Acute HIV Infection New Frontiers for HIV Prevention

![AHI • 1% of patients with negative tests for EBV had AHI [1] • AHI • 1% of patients with negative tests for EBV had AHI [1] •](https://slidetodoc.com/presentation_image/427ac7cb9109dd5d1a79750617473173/image-20.jpg)
![Role of AHI in Secondary Transmissions • Koopman [1] and Jacquez [2] used population Role of AHI in Secondary Transmissions • Koopman [1] and Jacquez [2] used population](https://slidetodoc.com/presentation_image/427ac7cb9109dd5d1a79750617473173/image-28.jpg)



- Slides: 48
Acute HIV Infection: New Frontiers for HIV Prevention Antonio E. Urbina, MD Medical Director HIV Education and Training St. Vincent Catholic Medical Center-Manhattan May 17, 2006 St. Vincent Catholic Medical Center is a Local Performance Site of the NY/NJ AETC
Lifetime Cost of HIV Care in the US in the Current Treatment Era $500, 000 B R Schackman, et al Abstract, 3 rd IAS Conference
HIV Incidence Since 1999, HIV infections have remained steady at 40 -45, 000/year CDC HIV/AIDS Surveillance Report
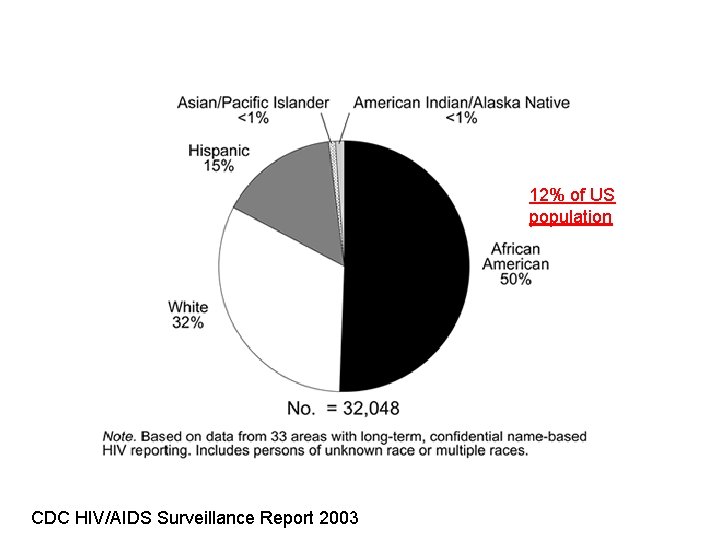
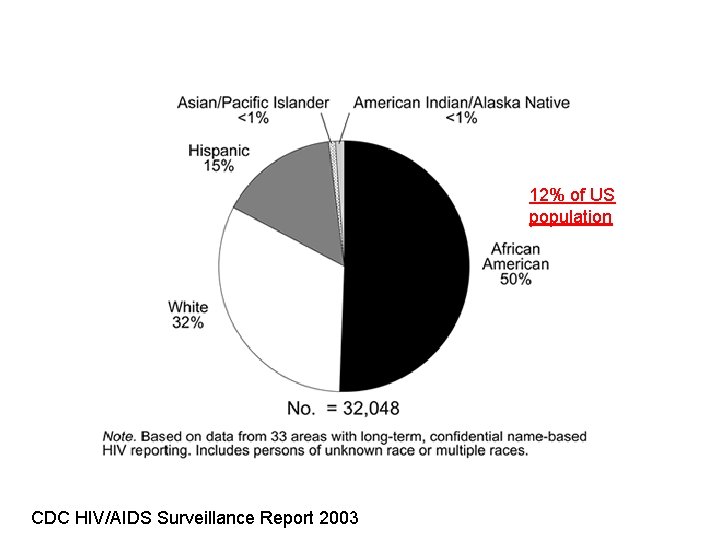
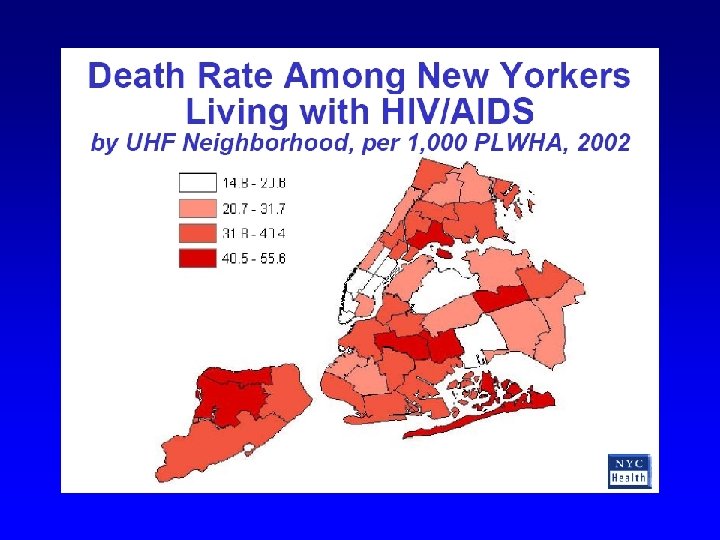
12% of US population CDC HIV/AIDS Surveillance Report 2003
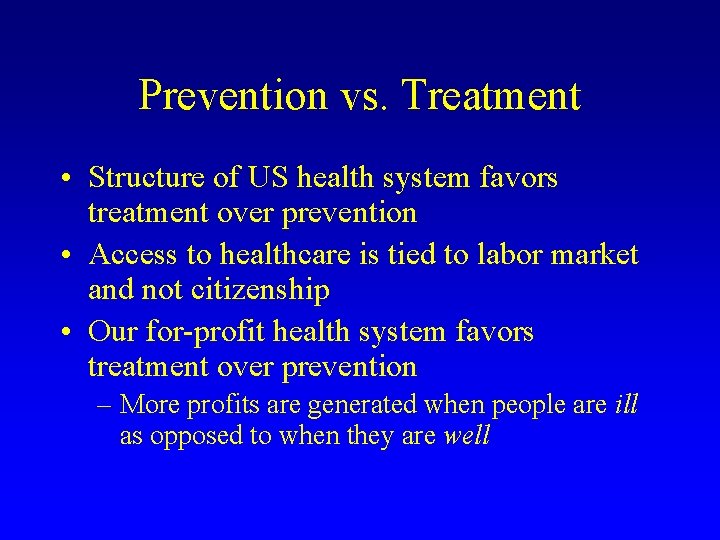
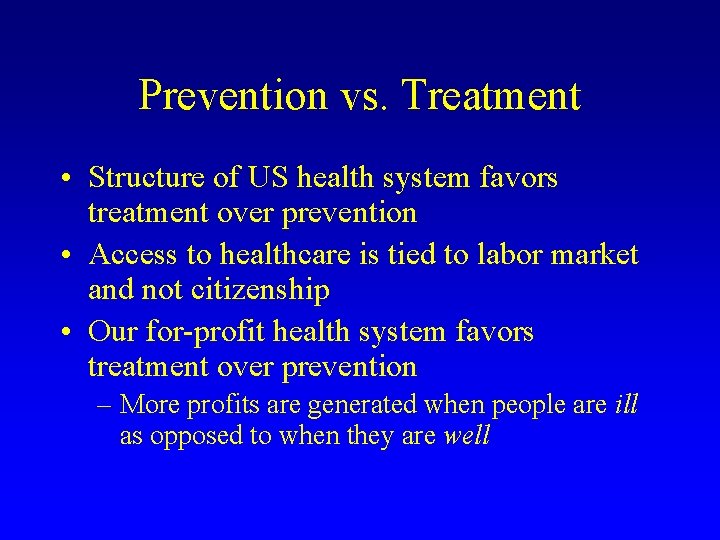
Prevention vs. Treatment • Structure of US health system favors treatment over prevention • Access to healthcare is tied to labor market and not citizenship • Our for-profit health system favors treatment over prevention – More profits are generated when people are ill as opposed to when they are well
