Narrative Medicine literature and family medicine education Dr


- Slides: 28
Narrative Medicine, literature and family medicine education Dr. Leonard Bloom Dr. Denice Lewis Dr. Alan Ng Faculty Retreat, Department of Family Medicine, University of Ottawa Calabogie, ON, October 21, 2018
Questions and Intended Learning Outcomes Why are medical humanities important? Why is narrative medicine important? How can close reading of short stories help me as a teacher of family medicine?
Case #1 Doree is a 23 year old woman who is being seen for the first time by your resident, Dr. Ash. She presents to the urgent care clinic that your practice runs to see same day issues-the appointment system is designed to be brief with 10 minutes allowed for each appointment. Doree comes in with central abdominal pain and bloating.
Dr. Ash looks at the chart and notes Doree has never been seen here before. Dr. Ash takes a brief history and learns that she has had these symptoms for about a year and a half, they are quite troubling and now interfering with her ability to work. She also mentions she has been to walk-in clinics on three previous occasions with this problem and had an ultrasound ordered which showed‘nothing significant’.
There are no obvious red flag symptoms (weight loss, blood in stool, vomiting). She was given pantoprazole by the walk-in doctor but 2 months later she still feels the same. Her examination is unremarkable.
Dr. Ash sits back in her chair, wondering what to do next. She is already running 20 minutes behind and the waiting room is full. As her preceptor, how would advise Dr. Ash?
Case #2 Shoba is a 35 year old woman with chest pain and palpitations. She presents to the urgent care clinic and is being seen by Dr. Ash, your resident. She does not attend frequently but in her chart you see two notes from the ER-both visits within the last 2 weeks. The first note concluded she had ‘non-cardiac chest pain’ and she was sent home, but she returned to the ER 4 days later with the same symptoms and was seen by cardiology.
She had a number of tests including and ECG and stress test, blood work, and the diagnosis was ‘non-cardiac chest pain’. She was put on a trial of omeprazole and asked to follow up with her family physician.
Dr. Ash takes a brief history. Shoba appears anxious but denies any major stress. Cardiovascular examination is normal. Shoba is worried about her heart. Dr. Ash sits back in her chair wondering what to do next. Now she is really running further behind. As Dr. Ash’s preceptor, what would you advise her?
