator. Authorizes the conformance testing vendors. © 2018 CAQH, All Rights Reserved. Reviews and approves the Certification applications, e. g. trading partner dependencies, number of platforms, and conformance test reports before a Certification Seal is awarded. 44
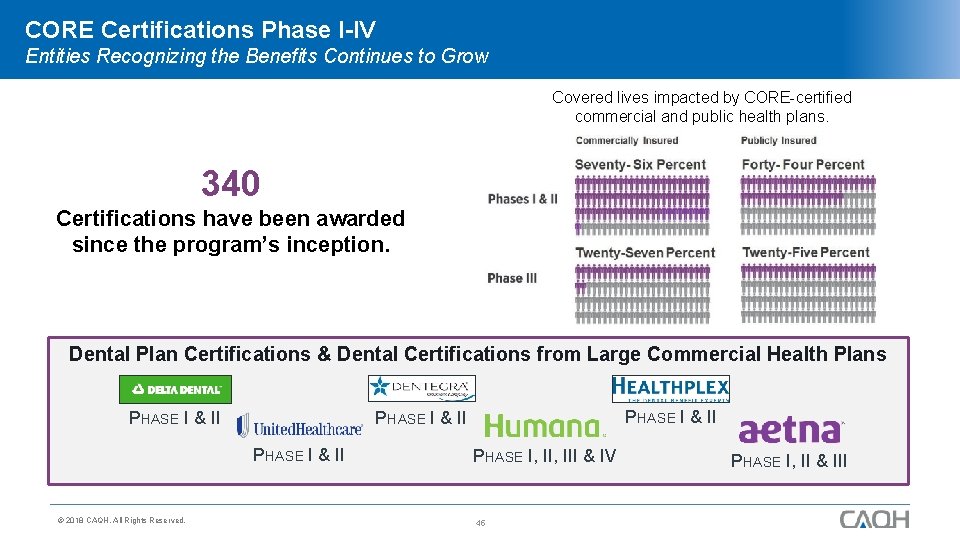
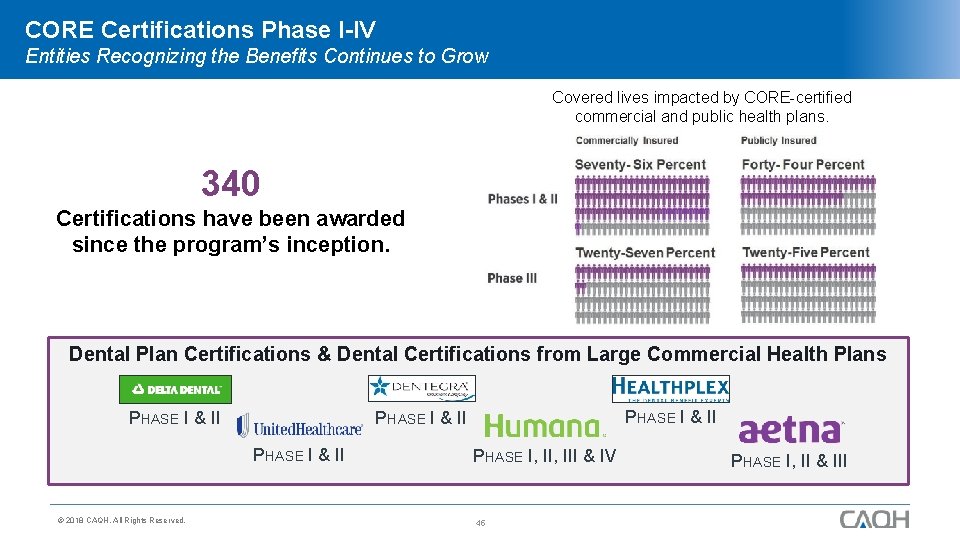
CORE Certifications Phase I-IV Entities Recognizing the Benefits Continues to Grow Covered lives impacted by CORE-certified commercial and public health plans. 340 Certifications have been awarded since the program’s inception. Dental Plan Certifications & Dental Certifications from Large Commercial Health Plans PHASE I & II © 2018 CAQH, All Rights Reserved. PHASE I & II PHASE I, III & IV 45 PHASE I, II & III
Voluntary CORE Certification Benefits for Dental Industry Positions dental industry as leaders in administrative efficiencies. Ensures real-time access to eligibility information for beneficiaries. Allows dental providers to improve their revenue cycles by standardizing claim adjustment code combinations and making it easier to receive payments via EFT. Lowers cost within claim processing systems, including costly and cumbersome paper checks. Enhances opportunity for interoperability between providers and dental payers Improves relationships between providers, payers, and vendors. Gives assurance of conformance with federally mandated operating rules. © 2018 CAQH, All Rights Reserved. 46
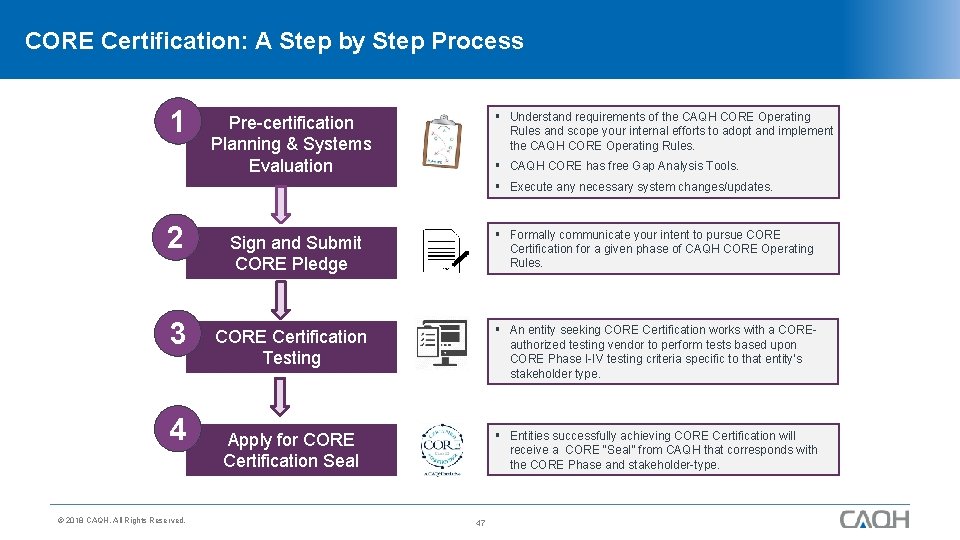
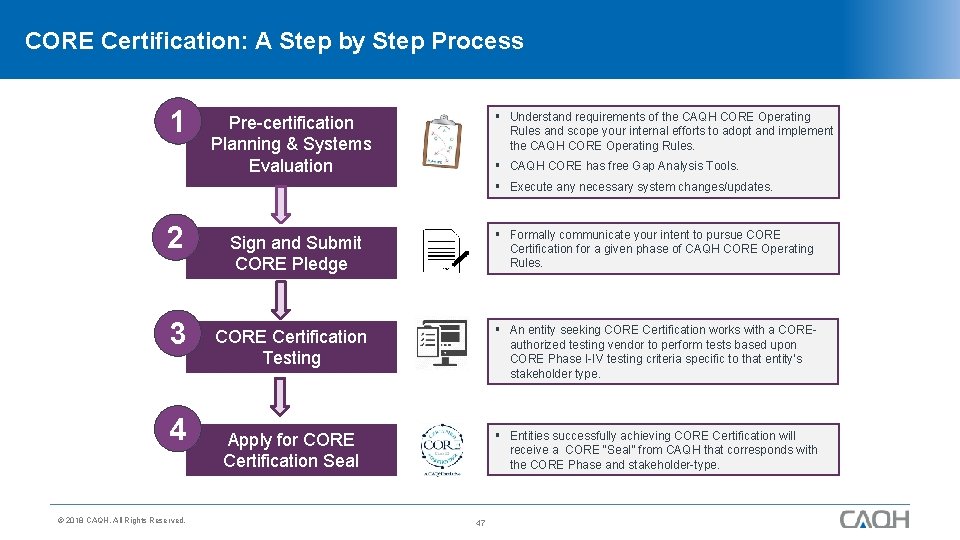
CORE Certification: A Step by Step Process 1 § Understand requirements of the CAQH CORE Operating Rules and scope your internal efforts to adopt and implement the CAQH CORE Operating Rules. Pre-certification Planning & Systems Evaluation § CAQH CORE has free Gap Analysis Tools. § Execute any necessary system changes/updates. 2 3 4 © 2018 CAQH, All Rights Reserved. § Formally communicate your intent to pursue CORE Certification for a given phase of CAQH CORE Operating Rules. Sign and Submit CORE Pledge CORE Certification Testing § An entity seeking CORE Certification works with a COREauthorized testing vendor to perform tests based upon CORE Phase I-IV testing criteria specific to that entity’s stakeholder type. Apply for CORE Certification Seal § Entities successfully achieving CORE Certification will receive a CORE “Seal” from CAQH that corresponds with the CORE Phase and stakeholder-type. 47
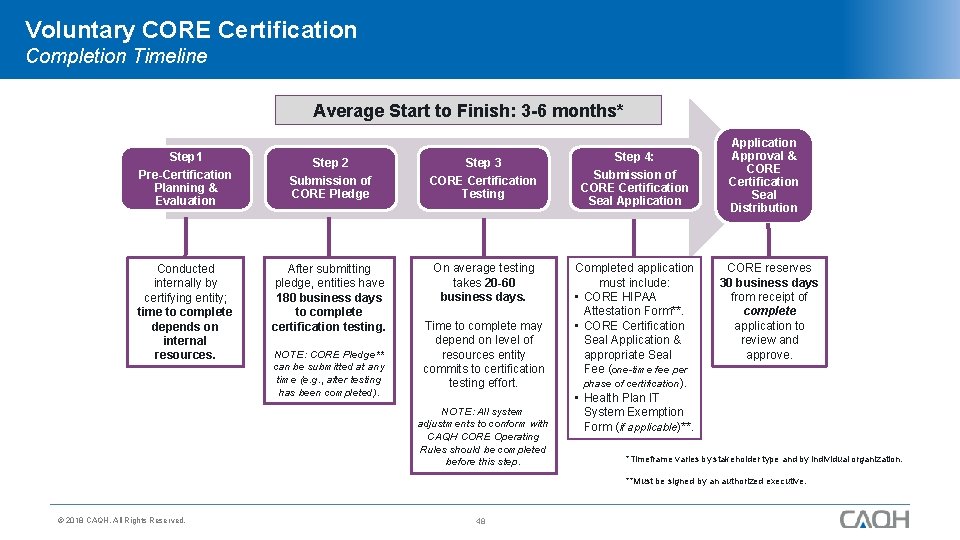
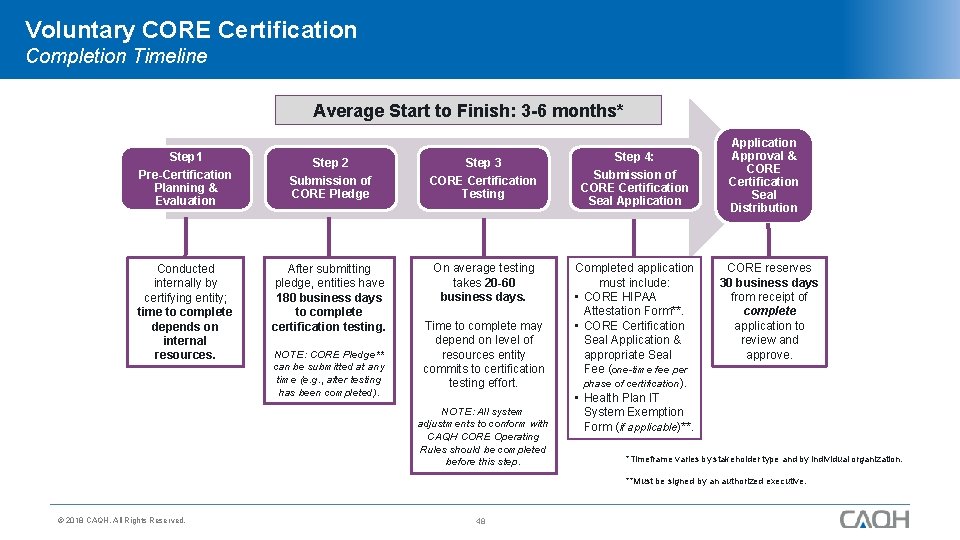