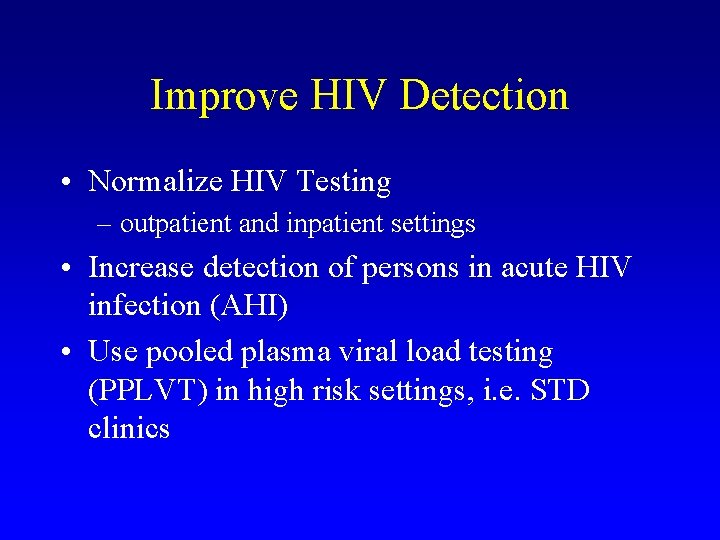
Improve HIV Detection • Normalize HIV Testing – outpatient and inpatient settings • Increase detection of persons in acute HIV infection (AHI) • Use pooled plasma viral load testing (PPLVT) in high risk settings, i. e. STD clinics
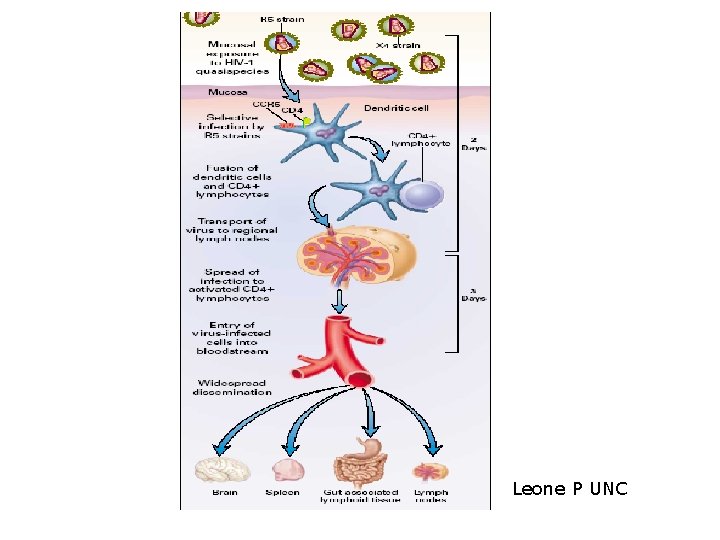
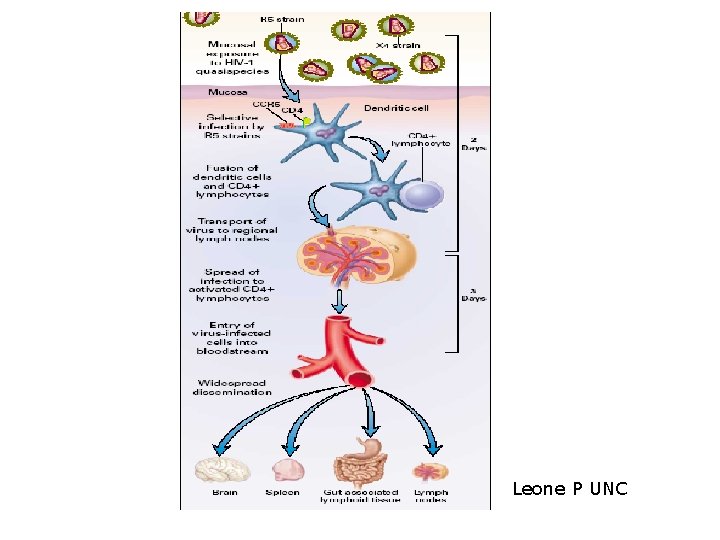
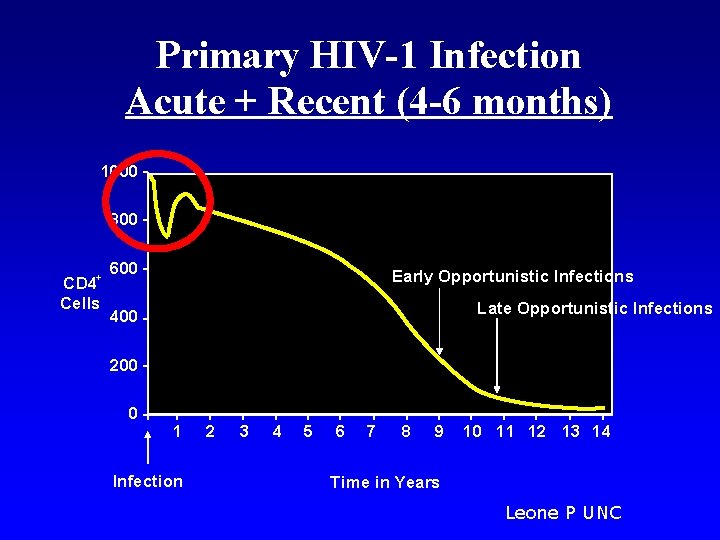
Leone P UNC
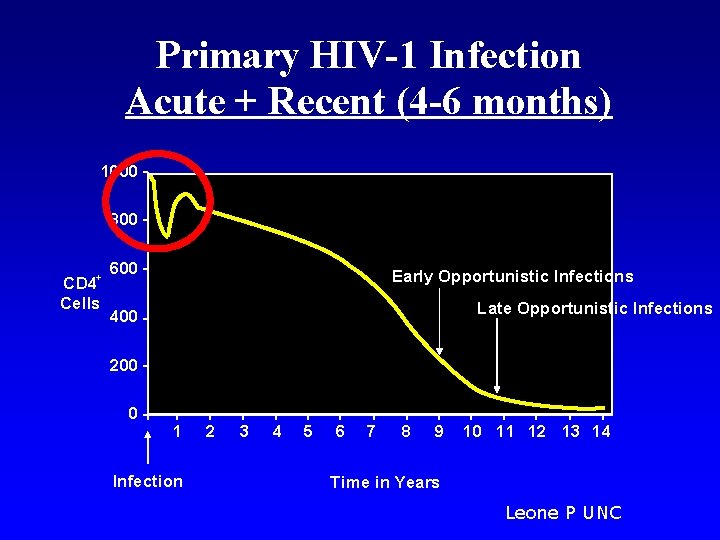
Primary HIV-1 Infection Acute + Recent (4 -6 months) 1000 800 + CD 4 Cells 600 Early Opportunistic Infections Late Opportunistic Infections 400 200 0 1 Infection 2 3 4 5 6 7 8 9 10 11 12 13 14 Time in Years Leone P UNC
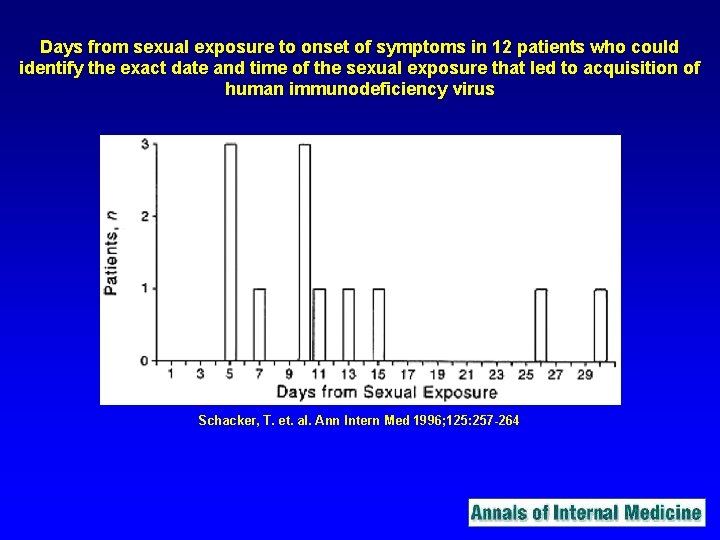
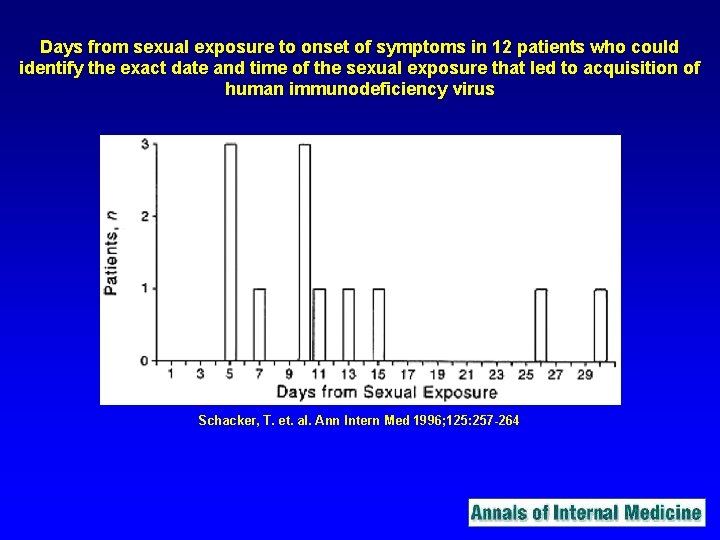
Days from sexual exposure to onset of symptoms in 12 patients who could identify the exact date and time of the sexual exposure that led to acquisition of human immunodeficiency virus Schacker, T. et. al. Ann Intern Med 1996; 125: 257 -264
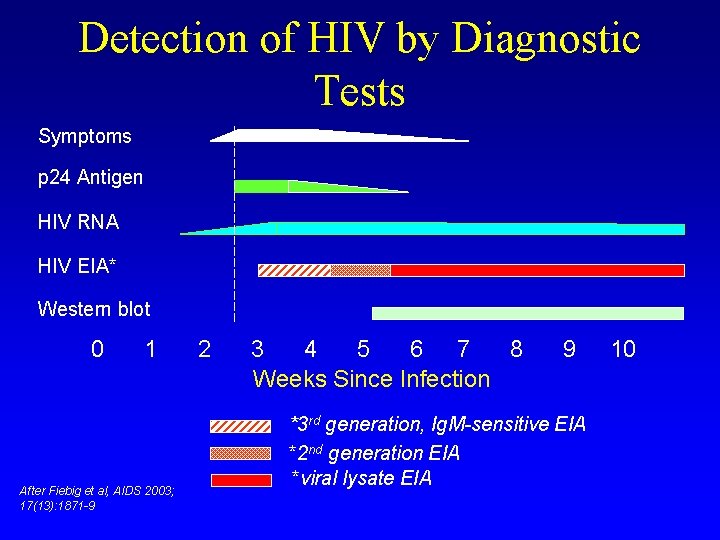
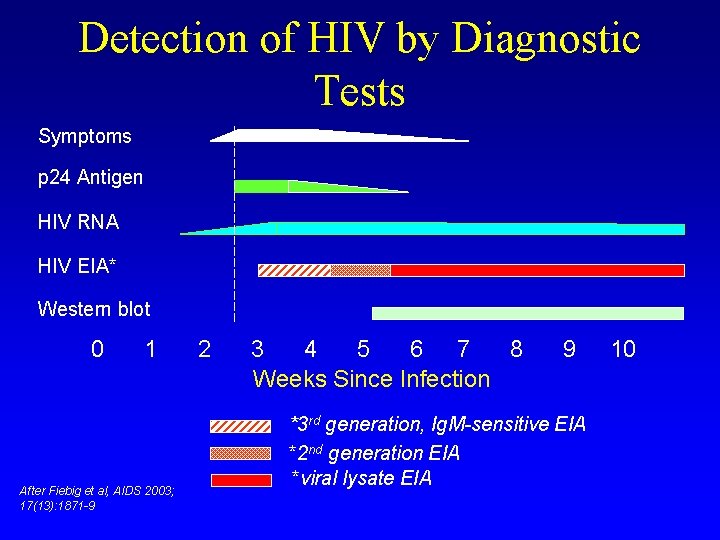
Detection of HIV by Diagnostic Tests Symptoms p 24 Antigen HIV RNA HIV EIA* Western blot 0 1 After Fiebig et al, AIDS 2003; 17(13): 1871 -9 2 3 4 5 6 7 8 Weeks Since Infection 9 *3 rd generation, Ig. M-sensitive EIA *2 nd generation EIA *viral lysate EIA 10
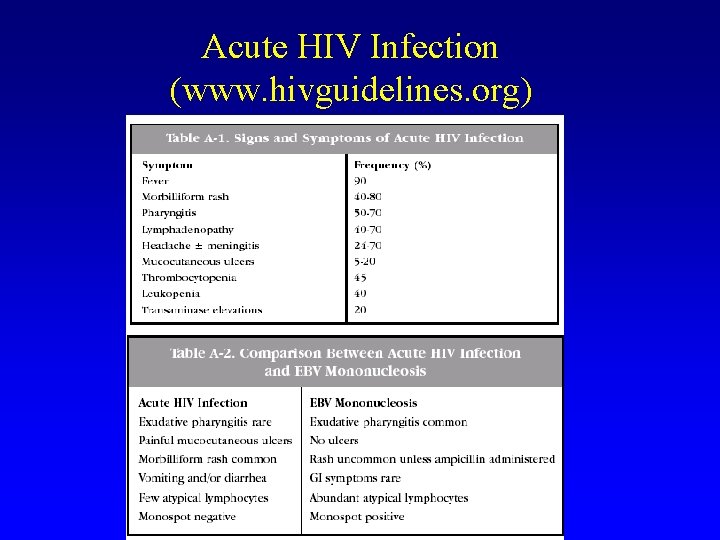
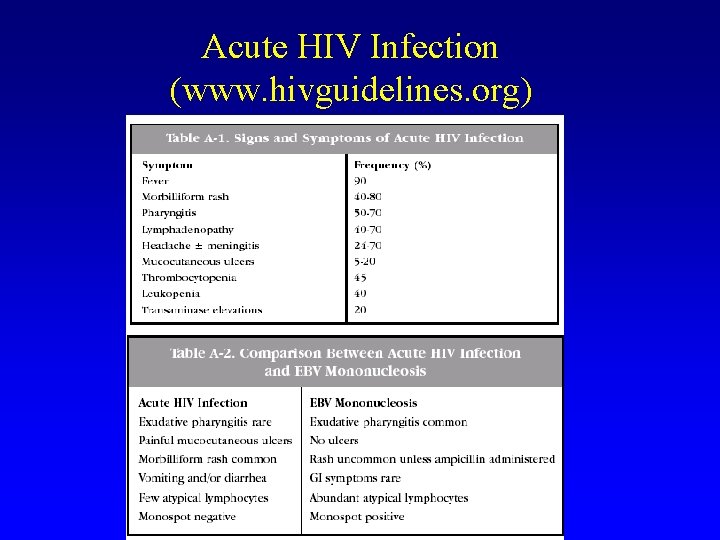
Acute HIV Infection (www. hivguidelines. org)
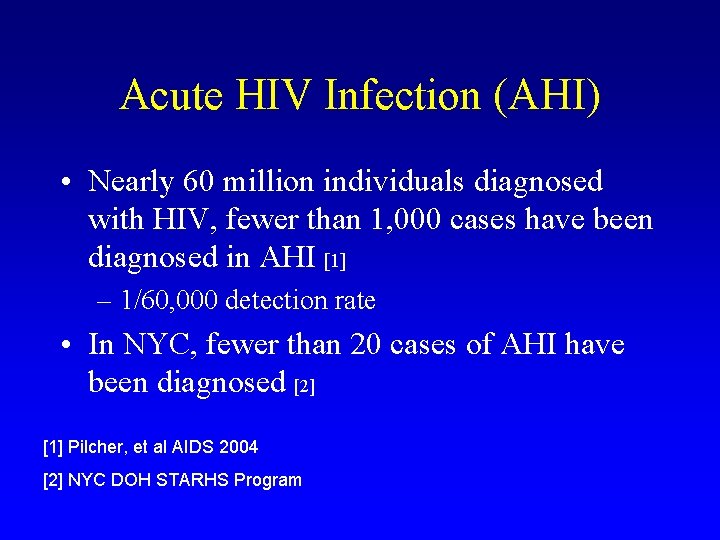
How effective are we at capturing AHI?
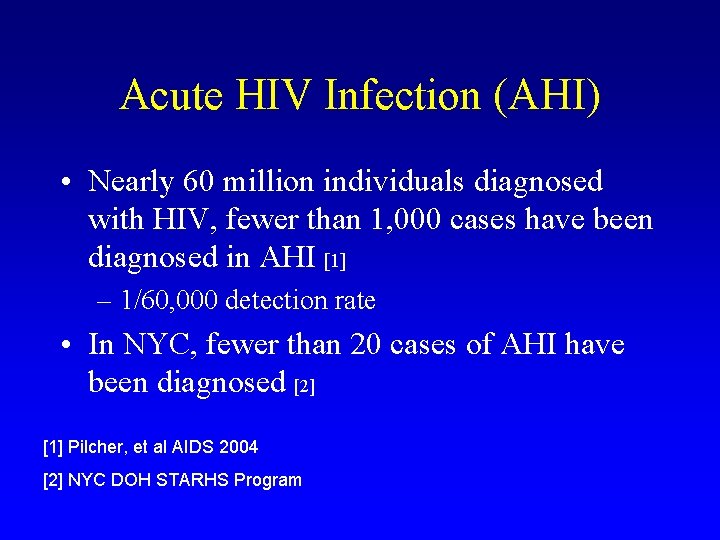
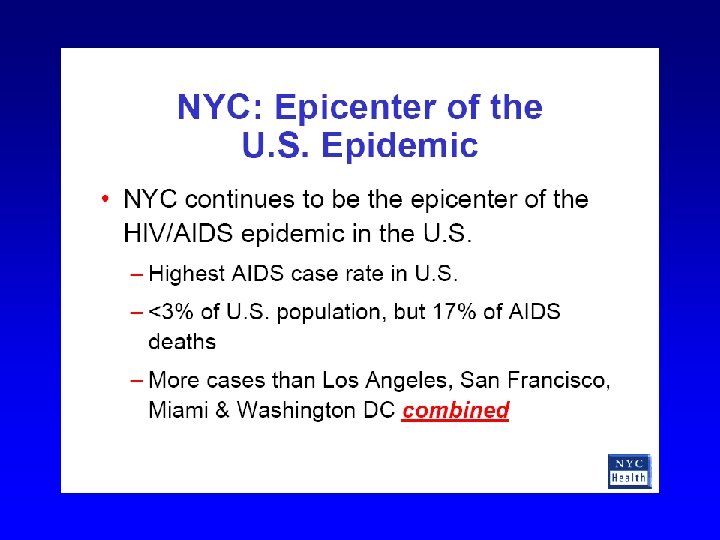
