Multiple Sclerosis Faizan zaffar kashoo What is Multiple








- Slides: 28

Multiple Sclerosis Faizan zaffar kashoo
What is Multiple Sclerosis? q It is an Auto Immune Disease which is when the body starts to destroy itself. q It is a life-long disease with no cure. q In MS, the body attacks and destroys the fatty tissue called myelin that insulates an axon/nerve, and is called demyelination. q If damage is severe it can also destroy the nerve/axon itself. q MS affects the central nervous system and inflames the white matter in the brain which creates plaques. .

What is Multiple Sclerosis? • Multiple Sclerosis (MS) is an chronic inflammatory demyelinating disease of the brain and spinal cord.
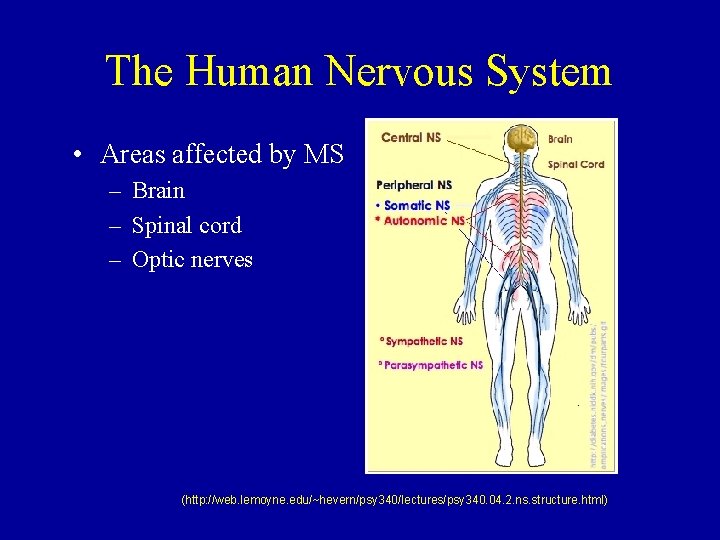
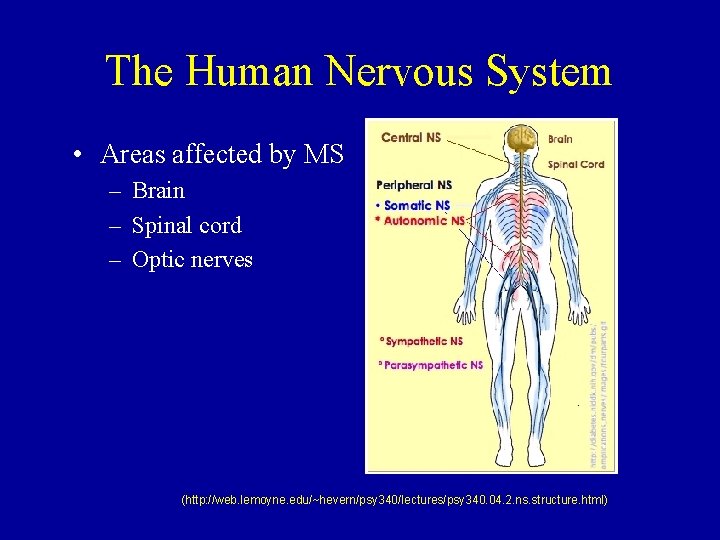
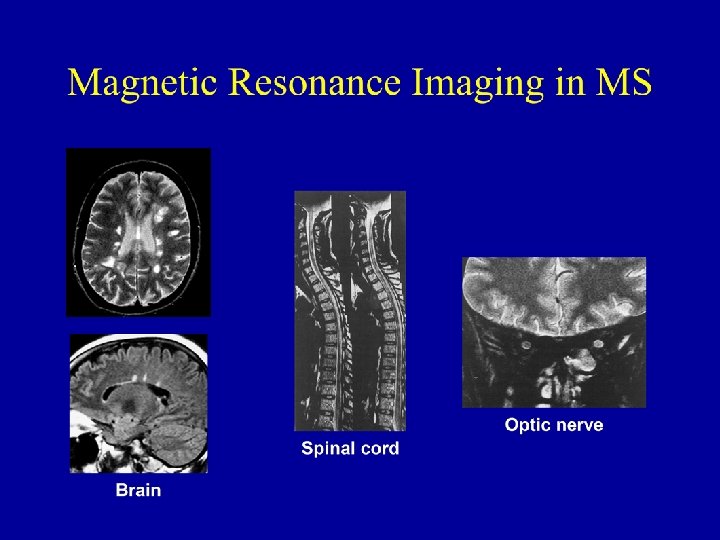
