MULTIPLE PREGNANCY Ghadeer AlShaikh MD FRCSC Assistant Professor








- Slides: 38
MULTIPLE PREGNANCY Ghadeer Al-Shaikh, MD, FRCSC Assistant Professor & Consultant Obstetrics & Gynecology Urogynecology & Pelvic Reconstructive Surgery Department of Obstetrics & Gynecology College of Medicine King Saud University
MULTIPLE PREGNANCY Twin pregnancy represents 2 to 3% of all pregnancies. The PNMR is 5 times that of singleton

DIZYGOTIC TWINS Most common represents 2/3 of cases. Fertilization of more than one egg by more than one sperm. Non identical , may be of different sex. Two chorion and two amnion. Placenta may be separate or fused.
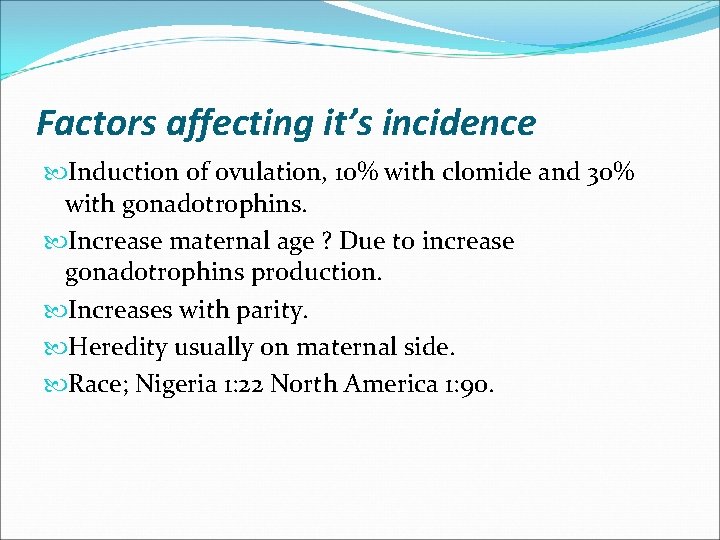
Factors affecting it’s incidence Induction of ovulation, 10% with clomide and 30% with gonadotrophins. Increase maternal age ? Due to increase gonadotrophins production. Increases with parity. Heredity usually on maternal side. Race; Nigeria 1: 22 North America 1: 90.
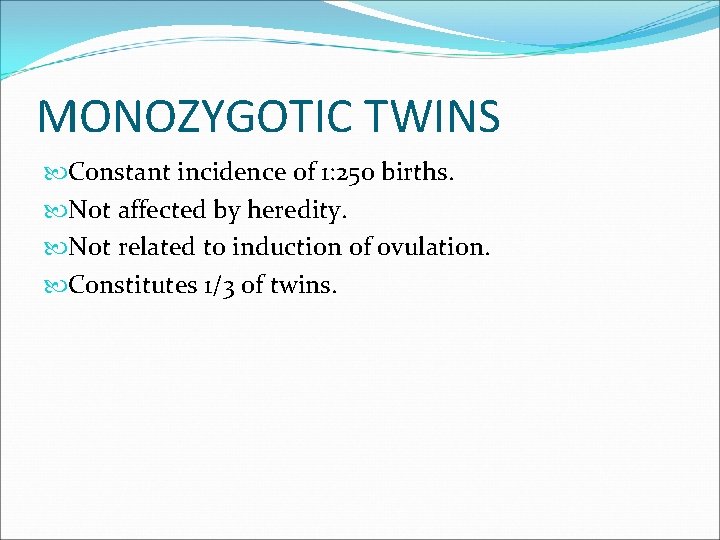
MONOZYGOTIC TWINS Constant incidence of 1: 250 births. Not affected by heredity. Not related to induction of ovulation. Constitutes 1/3 of twins.
