Overview and Introduction Alzheimers Disease The Challenge of
- Slides: 27
Overview and Introduction Alzheimer’s Disease The Challenge of Early Diagnosis
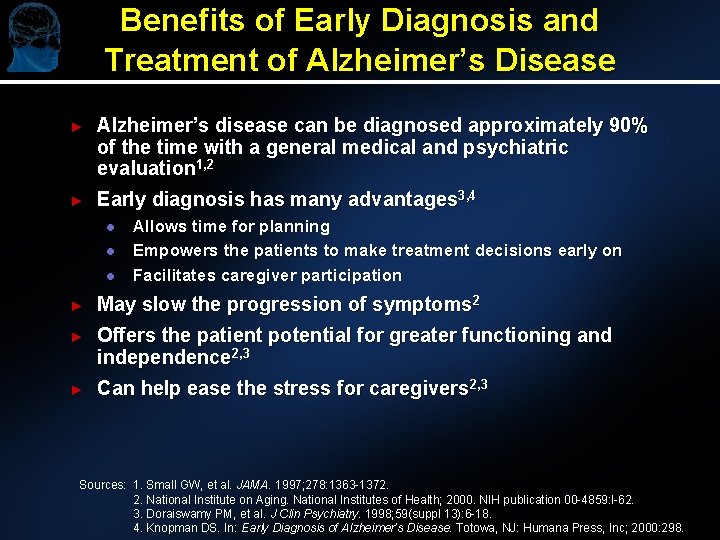
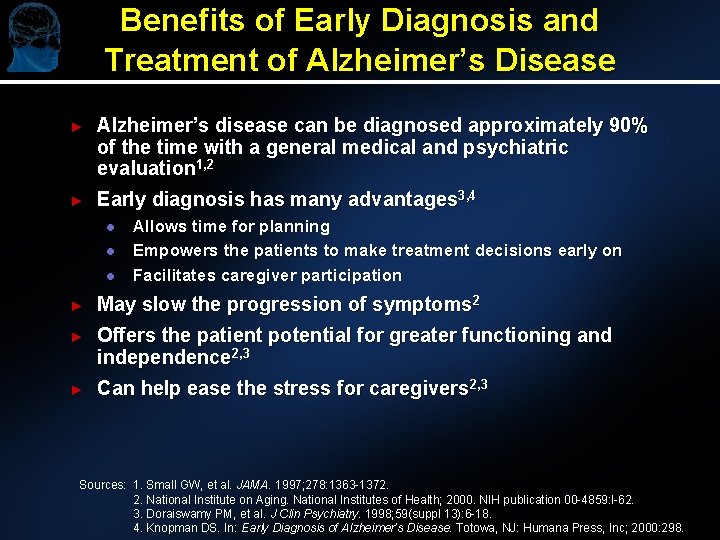
Benefits of Early Diagnosis and Treatment of Alzheimer’s Disease ► Alzheimer’s disease can be diagnosed approximately 90% of the time with a general medical and psychiatric evaluation 1, 2 ► Early diagnosis has many advantages 3, 4 l l l Allows time for planning Empowers the patients to make treatment decisions early on Facilitates caregiver participation ► May slow the progression of symptoms 2 ► Offers the patient potential for greater functioning and independence 2, 3 ► Can help ease the stress for caregivers 2, 3 Sources: 1. Small GW, et al. JAMA. 1997; 278: 1363 -1372. 2. National Institute on Aging. National Institutes of Health; 2000. NIH publication 00 -4859: l-62. 3. Doraiswamy PM, et al. J Clin Psychiatry. 1998; 59(suppl 13): 6 -18. 4. Knopman DS. In: Early Diagnosis of Alzheimer’s Disease. Totowa, NJ: Humana Press, Inc; 2000: 298.
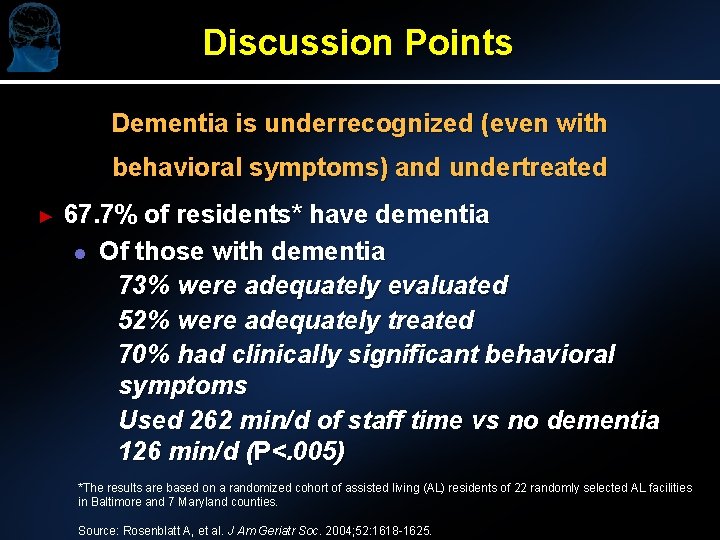
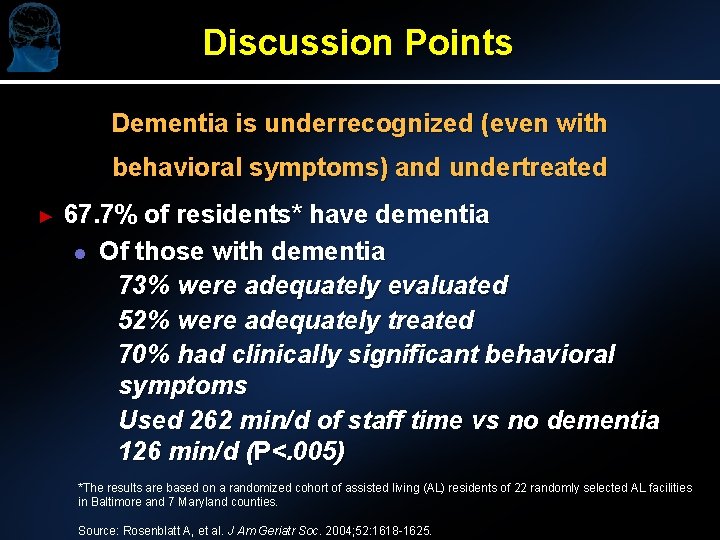
Discussion Points Dementia is underrecognized (even with behavioral symptoms) and undertreated ► 67. 7% of residents* have dementia l Of those with dementia 73% were adequately evaluated 52% were adequately treated 70% had clinically significant behavioral symptoms Used 262 min/d of staff time vs no dementia 126 min/d (P<. 005) *The results are based on a randomized cohort of assisted living (AL) residents of 22 randomly selected AL facilities in Baltimore and 7 Maryland counties. Source: Rosenblatt A, et al. J Am Geriatr Soc. 2004; 52: 1618 -1625.
