Zika Virus and Pregnancy Dr Rick Mentz FRCSC







- Slides: 33
Zika Virus and Pregnancy Dr. Rick Mentz, FRCSC Obstetrics and Gynecology
Disclosure No disclosures
First time in history “ Never before in history has there been a situation where a bite from a mosquito could result in a devastating malformation. ” - Dr. Tom Frieden, CDC Director Fortune, April 13, 2016 “…the last time an infectious pathogen (rubella) caused an epidemic of congenital defects was more than 50 years ago…” - New England Journal of Medicine, April 13, 2016
Learning Objectives • • • Review epidemiology of Zika virus (ZIKV) ZIKV in pregnancy & the congenital impact Diagnosing & testing for ZIKV Preventing ZIKV Surveillance of ZIKV in Canada
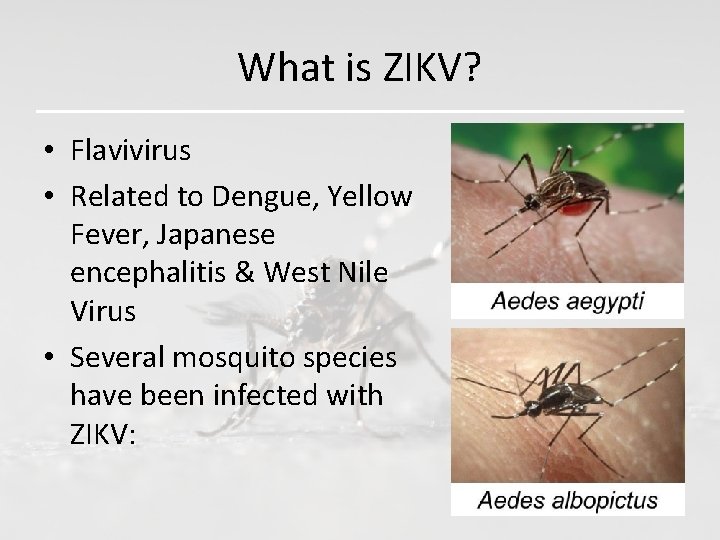
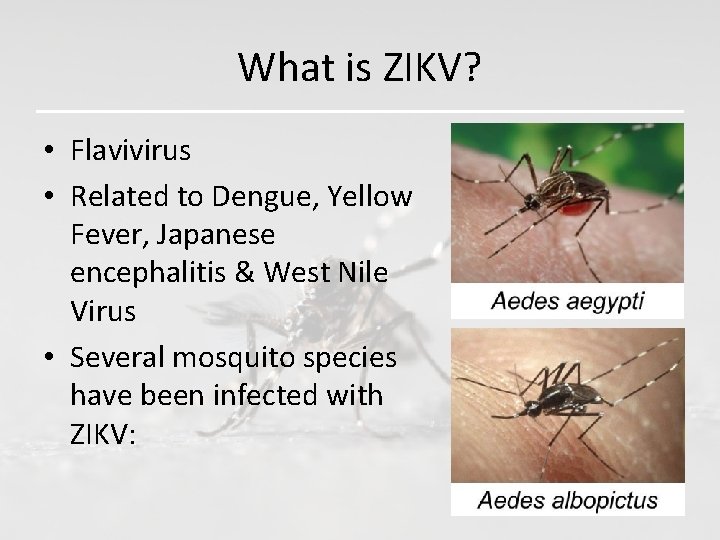
What is ZIKV? • Flavivirus • Related to Dengue, Yellow Fever, Japanese encephalitis & West Nile Virus • Several mosquito species have been infected with ZIKV:
