MULTIPLE SCLEROSIS Dr Sadik AL Ghazawi Associated Professor


- Slides: 76
MULTIPLE SCLEROSIS Dr Sadik AL Ghazawi Associated Professor Neurologist MRCP, FRCP UK
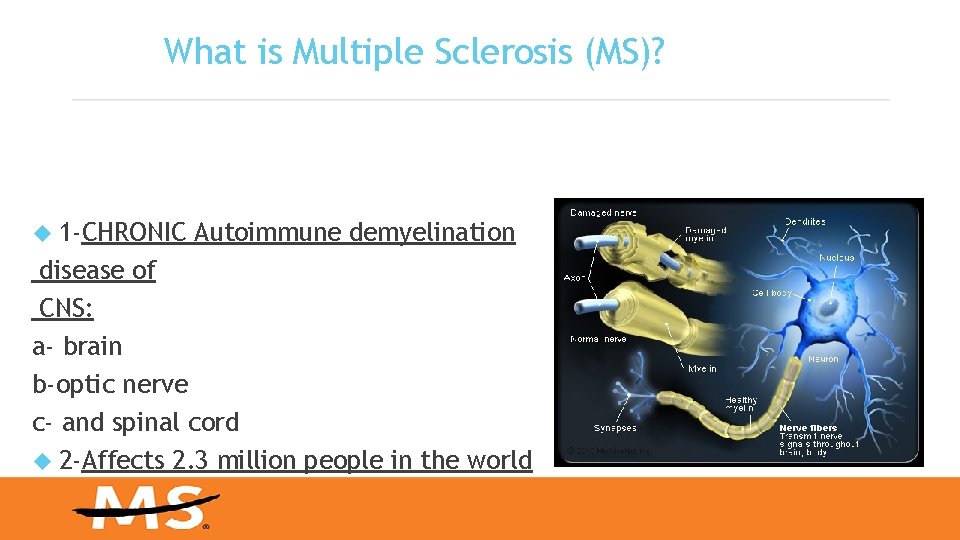
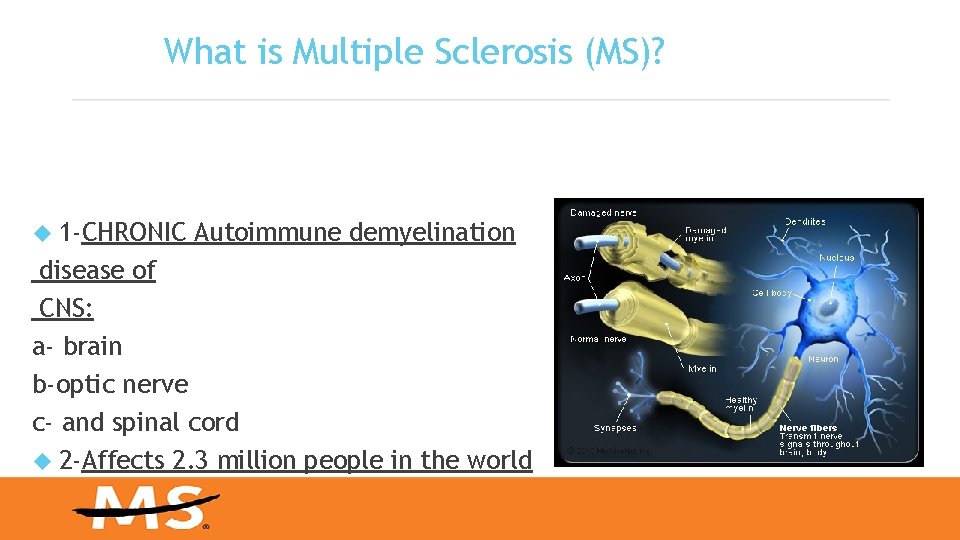
What is Multiple Sclerosis (MS)? 1 -CHRONIC Autoimmune demyelination disease of CNS: a- brain b-optic nerve c- and spinal cord 2 -Affects 2. 3 million people in the world
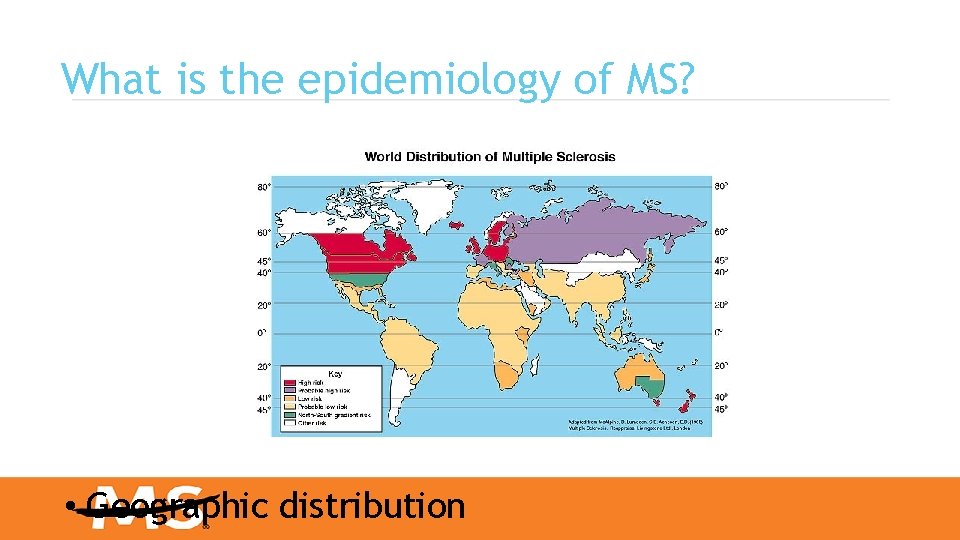
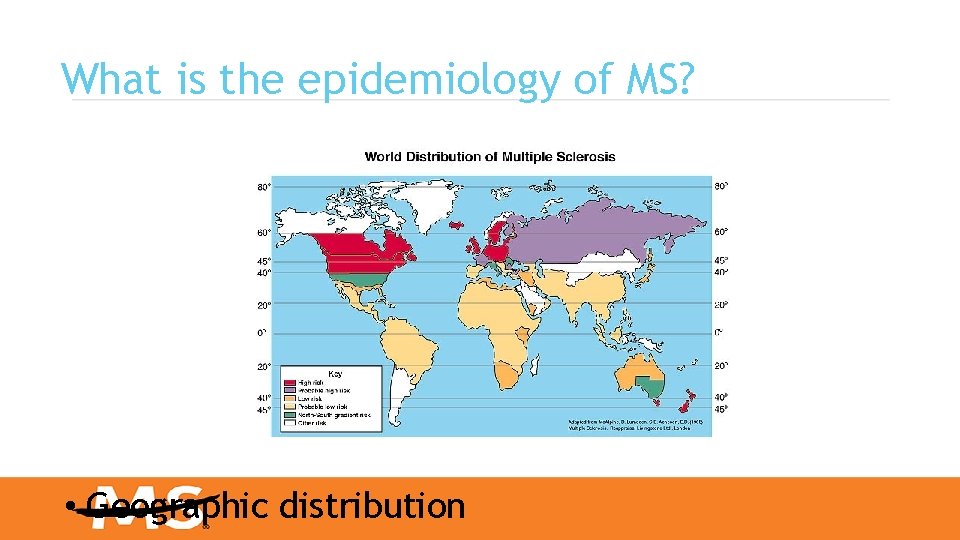
What is the epidemiology of MS? • Geographic distribution
What are the possible risk factors? 1 -Infections : viral , bacterial, fungal. 2 -Age: 15 yr. -45 yr. 3 -Gender : female: male 3: 1 4 -Genetic Factors 5 -DR 15 haplotype 6 -Autoimmune diseases 7 -Race 8 -Climate
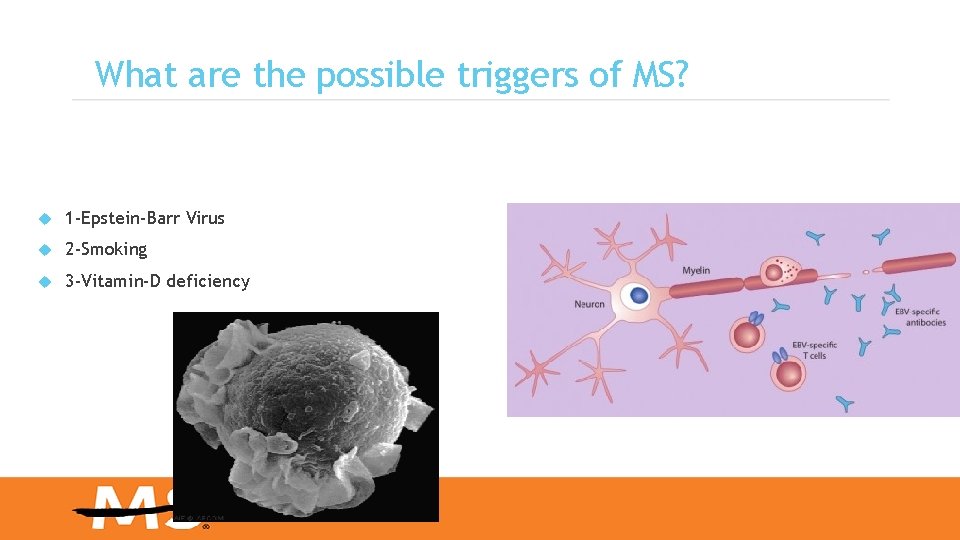
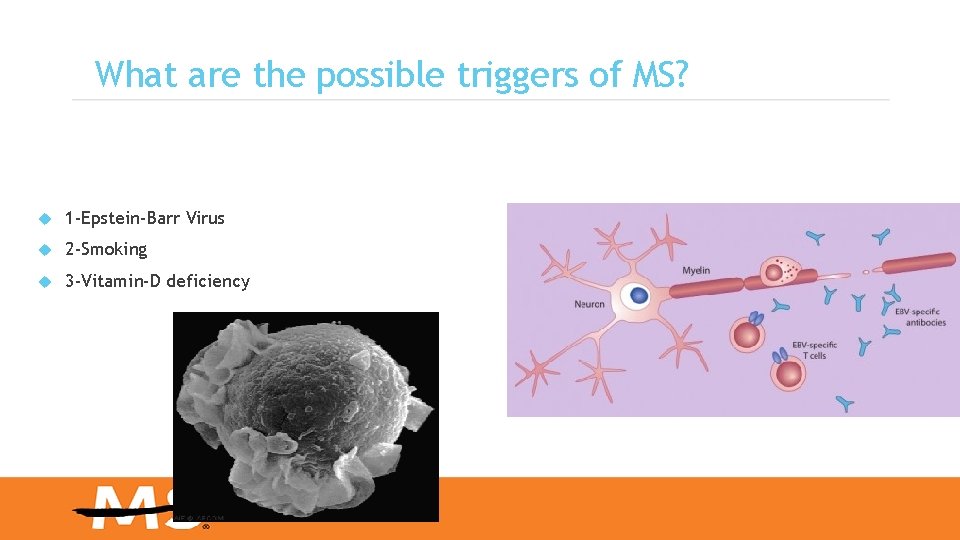
What are the possible triggers of MS? 1 -Epstein-Barr Virus 2 -Smoking 3 -Vitamin-D deficiency
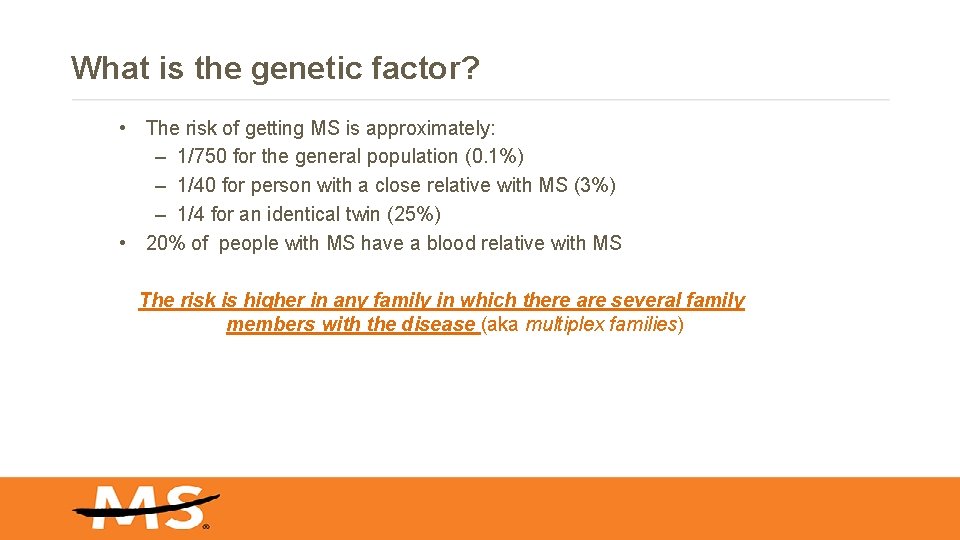
What is the genetic factor? • The risk of getting MS is approximately: – 1/750 for the general population (0. 1%) – 1/40 for person with a close relative with MS (3%) – 1/4 for an identical twin (25%) • 20% of people with MS have a blood relative with MS The risk is higher in any family in which there are several family members with the disease (aka multiplex families)
Genetics 1 -the probability of developing the disease is higher in relatives of an affected person, with a greater risk among those more closely related. EXAMPLE identical twins both are affected about 30% of the time, while around 5% for nonidentical twins and 3 -if both parents are affected the risk in their children is 10 times that of the general population. 4 - MS is also more common in some ethnic groups than others
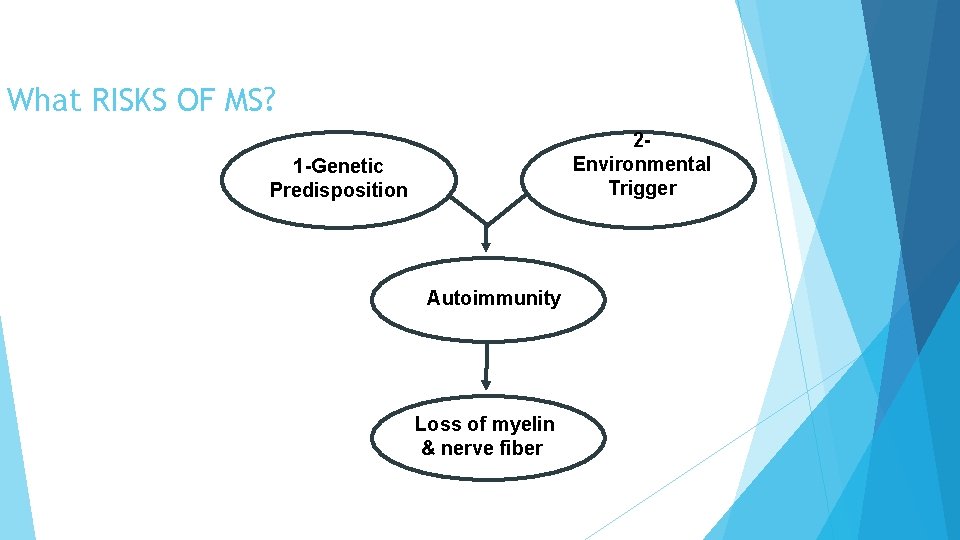
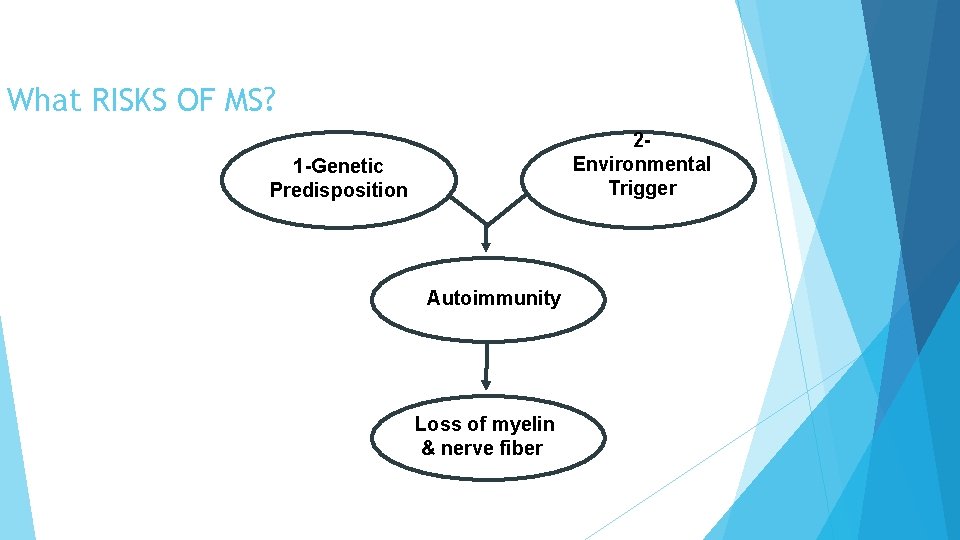
What RISKS OF MS? 2 Environmental Trigger 1 -Genetic Predisposition Autoimmunity Loss of myelin & nerve fiber
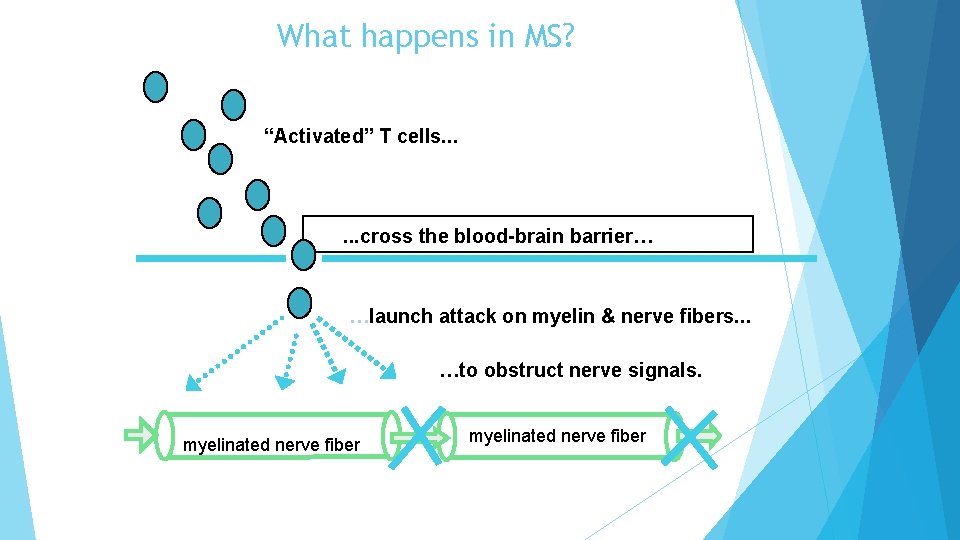
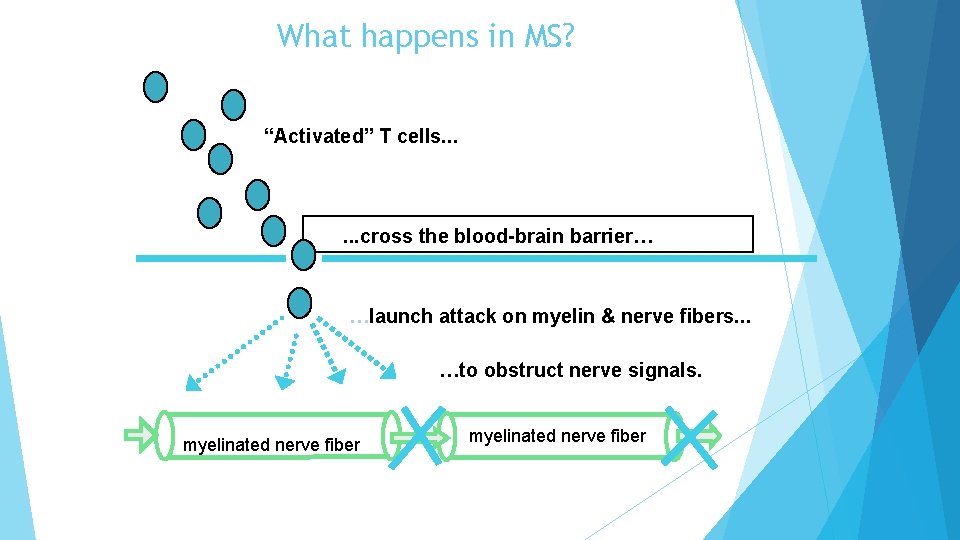
What happens in MS? “Activated” T cells. . . cross the blood-brain barrier… …launch attack on myelin & nerve fibers. . . …to obstruct nerve signals. myelinated nerve fiber
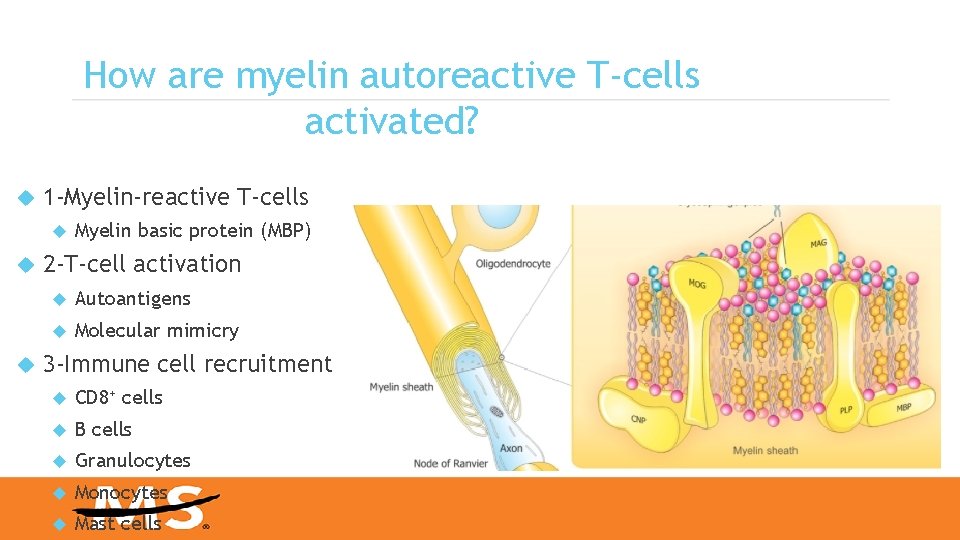
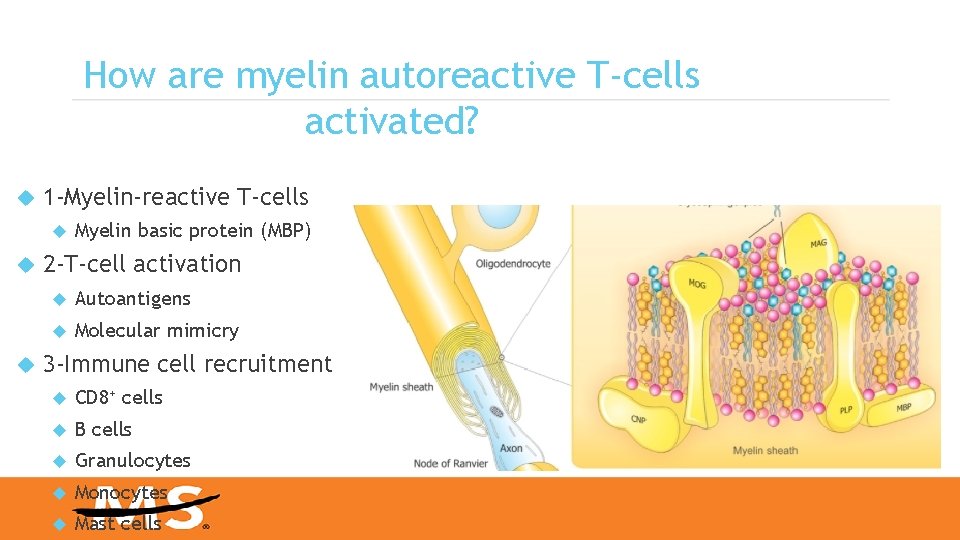