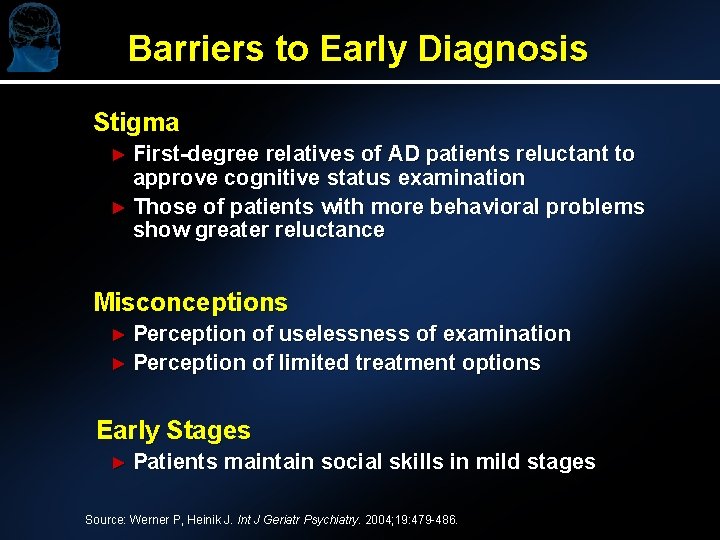
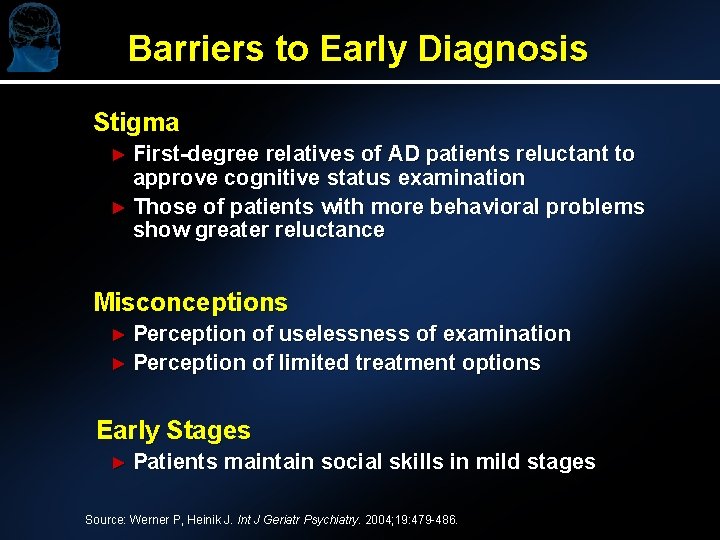
Barriers to Early Diagnosis Stigma ► First-degree relatives of AD patients reluctant to approve cognitive status examination ► Those of patients with more behavioral problems show greater reluctance Misconceptions ► Perception of uselessness of examination ► Perception of limited treatment options Early Stages ► Patients maintain social skills in mild stages Source: Werner P, Heinik J. Int J Geriatr Psychiatry. 2004; 19: 479 -486.
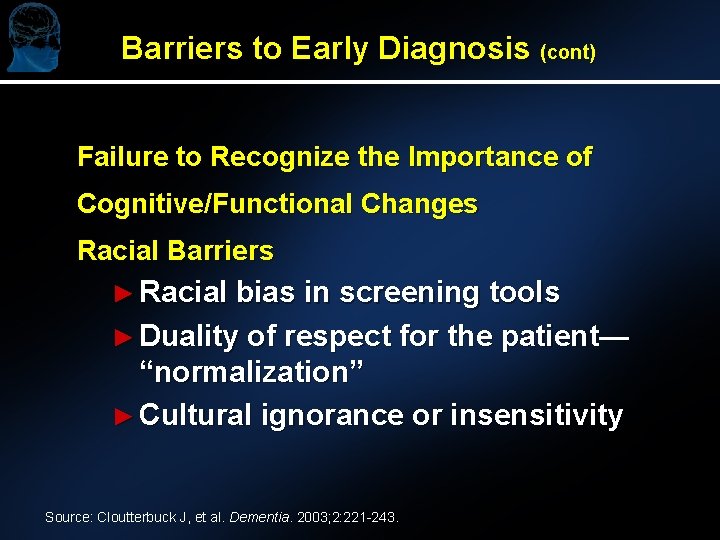
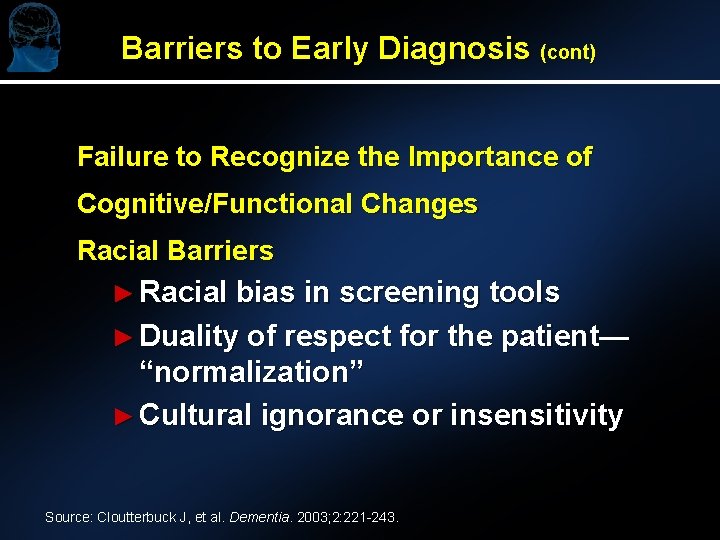
Barriers to Early Diagnosis (cont) Failure to Recognize the Importance of Cognitive/Functional Changes Racial Barriers ► Racial bias in screening tools ► Duality of respect for the patient— “normalization” ► Cultural ignorance or insensitivity Source: Cloutterbuck J, et al. Dementia. 2003; 2: 221 -243.
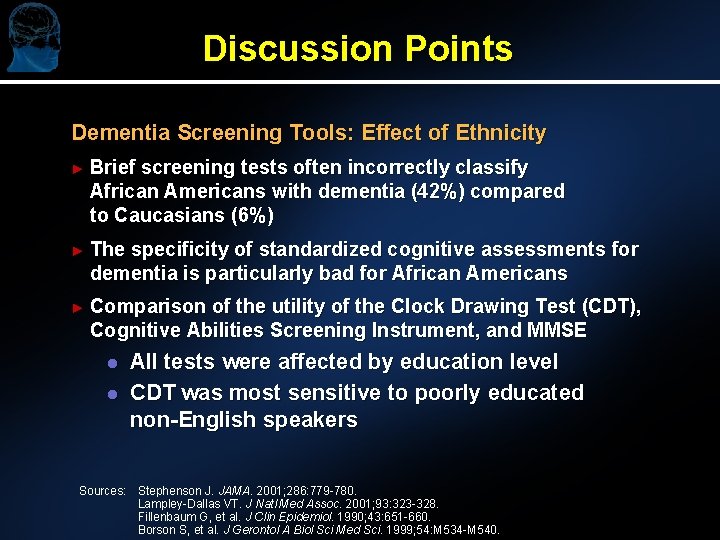
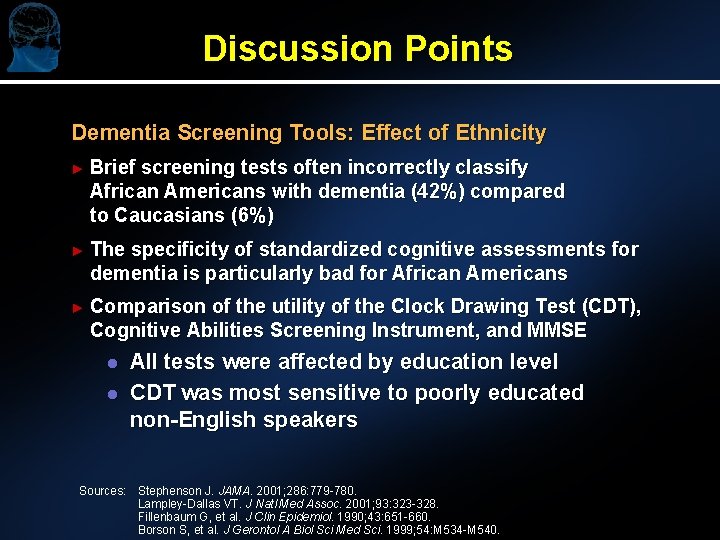
Discussion Points Dementia Screening Tools: Effect of Ethnicity ► Brief screening tests often incorrectly classify African Americans with dementia (42%) compared to Caucasians (6%) ► The specificity of standardized cognitive assessments for dementia is particularly bad for African Americans ► Comparison of the utility of the Clock Drawing Test (CDT), Cognitive Abilities Screening Instrument, and MMSE l l All tests were affected by education level CDT was most sensitive to poorly educated non-English speakers Sources: Stephenson J. JAMA. 2001; 286: 779 -780. Lampley-Dallas VT. J Natl Med Assoc. 2001; 93: 323 -328. Fillenbaum G, et al. J Clin Epidemiol. 1990; 43: 651 -660. Borson S, et al. J Gerontol A Biol Sci Med Sci. 1999; 54: M 534 -M 540.
