Malignant Hyperthermia Catherine Maw 24102012 OUTLINE Define and












- Slides: 34
Malignant Hyperthermia Catherine Maw 24/10/2012
OUTLINE • • • Define and discuss aetiology of thermal disorders Relevance to ICU Clinical Presentation of MH Differential diagnosis and pitfalls Treatment in theatre and ICU Subsequent management
Thermoregulation • Balance between heat production and loss • Hypothalamic thermoregulatory centre • “Pyrexia” = resetting of thermoregulatory set point to a higher level by activation of heat conserving mechanisms • “Hyperthermia” = failure of effector mechanisms to maintain the normal set point

Fever in the ICU • • Regulated hyperthermia Endogenous pyrogens (IL 6 and PGE 2) act on the hypothalamus Reset thermoregulatory set point to higher temp Effector organs prevent heat loss May be protective When pyrogens decrease, set point decreases Deleterious effects (↑CO, O 2 consumption, CO 2 production)
Hyperthermia • Failure of effector mechanisms to maintain the hypothalamic set point (core ≥ 40°C) • Heat stroke • Drug induced hyperthermias (MH, NMS, Serotonin syndrome, sympathomimetic syndrome, anticholinergic syndrome) • Heat injury is the insult • Protein denaturation and lipid dissolution at 42°C (core)
Why is it fatal? • • Direct cellular damage Increases membrane permeability Activation of Na-K-ATPase pump ATP depletion Tissue oedema Cytokine activation, coagulation cascade activation Cellular death (lactate, hyperkalaemia, acidosis) Similar picture to sepsis
Why? • • Metabolic acidosis Hyperkalaemia Rhabdomyolysis Renal failure DIC Liver failure Death
Australian History • • • 1960: Dr Jim Villiers at Royal Melbourne Hospital Patient with 10 family members who died under GA Patient had malignant hyperthermia (MH) Villiers presented the successful anaesthetic outcome 1972: Lancet. Denborough and Lovell. Royal Melbourne (one of 3) centres for MH
Definition and Aetiology • Pharmacological disease of skeletal muscle • Hypermetabolic crisis • Induced by exposure to volatile anaesthetic agents or Suxamethonium • Loss of normal calcium homeostasis • Unregulated release of Calcium form the sarcoplasmic reticulum • Myocyte hypermetabolism
Relevance • • • Anaesthetic complication Ongoing patient care will always involve ICU Insidious versus acute True MH rare Hyperthermia differentials more common
Epidemiology • • • 1 in 10, 000 to 1 in 30, 000 anaesthetics Young adults (45 -55% of cases in <19 years) More frequent in minor ops Male > Female 2: 1 Mortality previously 70 -80% Reduced to 2 -3% now

