Managing Asthma In The School Setting Natomas Unified






- Slides: 41
Managing Asthma In The School Setting Natomas Unified School District
What You Need To Know • • What is asthma? What happens during an asthma episode What can cause an asthma episode Early warning signs of an asthma episode What to do if a child is having an “asthma attack” When to call 911 How to use a peak flow meter How to use an inhaler
What is Asthma? • Asthma is a CHRONIC lung disease that affects people of all ages and race. • It is caused by inflammation (swelling) of the lining of the airways (windpipes). • The inflammation causes the airway to narrow (bronchoconstriction) and makes it difficult to breathe. • The lungs produce excessive mucus, further narrowing the airways.
What is Asthma? • Asthma often begins in childhood (it is frequently associated with an allergic reaction) however, it can develop at anytime in life. • Currently there is no cure for asthma. It is a breathing problem that a person has to live with for the rest of his/her life. With proper care asthma can be controlled and allows a person to live a full normal life.
What is Asthma? Asthma is a disease that: • Is chronic • Produces recurring episodes of breathing problems – Coughing – Wheezing – Chest tightness – Shortness of breath • Cannot be cured, but can be controlled

Cost of Asthma • Quality of life (sick most of the time if not controlled) • Education (Leading cause of school absences) – Over 14 million school day missed • Work – Productivity (parents, other caretaker) • Hospital/ER Visits – $13 Billion dollars
An Asthma Episode (“Asthma Attack”) • When a person has trouble breathing because of asthma, the problem is in the airways of the lungs. • The airways become narrow because they are swollen. This is caused by: – Tightening of the muscles around the airways; – Swelling of the lining of the airways; – The lungs produces mucus that clogs the small airways.
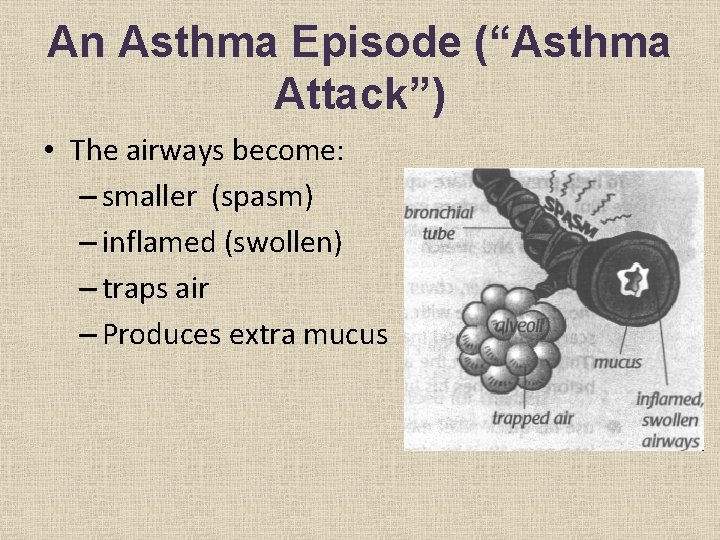
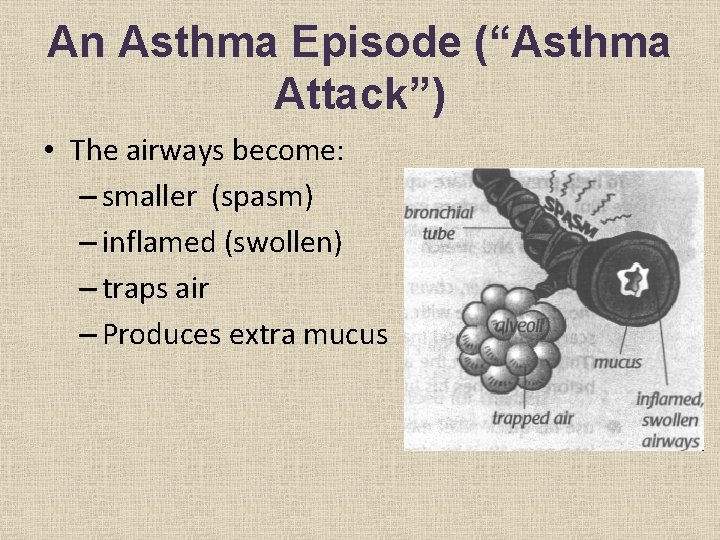
An Asthma Episode (“Asthma Attack”) • The airways become: – smaller (spasm) – inflamed (swollen) – traps air – Produces extra mucus
An Asthma Episode (“Asthma Attack”) • Breathing gets harder as the person tries to force air through the narrower airways. • The air the person breathes may make a wheezing or whistling sounds, and may cause them to cough or spit up mucus. • An asthma episode is a problem that can be life threatening if not taken care of right way.