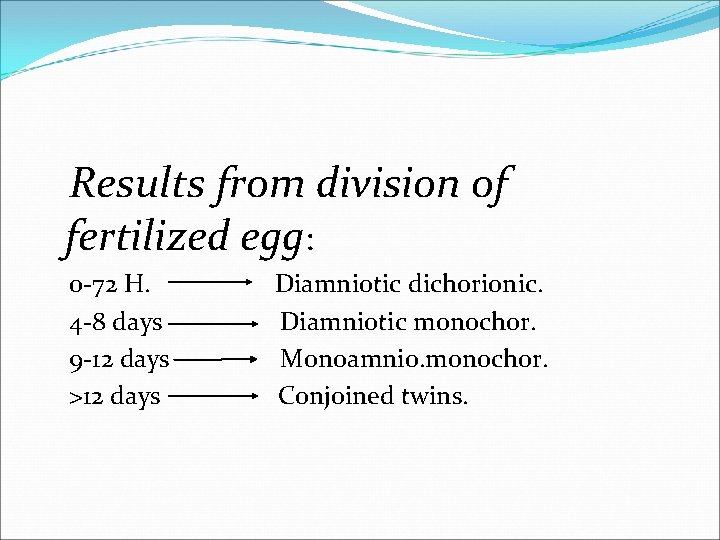
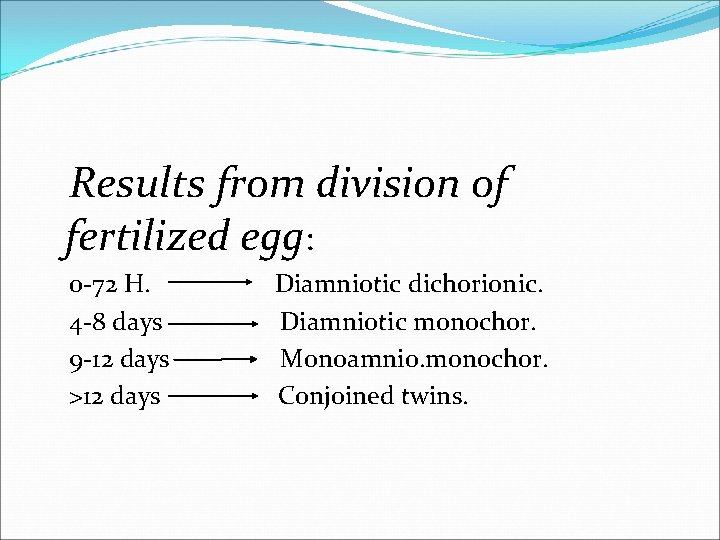
Results from division of fertilized egg: 0 -72 H. 4 -8 days 9 -12 days >12 days Diamniotic dichorionic. Diamniotic monochor. Monoamnio. monochor. Conjoined twins.
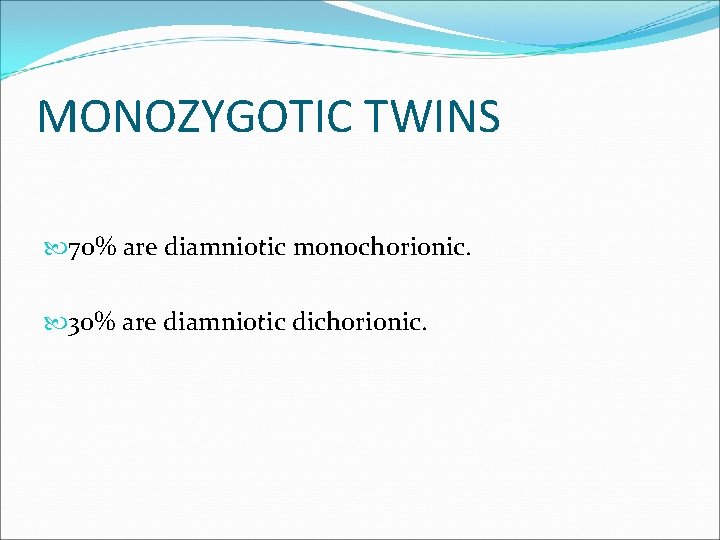
MONOZYGOTIC TWINS 70% are diamniotic monochorionic. 30% are diamniotic dichorionic.
Determination of zygosity Very important as most of the complications occur in monochorionic monozygotic twins.
During pregnancy by USS Very accurate in the first trimester, two sacs, presence of thick chorion between amniotic memb. Less accurate in the second trimester the chorion become thin and fuse with the amniotic memb.


Different sex indicates dizygotic twins. Separate placentas indicates dizygotic twins
Determination of zygozity After Birth By examination of the MEMBRANE, PLACENTA, SEX , BLOOD group. Examination of the newborn DNA and HLA may be needed in few cases.
