Midnight Laundry Enuresis Encopresis and Diarrhea Tory Davis

- Slides: 35
Midnight Laundry Enuresis, Encopresis and Diarrhea Tory Davis, PA-C
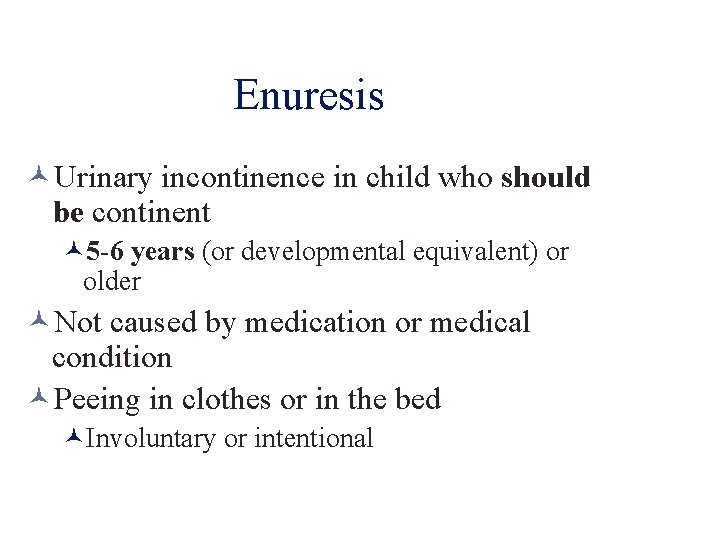
Enuresis Urinary incontinence in child who should be continent 5 -6 years (or developmental equivalent) or older Not caused by medication or medical condition Peeing in clothes or in the bed Involuntary or intentional
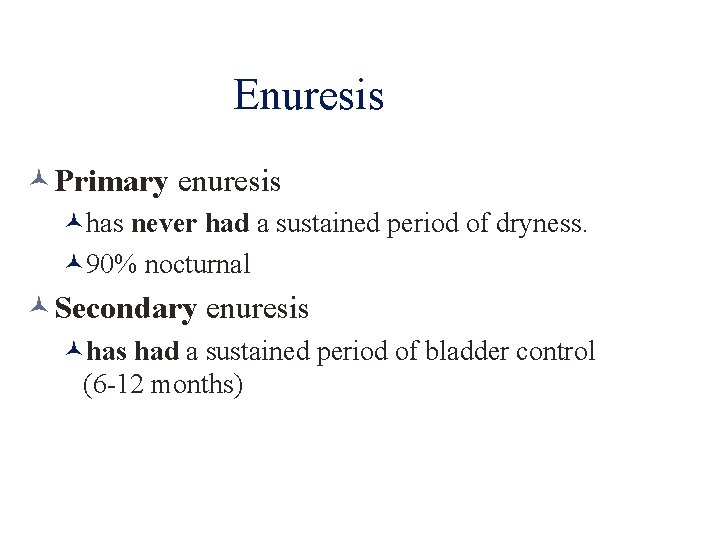
Enuresis Primary enuresis has never had a sustained period of dryness. 90% nocturnal Secondary enuresis had a sustained period of bladder control (6 -12 months)
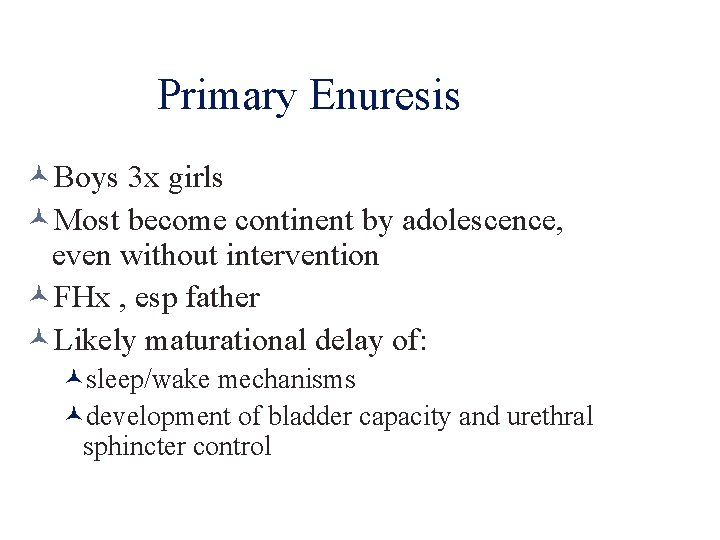
Primary Enuresis Boys 3 x girls Most become continent by adolescence, even without intervention FHx , esp father Likely maturational delay of: sleep/wake mechanisms development of bladder capacity and urethral sphincter control
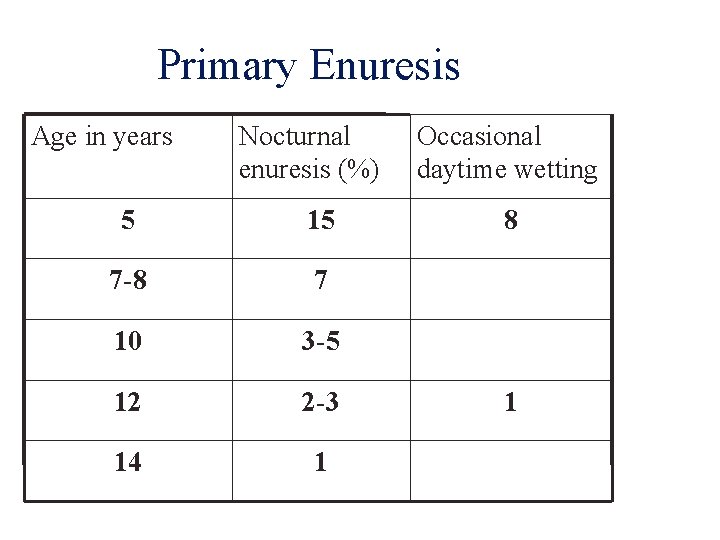
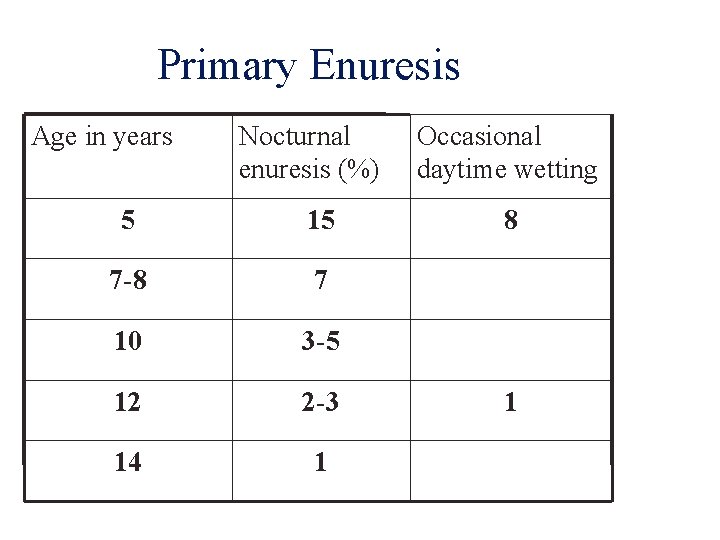
Primary Enuresis Age in years Nocturnal enuresis (%) 5 15 7 -8 7 10 3 -5 12 2 -3 14 1 Occasional daytime wetting 8 1
Daytime Enuresis More common in : Kids with hyperactivity Timid/shy kids Boys = Girls 60 -80% also have nocturnal wetting
Secondary Enuresis Onset after child has had sustained period of continence Often follows a stressful event Loss, new sibling, family discord, move, new school, abuse
Differential UTI *MC Distal urethritis (bubble bath) Neurological disorders- congenital or acquired Congenital anomalies (spina bifida) Seizure disorders Diabetes (mellitus or insipidus) Structural abnormalities of the urinary tract (urethral cyst, urethral duplication, obstruction)
Diagnosis Take a good history Do a good physical Observe child’s urinary stream Straining, dribbling, stress incontinence? Urinalysis and urine culture
Treatment Emphasize that noc wetting is likely developmental lag NOT acting out, etc Patient understanding and encouragement Spontaneous cure ~15%/year Avoidance of punitive measures Encourage child participation
Treatment Counseling Child has active role: keeps calendar, helps with the midnight laundry, talk to the PA Positive reinforcement, remove guilt/blame Bladder training Hold urine longer during day, limit fluids after dinner, practice start/stop urine flow on toilet, pee just before bed. Helpful ~40% Potty pager/ alarm
Meds DDAVP (desmopressin acetate) intranasal qhs. Complete remission during tx 50%, high relapse on discontinuation. Good for special events (camp, sleepovers) and as “bridge” Imipramine (TCA) 25 -50 qhs Anticholinergic side effects
Encopresis Fecal incontinence in child who should be continent. 4 years (or developmental equivalent) or older Not due to medication or medical condition Involuntary (usually) or intentional 1 -1. 5% of school-aged kiddos, very rare in adolescence Boys 4 x girls
Functional Encopresis Types Retentive Continuous Discontinuous Toilet phobia
Retentive Encopresis *MC Psychogenic Megacolon Child withholds BMs constipation fecal impaction seepage of liquid feces (Type 7!) around impaction and out onto skivvies. Marked constipation Painful defecation Retention reduced sensory feedback Rectal wall stretch causes contractile strength Harder stools due to increased water absorption Then what happens…?
Continuous Encopresis Children who have never gained primary control of bowel function. Poop in underwear. Doesn’t care. No regard for social norms. Typically lacks bowel/potty training Often family social/intellectual disadvantage The encopresis is the least of your worries with this child
Discontinuous Encopresis Hx of normal bowel control for extended period Like secondary enuresis, usually in response to stressful event Sometimes voluntary follow-through (smearing, etc)
Etiologic considerations Inefficient motility Medical management for (perceived? ) bowel disorder Painful defecation (fissures, etc) Surgical hx (imperforate anus) Unrealistic parental expectation
Consequences Fear Shame Isolation Depression
History Bowel pattern since birth Age of onset of problems/symptoms Management attempt and effects Associations (ie with stressors)
Physical Exam
Management (Levine) Counseling Phase Demystify: Review colon function Normal and abnormal Draw a picture Show imaging Remove blame Explain treatment plan Emphasize intestinal muscle building
Inpatient Catharsis When? Severe retention Poor outlook for home compliance What? Saline enemas bid 3 -7 days Bisacodyl suppositories bid 3 -7 days Sit on toilet 15 min pc
Outpatient Catharsis Mild: Senna daily x 1 -2 weeks Moderate-Severe: 3 day cycles Day 1: Fleet’s enema bid Day 2: Bisacodyl suppository BID Day 3: Bisacodyl suppository once Follow-up x-ray to confirm catharsis
Maintenance Sit on toilet bid x 10 min, after meals 2 T mineral oil po bid x 4 -6 months MVI supplement Eat fiber! Oral laxative (senna) q day or qod x 1 month Read Anna Karinina ? ? Reward- sticker chart, etc
Follow-Up q 1 -2 months Check compliance Monitor for relapse Document progress
Thoughts on Potty Teaching Teach your parents well… Readiness signals: dry periods, interest in toilet, wants to be changed when wet, can follow directions No power struggles Respect child’s autonomy Applaud child’s success Accidents happen

Poop Song http: //www. youtube. com/watch? v=POIg. Xyvz. UU&feature=rec-rn
Acute Diarrhea Gastroenteritis Infectious Food poisoning Antibiotic-associated Overfeeding Great Ddx chart in Nelson text
Acute diarrhea Complete history Include day care, travel, animal contact, foods, antibiotics Physical Exam Stool- check for WBCs and occult blood If neg, think viral If pos- r/o (or in) bacterial cause, then consider IBD
Acute diarrhea management Cure initiating event Correct dehydration and e-lyte deficits Manage complications from mucosal injury NO Imodium, Lomotil, paragoric, etc
Chronic Diarrhea Post-infectious secondary lactase deficiency Cow’s milk intolerance Toddler’s diarrhea Celiac disease CF IBS IBD Giardiasis Laxative abuse AIDS enteropathy
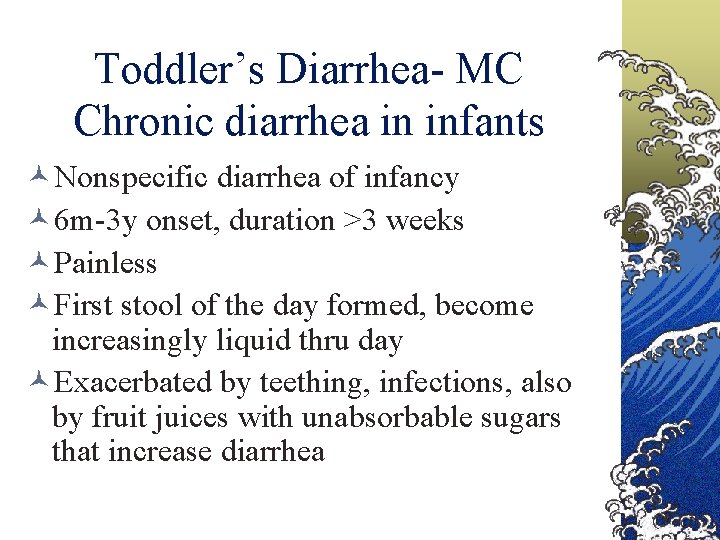
Toddler’s Diarrhea- MC Chronic diarrhea in infants Nonspecific diarrhea of infancy 6 m-3 y onset, duration >3 weeks Painless First stool of the day formed, become increasingly liquid thru day Exacerbated by teething, infections, also by fruit juices with unabsorbable sugars that increase diarrhea
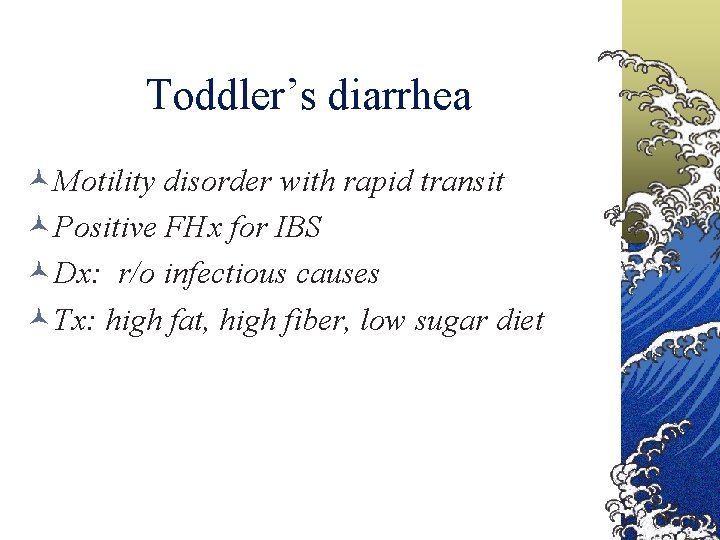
Toddler’s diarrhea Motility disorder with rapid transit Positive FHx for IBS Dx: r/o infectious causes Tx: high fat, high fiber, low sugar diet
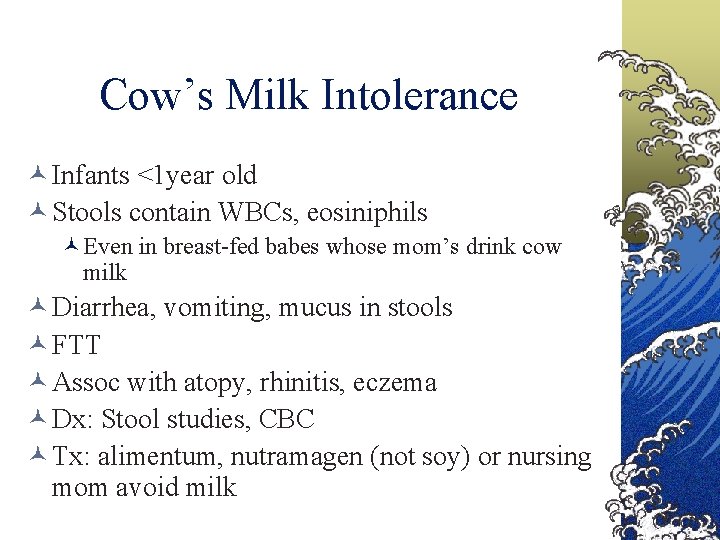
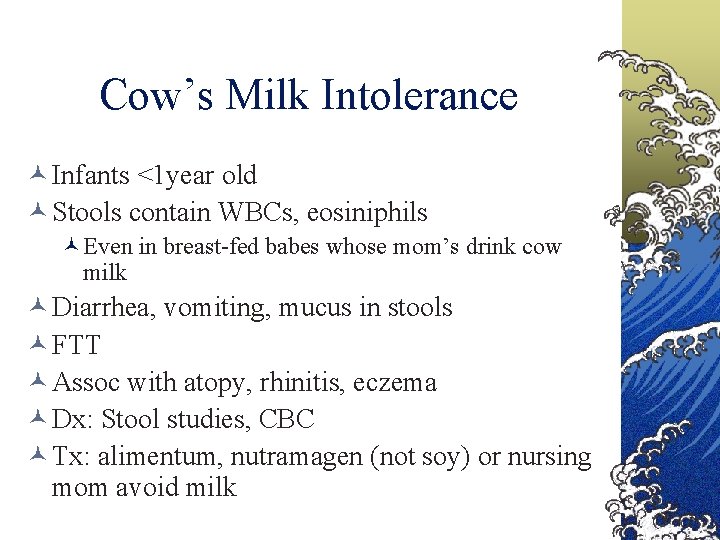
Cow’s Milk Intolerance Infants <1 year old Stools contain WBCs, eosiniphils Even in breast-fed babes whose mom’s drink cow milk Diarrhea, vomiting, mucus in stools FTT Assoc with atopy, rhinitis, eczema Dx: Stool studies, CBC Tx: alimentum, nutramagen (not soy) or nursing mom avoid milk