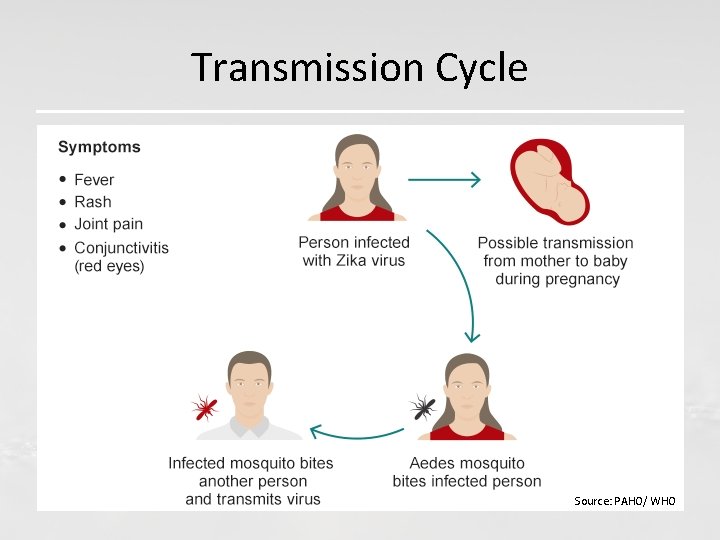
How is it transmitted to humans? • Mosquito bite is primary mode of • • transmission Intrauterine and perinatal transmission Sexual transmission Laboratory exposure & Probable blood transfusion
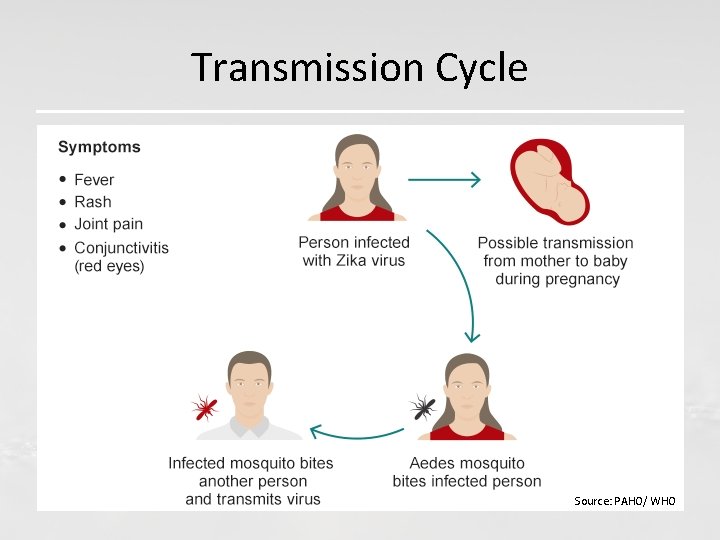
Transmission Cycle Source: PAHO/ WHO

ZIKV • • • Incubation period: 3 -12 days Viremia 3 -5 days, Saliva, urine, cervical mucous > 1 wk, Semen – 6 mo Ig. M Ab evolve thereafter ZIKV RNA in breast milk, no documented reports of transmission

ZIKV – Clinical manifestations • 80% of those infected are asymptomatic • 20% mild disease (acute fever, maculopapular rash, arthralgia, conjunctivitis) ~ 1 week • Severe disease uncommon • Associated with Guillian-Barre Syndrome (risk 2/10 000) • Neurologic sequelae of ZIKV broader than thought
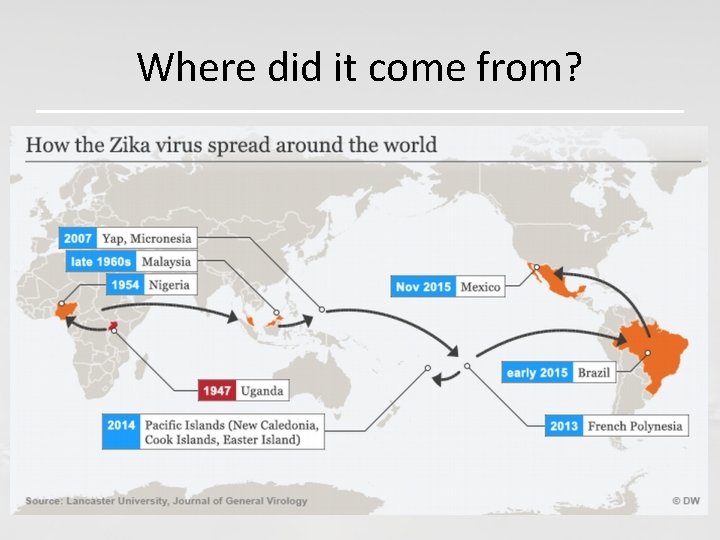
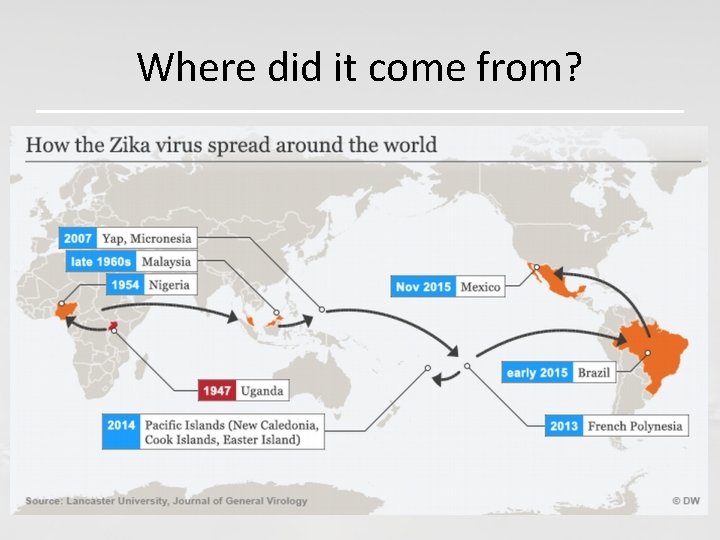
Where did it come from?

