MANAGEMENT OF ACUTE AND CHRONIC PANCREATITIS R A




- Slides: 35
MANAGEMENT OF ACUTE AND CHRONIC PANCREATITIS R. A. Singh MD FRCPC AGAF Clinical Assistant Professor of Medicine Division of Gastroenterology, UBC

Disclosures • Speaker honorarium from: Takeda Abbvie Janssen Pentax • Clinical Research Funds Celgene Gilead Takeda Janssen No financial disclosures for this specific talk
Learning Objectives • Distinguish the pathophysiology, complications and management between acute and chronic pancreatitis • Distinguish between the in- patient management between acute and chronic pancreatitis
Introduction • Acute Pancreatitis (AP) and Chronic Pancreatitis(CP) are two distinct disease states • Most common cause of AP is gallstones and alcohol • Less common cause include hyperlipidemia, hypercalcemia, celiac disease, autoimmune, drugs • Chronic Pancreatitis is rarely dealt with in hospital • CP is usually caused by alcohol • Smoking is an independent risk factor for CP progression
Pathophysiology • Acute pancreatitis is caused by acute inflammation of the pancreatic parenchyma • Acute inflammation can lead to systemic inflammatory response syndrome ( SIRS) • SIRS can lead to respiratory depression, renal failure and hypovolemic shock • Sepsis is typically caused by transmural lumenal bacterial migration
