Module 4 HIV Infection in Women HIV Infection



- Slides: 29
Module 4 HIV Infection in Women
HIV Infection in Women • Garrett Colmorgen, MD, Director Maternal Fetal Medicine, Christiana Care Health Services, Wilmington, Delaware • Staff of the Pennsylvania/Mid-Atlantic AIDS Education & Training Center, Delaware Local Performance Site - P. Lincoln, N. Bennett, M. A. Bartkowski
Demographics of HIV in Women • Fastest growing group in the United States • 4 th leading cause of death aged 25 to 44 in the United States • Disproportionately affects African Americans & Hispanics living on the eastern seaboard CDC-2000
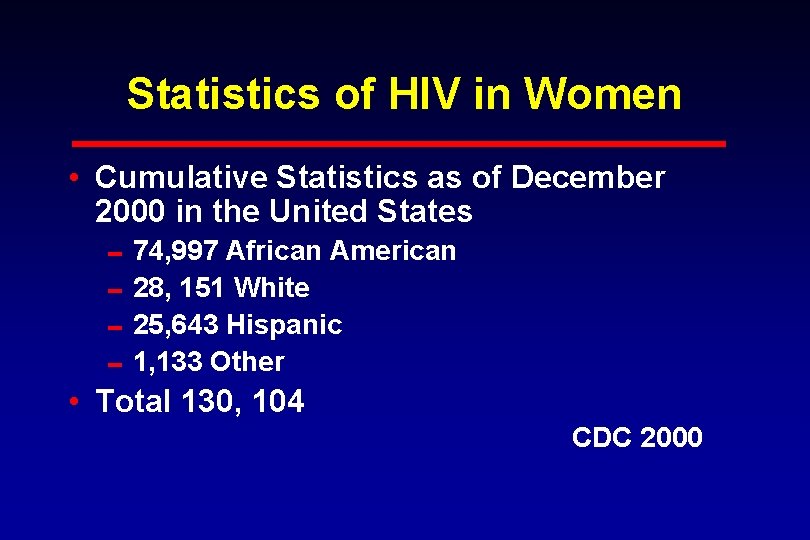
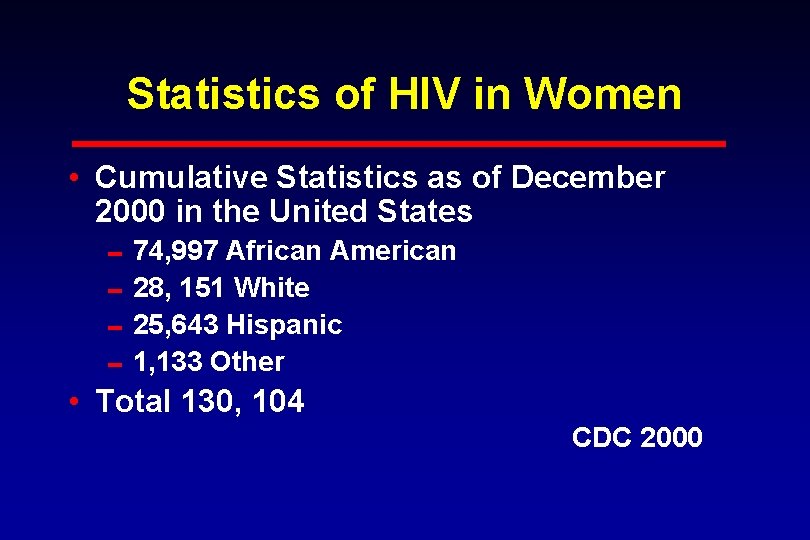
Statistics of HIV in Women • Cumulative Statistics as of December 2000 in the United States 074, 997 African American 028, 151 White 025, 643 Hispanic 01, 133 Other • Total 130, 104 CDC 2000
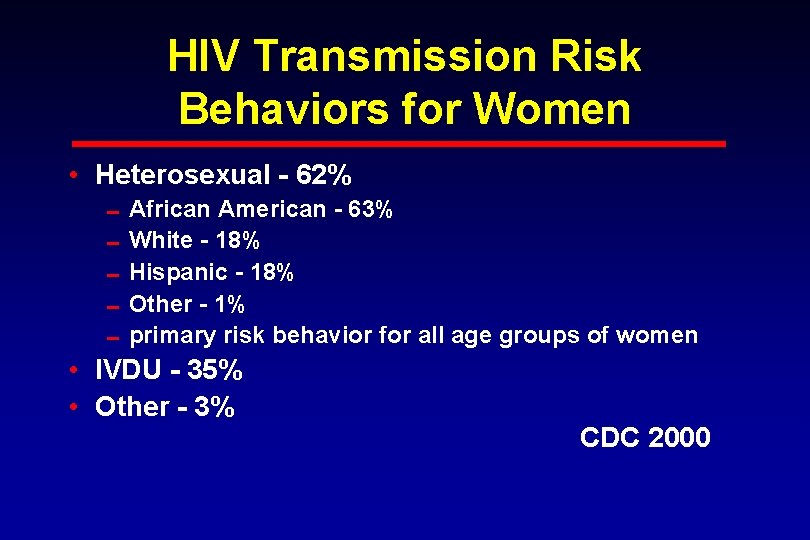
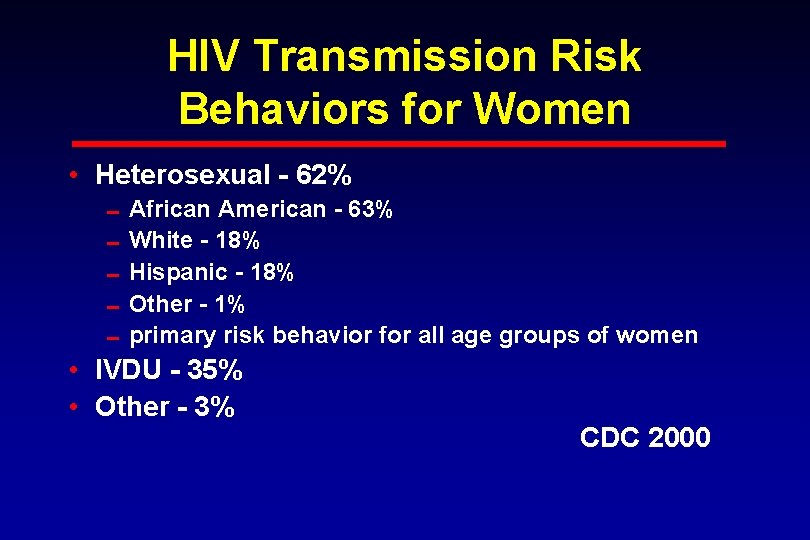
HIV Transmission Risk Behaviors for Women • Heterosexual - 62% 0 African American - 63% 0 White - 18% 0 Hispanic - 18% 0 Other - 1% 0 primary risk behavior for all age groups of women • IVDU - 35% • Other - 3% CDC 2000
Female Condom • “Reality” - only brand currently marketed in the US • Made of polyurethane, sheath closed at one end with flexible rings at both ends Anderson, J. 2001
Microbicides • Strategy enabling women to have control over safer sex/prevention of HIV • Nonoxynol-9 increases risk of HIV infection • Clinical trials of topical microbicides are being conducted Anderson, J. 2001
Gender Bias Transmission • More efficient from man to woman than woman to man • Related to number of infectious particles in body fluid • Related to volume of fluids exchanged • Related to surface area coming in contact with infected body fluid HRSA: BPHC & AETC