Where is ZIKV now? Source: CDC
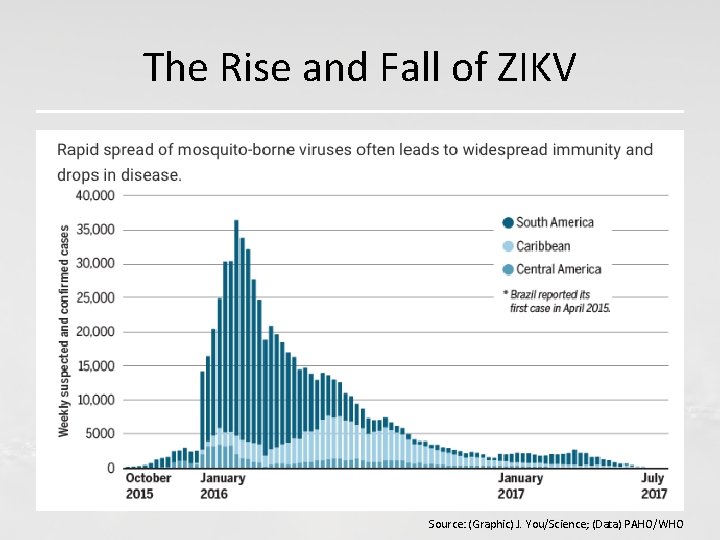
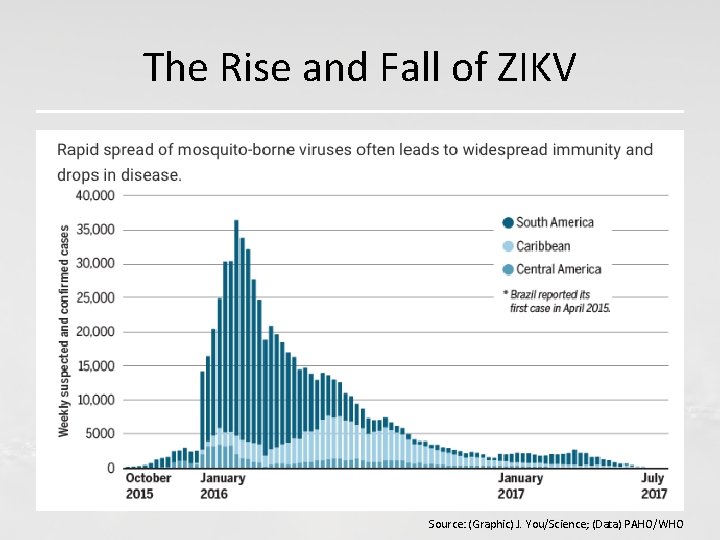
The Rise and Fall of ZIKV Source: (Graphic) J. You/Science; (Data) PAHO/WHO
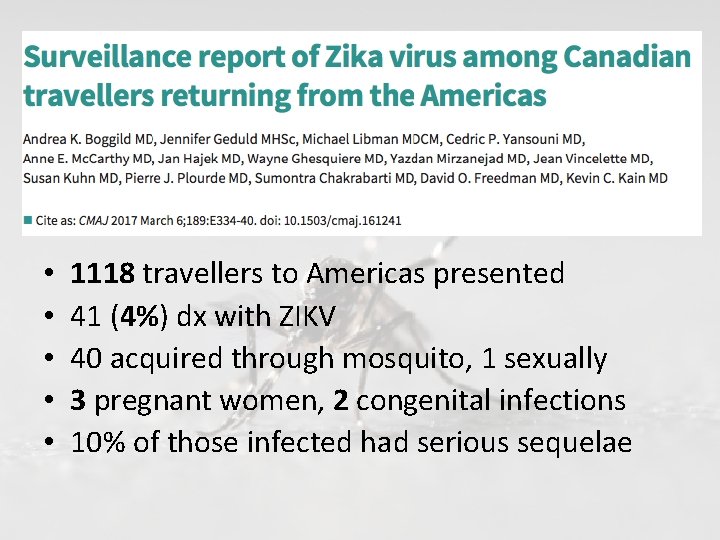
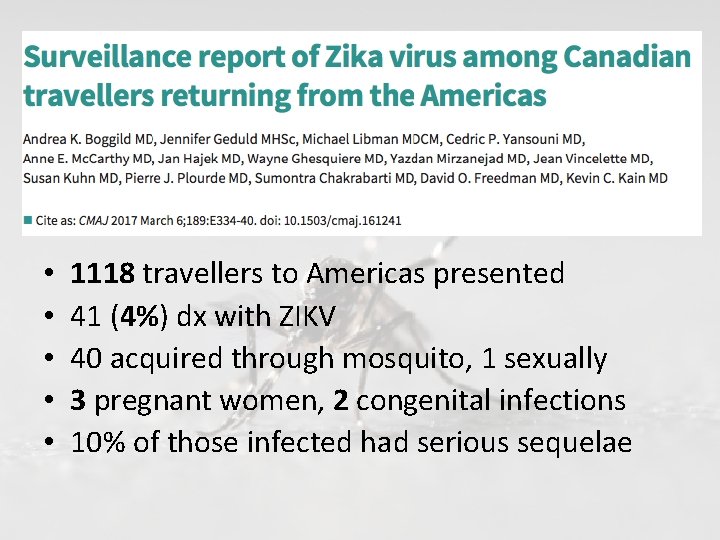
• • • 1118 travellers to Americas presented 41 (4%) dx with ZIKV 40 acquired through mosquito, 1 sexually 3 pregnant women, 2 congenital infections 10% of those infected had serious sequelae

Surveillance in Canada Source: PHAC

ZIKV and Pregnancy
ZIKV and Pregnancy • Pregnant women can be infected with ZIKV • ZIKV may be passed to a fetus around the time of conception • If a woman is infected during pregnancy, ZIKV can be passed to the fetus during pregnancy or around the time of birth

ZIKV and Pregnancy • Incidence of ZIKV in pregnant women is not known • Infection can occur in any trimester • No evidence that pregnant women are more susceptible to Zika than non-pregnant women • Clinical course of Zika is similar for pregnant women & non-pregnant women
ZIKV and Pregnancy • There is evidence of ZIKV detected in: - amniotic fluid - placenta - fetal brain tissue - products of conception • A CDC study released in December 2016, found that ZIKV can continue to replicate in infants’ brains even after birth
ZIKV and Pregnancy • Zika is a cause of Microcephaly
