Malignant hyperthermia Dr S Spijkerman Pathogenesis Pharmacogenetic disorder
- Slides: 11
Malignant hyperthermia Dr S Spijkerman
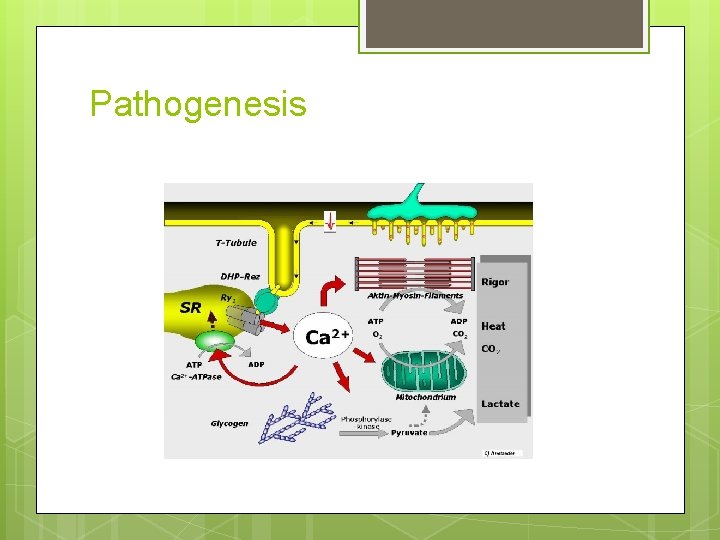
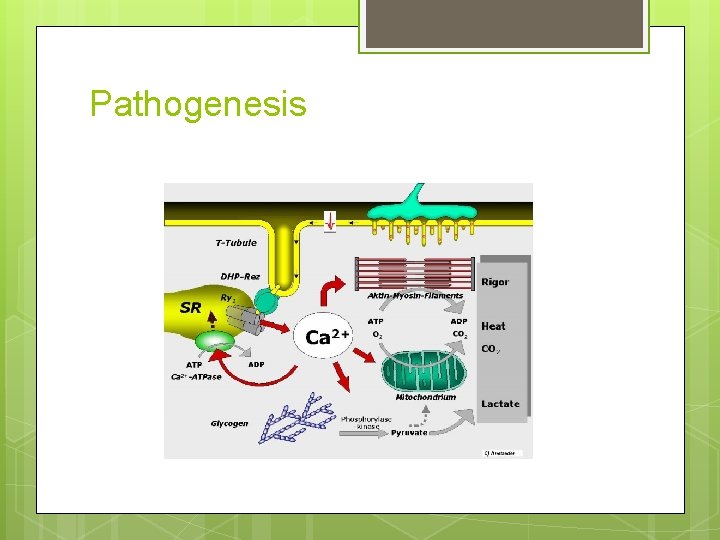
Pathogenesis
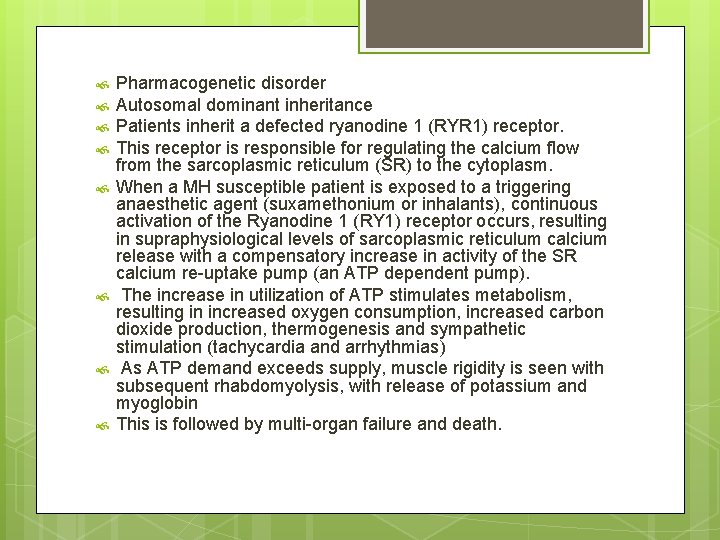
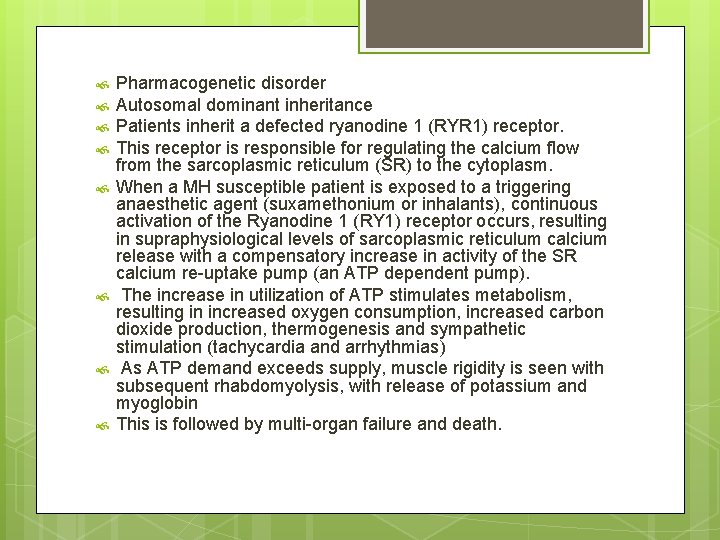
Pharmacogenetic disorder Autosomal dominant inheritance Patients inherit a defected ryanodine 1 (RYR 1) receptor. This receptor is responsible for regulating the calcium flow from the sarcoplasmic reticulum (SR) to the cytoplasm. When a MH susceptible patient is exposed to a triggering anaesthetic agent (suxamethonium or inhalants), continuous activation of the Ryanodine 1 (RY 1) receptor