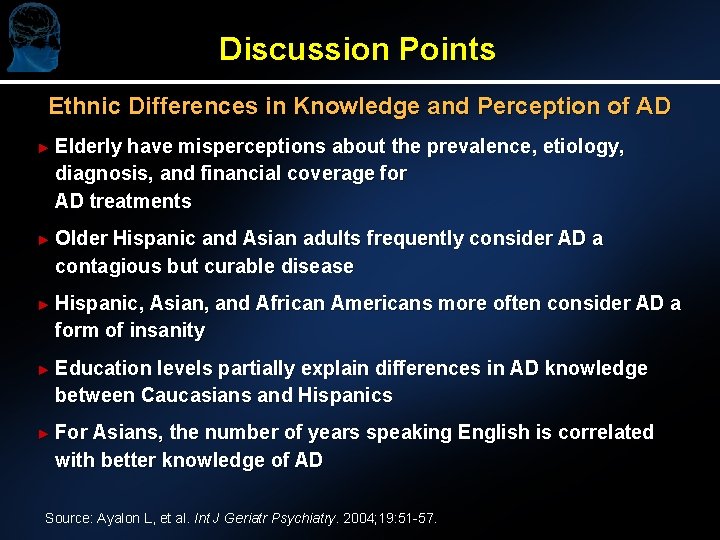
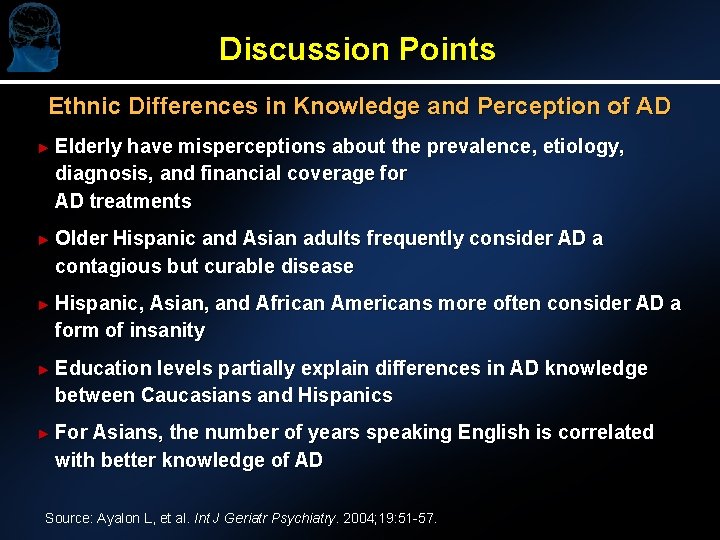
Discussion Points Ethnic Differences in Knowledge and Perception of AD ► Elderly have misperceptions about the prevalence, etiology, diagnosis, and financial coverage for AD treatments ► Older Hispanic and Asian adults frequently consider AD a contagious but curable disease ► Hispanic, Asian, and African Americans more often consider AD a form of insanity ► Education levels partially explain differences in AD knowledge between Caucasians and Hispanics ► For Asians, the number of years speaking English is correlated with better knowledge of AD Source: Ayalon L, et al. Int J Geriatr Psychiatry. 2004; 19: 51 -57.
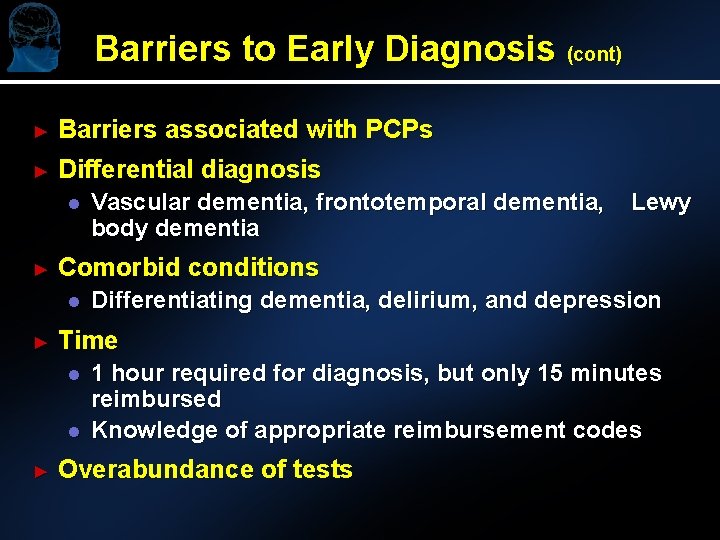
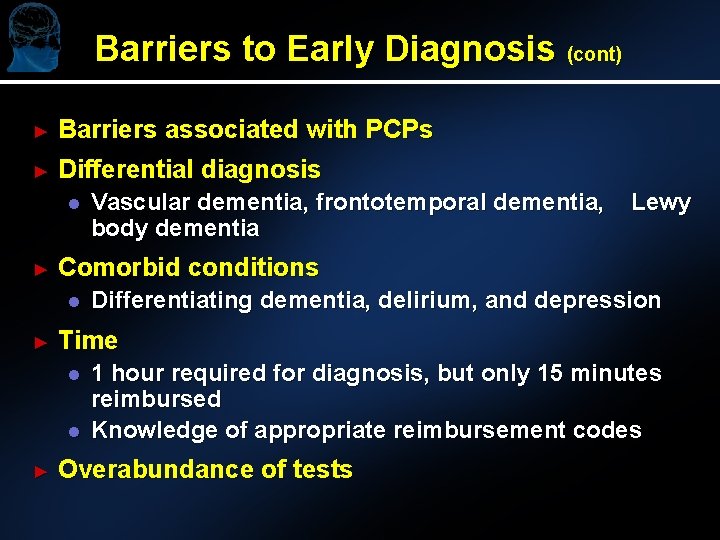
Barriers to Early Diagnosis (cont) ► Barriers associated with PCPs ► Differential diagnosis l ► Differentiating dementia, delirium, and depression Time l l ► Lewy Comorbid conditions l ► Vascular dementia, frontotemporal dementia, body dementia 1 hour required for diagnosis, but only 15 minutes reimbursed Knowledge of appropriate reimbursement codes Overabundance of tests
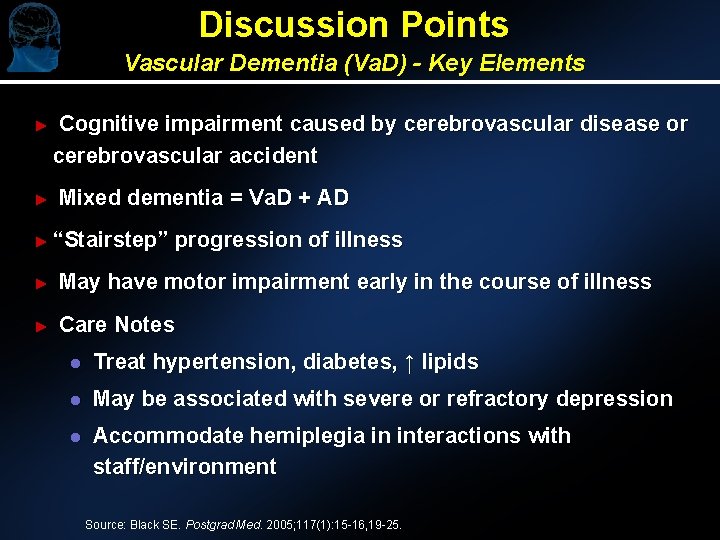
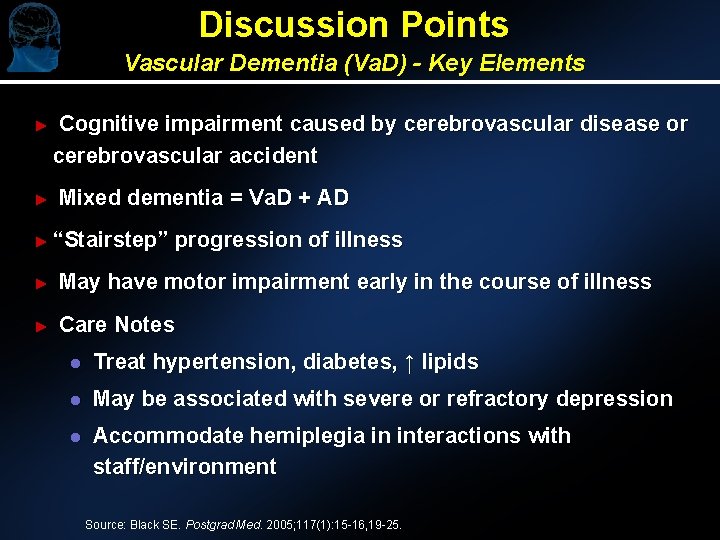
Discussion Points Vascular Dementia (Va. D) - Key Elements ► ► Cognitive impairment caused by cerebrovascular disease or cerebrovascular accident Mixed dementia = Va. D + AD ► “Stairstep” progression of illness ► May have motor impairment early in the course of illness ► Care Notes l Treat hypertension, diabetes, ↑ lipids l May be associated with severe or refractory depression l Accommodate hemiplegia in interactions with staff/environment Source: Black SE. Postgrad Med. 2005; 117(1): 15 -16, 19 -25.