What Can Cause An Asthma Episode • Asthma episode is caused by certain factors known as triggers. • Asthma triggers differ from child to child. • These triggers falls into 3 general categories: – Allergens – Irritants – Physical Conditions
Allergens • Allergens – are the most common cause of asthma attacks. They are usually inhaled. • Allergens include but are not limited to: – Warm-blooded pet dander (dogs, cats, birds, and small rodents) – House dust mites – Cockroaches – Pollens from grass and trees – Molds (indoors and outdoors)
Irritants • Irritants – things that a person can be exposed to: – Cigarette smoke, wood dust – Scented products (hair spray, perfume, cosmetics…etc. ) – Cleaning products (glass cleaners, bathroom cleaners, laundry detergents…etc. ) – Strong odors from fresh paint or cooking – Automobile fumes and air pollution – Chemicals (pesticides, lawn treatments…etc. )
Physical Conditions • Physical Conditions: – Infections in the upper airways, such as colds (a common trigger for both children and adults) – Exercise (exercise induced asthma) – Strong expressions of feelings (crying, laughing) – Changes in weather and temperature, cold air, dry air – Heartburn
Early warning signs of an asthma episode • An asthma episode begins slowly. • Most children feels warning signs when an episode is starting. • Often times an asthma episode is precipitated by a cold or a flu.
Early Warning Signs • Dry cough • Feeling tired (not wanting to play) • Feeling sad, angry • Trouble sleeping • Stuffy nose, runny nose, watery eyes • Sneezing, itchy throat • Stomachache • Headache • Fast heartbeat • Tight chest • Shortness of breath or fast breathing • Wheezing, noises when breathing • Ear pain • Drop in peak flow meter scores
What do you do if a child is having an asthma episode (asthma attack)?
What to do if someone has an asthma “attack” • Evaluate the situation • Remain calm • Are their lips, tongue, or nail beds turning? • Is there a change in level of consciousness or confusion? • Be reassuring
Green Zone This means the child is doing well • No coughing • No wheezing • No chest tightness • No shortness of breath Student can go back to class
Yellow Zone Student has a: • Cough • Wheezy • Chest tightness • Short of breath
What to do: • Have the student sit in an upright position. • Check the asthma management plan • Check to see if the student has a peak flow meter and /or inhaler at school
Yellow Zone continued… • If he/she has a peak flow meter and/or inhaler have them use it as prescribed. • Make sure to follow the doctor’s orders. How many puffs does the order say? • May give room temperature water to drink. • Have them rest in the health office until they are in the green zone.
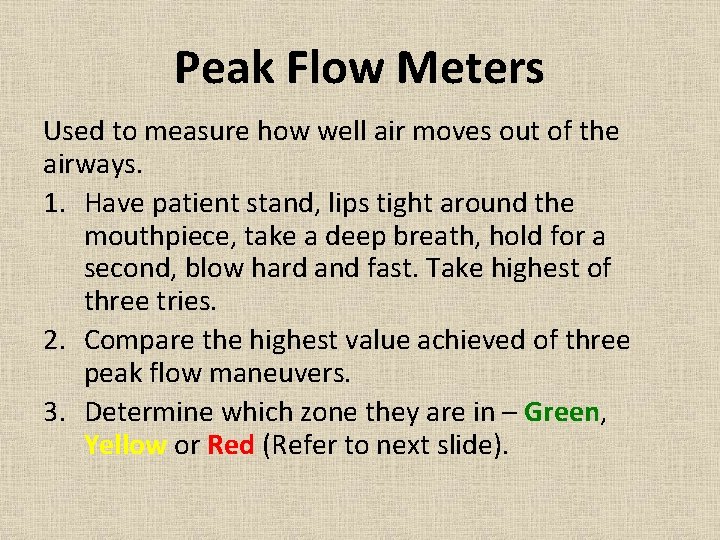
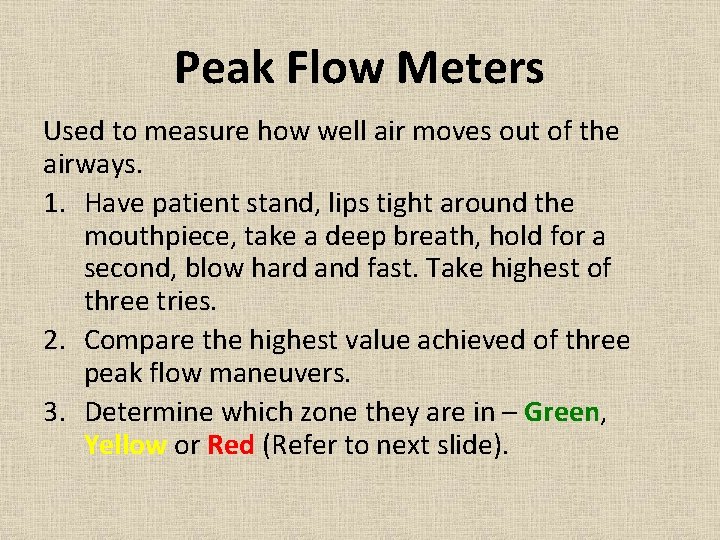
Peak Flow Meters Used to measure how well air moves out of the airways. 1. Have patient stand, lips tight around the mouthpiece, take a deep breath, hold for a second, blow hard and fast. Take highest of three tries. 2. Compare the highest value achieved of three peak flow maneuvers. 3. Determine which zone they are in – Green, Yellow or Red (Refer to next slide).