How are myelin autoreactive T-cells activated? 1 -Myelin-reactive T-cells Myelin basic protein (MBP) 2 -T-cell activation Autoantigens Molecular mimicry 3 -Immune cell recruitment CD 8+ cells B cells Granulocytes Monocytes Mast cells
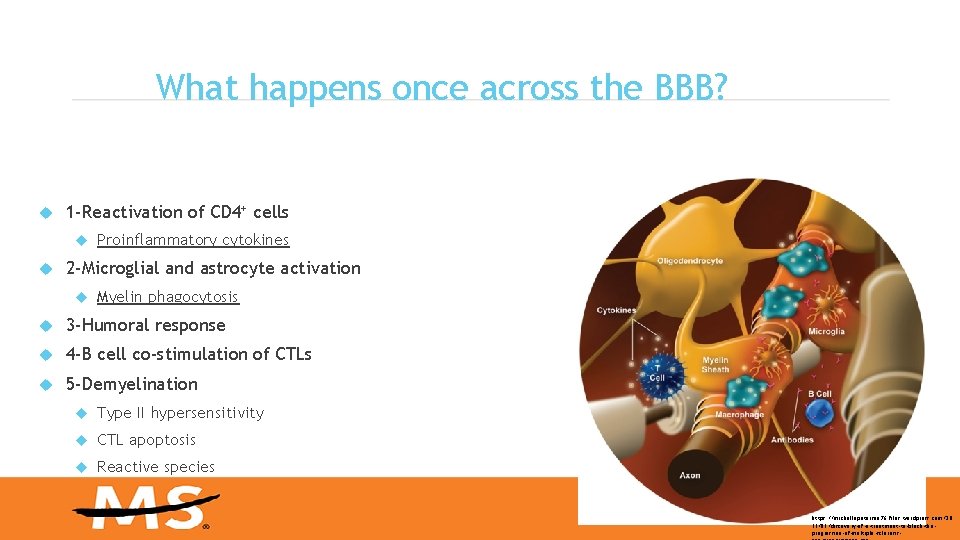
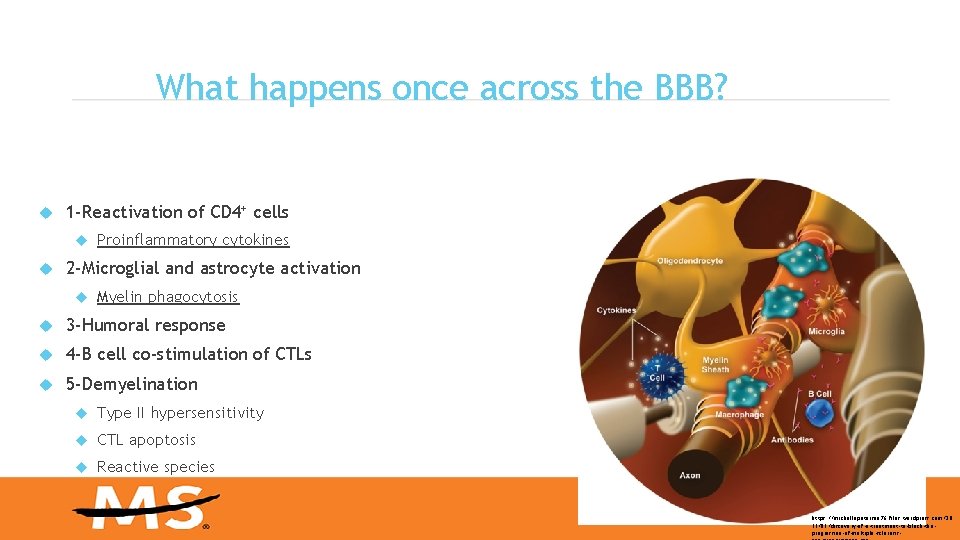
What happens once across the BBB? 1 -Reactivation of CD 4+ cells Proinflammatory cytokines 2 -Microglial and astrocyte activation Myelin phagocytosis 3 -Humoral response 4 -B cell co-stimulation of CTLs 5 -Demyelination Type II hypersensitivity CTL apoptosis Reactive species https: //michellepetersen 76. files. wordpress. com/20 15/05/discovery-of-a-treatment-to-block-theprogression-of-multiple-sclerosis-
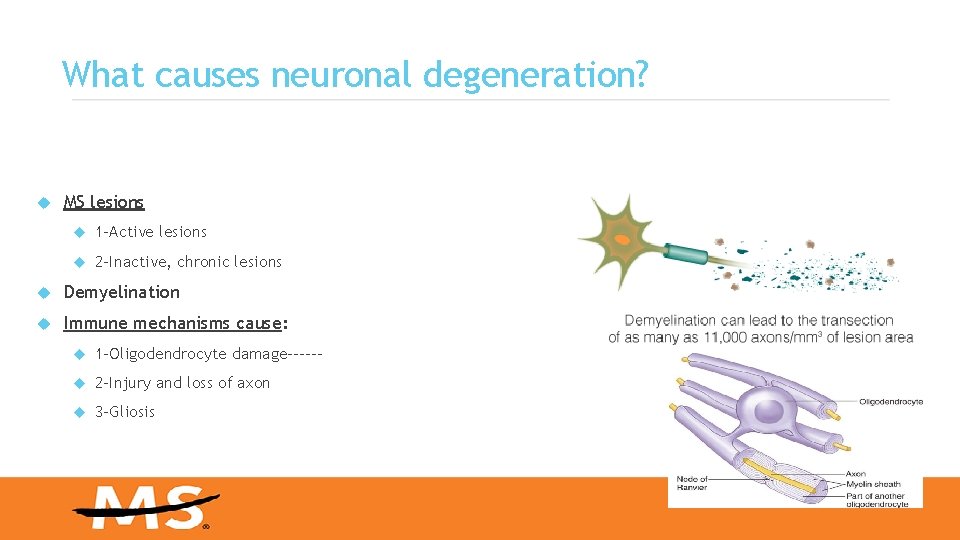
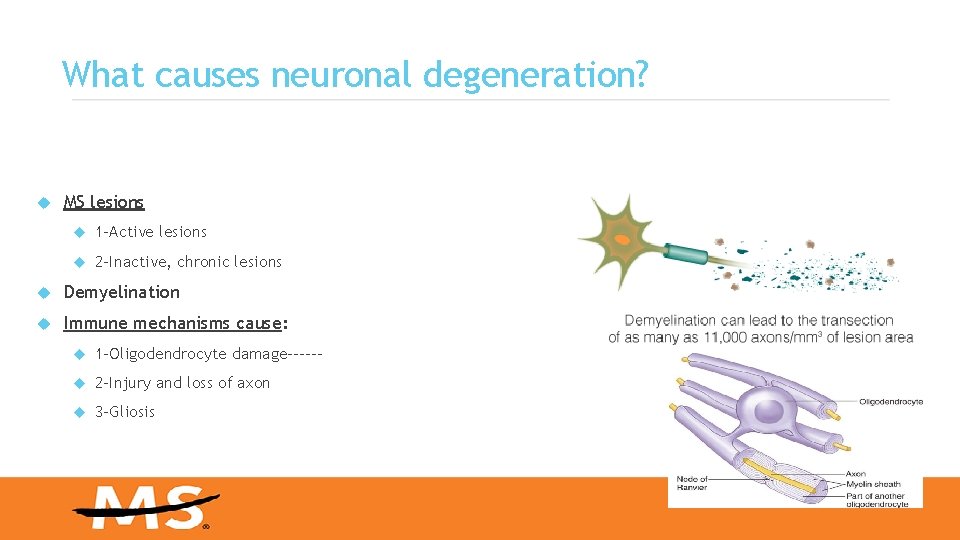
What causes neuronal degeneration? MS lesions 1 -Active lesions 2 -Inactive, chronic lesions Demyelination Immune mechanisms cause: 1 -Oligodendrocyte damage------ 2 -Injury and loss of axon 3 -Gliosis
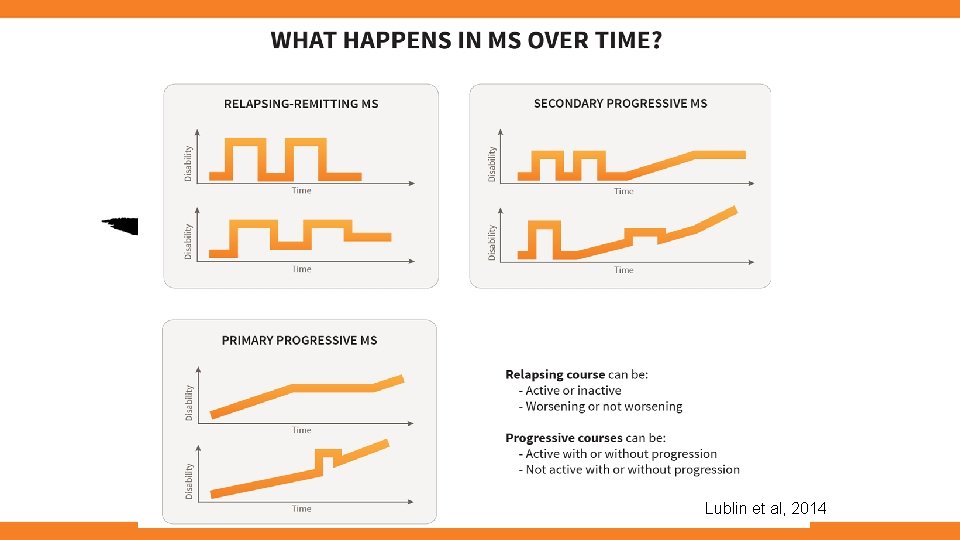
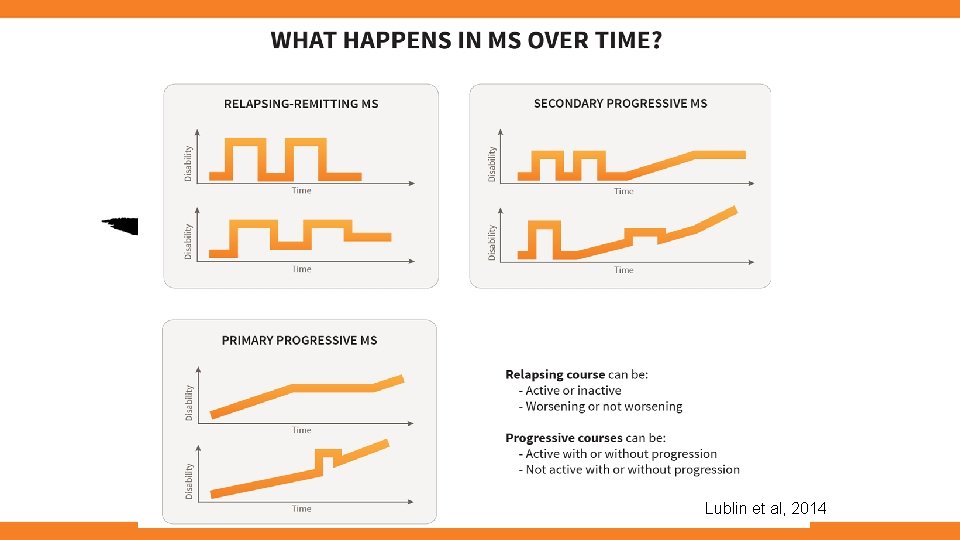
Lublin et al, 2014
The relapsing-remitting subtype. 1 ---80 -85 present. 2 ---female predominant. 3 -- characterized by unpredictable rapid onset relapses followed by period of months or years of partial or complete recovery.
Ø 4 --Attack is a symptoms or objectively observed signs suggestive demyelination process with duration of at least 24 hours, in the absence of fever or infection. Ø 5 -For paroxysmal symptoms (such as paroxysmal dysarthria, tonic spasms, or paroxysmal sensory symptoms) to be considered an attack, must be recurrent over at least 24 hours.
6 --Once MS has been established , we must evaluate for evidence of ination in space( DIS) (multiple areas) , and for dissemination in time( DIT)(ongoing disease activity over time). dissem
7 -- Deficits that occur during attacks may either A-Resolve or leave problems in about 40% of attacks. B-being more common the longer a person has had the disease.
8 -When deficits always resolve between attacks, this is sometimes referred to as benign MS, although people will still build up some degree of disability in the long term.
Secondary Progressive MS • 1 -Majority of RRMS many years following onset • 2 -Progressive impairment (spastic gait disturbance) between or in absence of attacks – with ongoing relapses – Substantial ongoing on new MRI inflammatory lesions