Acute HIV Infection (AHI) • Nearly 60 million individuals diagnosed with HIV, fewer than 1, 000 cases have been diagnosed in AHI [1] – 1/60, 000 detection rate • In NYC, fewer than 20 cases of AHI have been diagnosed [2] [1] Pilcher, et al AIDS 2004 [2] NYC DOH STARHS Program

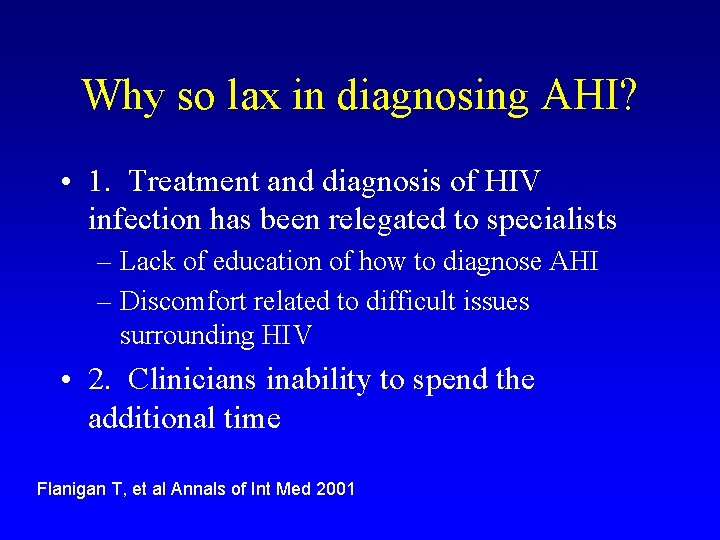
Why so lax in diagnosing AHI? • 1. Treatment and diagnosis of HIV infection has been relegated to specialists – Lack of education of how to diagnose AHI – Discomfort related to difficult issues surrounding HIV • 2. Clinicians inability to spend the additional time Flanigan T, et al Annals of Int Med 2001
![AHI 1 of patients with negative tests for EBV had AHI 1 AHI • 1% of patients with negative tests for EBV had AHI [1] •](https://slidetodoc.com/presentation_image/427ac7cb9109dd5d1a79750617473173/image-20.jpg)
AHI • 1% of patients with negative tests for EBV had AHI [1] • 1% of patients with “any viral syndrome” in a Boston urgent care center had AHI [2] • In a Malawi STD clinic, 2. 8% of all male clients with acute STD had AHI [3] [1] Rosenberg, et al N Engl J Med 1999 [2] Pincus, et al Clin Infect Dis 2003 [3] Pilcher, et al AIDS 2004
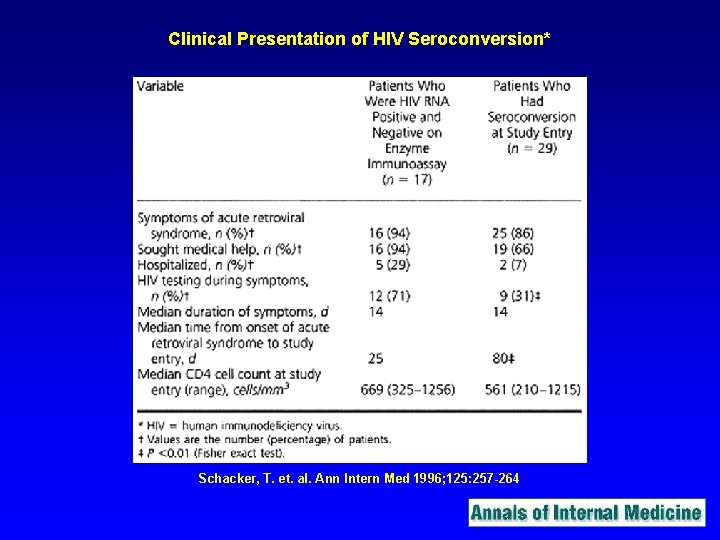
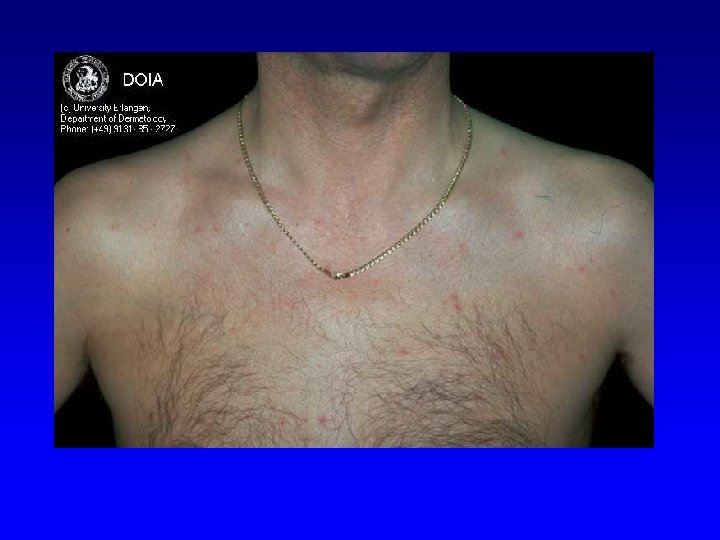
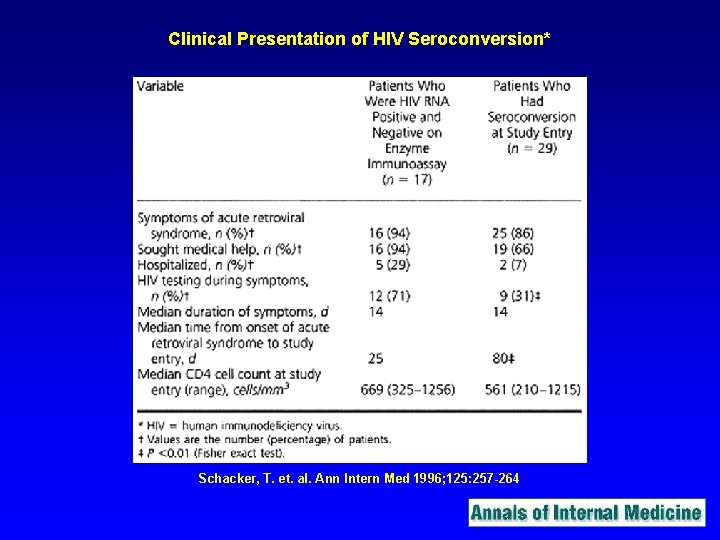
Clinical Presentation of HIV Seroconversion* Schacker, T. et. al. Ann Intern Med 1996; 125: 257 -264
How do you diagnose?
ICD-9 Code for AHI (exposure to HIV) VO 1. 7
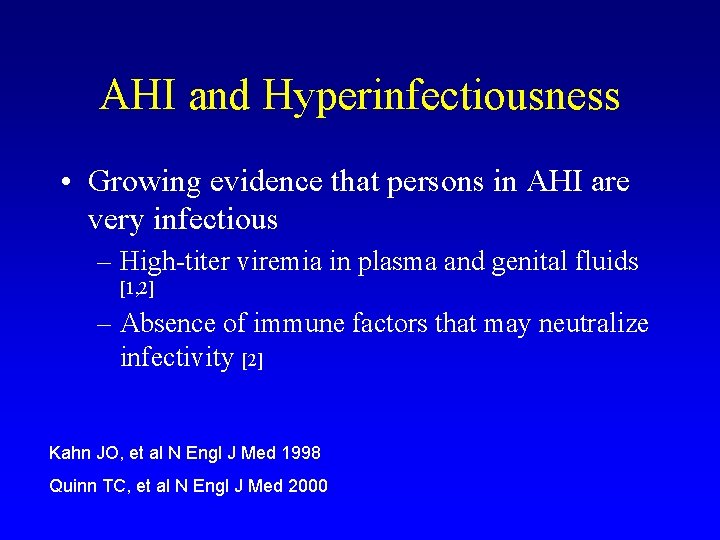
AHI and Hyperinfectiousness • Growing evidence that persons in AHI are very infectious – High-titer viremia in plasma and genital fluids [1, 2] – Absence of immune factors that may neutralize infectivity [2] Kahn JO, et al N Engl J Med 1998 Quinn TC, et al N Engl J Med 2000