Congenital Zika Syndrome Pattern of congenital anomalies associated with ZIKV infection during pregnancy that includes: 1. Severe microcephaly resulting in a partially collapsed skull 2. Thin cerebral cortices with subcortical calcifications 3. Eye anomalies, incl. macular scarring and focal pigmentary retinal mottling 4. Congenital contractures or limited range of joint motion 5. Marked early hypertonia, or too much muscle tone & symptoms of extrapyramidal involvement
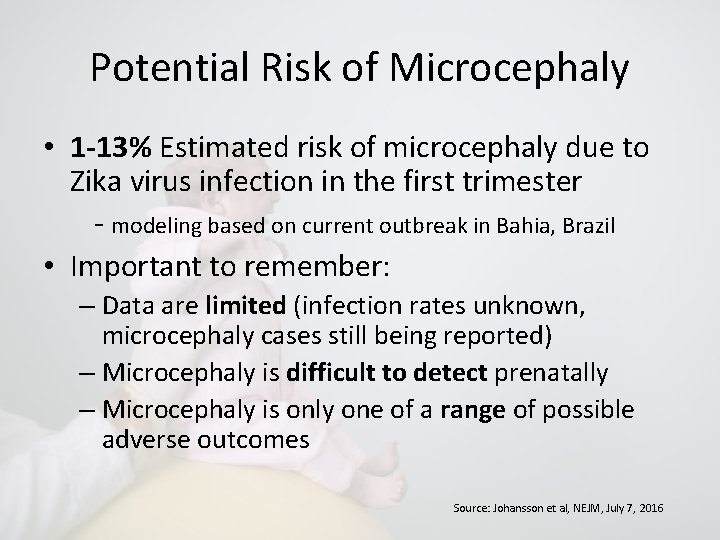
Potential Risk of Microcephaly • 1 -13% Estimated risk of microcephaly due to Zika virus infection in the first trimester - modeling based on current outbreak in Bahia, Brazil • Important to remember: – Data are limited (infection rates unknown, microcephaly cases still being reported) – Microcephaly is difficult to detect prenatally – Microcephaly is only one of a range of possible adverse outcomes Source: Johansson et al, NEJM, July 7, 2016

Potential Risk of Birth Defects Related to Zika Among pregnant women in the US with lab evidence of possible ZIKV infection: • Overall about 6% of fetuses or infants had birth defects potentially related to Zika virus infection • Similar proportions of pregnancies with birth defects (~6%) among both symptomatic and asymptomatic pregnant women • Among women with infection in the 1 st trimester, birth defects were reported in 11% of fetuses or infants Source: Honein et al, JAMA, January 2017
What is a pregnancy care provider to do?