Ø 1 -25% to 40% of patients with relapsing remitting MS go on to a secondary progressive course after an average of about 20 years. Ø 2 -diagnosed when, after an initial relapsing-remitting course, a patient demonstrates disease progression independent of relapses for at least 6 months.
Ø 3 -deterioration with respect to gait, balance, spasticity, and bladder ction , Many patients experience cognitive decline. fun
Primary Progressive MS • Presents with progressive myelopathic gait, cerebellar ataxia or cognitive impairment without clear history of any clinical attacks • Clinical progression must be for at least 1 year and accompanied by a combination of brain&spinal abnormalities and/or CSF abnormalities consistent with MS
The primary progressive subtype= 1 - occurs in approximately 10– 20% of individuals, with no remission after the initial symptoms. 2 - It is characterized by progression of disability from onset, with no, or only occasional and minor, remissions and improvements.
3 -10% to 15%. 4 -insidious onset of symptoms followed by gradual deterioration over time. 5 -Clinical disease in these patients typically presents as a progressive myelopathy, and less frequently as a brainstem or cerebellar syndrome.
6 -Older. 7 -no clear gender predominance 8 -MRI lesions : Ø fewer in number Øless likely to enhance with gadolinium compared to relapsing-remitting MS.
9 -The usual age of onset for the primary progressive subtype is later than of the relapsing-remitting subtype. 10 -- It is similar to the age that secondary progressive usually begins in relapsing-remitting MS, around 40 years
Clinically Isolated Syndrome (CIS) 1 -A first neurologic event suggestive of demyelination 2 -Individuals with CIS are at high risk for developing clinically definite MS if the neurologic event is accompanied by multiple, clinically silent (asymptomatic) lesions on MRI typical of MS 27
CLINICALLY ISOLATED SYNDROM (CIS) 1 -the condition begins in 85% of cases as clinically isolated syndrome (CIS). 2 --45% having motor or sensory problems. 3 --20% having optic neuritis, and 28
4 -10% having symptoms related brain stem dysfunction, 5 -while the remaining 25% have more than one of the previous difficulties 29