Risk Factors for Male to Female HIV Transmission • Anal Intercourse • Lack of male circumcision • Genital ulcers (syphilis, herpes simplex, chancroid) • Sexually Transmitted Diseases • Multiple sexual partners

Special Consideration • Early Adolescent 0 immaturity of the female genital track increases risk of transmission • Women over 50 years of age 0 atrophic vaginitis caused by decreased lubrication 0 older females are generally not perceived to be at risk
Natural History of HIV Disease in Women • Same as in men except for GYN symptoms and disease conditions • 1993 CDC added invasive cervical cancer as an AIDS defining condition • Women are often diagnosed late • Women may have barriers to care HRSA: BPHC & AETC
Challenges in Caring for Women with HIV • Statistically economically poorer than men • More likely to be single parents 0 lack of child care 0 lack of support • More likely to be uninsured HRSA: BPHC & AETC
Signs and Symptoms of HIV in Women • Acute Seroconversion - (No distinct gender differences however many of these s&s often go under addressed) 0 fever 0 swollen glands Bartlett, J. 1999
Signs and Symptoms of HIV in Women cont’ 0 Rash - macular or maculopapular, usually nonpururitic. Truncal / facial distribution can involve arms and legs. Often appears several days past onset of fever. 0 Fatigue 0 Mono-spot test is negative 0 Bartlett, J. 1999
HIV-Related Gynecological Conditions • • • Vaginal candidiasis Human Papilloma Virus Genital Ulcers Pelvic Inflammatory Disease Cervical Dysplasia/Neoplasia Menstrual Disturbances HRSA: BPHC & AETC
Diagnostic Studies • Pap smear 0 two studies the first year of diagnosis 0 annually if normal 0 recommended every 6 months if HIV is symptomatic • Colposcopy USPHS/IDSA 2001

Prenatal & Family Planning HIV Screening • DHHS guidelines suggest universal HIV testing with patient notification as a routine component of prenatal care • Pre and post test counseling & informed consent - laws vary by state USPHS/IDSA 2001