Genetics of MH • Majority of MH susceptible patients have mutations on RYR 1 or DHP genes • Inherited or spontaneous • 50% Autosomal Dominant • 200 mutations identified • 29 have causality
Pathophysiology ctd • Sustained muscle contraction due to high levels of myoplasmic calcium • Heat generated (initial insult) • Cascade similar to sepsis/systemic inflammation • Initial aerobic metabolism generating CO 2 and → cellular acidosis • Then Oxygen and ATP depletion → worsening acidosis and lactate production • Depleted energy → muscle death and rhabdomyolysis
Risk Factors • • Positive family history Previous exposure to Suxamethonium or volatiles Exertional heat stroke Exercise induced rhabdomyolysis Central core disease Scoliosis Strabismus surgery
Diagnosis
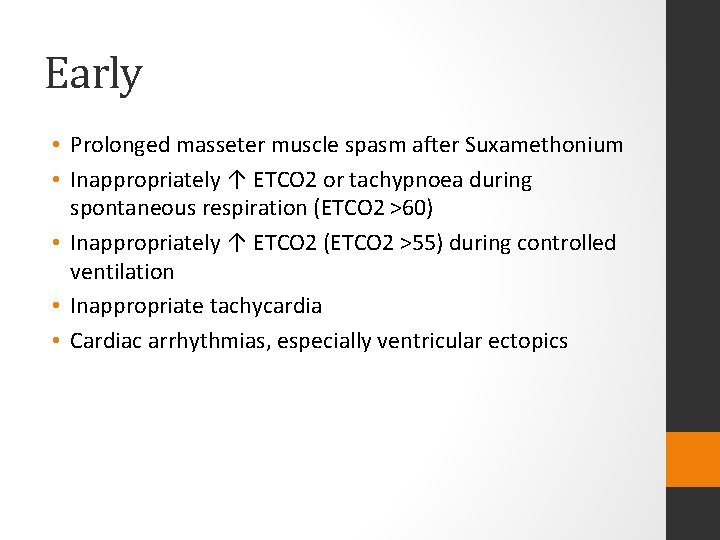
Early • Prolonged masseter muscle spasm after Suxamethonium • Inappropriately ↑ ETCO 2 or tachypnoea during spontaneous respiration (ETCO 2 >60) • Inappropriately ↑ ETCO 2 (ETCO 2 >55) during controlled ventilation • Inappropriate tachycardia • Cardiac arrhythmias, especially ventricular ectopics
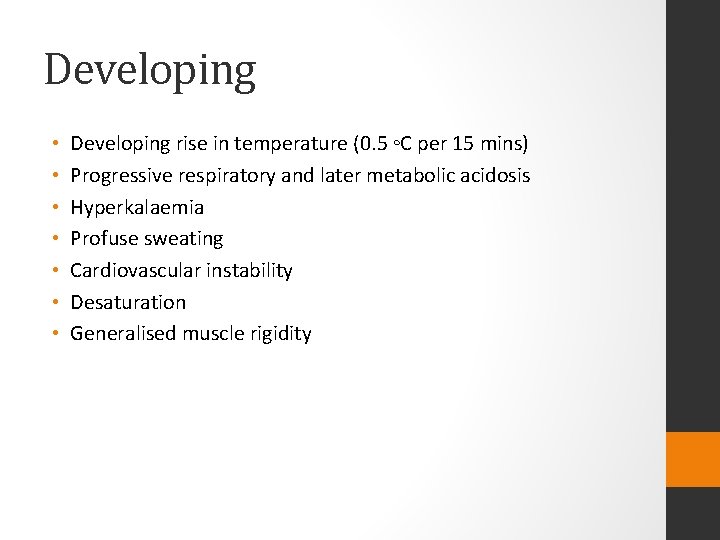
Developing • • Developing rise in temperature (0. 5 ◦C per 15 mins) Progressive respiratory and later metabolic acidosis Hyperkalaemia Profuse sweating Cardiovascular instability Desaturation Generalised muscle rigidity
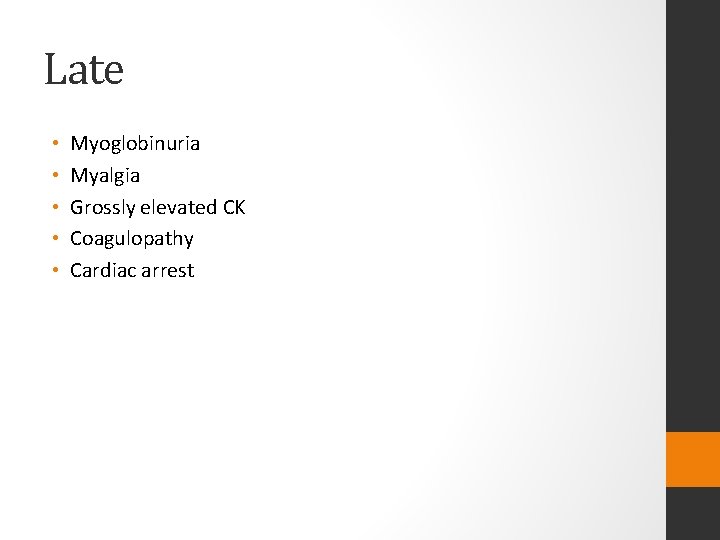
Late • • • Myoglobinuria Myalgia Grossly elevated CK Coagulopathy Cardiac arrest
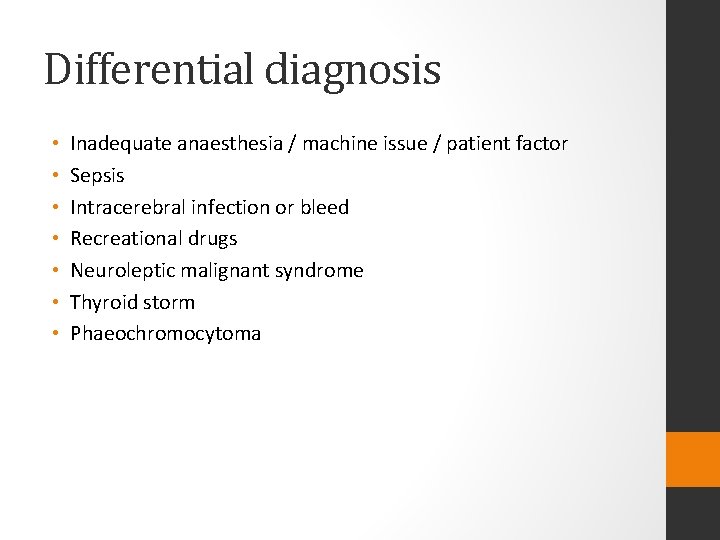
Differential diagnosis • • Inadequate anaesthesia / machine issue / patient factor Sepsis Intracerebral infection or bleed Recreational drugs Neuroleptic malignant syndrome Thyroid storm Phaeochromocytoma
Management • • • ANZCA suggest MH Resource kit Link to mhanz Task cards based on the aviation safety model If diagnosis is suspected: Declare Emergency Call for HELP and send for MH resource kit Turn off the volatile and remove vaporisers Hyperventilate on >15 l/min fresh gas flows with 100% O 2 TIVA