occurs, resulting in supraphysiological levels of sarcoplasmic reticulum calcium release with a compensatory increase in activity of the SR calcium re-uptake pump (an ATP dependent pump). The increase in utilization of ATP stimulates metabolism, resulting in increased oxygen consumption, increased carbon dioxide production, thermogenesis and sympathetic stimulation (tachycardia and arrhythmias) As ATP demand exceeds supply, muscle rigidity is seen with subsequent rhabdomyolysis, with release of potassium and myoglobin This is followed by multi-organ failure and death.
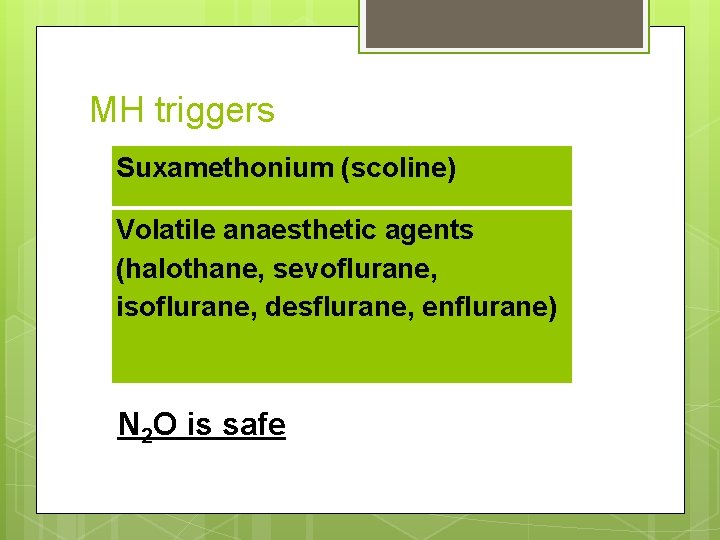
MH triggers Suxamethonium (scoline) Volatile anaesthetic agents (halothane, sevoflurane, isoflurane, desflurane, enflurane) N 2 O is safe