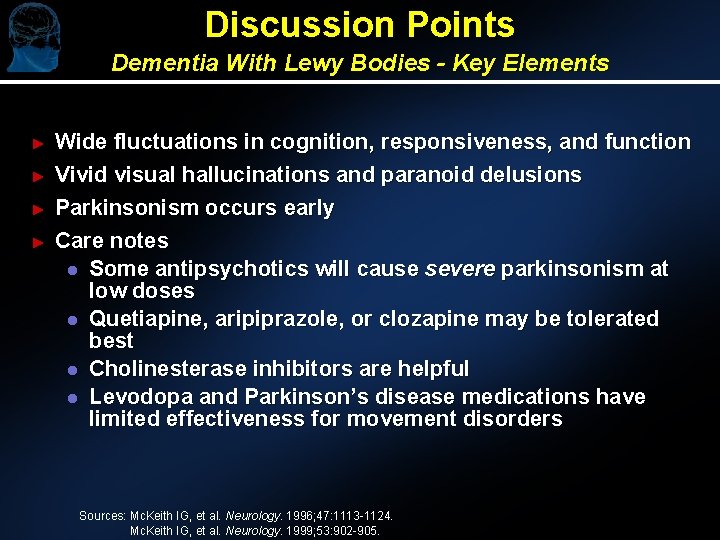
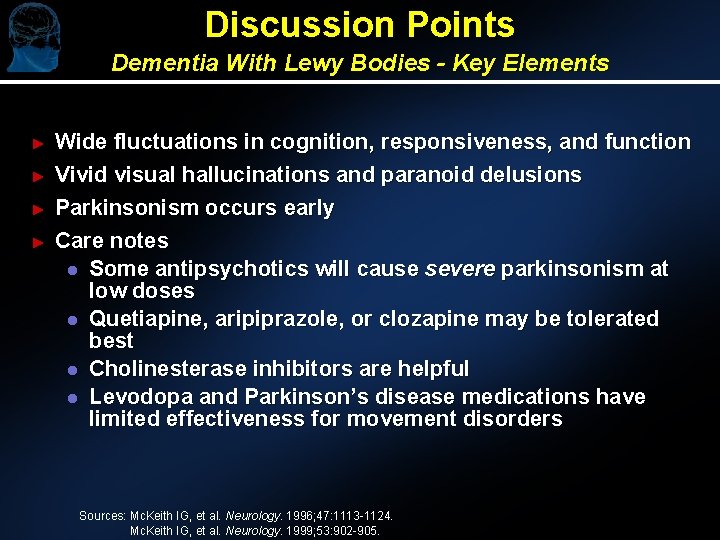
Discussion Points Dementia With Lewy Bodies - Key Elements ► ► Wide fluctuations in cognition, responsiveness, and function Vivid visual hallucinations and paranoid delusions Parkinsonism occurs early Care notes l Some antipsychotics will cause severe parkinsonism at low doses l Quetiapine, aripiprazole, or clozapine may be tolerated best l Cholinesterase inhibitors are helpful l Levodopa and Parkinson’s disease medications have limited effectiveness for movement disorders Sources: Mc. Keith IG, et al. Neurology. 1996; 47: 1113 -1124. Mc. Keith IG, et al. Neurology. 1999; 53: 902 -905.
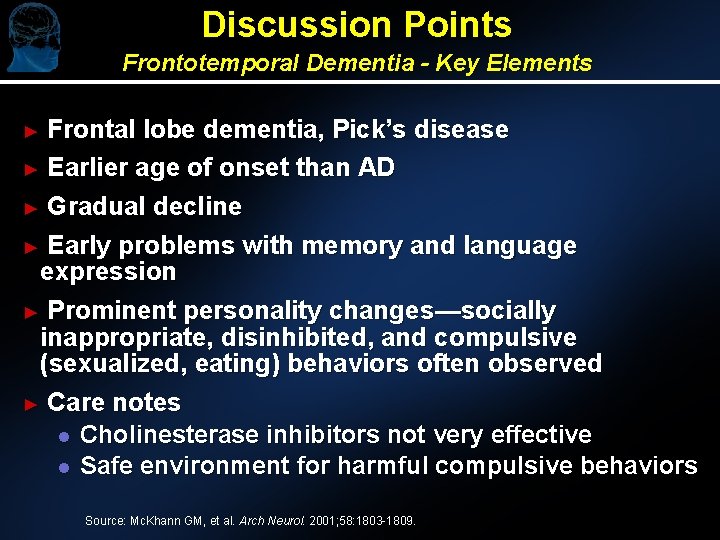
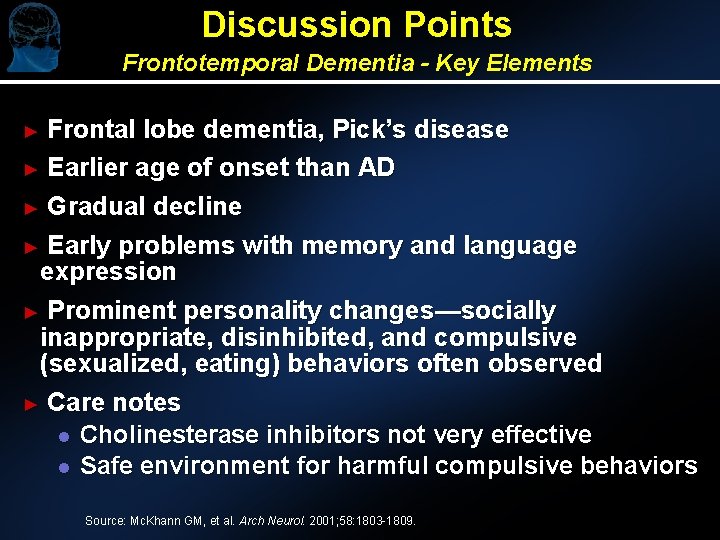
Discussion Points Frontotemporal Dementia - Key Elements Frontal lobe dementia, Pick’s disease ► Earlier age of onset than AD ► Gradual decline ► Early problems with memory and language expression ► Prominent personality changes—socially inappropriate, disinhibited, and compulsive (sexualized, eating) behaviors often observed ► Care notes l Cholinesterase inhibitors not very effective l Safe environment for harmful compulsive behaviors ► Source: Mc. Khann GM, et al. Arch Neurol. 2001; 58: 1803 -1809.