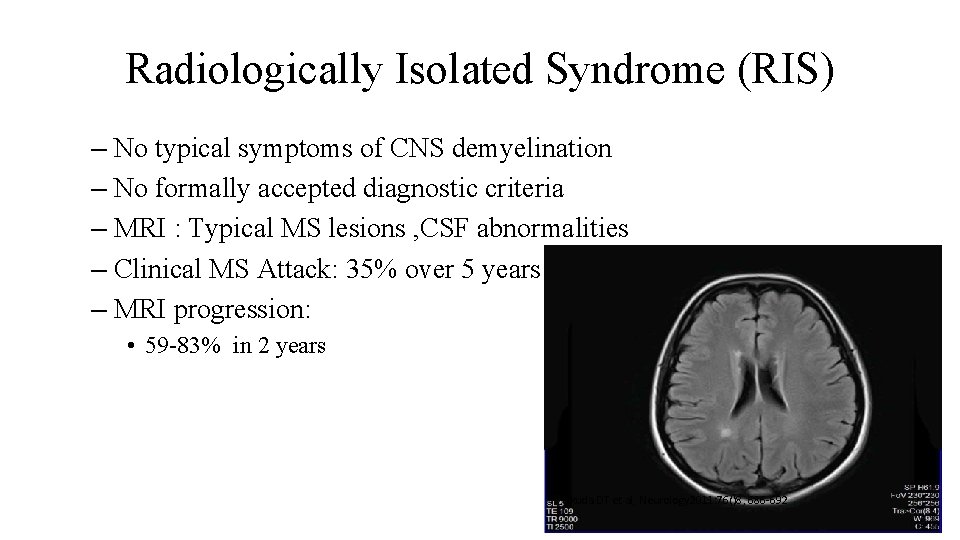
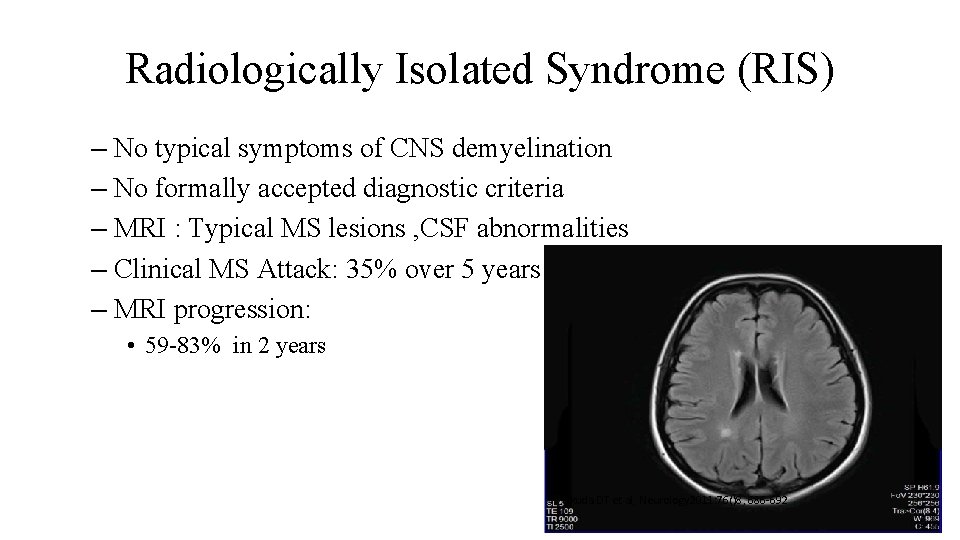
Radiologically Isolated Syndrome (RIS) – No typical symptoms of CNS demyelination – No formally accepted diagnostic criteria – MRI : Typical MS lesions , CSF abnormalities – Clinical MS Attack: 35% over 5 years – MRI progression: • 59 -83% in 2 years Okuda DT et al, Neurology 2011: 76()8, 686 -692
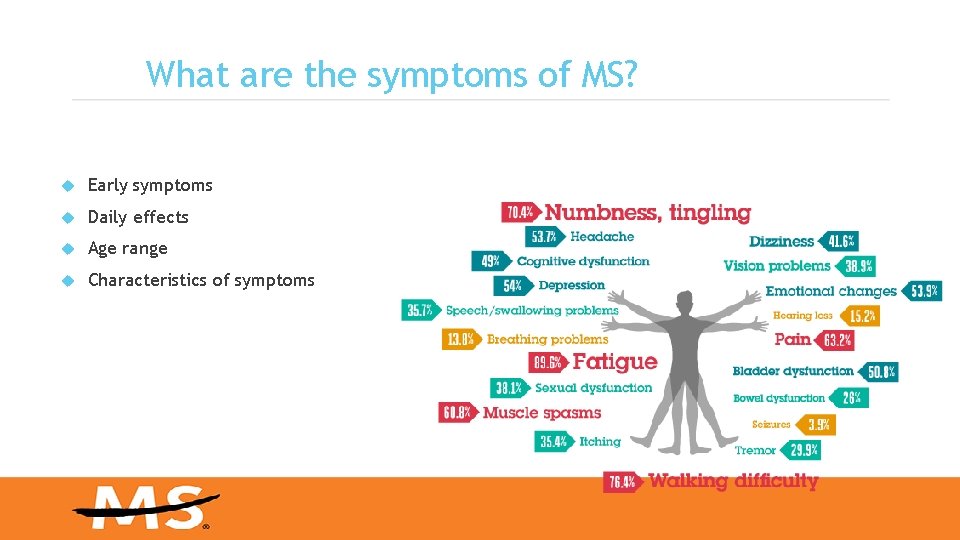
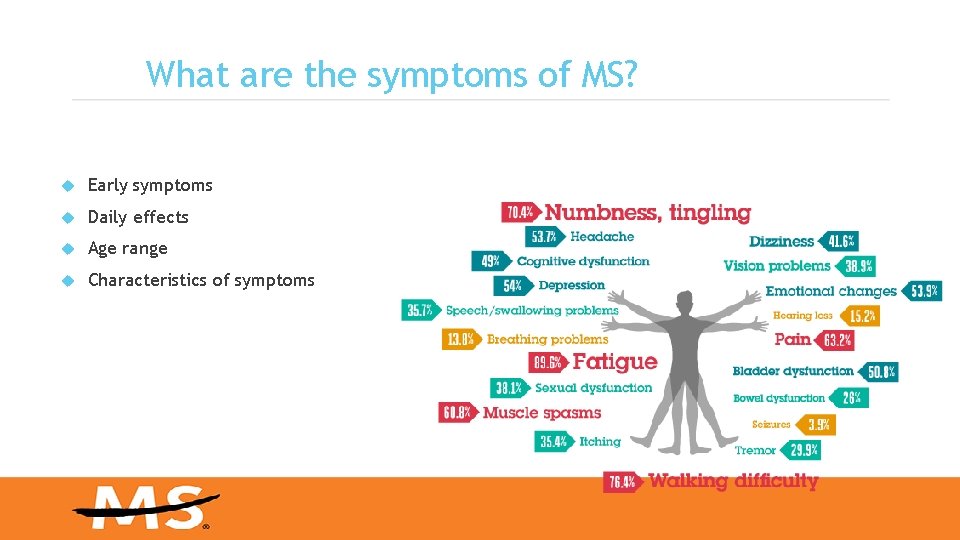
What are the symptoms of MS? Early symptoms Daily effects Age range Characteristics of symptoms
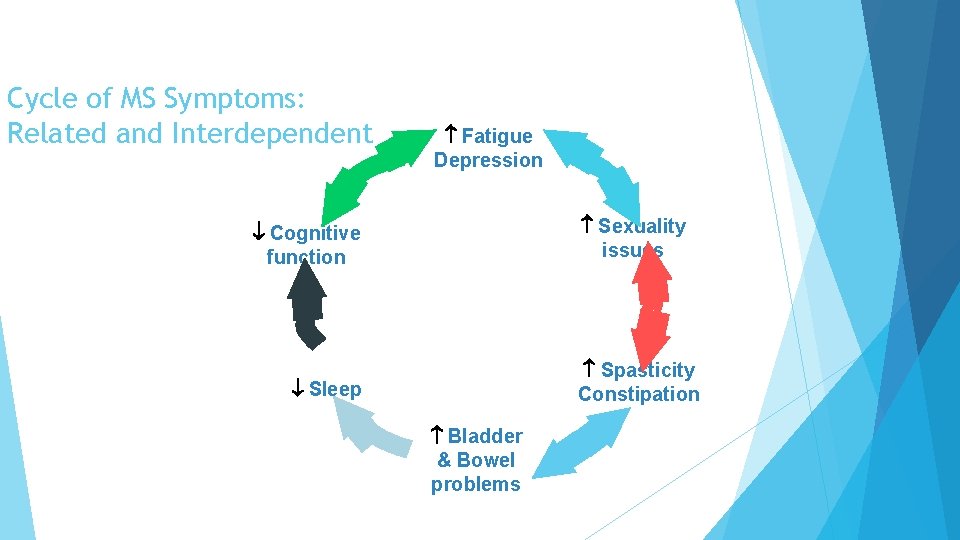
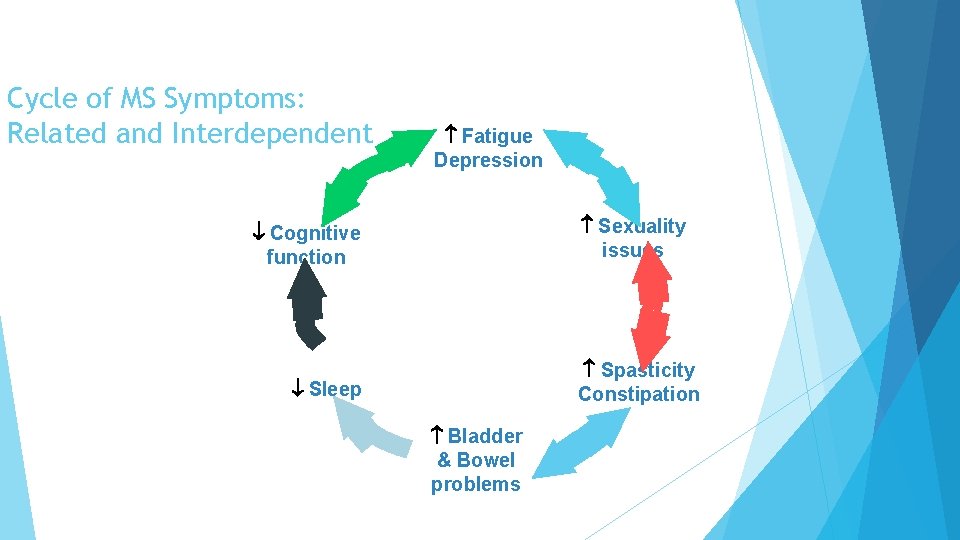
Cycle of MS Symptoms: Related and Interdependent Fatigue Depression Sexuality issues Cognitive function Spasticity Constipation Sleep Bladder & Bowel problems
Features Consistent With MS • • Relapses and remissions Age Onset between ages 15 and 50 Optic neuritis Lhermitte's sign Internuclear ophthalmoplegia Fatigue Uhthoff's phenomenon
How is MS diagnosed? MS is a clinical diagnosis 1 -Medical history 2 -SIGNS And symptoms 3 -Laboratory tests Requires dissemination in time and space: 1 -Space: Evidence of scarring (plaques) in at least two separate areas of the CNS (space) 2 -Time: Evidence that the plaques occurred at different points in time There must be no other explanation
Diagnosis of MS 1 -No single test for diagnosing MS 2 -Usually diagnosed when all other possibilities ruled out 3 -Many tests A-Medical history B-Nervous system functioning C-MRI Mc. Donald criteria D-Evoked potential tests, spinal tap
INITIAL SYMPTOMS 1 - ascending numbness starting in the feet; - bilateral hand numbness; - hemiparesthesia; - dysesthesia in one of the above distributions; - generalized heat intolerance
Sensory systems: 2 --Lhermitte's sign-dysesthetic pain-paresthesia-numbness-dorsal column signs (i. e. , . severe decrease or loss of vibratory sense and proprioception,
Ongoing Symptoms and Signs Motor system: 3 -weakness (variable severity mono- and paraparesis, hemiparesis, quadriparesis)- 4 -increased spasticity resulting in spastic gait 5 -pathologic signs (Babinski's, , Hoffmann, etc. ) -dysarthria
Cerebellar signs 1 -incoordination (dysdiadochokinesia, problems with heel-to-shin test)-slowing of rapid repeating movements-cerebellar ataxia (ataxic gait) 2 -scanning speech- 3 -loss of balance