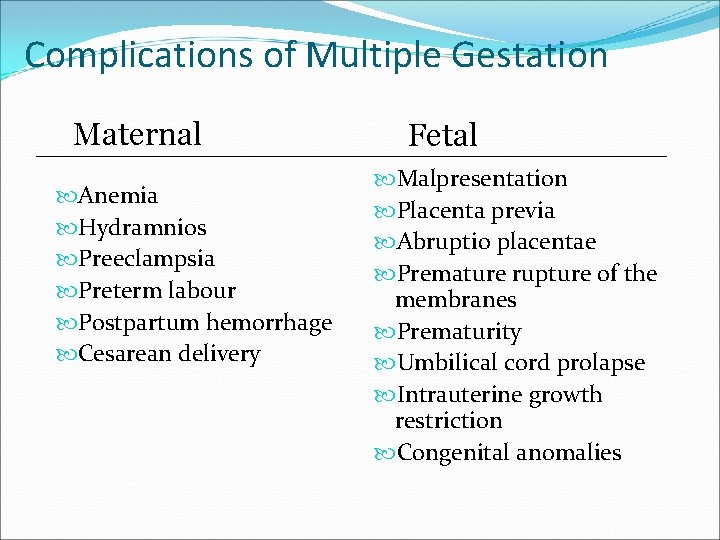
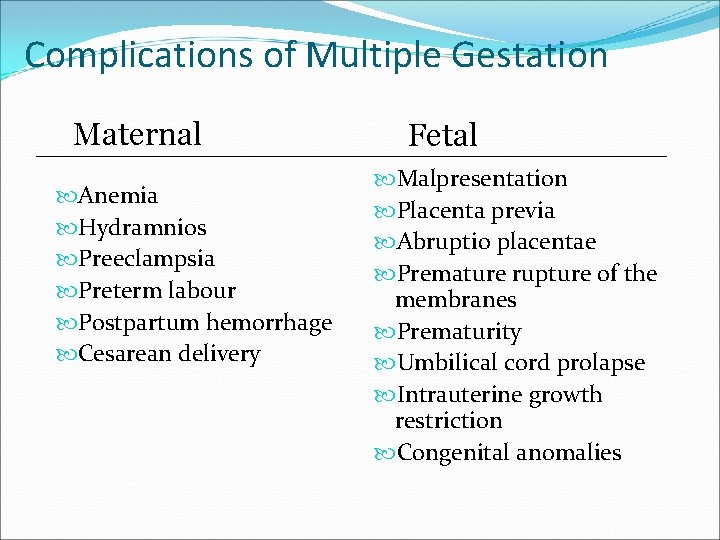
Complications of Multiple Gestation Maternal Anemia Hydramnios Preeclampsia Preterm labour Postpartum hemorrhage Cesarean delivery Fetal Malpresentation Placenta previa Abruptio placentae Premature rupture of the membranes Prematurity Umbilical cord prolapse Intrauterine growth restriction Congenital anomalies
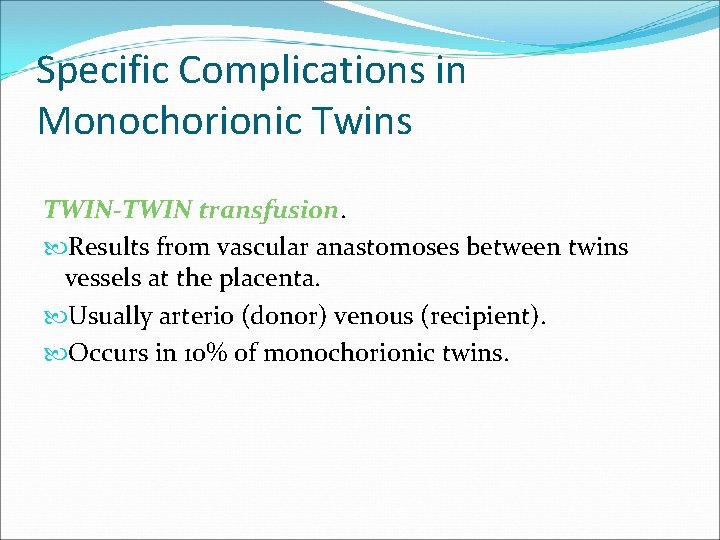
Specific Complications in Monochorionic Twins TWIN-TWIN transfusion. Results from vascular anastomoses between twins vessels at the placenta. Usually arterio (donor) venous (recipient). Occurs in 10% of monochorionic twins.