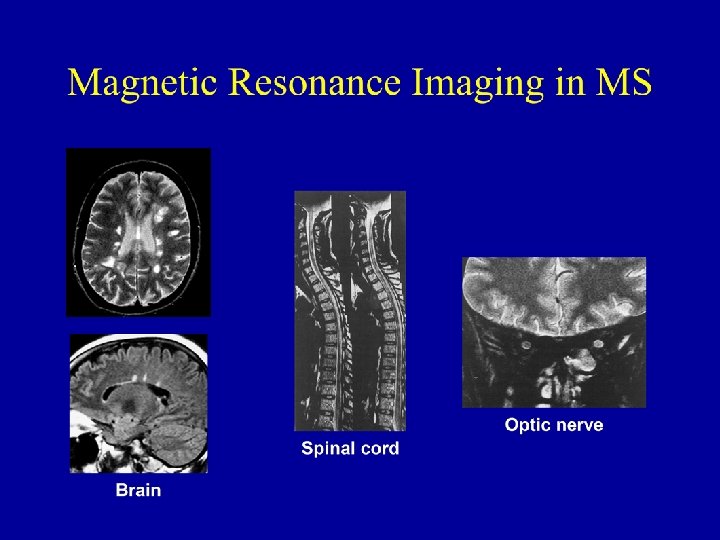
The Human Nervous System • Areas affected by MS – Brain – Spinal cord – Optic nerves (http: //web. lemoyne. edu/~hevern/psy 340/lectures/psy 340. 04. 2. ns. structure. html)
How Common is MS and Who Gets It? • • • 8, 000 – 10, 000 new cases are diagnosed annually Affects nearly 500, 000 individuals in the U. S. Occurs most frequently between ages 25 - 35 Female: male ratio = 2: 1 More frequent in populations native to areas further away from the equator
What Causes MS? • Genetics • Environmental factors
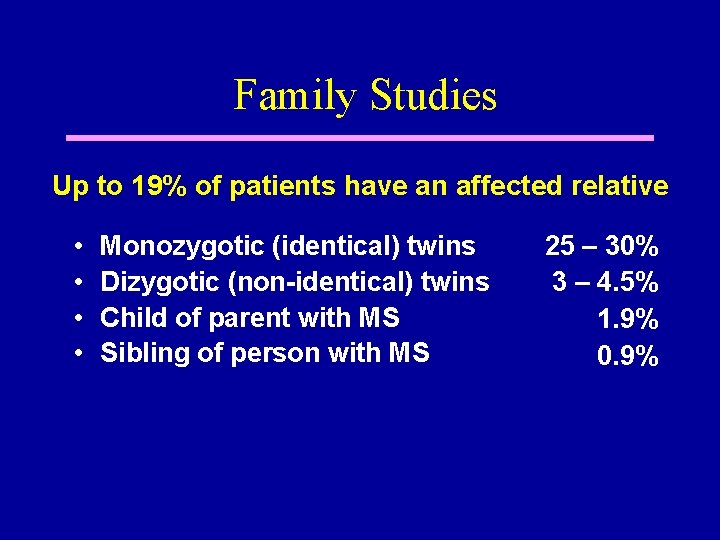
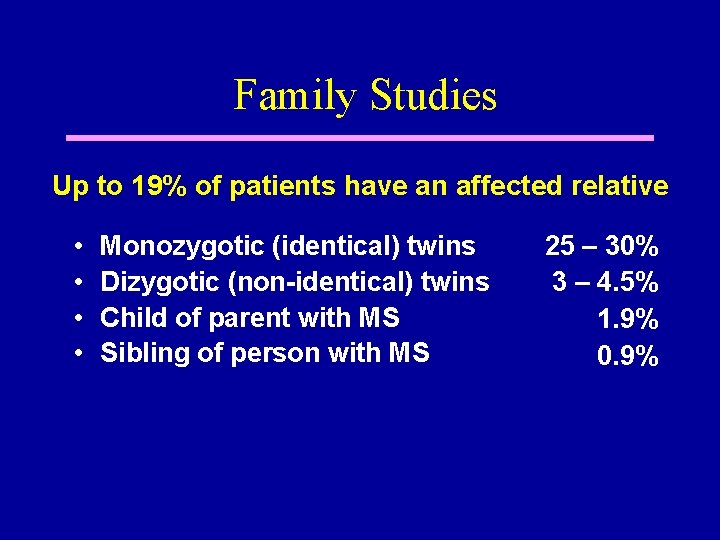
Family Studies Up to 19% of patients have an affected relative • • Monozygotic (identical) twins Dizygotic (non-identical) twins Child of parent with MS Sibling of person with MS 25 – 30% 3 – 4. 5% 1. 9% 0. 9%