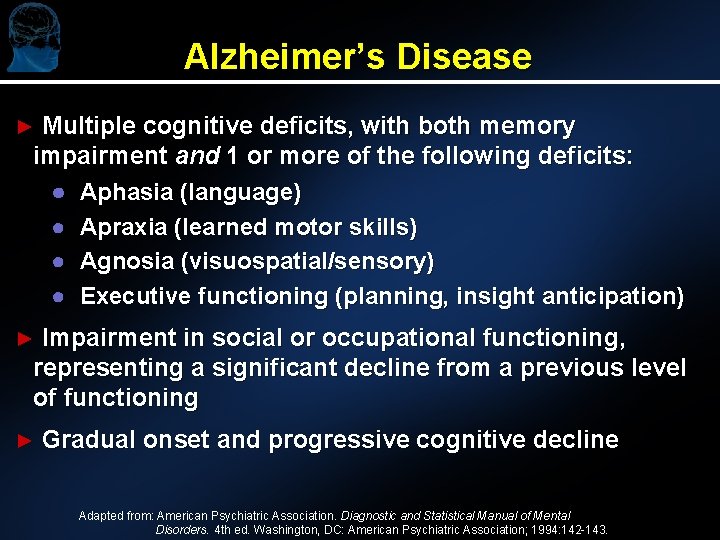
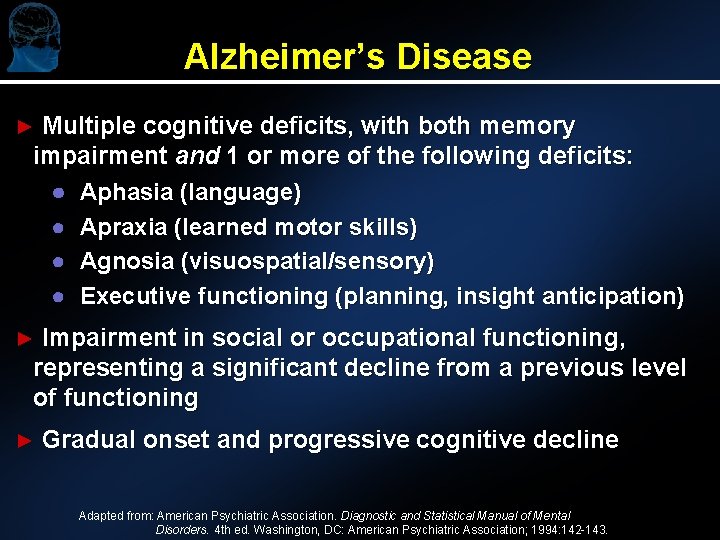
Alzheimer’s Disease ► Multiple cognitive deficits, with both memory impairment and 1 or more of the following deficits: ● Aphasia (language) ● Apraxia (learned motor skills) ● Agnosia (visuospatial/sensory) ● Executive functioning (planning, insight anticipation) ► Impairment in social or occupational functioning, representing a significant decline from a previous level of functioning ► Gradual onset and progressive cognitive decline Adapted from: American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4 th ed. Washington, DC: American Psychiatric Association; 1994: 142 -143.
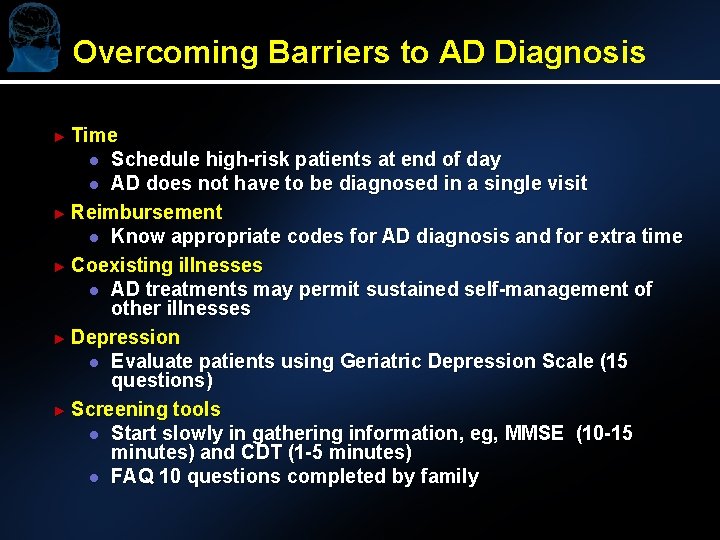
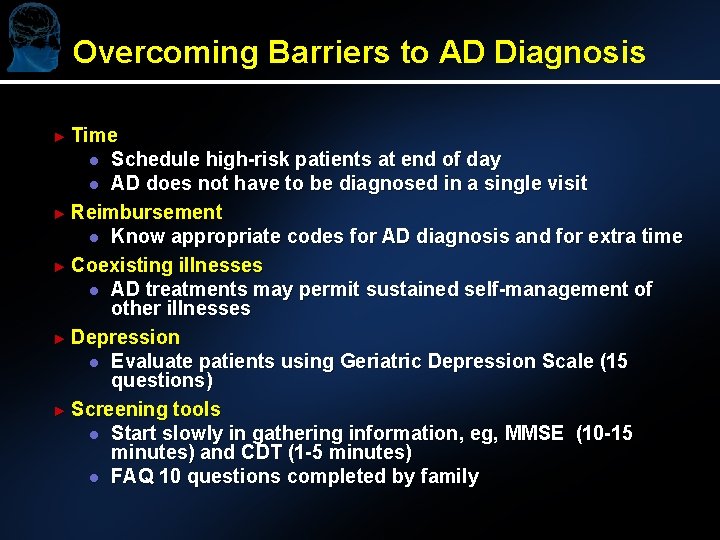
Overcoming Barriers to AD Diagnosis ► Time Schedule high-risk patients at end of day l AD does not have to be diagnosed in a single visit ► Reimbursement l Know appropriate codes for AD diagnosis and for extra time ► Coexisting illnesses l AD treatments may permit sustained self-management of other illnesses ► Depression l Evaluate patients using Geriatric Depression Scale (15 questions) ► Screening tools l Start slowly in gathering information, eg, MMSE (10 -15 minutes) and CDT (1 -5 minutes) l FAQ 10 questions completed by family l
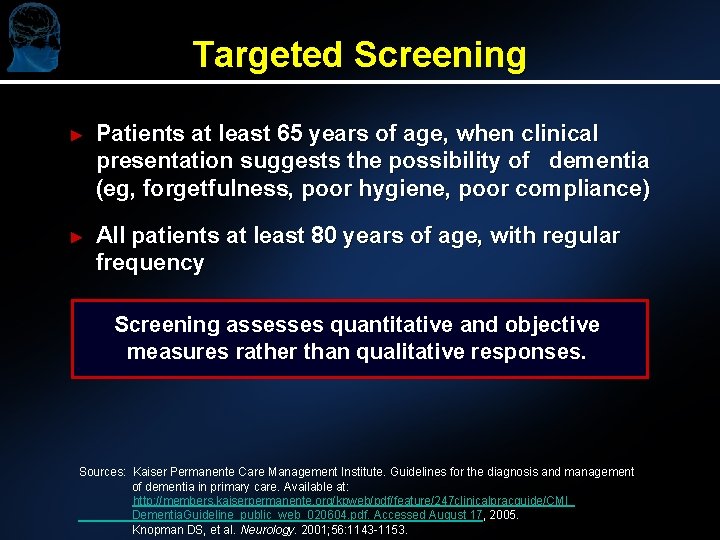
Targeted Screening ► Patients at least 65 years of age, when clinical presentation suggests the possibility of dementia (eg, forgetfulness, poor hygiene, poor compliance) ► All patients at least 80 years of age, with regular frequency Screening assesses quantitative and objective measures rather than qualitative responses. Sources: Kaiser Permanente Care Management Institute. Guidelines for the diagnosis and management of dementia in primary care. Available at: http: //members. kaiserpermanente. org/kpweb/pdf/feature/247 clinicalpracguide/CMI_ Dementia. Guideline_public_web_020604. pdf. Accessed August 17, 2005. Knopman DS, et al. Neurology. 2001; 56: 1143 -1153.