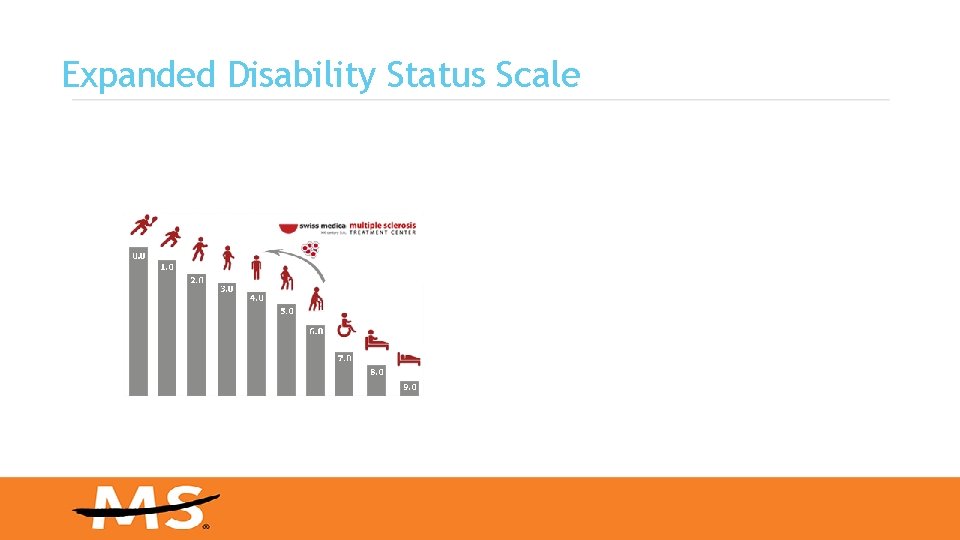
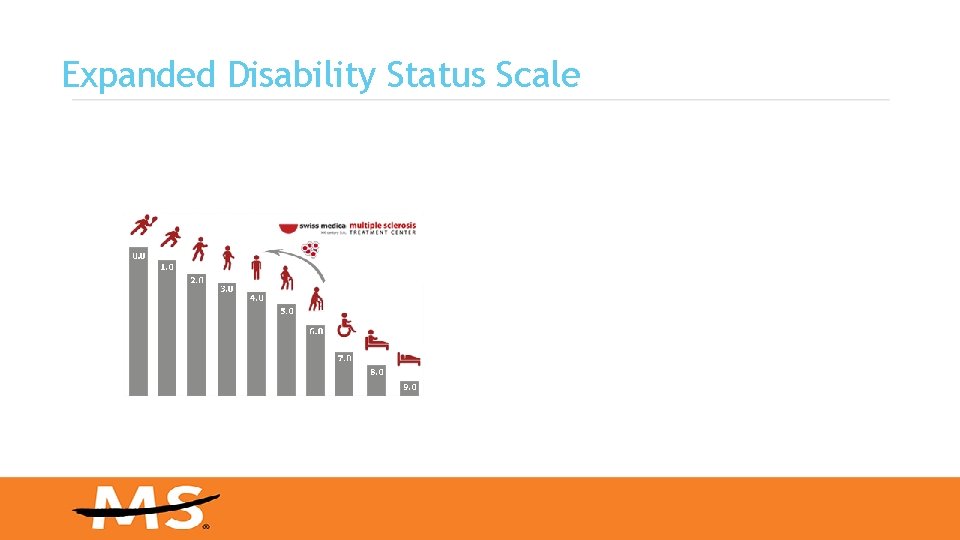
Expanded Disability Status Scale
What tests may be used to help confirm the diagnosis? 1 -Magnetic resonance imaging (MRI) 2 -Visual evoked potentials (VEP) 3 -Lumbar puncture
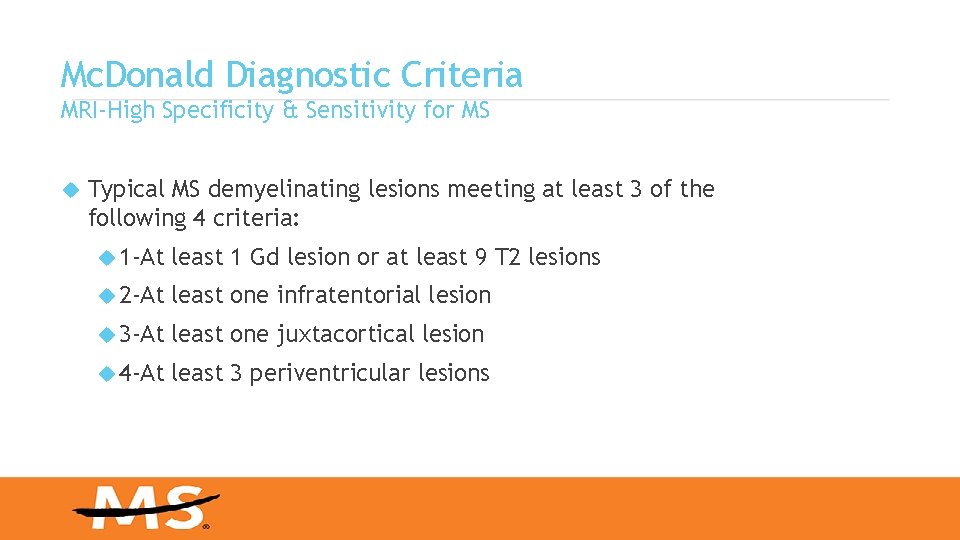
Mc. Donald Diagnostic Criteria MRI-High Specificity & Sensitivity for MS Typical MS demyelinating lesions meeting at least 3 of the following 4 criteria: 1 -At least 1 Gd lesion or at least 9 T 2 lesions 2 -At least one infratentorial lesion 3 -At least one juxtacortical lesion 4 -At least 3 periventricular lesions
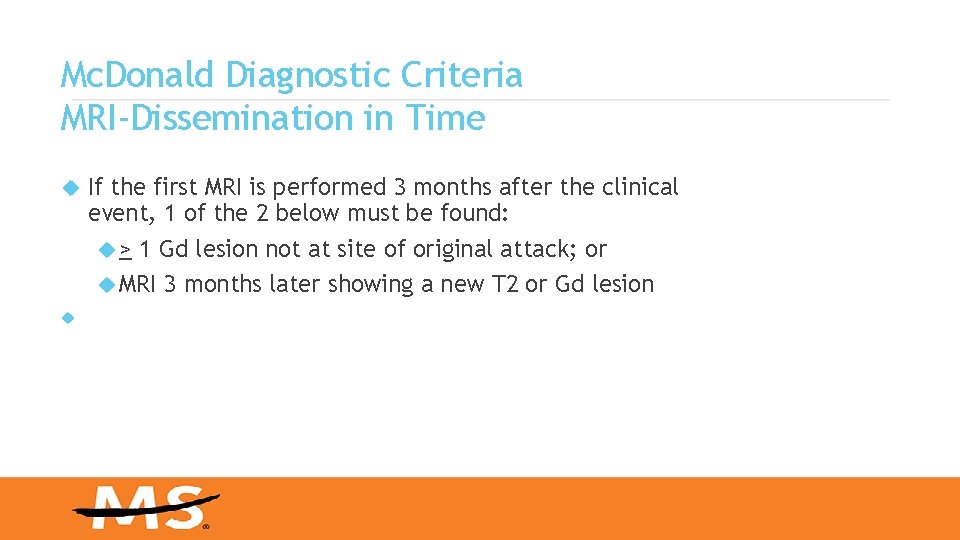
Mc. Donald Diagnostic Criteria MRI-Dissemination in Time If the first MRI is performed 3 months after the clinical event, 1 of the 2 below must be found: > 1 Gd lesion not at site of original attack; or MRI 3 months later showing a new T 2 or Gd lesion
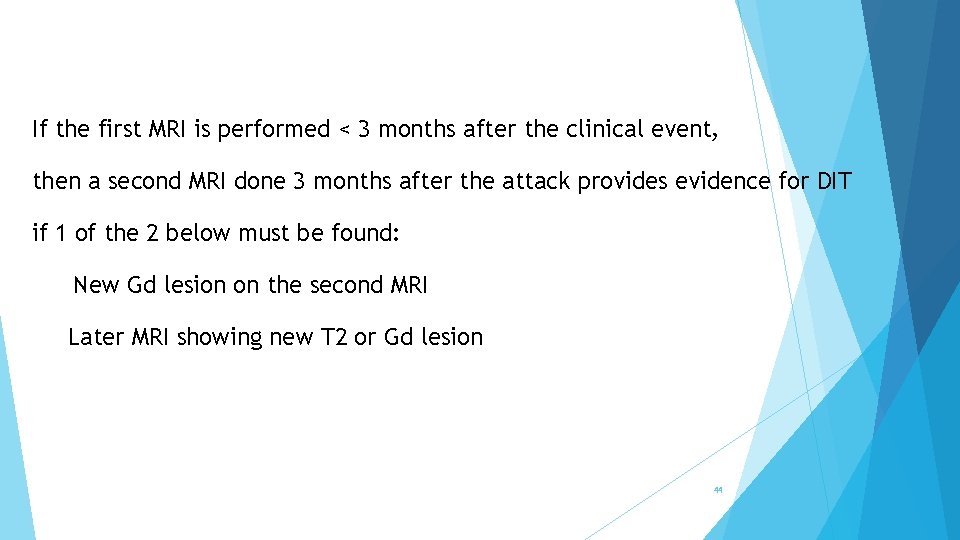
If the first MRI is performed < 3 months after the clinical event, then a second MRI done 3 months after the attack provides evidence for DIT if 1 of the 2 below must be found: New Gd lesion on the second MRI Later MRI showing new T 2 or Gd lesion 44
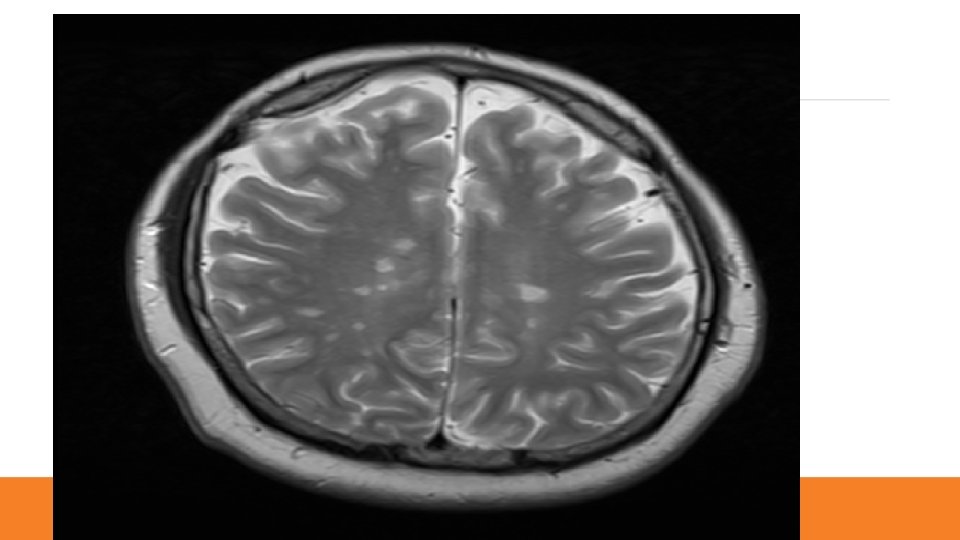
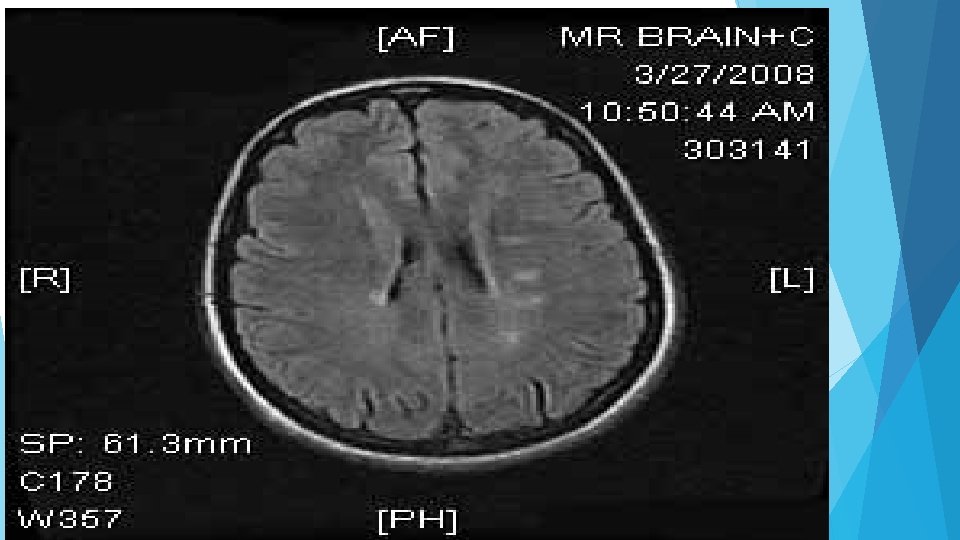
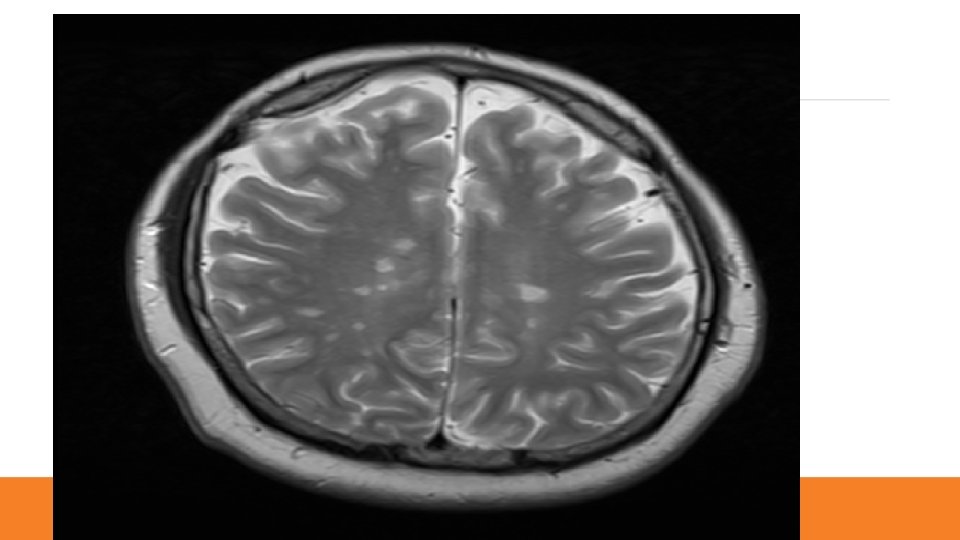
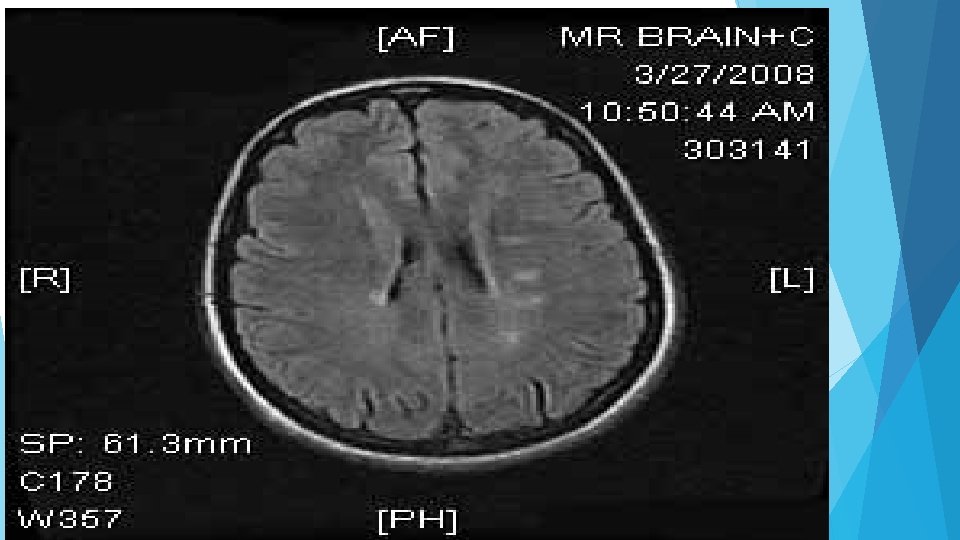
Case : MRI Brain


Case 2: MRI Spine
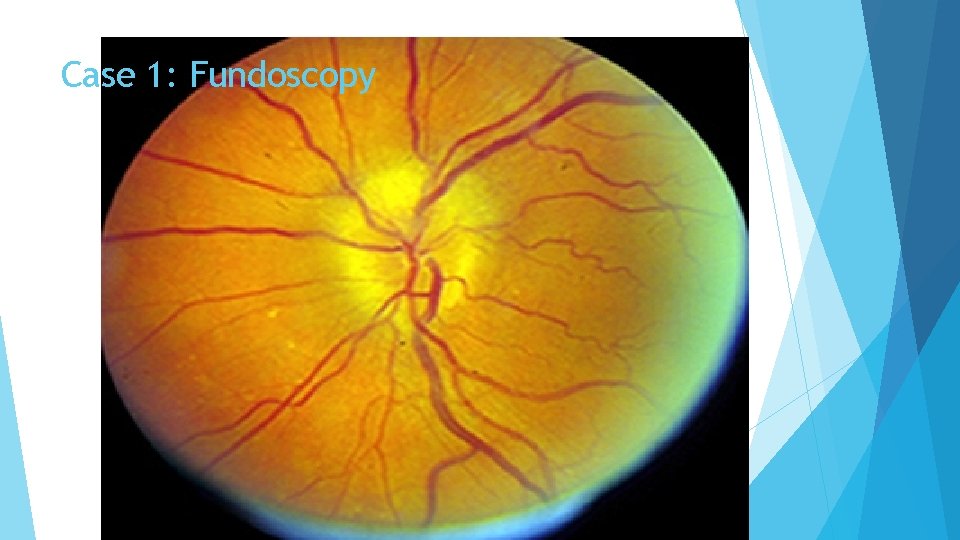
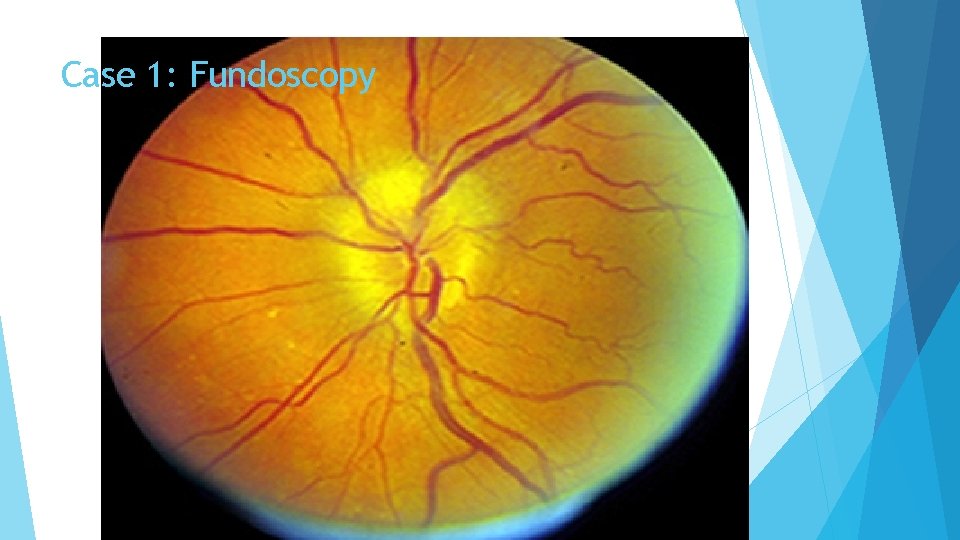
Case 1: Fundoscopy
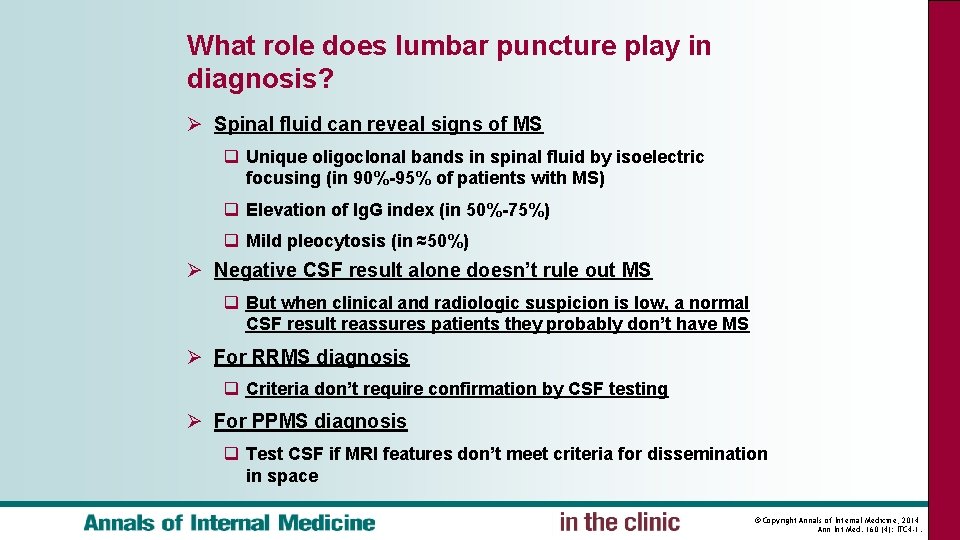
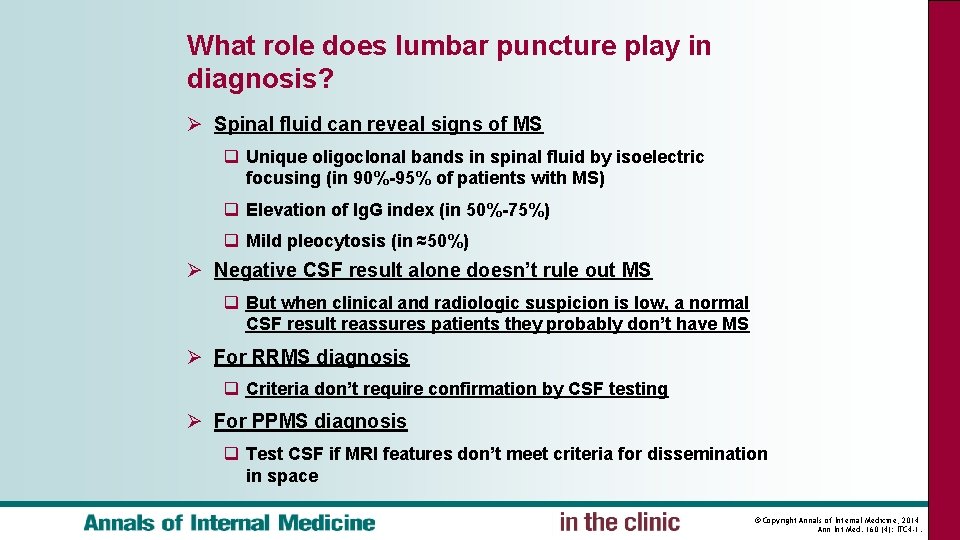
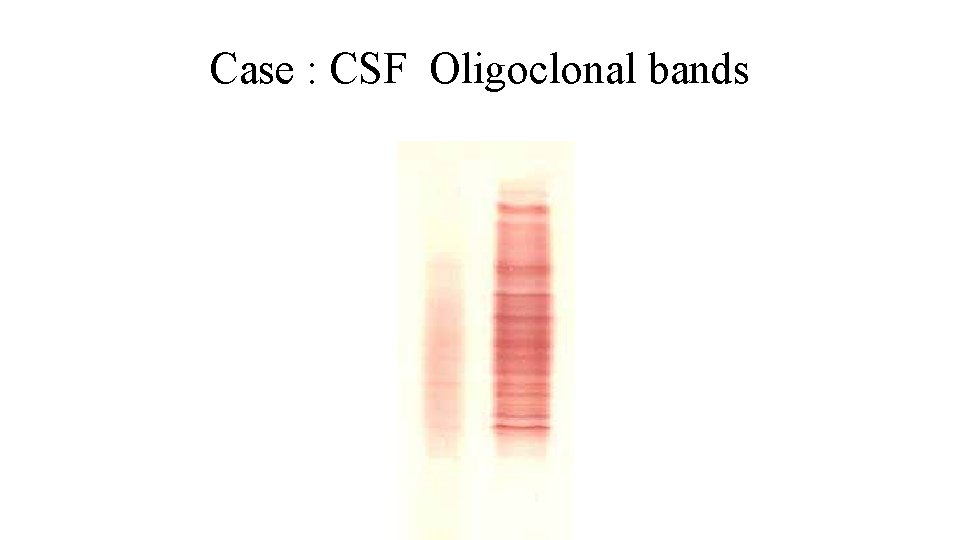
What role does lumbar puncture play in diagnosis? Ø Spinal fluid can reveal signs of MS q Unique oligoclonal bands in spinal fluid by isoelectric focusing (in 90%-95% of patients with MS) q Elevation of Ig. G index (in 50%-75%) q Mild pleocytosis (in ≈50%) Ø Negative CSF result alone doesn’t rule out MS q But when clinical and radiologic suspicion is low, a normal CSF result reassures patients they probably don’t have MS Ø For RRMS diagnosis q Criteria don’t require confirmation by CSF testing Ø For PPMS diagnosis q Test CSF if MRI features don’t meet criteria for dissemination in space © Copyright Annals of Internal Medicine, 2014 Ann Int Med. 160 (4): ITC 4 -1.