Pregnancy • Does not appear to accelerate HIV infection
Perinatal HIV Transmission May Occur • Antepartum 0 during pregnancy • Intrapartum 0 during labor 0 during delivery • Postpartum-through breast feeding HRSA: BPHC & AETC
Reducing Perinatal Transmission • ACTG 076 0 women given AZT after first trimester 0 AZT administered intravenously during labor 0 newborn receives AZT for 6 weeks 0 transmission reduced by 67. 5% • Combination therapy has reduced the rate even further HRSA: BPHC & AETC
Antepartum/Intrapartum Management Considerations • • Avoid amniocentesis Avoid premature rupture of membranes Avoid fetal scalp monitoring Delay episiotomy HRSA: BPHC & AETC
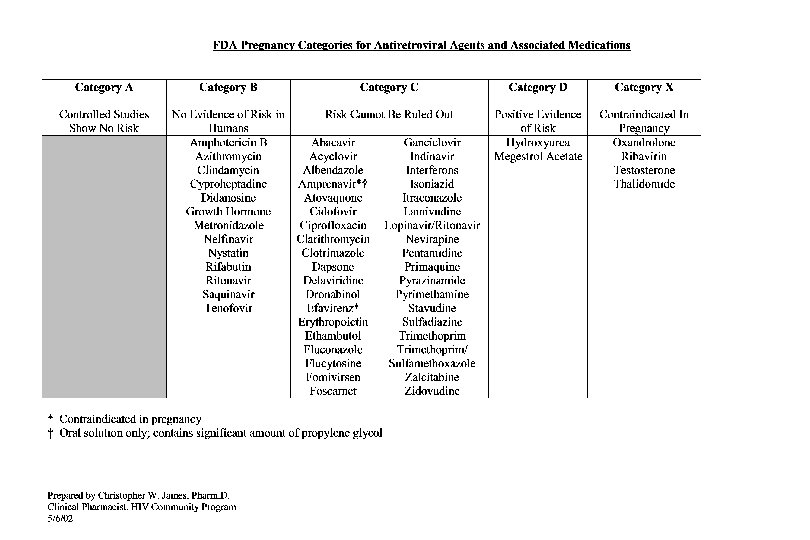
HIV Medications to avoid during Pregnancy • Efavirenz - associated with anencephaly, anopthalmia Neural tube defects in primates • Indinavir - Potential for nephrolithiasis and neonatal hyperbilirubinemia De. Lorenzo, L. 2001
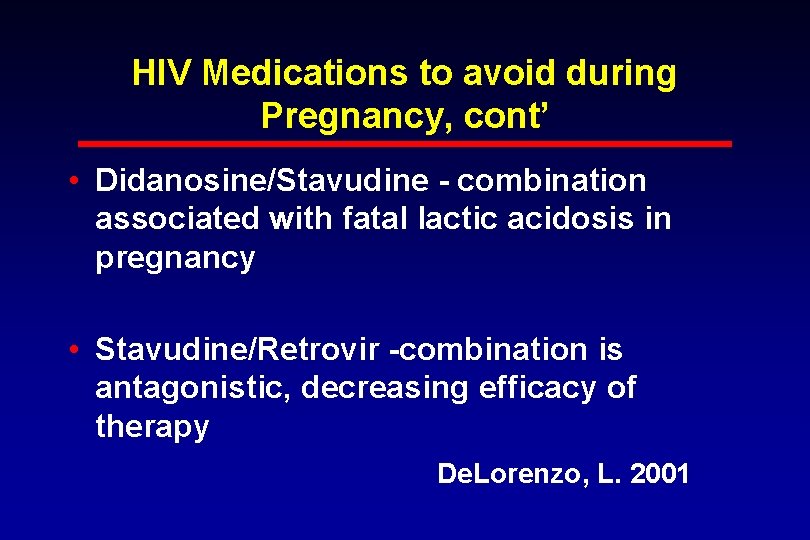
HIV Medications to avoid during Pregnancy, cont’ • Didanosine/Stavudine - combination associated with fatal lactic acidosis in pregnancy • Stavudine/Retrovir -combination is antagonistic, decreasing efficacy of therapy De. Lorenzo, L. 2001
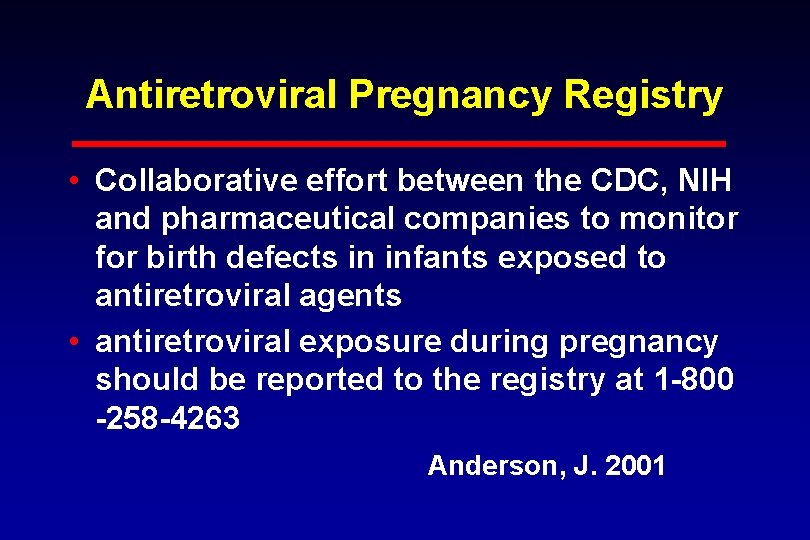
Antiretroviral Pregnancy Registry • Collaborative effort between the CDC, NIH and pharmaceutical companies to monitor for birth defects in infants exposed to antiretroviral agents • antiretroviral exposure during pregnancy should be reported to the registry at 1 -800 -258 -4263 Anderson, J. 2001
Current Prevention Message-Is it Reality ? • • • Abstinence Monogamy Reduce number of partners Ask partner about history of infection Enforce use of condoms Colmorgen, G. 1999