Voluntary CORE Certification Completion Timeline Average Start to Finish: 3 -6 months* Step 1 Pre-Certification Planning & Evaluation Conducted internally by certifying entity; time to complete depends on internal resources. Step 2 Step 3 Submission of CORE Pledge CORE Certification Testing After submitting pledge, entities have 180 business days to complete certification testing. On average testing takes 20 -60 business days. NOTE: CORE Pledge** can be submitted at any time (e. g. , after testing has been completed). Time to complete may depend on level of resources entity commits to certification testing effort. NOTE: All system adjustments to conform with CAQH CORE Operating Rules should be completed before this step. Step 4: Submission of CORE Certification Seal Application Completed application must include: • CORE HIPAA Attestation Form**. • CORE Certification Seal Application & appropriate Seal Fee (one-time fee per phase of certification). • Health Plan IT System Exemption Form (if applicable)**. Application Approval & CORE Certification Seal Distribution CORE reserves 30 business days from receipt of complete application to review and approve. *Timeframe varies by stakeholder type and by individual organization. **Must be signed by an authorized executive. © 2018 CAQH, All Rights Reserved. 48
Voluntary CORE Certification: Resources § CAQH CORE Analysis and Planning Guides: Identifies system/software gaps and helps create a project plan to complete any necessary system remediation. § CAQH CORE Certification Test Suites & CAQH CORE Master Test Bed Data: Identifies stakeholder-specific conformance testing requirements of the CAQH CORE Operating Rules for voluntary CAQH CORE Certification. § CAQH CORE staff support via phone (202. 517. 0375) and email (CORE@CAQH. org). § Free resources from Edifecs, CORE-authorized Testing Vendor (Info. Core. Certification@edifecs. com). § CAQH CORE FAQs: Addresses questions pertaining to technical rule requirements and stakeholder specific implementation on the CAQH CORE Operating Rules. § e-Learning Tools: Provides interactive dashboards and modules to learn about Voluntary CORE Certification. © 2018 CAQH, All Rights Reserved. 49
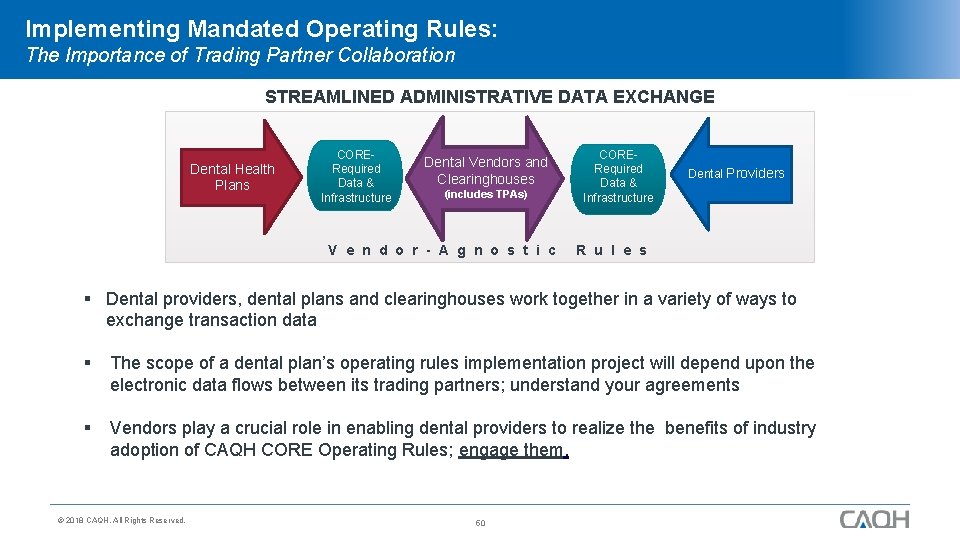
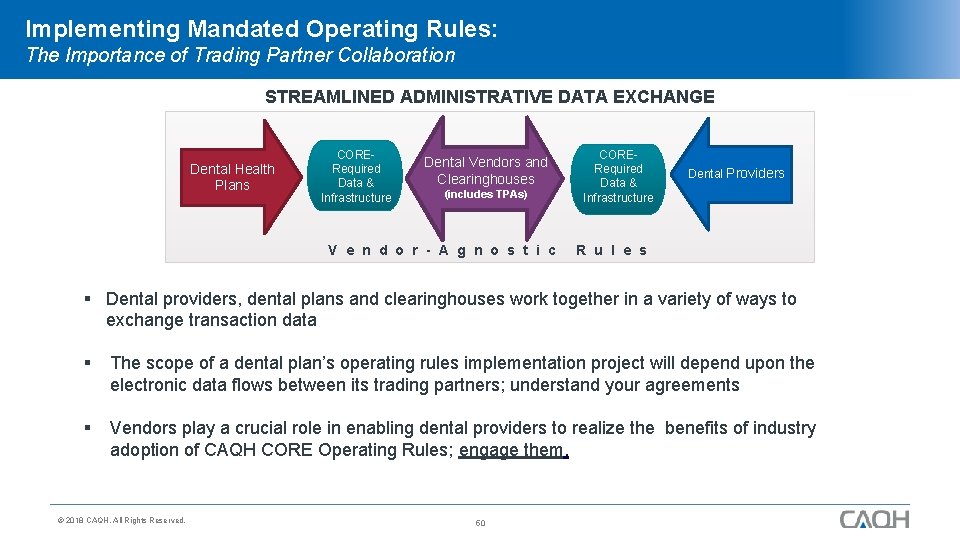
Implementing Mandated Operating Rules: The Importance of Trading Partner Collaboration STREAMLINED ADMINISTRATIVE DATA EXCHANGE Dental Health Plans CORERequired Data & Infrastructure Dental Vendors and Clearinghouses (includes TPAs) V e n d o r - A g n o s t i c CORERequired Data & Infrastructure Dental Providers R u l e s § Dental providers, dental plans and clearinghouses work together in a variety of ways to exchange transaction data § The scope of a dental plan’s operating rules implementation project will depend upon the electronic data flows between its trading partners; understand your agreements § Vendors play a crucial role in enabling dental providers to realize the benefits of industry adoption of CAQH CORE Operating Rules; engage them. © 2018 CAQH, All Rights Reserved. 50
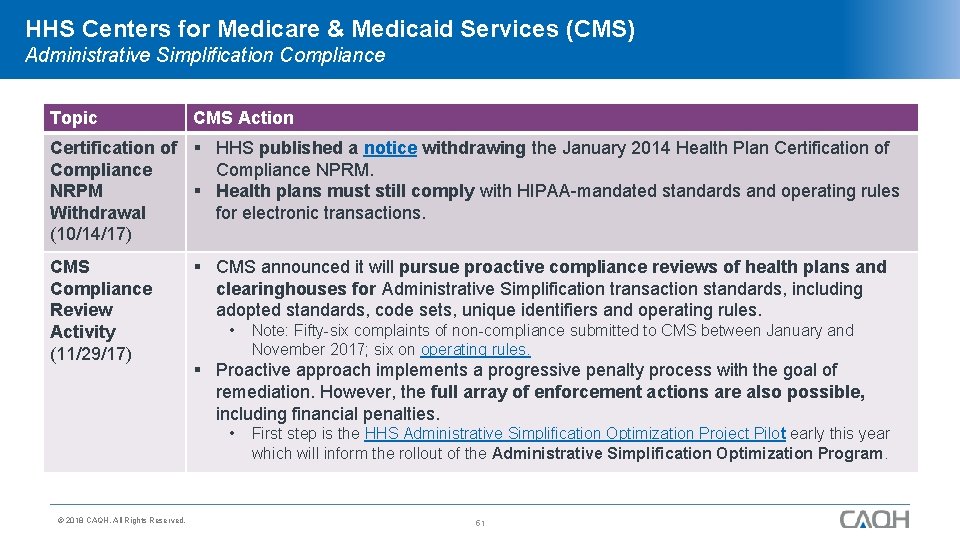