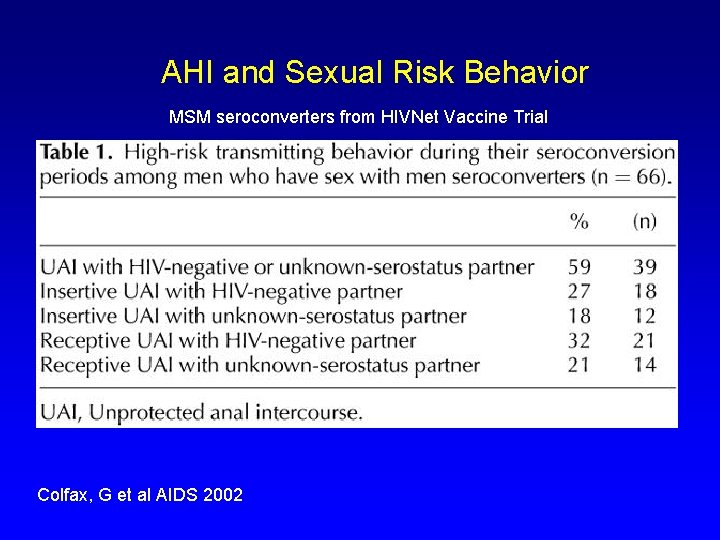
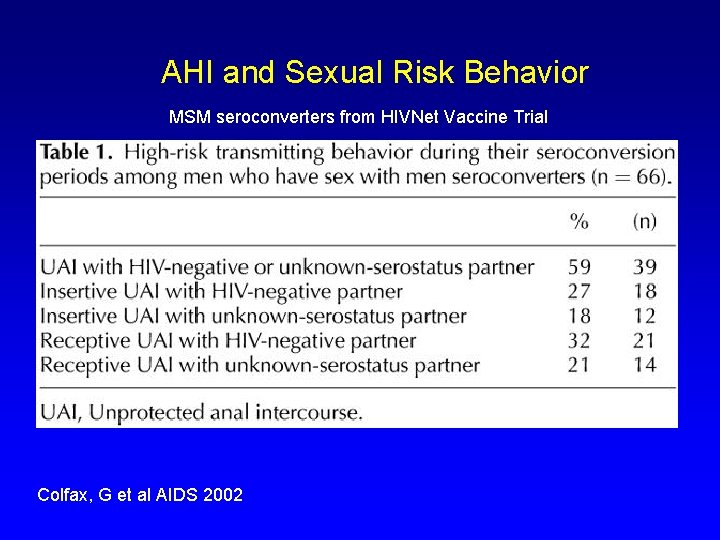
AHI and Sexual Risk Behavior MSM seroconverters from HIVNet Vaccine Trial Colfax, G et al AIDS 2002
![Role of AHI in Secondary Transmissions Koopman 1 and Jacquez 2 used population Role of AHI in Secondary Transmissions • Koopman [1] and Jacquez [2] used population](https://slidetodoc.com/presentation_image/427ac7cb9109dd5d1a79750617473173/image-28.jpg)
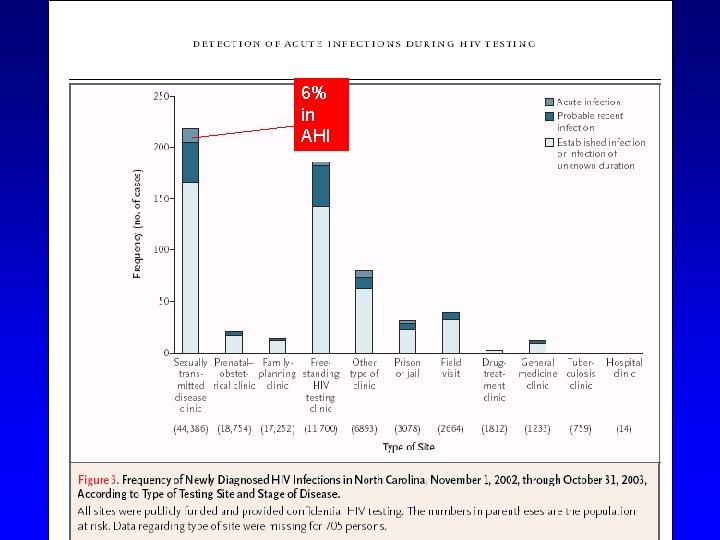
Role of AHI in Secondary Transmissions • Koopman [1] and Jacquez [2] used population modeling to argue that the spread of HIV from patients in AHI could contribute disproportionately to the epidemic – suggested that patients in AHI could be up to 1, 000 x more infectious than those in chronic infection Koopman JS, et al J Acquir Immune Defic Synd Hum Retrovirol 1997 Jacquez JA, et al J Acquir Immune Defic Syndr 1994

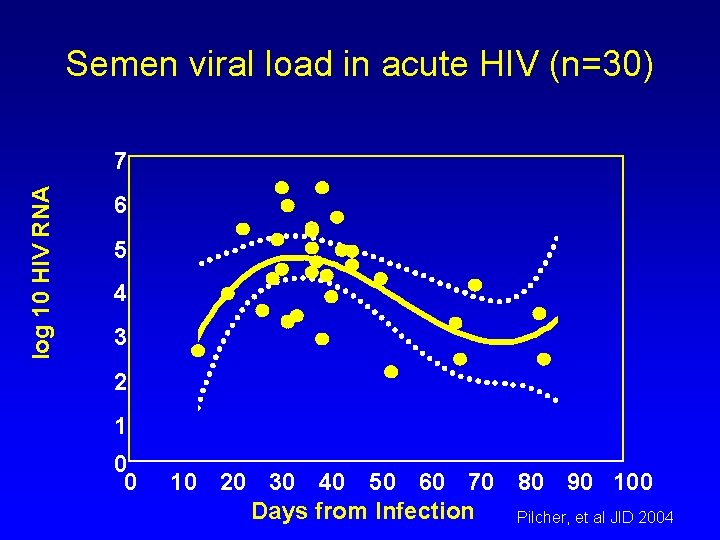
Blood viral load in acute HIV (n=171) log 10 HIV RNA Average fitted curve, with 95% confidence intervals 8 7 6 5 4 3 2 1 0 8 -10 fold increase risk from peak to day 54 0 100 200 300 Days from Infection Peak: day 23 Pilcher, et al JID 2004
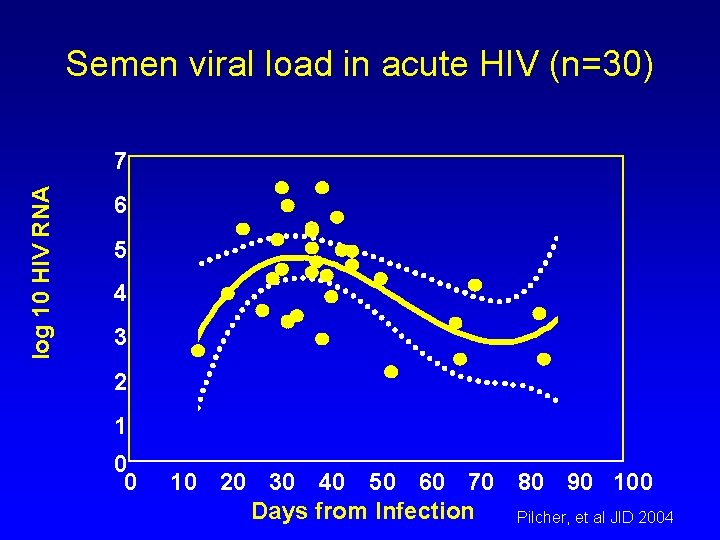
Semen viral load in acute HIV (n=30) log 10 HIV RNA 7 6 5 4 3 2 1 0 0 10 20 30 40 50 60 70 80 90 100 Days from Infection Pilcher, et al JID 2004
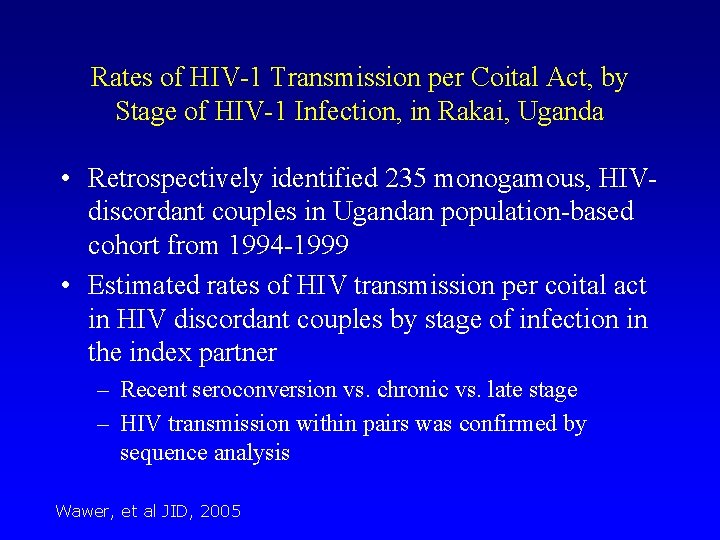
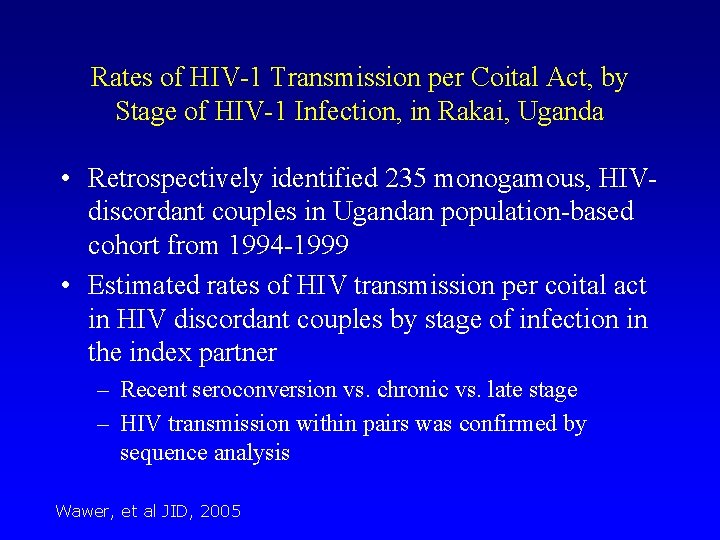
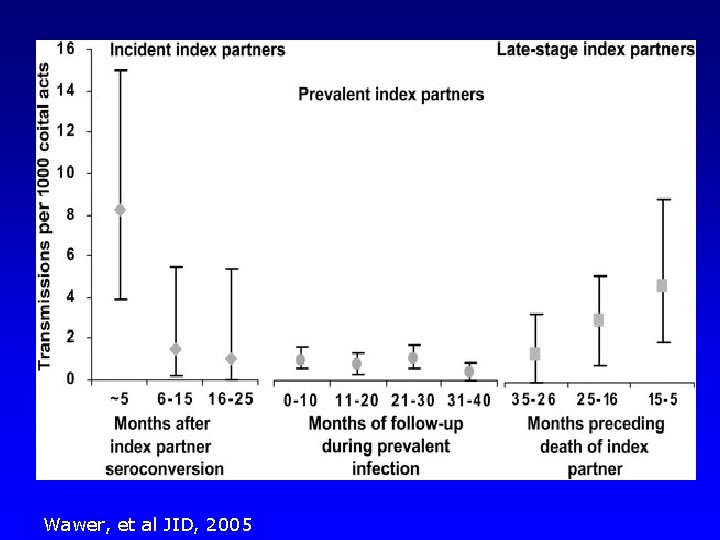