Discussion Points ► Is there a relationship between mild cognitive impairment (MCI) and AD? (16% of MCI patients convert to AD per year) ► How do we differentiate MCI from AD? ► Government recommendation not to screen (Agency for Healthcare Research and Quality)
The Case for Universal Cognitive Screening ► Memory complaints are common and can be associated with subsequent dementia ► Early dementia symptoms can be difficult to recognize ► Cognitive impairment affects how medical care is provided l l l Management (and costs) of other diseases Follow through with medical recommendations Prevention of complications
Discussion Points ► Which screening tools do you recommend? l A dialogue on the utility of screening tools ► Educational preceptorship—warning signs and public awareness l Community l Doctors l Consumers l Alzheimer’s Association
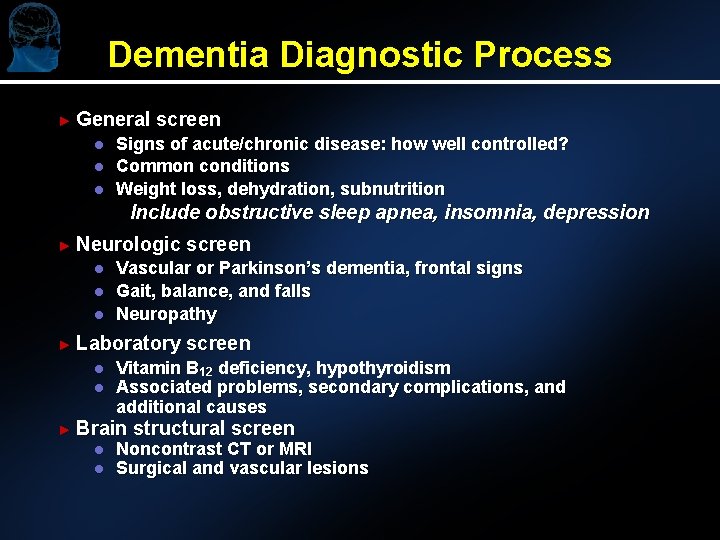
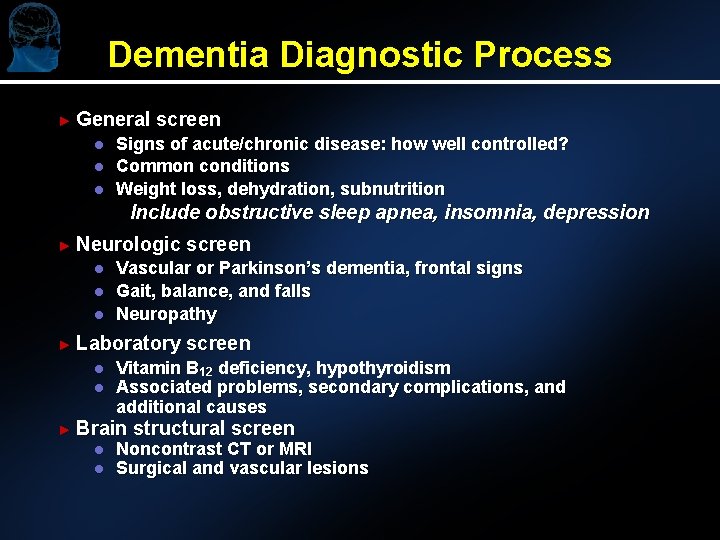
Dementia Diagnostic Process ► General l screen Signs of acute/chronic disease: how well controlled? Common conditions Weight loss, dehydration, subnutrition Include obstructive sleep apnea, insomnia, depression ► Neurologic l l l Vascular or Parkinson’s dementia, frontal signs Gait, balance, and falls Neuropathy ► Laboratory l l screen Vitamin B 12 deficiency, hypothyroidism Associated problems, secondary complications, and additional causes ► Brain l l screen structural screen Noncontrast CT or MRI Surgical and vascular lesions
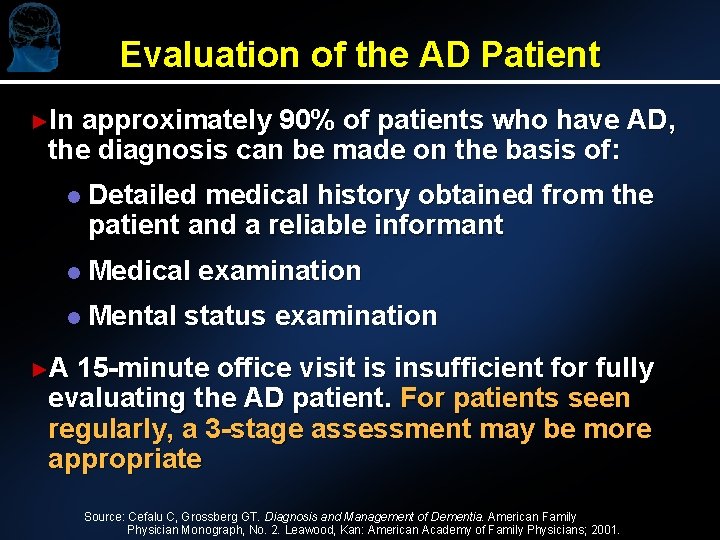
Evaluation of the AD Patient ►In approximately 90% of patients who have AD, the diagnosis can be made on the basis of: l Detailed medical history obtained from the patient and a reliable informant l Medical examination l Mental status examination ►A 15 -minute office visit is insufficient for fully evaluating the AD patient. For patients seen regularly, a 3 -stage assessment may be more appropriate Source: Cefalu C, Grossberg GT. Diagnosis and Management of Dementia. American Family Physician Monograph, No. 2. Leawood, Kan: American Academy of Family Physicians; 2001.
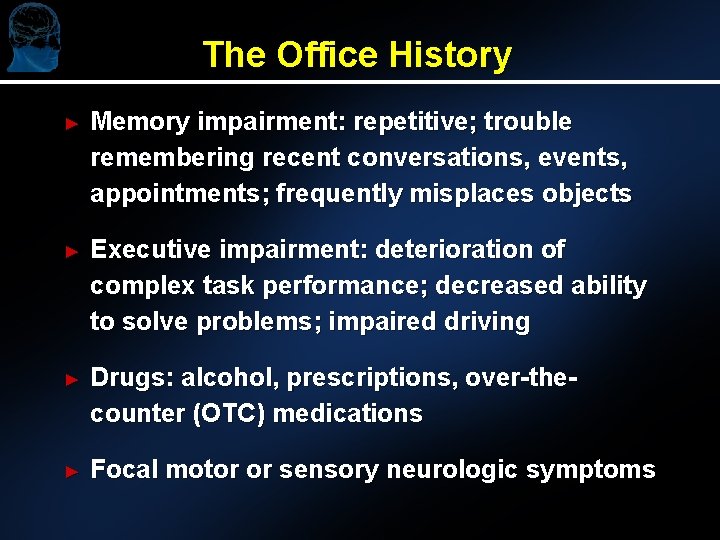
The Office History ► Memory impairment: repetitive; trouble remembering recent conversations, events, appointments; frequently misplaces objects ► Executive impairment: deterioration of complex task performance; decreased ability to solve problems; impaired driving ► Drugs: alcohol, prescriptions, over-thecounter (OTC) medications ► Focal motor or sensory neurologic symptoms
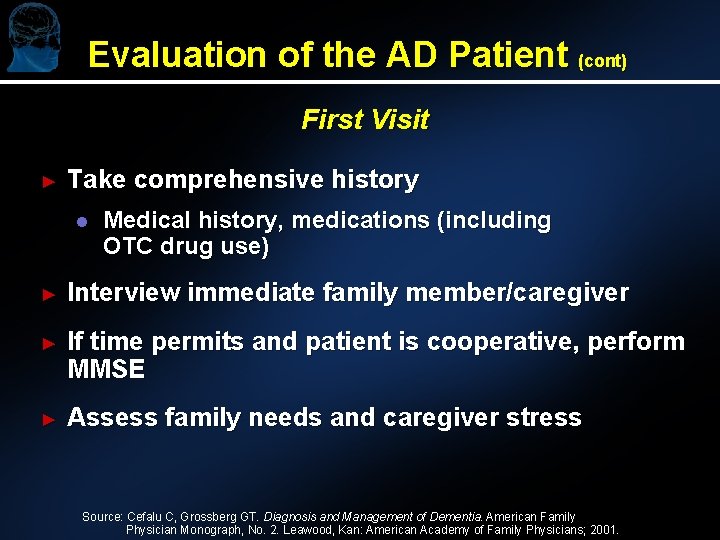
Evaluation of the AD Patient (cont) First Visit ► Take comprehensive history l Medical history, medications (including OTC drug use) ► Interview immediate family member/caregiver ► If time permits and patient is cooperative, perform MMSE ► Assess family needs and caregiver stress Source: Cefalu C, Grossberg GT. Diagnosis and Management of Dementia. American Family Physician Monograph, No. 2. Leawood, Kan: American Academy of Family Physicians; 2001.