Ongoing Care • ICU for ventilatory support, haemodynamic monitoring, renal support • CK peaks at 14 hours • Dantrolene does not effect cardiac or smooth muscle • Recrudescence in 25% • 1 mg/kg Dantrolene every 6 hours for 48 hours
MH Susceptibility Testing • Gold standard is the contracture test • In vitro response of a fresh sample of muscle tissue to Caffeine or Halothane • Muscle strip in physiological solution is attached to a strain gauge and electrically stimulated to measure baseline tension • Repeat in Halothane and Caffeine • High sensitivity and specificity • Expensive and specialist referral needed • Genetic testing cheaper but sensitivity 30 -50%


 Hyperthermia causes
Hyperthermia causes Barriere model
Barriere model Kernconcepten maw
Kernconcepten maw What does o mischief thou art swift mean
What does o mischief thou art swift mean Rationele actor paradigma
Rationele actor paradigma Ar armaturen
Ar armaturen Tan maw pin
Tan maw pin Malignant and benign tumors
Malignant and benign tumors Liposarcoma
Liposarcoma Benign and malignant tumor
Benign and malignant tumor Benign or malignant
Benign or malignant Malignant neuroleptic syndrome
Malignant neuroleptic syndrome Risk factors for malignant melanoma
Risk factors for malignant melanoma Malignant hypertension management
Malignant hypertension management Kitwood flower of needs
Kitwood flower of needs Neuroleptic malignant syndrome
Neuroleptic malignant syndrome Hypokalemia
Hypokalemia Malignant hypertension treatment
Malignant hypertension treatment Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Malignant mesothelioma
Malignant mesothelioma Malignant neoplasm of liver
Malignant neoplasm of liver Carcinoma in situ
Carcinoma in situ Neuroleptic malignant syndrome mnemonic
Neuroleptic malignant syndrome mnemonic Hypertensive emergency definition
Hypertensive emergency definition Histological features of malignant cells
Histological features of malignant cells Hematocrit
Hematocrit Calcium channel blockers examples
Calcium channel blockers examples Example of topic outline and sentence outline
Example of topic outline and sentence outline Business accounting and finance catherine gowthorpe
Business accounting and finance catherine gowthorpe Wuthering heights chapter 23 summary
Wuthering heights chapter 23 summary Catherine olivieri
Catherine olivieri The six wives of henry viii
The six wives of henry viii Catherine cook entrepreneur
Catherine cook entrepreneur Catherine armand
Catherine armand Catherine moynihan
Catherine moynihan