Pathophysiology • Chronic pancreatitis is caused by chronic inflammation and fibrosis • This damage can lead to exocrine dysfunction ( diarrhea) or endocrine dysfunction ( diabetes) and cancer • Pain is common • Acute on chronic pancreatitis is caused by acute parenchymal inflammation on the background of CP • This leads to self limited abdominal pain and short stays in hospital • Serious acute complications are rare
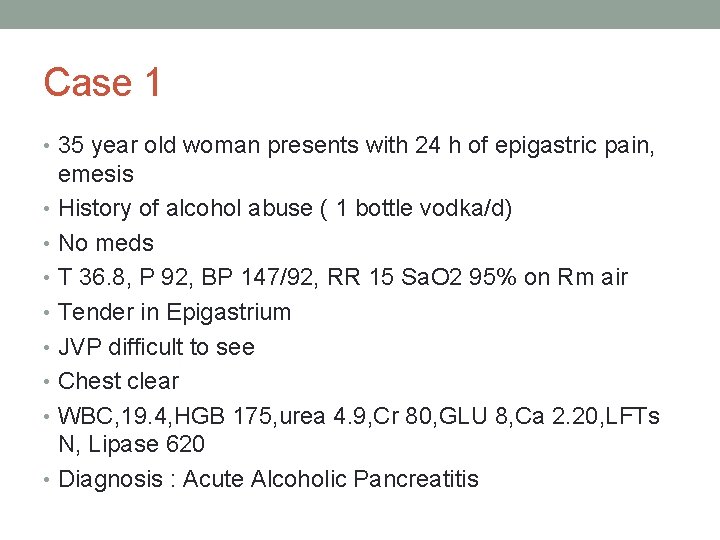
Case 1 • 35 year old woman presents with 24 h of epigastric pain, emesis • History of alcohol abuse ( 1 bottle vodka/d) • No meds • T 36. 8, P 92, BP 147/92, RR 15 Sa. O 2 95% on Rm air • Tender in Epigastrium • JVP difficult to see • Chest clear • WBC, 19. 4, HGB 175, urea 4. 9, Cr 80, GLU 8, Ca 2. 20, LFTs N, Lipase 620 • Diagnosis : Acute Alcoholic Pancreatitis
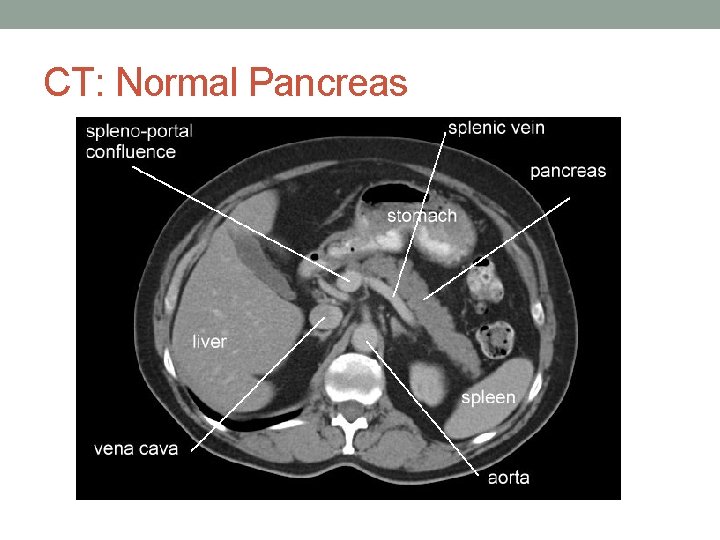
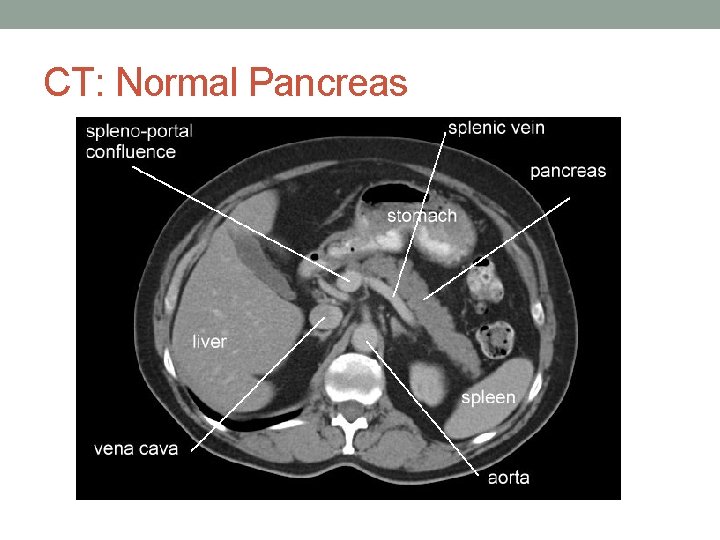
CT: Normal Pancreas

Case 1
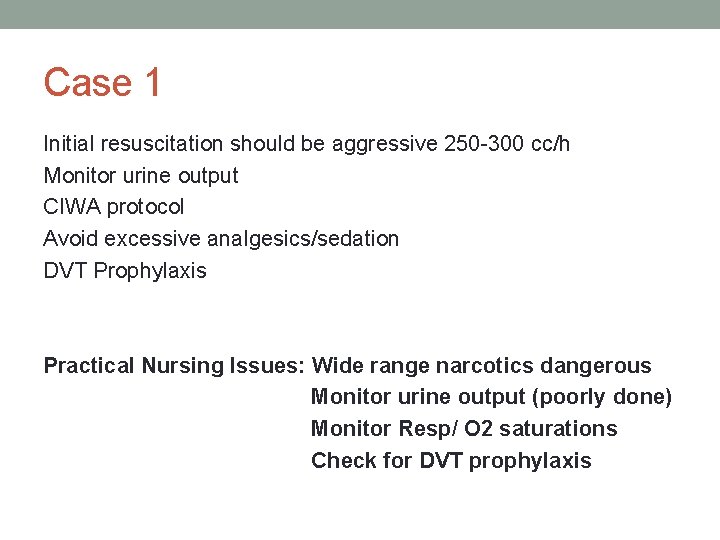