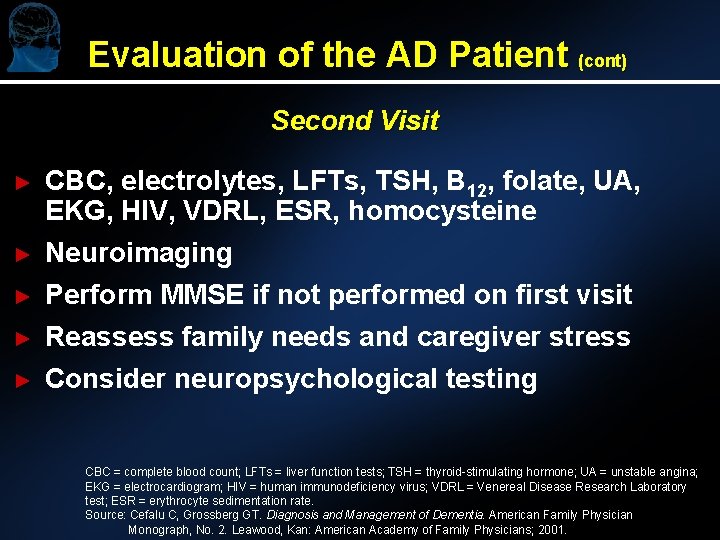
Evaluation of the AD Patient (cont) Second Visit ► ► ► CBC, electrolytes, LFTs, TSH, B 12, folate, UA, EKG, HIV, VDRL, ESR, homocysteine Neuroimaging Perform MMSE if not performed on first visit Reassess family needs and caregiver stress Consider neuropsychological testing CBC = complete blood count; LFTs = liver function tests; TSH = thyroid-stimulating hormone; UA = unstable angina; EKG = electrocardiogram; HIV = human immunodeficiency virus; VDRL = Venereal Disease Research Laboratory test; ESR = erythrocyte sedimentation rate. Source: Cefalu C, Grossberg GT. Diagnosis and Management of Dementia. American Family Physician Monograph, No. 2. Leawood, Kan: American Academy of Family Physicians; 2001.
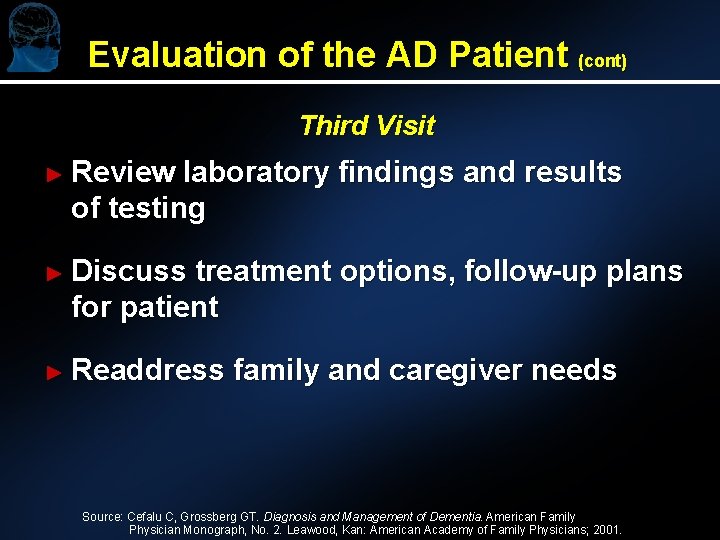
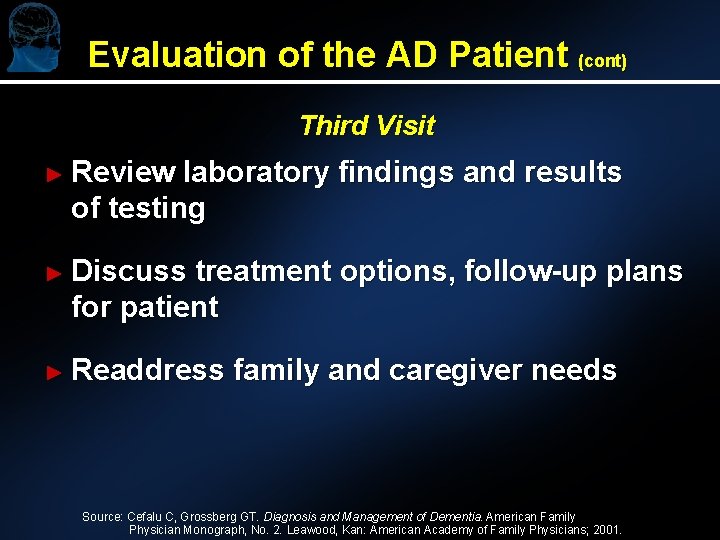
Evaluation of the AD Patient (cont) Third Visit ► Review laboratory findings and results of testing ► Discuss treatment options, follow-up plans for patient ► Readdress family and caregiver needs Source: Cefalu C, Grossberg GT. Diagnosis and Management of Dementia. American Family Physician Monograph, No. 2. Leawood, Kan: American Academy of Family Physicians; 2001.
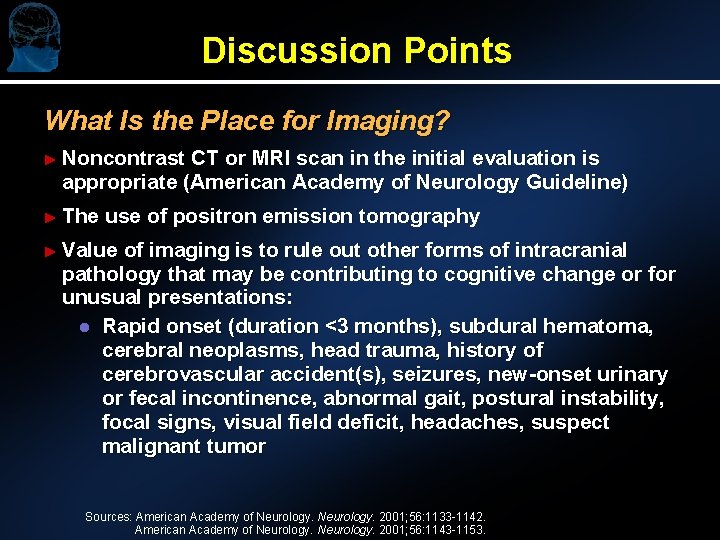
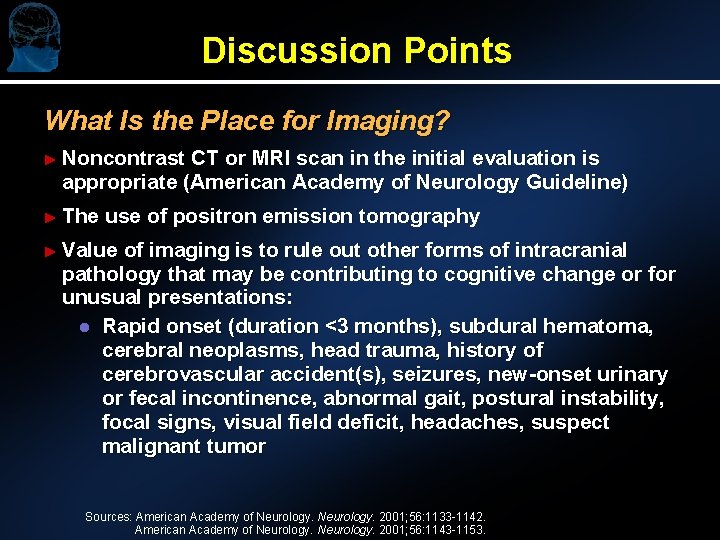
Discussion Points What Is the Place for Imaging? ► Noncontrast CT or MRI scan in the initial evaluation is appropriate (American Academy of Neurology Guideline) ► The use of positron emission tomography ► Value of imaging is to rule out other forms of intracranial pathology that may be contributing to cognitive change or for unusual presentations: l Rapid onset (duration <3 months), subdural hematoma, cerebral neoplasms, head trauma, history of cerebrovascular accident(s), seizures, new-onset urinary or fecal incontinence, abnormal gait, postural instability, focal signs, visual field deficit, headaches, suspect malignant tumor Sources: American Academy of Neurology. 2001; 56: 1133 -1142. American Academy of Neurology. 2001; 56: 1143 -1153.