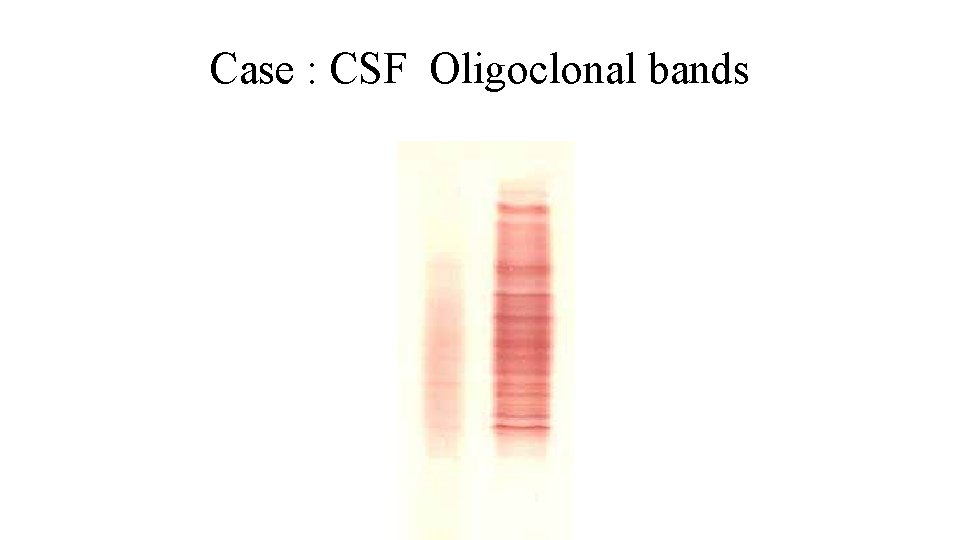
Case : CSF Oligoclonal bands
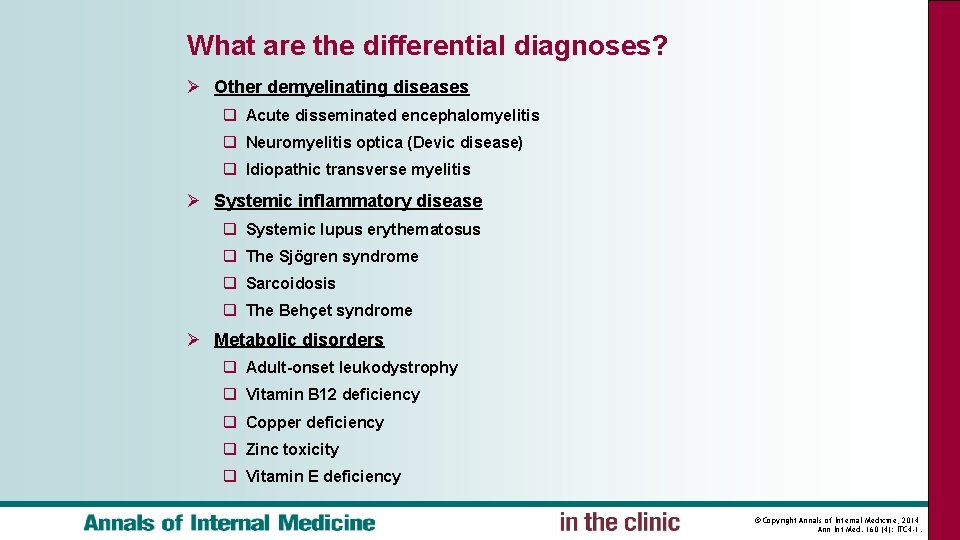
What are the differential diagnoses? Ø Other demyelinating diseases q Acute disseminated encephalomyelitis q Neuromyelitis optica (Devic disease) q Idiopathic transverse myelitis Ø Systemic inflammatory disease q Systemic lupus erythematosus q The Sjögren syndrome q Sarcoidosis q The Behçet syndrome Ø Metabolic disorders q Adult-onset leukodystrophy q Vitamin B 12 deficiency q Copper deficiency q Zinc toxicity q Vitamin E deficiency © Copyright Annals of Internal Medicine, 2014 Ann Int Med. 160 (4): ITC 4 -1.
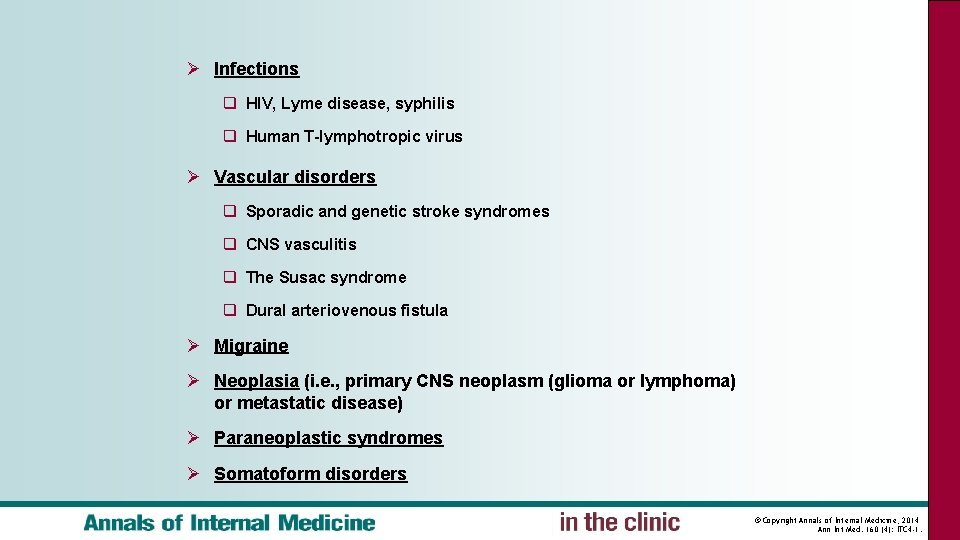
Ø Infections q HIV, Lyme disease, syphilis q Human T-lymphotropic virus Ø Vascular disorders q Sporadic and genetic stroke syndromes q CNS vasculitis q The Susac syndrome q Dural arteriovenous fistula Ø Migraine Ø Neoplasia (i. e. , primary CNS neoplasm (glioma or lymphoma) or metastatic disease) Ø Paraneoplastic syndromes Ø Somatoform disorders © Copyright Annals of Internal Medicine, 2014 Ann Int Med. 160 (4): ITC 4 -1.
An Overview of Treatment Strategies
How is MS treated? 1 -There is no cure for MS 2 -Treatments FOR: A-MS attacks or acute relapse. B-Immune Modify agents to prevent progression and reduce activity Of the disease. 3 -Treatment of symptoms
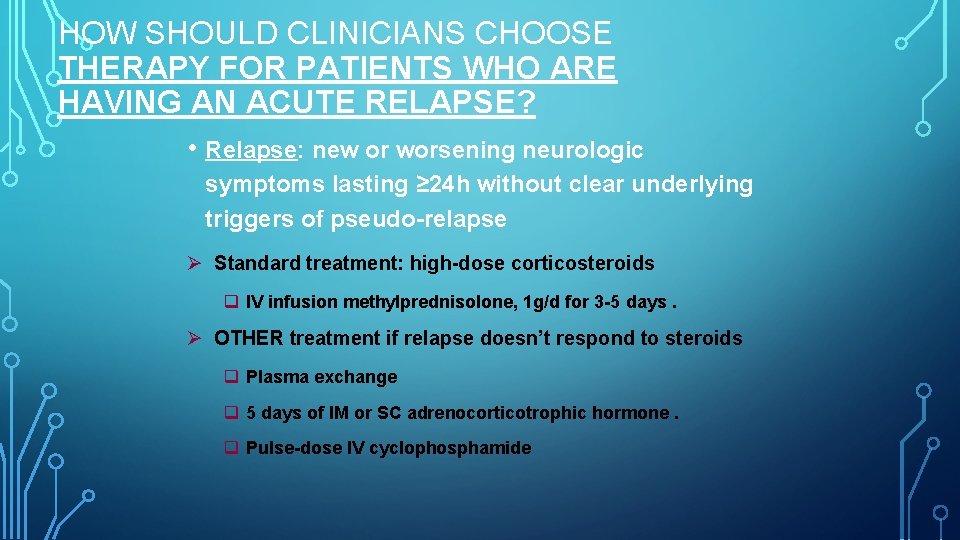
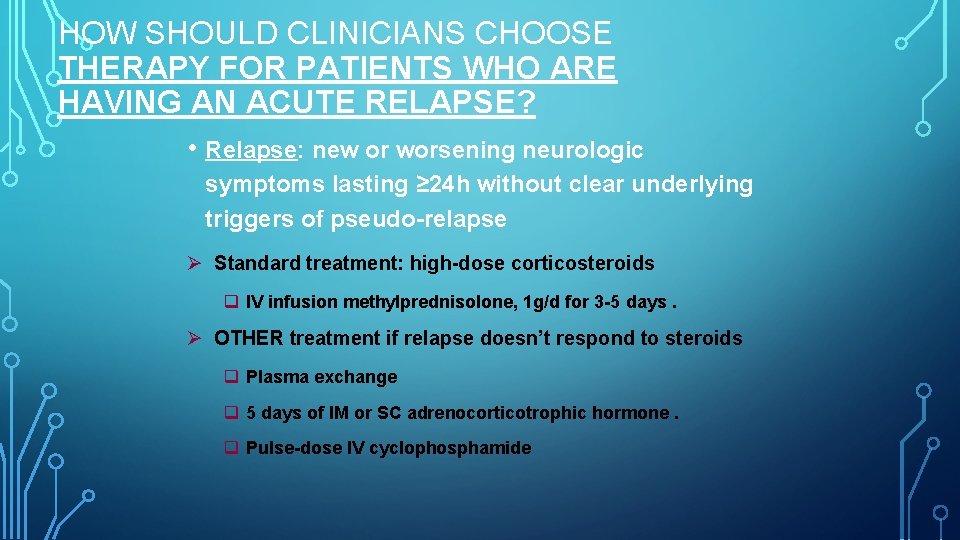
HOW SHOULD CLINICIANS CHOOSE THERAPY FOR PATIENTS WHO ARE HAVING AN ACUTE RELAPSE? • Relapse: new or worsening neurologic symptoms lasting ≥ 24 h without clear underlying triggers of pseudo-relapse Ø Standard treatment: high-dose corticosteroids q IV infusion methylprednisolone, 1 g/d for 3 -5 days. Ø OTHER treatment if relapse doesn’t respond to steroids q Plasma exchange q 5 days of IM or SC adrenocorticotrophic hormone. q Pulse-dose IV cyclophosphamide
Disease-Modifying Drugs for RRMS 1 -All reduce attack frequency and severity, reduce lesions on MRI, and probably slow disease progression. 2 -These medications are not designed to: A-Cure the disease B-Make people feel better C-Alleviate symptoms
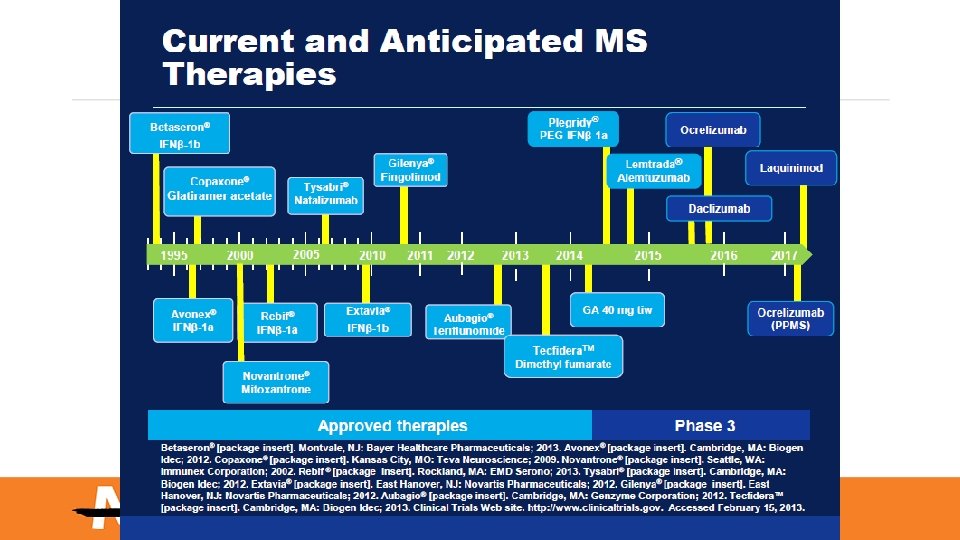
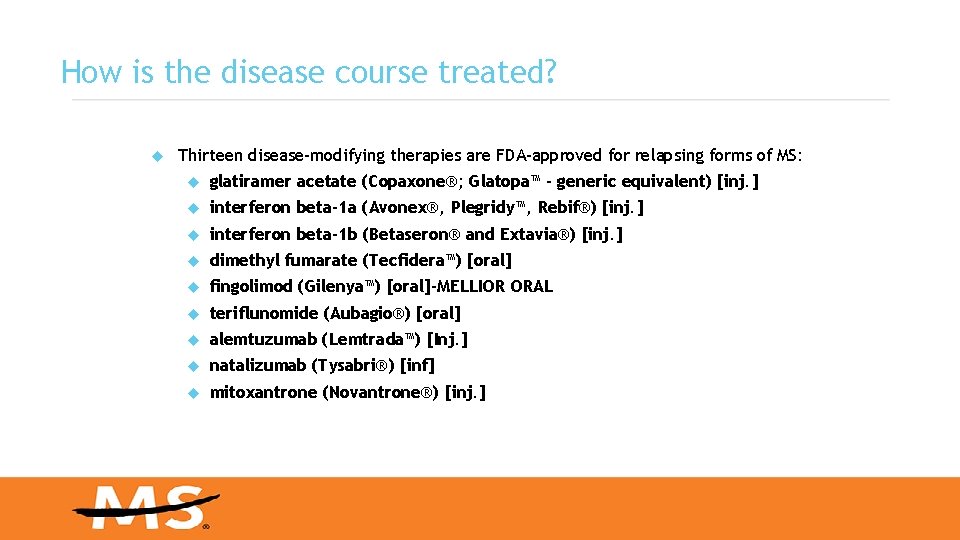
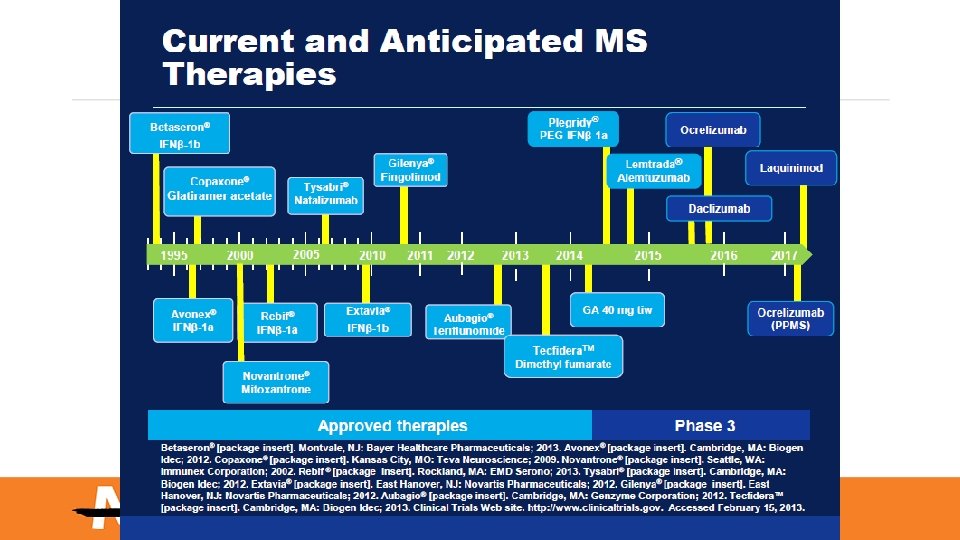
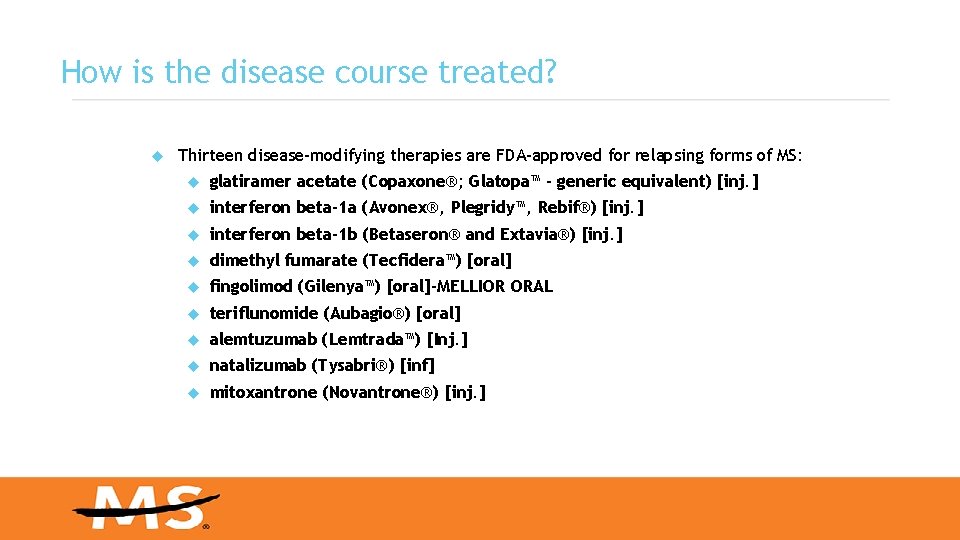
How is the disease course treated? Thirteen disease-modifying therapies are FDA-approved for relapsing forms of MS: glatiramer acetate (Copaxone®; Glatopa™ - generic equivalent) [inj. ] interferon beta-1 a (Avonex®, Plegridy™, Rebif®) [inj. ] interferon beta-1 b (Betaseron® and Extavia®) [inj. ] dimethyl fumarate (Tecfidera™) [oral] fingolimod (Gilenya™) [oral]-MELLIOR ORAL teriflunomide (Aubagio®) [oral] alemtuzumab (Lemtrada™) [Inj. ] natalizumab (Tysabri®) [inf] mitoxantrone (Novantrone®) [inj. ]