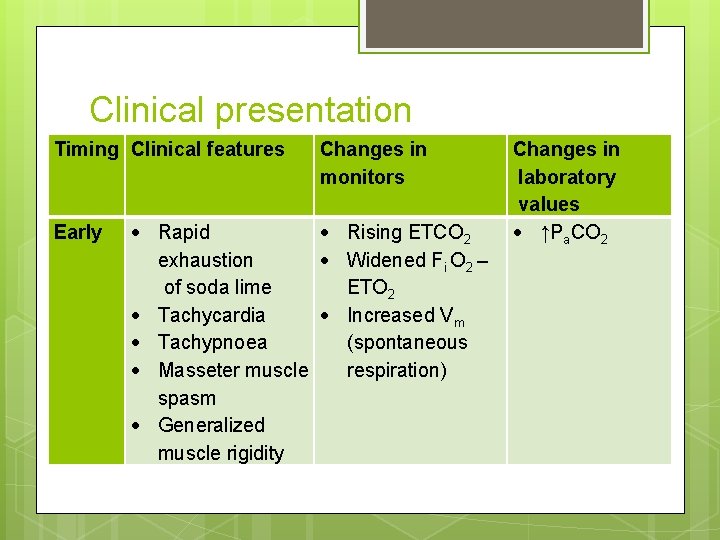
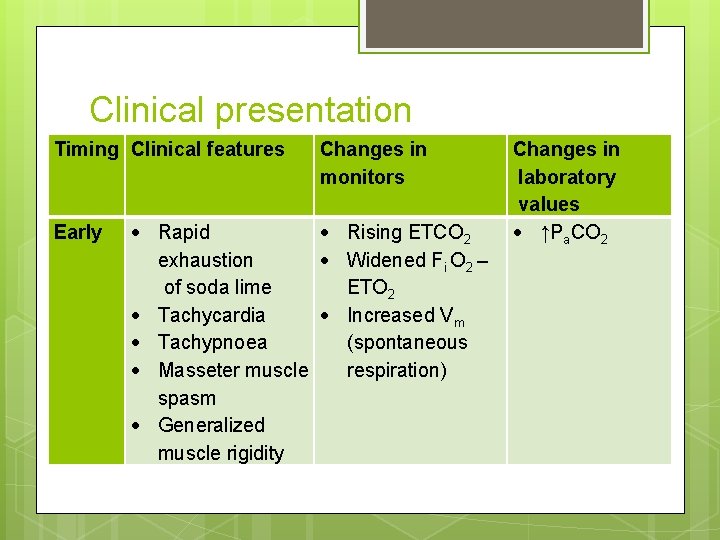
Clinical presentation Timing Clinical features Early Changes in monitors Rapid exhaustion of soda lime Tachycardia Tachypnoea Masseter muscle spasm Generalized muscle rigidity Rising ETCO 2 Widened Fi O 2 – ETO 2 Increased Vm (spontaneous respiration) Changes in laboratory values ↑Pa. CO 2
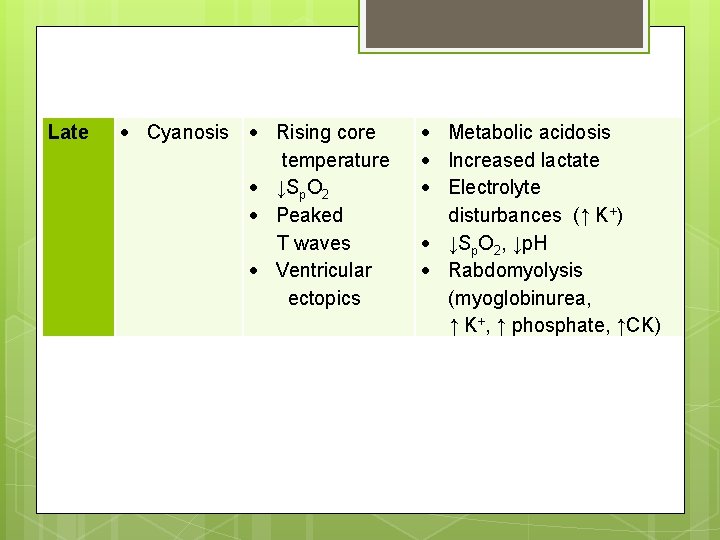
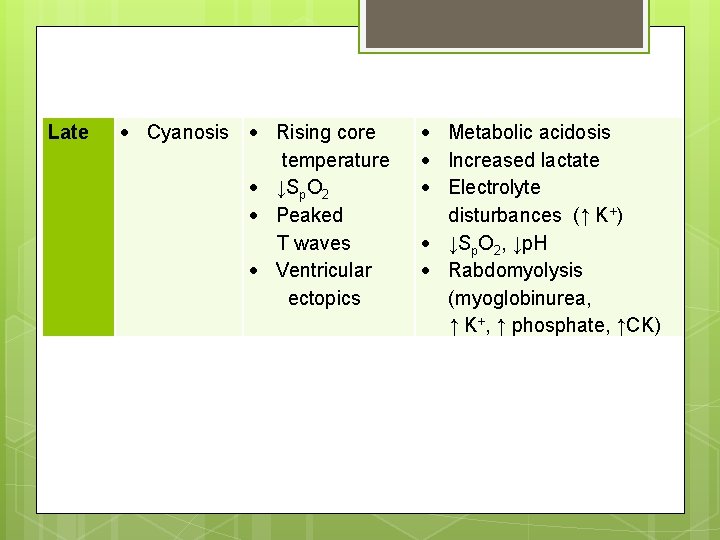
Late Cyanosis Rising core temperature ↓Sp. O 2 Peaked T waves Ventricular ectopics Metabolic acidosis Increased lactate Electrolyte disturbances (↑ K+) ↓Sp. O 2, ↓p. H Rabdomyolysis (myoglobinurea, ↑ K+, ↑ phosphate, ↑CK)