Rates of HIV-1 Transmission per Coital Act, by Stage of HIV-1 Infection, in Rakai, Uganda • Retrospectively identified 235 monogamous, HIVdiscordant couples in Ugandan population-based cohort from 1994 -1999 • Estimated rates of HIV transmission per coital act in HIV discordant couples by stage of infection in the index partner – Recent seroconversion vs. chronic vs. late stage – HIV transmission within pairs was confirmed by sequence analysis Wawer, et al JID, 2005
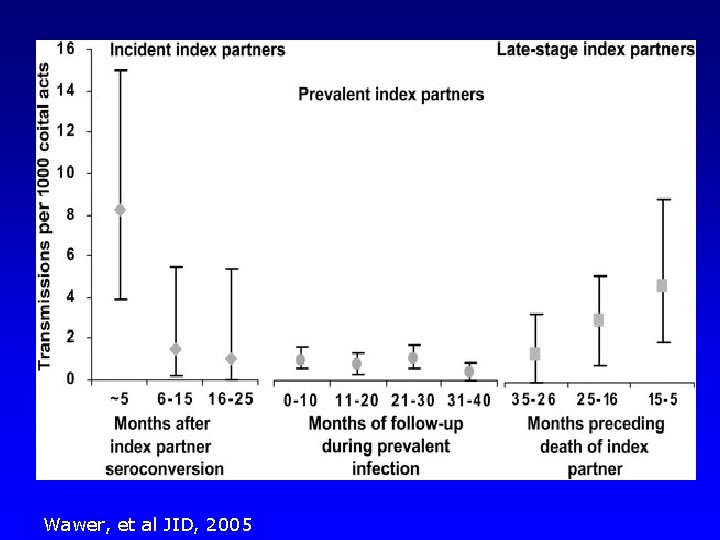
Wawer, et al JID, 2005
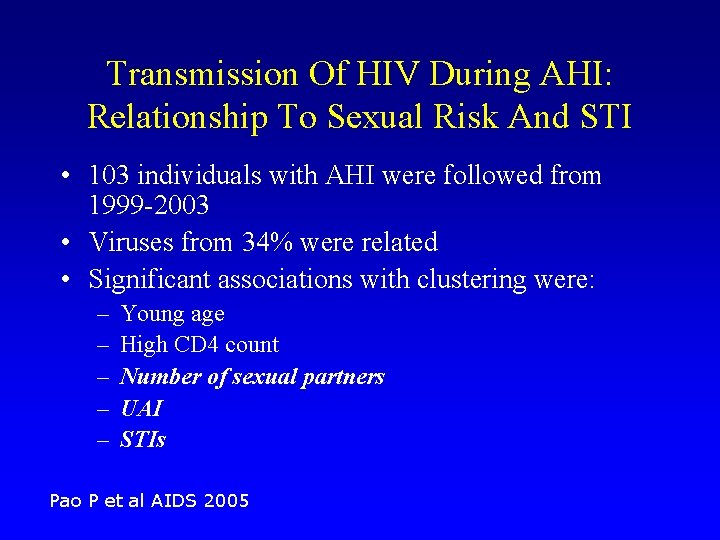
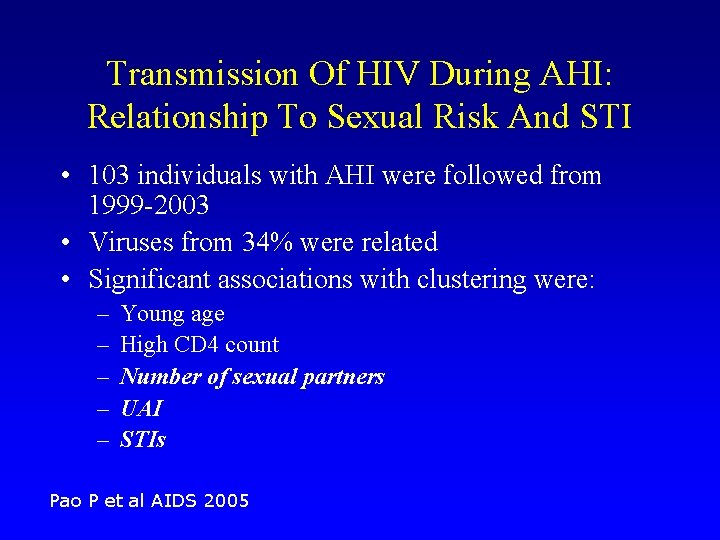
Transmission Of HIV During AHI: Relationship To Sexual Risk And STI • 103 individuals with AHI were followed from 1999 -2003 • Viruses from 34% were related • Significant associations with clustering were: – – – Young age High CD 4 count Number of sexual partners UAI STIs Pao P et al AIDS 2005

Clustering: efficient dissemination by core groups and identification of networks “Efficient disseminator” Identification of network Identification via PHI “Acute Case”
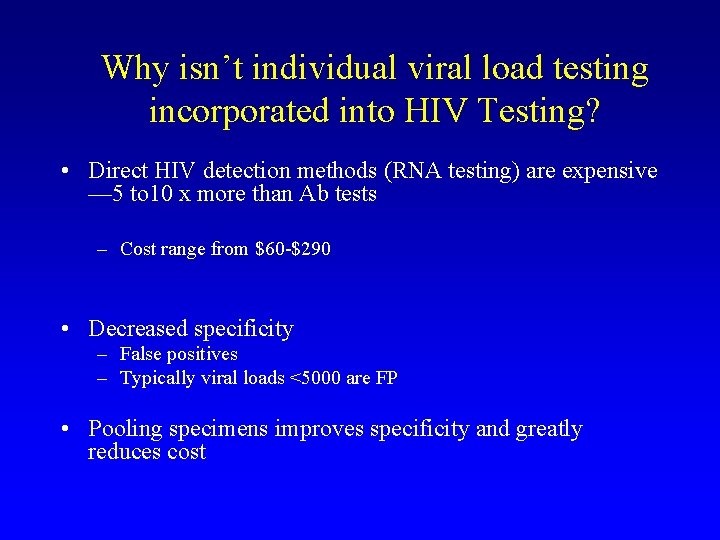
Why isn’t individual viral load testing incorporated into HIV Testing? • Direct HIV detection methods (RNA testing) are expensive — 5 to 10 x more than Ab tests – Cost range from $60 -$290 • Decreased specificity – False positives – Typically viral loads <5000 are FP • Pooling specimens improves specificity and greatly reduces cost
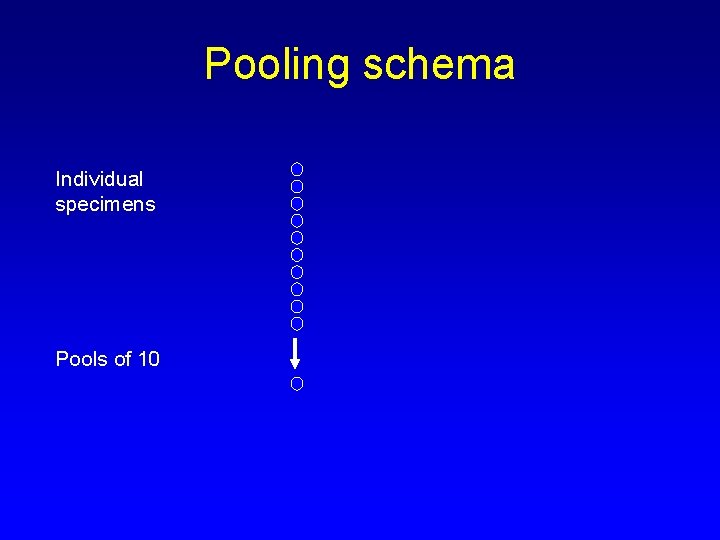
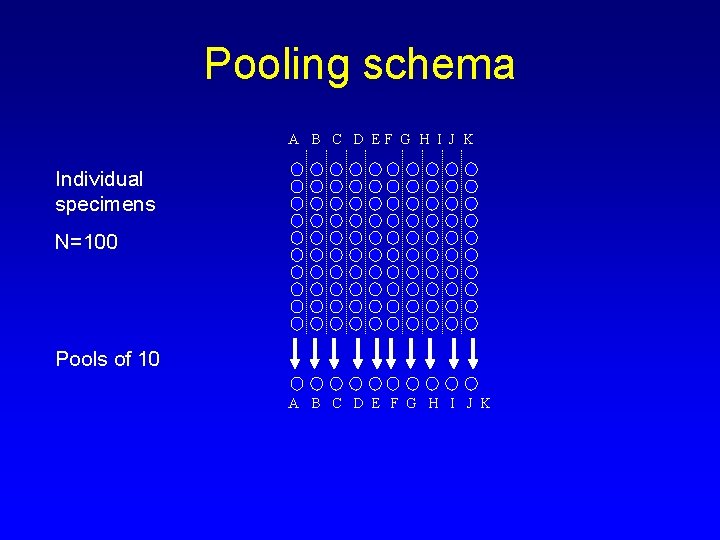
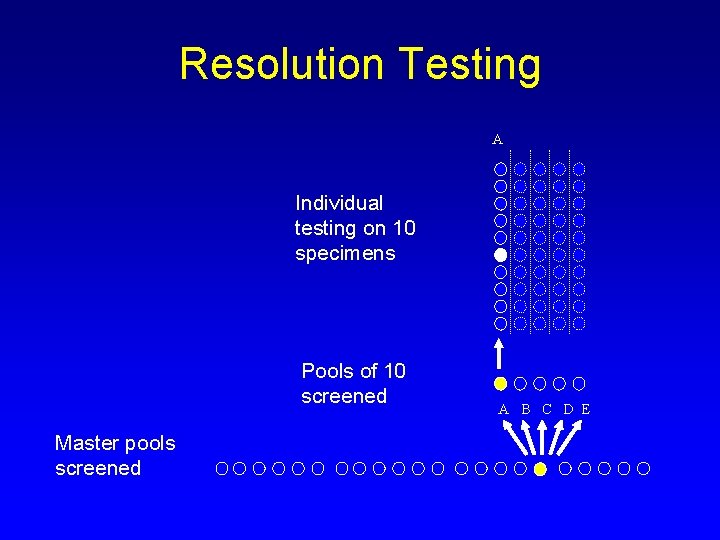
Pooling schema Individual specimens Pools of 10
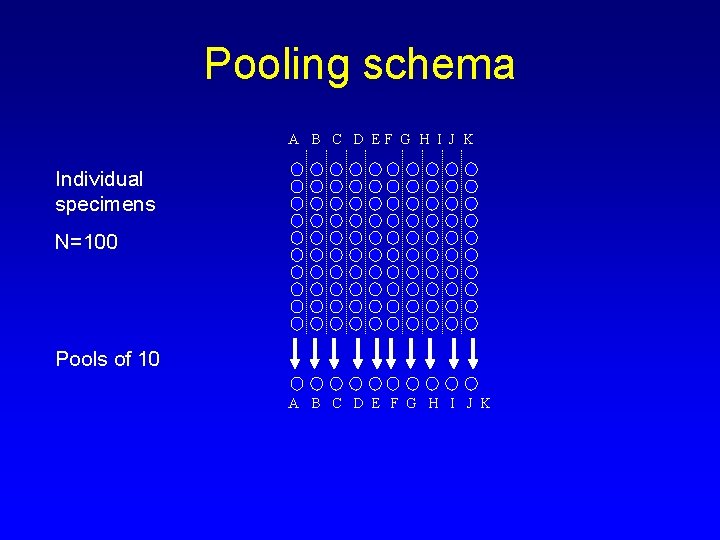