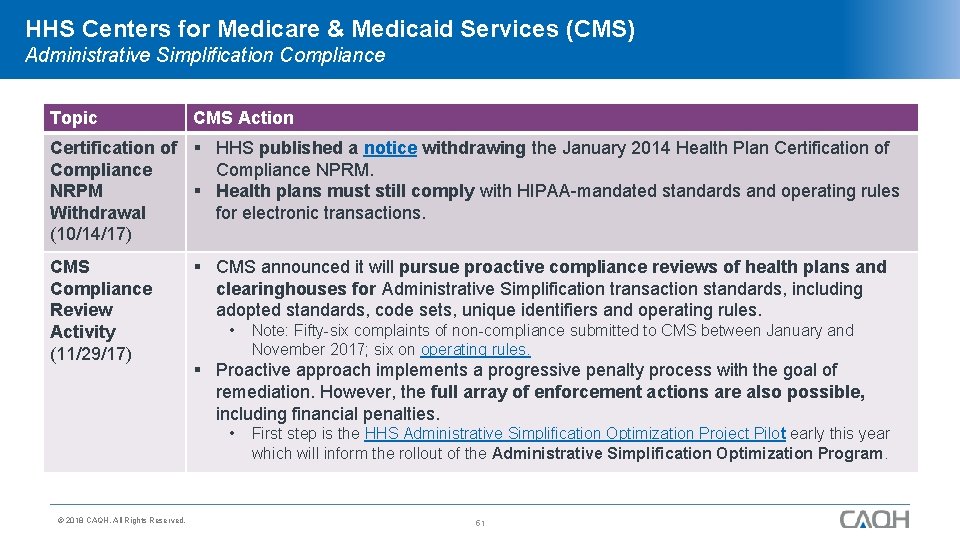
HHS Centers for Medicare & Medicaid Services (CMS) Administrative Simplification Compliance Topic CMS Action Certification of § HHS published a notice withdrawing the January 2014 Health Plan Certification of Compliance NPRM. NRPM § Health plans must still comply with HIPAA-mandated standards and operating rules Withdrawal for electronic transactions. (10/14/17) CMS Compliance Review Activity (11/29/17) § CMS announced it will pursue proactive compliance reviews of health plans and clearinghouses for Administrative Simplification transaction standards, including adopted standards, code sets, unique identifiers and operating rules. • § Proactive approach implements a progressive penalty process with the goal of remediation. However, the full array of enforcement actions are also possible, including financial penalties. • © 2018 CAQH, All Rights Reserved. Note: Fifty-six complaints of non-compliance submitted to CMS between January and November 2017; six on operating rules. First step is the HHS Administrative Simplification Optimization Project Pilot early this year which will inform the rollout of the Administrative Simplification Optimization Program. 51
Demonstrate Due Diligence with CORE Certification Prepare for Potential Compliance Reviews Conformance with Federal Mandates CORE Certification Prepares Industry for Compliance Reviews § Compliance with Administrative Simplification requirements yields benefits to the healthcare industry; $9. 4 billion in potential savings according to the CAQH Index. § CORE Certification helps organizations demonstrate, document and certify conformance with federally mandated operating rules and standards, positioning entities for potential external audits and penalties. § Healthcare providers, health plans, payers and other HIPAA -covered entities must comply with operating rules and adopted standards according to federal regulation. § It allows the industry to monitor, regulate and correct itself enabling preparation for enforcement audits and associated penalties where instances of non-compliance could cost up to $1. 5 million. § CORE Certification provides a way for organizations to demonstrate their IT system or product is operating in conformance with applicable requirements of a specific phase(s) of the CAQH CORE Operating Rules. © 2018 CAQH, All Rights Reserved. 52
CAQH CORE Future Focus © 2018 CAQH, All Rights Reserved. 53
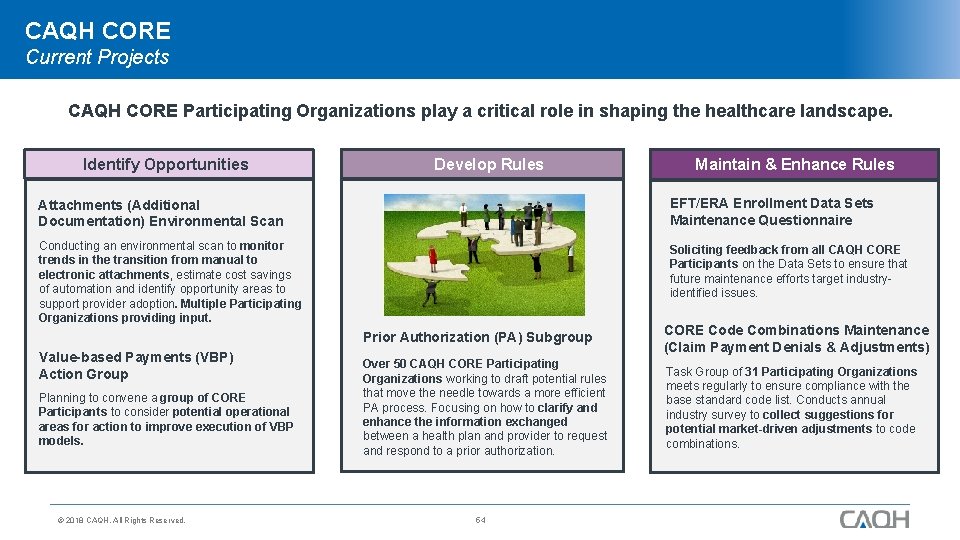
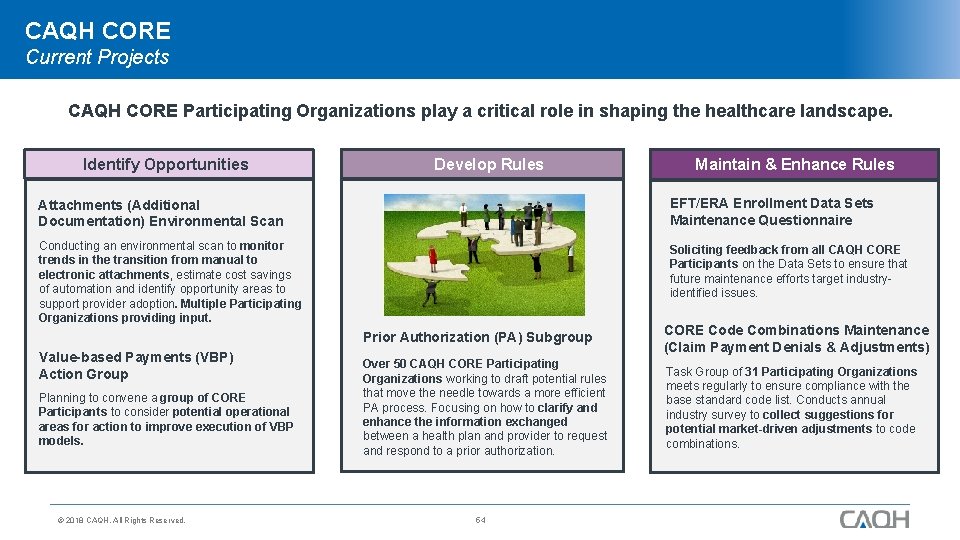