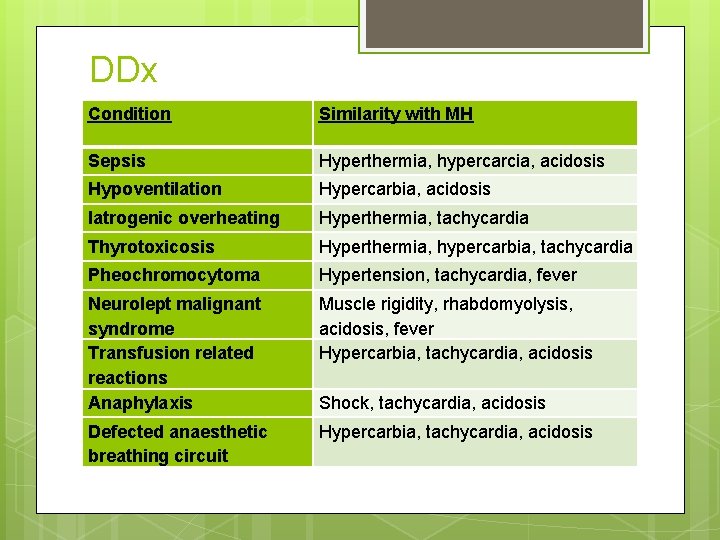
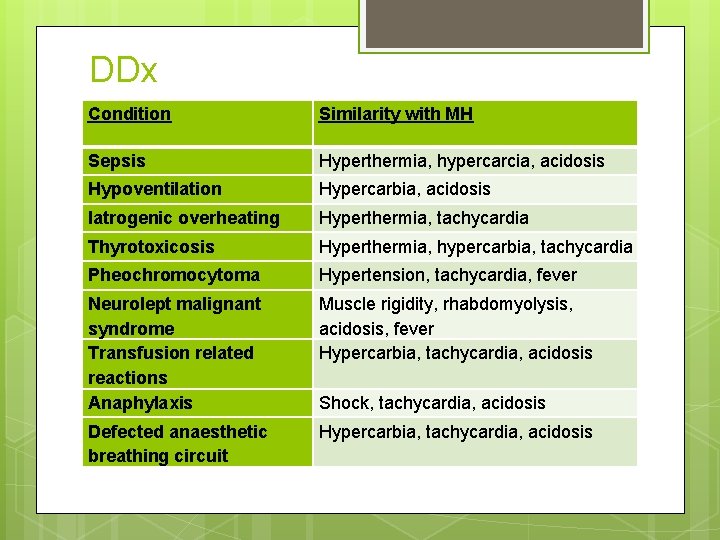
DDx Condition Similarity with MH Sepsis Hyperthermia, hypercarcia, acidosis Hypoventilation Hypercarbia, acidosis Iatrogenic overheating Hyperthermia, tachycardia Thyrotoxicosis Hyperthermia, hypercarbia, tachycardia Pheochromocytoma Hypertension, tachycardia, fever Neurolept malignant syndrome Transfusion related reactions Anaphylaxis Muscle rigidity, rhabdomyolysis, acidosis, fever Hypercarbia, tachycardia, acidosis Defected anaesthetic breathing circuit Hypercarbia, tachycardia, acidosis Shock, tachycardia, acidosis
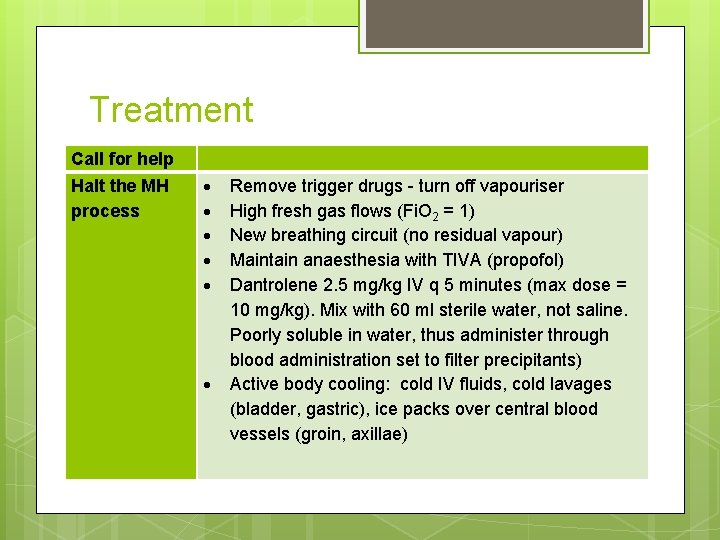