Groups for Which MS Genetic Traits Have Been Identified: • • • Japanese African American Mexican Arabian Sardinian (Italy) Swedish Norwegian French Canadian Finnish
Not Everyone with a Genetic Risk Will Develop MS – Why? • Risk is modified by Environmental factors – Sunlight – Diet (e. g. , vitamin D) – Other lifetime experiences (infections? )
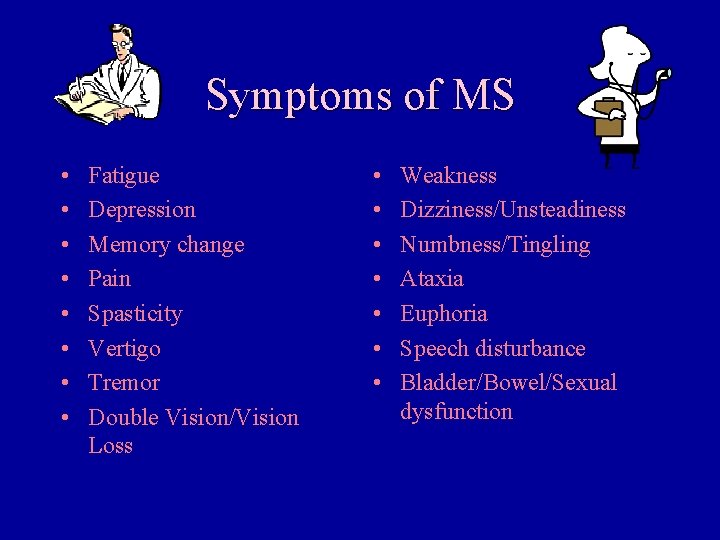
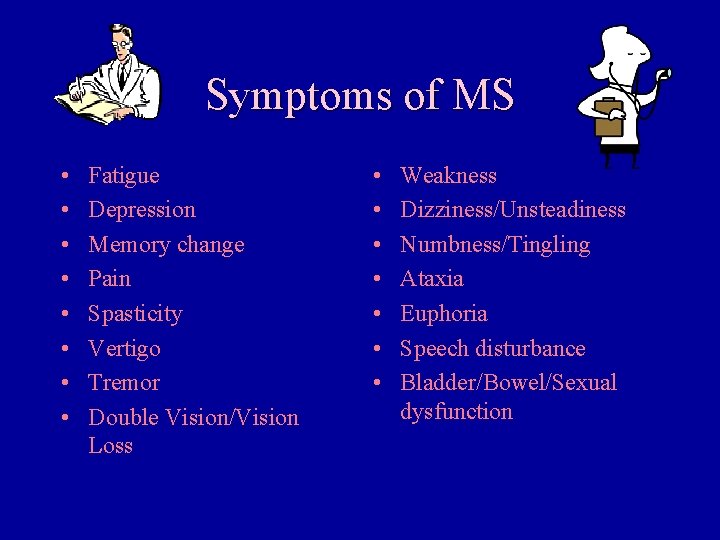
Symptoms of MS • • Fatigue Depression Memory change Pain Spasticity Vertigo Tremor Double Vision/Vision Loss • • Weakness Dizziness/Unsteadiness Numbness/Tingling Ataxia Euphoria Speech disturbance Bladder/Bowel/Sexual dysfunction

Multiple Sclerosis Clinical Subtypes Secondary-progressive Disability Relapsing-remitting Time Progressive-relapsing Disability Primary-progressive Time
How Is MS Diagnosed? • At least two episodes of symptoms – Occur at different points in time – Result from involvement of different areas of the central nervous system • Absence of other treatable causes for the symptoms • Results of neurological testing

How Is MS Diagnosed? • • Neurological examination Magnetic resonance imaging (MRI) Scan Blood tests Lumbar Puncture (spinal tap): occasionally performed • Other testing: infrequently performed