CAQH CORE Current Projects CAQH CORE Participating Organizations play a critical role in shaping the healthcare landscape. Identify Opportunities Develop Rules Maintain & Enhance Rules Attachments (Additional Documentation) Environmental Scan EFT/ERA Enrollment Data Sets Maintenance Questionnaire Conducting an environmental scan to monitor trends in the transition from manual to electronic attachments, estimate cost savings of automation and identify opportunity areas to support provider adoption. Multiple Participating Organizations providing input. Soliciting feedback from all CAQH CORE Participants on the Data Sets to ensure that future maintenance efforts target industryidentified issues. Value-based Payments (VBP) Action Group Planning to convene a group of CORE Participants to consider potential operational areas for action to improve execution of VBP models. © 2018 CAQH, All Rights Reserved. Prior Authorization (PA) Subgroup CORE Code Combinations Maintenance (Claim Payment Denials & Adjustments) Over 50 CAQH CORE Participating Organizations working to draft potential rules that move the needle towards a more efficient PA process. Focusing on how to clarify and enhance the information exchanged between a health plan and provider to request and respond to a prior authorization. Task Group of 31 Participating Organizations meets regularly to ensure compliance with the base standard code list. Conducts annual industry survey to collect suggestions for potential market-driven adjustments to code combinations. 54
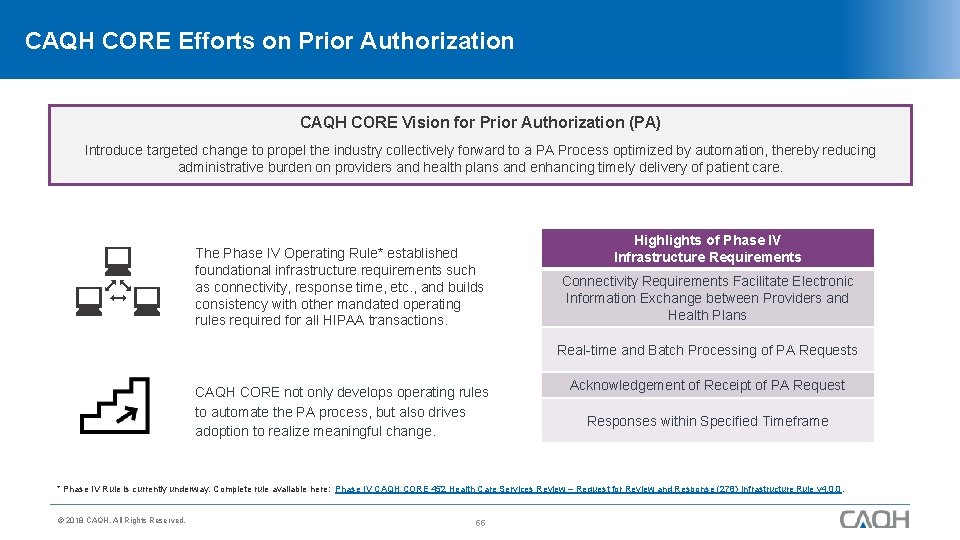
CAQH CORE Efforts on Prior Authorization CAQH CORE Vision for Prior Authorization (PA) Introduce targeted change to propel the industry collectively forward to a PA Process optimized by automation, thereby reducing administrative burden on providers and health plans and enhancing timely delivery of patient care. The Phase IV Operating Rule* established foundational infrastructure requirements such as connectivity, response time, etc. , and builds consistency with other mandated operating rules required for all HIPAA transactions. Highlights of Phase IV Infrastructure Requirements Connectivity Requirements Facilitate Electronic Information Exchange between Providers and Health Plans Real-time and Batch Processing of PA Requests CAQH CORE not only develops operating rules to automate the PA process, but also drives adoption to realize meaningful change. Acknowledgement of Receipt of PA Request Responses within Specified Timeframe * Phase IV Rule is currently underway. Complete rule available here: Phase IV CAQH CORE 452 Health Care Services Review – Request for Review and Response (278) Infrastructure Rule v 4. 0. 0. © 2018 CAQH, All Rights Reserved. 55
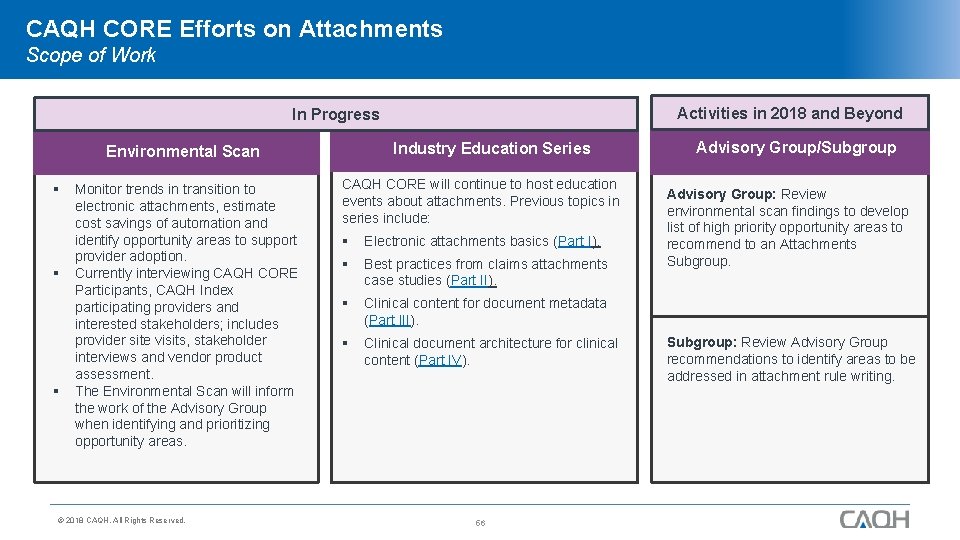