Case 1 Initial resuscitation should be aggressive 250 -300 cc/h Monitor urine output CIWA protocol Avoid excessive analgesics/sedation DVT Prophylaxis Practical Nursing Issues: Wide range narcotics dangerous Monitor urine output (poorly done) Monitor Resp/ O 2 saturations Check for DVT prophylaxis
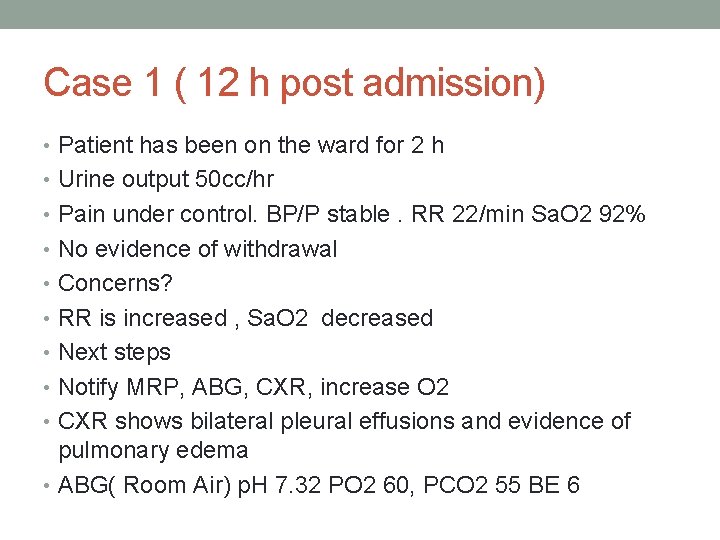
Case 1 ( 12 h post admission) • Patient has been on the ward for 2 h • Urine output 50 cc/hr • Pain under control. BP/P stable. RR 22/min Sa. O 2 92% • No evidence of withdrawal • Concerns? • RR is increased , Sa. O 2 decreased • Next steps • Notify MRP, ABG, CXR, increase O 2 • CXR shows bilateral pleural effusions and evidence of pulmonary edema • ABG( Room Air) p. H 7. 32 PO 2 60, PCO 2 55 BE 6
Case 1 • ICU asked to assess • Patient brought to ICU for observation • Patient continues to deteriorate in ICU and is intubated within 2 hr of admission to ICU ( 16 h post admission) • Practical Nursing Issues: AP patients can deteriorate quickly, changes in respiratory status can be subtle
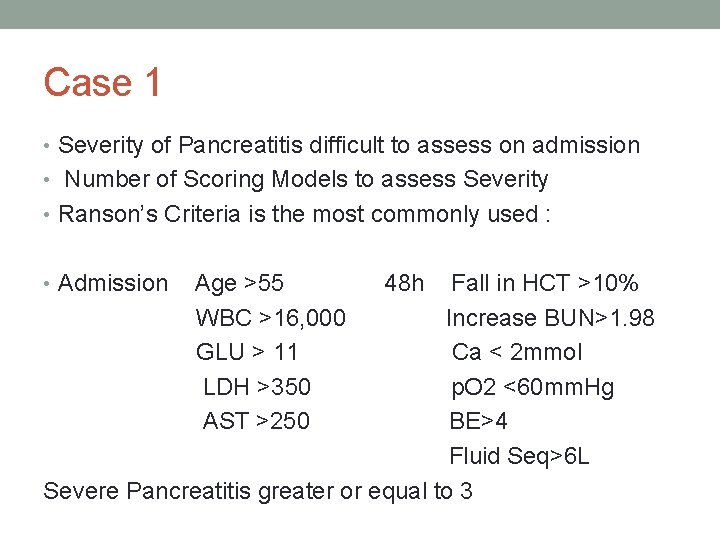
Case 1 • Severity of Pancreatitis difficult to assess on admission • Number of Scoring Models to assess Severity • Ranson’s Criteria is the most commonly used : • Admission Age >55 WBC >16, 000 GLU > 11 LDH >350 AST >250 48 h Fall in HCT >10% Increase BUN>1. 98 Ca < 2 mmol p. O 2 <60 mm. Hg BE>4 Fluid Seq>6 L Severe Pancreatitis greater or equal to 3