Narrative medicine and the curriculum CANMEDs Roles and competencies • Communication skills • Patient-centred care • Biopsychosocial paradigms
Patient concerns • • • Doctors don’t listen Doctors appear disinterested Doctors interrupt Doctors make assumptions Doctors don’t address patient concerns
The doctor’s defence • • Complaining about ‘difficult patients’ Pressures of time Pressures of numbers/list size Travesties of consumer medicine
The role of narrative medicine Rita Charron-the 4 divides There are 4 divides that contribute to the disconnection that might occur between the doctor and the patient
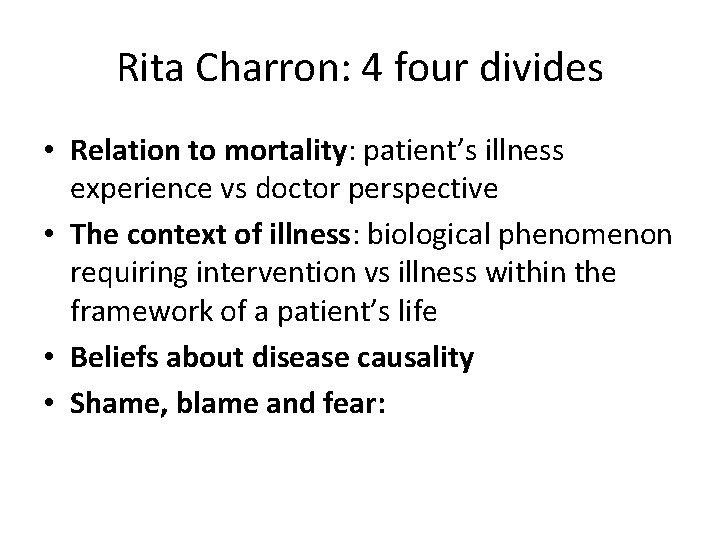
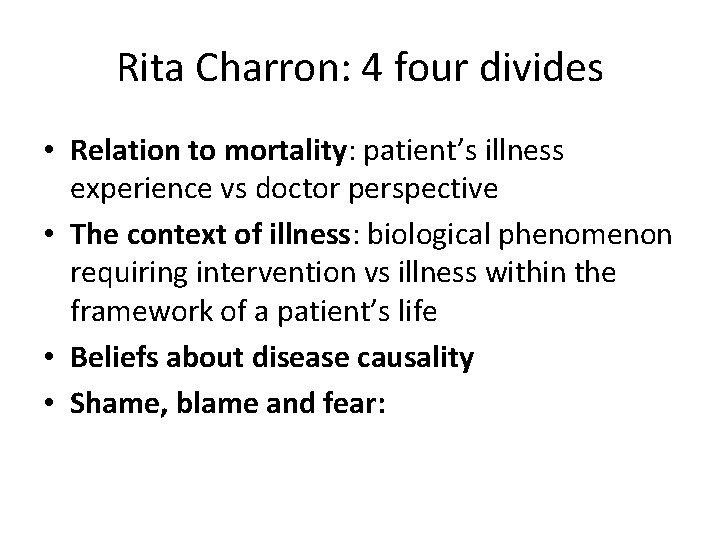
Rita Charron: 4 four divides • Relation to mortality: patient’s illness experience vs doctor perspective • The context of illness: biological phenomenon requiring intervention vs illness within the framework of a patient’s life • Beliefs about disease causality • Shame, blame and fear:


John Launer-the 7 Cs • • Conversations Curiosity Context Complexity Challenge Caution Care
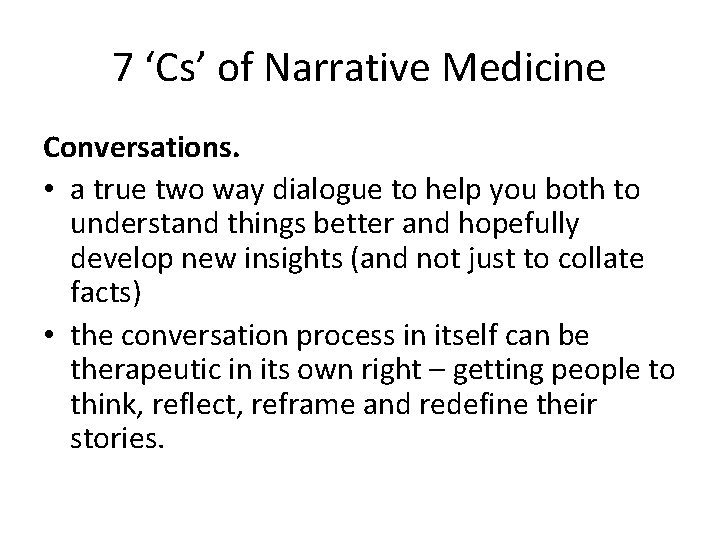
7 ‘Cs’ of Narrative Medicine Conversations. • a true two way dialogue to help you both to understand things better and hopefully develop new insights (and not just to collate facts) • the conversation process in itself can be therapeutic in its own right – getting people to think, reflect, reframe and redefine their stories.
Curiosity • genuinely being interested and curious. • queries you raise will help the other to think and reflect – and perhaps helping them to reframe and redefine their stories.
Contexts • context of their families, friends, community, beliefs, values and so on) • how have they decided to ‘frame’ their story?
Complexity • Life is not simple. So why do we (doctors) always try to fix life’s problems with concrete and rigid solutions? • A sense of complexity gets away from fixed ideas of cause and effect, unchangeable positions and over-concrete solutions
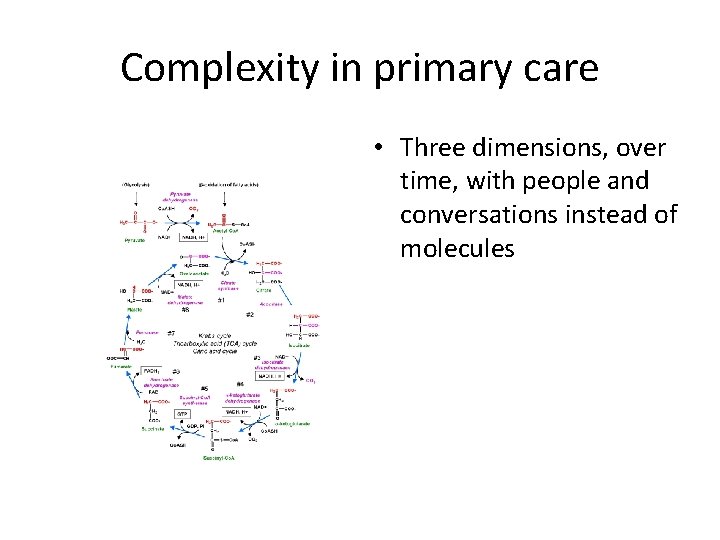
Complexity in primary care • Three dimensions, over time, with people and conversations instead of molecules
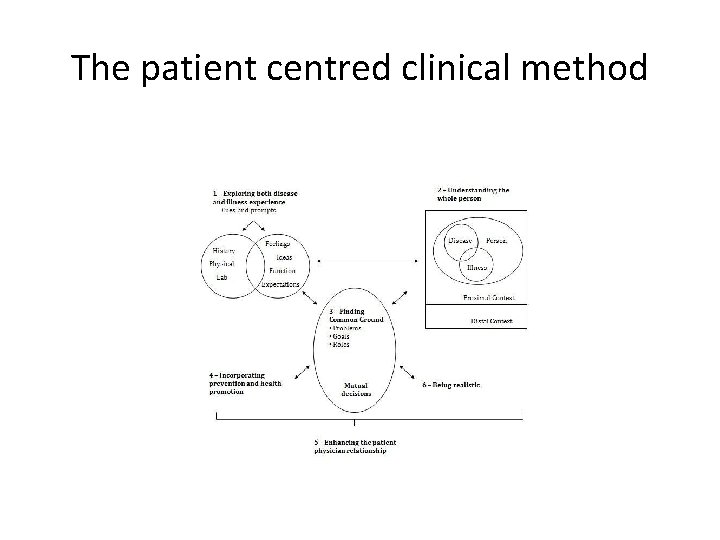
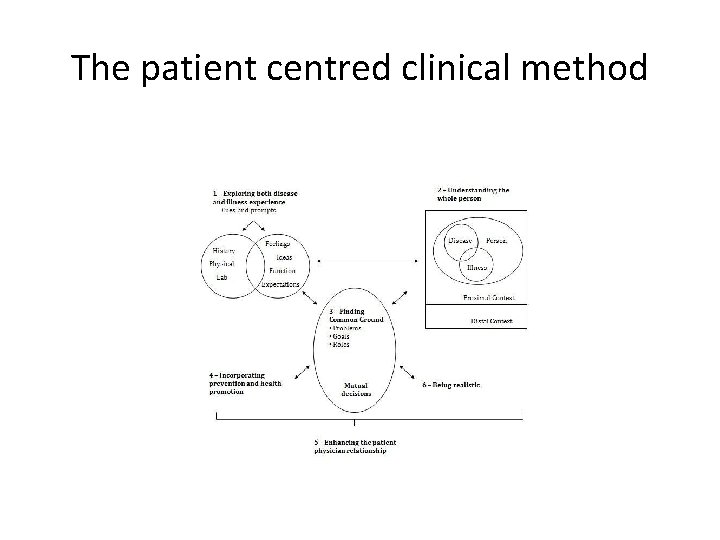
The patient centred clinical method
Creativity/challenge. • Can you help patient create a better account of what’s going on for them? • Can you help them make a better story? • Better stories create better realities.
Caution Sometimes, patients come in with straightforward problems/questions for which they want straight forward answers.