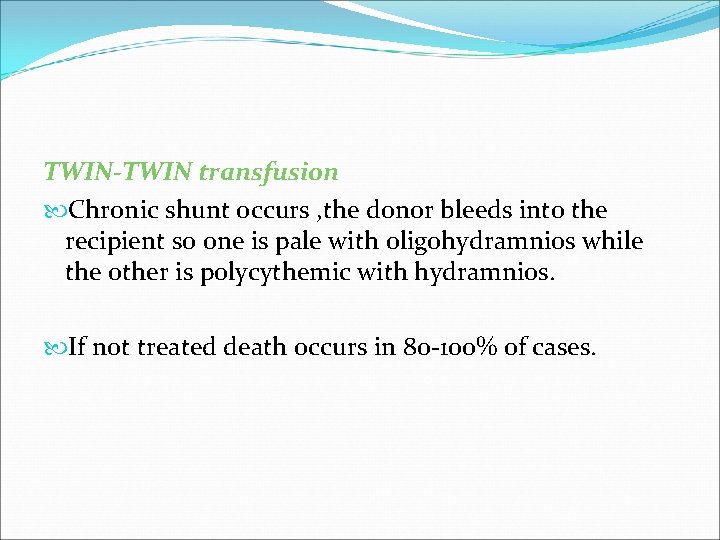
TWIN-TWIN transfusion Chronic shunt occurs , the donor bleeds into the recipient so one is pale with oligohydramnios while the other is polycythemic with hydramnios. If not treated death occurs in 80 -100% of cases.
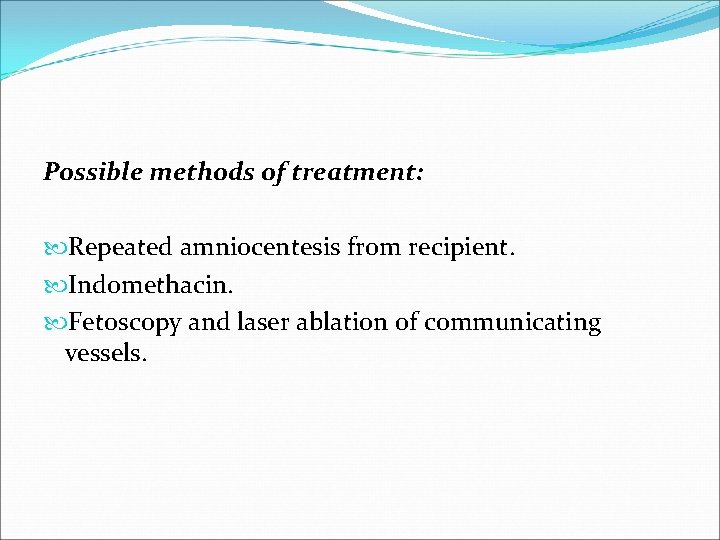
Possible methods of treatment: Repeated amniocentesis from recipient. Indomethacin. Fetoscopy and laser ablation of communicating vessels.

Other Complications in Monochorionic Twins: Congenital malformation. Twice that of singleton. Umbilical cord anomalies. In 3 – 4 %. Conjoined twins. Rare 1: 70000 deli varies. The majority are thoracopagus. PNMR of monochorionic is 5 times that of dichorionic twins(120 VS 24/ 1000 births)
Maternal Physiological Adaptation Ø Increase blood volume and cardiac output. Ø Increase demand for iron and folic acid. Ø Maternal respiratory difficulty. Ø Excess fluid retention and edema. Ø Increase attacks of supine hypotension.
DIAGNOSIS OF MULTIPLE PREGNANCY Ø +ve family history mainly on maternal side. Ø +ve history of ovulation induction. Ø Exaggerated symptoms of pregnancy. Ø Marked edema of lower limb. Ø Discrepancy between date and uterine size. Ø Palpation of many fetal parts.
Ø Auscultation of two fetal heart beats at two different sites with a difference of 10 beats Ø USS Two sacs by 5 weeks by TV USS. Two embryos by 7 weeks by TV USS.