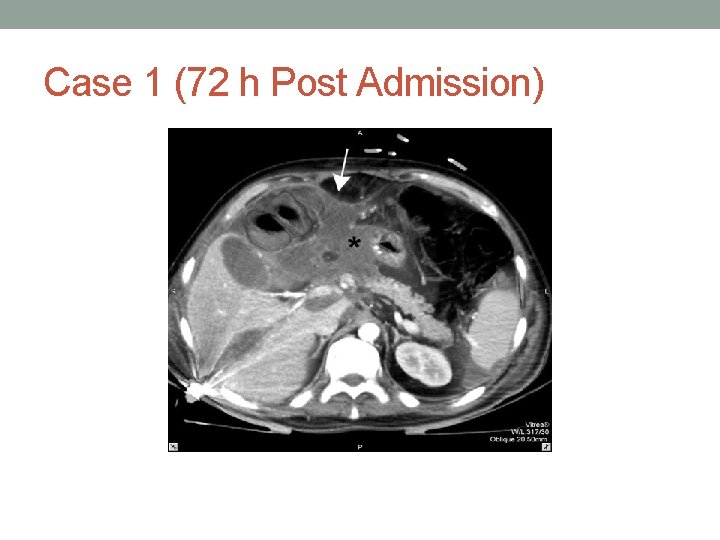
Case 1 • Radiographic Evidence of Necrosis, Significant Peripancreatitic edema/fluid indicate severe pancreatitis • Admission CT may not show necrosis or significant peripancreatic edema
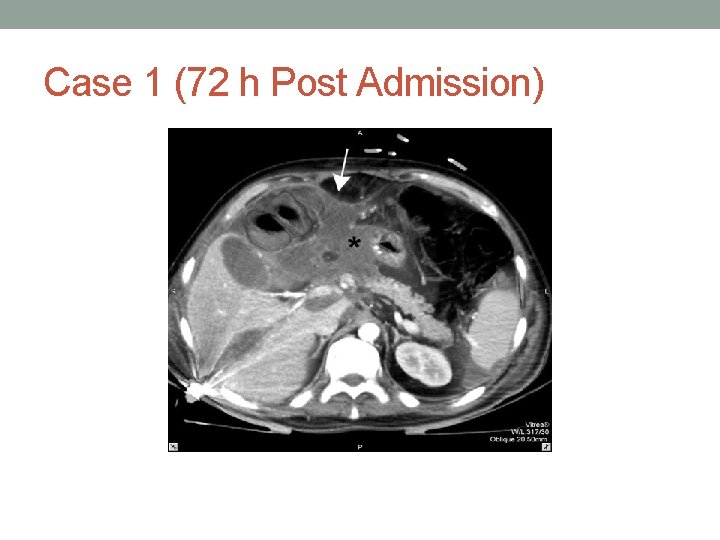
Case 1 (72 h Post Admission)
Case 1 • Severe Pancreatitis based on Ranson’s Criteria and CT • Enteral feeds should be considered for all patients with severe pancreatitis • Feeding should start by 72 h • NG feeds likely acceptable • Semi elemental feeds
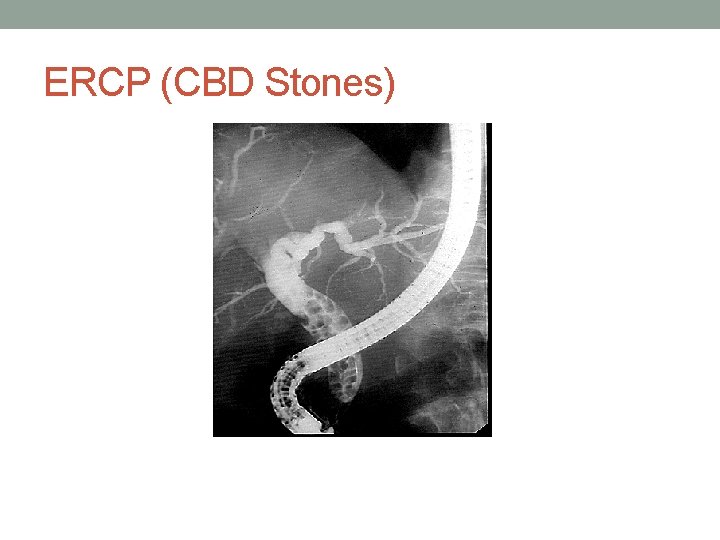
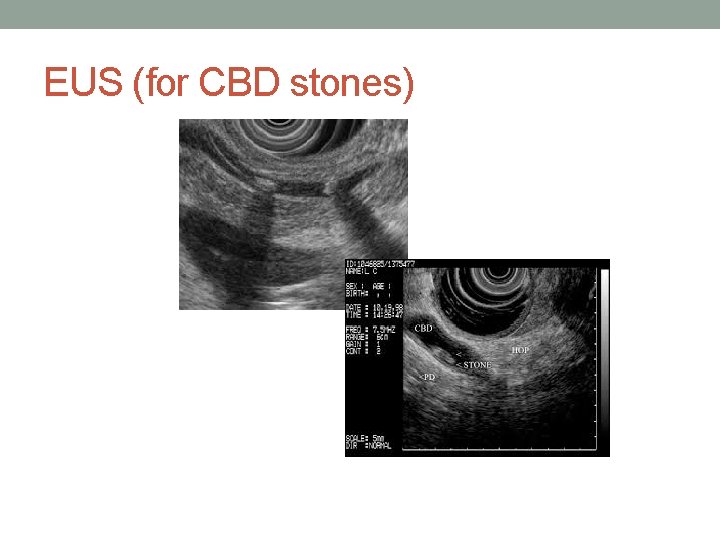
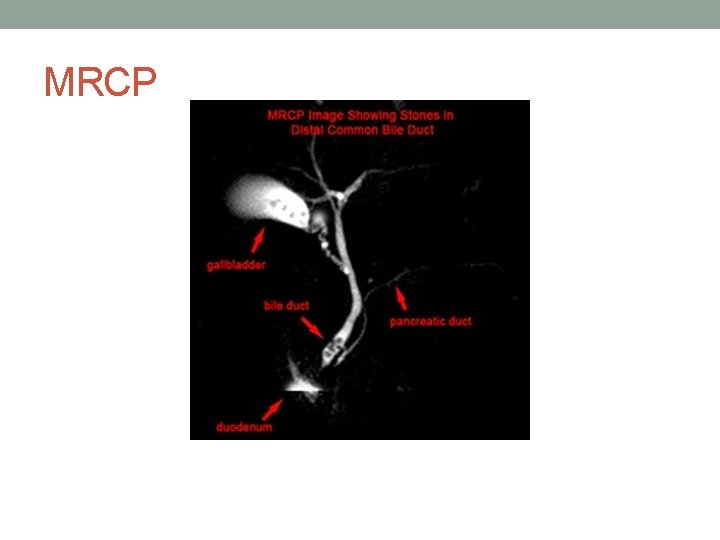
Case 1: Role for ERCP? • ERCP indicated for biliary pancreatitis with jaundice, dilated biliary tree, ascending cholangitis • If risk for stone is low or moderate, less invasive imaging with MRCP or EUS indicated first
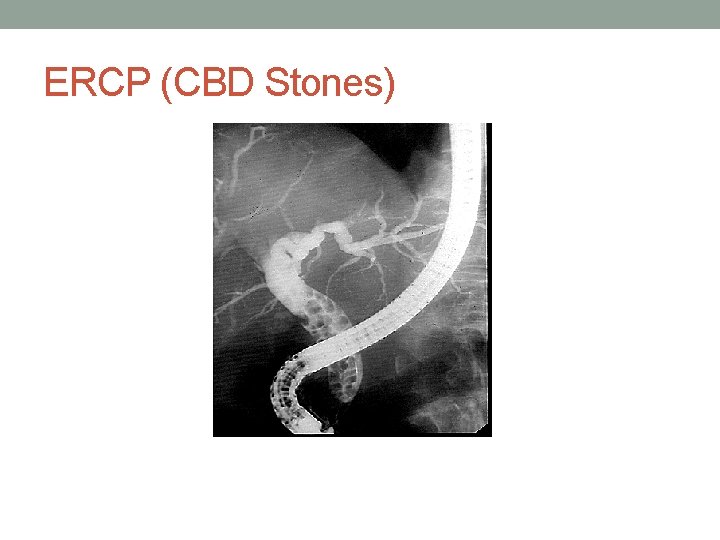
ERCP (CBD Stones)
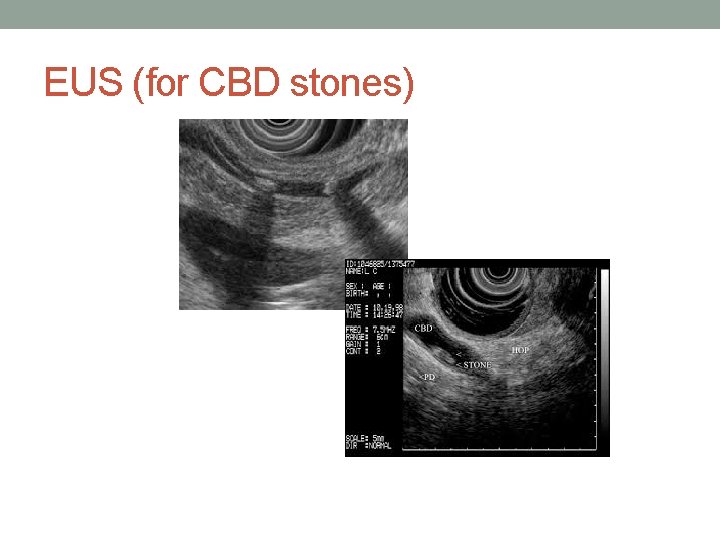
EUS (for CBD stones)
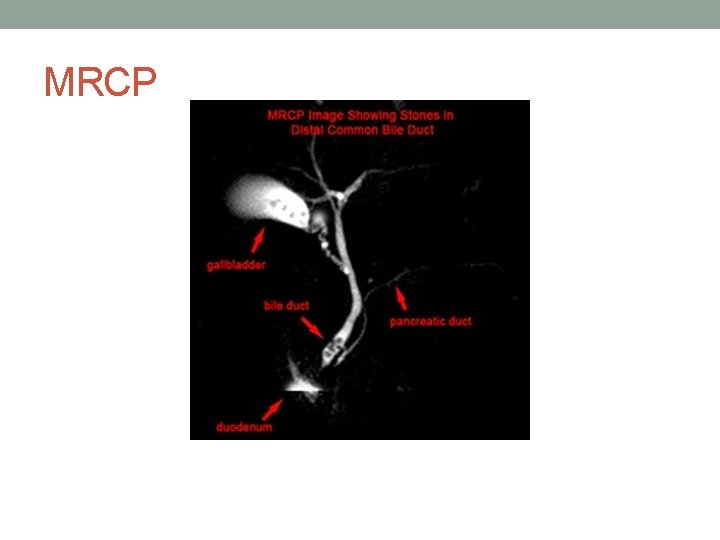
MRCP
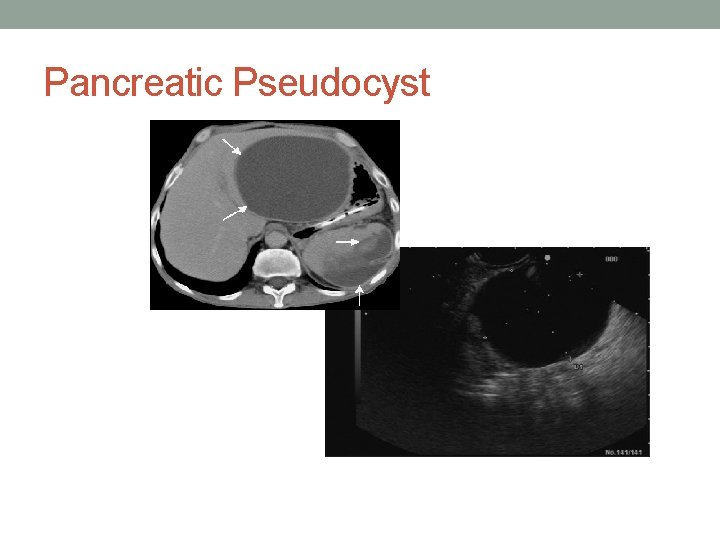