Care. • You have to show genuine care for the narrative approach to work. • That means being truly listening, showing respect, treating others as equal and showing a true genuine interest in wanting to help the person.
Close reading-why bother? • Complex texts: Close reading helps residents to read texts that may be above their comfort level (complex patients) • ‘Gist Reading’: Close reading defends against gist reading, a term referring to understanding the main idea of a text and discussing it –there is more to a text than just the main idea (disease vs illness experience) • Language sensitivity: Close reading develops language sensitivity- syntax, rhythm and structure-like ‘number sense’ in math, or ‘patient sense’ when communicating with patients, ‘reading sense’ develops an ear for tone and the subtle moves that create it
Further reading • Charon R. Narrative Medicine. Oxford University Press 2006 • Stewart M, Brown JB et al. Patient Centred Medicine. Radcliffe 2014 • Freeman T, Mc. Whinney’s Textbook of Family Medicine 4 th ed. Oxford University Press 2016 • Launer J. Narrative-based primary care> Radcliffe 2002
 Duke medicine grand rounds
Duke medicine grand rounds Fictional narrative writing
Fictional narrative writing Difference between narrative and story
Difference between narrative and story Conjugal family
Conjugal family Types of family in community medicine
Types of family in community medicine Principles of family medicine
Principles of family medicine Halifax family medicine residency
Halifax family medicine residency Meritus family medicine
Meritus family medicine Family medicine fellowship
Family medicine fellowship Milestones family medicine
Milestones family medicine Janalynn beste md
Janalynn beste md Principles of primary care
Principles of primary care Family medicine def
Family medicine def Internal medicine shelf exam passing score
Internal medicine shelf exam passing score Function of the family
Function of the family Unfunded residency positions
Unfunded residency positions Af williams family medicine center
Af williams family medicine center Kaiser san diego family medicine residency
Kaiser san diego family medicine residency Family medicine in ethiopia
Family medicine in ethiopia Cabarrus family medicine concord
Cabarrus family medicine concord Uthscsa family medicine residency
Uthscsa family medicine residency Slu ent residents
Slu ent residents Family apgar
Family apgar Dr riaz qureshi
Dr riaz qureshi Isu family medicine
Isu family medicine Urt
Urt Family medicine meaning
Family medicine meaning Dr margaret wiedmann
Dr margaret wiedmann Screem res scoring
Screem res scoring