Pooling schema A B C D EF G H I J K Individual specimens N=100 Pools of 10 A B C D E F G H I J K
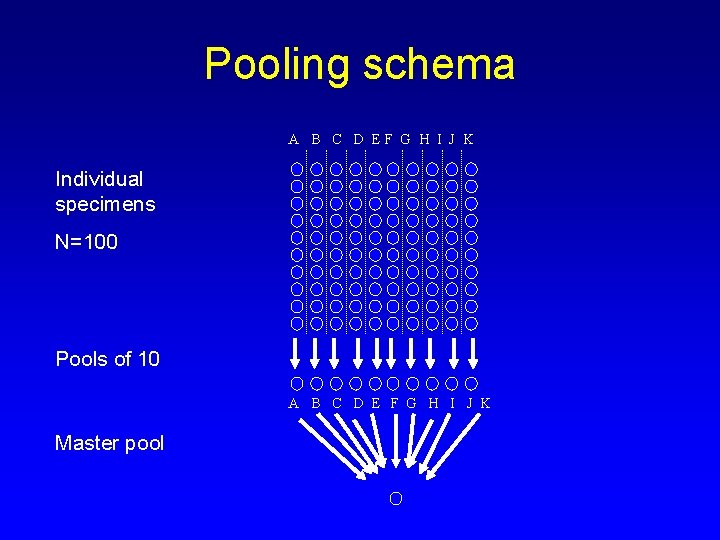
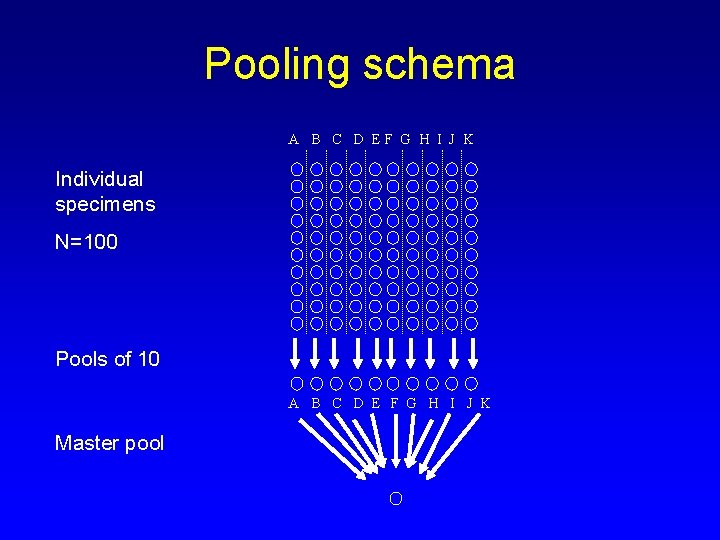
Pooling schema A B C D EF G H I J K Individual specimens N=100 Pools of 10 A B C D E F G H I J K Master pool
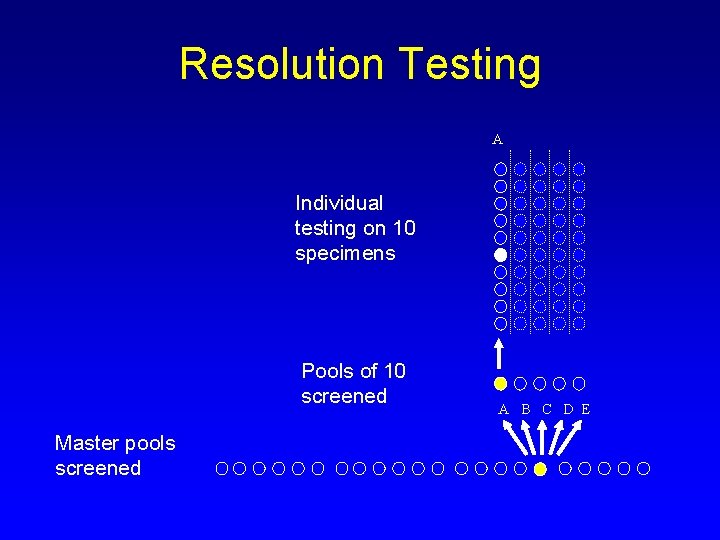
Resolution Testing A Individual testing on 10 specimens Pools of 10 screened Master pools screened A B C D E
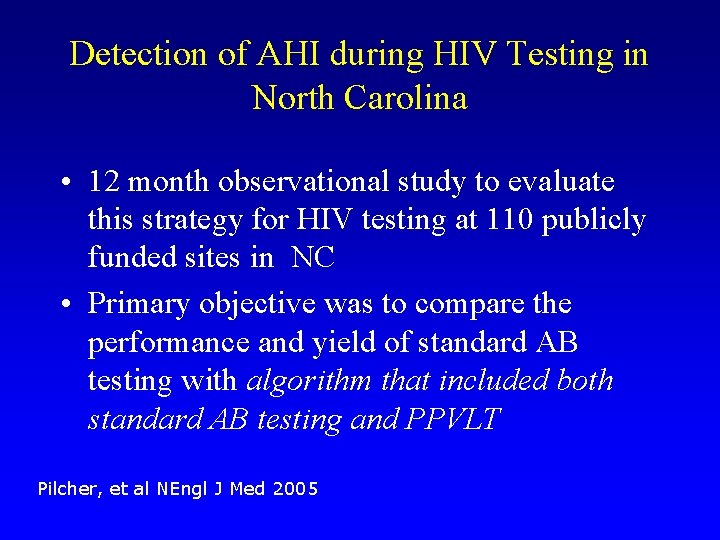
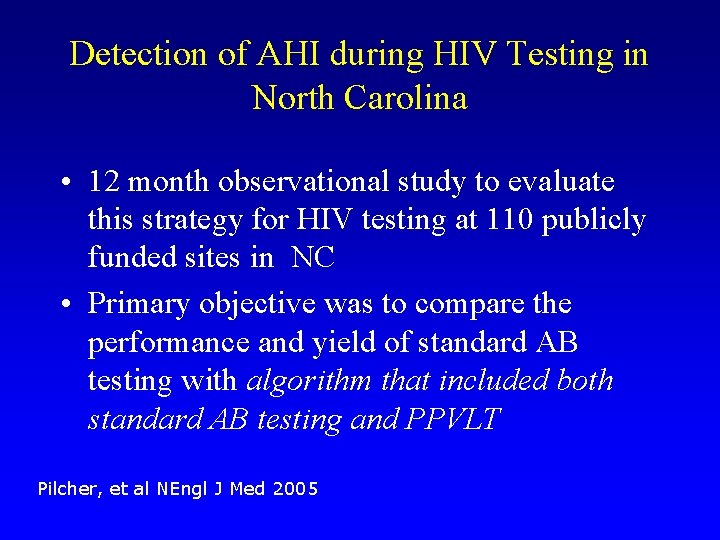
Detection of AHI during HIV Testing in North Carolina • 12 month observational study to evaluate this strategy for HIV testing at 110 publicly funded sites in NC • Primary objective was to compare the performance and yield of standard AB testing with algorithm that included both standard AB testing and PPVLT Pilcher, et al NEngl J Med 2005
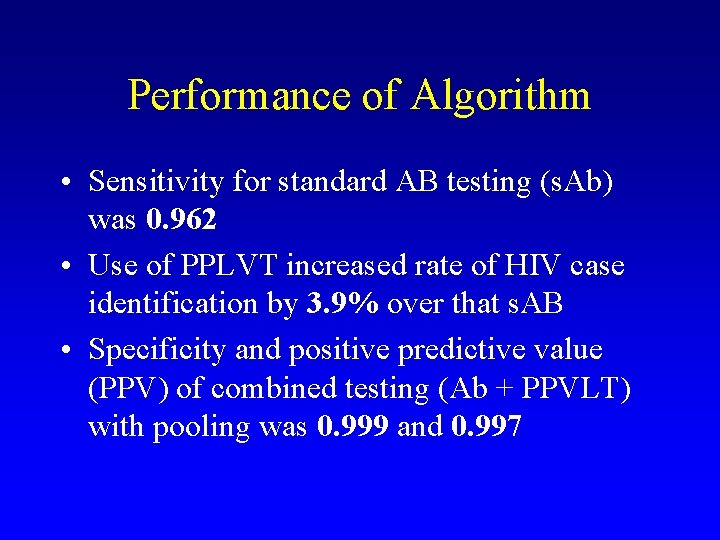
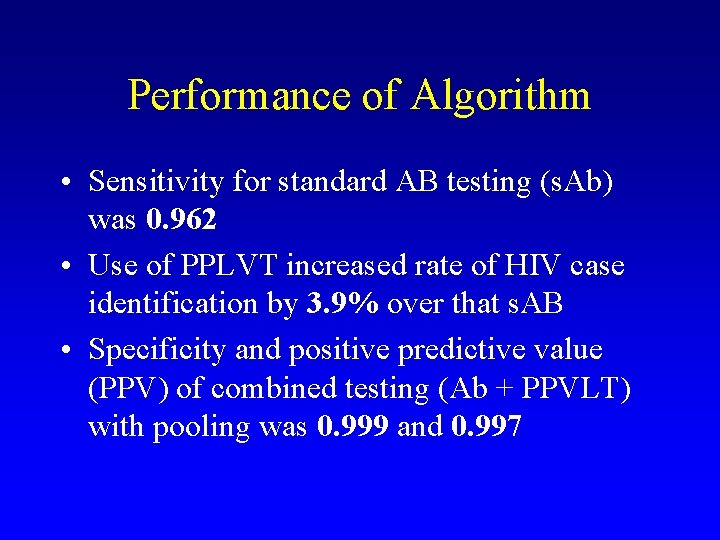
Performance of Algorithm • Sensitivity for standard AB testing (s. Ab) was 0. 962 • Use of PPLVT increased rate of HIV case identification by 3. 9% over that s. AB • Specificity and positive predictive value (PPV) of combined testing (Ab + PPVLT) with pooling was 0. 999 and 0. 997
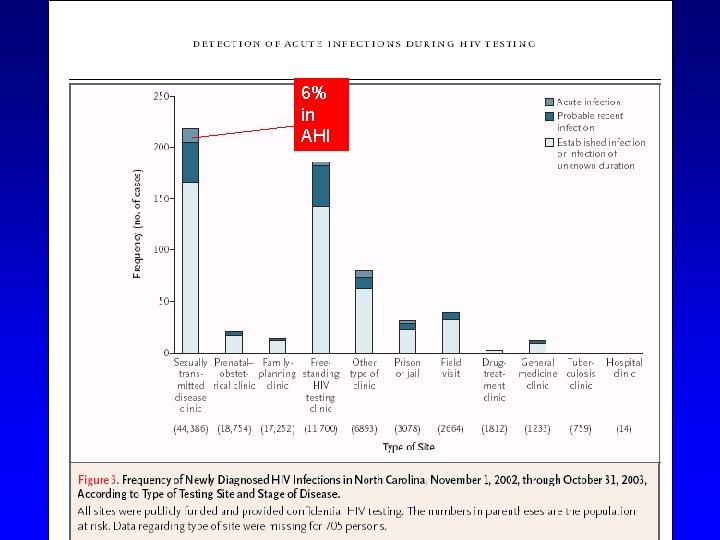
6% in AHI
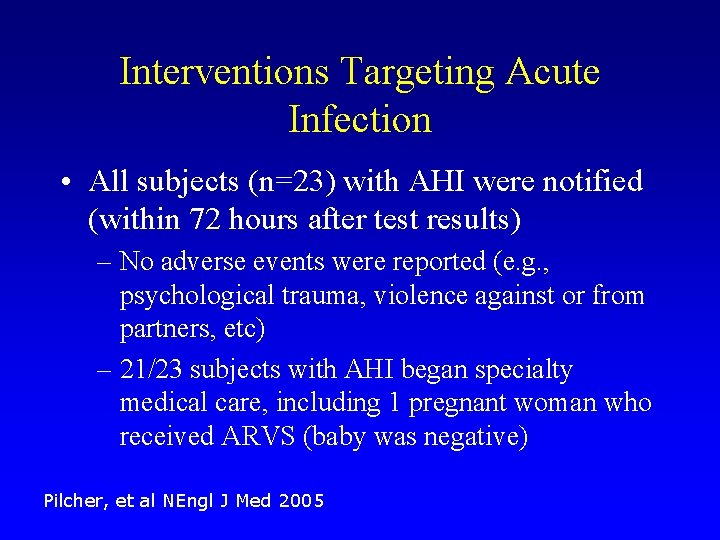
Interventions Targeting Acute Infection • All subjects (n=23) with AHI were notified (within 72 hours after test results) – No adverse events were reported (e. g. , psychological trauma, violence against or from partners, etc) – 21/23 subjects with AHI began specialty medical care, including 1 pregnant woman who received ARVS (baby was negative) Pilcher, et al NEngl J Med 2005