Peak Flow Meters
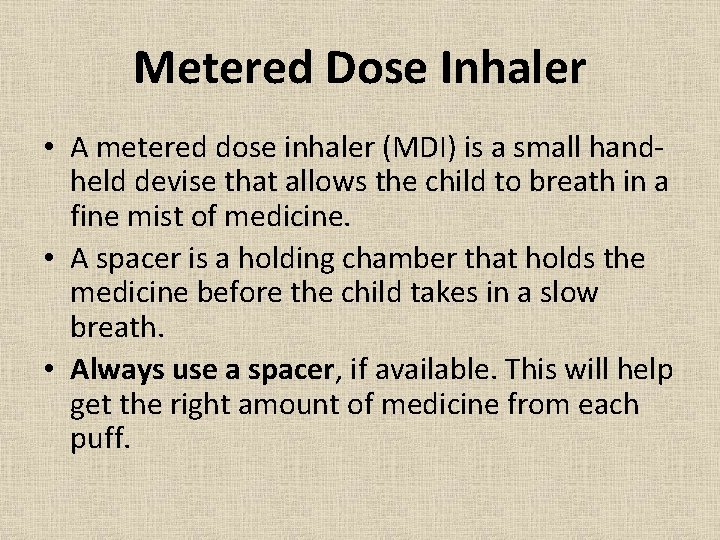
Metered Dose Inhaler • A metered dose inhaler (MDI) is a small handheld devise that allows the child to breath in a fine mist of medicine. • A spacer is a holding chamber that holds the medicine before the child takes in a slow breath. • Always use a spacer, if available. This will help get the right amount of medicine from each puff.
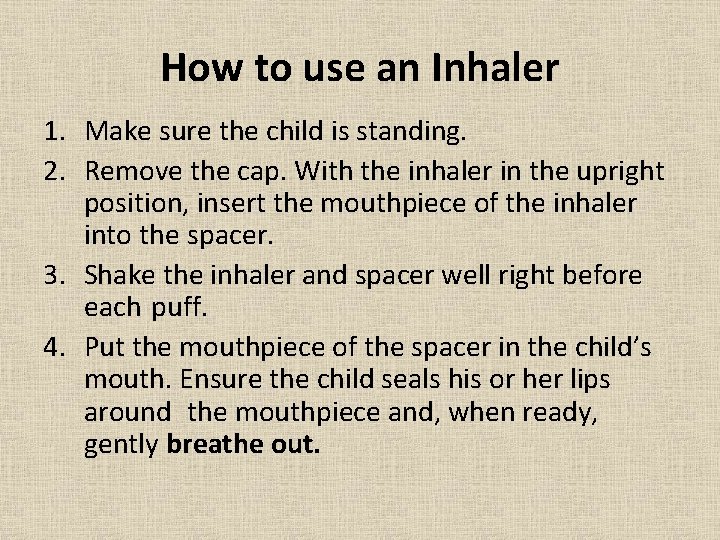
How to use an Inhaler 1. Make sure the child is standing. 2. Remove the cap. With the inhaler in the upright position, insert the mouthpiece of the inhaler into the spacer. 3. Shake the inhaler and spacer well right before each puff. 4. Put the mouthpiece of the spacer in the child’s mouth. Ensure the child seals his or her lips around the mouthpiece and, when ready, gently breathe out.