CAQH CORE Efforts on Attachments Scope of Work Activities in 2018 and Beyond In Progress Industry Education Series Environmental Scan § § § Monitor trends in transition to electronic attachments, estimate cost savings of automation and identify opportunity areas to support provider adoption. Currently interviewing CAQH CORE Participants, CAQH Index participating providers and interested stakeholders; includes provider site visits, stakeholder interviews and vendor product assessment. The Environmental Scan will inform the work of the Advisory Group when identifying and prioritizing opportunity areas. © 2018 CAQH, All Rights Reserved. CAQH CORE will continue to host education events about attachments. Previous topics in series include: § Electronic attachments basics (Part I). § Best practices from claims attachments case studies (Part II). § Clinical content for document metadata (Part III). § Clinical document architecture for clinical content (Part IV). 56 Advisory Group/Subgroup Advisory Group: Review environmental scan findings to develop list of high priority opportunity areas to recommend to an Attachments Subgroup: Review Advisory Group recommendations to identify areas to be addressed in attachment rule writing.
New CAQH CORE Report: All Together Now Applying the Lessons of FFS to Streamline Adoption of VBP The report analyzes operational challenges that may slow or add costs to the implementation of value-based payment. The research found that industry collaboration is needed to minimize variations and identified opportunity areas that, if improved, would smooth implementation. Contents of Report 5 Opportunity Areas 9 Recommendations § Data Quality & Standardization § Interoperability § Patient Risk Stratification § Provider Attribution § Quality Measurement Includes nine recommendations and strategies to address challenges which may be implemented by CAQH CORE and/or others. 12+ Candidate Orgs Identifies over a dozen candidate organizations – industry organizations and leaders – to successfully propel VBP operations. © 2018 CAQH, All Rights Reserved. 57
Become a CAQH CORE Participating Organization to Maximize Benefits! Healthcare administration is rapidly changing. Be a part of CAQH CORE’s mission to drive the creation and adoption of new healthcare operating rules. Represent your organization. Work with others around the industry. 2018 Priorities – special content available only to CAQH CORE Participating Organizations. Communicate to industry partners and with your organization’s leadership. VPB | ATTACHMENTS | PRIOR AUTH. Present on CAQH CORE education sessions. Click here for more information on joining CAQH CORE as well as a complete list of Participating Organizations. © 2018 CAQH, All Rights Reserved. 58
CORE Certification E-Learning Resources www. caqh. org/core/elearning-resources Understand the four components needed to complete voluntary CORE Certification. © 2018 CAQH, All Rights Reserved. Learn about the new CORE Certification Application Portal. 59 Explore an interactive map to see which Medicaid entities around the country have achieved CORE Certification.