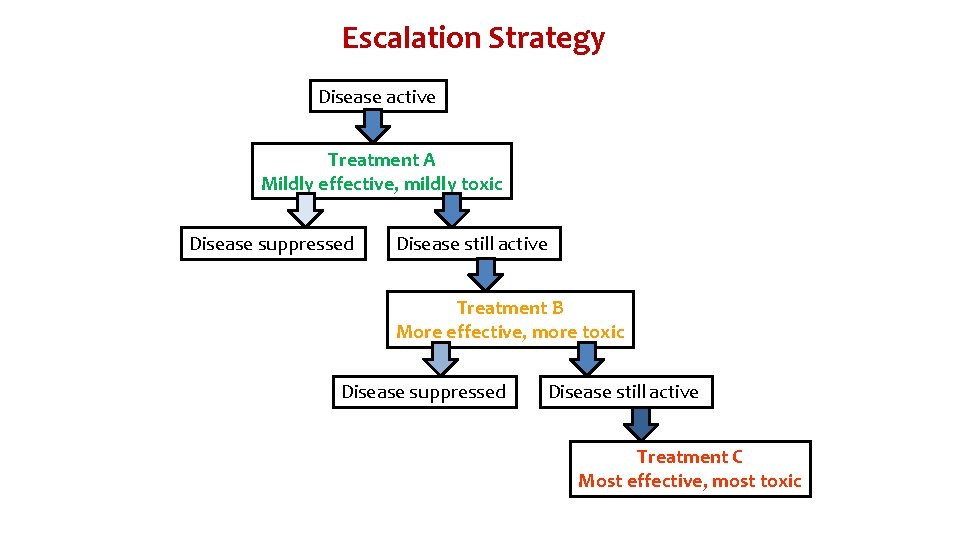
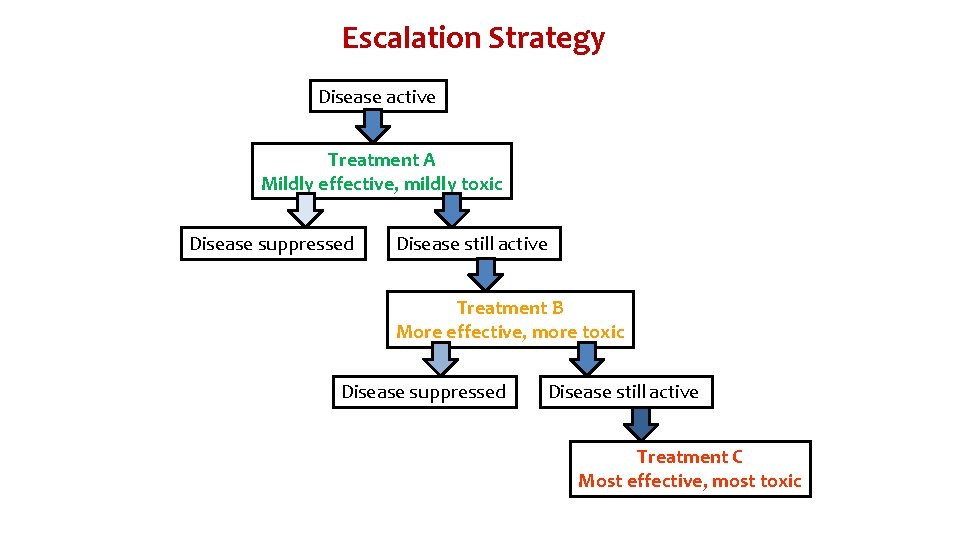
Escalation Strategy Disease active Treatment A Mildly effective, mildly toxic Disease suppressed Disease still active Treatment B More effective, more toxic Disease suppressed Disease still active Treatment C Most effective, most toxic
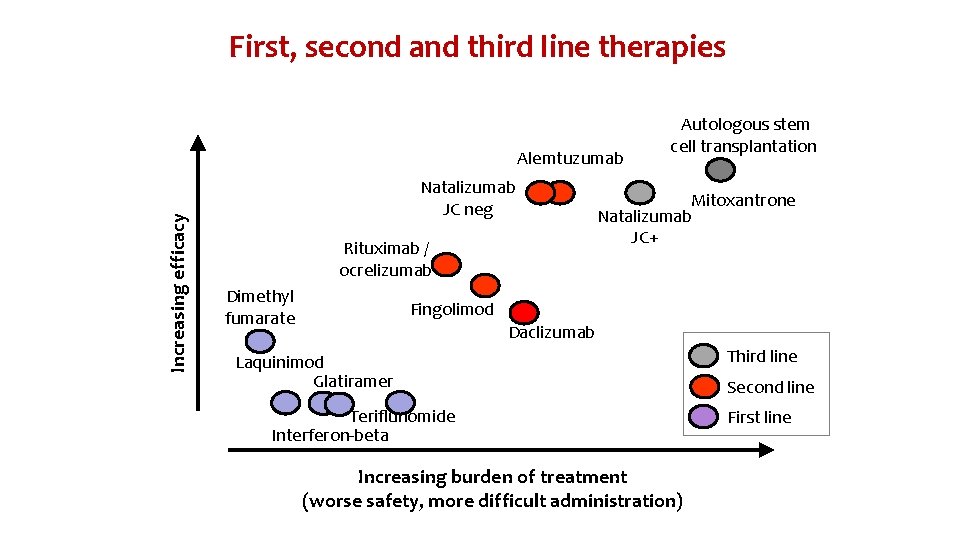
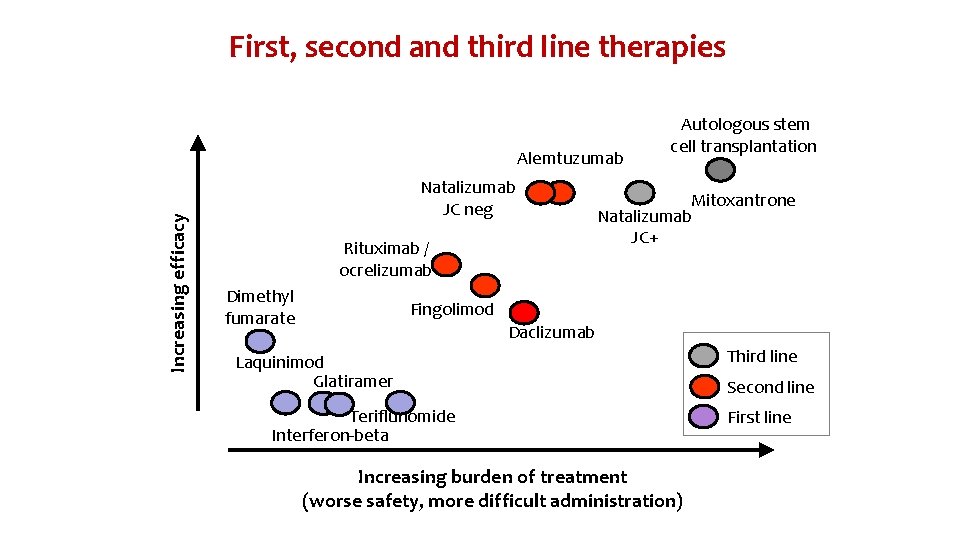
First, second and third line therapies Increasing efficacy Alemtuzumab Natalizumab JC neg Rituximab / ocrelizumab Dimethyl fumarate Autologous stem cell transplantation Mitoxantrone Natalizumab JC+ Fingolimod Daclizumab Laquinimod Glatiramer Teriflunomide Interferon-beta Increasing burden of treatment (worse safety, more difficult administration) Third line Second line First line
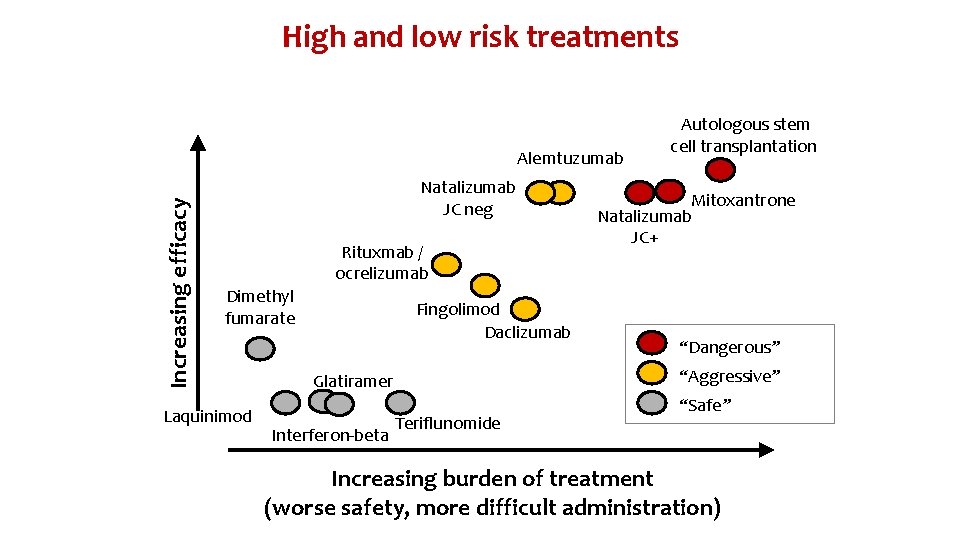
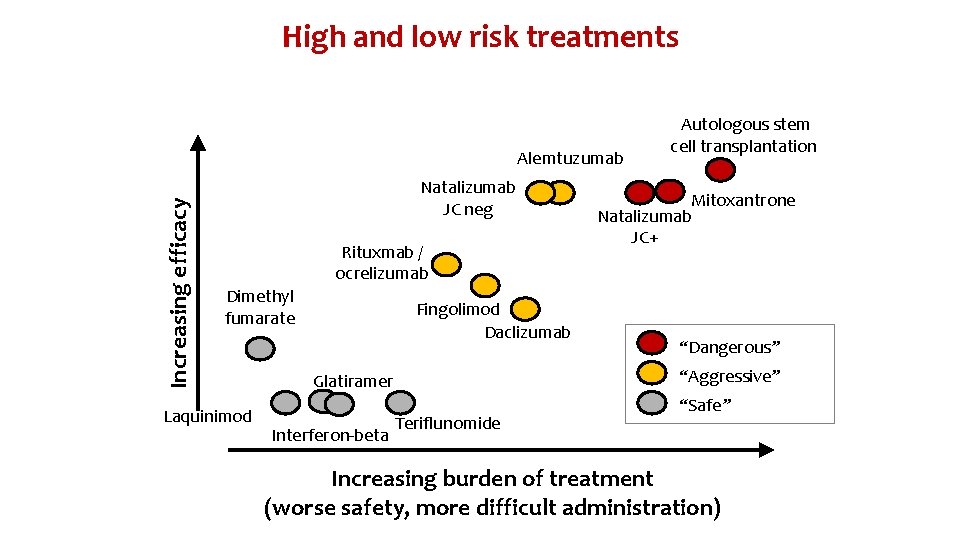
High and low risk treatments Increasing efficacy Alemtuzumab Natalizumab JC neg Rituxmab / ocrelizumab Dimethyl fumarate Laquinimod Fingolimod Daclizumab Mitoxantrone Natalizumab JC+ “Dangerous” “Aggressive” Glatiramer Interferon-beta Autologous stem cell transplantation Teriflunomide “Safe” Increasing burden of treatment (worse safety, more difficult administration)
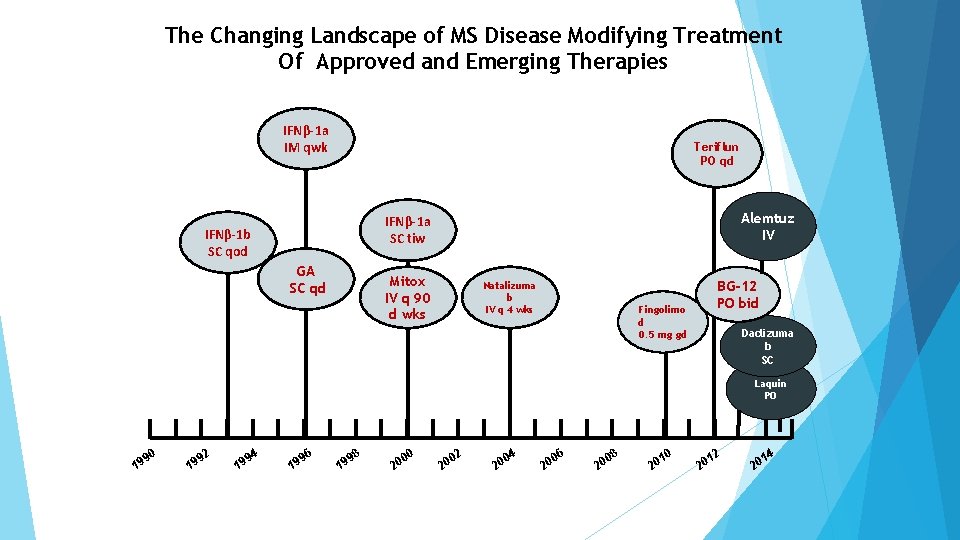
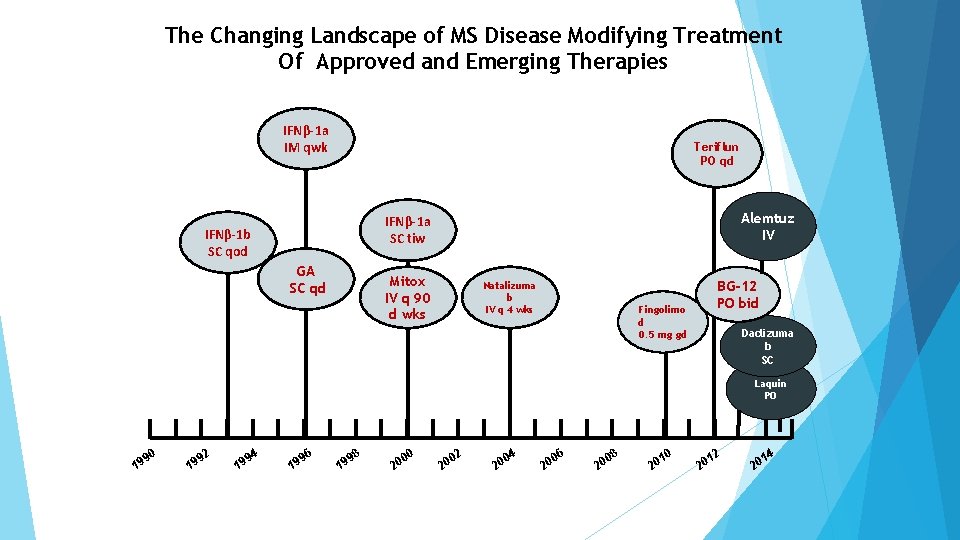
The Changing Landscape of MS Disease Modifying Treatment Of Approved and Emerging Therapies IFNβ-1 a IM qwk Teriflun PO qd Alemtuz IV IFNβ-1 a SC tiw IFNβ-1 b SC qod GA SC qd Mitox IV q 90 d wks Natalizuma b IV q 4 wks BG-12 PO bid Fingolimo d 0. 5 mg gd Daclizuma b SC Laquin PO 90 19 92 19 94 19 96 19 98 19 00 20 02 20 04 20 06 20 08 20 10 20 12 20 14 20
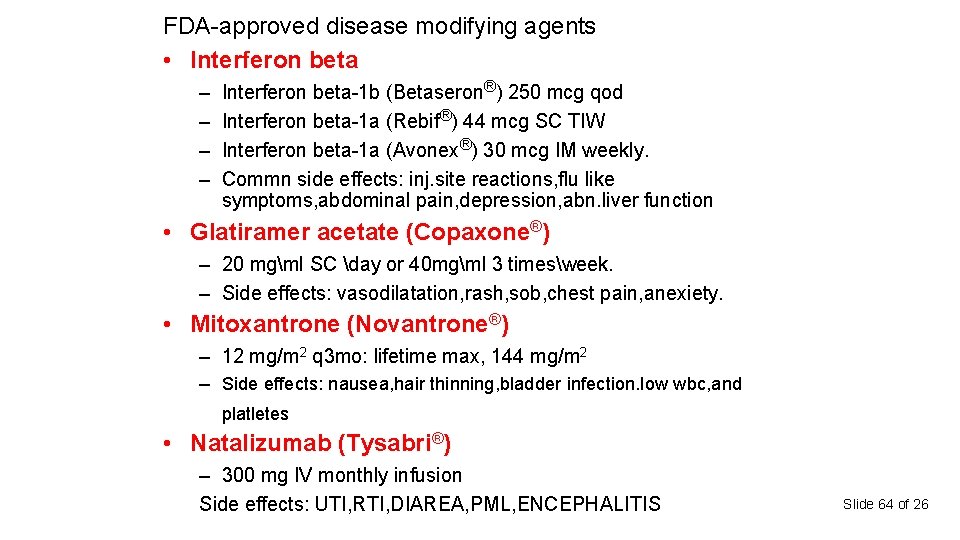
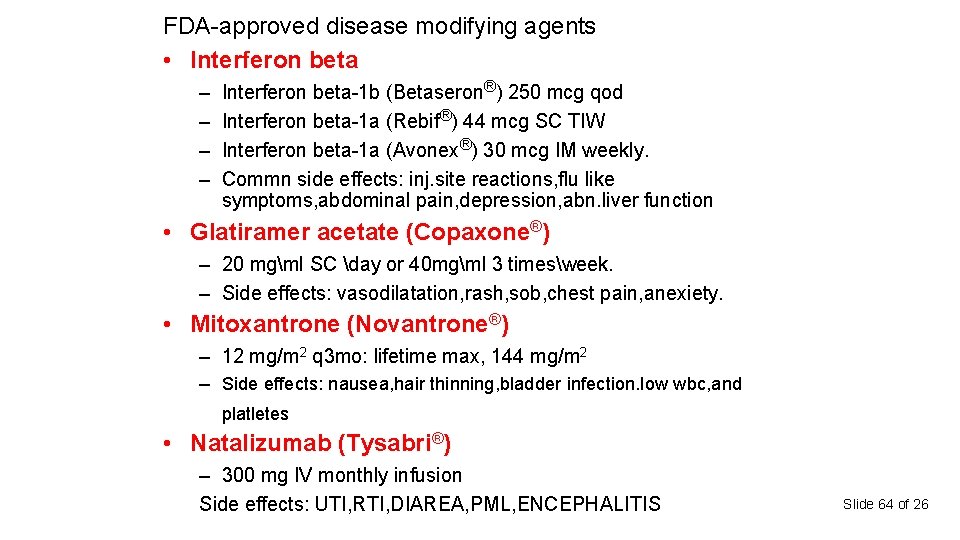
FDA-approved disease modifying agents • Interferon beta – – Interferon beta-1 b (Betaseron®) 250 mcg qod Interferon beta-1 a (Rebif®) 44 mcg SC TIW Interferon beta-1 a (Avonex®) 30 mcg IM weekly. Commn side effects: inj. site reactions, flu like symptoms, abdominal pain, depression, abn. liver function • Glatiramer acetate (Copaxone®) – 20 mgml SC day or 40 mgml 3 timesweek. – Side effects: vasodilatation, rash, sob, chest pain, anexiety. • Mitoxantrone (Novantrone®) – 12 mg/m 2 q 3 mo: lifetime max, 144 mg/m 2 – Side effects: nausea, hair thinning, bladder infection. low wbc, and platletes • Natalizumab (Tysabri®) – 300 mg IV monthly infusion Side effects: UTI, RTI, DIAREA, PML, ENCEPHALITIS Slide 64 of 26