Interventions Targeting Acute Infection • 48 sexual partners of subjects with AHI received counseling for risk reduction – 18 of these (38%) had HIV infection • 13 (27%) previously recognized • 5 (10 %) newly diagnosed • 11 were probably the source of the AHI – 10 were aware of their status, but only 3 disclosed to partners – 3 of possible transmitters had been named in surveillance records as potential source of infection in 3 other cases suggesting roles as “core transmitters” Pilcher, et al NEngl J Med 2005
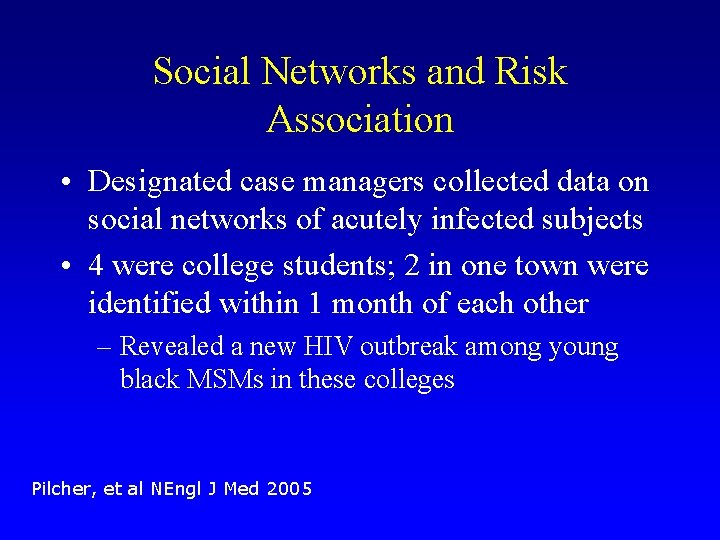
Social Networks and Risk Association • Designated case managers collected data on social networks of acutely infected subjects • 4 were college students; 2 in one town were identified within 1 month of each other – Revealed a new HIV outbreak among young black MSMs in these colleges Pilcher, et al NEngl J Med 2005
Costs • PPLVT added an additional $3. 63 per specimen and $17, 515 per additional index case identified • Added only 3. 3% increase over annual budget Pilcher, et al NEngl J Med 2005
Thanks • • Frederick Siegal, MD Barbara Johnston, MD Paul Galatowitsch, Ph. D All staff at the HIV Center
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Acute specific surgical infection
Acute specific surgical infection Broncheols
Broncheols Active phagocytes that increase rapidly acute infection
Active phagocytes that increase rapidly acute infection Alister stevens
Alister stevens Vnode unix
Vnode unix Boeing research and technology
Boeing research and technology Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Define infection prevention chapter 5