Antenatal Care AIM Prolongation of gestation age, increase fetal weight. Improve PNM and morbidity. Decrease incidence of maternal complications.
Antenatal Care Follow Up Every two weeks. Iron and folic acid to avoid anemia. Assess cervical length and competency.
Antenatal Care Fetal Surveillance Monthly USS from 24 weeks to assess fetal growth and weight. A discordinate weight difference of >25% is abnormal (IUGR). Weekly CTG from 36 weeks.
Method Of Delivery Vertex- Vertex (50%) Vaginal delivery. Vertex- Breech (20%) Vaginal delivery by senior obstetrician


Method Of Delivery Breech- Vertex( 20%) Safer to deliver by CS to avoid the rare interlocking twins( 1: 1000 twins ). Breech-Breech( 10%) Usually by CS.
Method Of Delivery in Monochorionic Twins C/S
Perinatal Outcome PNMR is 5 times that of singleton (30 -50/1000 births). RDS accounts for 50% 0 f PNMR. 2 nd twin is more affected. Birth trauma. 2 ND twin is 4 times affected than 1 st. Incidence of SB is twice that of singleton.
Perinatal Outcome Congenital anomalies is responsible for 15% of PNMR. Cerebral hemorrhage and birth asphyxia are responsible for 10% of PNMR. Cerebral palsy is 4 times that of singleton. 50% of twins babies are borne with low birth(<2500 gms. ) from prematurity & IUGR.
INTRAUTERINE DEATH OF ONE TWIN Ø Early in pregnancy usually no risk. Ø In 2 nd or 3 rd trimester: Increase risk of DIC. Increase risk of thrombosis in the a live one The risk is much higher in monochorionic than in dichorionic twins
The alive baby should be delivered by 32 -34 weeks in monochorionic twins.
HIGH RANK MULTIPLE GESTATION Spontaneous triplets 1: 8000 births. Spontaneous quadruplets 1: 700, 000 births. The main risk is sever prematurity. CS is the usual and safe mode of delivary. High PNMR of 50 -100 / 1000 births


Thank You!!!
 Ghadeer khum
Ghadeer khum Early pregnancy pictures of spotting during pregnancy
Early pregnancy pictures of spotting during pregnancy Promotion from associate professor to professor
Promotion from associate professor to professor Cuhk assistant professor salary
Cuhk assistant professor salary Multiple pregnancy nursing diagnosis
Multiple pregnancy nursing diagnosis Multiple instruction single data
Multiple instruction single data Multiple probe vs multiple baseline
Multiple probe vs multiple baseline Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Implantation steps
Implantation steps Hormones during pregnancy
Hormones during pregnancy Taxonomy of goat
Taxonomy of goat Midwives prayer
Midwives prayer Type 1 type 2 error power
Type 1 type 2 error power Rapiprazole
Rapiprazole Endoscopy in pregnancy guidelines
Endoscopy in pregnancy guidelines Acute fatty liver of pregnancy
Acute fatty liver of pregnancy High levels of fibrinogen in pregnancy
High levels of fibrinogen in pregnancy Acute fatty liver of pregnancy
Acute fatty liver of pregnancy Liquor in pregnancy
Liquor in pregnancy Nalador
Nalador Malaria in pregnancy definition
Malaria in pregnancy definition Chapter 5 reproducible master a pregnancy vocabulary
Chapter 5 reproducible master a pregnancy vocabulary Coomb s test
Coomb s test Trombostenin
Trombostenin Hispanic cultural views on teenage pregnancy
Hispanic cultural views on teenage pregnancy Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Pregnancy category a
Pregnancy category a Bhiva guidelines pregnancy
Bhiva guidelines pregnancy Mitchella repens pregnancy
Mitchella repens pregnancy Anemia in pregnancy guideline
Anemia in pregnancy guideline Pregnancy trimester breakdown
Pregnancy trimester breakdown Endocrinology of pregnancy
Endocrinology of pregnancy Mtp act
Mtp act Adoloscense
Adoloscense Do you get period pains when pregnant
Do you get period pains when pregnant Sajda during pregnancy
Sajda during pregnancy Loratadine pregnancy category
Loratadine pregnancy category Height of fundus during pregnancy
Height of fundus during pregnancy Hypothyroidism treatment in pregnancy
Hypothyroidism treatment in pregnancy