Case 1 • Patient recovers and is discharged • She represents to hospital 2 months later with LUQ pain, early satiety and intermittent emesis. VSS; afebrile • Lab work shows a mild increase in lipase, normal WBC • CT shows a large 9 x 6 cm loculated cyst in the lesser sac compressing the stomach • Diagnosis : Pseudocyst
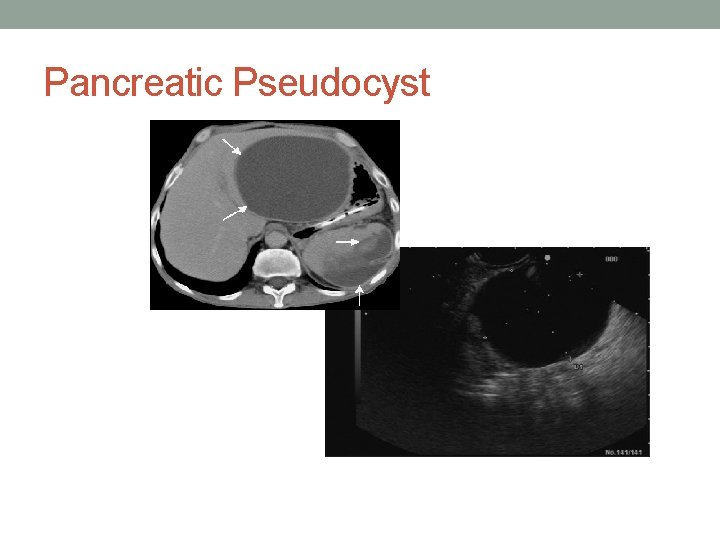
Pancreatic Pseudocyst
Pancreatic Pseudocyst Drainage • Percutaneous Drainage • Endoscopic Drainage ( ERCP v EUS approach) • Surgical
Percutaneous Drainage • Largely historical interest • Used primarily for acutely infected fluid collections • Drainage results poor • Fistula formation
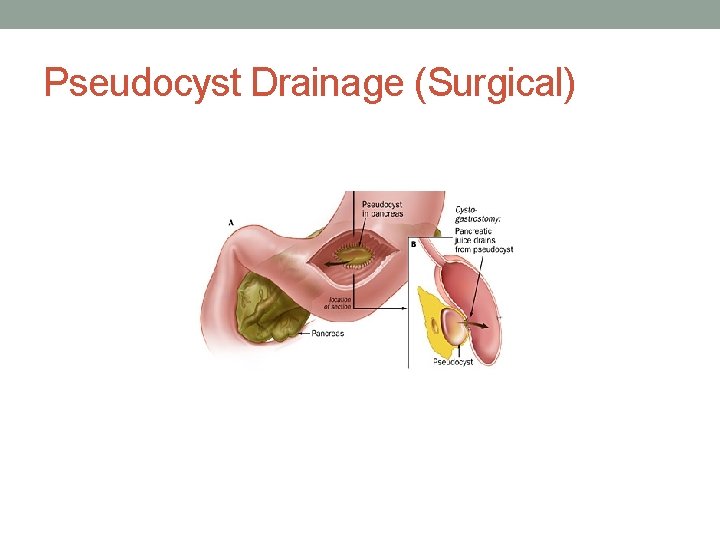
Surgical Drainage • More morbid than endoscopic drainage • Indicated for Complex loculated pseudocysts • Indicated for Cysts not causing bulge in the stomach • Indicated for failed drainage procedures
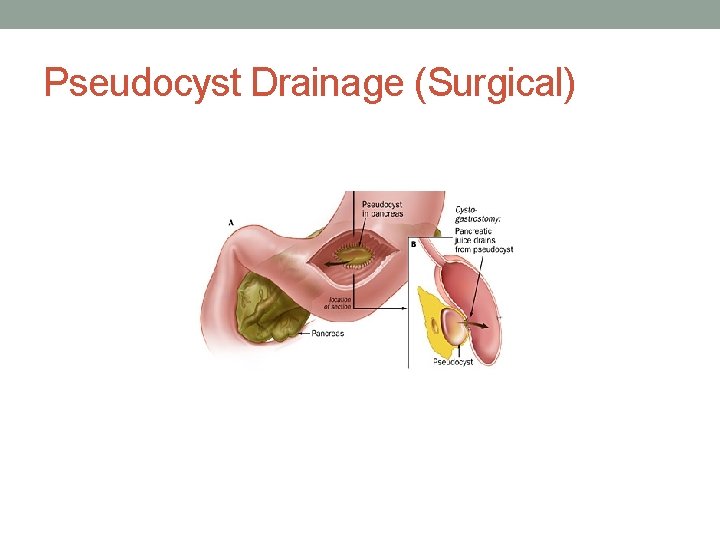
Pseudocyst Drainage (Surgical)
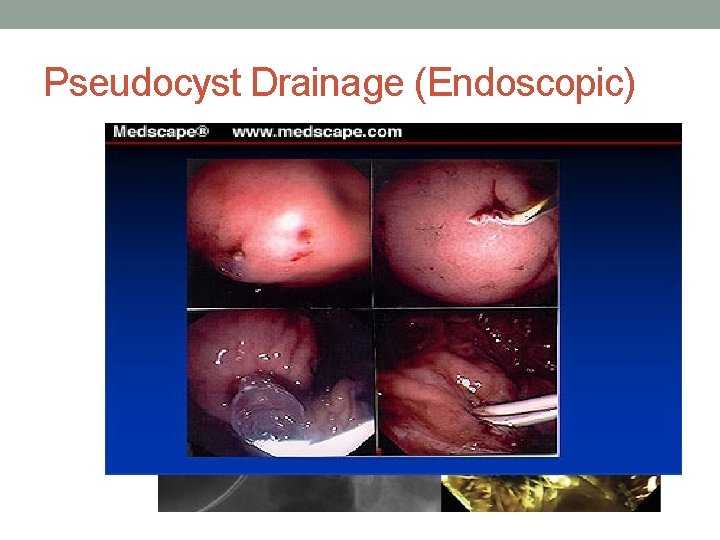
Pseudocyst Drainage ( Endoscopic) • ERCP approach. Needle knife cut followed by placement of double pigtail stents • EUS guided and placement of fully covered metal stent • Echoendoscope is not the ideal scope for pseudocyst draineage