Thank you for joining us! @CAQH Website: www. CAQH. org/CORE Email: CORE@CAQH. org The CAQH CORE Mission Drive the creation and adoption of healthcare operating rules that support standards, accelerate interoperability, and align administrative and clinical activities among providers, payers and consumers. © 2018 CAQH, All Rights Reserved. 60
Appendix © 2018 CAQH, All Rights Reserved. 61
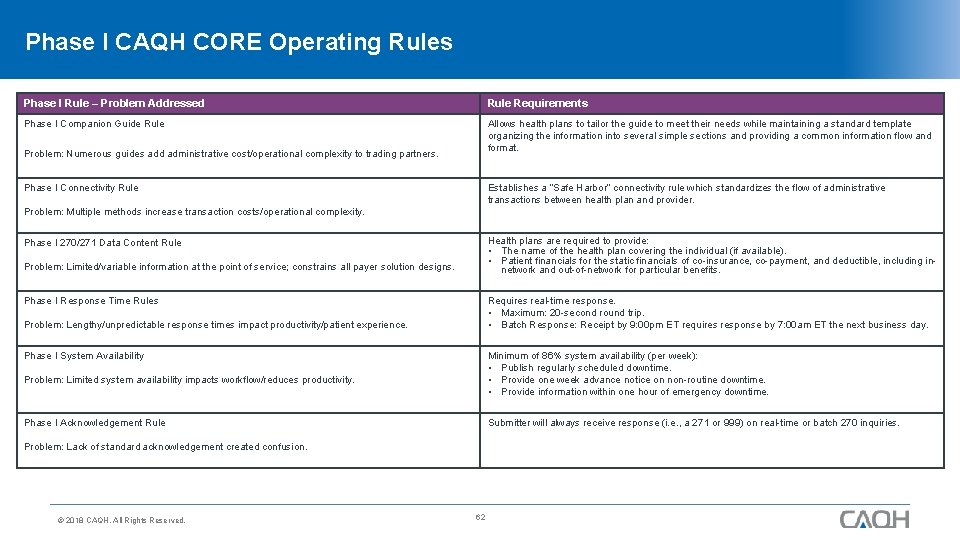
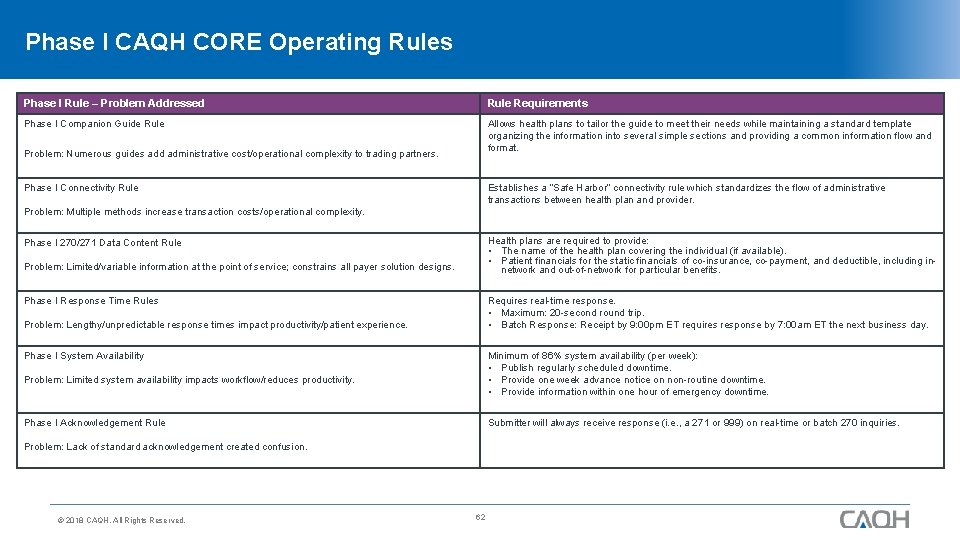
Phase I CAQH CORE Operating Rules Phase I Rule – Problem Addressed Rule Requirements Phase I Companion Guide Rule Allows health plans to tailor the guide to meet their needs while maintaining a standard template organizing the information into several simple sections and providing a common information flow and format. Problem: Numerous guides add administrative cost/operational complexity to trading partners. Phase I Connectivity Rule Establishes a “Safe Harbor” connectivity rule which standardizes the flow of administrative transactions between health plan and provider. Problem: Multiple methods increase transaction costs/operational complexity. Health plans are required to provide: • The name of the health plan covering the individual (if available). • Patient financials for the static financials of co-insurance, co-payment, and deductible, including innetwork and out-of-network for particular benefits. Phase I 270/271 Data Content Rule Click to add title Problem: Limited/variable information at the point of service; constrains all payer solution designs. Phase I Response Time Rules Requires real-time response. • Maximum: 20 -second round trip. • Batch Response: Receipt by 9: 00 pm ET requires response by 7: 00 am ET the next business day. Problem: Lengthy/unpredictable response times impact productivity/patient experience. Phase I System Availability Minimum of 86% system availability (per week): • Publish regularly scheduled downtime. • Provide one week advance notice on non-routine downtime. • Provide information within one hour of emergency downtime. Problem: Limited system availability impacts workflow/reduces productivity. Phase I Acknowledgement Rule Submitter will always receive response (i. e. , a 271 or 999) on real-time or batch 270 inquiries. Problem: Lack of standard acknowledgement created confusion. © 2018 CAQH, All Rights Reserved. 62
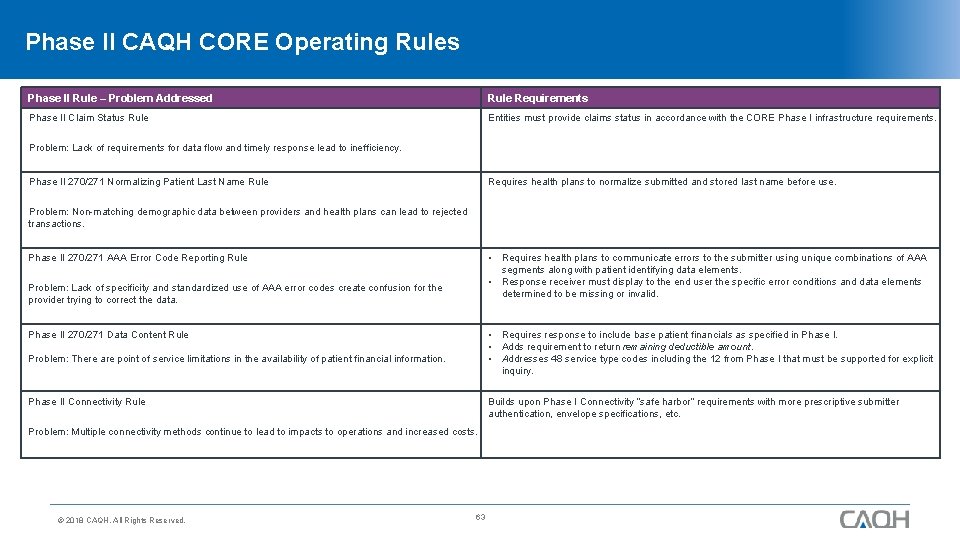
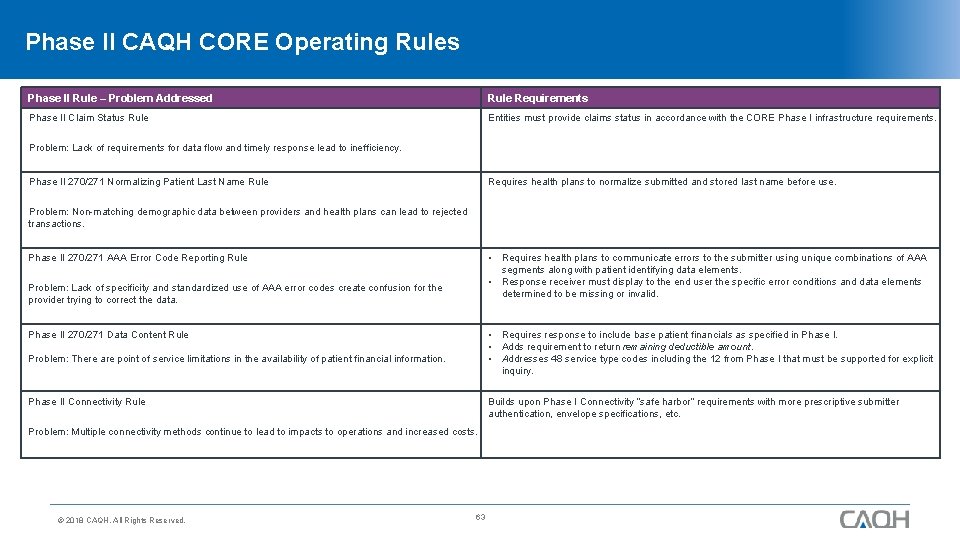
Phase II CAQH CORE Operating Rules Phase II Rule – Problem Addressed Rule Requirements Phase II Claim Status Rule Entities must provide claims status in accordance with the CORE Phase I infrastructure requirements. Problem: Lack of requirements for data flow and timely response lead to inefficiency. Phase II 270/271 Normalizing Patient Last Name Rule Requires health plans to normalize submitted and stored last name before use. Problem: Non-matching demographic data between providers and health plans can lead to rejected transactions. Phase II 270/271 AAA Error Code Reporting Rule • Requires health plans to communicate errors to the submitter using unique combinations of AAA segments along with patient identifying data elements. • Response receiver must display to the end user the specific error conditions and data elements determined to be missing or invalid. Click to add title Problem: Lack of specificity and standardized use of AAA error codes create confusion for the provider trying to correct the data. • Requires response to include base patient financials as specified in Phase I. • Adds requirement to return remaining deductible amount. • Addresses 48 service type codes including the 12 from Phase I that must be supported for explicit inquiry. Phase II 270/271 Data Content Rule Problem: There are point of service limitations in the availability of patient financial information. Phase II Connectivity Rule Builds upon Phase I Connectivity “safe harbor” requirements with more prescriptive submitter authentication, envelope specifications, etc. Problem: Multiple connectivity methods continue to lead to impacts to operations and increased costs. © 2018 CAQH, All Rights Reserved. 63