Travel Recommendations • Talk to your patients and partners about travel plans and history • Pregnant women or women planning to become pregnant – advise NOT to travel to countries with active ZIKV transmission • If travelling: – long pants and sleeves – sleep in screened in/air conditioned room – DEET, picaridin and IR 3535 safe in pregnancy Source: PHAC November 2016
Pregnancy Delay Post Travel • Delay conception 2 months if the woman was the traveller • Male partner traveller – condoms/abstinence duration of pregnancy, delay conception 6 months post travel – Serologic/sperm testing of asymptomatic men for ZIKV not currently supported – Sperm washing/IUI considered – degree of risk reduction unknown Source: PHAC November 2016
Who To Test? • Anyone symptomatic with a travel history to the affected areas where symptoms developed 3 days after arrival to 14 days after return • Anyone symptomatic and exposed (ie sexual) to a confirmed case within 3 days post exposure to 14 days after last exposure Source: PHAC November 2016
Who To Test? • All pregnant women returning from Zika area • Women pregnant within 2 months of travelling to Zika area • Pregnant women, unprotected intercourse with male who has been to Zika area in the last 6 months • Pregnant women with ultrasound findings consistent with congenital infection AND history of possible exposure • All patients who become acutely ill within 14 d of return from Zika area • Patients with Guillain-Barre Syndrome, ADEM, myelitis with history of possible exposure Source:
Referral pathway for pregnant women being offered Zika virus testing: • Recommended that women being evaluated for possible Zika virus be offered obstetrical US at time of presentation & again at 19 -20 w – Preliminary or confirmed positive test/abnormality on US consistent with congenital infection Refer to RID at BCWH – Negative of unknown serology and normal US consider offering monthly US for reassurance Source:
How to Test • SYMPTOMATIC: – ZIKV RT PCR (blood/urine) within 10 d of symptom onset – ZIKV Ig. M if > 10 d since symptom onset • ASYMPTOMATIC PREGNANT: – ZIKV Ig. M 2 (4) w post exposure (NML recommendation) – if Ig. M positive – must be confirmed as ZIKV as much cross reaction with other flaviviruses
National Microbiology Laboratory TAT (Turn around time) • PCR: minimum 5 business days • Ig. M ELISA: minimum 7 business days • PRNT (Plague Reduction Neutralization Test): minimum 14 business days after ELISA result • MANY Ig. M requests being returned until further details provided: – travel locations and dates – clinical symptoms and signs – gestational age at time of travel
Management of suspected/probable cases in pregnancy • No prophylaxis/vaccine available other than avoidance of exposure • No antivirals known effective • TOP may be considered for patient • Prepare for appropriate location for delivery
ZIKA Prevention – Future possibilities • Oxitec – genetically modified mosquitoes • Recombinant vaccine, VLP, killed inactivated
Questions
 Is the zika virus lytic or lysogenic
Is the zika virus lytic or lysogenic Rick mentz
Rick mentz Dr rick mentz
Dr rick mentz Zika
Zika Spotting differential diagnosis
Spotting differential diagnosis What is visitor pre registration in picme
What is visitor pre registration in picme Pregnancy and fetal development brainpop answers
Pregnancy and fetal development brainpop answers Mississippi classification of hellp syndrome
Mississippi classification of hellp syndrome Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Trimester graphic organizer
Trimester graphic organizer Icd 10 kontrol nifas normal
Icd 10 kontrol nifas normal Adoloscense
Adoloscense Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Do pregnancy cramps feel like period cramps
Do pregnancy cramps feel like period cramps Singapore bible college
Singapore bible college Rick lawford
Rick lawford Rick snodgrass
Rick snodgrass When was rick riordan born
When was rick riordan born Andreas gohritz
Andreas gohritz Rick trebino lectures
Rick trebino lectures Dynamodb shard size
Dynamodb shard size Rick cruz hisd
Rick cruz hisd Rick stepp san antonio
Rick stepp san antonio Rick domingo faa
Rick domingo faa Dr rick griffith
Dr rick griffith My lan graziani
My lan graziani Rick griffith bible study downloads
Rick griffith bible study downloads Rick malter
Rick malter Paulsen
Paulsen Rick lawford
Rick lawford Dr rick griffith
Dr rick griffith Rick donlan
Rick donlan