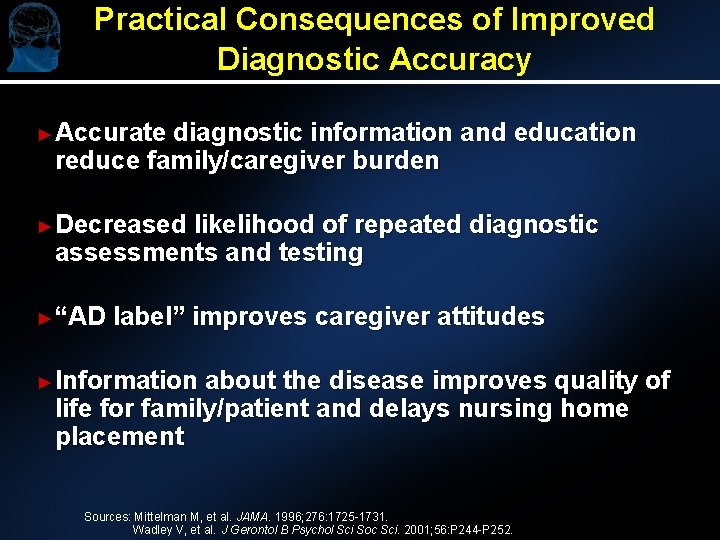
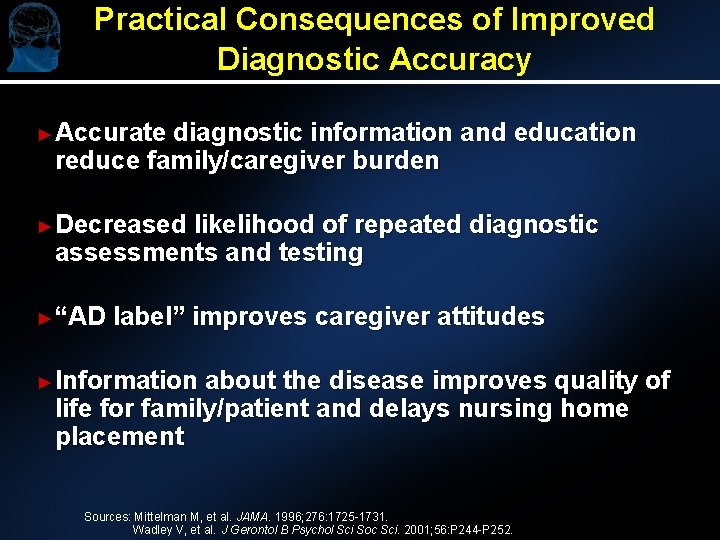
Practical Consequences of Improved Diagnostic Accuracy ►Accurate diagnostic information and education reduce family/caregiver burden ►Decreased likelihood of repeated diagnostic assessments and testing ►“AD label” improves caregiver attitudes ►Information about the disease improves quality of life for family/patient and delays nursing home placement Sources: Mittelman M, et al. JAMA. 1996; 276: 1725 -1731. Wadley V, et al. J Gerontol B Psychol Sci Soc Sci. 2001; 56: P 244 -P 252.
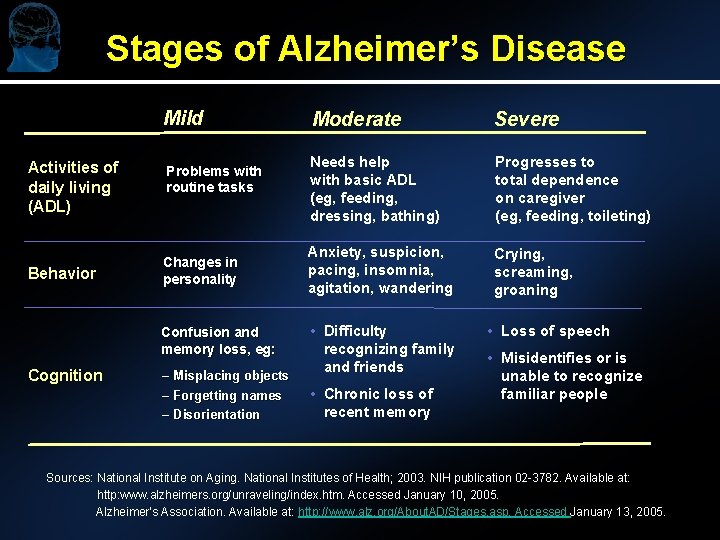
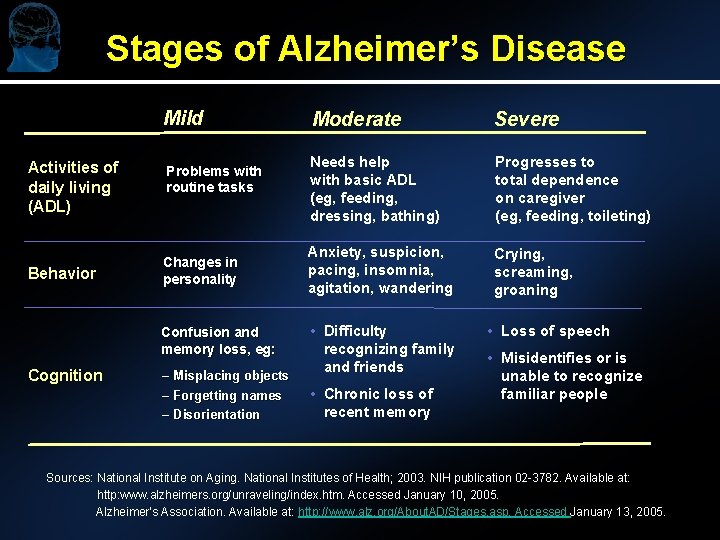
Stages of Alzheimer’s Disease Mild Activities of daily living (ADL) Behavior Problems with routine tasks Changes in personality Confusion and memory loss, eg: Cognition – Misplacing objects – Forgetting names – Disorientation Moderate Severe Needs help with basic ADL (eg, feeding, dressing, bathing) Progresses to total dependence on caregiver (eg, feeding, toileting) Anxiety, suspicion, pacing, insomnia, agitation, wandering Crying, screaming, groaning • Difficulty recognizing family and friends • Chronic loss of recent memory • Loss of speech • Misidentifies or is unable to recognize familiar people Sources: National Institute on Aging. National Institutes of Health; 2003. NIH publication 02 -3782. Available at: http: www. alzheimers. org/unraveling/index. htm. Accessed January 10, 2005. Alzheimer’s Association. Available at: http: //www. alz. org/About. AD/Stages. asp. Accessed January 13, 2005.
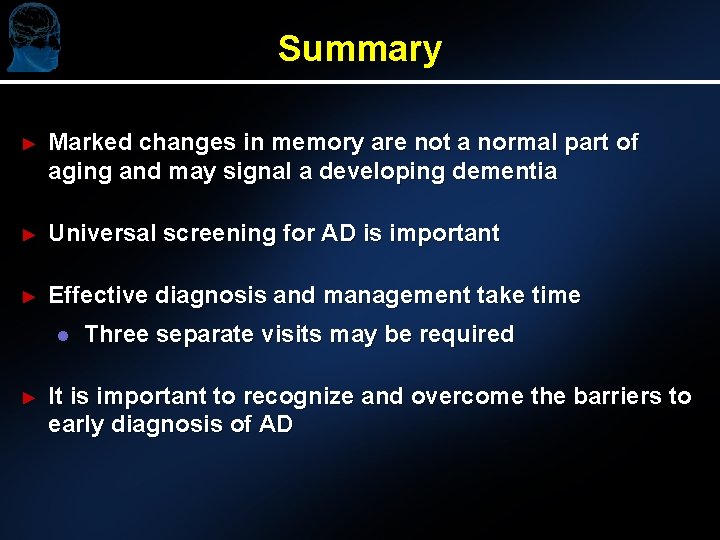
Summary ► Marked changes in memory are not a normal part of aging and may signal a developing dementia ► Universal screening for AD is important ► Effective diagnosis and management take time l ► Three separate visits may be required It is important to recognize and overcome the barriers to early diagnosis of AD
 Communicable disease and non communicable disease
Communicable disease and non communicable disease Georgia alzheimers planning
Georgia alzheimers planning Fast score dementia
Fast score dementia Alzheimers sjukdom
Alzheimers sjukdom Alzheimers nz conference 2020
Alzheimers nz conference 2020 Site:slidetodoc.com
Site:slidetodoc.com Alzheimers society contented dementia
Alzheimers society contented dementia Alzheimer's eye test joke
Alzheimer's eye test joke Welcome to teen challenge uk - teen challenge uk
Welcome to teen challenge uk - teen challenge uk Multicullar
Multicullar Papercut job tickerting print software
Papercut job tickerting print software Introduction product overview
Introduction product overview Introduction product overview
Introduction product overview Introduction product overview
Introduction product overview Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Chụp tư thế worms-breton
Chụp tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ 101012 bằng
101012 bằng