Define infection prevention chapter 5 Stakeholders in hiv prevention
Stakeholders in hiv prevention Global hiv prevention coalition
Global hiv prevention coalition Chapter 9 frontiers of biotechnology
Chapter 9 frontiers of biotechnology Richard walker frontiers
Richard walker frontiers Frontiers of biotechnology chapter 9
Frontiers of biotechnology chapter 9 Frontiers of biotechnology chapter 9
Frontiers of biotechnology chapter 9 Frontiers in chemical engineering
Frontiers in chemical engineering Frontiers
Frontiers Frontiers in bioscience impact factor
Frontiers in bioscience impact factor Weakening frontiers meaning
Weakening frontiers meaning Cop 4910
Cop 4910 Frontiers in bioinformatics
Frontiers in bioinformatics Frontiers
Frontiers Hfsp letter of intent
Hfsp letter of intent Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Typiska novell drag
Typiska novell drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Returpilarna
Returpilarna Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Tidböcker
Tidböcker Sura för anatom
Sura för anatom Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Att skriva en debattartikel
Att skriva en debattartikel Autokratiskt ledarskap
Autokratiskt ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Arkimedes princip formel
Arkimedes princip formel Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Kyssande vind
Kyssande vind Presentera för publik crossboss
Presentera för publik crossboss Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Bat mitza
Bat mitza Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter