MANAGING PRIMARY HEADACHES AN OVERVIEW FAYYAZ AHMED HULL


- Slides: 49
MANAGING PRIMARY HEADACHES AN OVERVIEW FAYYAZ AHMED HULL & EAST YORKSHIRE HOSPITALS NHS TRUST
LEARNING OUTCOME The Current management strategy for common primary headache disorders n Appraisal of currently available treatments n New treatments on the horizon n
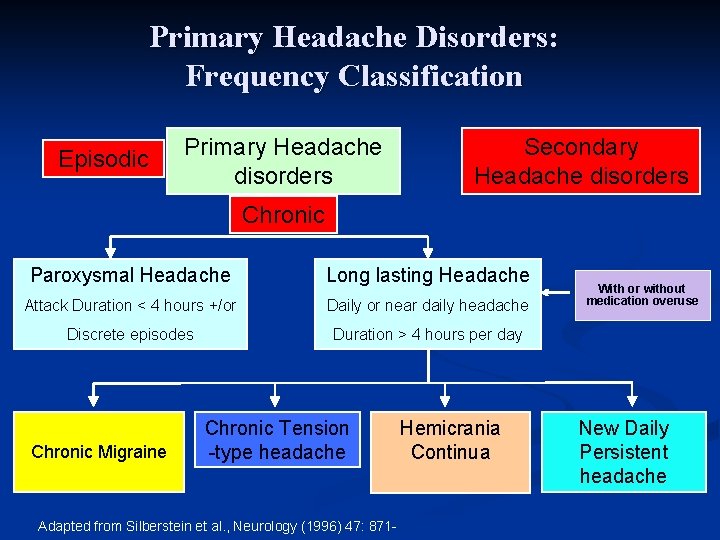
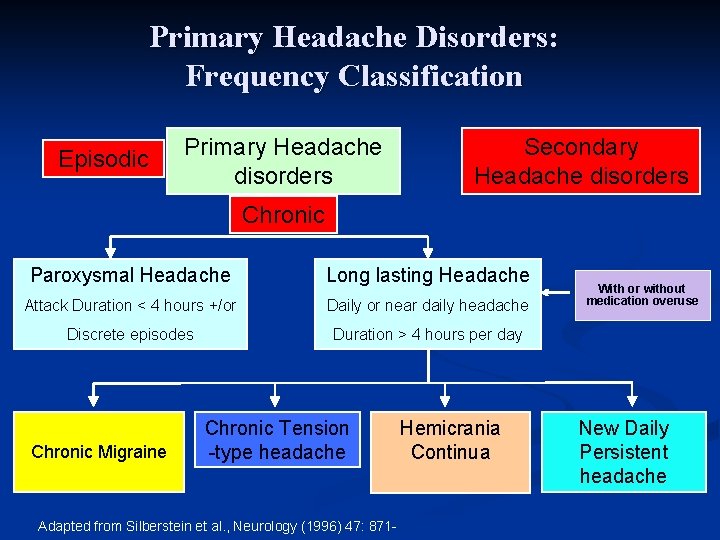
Primary Headache Disorders: Frequency Classification Episodic Primary Headache disorders Secondary Headache disorders Chronic Paroxysmal Headache Long lasting Headache Attack Duration < 4 hours +/or Daily or near daily headache Discrete episodes Duration > 4 hours per day Chronic Migraine Chronic Tension -type headache Adapted from Silberstein et al. , Neurology (1996) 47: 871 - Hemicrania Continua With or without medication overuse New Daily Persistent headache
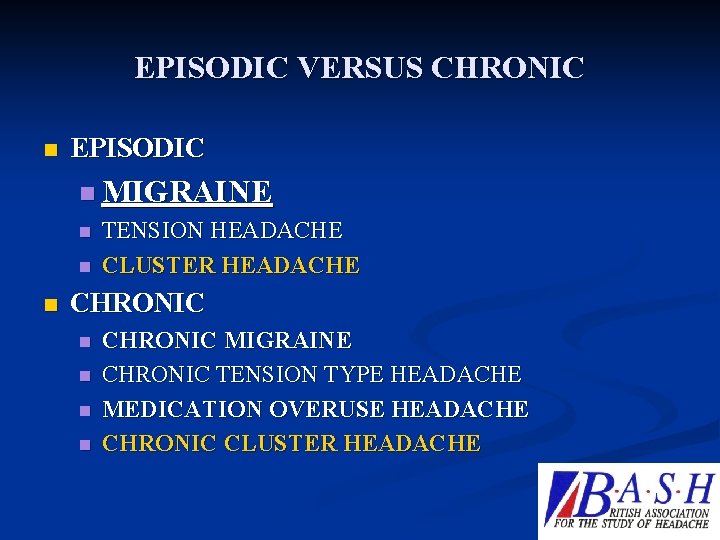
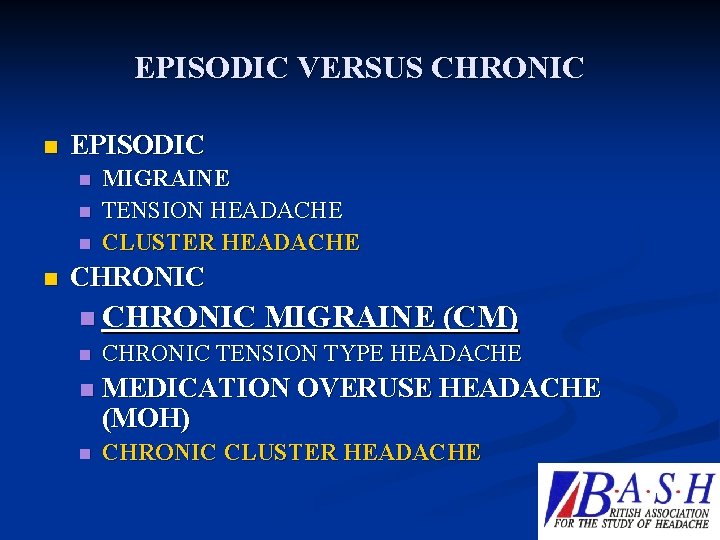
EPISODIC VERSUS CHRONIC n EPISODIC n MIGRAINE n n n TENSION HEADACHE CLUSTER HEADACHE CHRONIC n n CHRONIC MIGRAINE CHRONIC TENSION TYPE HEADACHE MEDICATION OVERUSE HEADACHE CHRONIC CLUSTER HEADACHE

11/9/2020
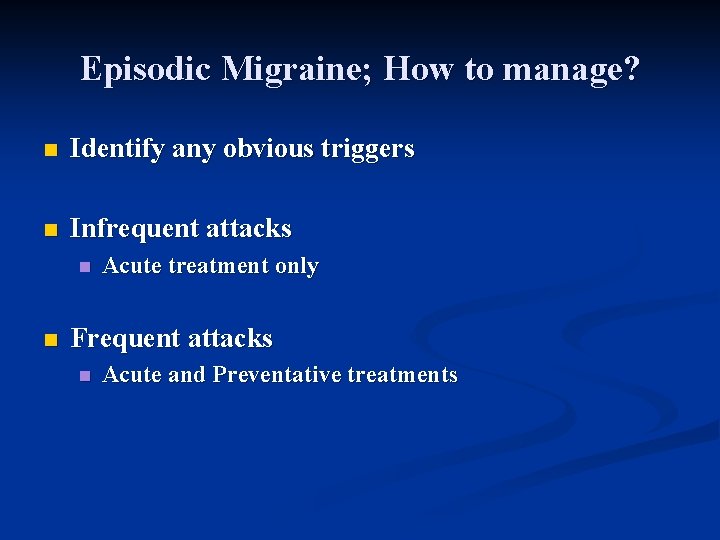
Episodic Migraine; How to manage? n Identify any obvious triggers n Infrequent attacks n n Acute treatment only Frequent attacks n Acute and Preventative treatments
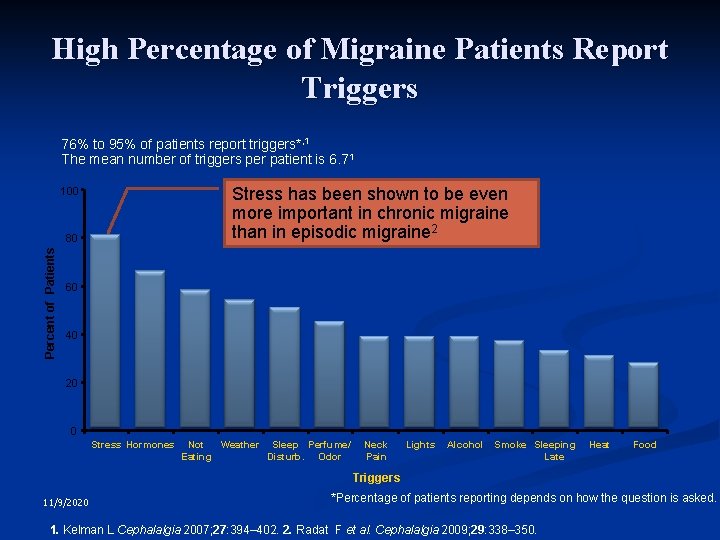
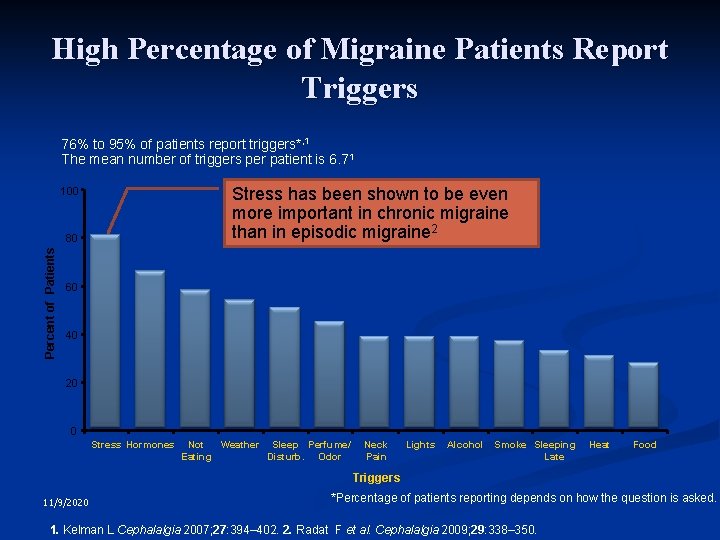
High Percentage of Migraine Patients Report Triggers 76% to 95% of patients report triggers*, 1 The mean number of triggers per patient is 6. 71 Stress has been shown to be even more important in chronic migraine than in episodic migraine 2 100 Percent of Patients 80 60 40 20 0 Stress Hormones Not Weather Sleep Perfume/ Eating Disturb. Odor Neck Pain Lights Alcohol Smoke Sleeping Late Heat Food Triggers 11/9/2020 *Percentage of patients reporting depends on how the question is asked. 1. Kelman L Cephalalgia 2007; 27: 394– 402. 2. Radat F et al. Cephalalgia 2009; 29: 338– 350. 7
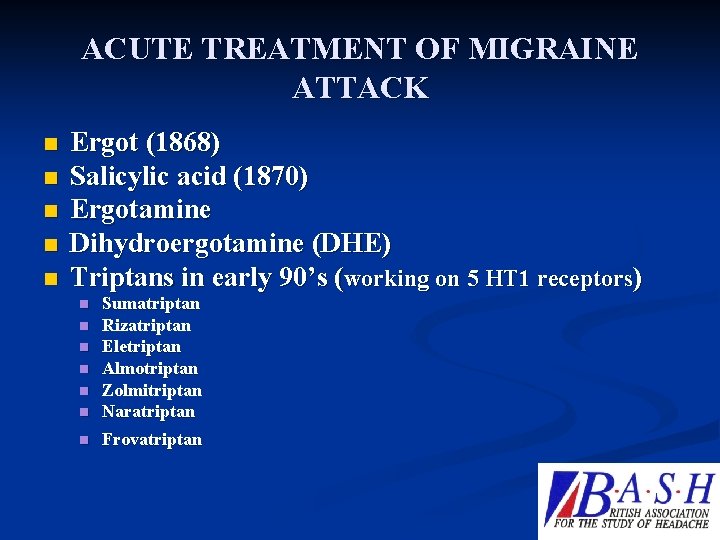
ACUTE TREATMENT OF MIGRAINE ATTACK n n n Ergot (1868) Salicylic acid (1870) Ergotamine Dihydroergotamine (DHE) Triptans in early 90’s (working on 5 HT 1 receptors) n Sumatriptan Rizatriptan Eletriptan Almotriptan Zolmitriptan Naratriptan n Frovatriptan n n
Migraine; How to manage? n Standard abortive therapy 11/9/2020 9
Acute Rx: Key Message Avoid opiates or combination analgesics with barbiturates, caffeine n Restrict the use to no more than two days/doses per week n NSAID has the lowest potential for medication overuse n
New Rx on the Horizon CGRP antagonists or Gepants n Glutamate Receptor Antagonists n Vanilloid (TRPV 1) receptor antagonists n Nitric Oxide Synthetase inhibitors n Prostanoid Receptor Antagonist n
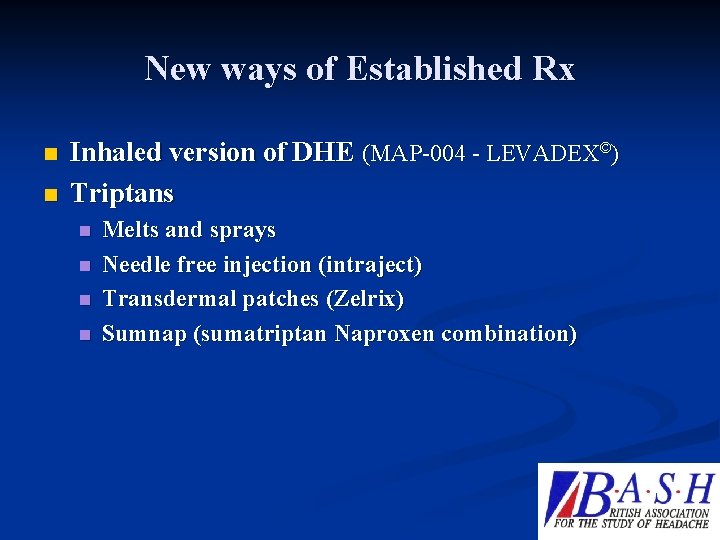
New ways of Established Rx n n Inhaled version of DHE (MAP-004 - LEVADEX©) Triptans n n Melts and sprays Needle free injection (intraject) Transdermal patches (Zelrix) Sumnap (sumatriptan Naproxen combination)
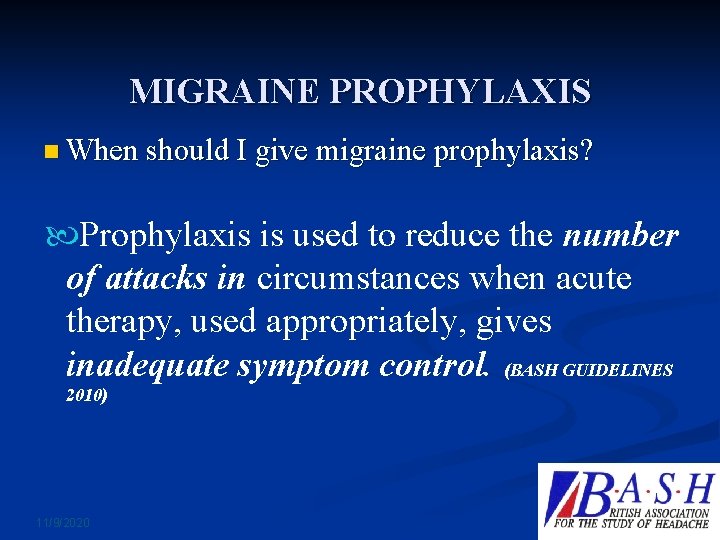
MIGRAINE PROPHYLAXIS n When should I give migraine prophylaxis? Prophylaxis is used to reduce the number of attacks in circumstances when acute therapy, used appropriately, gives inadequate symptom control. (BASH GUIDELINES 2010) 11/9/2020 13
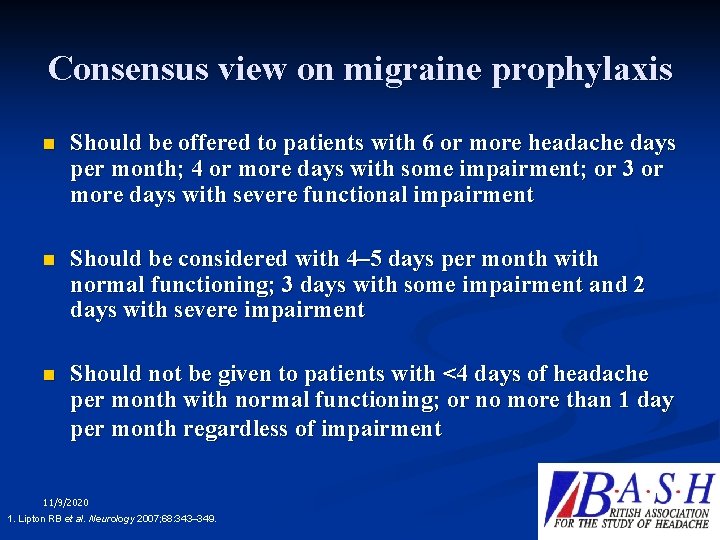
Consensus view on migraine prophylaxis n Should be offered to patients with 6 or more headache days per month; 4 or more days with some impairment; or 3 or more days with severe functional impairment n Should be considered with 4– 5 days per month with normal functioning; 3 days with some impairment and 2 days with severe impairment n Should not be given to patients with <4 days of headache per month with normal functioning; or no more than 1 day per month regardless of impairment 11/9/2020 1. Lipton RB et al. Neurology 2007; 68: 343– 349. 14
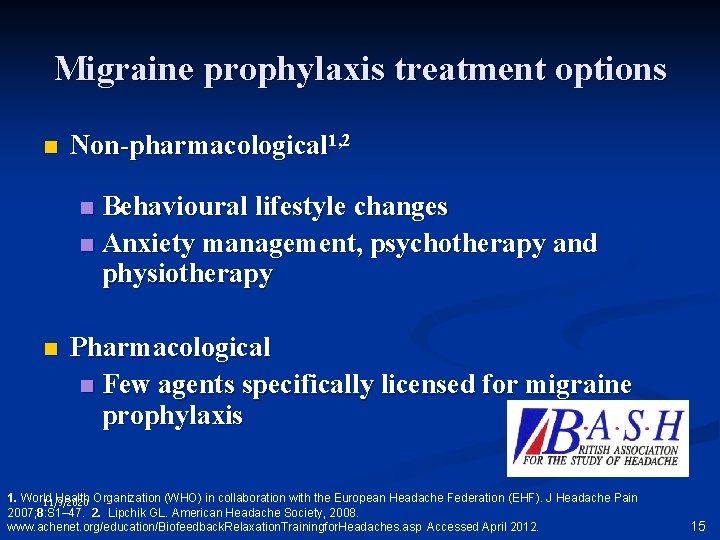
Migraine prophylaxis treatment options n Non-pharmacological 1, 2 Behavioural lifestyle changes n Anxiety management, psychotherapy and physiotherapy n n Pharmacological n Few agents specifically licensed for migraine prophylaxis 1. World Health Organization (WHO) in collaboration with the European Headache Federation (EHF). J Headache Pain 11/9/2020 2007; 8: S 1– 47. 2. Lipchik GL. American Headache Society, 2008. www. achenet. org/education/Biofeedback. Relaxation. Trainingfor. Headaches. asp Accessed April 2012. 15
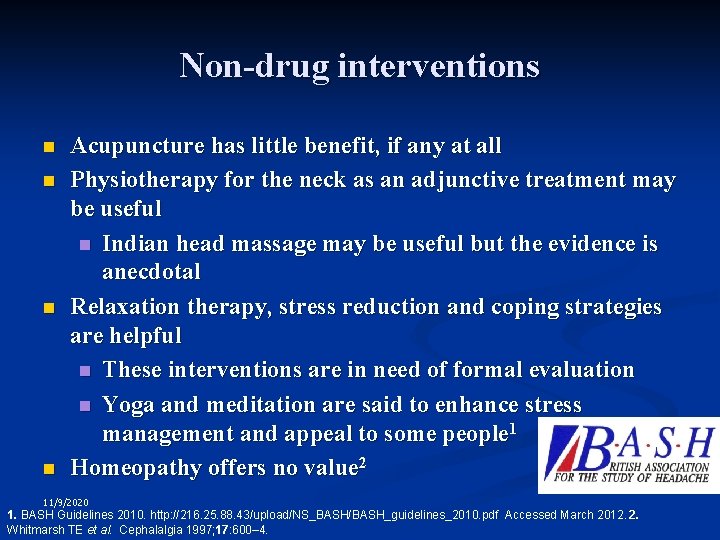
Non-drug interventions n n Acupuncture has little benefit, if any at all Physiotherapy for the neck as an adjunctive treatment may be useful n Indian head massage may be useful but the evidence is anecdotal Relaxation therapy, stress reduction and coping strategies are helpful n These interventions are in need of formal evaluation n Yoga and meditation are said to enhance stress management and appeal to some people 1 Homeopathy offers no value 2 11/9/2020 1. BASH Guidelines 2010. http: //216. 25. 88. 43/upload/NS_BASH/BASH_guidelines_2010. pdf Accessed March 2012. 2. Whitmarsh TE et al. Cephalalgia 1997; 17: 600– 4. 16
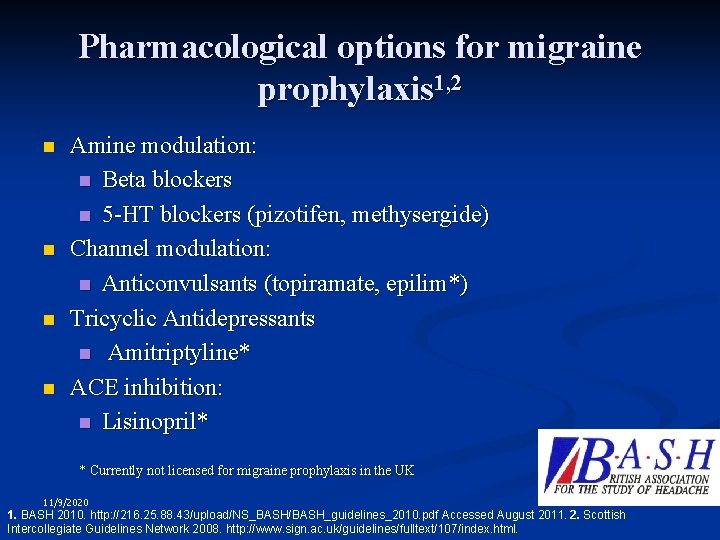
Pharmacological options for migraine prophylaxis 1, 2 n n Amine modulation: n Beta blockers n 5 -HT blockers (pizotifen, methysergide) Channel modulation: n Anticonvulsants (topiramate, epilim*) Tricyclic Antidepressants n Amitriptyline* ACE inhibition: n Lisinopril* * Currently not licensed for migraine prophylaxis in the UK 11/9/2020 1. BASH 2010. http: //216. 25. 88. 43/upload/NS_BASH/BASH_guidelines_2010. pdf Accessed August 2011. 2. Scottish Intercollegiate Guidelines Network 2008. http: //www. sign. ac. uk/guidelines/fulltext/107/index. html. 17
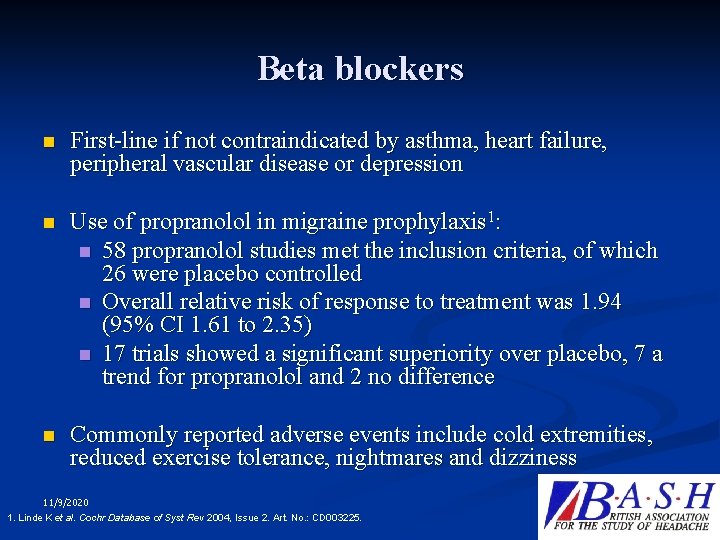
Beta blockers n First-line if not contraindicated by asthma, heart failure, peripheral vascular disease or depression n Use of propranolol in migraine prophylaxis 1: n 58 propranolol studies met the inclusion criteria, of which 26 were placebo controlled n Overall relative risk of response to treatment was 1. 94 (95% CI 1. 61 to 2. 35) n 17 trials showed a significant superiority over placebo, 7 a trend for propranolol and 2 no difference n Commonly reported adverse events include cold extremities, reduced exercise tolerance, nightmares and dizziness 11/9/2020 1. Linde K et al. Cochr Database of Syst Rev 2004, Issue 2. Art. No. : CD 003225. 18
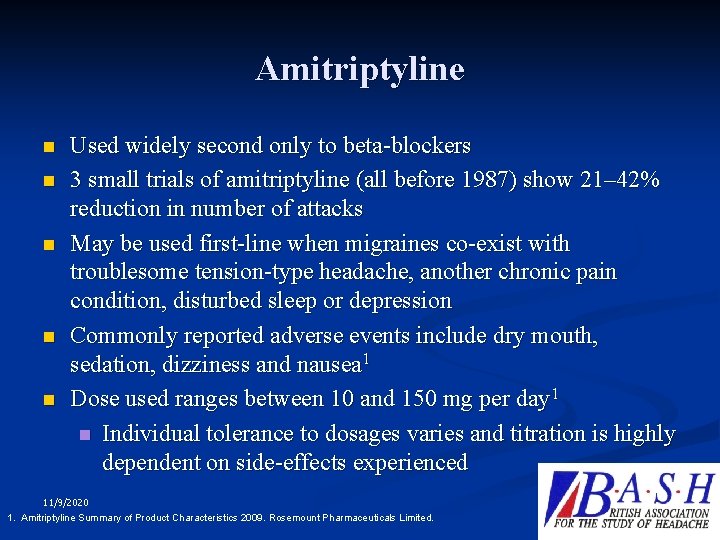
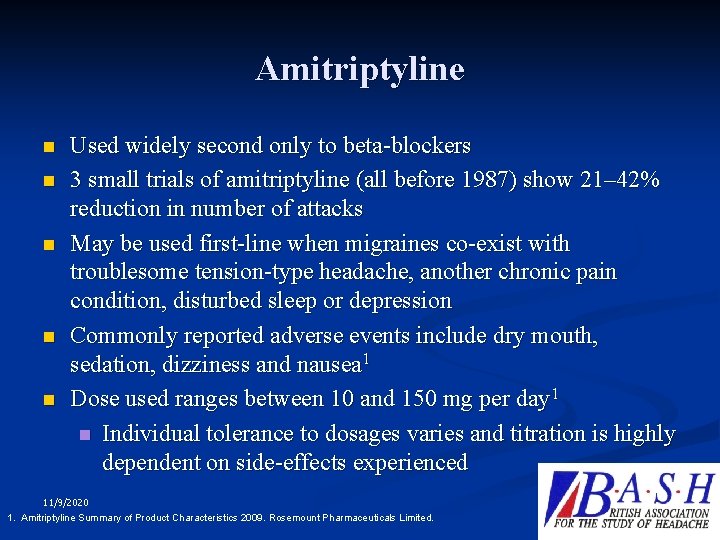
Amitriptyline n n n Used widely second only to beta-blockers 3 small trials of amitriptyline (all before 1987) show 21– 42% reduction in number of attacks May be used first-line when migraines co-exist with troublesome tension-type headache, another chronic pain condition, disturbed sleep or depression Commonly reported adverse events include dry mouth, sedation, dizziness and nausea 1 Dose used ranges between 10 and 150 mg per day 1 n Individual tolerance to dosages varies and titration is highly dependent on side-effects experienced 11/9/2020 1. Amitriptyline Summary of Product Characteristics 2009. Rosemount Pharmaceuticals Limited. 19
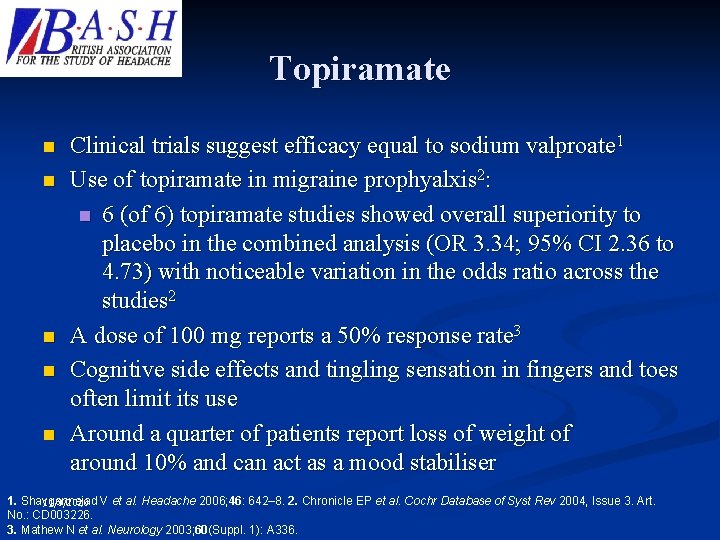
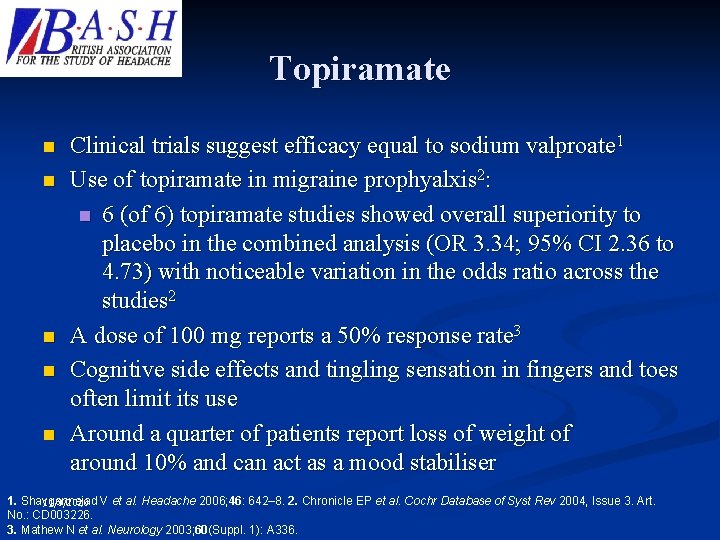
Topiramate n n n Clinical trials suggest efficacy equal to sodium valproate 1 Use of topiramate in migraine prophyalxis 2: n 6 (of 6) topiramate studies showed overall superiority to placebo in the combined analysis (OR 3. 34; 95% CI 2. 36 to 4. 73) with noticeable variation in the odds ratio across the studies 2 A dose of 100 mg reports a 50% response rate 3 Cognitive side effects and tingling sensation in fingers and toes often limit its use Around a quarter of patients report loss of weight of around 10% and can act as a mood stabiliser 1. Shaygannejad V et al. Headache 2006; 46: 642– 8. 2. Chronicle EP et al. Cochr Database of Syst Rev 2004, Issue 3. Art. 11/9/2020 No. : CD 003226. 3. Mathew N et al. Neurology 2003; 60(Suppl. 1): A 336. 20
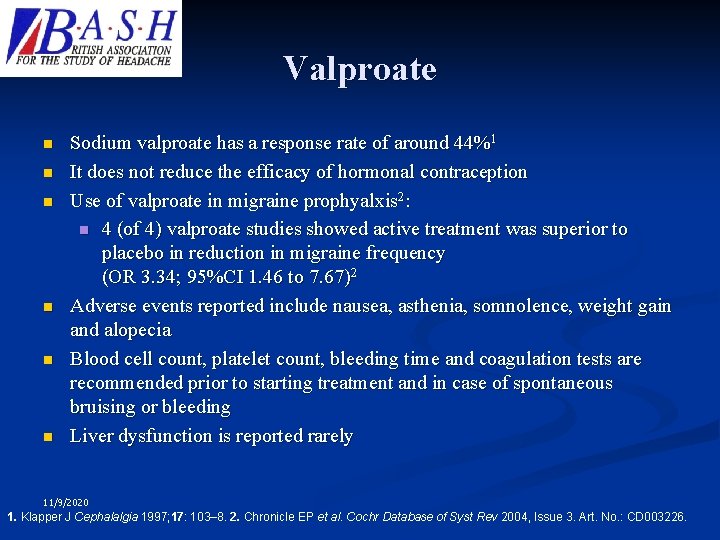
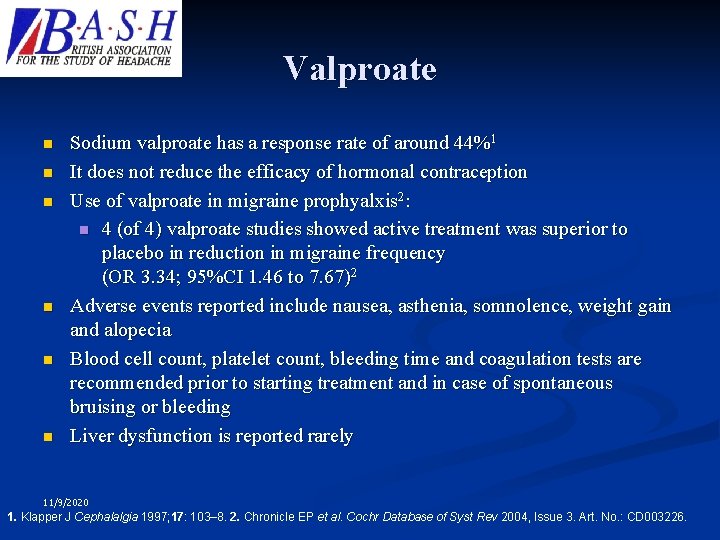
Valproate n n n Sodium valproate has a response rate of around 44%1 It does not reduce the efficacy of hormonal contraception Use of valproate in migraine prophyalxis 2: n 4 (of 4) valproate studies showed active treatment was superior to placebo in reduction in migraine frequency (OR 3. 34; 95%CI 1. 46 to 7. 67)2 Adverse events reported include nausea, asthenia, somnolence, weight gain and alopecia Blood cell count, platelet count, bleeding time and coagulation tests are recommended prior to starting treatment and in case of spontaneous bruising or bleeding Liver dysfunction is reported rarely 11/9/2020 1. Klapper J Cephalalgia 1997; 17: 103– 8. 2. Chronicle EP et al. Cochr Database of Syst Rev 2004, Issue 3. Art. No. : CD 003226. 21
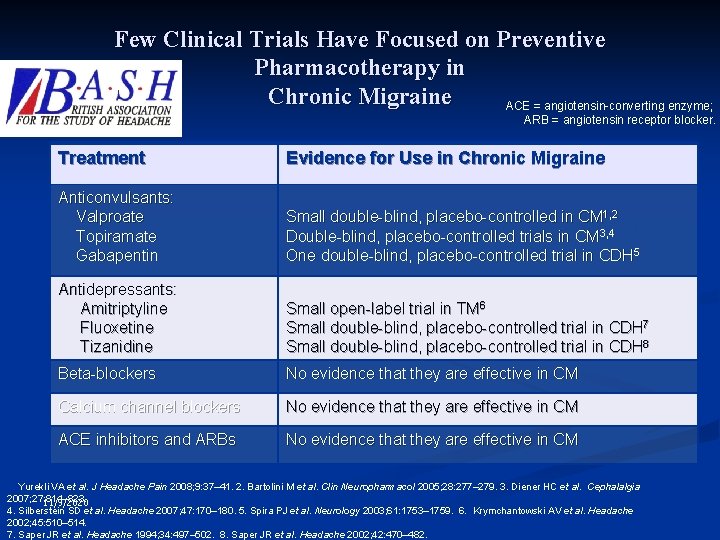
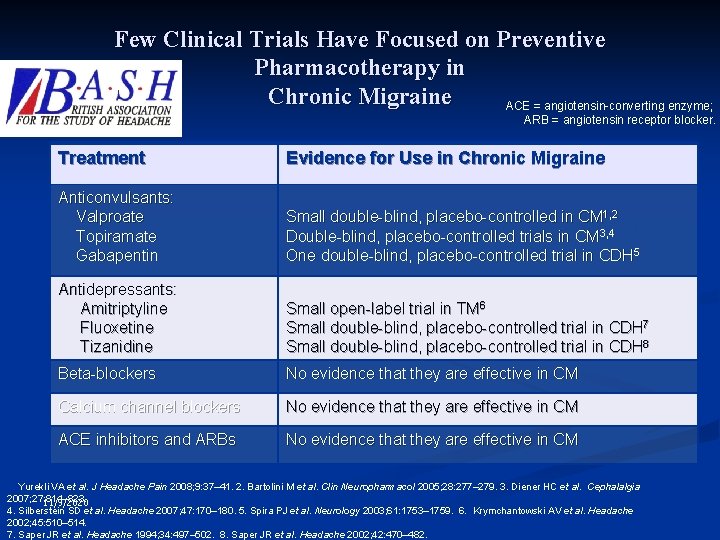
Few Clinical Trials Have Focused on Preventive Pharmacotherapy in Chronic Migraine ACE = angiotensin-converting enzyme; ARB = angiotensin receptor blocker. Treatment Evidence for Use in Chronic Migraine Anticonvulsants: Valproate Topiramate Gabapentin Small double-blind, placebo-controlled in CM 1, 2 Double-blind, placebo-controlled trials in CM 3, 4 One double-blind, placebo-controlled trial in CDH 5 Antidepressants: Amitriptyline Fluoxetine Tizanidine Small open-label trial in TM 6 Small double-blind, placebo-controlled trial in CDH 7 Small double-blind, placebo-controlled trial in CDH 8 Beta-blockers No evidence that they are effective in CM Calcium channel blockers No evidence that they are effective in CM ACE inhibitors and ARBs No evidence that they are effective in CM 1. Yurekli VA et al. J Headache Pain 2008; 9: 37– 41. 2. Bartolini M et al. Clin Neuropharmacol 2005; 28: 277– 279. 3. Diener HC et al. Cephalalgia 2007; 27: 814– 823. 11/9/2020 4. Silberstein SD et al. Headache 2007; 47: 170– 180. 5. Spira PJ et al. Neurology 2003; 61: 1753– 1759. 6. Krymchantowski AV et al. Headache 2002; 45: 510– 514. 7. Saper JR et al. Headache 1994; 34: 497– 502. 8. Saper JR et al. Headache 2002; 42: 470– 482. 22
EPISODIC VERSUS CHRONIC n EPISODIC n n MIGRAINE TENSION HEADACHE CLUSTER HEADACHE CHRONIC n CHRONIC MIGRAINE (CM) n CHRONIC TENSION TYPE HEADACHE n MEDICATION OVERUSE HEADACHE (MOH) n CHRONIC CLUSTER HEADACHE
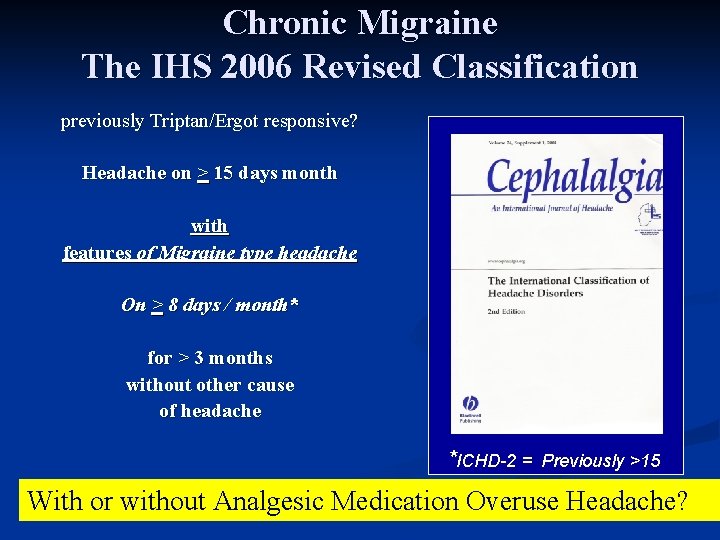
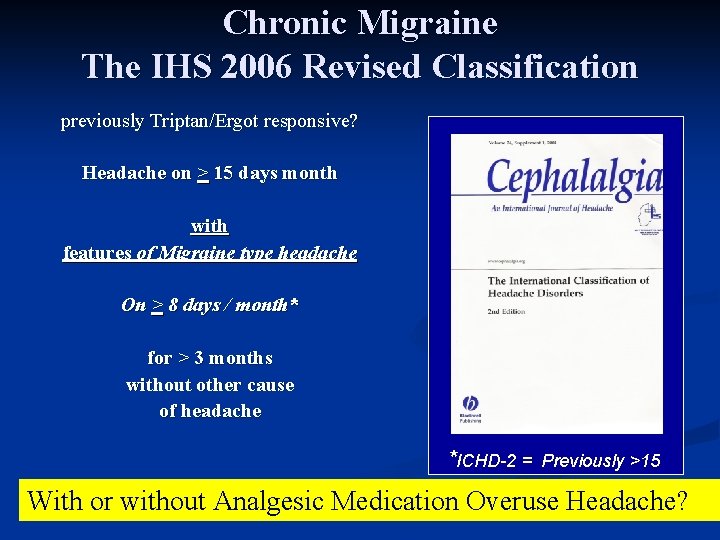
Chronic Migraine The IHS 2006 Revised Classification previously Triptan/Ergot responsive? Headache on > 15 days month with features of Migraine type headache On > 8 days / month* for > 3 months without other cause of headache *ICHD-2 = Previously >15 With or without Analgesic Medication Overuse Headache?
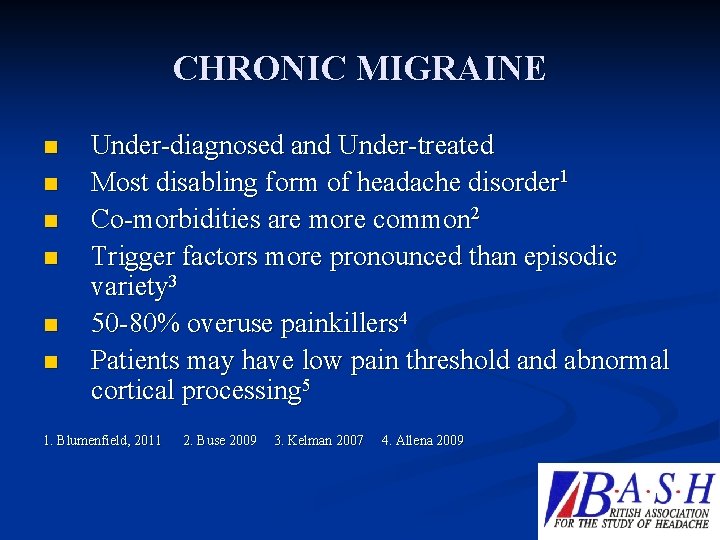
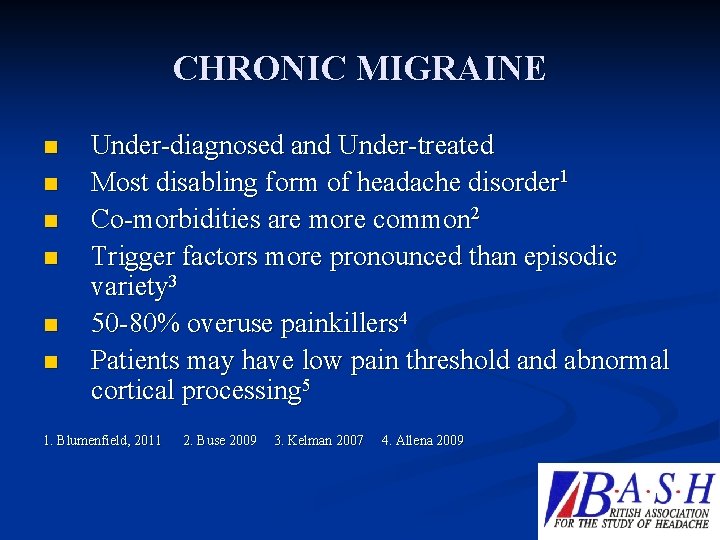
CHRONIC MIGRAINE n n n Under-diagnosed and Under-treated Most disabling form of headache disorder 1 Co-morbidities are more common 2 Trigger factors more pronounced than episodic variety 3 50 -80% overuse painkillers 4 Patients may have low pain threshold and abnormal cortical processing 5 1. Blumenfield, 2011 2. Buse 2009 3. Kelman 2007 4. Allena 2009
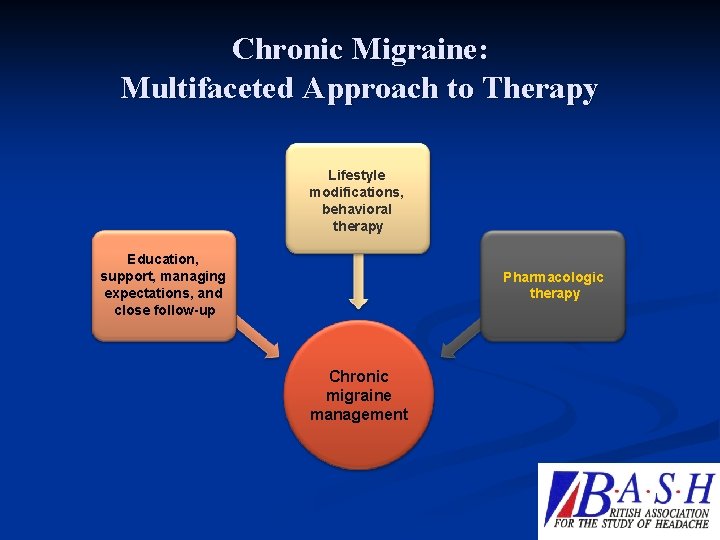
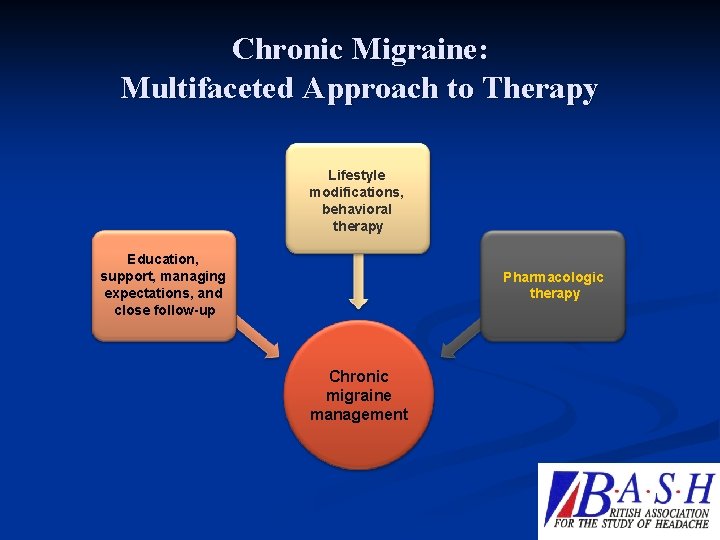
Chronic Migraine: Multifaceted Approach to Therapy Lifestyle modifications, behavioral therapy Education, support, managing expectations, and close follow-up Pharmacologic therapy Chronic migraine management Dodick DW N Engl J Med 2006; 354: 158– 165. 26
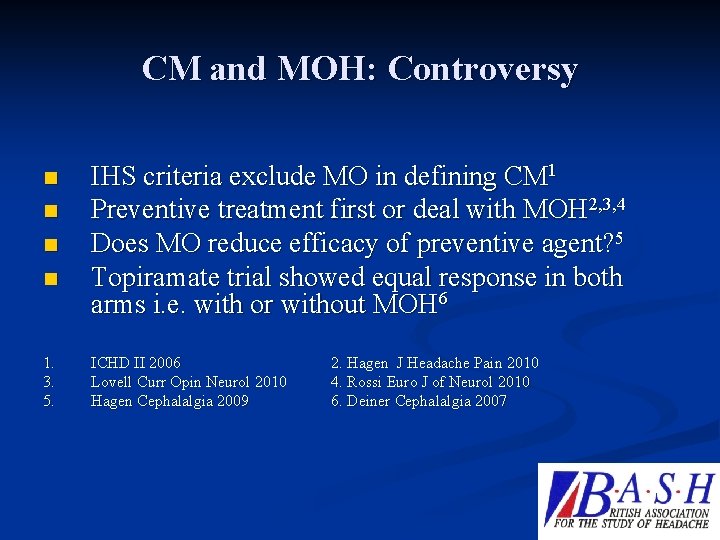
CM and MOH: Controversy n n 1. 3. 5. IHS criteria exclude MO in defining CM 1 Preventive treatment first or deal with MOH 2, 3, 4 Does MO reduce efficacy of preventive agent? 5 Topiramate trial showed equal response in both arms i. e. with or without MOH 6 ICHD II 2006 Lovell Curr Opin Neurol 2010 Hagen Cephalalgia 2009 2. Hagen J Headache Pain 2010 4. Rossi Euro J of Neurol 2010 6. Deiner Cephalalgia 2007
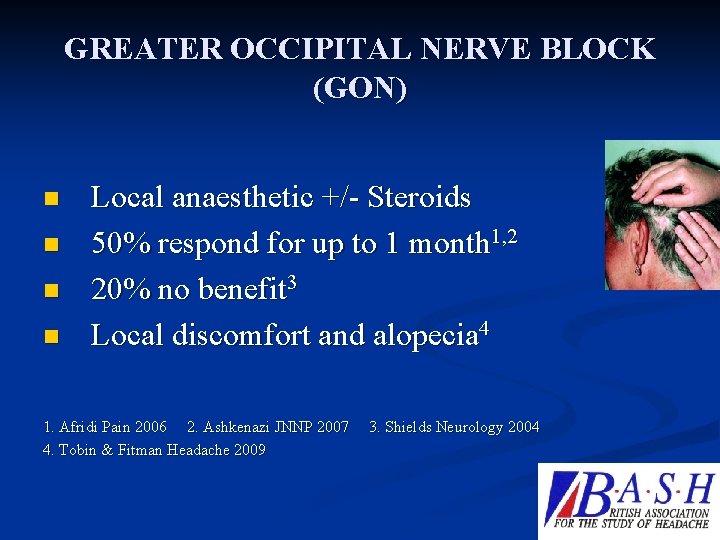
GREATER OCCIPITAL NERVE BLOCK (GON) n n Local anaesthetic +/- Steroids 50% respond for up to 1 month 1, 2 20% no benefit 3 Local discomfort and alopecia 4 1. Afridi Pain 2006 2. Ashkenazi JNNP 2007 4. Tobin & Fitman Headache 2009 3. Shields Neurology 2004
Botox in Migraine
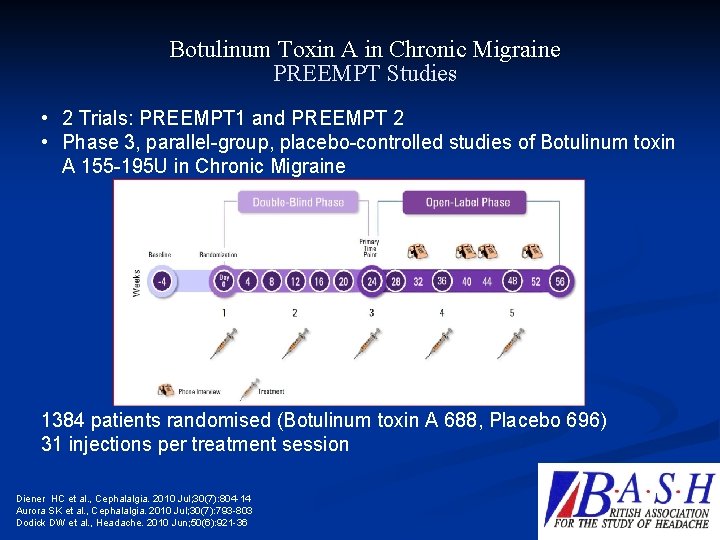
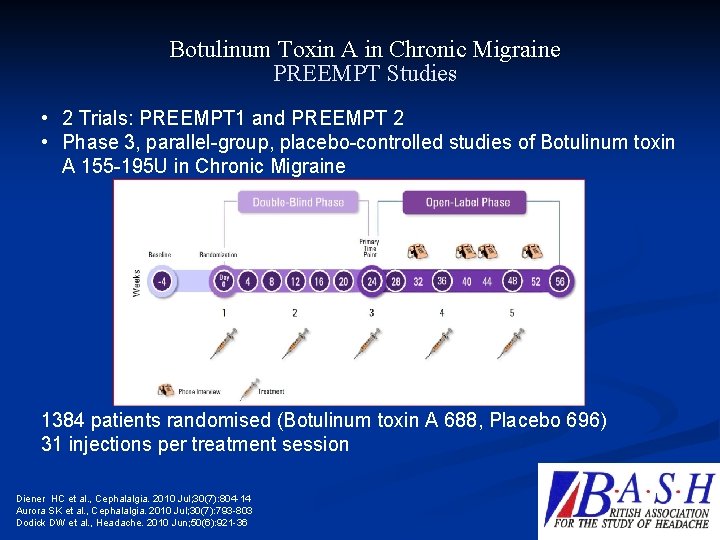
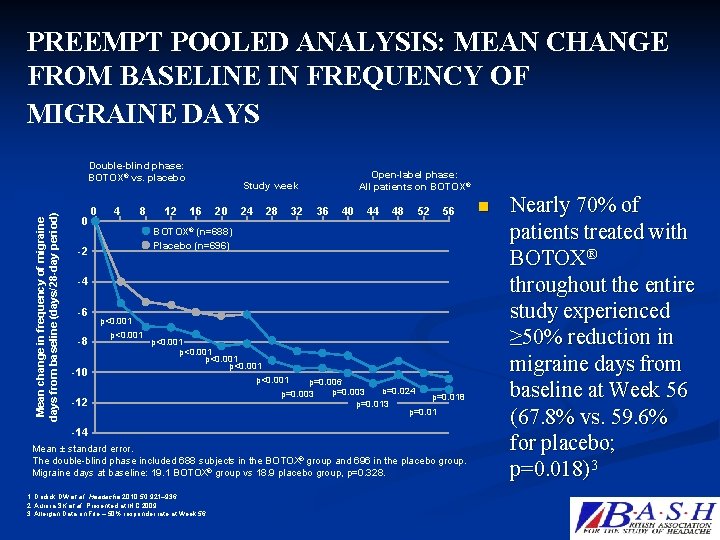
Botulinum Toxin A in Chronic Migraine PREEMPT Studies • 2 Trials: PREEMPT 1 and PREEMPT 2 • Phase 3, parallel-group, placebo-controlled studies of Botulinum toxin A 155 -195 U in Chronic Migraine 1384 patients randomised (Botulinum toxin A 688, Placebo 696) 31 injections per treatment session Diener HC et al. , Cephalalgia. 2010 Jul; 30(7): 804 -14 Aurora SK et al. , Cephalalgia. 2010 Jul; 30(7): 793 -803 Dodick DW et al. , Headache. 2010 Jun; 50(6): 921 -36
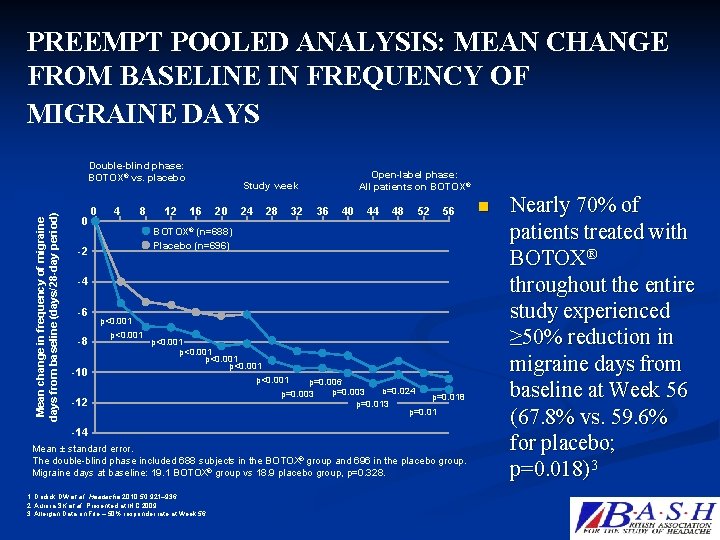
PREEMPT POOLED ANALYSIS: MEAN CHANGE FROM BASELINE IN FREQUENCY OF MIGRAINE DAYS Mean change in frequency migraine days from baseline (days/28 -day period) Mean change in frequency of migraine days from baseline (days/28 -day period) Double-blind phase: BOTOX® vs. placebo 0 0 4 8 12 Open-label phase: All patients on BOTOX® Study week 16 20 24 28 32 36 40 44 48 52 56 BOTOX® (n=688) Placebo (n=696) -2 -4 -6 -8 -10 p<0. 001 p<0. 001 -12 p=0. 006 p=0. 024 p=0. 003 p=0. 018 p=0. 013 p=0. 01 -14 Mean ± standard error. The double-blind phase included 688 subjects in the BOTOX® group and 696 in the placebo group. Migraine days at baseline: 19. 1 BOTOX® group vs 18. 9 placebo group, p=0. 328. 1. Dodick DW et al. Headache 2010; 50: 921– 936. 2. Aurora SK et al. Presented at IHC 2009. 3. Allergan Data on File – 50% responder rate at Week 56. n Nearly 70% of patients treated with BOTOX® throughout the entire study experienced ≥ 50% reduction in migraine days from baseline at Week 56 (67. 8% vs. 59. 6% for placebo; p=0. 018)3
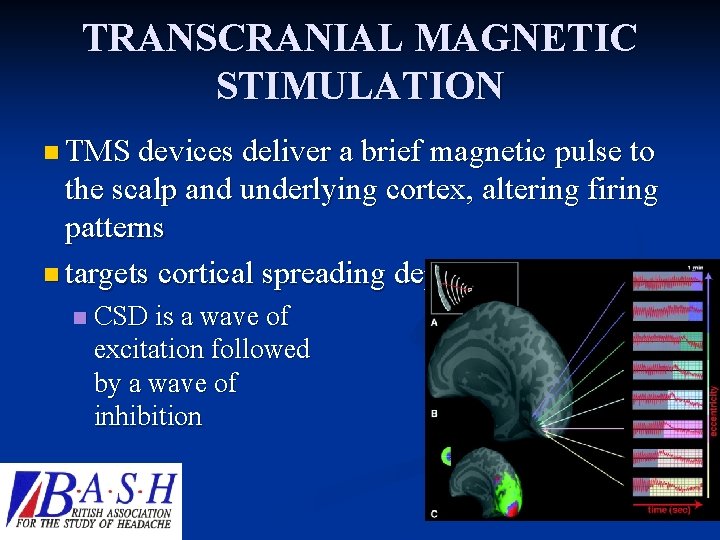
TRANSCRANIAL MAGNETIC STIMULATION n TMS devices deliver a brief magnetic pulse to the scalp and underlying cortex, altering firing patterns n targets cortical spreading depression (CSD) n CSD is a wave of excitation followed by a wave of inhibition
Transcranial Magnetic Stimulation for Migraine: A safety Review: Dodick et al Headache 2010; 50(7): 1153 -63 11/9/2020 33
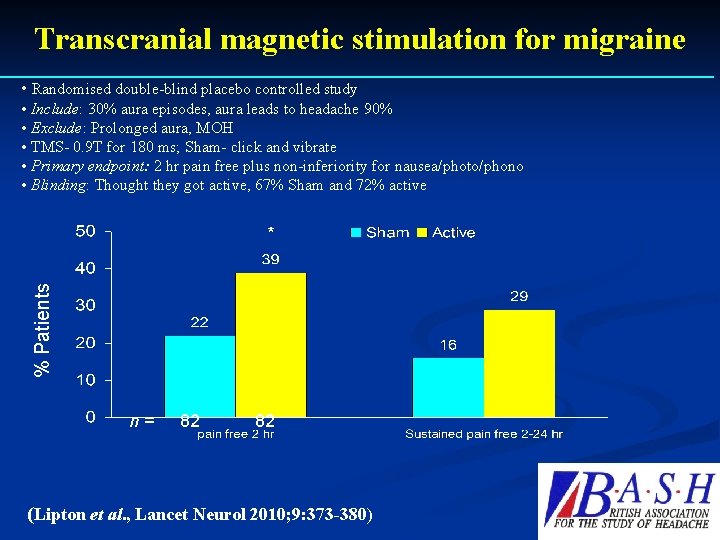
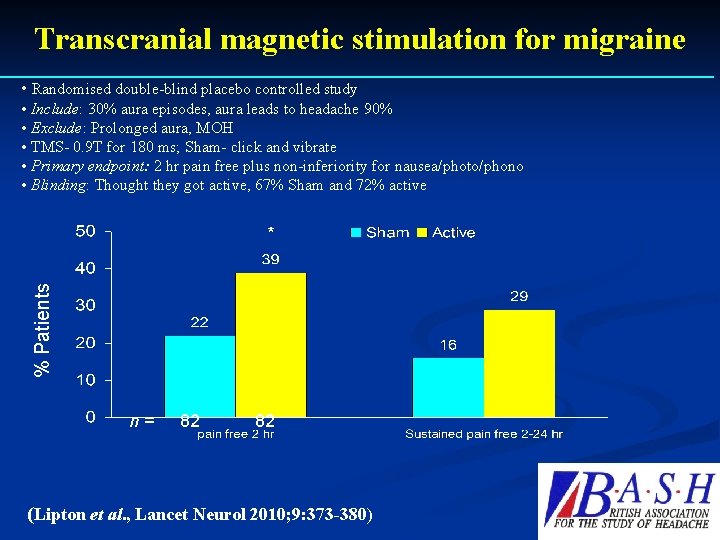
Transcranial magnetic stimulation for migraine • Randomised double-blind placebo controlled study • Include: 30% aura episodes, aura leads to headache 90% • Exclude: Prolonged aura, MOH • TMS- 0. 9 T for 180 ms; Sham- click and vibrate • Primary endpoint: 2 hr pain free plus non-inferiority for nausea/photo/phono • Blinding: Thought they got active, 67% Sham and 72% active % Patients * n = 82 (Lipton et al. , Lancet Neurol 2010; 9: 373 -380)

Occipital Nerve Stimulator: St Jude’s device n CE Marked n Chronic Migraine and intractable TAC 11/9/2020 35
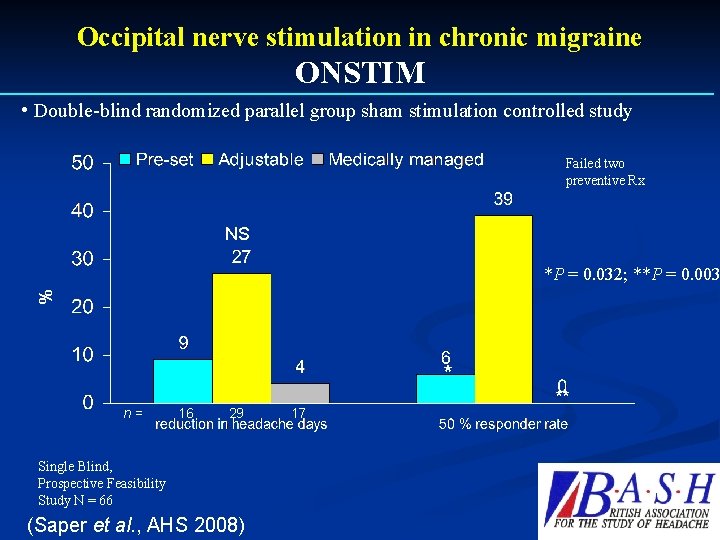
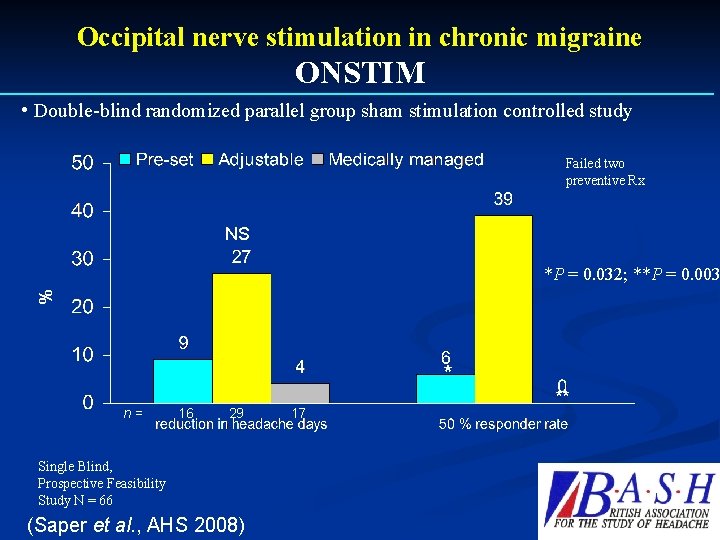
Occipital nerve stimulation in chronic migraine ONSTIM • Double-blind randomized parallel group sham stimulation controlled study Failed two preventive Rx NS % *P = 0. 032; **P = 0. 003 * n = 16 29 17 Single Blind, Prospective Feasibility Study N = 66 (Saper et al. , AHS 2008) **
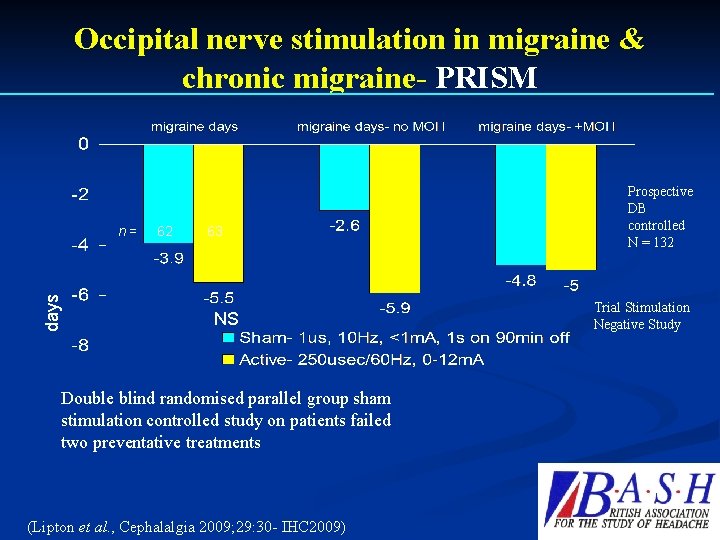
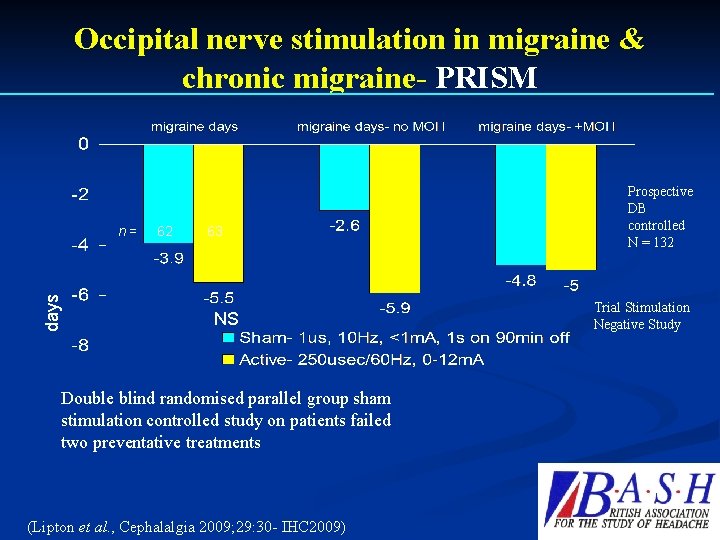
Occipital nerve stimulation in migraine & chronic migraine- PRISM days n = 62 63 NS Double blind randomised parallel group sham stimulation controlled study on patients failed two preventative treatments (Lipton et al. , Cephalalgia 2009; 29: 30 - IHC 2009) Prospective DB controlled N = 132 Trial Stimulation Negative Study
Gamma Core Vagal Nerve Stimulator n Received CE Marked n Low ampere Stimulation n Prophylaxis as well as acute Treatment. 11/9/2020 38
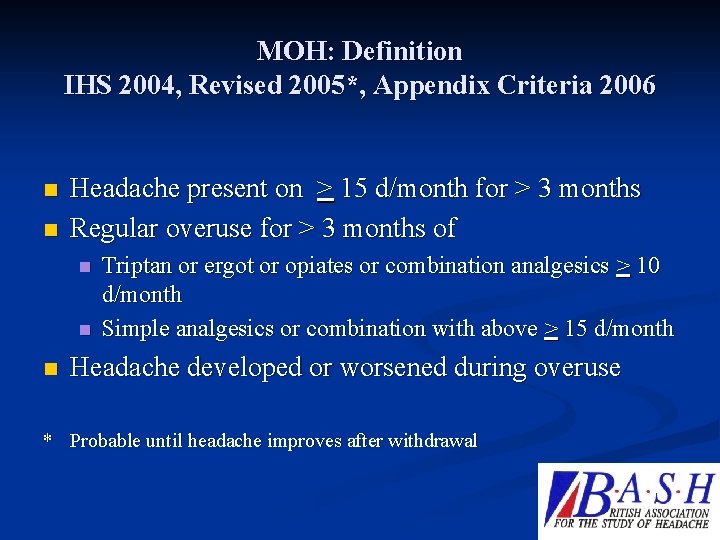
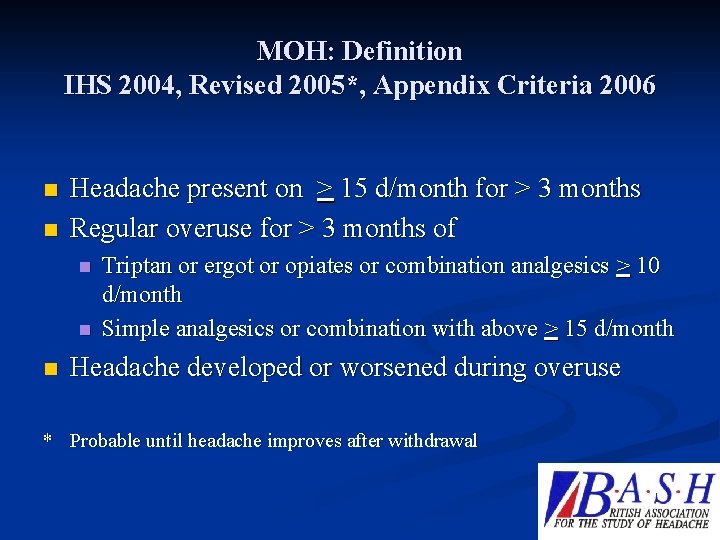
MOH: Definition IHS 2004, Revised 2005*, Appendix Criteria 2006 n n Headache present on > 15 d/month for > 3 months Regular overuse for > 3 months of n n n Triptan or ergot or opiates or combination analgesics > 10 d/month Simple analgesics or combination with above > 15 d/month Headache developed or worsened during overuse * Probable until headache improves after withdrawal
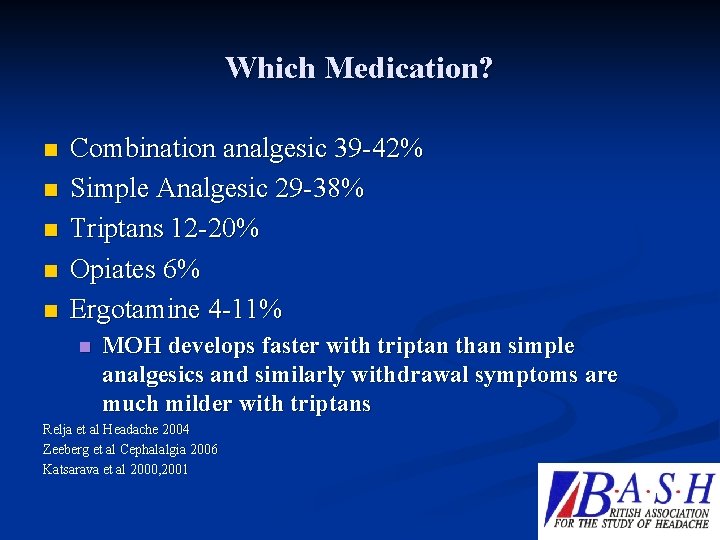
Which Medication? n n n Combination analgesic 39 -42% Simple Analgesic 29 -38% Triptans 12 -20% Opiates 6% Ergotamine 4 -11% n MOH develops faster with triptan than simple analgesics and similarly withdrawal symptoms are much milder with triptans Relja et al Headache 2004 Zeeberg et al Cephalalgia 2006 Katsarava et al 2000, 2001
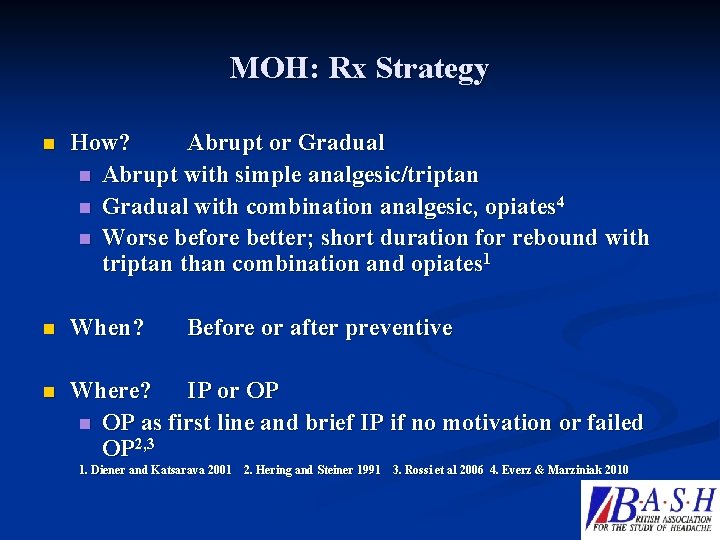
MOH: Rx Strategy n How? Abrupt or Gradual n Abrupt with simple analgesic/triptan n Gradual with combination analgesic, opiates 4 n Worse before better; short duration for rebound with triptan than combination and opiates 1 n When? n Where? IP or OP n OP as first line and brief IP if no motivation or failed OP 2, 3 Before or after preventive 1. Diener and Katsarava 2001 2. Hering and Steiner 1991 3. Rossi et al 2006 4. Everz & Marziniak 2010
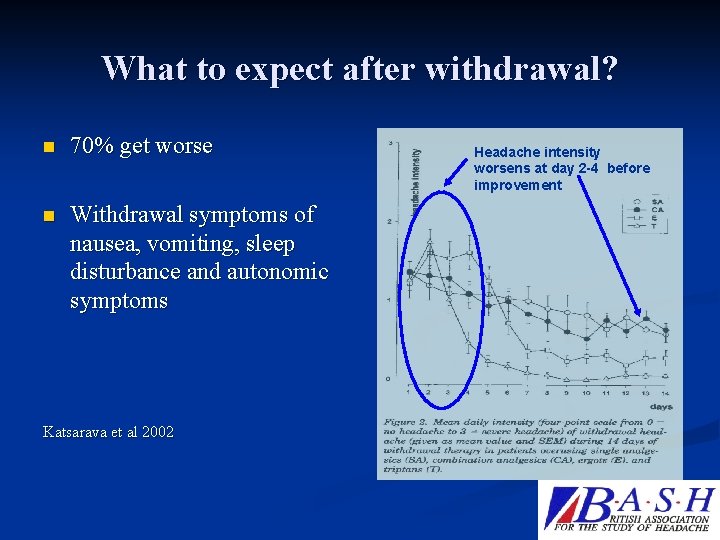
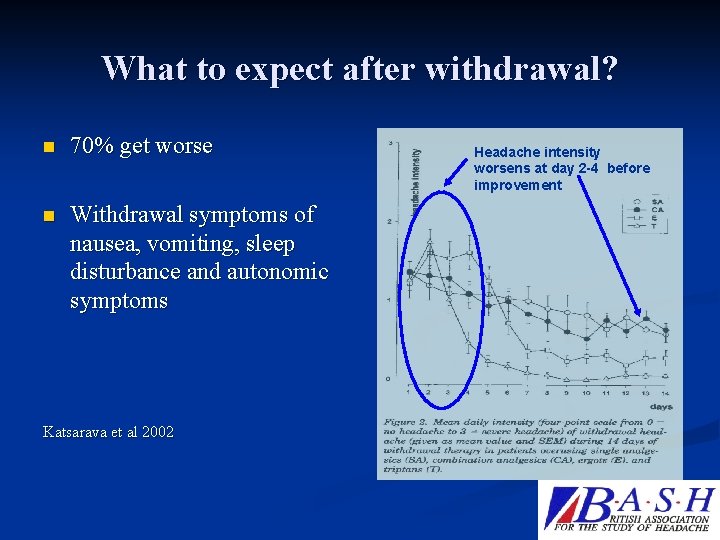
What to expect after withdrawal? n 70% get worse n Withdrawal symptoms of nausea, vomiting, sleep disturbance and autonomic symptoms Katsarava et al 2002 Headache intensity worsens at day 2 -4 before improvement
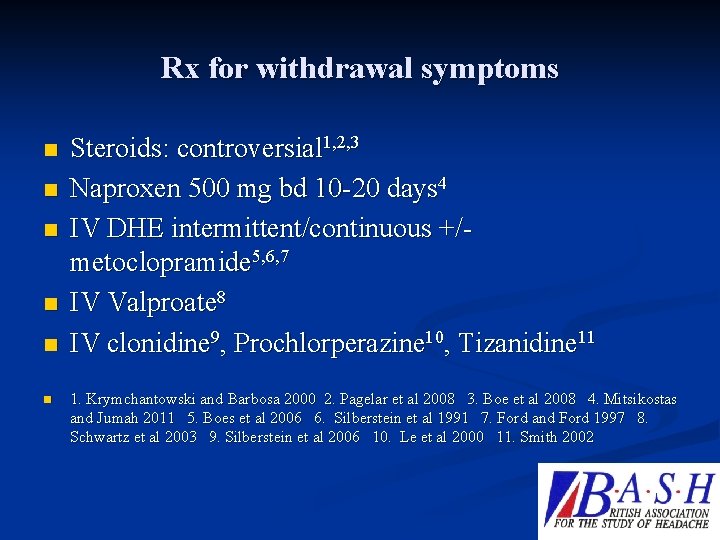
Rx for withdrawal symptoms n n n Steroids: controversial 1, 2, 3 Naproxen 500 mg bd 10 -20 days 4 IV DHE intermittent/continuous +/metoclopramide 5, 6, 7 IV Valproate 8 IV clonidine 9, Prochlorperazine 10, Tizanidine 11 1. Krymchantowski and Barbosa 2000 2. Pagelar et al 2008 3. Boe et al 2008 4. Mitsikostas and Jumah 2011 5. Boes et al 2006 6. Silberstein et al 1991 7. Ford and Ford 1997 8. Schwartz et al 2003 9. Silberstein et al 2006 10. Le et al 2000 11. Smith 2002
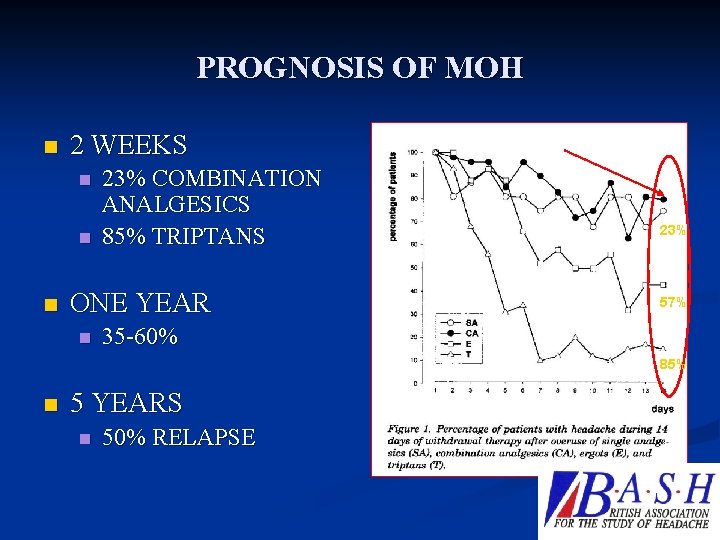
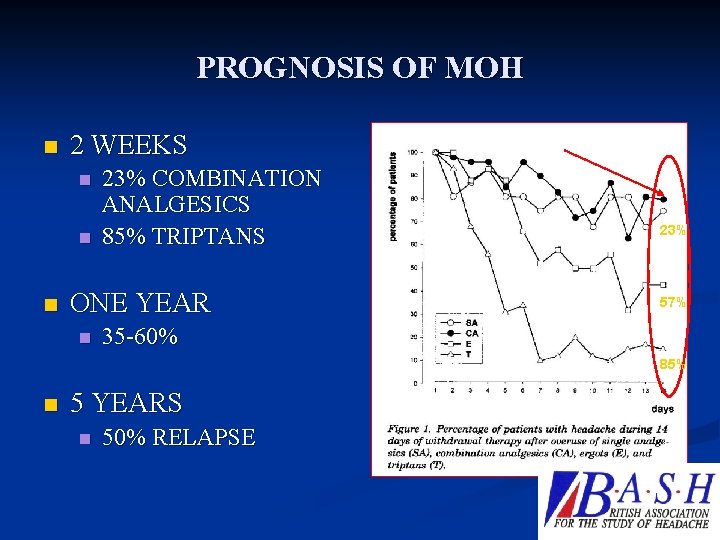
PROGNOSIS OF MOH n 2 WEEKS n n n 23% COMBINATION ANALGESICS 85% TRIPTANS ONE YEAR n 23% 57% 35 -60% 85% n 5 YEARS n 50% RELAPSE
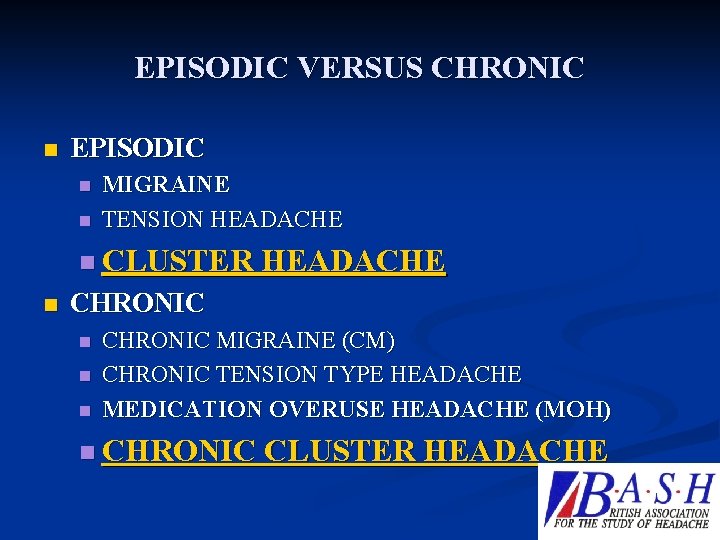
EPISODIC VERSUS CHRONIC n EPISODIC n n MIGRAINE TENSION HEADACHE n CLUSTER HEADACHE n CHRONIC n n n CHRONIC MIGRAINE (CM) CHRONIC TENSION TYPE HEADACHE MEDICATION OVERUSE HEADACHE (MOH) n CHRONIC CLUSTER HEADACHE
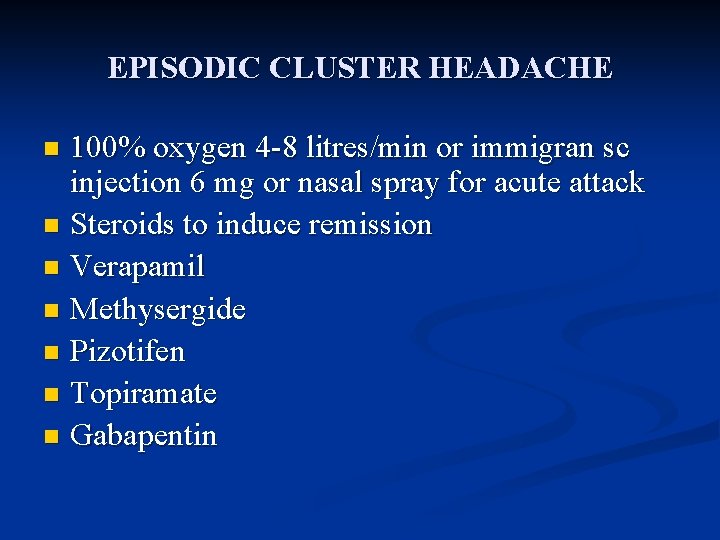
EPISODIC CLUSTER HEADACHE 100% oxygen 4 -8 litres/min or immigran sc injection 6 mg or nasal spray for acute attack n Steroids to induce remission n Verapamil n Methysergide n Pizotifen n Topiramate n Gabapentin n
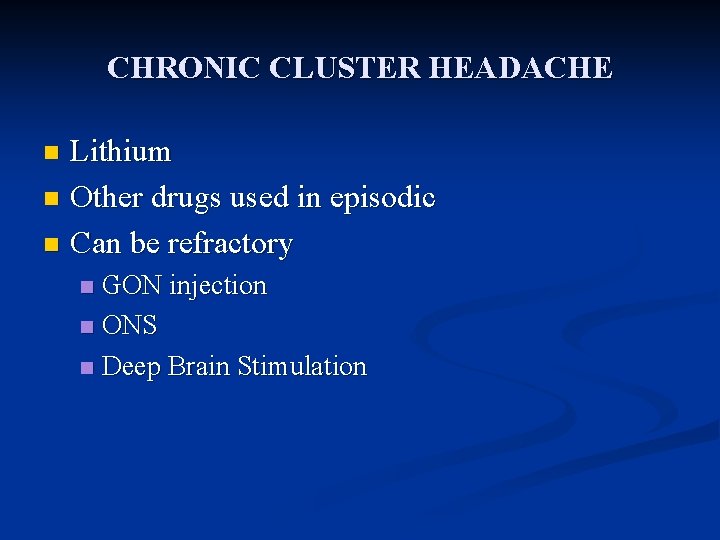
CHRONIC CLUSTER HEADACHE Lithium n Other drugs used in episodic n Can be refractory n GON injection n ONS n Deep Brain Stimulation n
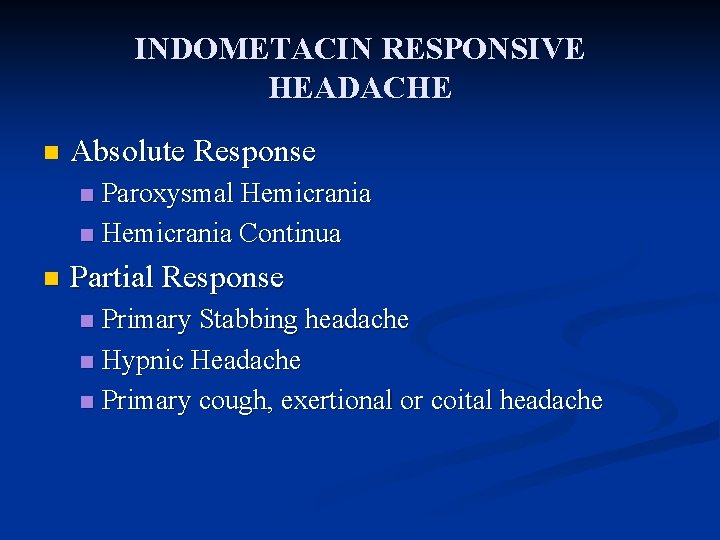
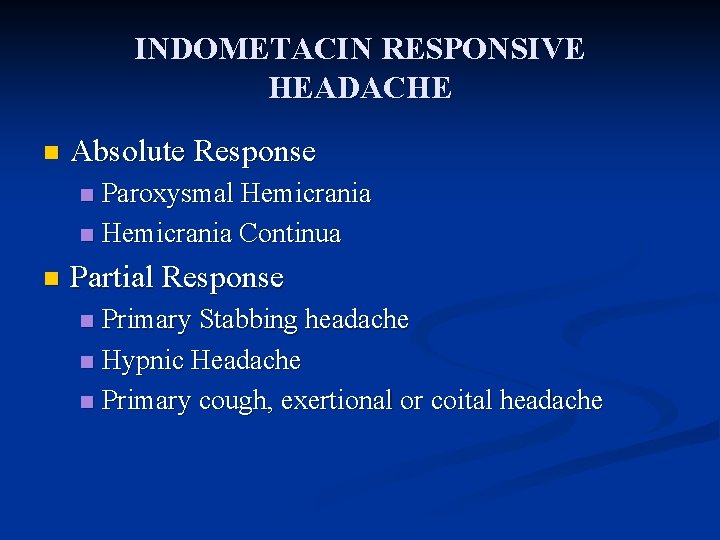
INDOMETACIN RESPONSIVE HEADACHE n Absolute Response Paroxysmal Hemicrania n Hemicrania Continua n n Partial Response Primary Stabbing headache n Hypnic Headache n Primary cough, exertional or coital headache n
THANKS n n n JOIN BASH ELECTRONIC OR PAPER COPY OF CEPHALALGIA REGULAR NEWSLETTERS INVITATION TO BASH EVENTS ABILITY TO CONTRIBUTE TO RESEARCH THROUGH INTERACTIVE WEBSITE (ABOUT TO LAUNCH)
 Fayyaz ahmed md
Fayyaz ahmed md Dr fayyaz ahmed
Dr fayyaz ahmed Types of headaches chart
Types of headaches chart Ahmed muhudiin ahmed
Ahmed muhudiin ahmed Gerundio del verbo ir
Gerundio del verbo ir Fiesta es un verbo
Fiesta es un verbo Verbo ir + a + infinitivo
Verbo ir + a + infinitivo Clifton primary school hull
Clifton primary school hull Coast guard manufacturers identification code
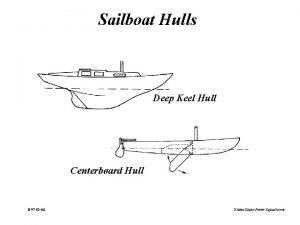
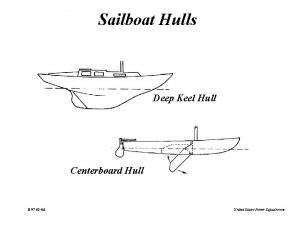
Coast guard manufacturers identification code Hull cut off equation for cylindrical magnetron
Hull cut off equation for cylindrical magnetron Hype people earth duh hey
Hype people earth duh hey Carlson design hull designer
Carlson design hull designer Convex hull collision detection
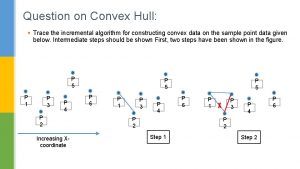
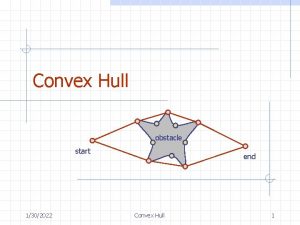
Convex hull collision detection Convex hull
Convex hull Deputy jody hull
Deputy jody hull Ace lie soap eye
Ace lie soap eye Apply for secondary school hull
Apply for secondary school hull Hin validation
Hin validation Hull comportamentismo
Hull comportamentismo Mackenzie hull
Mackenzie hull Hull shader
Hull shader Hull's landing menu
Hull's landing menu Jane dee hull elementary
Jane dee hull elementary Sarkadi édes ősz
Sarkadi édes ősz Convex hull
Convex hull Web services hull
Web services hull Clark leonard hull
Clark leonard hull Mimi hull
Mimi hull Ship hull
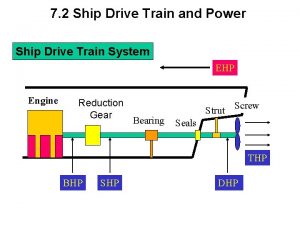
Ship hull Hull
Hull Vehicle hull identification number
Vehicle hull identification number Greek letters john c hull
Greek letters john c hull For hull, drive reduction is ____.
For hull, drive reduction is ____. Dynamic convex hull
Dynamic convex hull Boot top ship
Boot top ship Hlc hull
Hlc hull Hull white trinomial tree
Hull white trinomial tree Corn minus the hull and germ.
Corn minus the hull and germ. Hull speed
Hull speed Corn minus the hull and germ
Corn minus the hull and germ Hull white tree
Hull white tree Hull and propeller performance
Hull and propeller performance John c hull
John c hull Marpol annexes
Marpol annexes Ship structural components
Ship structural components Heidi hull fm global
Heidi hull fm global Transversely framed คือ
Transversely framed คือ Clark l. hull
Clark l. hull Chat hull
Chat hull Concave vs convex hull
Concave vs convex hull