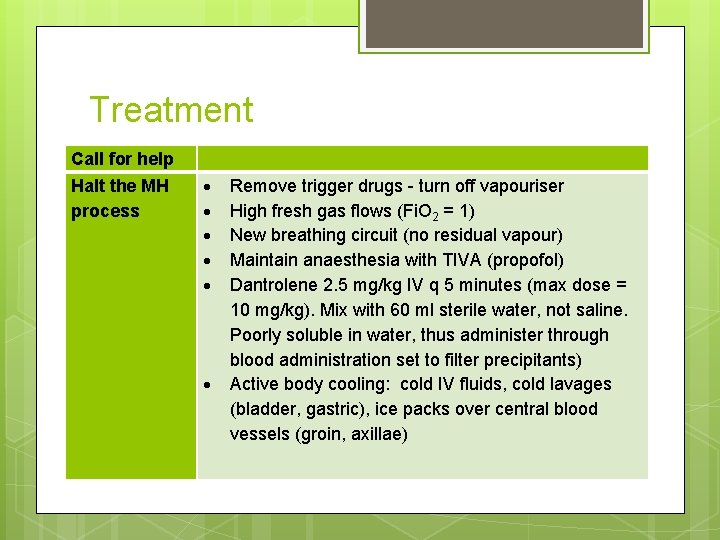
Treatment Call for help Halt the MH process Remove trigger drugs - turn off vapouriser High fresh gas flows (Fi. O 2 = 1) New breathing circuit (no residual vapour) Maintain anaesthesia with TIVA (propofol) Dantrolene 2. 5 mg/kg IV q 5 minutes (max dose = 10 mg/kg). Mix with 60 ml sterile water, not saline. Poorly soluble in water, thus administer through blood administration set to filter precipitants) Active body cooling: cold IV fluids, cold lavages (bladder, gastric), ice packs over central blood vessels (groin, axillae)
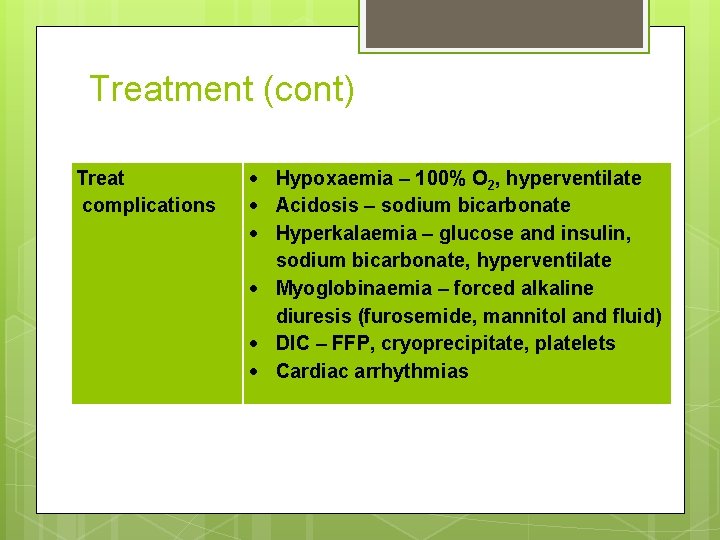
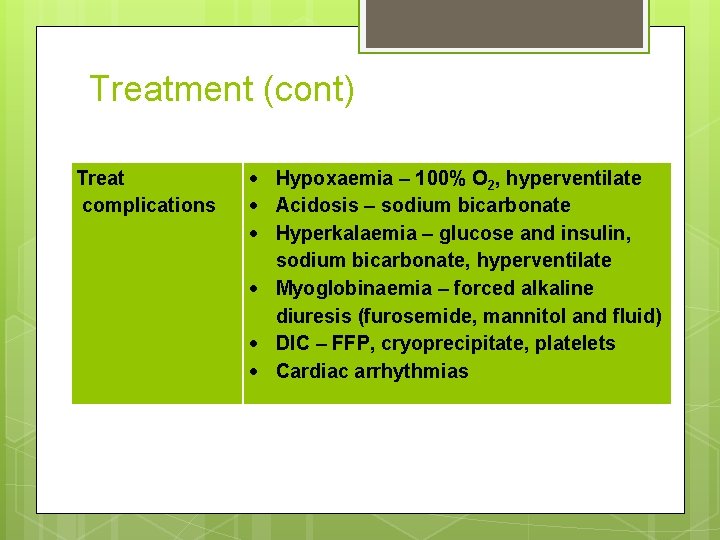