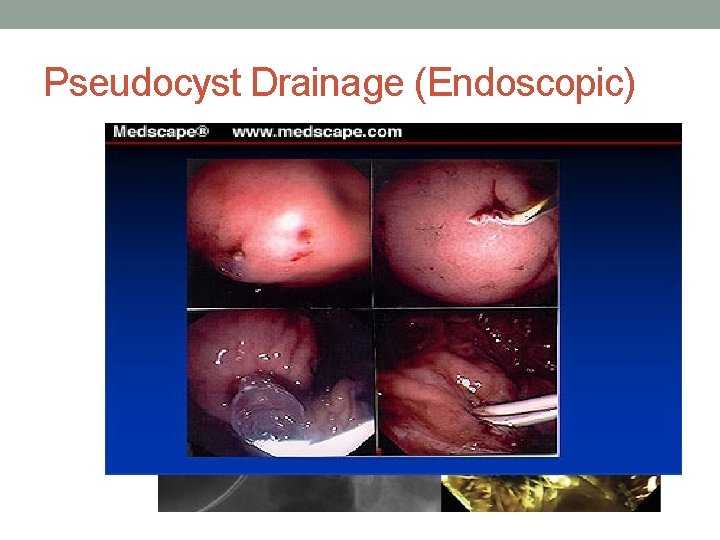
Pseudocyst Drainage (Endoscopic)

Pseudocyst (Endoscopic Drainage)
Acute Pancreatitis Key Points • First 48 h crucial • Aggressive fluid resuscitation required • Urine output should be monitored • Remember DVT prophylaxis • Beware of respiratory compromise and sepsis • Enteral feeding should be started early in SAP • Pseudocyst drainage can often be managed endoscopically
Case 2 • 43 yo man presents with epigastric pain for weeks. Some nausea. No vomiting. • Vitals stable; afebrile • CBC, lytes, BUN/Cr normal. GLU 10. 5 • Lipase 250 • CT Atrophic Pancreas, Numerous Calcifications in Pancreatic parenchyma. No peripancreatic edema or fluid • Dx Acute exacerbation of CP
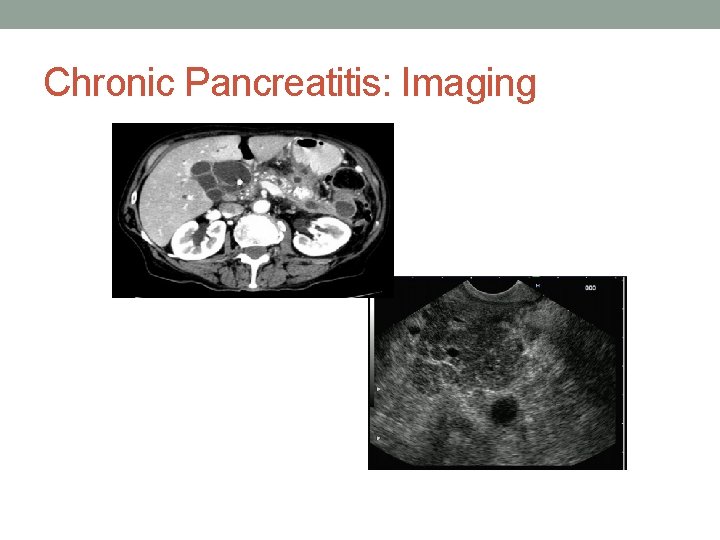
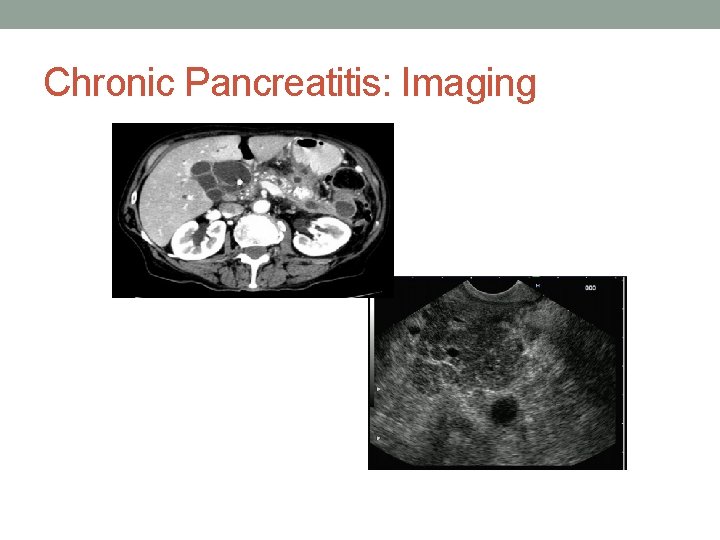
Chronic Pancreatitis: Imaging
Chronic Pancreatitis: Management • IV fluids and analgesics • Little risk of infection, SIRS or respiratory failure • Symptoms usually settle in a few days • Push for Alcohol and smoking cessation • Complications are typically long term such as pancreatic insufficiency, biliary obstruction and cancer • May be a role for pancreatic enzymes for pain control • Minimal role for EUS guided celiac plexus blockade