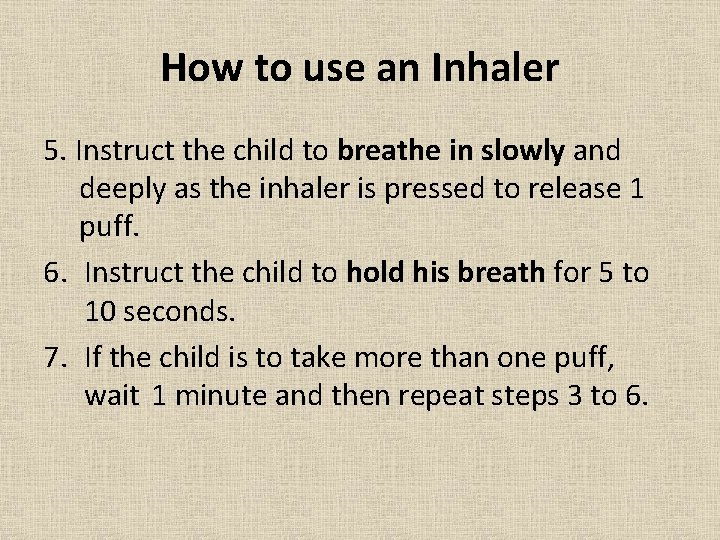
How to use an Inhaler 5. Instruct the child to breathe in slowly and deeply as the inhaler is pressed to release 1 puff. 6. Instruct the child to hold his breath for 5 to 10 seconds. 7. If the child is to take more than one puff, wait 1 minute and then repeat steps 3 to 6.

Yellow Zone continued… • If symptoms do not clear up after using the inhaler contact parent/guardian. • If no inhaler is available contact parent/guardian to bring one of pick student up. • Have the student stay indoors during recess, lunch recess, and PE if the air quality is poor.
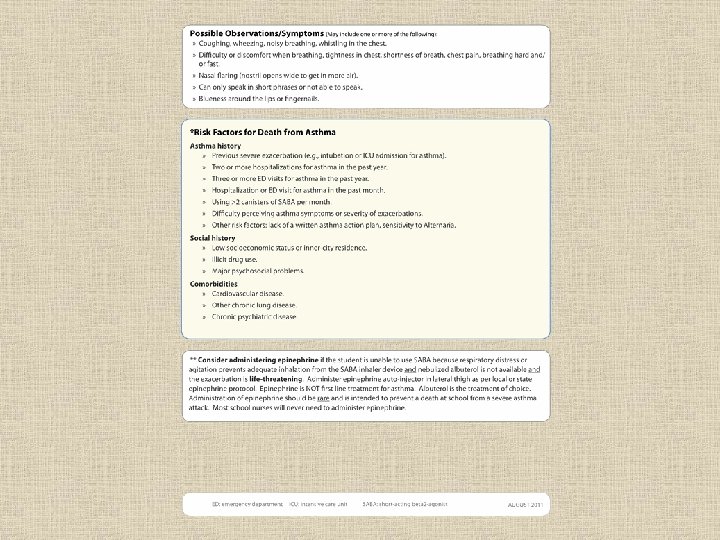
Red Zone • Student is VERY short of breath OR • The inhaler did not work • Trouble walking or talking due to shortness of breath • Lips and/or fingernails are blue
Red Zone continued… • Are symptoms worsening? • Are they having difficulty speaking in full sentences? • Loud wheezes or persistent cough • Is there a decreased level of consciousness?
Signs of difficulty breathing • Rapid or shallow breathing • Not able to speak in full sentences • Wheezing (high pitched sound) • Tightness in the chest
Signs of difficulty breathing continued… • Widening of the nostrils • Increased use of stomach and chest muscles • Excessive coughing • Appears very anxious

When to call 9 -1 -1 • Symptoms are getting worse • Signs of difficulty breathing • Decreased level of consciousness • Lips, tongue, or nail beds are blue
Resources • Allergy and Asthma Network/Mothers of Asthmatics 1 -800 -878 -4403 www. aanma. org • American College of Allergy, Asthma and Immunology 1 -800 -842 -7777 www. allergy. mcg. edu • American Lung Association 1800 -586 -4872 www. lungusa. org Asthma & Allergy Foundation of America (AAFA) 1 -800 -727 -8462 www. aafa. org Lung, Line, National Jewish Medical Research Center 1 -800 -222 -5864 www. njc. org National Institute of Allergy and Infectious Disease 1 -301 -496 -5717 www. niaid. nih. gov National Asthma Education and Prevention Program National Heart, Lung and Blood Institute 1 -301 -592 -8573 www. nhlbi. nih. gov