Treatment (cont) Treat complications Hypoxaemia – 100% O 2, hyperventilate Acidosis – sodium bicarbonate Hyperkalaemia – glucose and insulin, sodium bicarbonate, hyperventilate Myoglobinaemia – forced alkaline diuresis (furosemide, mannitol and fluid) DIC – FFP, cryoprecipitate, platelets Cardiac arrhythmias
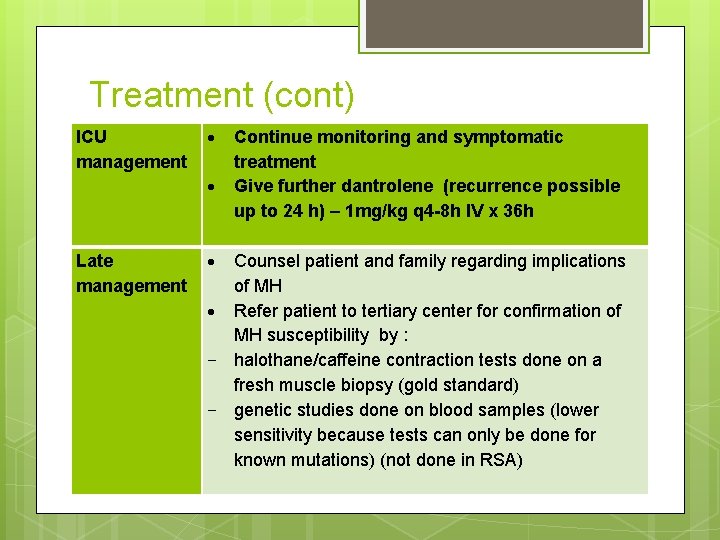
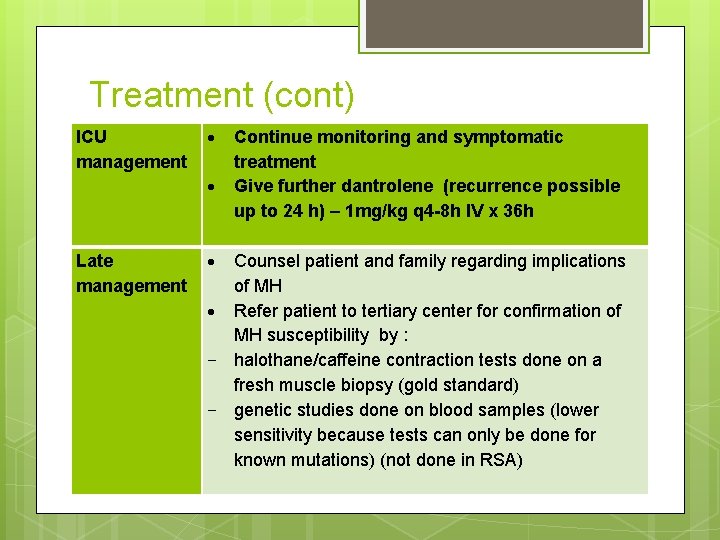
Treatment (cont) ICU management Late management Continue monitoring and symptomatic treatment Give further dantrolene (recurrence possible up to 24 h) – 1 mg/kg q 4 -8 h IV x 36 h Counsel patient and family regarding implications of MH Refer patient to tertiary center for confirmation of MH susceptibility by : - halothane/caffeine contraction