Chronic Pancreatitis: Risk of Cancer • Well documented increased risk • No surveillance guidelines • Tumour is often difficult to distinguish from focal chronic pancreatitis

Chronic Pancreatitis: Key Points • Hospitalized patients follow a benign course • Management is largely supportive • Priority is to eliminate triggers ( e. g. alcohol and smoking) • Pancreatic enzymes can be used to treat pain or steatorrhea
 Nursing management of chronic pancreatitis
Nursing management of chronic pancreatitis Pancreatitis film
Pancreatitis film Chronic pancreatitis guideline
Chronic pancreatitis guideline Hepatitis a incubation period
Hepatitis a incubation period Chronic pancreatitis
Chronic pancreatitis Cardinal sign of inflammation
Cardinal sign of inflammation Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Morphological pattern of inflammation
Morphological pattern of inflammation Acute and chronic
Acute and chronic Apical periodontitis
Apical periodontitis Pes statement for acute pancreatitis
Pes statement for acute pancreatitis What activates trypsinogen
What activates trypsinogen Ransons criteria
Ransons criteria Acute pancreatitis ct
Acute pancreatitis ct Drrista
Drrista Ranson criteria
Ranson criteria Carnett’s sign
Carnett’s sign Pncreas pain
Pncreas pain Ranson criteria for acute pancreatitis
Ranson criteria for acute pancreatitis Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Acute subacute chronic
Acute subacute chronic Gall bladder drawing
Gall bladder drawing Acute vs chronic heart failure
Acute vs chronic heart failure Flinders model of chronic health disorders
Flinders model of chronic health disorders Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Wagner chronic care model
Wagner chronic care model Nursing care plan for liver cirrhosis
Nursing care plan for liver cirrhosis Santa fe pain and spine
Santa fe pain and spine Pancreatitis and uti
Pancreatitis and uti Criterios de baltazar
Criterios de baltazar Clasificacion de bisap
Clasificacion de bisap Hipocalcemia en pancreatitis
Hipocalcemia en pancreatitis Clasificacion de cambridge pancreatitis cronica
Clasificacion de cambridge pancreatitis cronica Hipocalcemia en pancreatitis
Hipocalcemia en pancreatitis Sofa pancreatitis
Sofa pancreatitis Modified atlanta classification
Modified atlanta classification