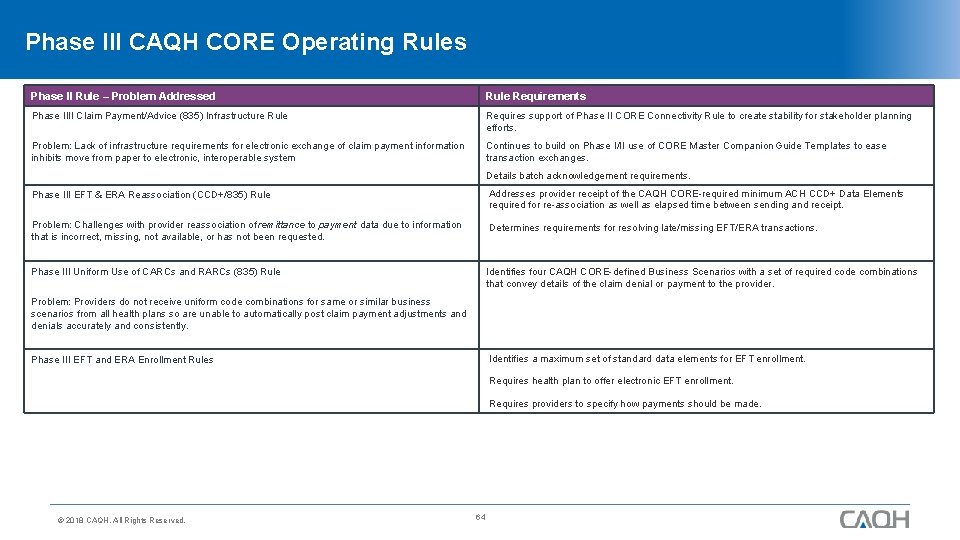
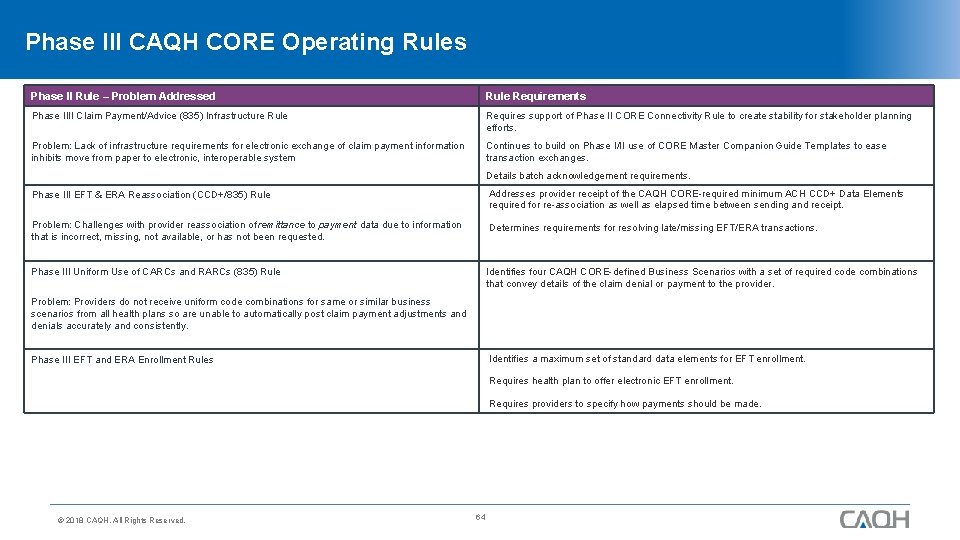
Phase III CAQH CORE Operating Rules Phase II Rule – Problem Addressed Rule Requirements Phase IIII Claim Payment/Advice (835) Infrastructure Rule Requires support of Phase II CORE Connectivity Rule to create stability for stakeholder planning efforts. Problem: Lack of infrastructure requirements for electronic exchange of claim payment information inhibits move from paper to electronic, interoperable system Continues to build on Phase I/II use of CORE Master Companion Guide Templates to ease transaction exchanges. Details batch acknowledgement requirements. Phase III EFT & ERA Reassociation (CCD+/835) Rule Addresses provider receipt of the CAQH CORE-required minimum ACH CCD+ Data Elements required for re-association as well as elapsed time between sending and receipt. Problem: Challenges with provider reassociation of remittance to payment data due to information that is incorrect, missing, not available, or has not been requested. Determines requirements for resolving late/missing EFT/ERA transactions. Phase III Uniform Use of CARCs and RARCs (835) Rule Click to add. Identifies titlefour CAQH CORE-defined Business Scenarios with a set of required code combinations that convey details of the claim denial or payment to the provider. Problem: Providers do not receive uniform code combinations for same or similar business scenarios from all health plans so are unable to automatically post claim payment adjustments and denials accurately and consistently. Identifies a maximum set of standard data elements for EFT enrollment. Phase III EFT and ERA Enrollment Rules Requires health plan to offer electronic EFT enrollment. Requires providers to specify how payments should be made. © 2018 CAQH, All Rights Reserved. 64
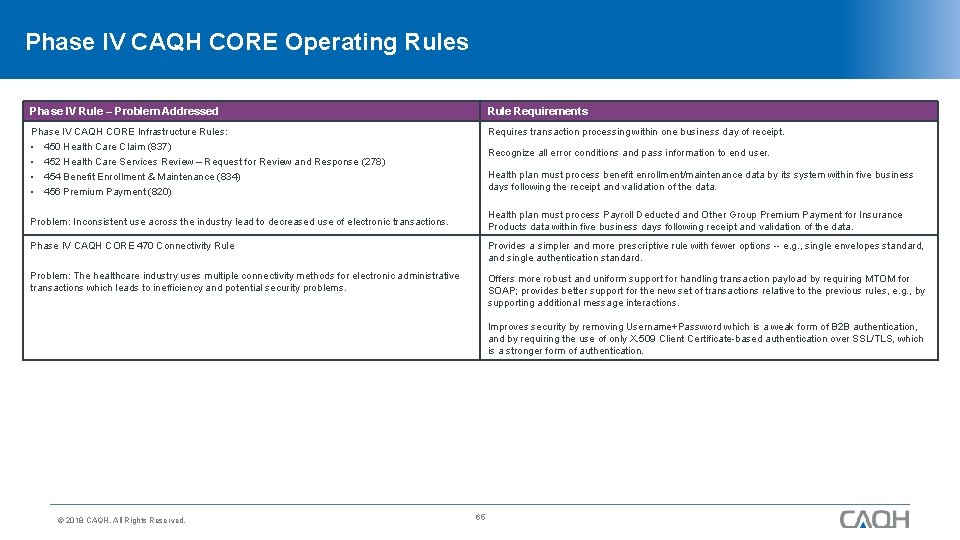
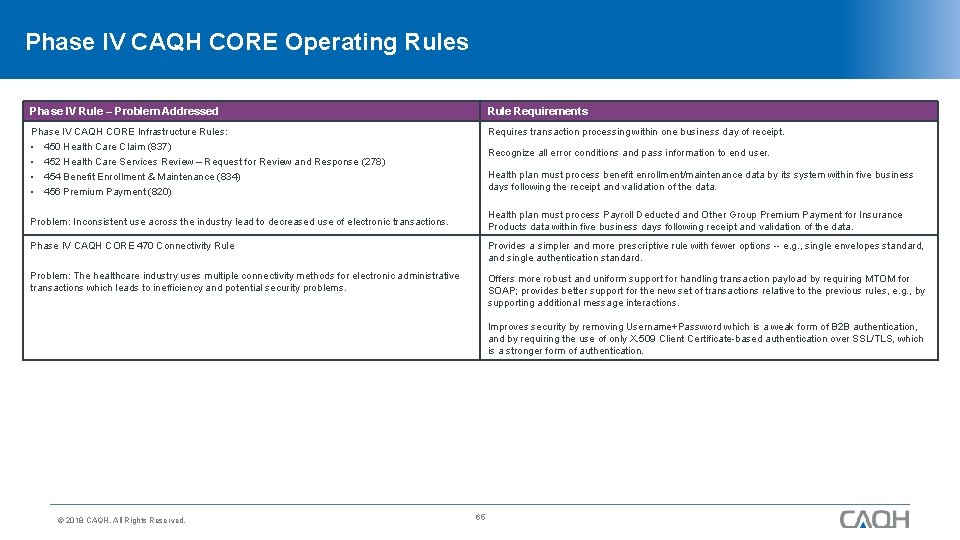
Phase IV CAQH CORE Operating Rules Phase IV Rule – Problem Addressed Rule Requirements Phase IV CAQH CORE Infrastructure Rules: • 450 Health Care Claim (837) Requires transaction processing within one business day of receipt. Recognize all error conditions and pass information to end user. • 452 Health Care Services Review – Request for Review and Response (278) • 454 Benefit Enrollment & Maintenance (834) • 456 Premium Payment (820) Health plan must process benefit enrollment/maintenance data by its system within five business days following the receipt and validation of the data. Health plan must process Payroll Deducted and Other Group Premium Payment for Insurance Products data within five business days following receipt and validation of the data. Problem: Inconsistent use across the industry lead to decreased use of electronic transactions. Phase IV CAQH CORE 470 Connectivity Rule Provides a simpler and more prescriptive rule with fewer options -- e. g. , single envelopes standard, and single authentication standard. Click to add. Offers title more robust and uniform support for handling transaction payload by requiring MTOM for Problem: The healthcare industry uses multiple connectivity methods for electronic administrative transactions which leads to inefficiency and potential security problems. SOAP; provides better support for the new set of transactions relative to the previous rules, e. g. , by supporting additional message interactions. Improves security by removing Username+Password which is a weak form of B 2 B authentication, and by requiring the use of only X. 509 Client Certificate-based authentication over SSL/TLS, which is a stronger form of authentication. © 2018 CAQH, All Rights Reserved. 65