Brain Atrophy (Shrinkage) in Untreated MS Images acquired over the course of 7 years from a single person with untreated MS
How is MS Treated and Managed? • Drug therapy – Treat new attacks (exacerbations) – Prevent the occurrence of future attacks – Slow or prevent disease progression – Treat the chronic symptoms of the disease • Psychosocial support
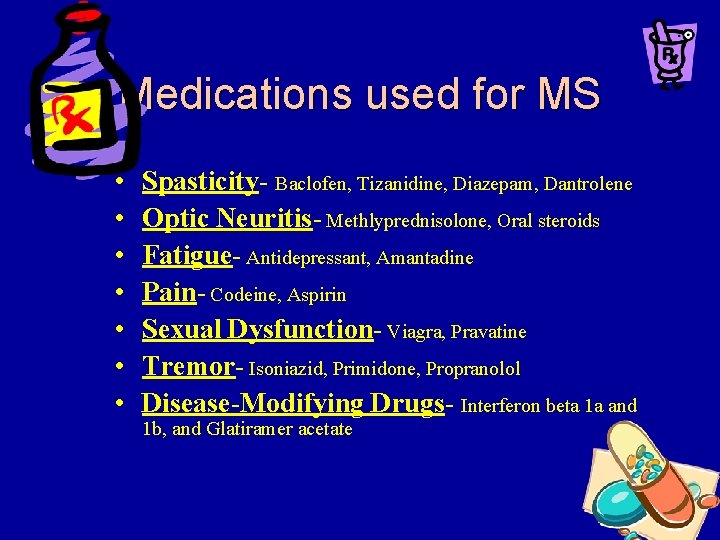
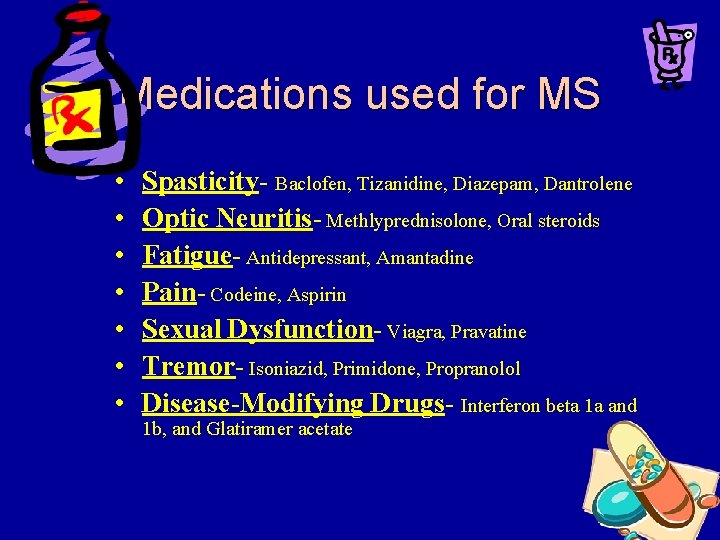
Medications used for MS • • Spasticity- Baclofen, Tizanidine, Diazepam, Dantrolene Optic Neuritis- Methlyprednisolone, Oral steroids Fatigue- Antidepressant, Amantadine Pain- Codeine, Aspirin Sexual Dysfunction- Viagra, Pravatine Tremor- Isoniazid, Primidone, Propranolol Disease-Modifying Drugs- Interferon beta 1 a and 1 b, and Glatiramer acetate
Disease-Modifying Drugs • Interferon Beta 1 a (Avonex and Rebif): is a protein that is a replica of human interferon. It suppress the immune system and helps to maintain the blood-brain barrier. You inject Avonex into the muscle once a week and Rebif is injected under the skin three times a week. This drug is useful to people who have definite progressive MS. One side effect of the drug is a flu like symptom. • Interferon Beta 1 b (Betaseron): is slightly different from our own interferon. This medication does the same thing as beta 1 a, but is injected just under the skin every two days. Side effects include irritation, bruising, and redness at the site of injection and the flu like symptoms. This is also given to people who have definite progressive MS.
Physiotherapy assessment • • • Strength Tone Range of motion Balance Coordination Cardiovascular and respiratory status • Bed mobility and transfer • Bowel and bladder impairment • Swallowing • Speech and communication impairment • Visual status • Sensory impairment • Activities of daily living • Cognition • Physical environment • Medical stability.

Measurement tools • Barthel index • Kurtzke scale • Multiple sclerosis quality of life inventory
Setting goals • Helping the patient solve problems • Problem solving and education are key aspects
fatigue • • • Modified fatigue impact scale Due to sleep deprivationurinary incontinence Muscle spasm Poor diet Depression
fatigue • • • Energy conservative techniques General exercises Breathing exercises Stretching Adaptive equipments

weakness • • Pnf Stretching Ankle Foot Orthrosis Strengthening strong muscles.
Balance • • Cerebellar problem is common Wide base to narrow base Low to high COG. Weighted cuff and weighed canes reduce tremors. • Collar to reduce tremor of neck
Sensory deficit • • Compensating for the loss Routine safety instructions Wheelchair cushioning Pressure relief techniques.
Ambulation and mobility • Wheelchair mobility training. • Electric wheelchair.