• Continue disease modifying drugus • Parenteral (IV) drugs – Monoclonal antibodies: rituximab/ocrelizumab, alemtuzumab, daclizumab • Oral Drugs – Fingolimod, teriflunomide, Dymethyl fumarate, laquinimod • Symptomatic therapies – Fampridine (4 -AP), nerispirdine Slide 65 of 26
Glatiramare acetate(copaxon) Glatiramer acetate, the active ingredient of COPAXONE, consists of the acetate salts of synthetic polypeptides containing four naturally occurring amino acids: L-glutamic acid, L-alanine, Ltyrosine, and L-lysine
COPAXON • COPAXONE 20 mg per m. L: administer once per day or • COPAXONE 40 mg per m. L: administer three times per week
FINGOLIMOD Sphingosine-1 -Phosphate (S 1 P) Receptor Agonist
Fingolimod Treatment with fingolimod 0. 5 mg: Significant benefits on relapse-related outcomes within first 3 months and on volume loss over 6 months effects of fingolimod treatment
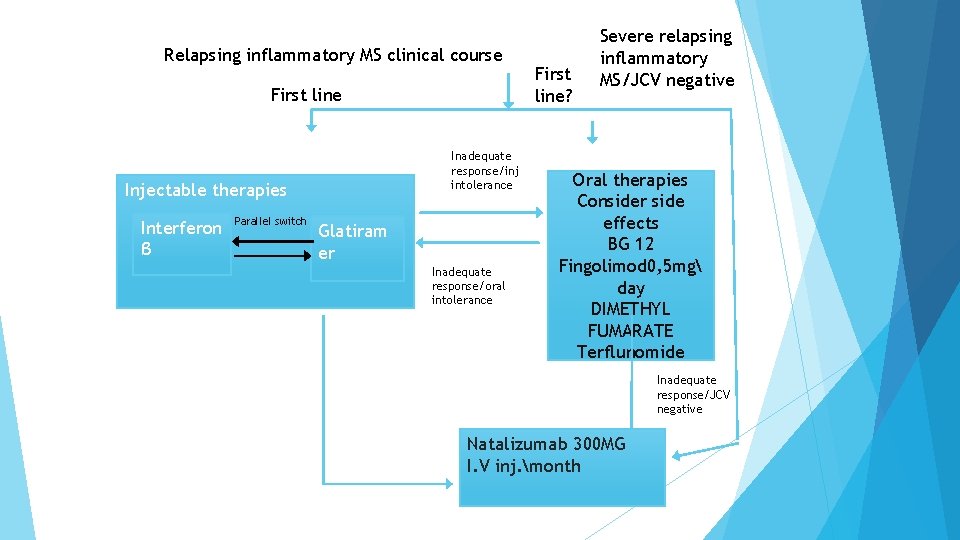
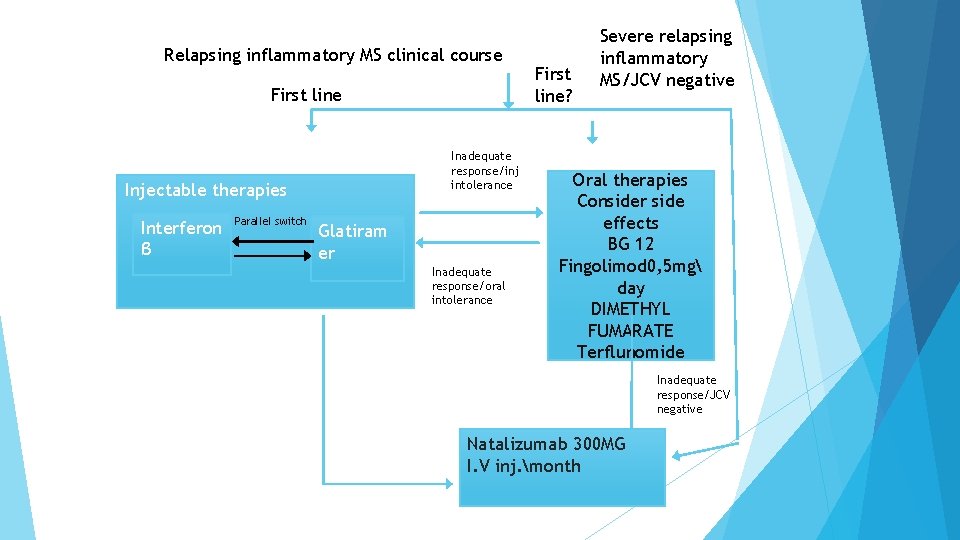
Relapsing inflammatory MS clinical course First line Inadequate response/inj intolerance Injectable therapies Interferon β Parallel switch Glatiram er Inadequate response/oral intolerance First line? Severe relapsing inflammatory MS/JCV negative Oral therapies Consider side effects BG 12 Fingolimod 0, 5 mg day DIMETHYL FUMARATE Terflunomide Inadequate response/JCV negative Natalizumab 300 MG I. V inj. month
What is the prognosis? One hallmark of MS is its unpredictability. Approximately 1/3 will have a very mild course Approximately 1/3 will have a moderate course Approximately 1/3 will become more disabled • Certain characteristics predict a better outcome: Female Onset before age 35 Sensory symptoms Monofocal rather than multifocal episodes Complete recovery following a relapse
Who is on the MS “Treatment Team”? • Neurologist Psychiatrist Urologist Psychotherapist Nurse Neuropsychologist Physiatrist Physical therapist Social worker/Care manager Pharmacist Occupational therapist Speech/language pathologist Primary care physician
So what do we know about MS? MS is a chronic, unpredictable disease The cause is still unknown MS affects each person differently; symptoms vary widely MS is not fatal, contagious, directly inherited, or always disabling
Early diagnosis and treatment are important Significant, on Available treatments reduce the number of relapses and may slow progression Treatment includes: attack management, symptom management, disease modification, rehab, emotional support 74
THANK YOU