References • Anderson, J. (Ed. ) (2001). A guide to the clinical care of women with HIV. Rockville, MD: HIV/AIDS Bureau, Health Resources and Services Administration. [Available on-line: http: //www. hab. hrsa. gov/publications. html]. • Bartlett, J. & Gallant, J. (2001). 2001 -2002 Medical Management of HIV Infection. [Available on-line: http; //hopkins-aids. edu
References, cont’ • Center for Disease Control and Prevention. (2002, February). Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1 -Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV 1 Transmission in the United States. [Available on-line: http: //www. hivatis. org. ]
References, cont’ • De. Lorenzo, L. (2001). Clinical Nursing Series. Nursing Care of the HIV-Infected Patient. Fourth Edition. Western Schools Press.
 C device module module 1
C device module module 1 Procentowe ryzyko zakażenia hiv
Procentowe ryzyko zakażenia hiv Hora de agora
Hora de agora A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Hiv
Hiv Hiv diagnostics conference
Hiv diagnostics conference Hiv cure
Hiv cure Bízom benned uram jézus
Bízom benned uram jézus Retrovrus
Retrovrus Leukopenia
Leukopenia Dot
Dot Hiv lifecycle
Hiv lifecycle Types of hiv counselling
Types of hiv counselling Hiv treatments
Hiv treatments Hiv positive results images
Hiv positive results images Where did hiv come from
Where did hiv come from Ibase hiv
Ibase hiv Hiv stays alive in dried blood
Hiv stays alive in dried blood Hiv transmissions
Hiv transmissions Klamydia syntomer
Klamydia syntomer Hiv
Hiv Hiv diagnosis algorithm
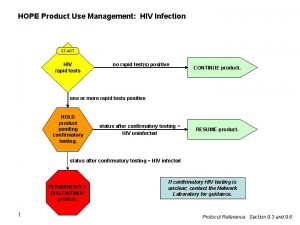
Hiv diagnosis algorithm Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Dot resposta
Dot resposta Hiv in adults
Hiv in adults Hiv test window period
Hiv test window period Phdp in hiv
Phdp in hiv Prinsip notifikasi pasangan
Prinsip notifikasi pasangan Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Hiv
Hiv