tests done on a fresh muscle biopsy (gold standard) - genetic studies done on blood samples (lower sensitivity because tests can only be done for known mutations) (not done in RSA)
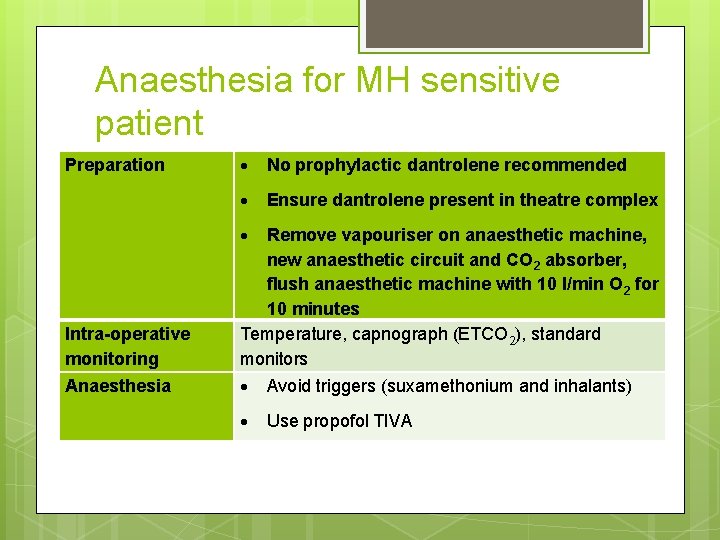
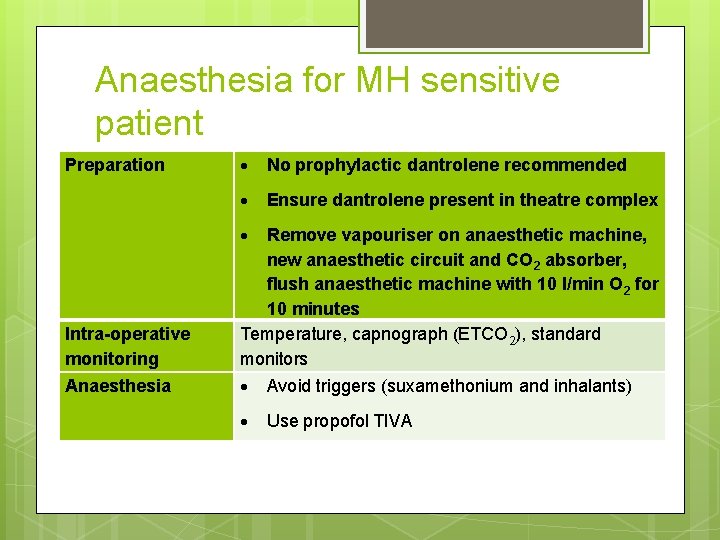
Anaesthesia for MH sensitive patient Preparation No prophylactic dantrolene recommended Ensure dantrolene present in theatre complex Intra-operative monitoring Remove vapouriser on anaesthetic machine, new anaesthetic circuit and CO 2 absorber, flush anaesthetic machine with 10 l/min O 2 for 10 minutes Temperature, capnograph (ETCO 2), standard monitors Anaesthesia Avoid triggers (suxamethonium and inhalants) Use propofol TIVA