 Penciptaan nilai adalah
Penciptaan nilai adalah Caqh provider data management
Caqh provider data management Caqh geoaccess
Caqh geoaccess Caqhpro
Caqhpro Caqh enroll hub
Caqh enroll hub Optical fibre
Optical fibre Bacteriological index formula
Bacteriological index formula Physical quality of life index and human development index
Physical quality of life index and human development index Diff between step index and graded index fiber
Diff between step index and graded index fiber Consistency limits and indices
Consistency limits and indices Primary index is dense or sparse
Primary index is dense or sparse Simpson's index vs simpson's diversity index
Simpson's index vs simpson's diversity index Clustered index và non clustered index
Clustered index và non clustered index Laspeyres formula
Laspeyres formula Value index formula
Value index formula Value received and value parted with
Value received and value parted with Volcano plot interpretation
Volcano plot interpretation D value and z value
D value and z value Saponification number
Saponification number Creating value and capturing value
Creating value and capturing value Future value of $1
Future value of $1 Relative value vs absolute value
Relative value vs absolute value What is the value of what is the value of
What is the value of what is the value of What is the value of what is the value of
What is the value of what is the value of Fulya batur
Fulya batur Virusmax
Virusmax Data quality and data cleaning an overview
Data quality and data cleaning an overview The two rows of elements that seem to be disconnected
The two rows of elements that seem to be disconnected Chicago time
Chicago time Multicullar
Multicullar An overview of data warehousing and olap technology
An overview of data warehousing and olap technology Data quality and data cleaning an overview
Data quality and data cleaning an overview Data quality and data cleaning an overview
Data quality and data cleaning an overview Overview of storage and indexing
Overview of storage and indexing Chapter 17 overview elements and their properties
Chapter 17 overview elements and their properties Www overview
Www overview Maximo work order priority
Maximo work order priority Universal modelling language
Universal modelling language Uml overview
Uml overview Vertical retailer
Vertical retailer Figure 12-1 provides an overview of the lymphatic vessels
Figure 12-1 provides an overview of the lymphatic vessels Systemic artery
Systemic artery Texas recapture districts
Texas recapture districts Walmart operations management
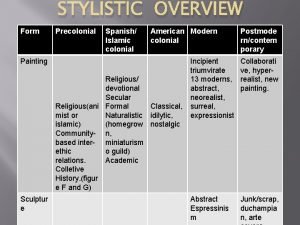
Walmart operations management Stylistic overview of philippine art
Stylistic overview of philippine art Structured analysis and structured design (sa/sd)
Structured analysis and structured design (sa/sd) Spring framework overview
Spring framework overview Nagios tactical overview
Nagios tactical overview Market overview managed file transfer solutions
Market overview managed file transfer solutions Sdn vs nfv
Sdn vs nfv Sbic program
Sbic program Unrestricted use stock
Unrestricted use stock Ariba overview
Ariba overview Safe overview
Safe overview Rfid technology overview
Rfid technology overview Overview in research example
Overview in research example Title
Title Overview of the major systemic arteries
Overview of the major systemic arteries Abstract overview
Abstract overview Pillar 2 solvency ii
Pillar 2 solvency ii Overview of physical storage media in dbms
Overview of physical storage media in dbms Overview of education in health care
Overview of education in health care Marcus scheuren
Marcus scheuren Ospf overview
Ospf overview Architecture review template
Architecture review template Scene 3 oedipus rex summary
Scene 3 oedipus rex summary