 Enuresis and encopresis
Enuresis and encopresis Constipation
Constipation Sindrome de gotard
Sindrome de gotard Encopresis diurna
Encopresis diurna The harp by harris burdick
The harp by harris burdick Archie smith boy wonder picture
Archie smith boy wonder picture Uninvited guests harris burdick
Uninvited guests harris burdick Tory reding
Tory reding Linie wężowe przechodzące przez tory należy układać:
Linie wężowe przechodzące przez tory należy układać: They call me a brainless tory
They call me a brainless tory Hyperechogén
Hyperechogén Guest laundry docket
Guest laundry docket Personification example
Personification example Thank you o my father
Thank you o my father Nicholas seeliger, md flpen 32413
Nicholas seeliger, md flpen 32413 Secretory diarrhea pathophysiology
Secretory diarrhea pathophysiology Foot crunchies map
Foot crunchies map Radwan
Radwan Bile acid diarrhea
Bile acid diarrhea Diarhea types
Diarhea types Severe dehydration
Severe dehydration Ddsep 9 free download
Ddsep 9 free download Vpims lucknow
Vpims lucknow Osmotic diarrhea meaning
Osmotic diarrhea meaning Chronic diarrhea
Chronic diarrhea Pig diarrhea chart
Pig diarrhea chart Overflow diarrhea pictures
Overflow diarrhea pictures Diarrhea
Diarrhea Bile acid diarrhea
Bile acid diarrhea Imnci diarrhea management
Imnci diarrhea management Hiv stool color
Hiv stool color Diarrhea chief complaint
Diarrhea chief complaint Chronic diarrhea
Chronic diarrhea Leishmania donovani transmission
Leishmania donovani transmission Diarrhea
Diarrhea Travelers diarrhea
Travelers diarrhea